c5e6af71bd653dc68f293ea8d422ca83.ppt
- Количество слайдов: 17
Barry Reisberg, M. D. Professor of Psychiatry Director, Fisher Alzheimer's Disease Program Clinical Director, Aging & Dementia Research Center Director, Clinical Core, NYU Alzheimer's Disease Center New York University School of Medicine
Agenda 3: 00 PM Introduction to Workshop Barry Reisberg, M. D. 3: 05 PM Cognitive dynamics: how variability in brain function influences the risk of cognitive decline Kenneth Rockwood M. D. , FRCPC, FRCP 3: 35 PM Current Knowledge of Methodologies for Clinical Trials in Pre-MCI Persons with Subjective Cognitive Impairment (SCI) Barry Reisberg, M. D. 4: 25 PM Discussion of Current Knowledge and Methodologies Joel Sadavoy M. D. , FRCPC 4: 35 PM Discussion of Clinical Instrumentation for Subject Selection and Assessment Barry Reisberg, M. D. 4: 55 PM Subject Interview Workshop Faculty and Participants 5: 25 PM Final Discussion Joel Sadavoy M. D. , FRCPC
GLOBAL DETERIORATION SCALE (GDS) Stage 1 1. No subjective complaints of memory deficit. No memory deficit evident on clinical interview.
GLOBAL DETERIORATION SCALE (GDS) Stage 2 2. Subjective complaints of memory deficit, most frequently in following areas: (a) forgetting where one has placed familiar objects; (b) forgetting names one formerly knew well. No objective evidence of memory deficit on clinical interview. No objective deficit in employment or social situations. Appropriate concern with respect to symptomatology.
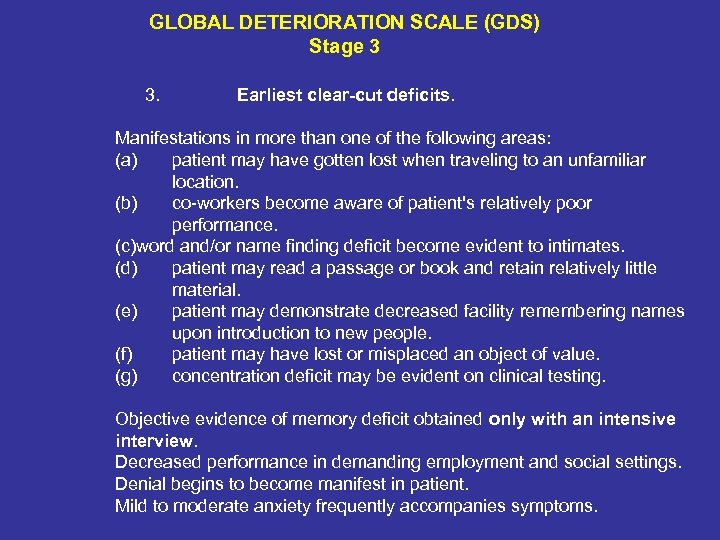
GLOBAL DETERIORATION SCALE (GDS) Stage 3 3. Earliest clear-cut deficits. Manifestations in more than one of the following areas: (a) patient may have gotten lost when traveling to an unfamiliar location. (b) co-workers become aware of patient's relatively poor performance. (c)word and/or name finding deficit become evident to intimates. (d) patient may read a passage or book and retain relatively little material. (e) patient may demonstrate decreased facility remembering names upon introduction to new people. (f) patient may have lost or misplaced an object of value. (g) concentration deficit may be evident on clinical testing. Objective evidence of memory deficit obtained only with an intensive interview. Decreased performance in demanding employment and social settings. Denial begins to become manifest in patient. Mild to moderate anxiety frequently accompanies symptoms.

Abridged Global Deterioration Scale Stage 1 No subjective memory deficit (no cognitive impairment); no problems with activities of daily living Stage 2 Subjective memory complaints (subjective cognitive impairment): Complaints of being forgetful, such as complaints of trouble with recall of names, complaints of misplacing objects Stage 3 Earliest clear deficits (mild cognitive impairment): Difficulties often noted at work; may have gotten lost; may have misplaced a valuable object Stage 4 Clear deficits on clinical examination (moderate cognitive impairment): Decreased knowledge of personal and/or current events; often trouble with travel and finances Stage 5 Can no longer survive independently in the community without some assistance (moderately severe cognitive impairment): Difficulty with recall of some important personal details (e. g. , address, names of one or more important schools attended); may require cuing for activities of daily living Stage 6 Largely unable to verbalize recent events in their life (severe cognitive impairment): May forget name of spouse; incontinence develops as this stage progresses; requires increasing assistance with activities of daily living; increased behavioral problems (e. g. , agitation, delusions) Stage 7 Few intelligible words or no verbal abilities (very severe cognitive impairment): Loses the ability to walk as this stage evolves Copyright © 2008 Barry Reisberg, M. D. All rights reserved. Abridged version published in Canadian Medical Association Journal, 2008; 179 (12); p. 1281. Modified from Reisberg, B. , Ferris, S. H. , de Leon, M. J, et al. The global deterioration scale for assessment of primary degenerative dementia. Am J Psychiatry, 1982; 139: 1136 -1139.
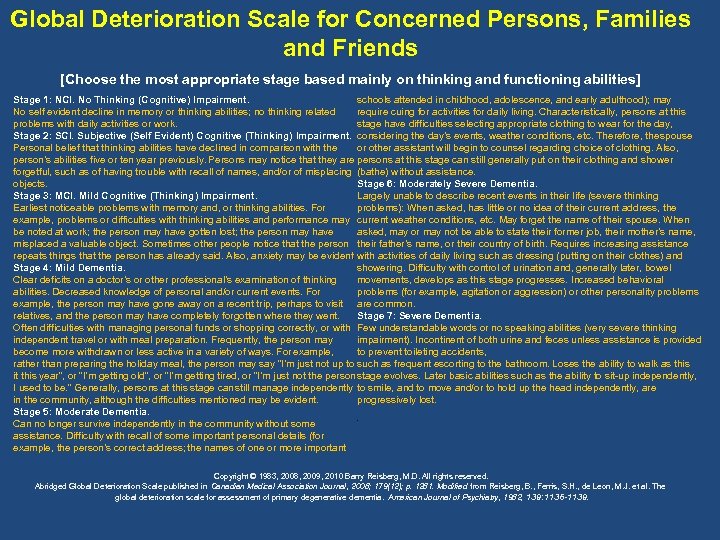
Global Deterioration Scale for Concerned Persons, Families and Friends [Choose the most appropriate stage based mainly on thinking and functioning abilities] Stage 1: NCI. No Thinking (Cognitive) Impairment. schools attended in childhood, adolescence, and early adulthood); may No self evident decline in memory or thinking abilities; no thinking related require cuing for activities for daily living. Characteristically, persons at this problems with daily activities or work. stage have difficulties selecting appropriate clothing to wear for the day, Stage 2: SCI. Subjective (Self Evident) Cognitive (Thinking) Impairment. considering the day’s events, weather conditions, etc. Therefore, the spouse Personal belief that thinking abilities have declined in comparison with the or other assistant will begin to counsel regarding choice of clothing. Also, person’s abilities five or ten year previously. Persons may notice that they are persons at this stage can still generally put on their clothing and shower forgetful, such as of having trouble with recall of names, and/or of misplacing (bathe) without assistance. objects. Stage 6: Moderately Severe Dementia. Stage 3: MCI. Mild Cognitive (Thinking) Impairment. Largely unable to describe recent events in their life (severe thinking Earliest noticeable problems with memory and, or thinking abilities. For problems): When asked, has little or no idea of their current address, the example, problems or difficulties with thinking abilities and performance may current weather conditions, etc. May forget the name of their spouse. When be noted at work; the person may have gotten lost; the person may have asked, may or may not be able to state their former job, their mother’s name, misplaced a valuable object. Sometimes other people notice that the person their father’s name, or their country of birth. Requires increasing assistance repeats things that the person has already said. Also, anxiety may be evident with activities of daily living such as dressing (putting on their clothes) and . showering. Difficulty with control of urination and, generally later, bowel Stage 4: Mild Dementia. movements, develops as this stage progresses. Increased behavioral Clear deficits on a doctor’s or other professional’s examination of thinking problems (for example, agitation or aggression) or other personality problems abilities. Decreased knowledge of personal and/or current events. For example, the person may have gone away on a recent trip, perhaps to visit are common. relatives, and the person may have completely forgotten where they went. Stage 7: Severe Dementia. Often difficulties with managing personal funds or shopping correctly, or with Few understandable words or no speaking abilities (very severe thinking impairment). Incontinent of both urine and feces unless assistance is provided independent travel or with meal preparation. Frequently, the person may to prevent toileting accidents, become more withdrawn or less active in a variety of ways. For example, rather than preparing the holiday meal, the person may say “I’m just not up to such as frequent escorting to the bathroom. Loses the ability to walk as this it this year”, or “I’m getting old”, or “I’m getting tired, or “I’m just not the person stage evolves. Later basic abilities such as the ability to sit-up independently, I used to be. ” Generally, persons at this stage can still manage independently to smile, and to move and/or to hold up the head independently, are progressively lost. in the community, although the difficulties mentioned may be evident. Stage 5: Moderate Dementia. Can no longer survive independently in the community without some assistance. Difficulty with recall of some important personal details (for example, the person’s correct address; the names of one or more important . Copyright © 1983, 2008, 2009, 2010 Barry Reisberg, M. D. All rights reserved. Abridged Global Deterioration Scale published in Canadian Medical Association Journal , 2008; 179(12); p. 1281. Modified from Reisberg, B. , Ferris, S. H. , de Leon, M. J. et al. The global deterioration scale for assessment of primary degenerative dementia. American Journal of Psychiatry, 1982, 139: 1136 -1139.
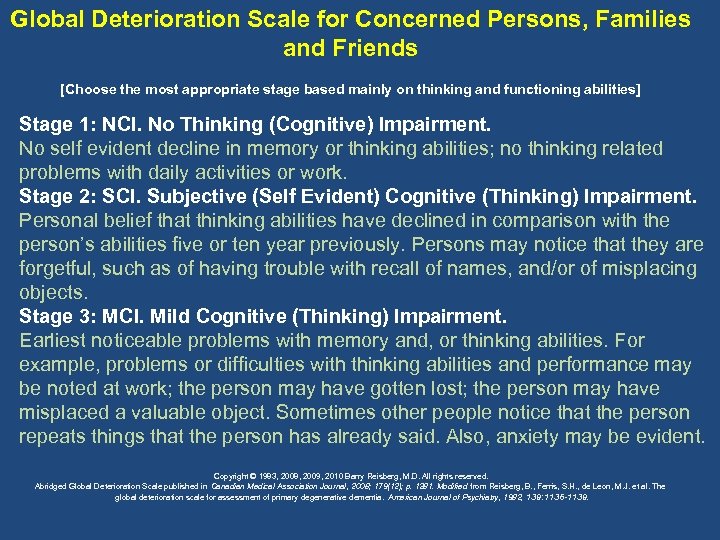
Global Deterioration Scale for Concerned Persons, Families and Friends [Choose the most appropriate stage based mainly on thinking and functioning abilities] Stage 1: NCI. No Thinking (Cognitive) Impairment. No self evident decline in memory or thinking abilities; no thinking related problems with daily activities or work. Stage 2: SCI. Subjective (Self Evident) Cognitive (Thinking) Impairment. Personal belief that thinking abilities have declined in comparison with the person’s abilities five or ten year previously. Persons may notice that they are forgetful, such as of having trouble with recall of names, and/or of misplacing objects. Stage 3: MCI. Mild Cognitive (Thinking) Impairment. Earliest noticeable problems with memory and, or thinking abilities. For example, problems or difficulties with thinking abilities and performance may be noted at work; the person may have gotten lost; the person may have misplaced a valuable object. Sometimes other people notice that the person repeats things that the person has already said. Also, anxiety may be evident. Copyright © 1983, 2008, 2009, 2010 Barry Reisberg, M. D. All rights reserved. Abridged Global Deterioration Scale published in Canadian Medical Association Journal , 2008; 179(12); p. 1281. Modified from Reisberg, B. , Ferris, S. H. , de Leon, M. J. et al. The global deterioration scale for assessment of primary degenerative dementia. American Journal of Psychiatry, 1982, 139: 1136 -1139.
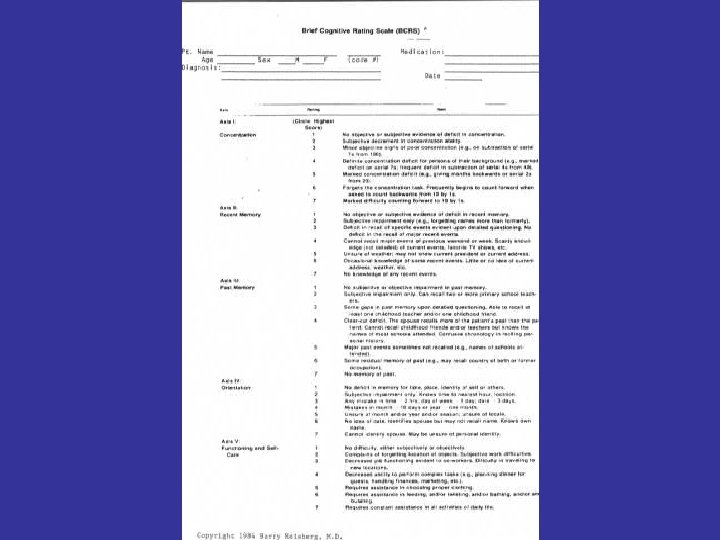
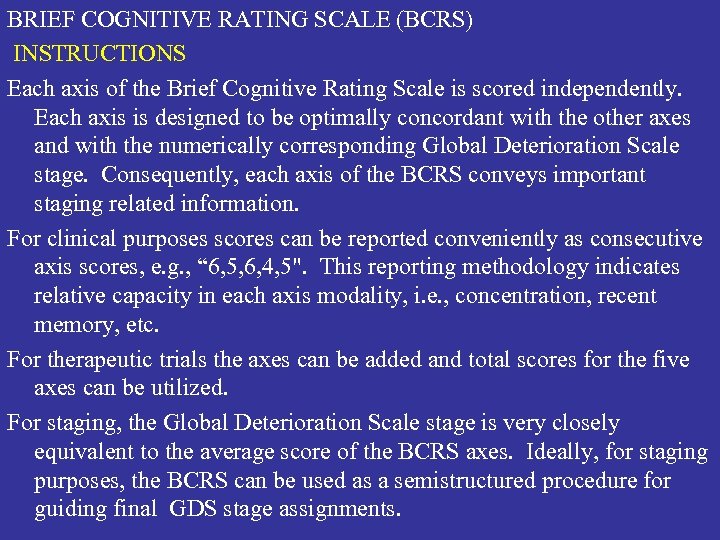
BRIEF COGNITIVE RATING SCALE (BCRS) INSTRUCTIONS Each axis of the Brief Cognitive Rating Scale is scored independently. Each axis is designed to be optimally concordant with the other axes and with the numerically corresponding Global Deterioration Scale stage. Consequently, each axis of the BCRS conveys important staging related information. For clinical purposes scores can be reported conveniently as consecutive axis scores, e. g. , “ 6, 5, 6, 4, 5". This reporting methodology indicates relative capacity in each axis modality, i. e. , concentration, recent memory, etc. For therapeutic trials the axes can be added and total scores for the five axes can be utilized. For staging, the Global Deterioration Scale stage is very closely equivalent to the average score of the BCRS axes. Ideally, for staging purposes, the BCRS can be used as a semistructured procedure for guiding final GDS stage assignments.
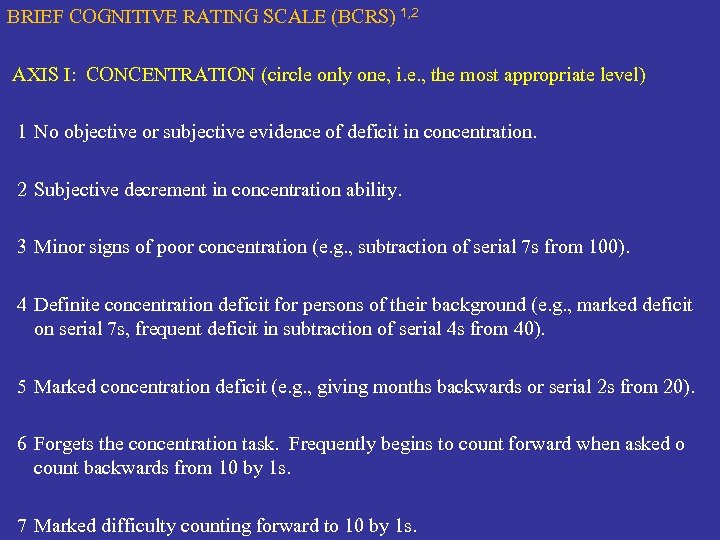
BRIEF COGNITIVE RATING SCALE (BCRS) 1, 2 AXIS I: CONCENTRATION (circle only one, i. e. , the most appropriate level) 1 2 3 4 No objective or subjective evidence of deficit in concentration. Subjective decrement in concentration ability. Minor signs of poor concentration (e. g. , subtraction of serial 7 s from 100). Definite concentration deficit for persons of their background (e. g. , marked deficit on serial 7 s, frequent deficit in subtraction of serial 4 s from 40). 5 Marked concentration deficit (e. g. , giving months backwards or serial 2 s from 20). 6 Forgets the concentration task. Frequently begins to count forward when asked o count backwards from 10 by 1 s. 7 Marked difficulty counting forward to 10 by 1 s.
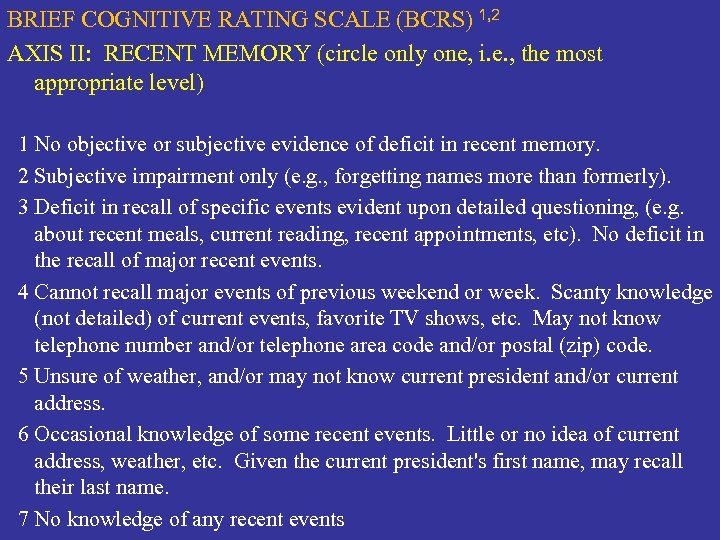
BRIEF COGNITIVE RATING SCALE (BCRS) 1, 2 AXIS II: RECENT MEMORY (circle only one, i. e. , the most appropriate level) 1 No objective or subjective evidence of deficit in recent memory. 2 Subjective impairment only (e. g. , forgetting names more than formerly). 3 Deficit in recall of specific events evident upon detailed questioning, (e. g. about recent meals, current reading, recent appointments, etc). No deficit in the recall of major recent events. 4 Cannot recall major events of previous weekend or week. Scanty knowledge (not detailed) of current events, favorite TV shows, etc. May not know telephone number and/or telephone area code and/or postal (zip) code. 5 Unsure of weather, and/or may not know current president and/or current address. 6 Occasional knowledge of some recent events. Little or no idea of current address, weather, etc. Given the current president's first name, may recall their last name. 7 No knowledge of any recent events
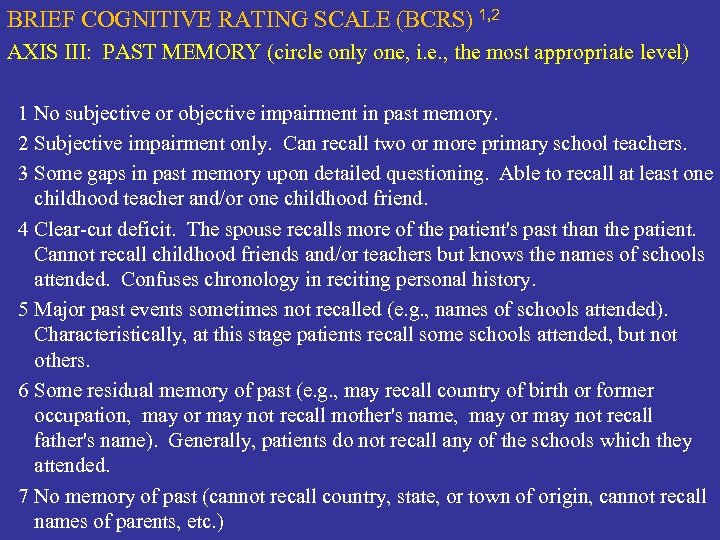
BRIEF COGNITIVE RATING SCALE (BCRS) 1, 2 AXIS III: PAST MEMORY (circle only one, i. e. , the most appropriate level) 1 No subjective or objective impairment in past memory. 2 Subjective impairment only. Can recall two or more primary school teachers. 3 Some gaps in past memory upon detailed questioning. Able to recall at least one childhood teacher and/or one childhood friend. 4 Clear-cut deficit. The spouse recalls more of the patient's past than the patient. Cannot recall childhood friends and/or teachers but knows the names of schools attended. Confuses chronology in reciting personal history. 5 Major past events sometimes not recalled (e. g. , names of schools attended). Characteristically, at this stage patients recall some schools attended, but not others. 6 Some residual memory of past (e. g. , may recall country of birth or former occupation, may or may not recall mother's name, may or may not recall father's name). Generally, patients do not recall any of the schools which they attended. 7 No memory of past (cannot recall country, state, or town of origin, cannot recall names of parents, etc. )
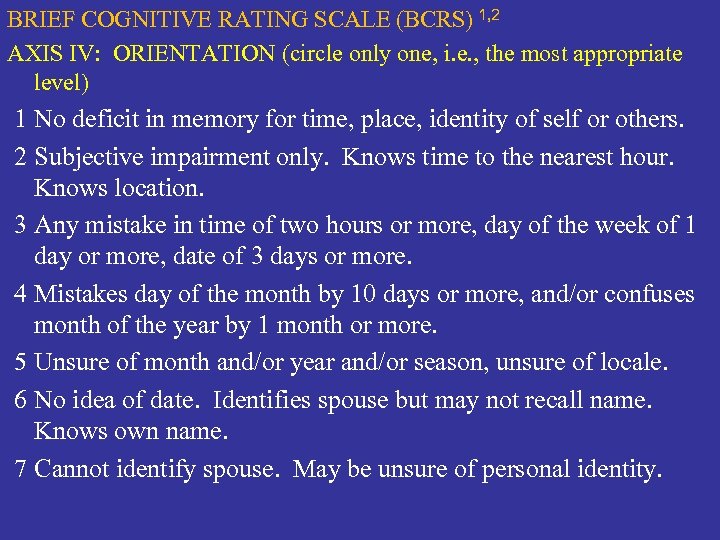
BRIEF COGNITIVE RATING SCALE (BCRS) 1, 2 AXIS IV: ORIENTATION (circle only one, i. e. , the most appropriate level) 1 No deficit in memory for time, place, identity of self or others. 2 Subjective impairment only. Knows time to the nearest hour. Knows location. 3 Any mistake in time of two hours or more, day of the week of 1 day or more, date of 3 days or more. 4 Mistakes day of the month by 10 days or more, and/or confuses month of the year by 1 month or more. 5 Unsure of month and/or year and/or season, unsure of locale. 6 No idea of date. Identifies spouse but may not recall name. Knows own name. 7 Cannot identify spouse. May be unsure of personal identity.
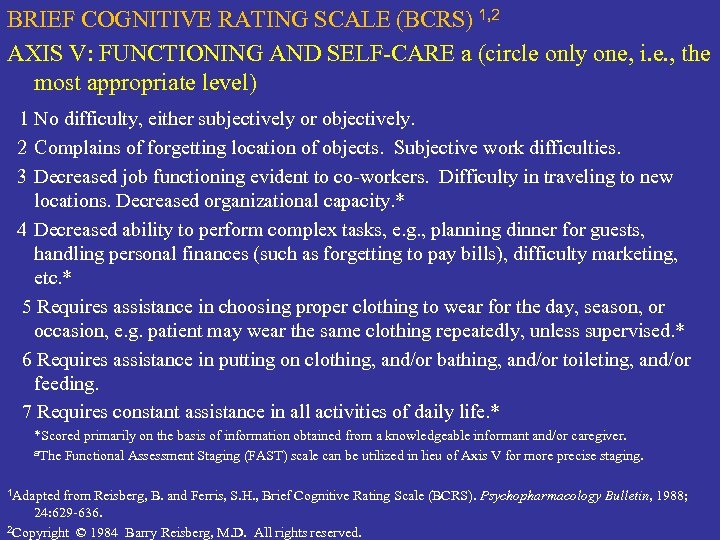
BRIEF COGNITIVE RATING SCALE (BCRS) 1, 2 AXIS V: FUNCTIONING AND SELF-CARE a (circle only one, i. e. , the most appropriate level) 1 No difficulty, either subjectively or objectively. 2 Complains of forgetting location of objects. Subjective work difficulties. 3 Decreased job functioning evident to co-workers. Difficulty in traveling to new locations. Decreased organizational capacity. * 4 Decreased ability to perform complex tasks, e. g. , planning dinner for guests, handling personal finances (such as forgetting to pay bills), difficulty marketing, etc. * 5 Requires assistance in choosing proper clothing to wear for the day, season, or occasion, e. g. patient may wear the same clothing repeatedly, unless supervised. * 6 Requires assistance in putting on clothing, and/or bathing, and/or toileting, and/or feeding. 7 Requires constant assistance in all activities of daily life. * *Scored primarily on the basis of information obtained from a knowledgeable informant and/or caregiver. a. The Functional Assessment Staging (FAST) scale can be utilized in lieu of Axis V for more precise staging. 1 Adapted from Reisberg, B. and Ferris, S. H. , Brief Cognitive Rating Scale (BCRS). Psychopharmacology 24: 629 -636. 2 Copyright © 1984 Barry Reisberg, M. D. All rights reserved. Bulletin, 1988;
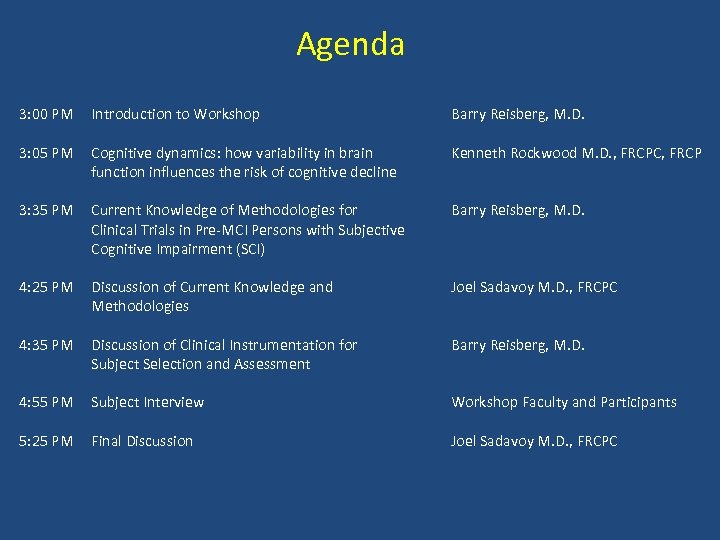
Agenda 3: 00 PM Introduction to Workshop Barry Reisberg, M. D. 3: 05 PM Cognitive dynamics: how variability in brain function influences the risk of cognitive decline Kenneth Rockwood M. D. , FRCPC, FRCP 3: 35 PM Current Knowledge of Methodologies for Clinical Trials in Pre-MCI Persons with Subjective Cognitive Impairment (SCI) Barry Reisberg, M. D. 4: 25 PM Discussion of Current Knowledge and Methodologies Joel Sadavoy M. D. , FRCPC 4: 35 PM Discussion of Clinical Instrumentation for Subject Selection and Assessment Barry Reisberg, M. D. 4: 55 PM Subject Interview Workshop Faculty and Participants 5: 25 PM Final Discussion Joel Sadavoy M. D. , FRCPC
Workshop Moderator Joel Sadavoy M. D. , FRCPC Professor of Psychiatry, University of Toronto, Sam and Judy Pencer Chair in Applied General Psychiatry, Director Cyril & Dorothy, Joel & Jill Reitman Institute for Alzheimer's Support and Training, Head Geriatric and Community Psychiatry Programs Mount Sinai Hospital
c5e6af71bd653dc68f293ea8d422ca83.ppt