Bacterial Infections Chapter 14.ppt
- Количество слайдов: 82
Bacterial Infections Chapter 14 Infections Caused by Gram Positive Organisms. Michael Hohnadel, D. O. 02/07/2006 1
• Staphylococcal Infections • General • 20% of adults are nasal carriers. • HIV infected are more frequent carriers. • Lesions are usually pustules, furuncles or erosions with honey colored crust. • Bullae, erythema, widespread desquamation possible. • Embolic phenomena with endocarditis: • Olser nodes • Janeway Lesions 2
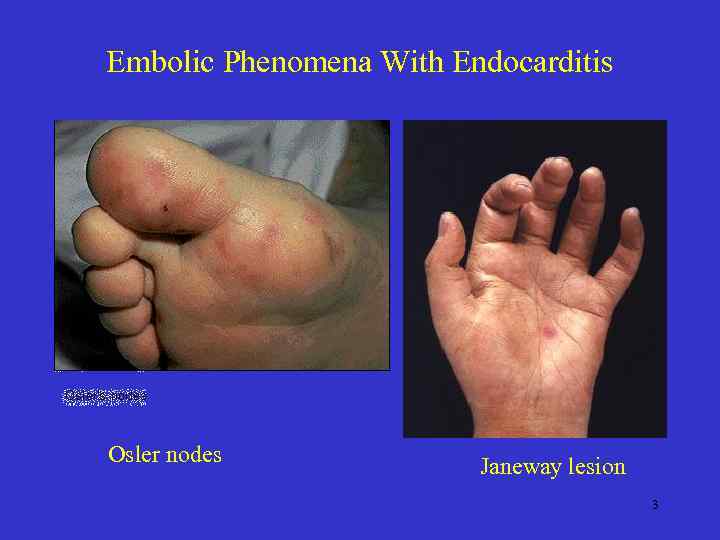
Embolic Phenomena With Endocarditis • Osler nodes Janeway lesion 3
Superficial Pustular Folliculitis • Also known as Impetigo of Bockhart • Presentation: Superficial folliculitis with thin wall, fragile pustules at follicular orifices. – Develops in crops and heal in a few days. – Favored locations: • Extremities and scalp • Face (esp periorally) • Etiology: S. Aureus. 4
Sycosis Vulgaris (Sycosis Barbae) • Perifollicular, Chronic , pustular staph infection of the bearded region. • Presentation: Itch/burn followed by small, perifollicular pustules which rupture. New crops of pustules frequently appear esp after shaving. • Slow spread. • Distinguishing feature is upper lip location and persistence. – Tinea is lower. – Herpes short lived – Pseudofolliculitis Barbea ingrown hair and papules. 5
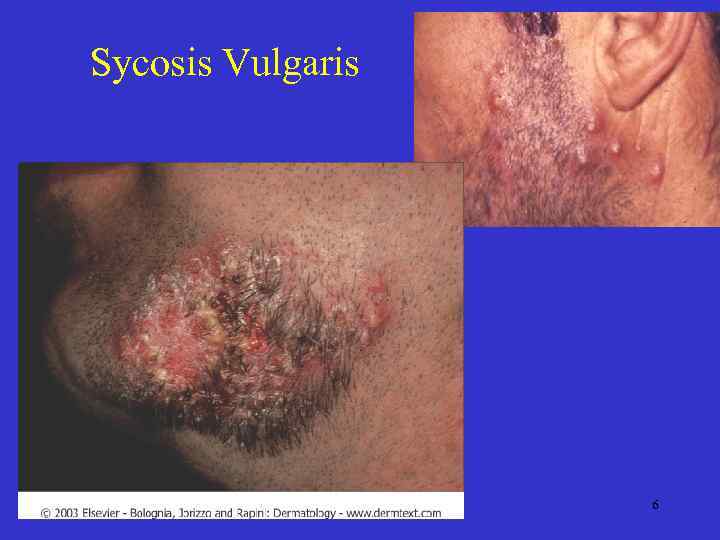
Sycosis Vulgaris 6
Sycosis Lupoides • Etiology: Staph. Aureus infection that, through extension, results in a central hairless scar surrounded by pustules. • Histopathology: Pyogenic folliculitis and perifolliculitis with deep extension into hair follicles often with edema. • Thought to resemble lupus vulgaris in appearance. 7
Treatment of Folliculitis • • Cleansing with soap and water. Bactroban (Mupirocin) Burrows solution for acute inflammation. Antibiotics: cephalosporin, penicillinase resistant PCN. 8
Furunculosis • Presentation: A perifollicular, round, tender abscess that ends in central suppuration. • Etiology: S. Aureus • Breaks in skin integrity is important. – Various systemic disorders may predispose. • Hospital epidemics of abx resistant staph. may occur – Meticulous hand washing is essential. 9

Furuncle 10

Furuncle / Carbuncle 11
Furunculosis • Treatment of acute lesions: – ABX may arrest early furuncles. – Incision and drainage AFTER furuncle is localized with definite fluctuation. • No incision of EAC or nasal furuncles. TX with ABX. – Upper lip and nose, ‘danger triangle’, requires prompt treatment with ABX to avoid possible venous sinus thrombosis, septicemia, meningitis. 12
Treatment of Chronic Furunculosis (Avoid auto-inoculation, Eliminate carrier state. ) – Sites of colonization: Nares, axilla, groin and perianal. – Use Anti-staph cleansers – soap, chlorhexidine. – Frequent laundering. – Bactroban to nares of pt and family members • BID to nares for one week (q 4 th week. ). – Rifampin 600 mg QD for 10 days with cloxacillin 500 mg QID (or Clindamycin 150 mg qd for 3 mo) 13
Pyogenic Paronychia • Presentation: Tender painful swelling involving the skin surrounding the fingernail. • Etiology: Moisture induced separation of eponychium from nail plate by trauma or moisture leading to secondary infection. – Often work related • Bacteria = acute abscess formation. Candida = chronic swelling. • Treatment: • • Avoid maceration / trauma I&D of abscess PCN, 1 st Gen Cephalosporin, augmentin. Chronic infection requires fungicide and a bactericide. 14
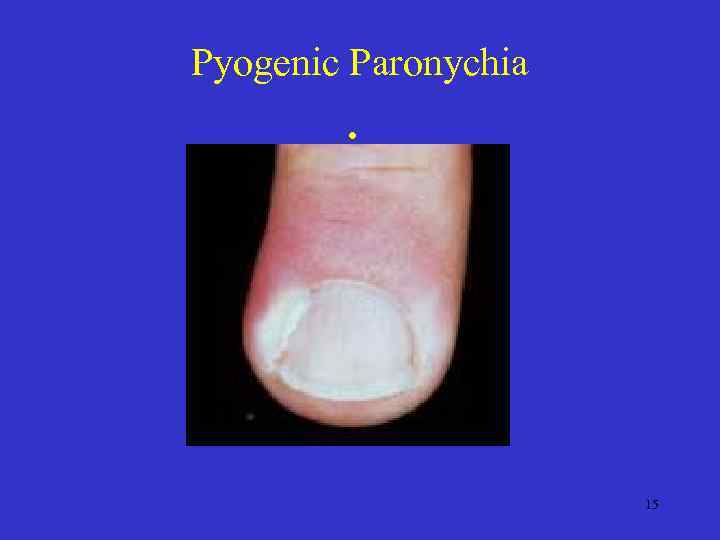
Pyogenic Paronychia • 15
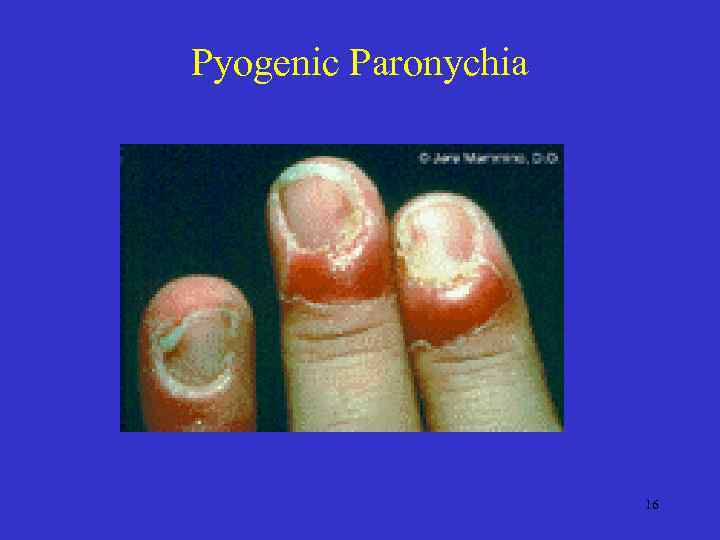
Pyogenic Paronychia 16
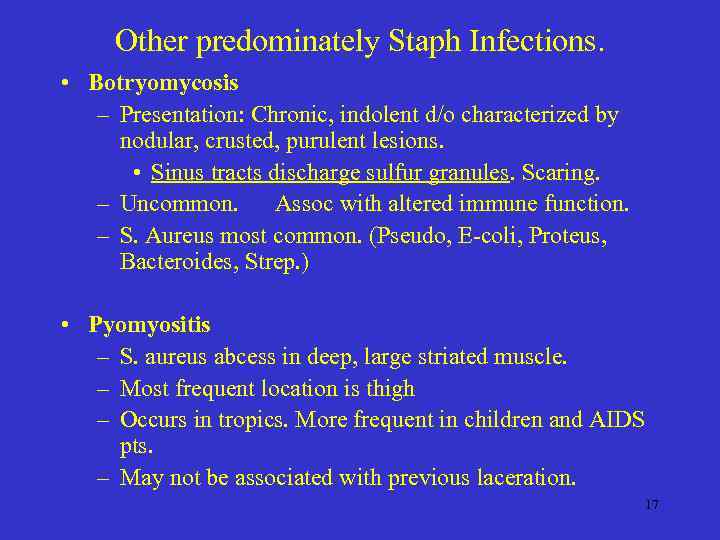
Other predominately Staph Infections. • Botryomycosis – Presentation: Chronic, indolent d/o characterized by nodular, crusted, purulent lesions. • Sinus tracts discharge sulfur granules. Scaring. – Uncommon. Assoc with altered immune function. – S. Aureus most common. (Pseudo, E-coli, Proteus, Bacteroides, Strep. ) • Pyomyositis – S. aureus abcess in deep, large striated muscle. – Most frequent location is thigh – Occurs in tropics. More frequent in children and AIDS pts. – May not be associated with previous laceration. 17
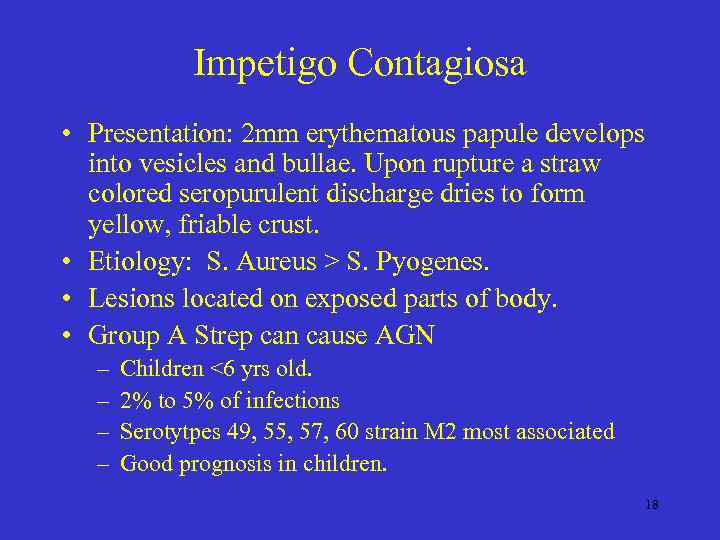
Impetigo Contagiosa • Presentation: 2 mm erythematous papule develops into vesicles and bullae. Upon rupture a straw colored seropurulent discharge dries to form yellow, friable crust. • Etiology: S. Aureus > S. Pyogenes. • Lesions located on exposed parts of body. • Group A Strep can cause AGN – – Children <6 yrs old. 2% to 5% of infections Serotytpes 49, 55, 57, 60 strain M 2 most associated Good prognosis in children. 18
Impetigo Contagiosa • Treatment – PCN, 1 st Gen. Cephalosporin. – Topical: bacitracin or mupirocin after soaking off crust. • Topical ABX prophylaxis of traumatic injury. – Reduced infection 47 % • Treatment of nares for carriers. 19
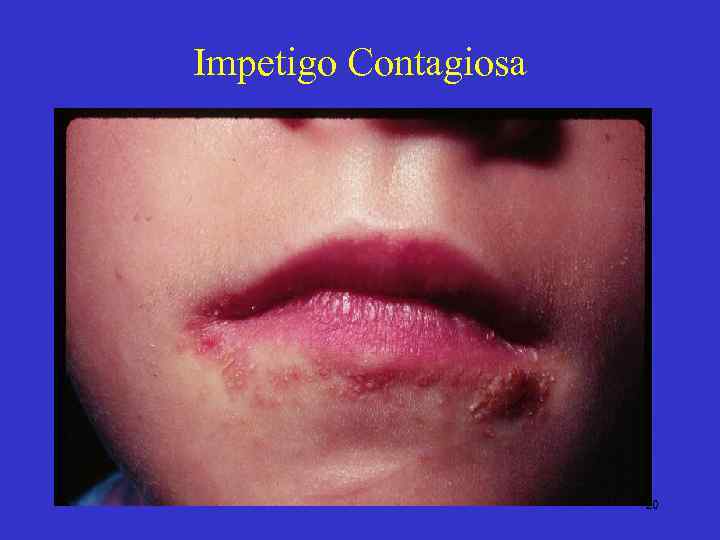
Impetigo Contagiosa • 20
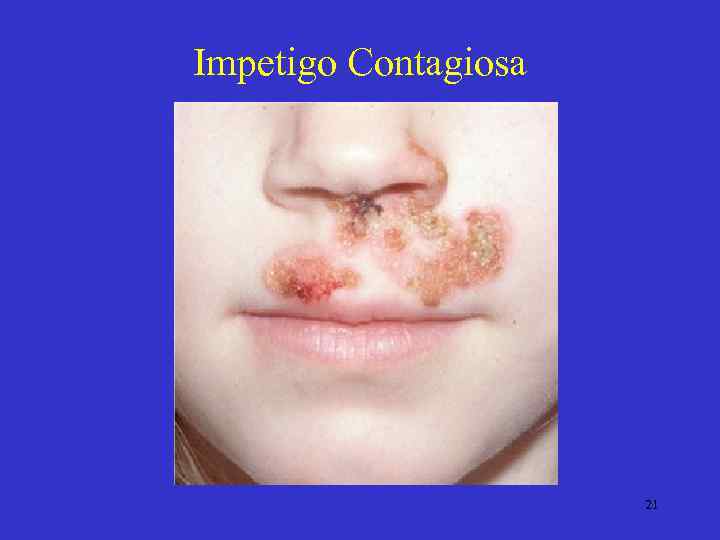
Impetigo Contagiosa 21

Impetigo Contagiosa 22
Bullous Impetigo • Presentation: Large, fragile bullae, suggestive of pemphigus. Rupture leaves a circinate, weepy crusted lesion (impetigo circinata). Collarette of scale present. • Affects newborns at the 4 -10 th days of life. Adults in warm climates. • Organism present in the lesions. 23
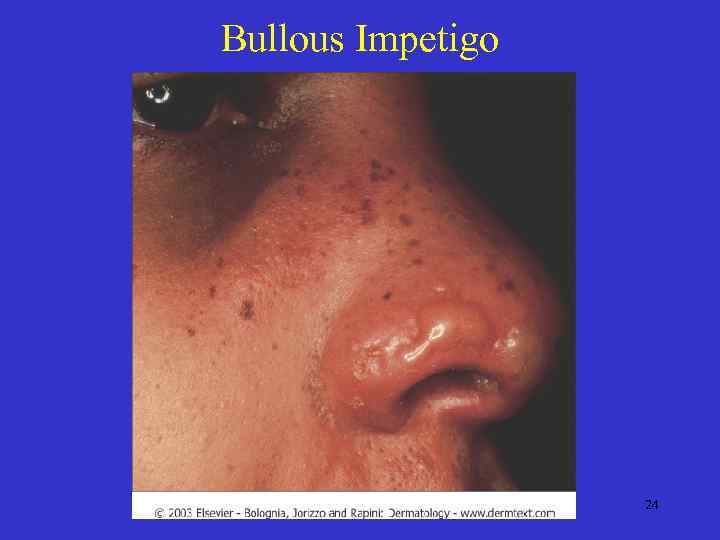
Bullous Impetigo 24

Bullous Impetigo 25
Staphylococcal Scalded Skin Syndrome. • Presentation: Febrile, rapidly evolving generalized desquamation of the skin. – Primarily affects neonates and children. Begins with skin tenderness and erythema of neck groin, axillae with sparing of palm and soles – Blistering occurs just beneath granular layer. – Positive Nikolsky’s sign • Etiology: Exotoxin from S. Aureus infection located at a mucosal surface (not in lesions). • Differentiate from TENS • Treatment as before. Prognosis is good. 26

Staphylococcal Scalded Skin Syndrome • Blister plane in granular layer 27

Staphylococcal Scalded Skin Syndrome 28
Toxic Shock Syndrome • Presentation: – Acute, febrile, multi-system disease. – One diagnostic criteria is widespread maculopapular eruption. • Causes: – S. Aureus : • Cervical mucosa historically in early 1980’s. • Also seen with: wounds, catheters, nasal packing. Mortality 12 %. – Group A Strep : • necrotizing fasciitis. Mortality 30%. 29
Toxic Shock Syndrome • Diagnosis: CDC – Temp >38. 9 C, erythematous eruption with desquamation of palms and soles 1 -2 wks after onset. Hypotension – AND involvement of three of more other systems • GI, muscular, renal, CNS. – AND Test for RMSF, Leptospirosis and rubeola as well as blood urine and CSF should be negative. • Treatment: – Systemic ABX, – Fluid therapy – Drainage of S. Aureus infected site. 30
Streptococcal Skin Infections 31
Ecthyma • Presentation: Vesicle/pustule which enlarges over several days and becomes thickly crusted. When crust is removed a superficial saucer shaped ulcer remains with elevated edges. – Nearly always on shins or dorsal feet. – Heals in a few weeks with scarring. • • Agent: Staph or Strep. Heals with scaring Gangrene in predisposed individuals. Treatment: Clean, topical and systemic ABX. 32
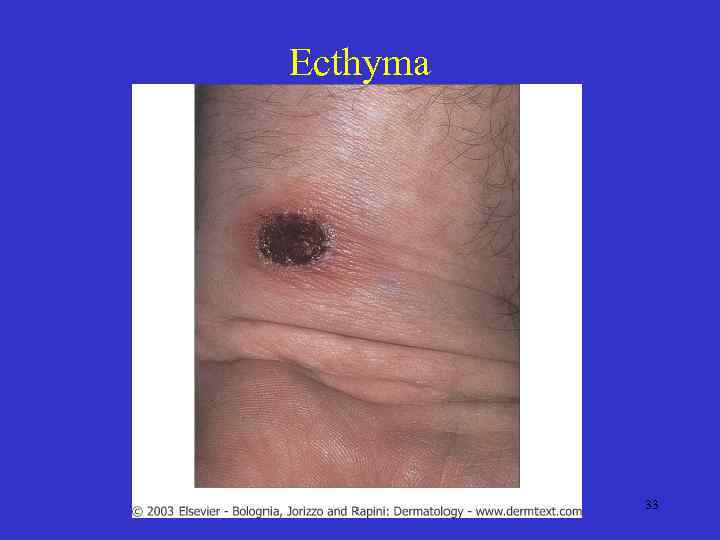
Ecthyma 33

Ecthyma • 34
Scarlet Fever • Presentation: 24 – 48 hrs after Strep. Pharyngitis onset. – Cutaneous: • Widespread erythema with 1 -2 mm papules. Begins on neck and spreads to trunk then extremities. • Pastia’s lines – accentuation over skin folds with petechia. • Circumoral pallor • Desquamation of palms and soles at appox two wks. – May be only evidence of disease. – Other: strawberry tongue • Causes: erythrogenic exotoxin of group A Strep. • Culture to recover organism or use streptolysin O titer if testing is late. • TX: PCN, E-mycin, Cloxacillin. 35
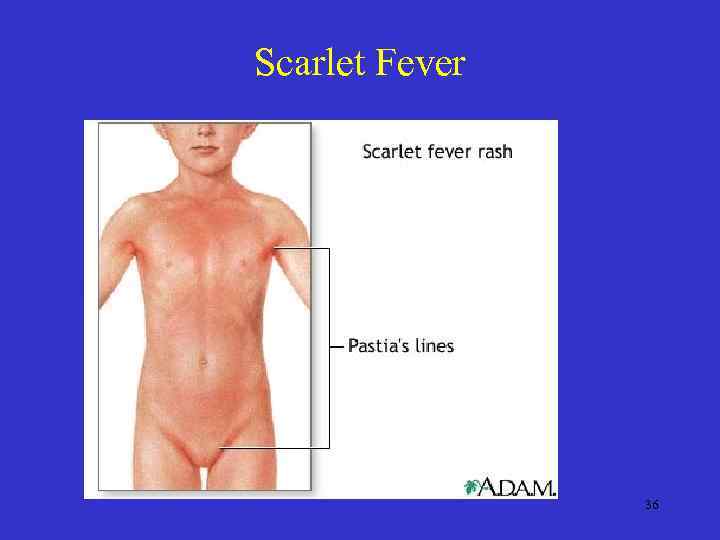
Scarlet Fever 36
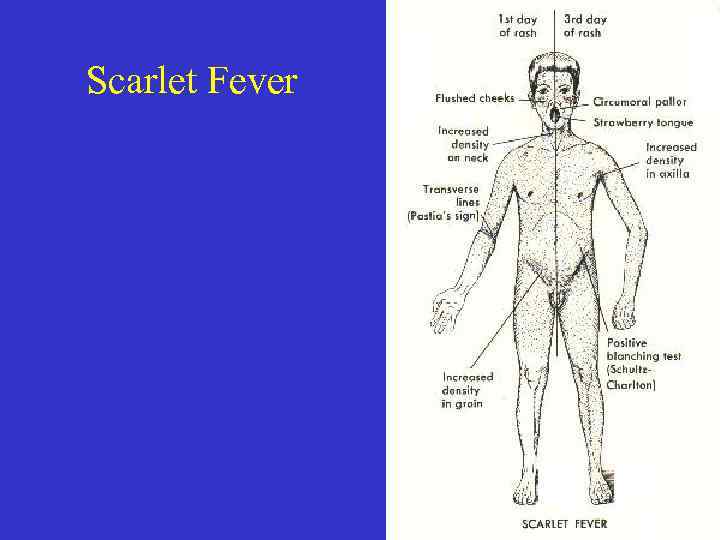
Scarlet Fever 37

Scarlet Fever Rash with circumoral pallor 38
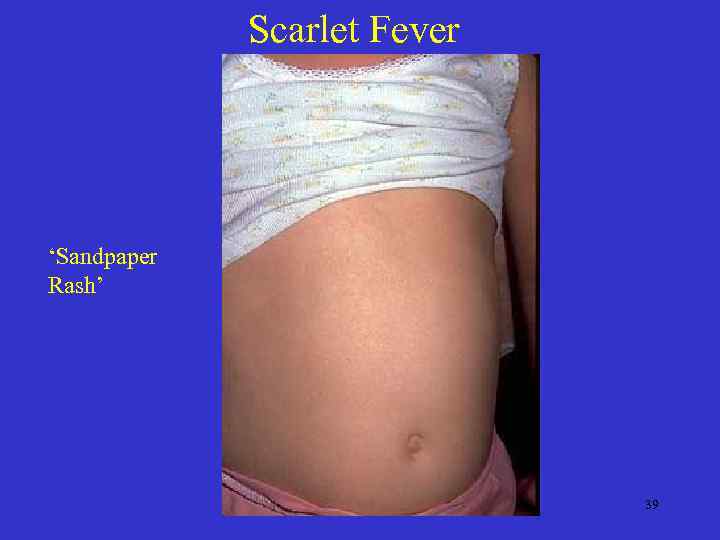
Scarlet Fever ‘Sandpaper Rash’ 39
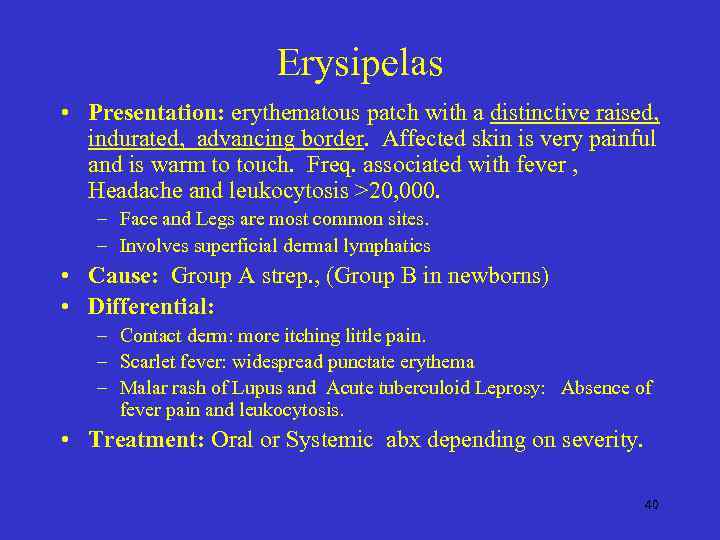
Erysipelas • Presentation: erythematous patch with a distinctive raised, indurated, advancing border. Affected skin is very painful and is warm to touch. Freq. associated with fever , Headache and leukocytosis >20, 000. – Face and Legs are most common sites. – Involves superficial dermal lymphatics • Cause: Group A strep. , (Group B in newborns) • Differential: – Contact derm: more itching little pain. – Scarlet fever: widespread punctate erythema – Malar rash of Lupus and Acute tuberculoid Leprosy: Absence of fever pain and leukocytosis. • Treatment: Oral or Systemic abx depending on severity. 40
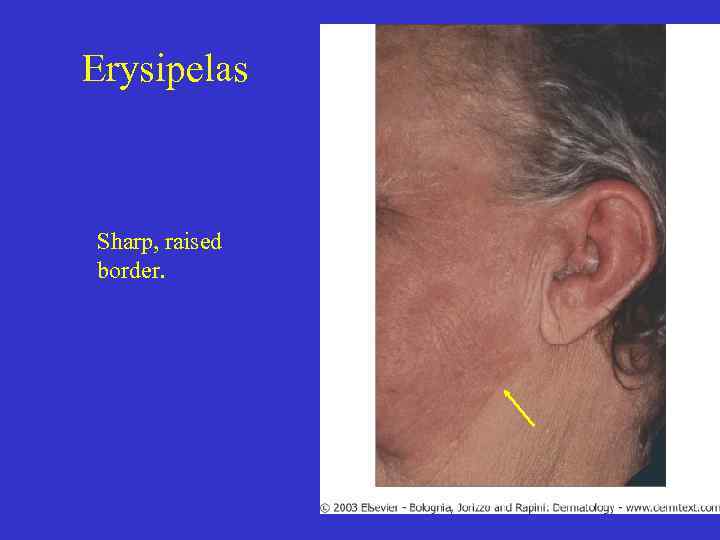
Erysipelas Sharp, raised border. 41
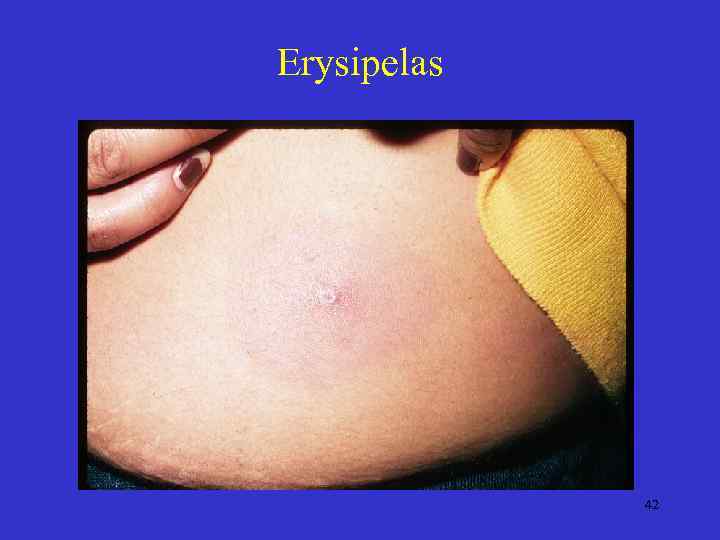
Erysipelas 42

Erysipelas 43
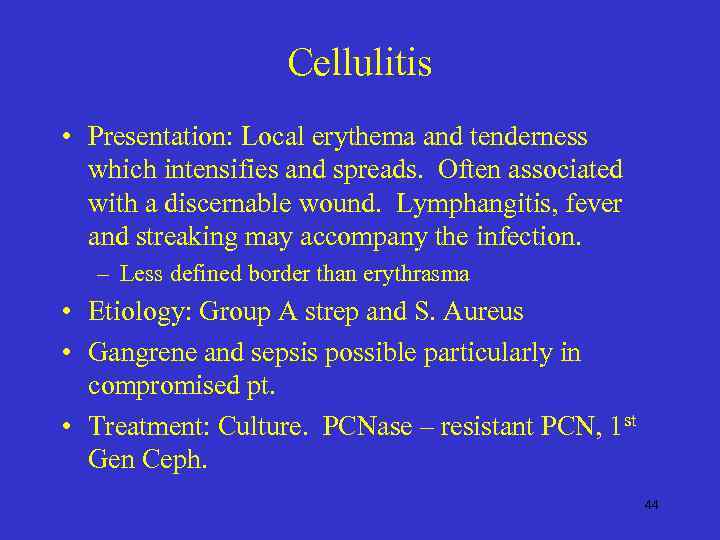
Cellulitis • Presentation: Local erythema and tenderness which intensifies and spreads. Often associated with a discernable wound. Lymphangitis, fever and streaking may accompany the infection. – Less defined border than erythrasma • Etiology: Group A strep and S. Aureus • Gangrene and sepsis possible particularly in compromised pt. • Treatment: Culture. PCNase – resistant PCN, 1 st Gen Ceph. 44
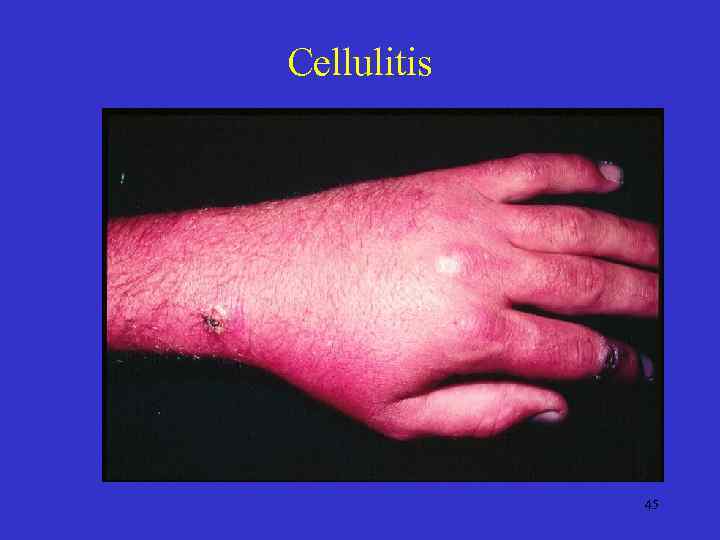
Cellulitis 45
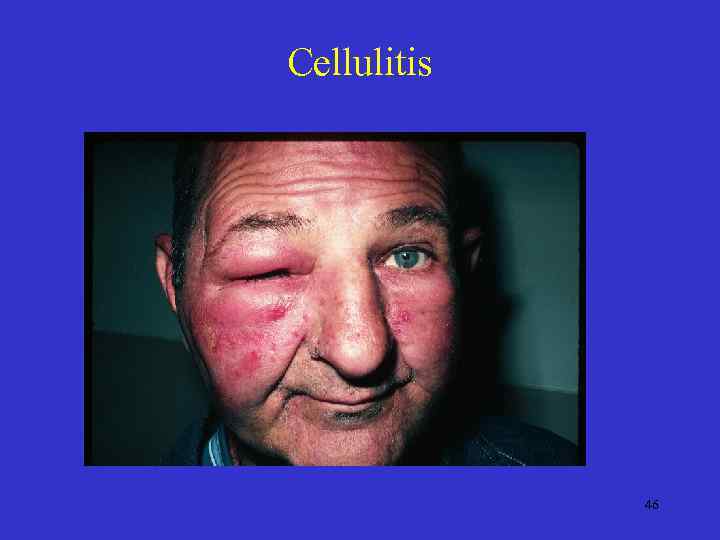
Cellulitis 46

Cellulitis 47
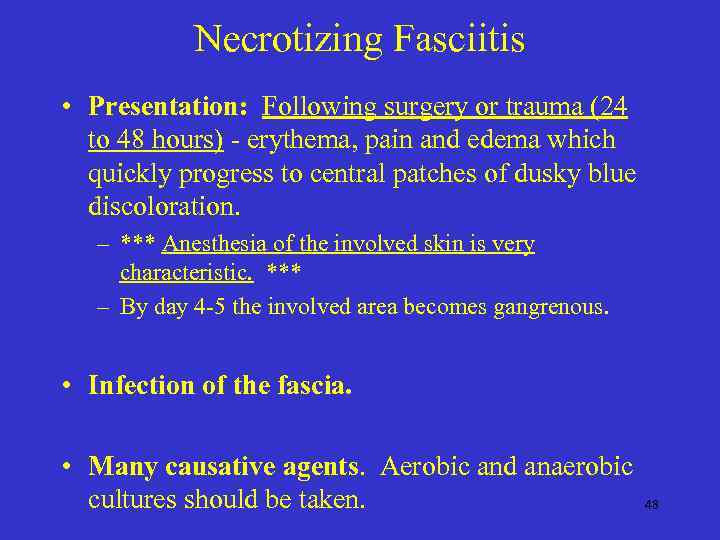
Necrotizing Fasciitis • Presentation: Following surgery or trauma (24 to 48 hours) - erythema, pain and edema which quickly progress to central patches of dusky blue discoloration. – *** Anesthesia of the involved skin is very characteristic. *** – By day 4 -5 the involved area becomes gangrenous. • Infection of the fascia. • Many causative agents. Aerobic and anaerobic cultures should be taken. 48
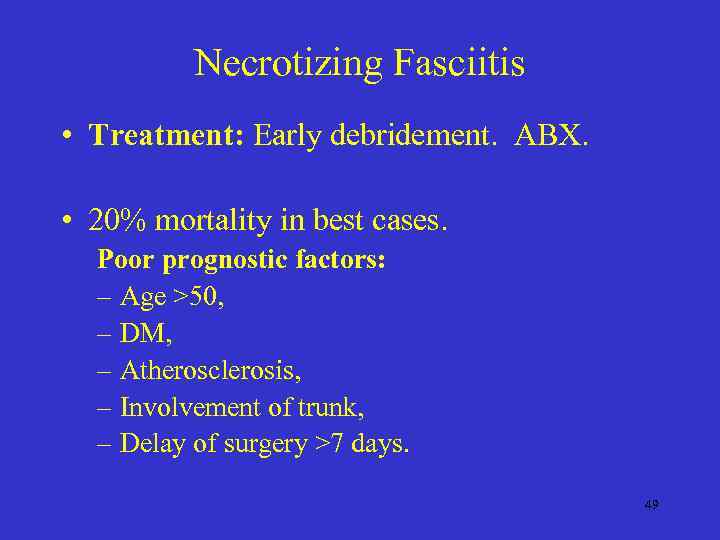
Necrotizing Fasciitis • Treatment: Early debridement. ABX. • 20% mortality in best cases. Poor prognostic factors: – Age >50, – DM, – Atherosclerosis, – Involvement of trunk, – Delay of surgery >7 days. 49
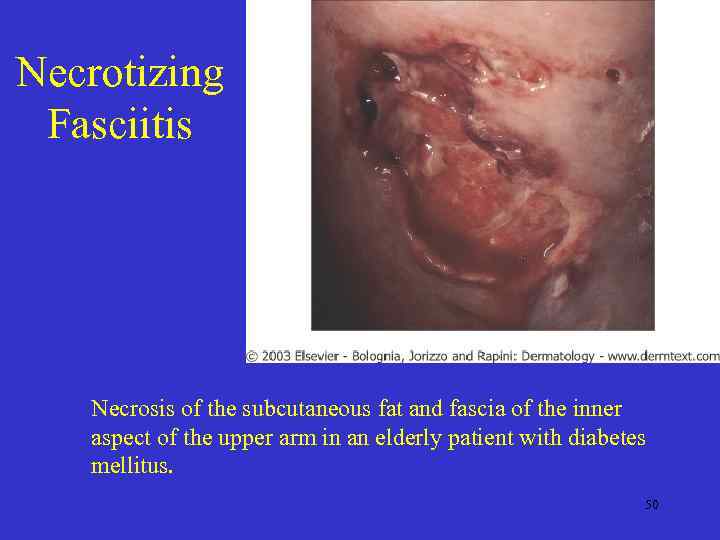
Necrotizing Fasciitis Necrosis of the subcutaneous fat and fascia of the inner aspect of the upper arm in an elderly patient with diabetes mellitus. 50
More Staph and Strep Infections Blistering Distal dactylitis • Superficial blisters on volar fat pads • Typical pt is 2 -16 yrs old Perianal Dermatitis • Superficial, perianal, well demarcated rim of erythema which is often confused with irritant dermatitis. • Typical pt is 1 -8 yrs old. Group B infection • Consider in any neonates. Also seen in adults with DM and peripheral vascular disease. Staph Iniae • 1997 first reported • Cellulitis of hands assoc with preparation of tilapia fish. 51
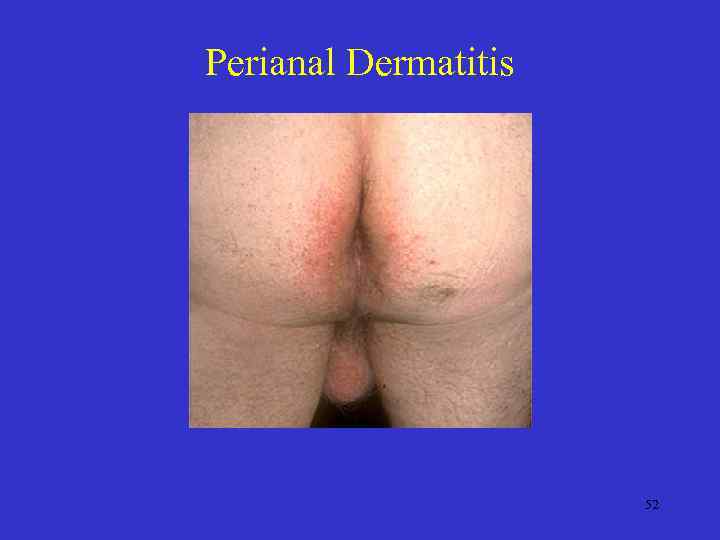
Perianal Dermatitis 52
Other Gram Positive Infections. 53
Erysipeloid of Rosenbach. • Presentation: Purple, often polygonal, sharply marginated patches occurring on the hands. The central portion of the lesion may fade as the border advances. New purplish patches appear at nearby sites ( or possibly distant sites). Painful. • • Causative agent: Erysipelothrix Rhusopathiae. Rod shaped grm (+) that forms long branching filaments. Culture on media fortified with serum at room temp. • Organism found on dead animal matter and the affliction is seen most commonly among fishermen (crabs, shrimp), veterinarians, and in the meat packing industry (esp pork) • Treatment: PCN 1. 0 gm/day 5 -10 days. 54

Erysipeloid 55
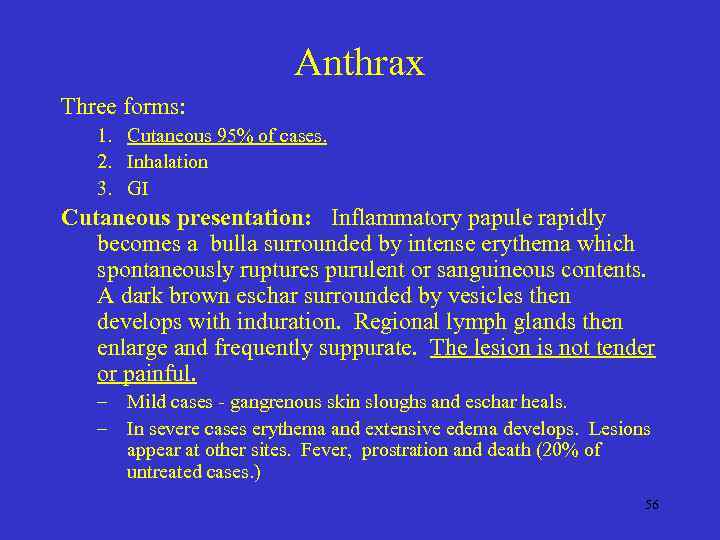
Anthrax Three forms: 1. Cutaneous 95% of cases. 2. Inhalation 3. GI Cutaneous presentation: Inflammatory papule rapidly becomes a bulla surrounded by intense erythema which spontaneously ruptures purulent or sanguineous contents. A dark brown eschar surrounded by vesicles then develops with induration. Regional lymph glands then enlarge and frequently suppurate. The lesion is not tender or painful. – Mild cases - gangrenous skin sloughs and eschar heals. – In severe cases erythema and extensive edema develops. Lesions appear at other sites. Fever, prostration and death (20% of untreated cases. ) 56
Anthrax • Human infection generally from infected animals. Human to human transmission is possible. • Diagnosis: smear with gram stain. Cultures of wound. – Gamma bacteriophage to identify – Mice serum titer. – Electrophoretic immunoblots. • Treatment: PCN G 2 million units IV q 6 hours for 4 -6 days followed by oral PCN for 7 -10 days. 57
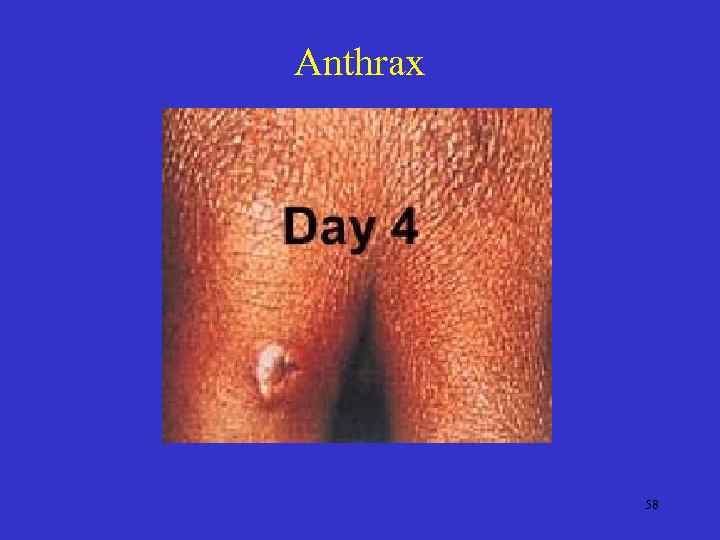
Anthrax 58
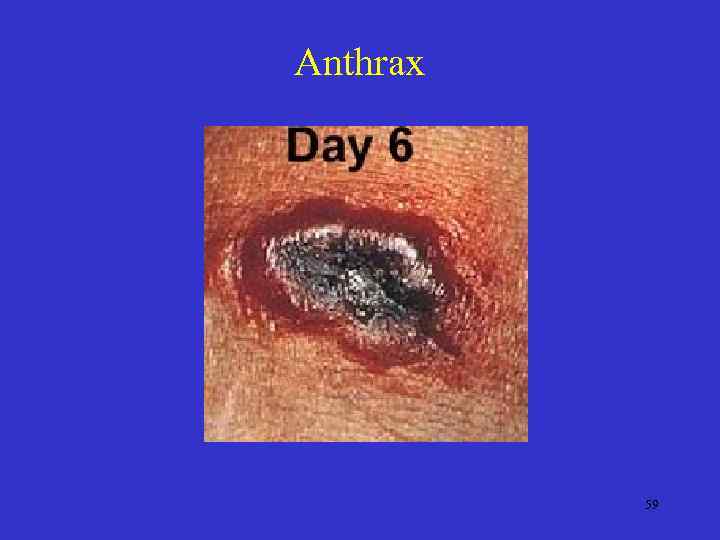
Anthrax 59
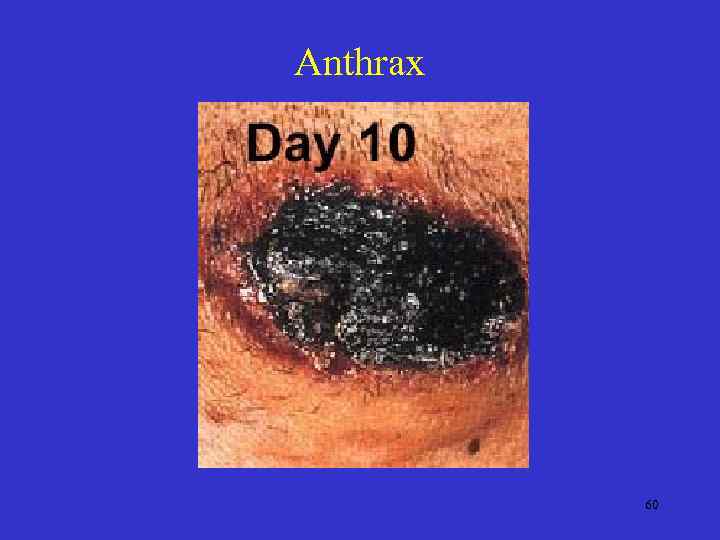
Anthrax 60
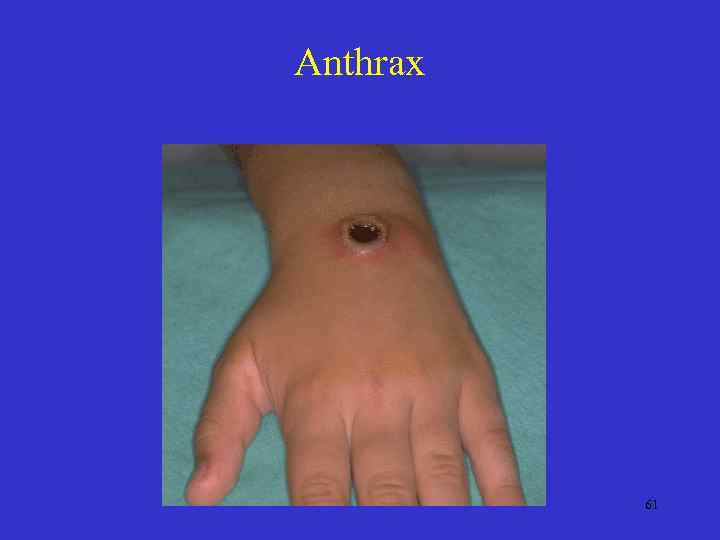
Anthrax 61
Listeriosis • Listeria Monocytogenes • Ubiquitous organism which usually causes meningitis of encephalitis. • Rare cutaneous affliction causing erythematous, tender papules and pustules with lymphadenopathy, fever and malaise. • Risk to immunosuppressed – Neonates: Granulomatosis infanta peptica. • May be missed on bacteriologic exam. Serologic test useful. • Treatment: sensitive to most ABX. 62
Cutaneous Diphtheria • Corynebacterium Diphtheriae infection in unimmunized individual • Presentation: – Ulcer with a hard rolled border with a pale blue tinge. A leathery gray membrane often coves the lesion. – Eczematous, impetinginous, vesicular or pustular scratches. • Paralysis and cardiac complications from diphtheria toxin are possible. • Common in tropical areas with most U. S. cases from nonimmunized migrant workers. • Treatment: Diphtheria antitoxin, E-mycin is DOC. Also rifampin and PCN. 63
Desert Sore • Ulcerative disease endemic amongst bushmen and soldiers in Australia. • Presentaion: Grouped vesicles on extremities which rupture to form superficial, indolent ulcers that may be 2. 0 cm in diameter. • Cause: Staph, Strep and Corynebacterium Diphtheria. • Treatment: Diphtheria antitoxin if organism present and topical ABX with oral PCN or Emycin. 64
Tropical Ulcer • Presentation: – Inflammatory papule with vesiculation and ulcer formation frequently with undermined edges. – Pseudomembrane may be present or simply crusting. – Minimal distress other then mild itching. – Usually single lesion on one extremity. – Auto inoculation spreads infection. • Most common in native laborers or school children during the ‘rainy season’. • Usually occur at sites of cutaneous injury. • Etiology: Many organisms found under description of ‘topical ulcer’: – Bacteriodes Fusiformis, spirochetes, anaerobes. 65
Differential: Tropical Ulcer – Vascular ulcers 1. Arteriosclerotic ulcer – deep to expose fascia and tendons. 2. HTN ischemic ulcer – shallow, painful mid to lower legs. 3. Venous ulcers – shallow, varicosities. Above medial malleolus. – Other: • • Desert ulcer – C diptheriae Gummatous ulcer – punched out, other syphilis signs. Tuberculous ulcer – not usually on leg. Mycotic ulcer – nodular with fungi on inspection. Buruli ulcer – Mycobacterium ulcerans. Leshmania ulcer – contans Leishmania tropicans, not on leg. Ulcer of blood abnormalities. 66
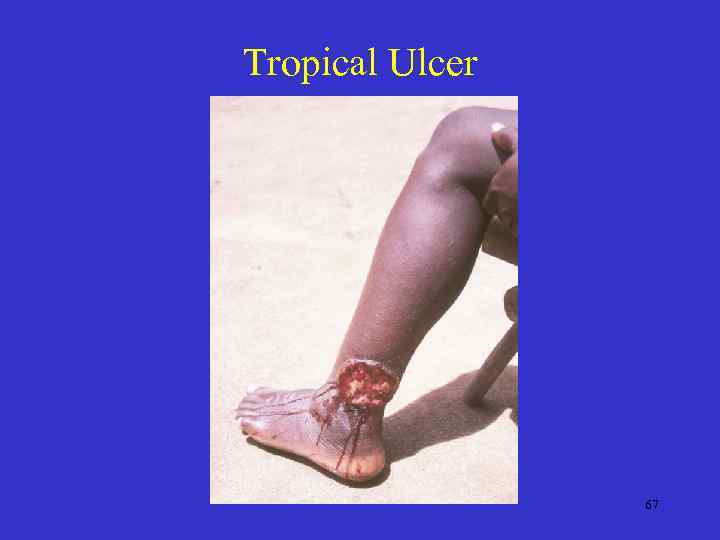
Tropical Ulcer 67
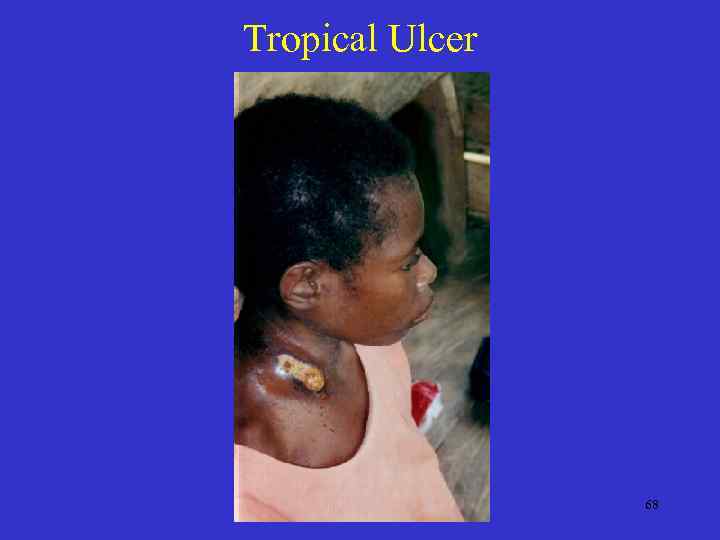
Tropical Ulcer 68
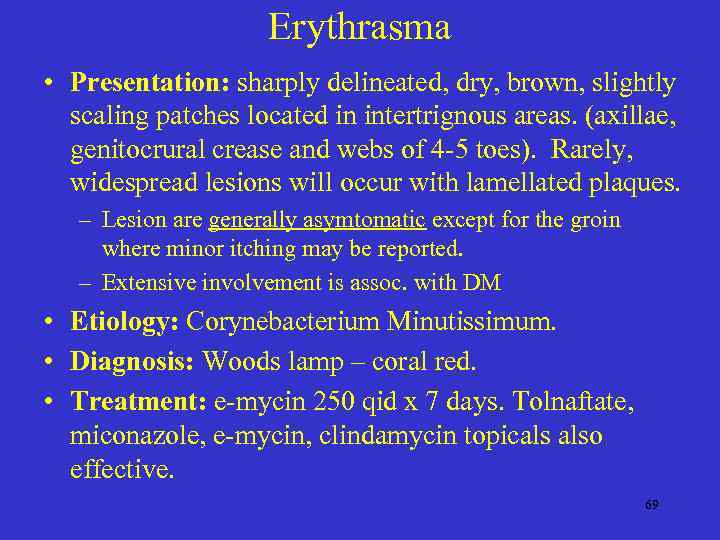
Erythrasma • Presentation: sharply delineated, dry, brown, slightly scaling patches located in intertrignous areas. (axillae, genitocrural crease and webs of 4 -5 toes). Rarely, widespread lesions will occur with lamellated plaques. – Lesion are generally asymtomatic except for the groin where minor itching may be reported. – Extensive involvement is assoc. with DM • Etiology: Corynebacterium Minutissimum. • Diagnosis: Woods lamp – coral red. • Treatment: e-mycin 250 qid x 7 days. Tolnaftate, miconazole, e-mycin, clindamycin topicals also effective. 69
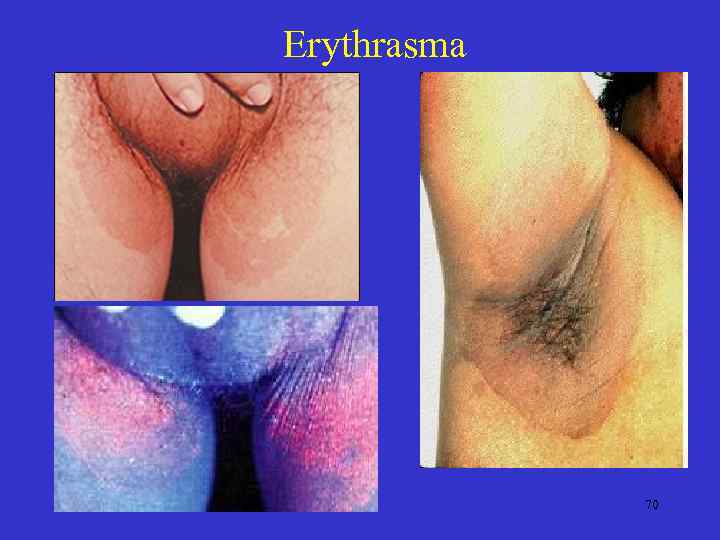
Erythrasma 70
Intertrigo • Presentation: Superficial inflammatory dermatitis where two skin surfaces are in apposition. • Etiology: Friction and moisture allows infection by bacteria (Staph, Strep, Pseudo. ) or fungi or both. 71

Intertrigo 72
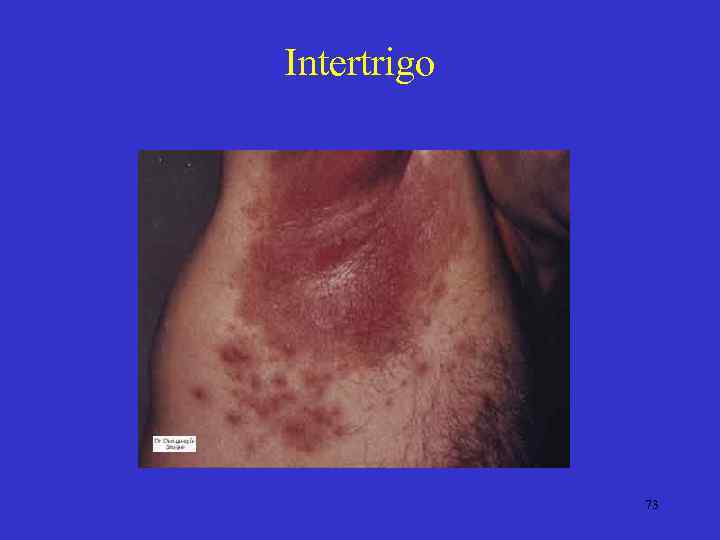
Intertrigo 73

Intertrigo 74
Pitted Keratolysis • Presentation: Thick, weight bearing portions of the soles gradually covered by asymptomatic round pits 1 -3 mm in diameter. Pits may become confluent forming furrows. Rarely, palms may be affected. • Etiology: unknown. Micrococcus sedentarius in synergy with corynebacteria is suspected • Men with sweaty feet are most susceptible. • Treatment: Topical E-mycin, clindamycin. Miconazole, benzoyl perioxide gel, Al. Cl solution. 75
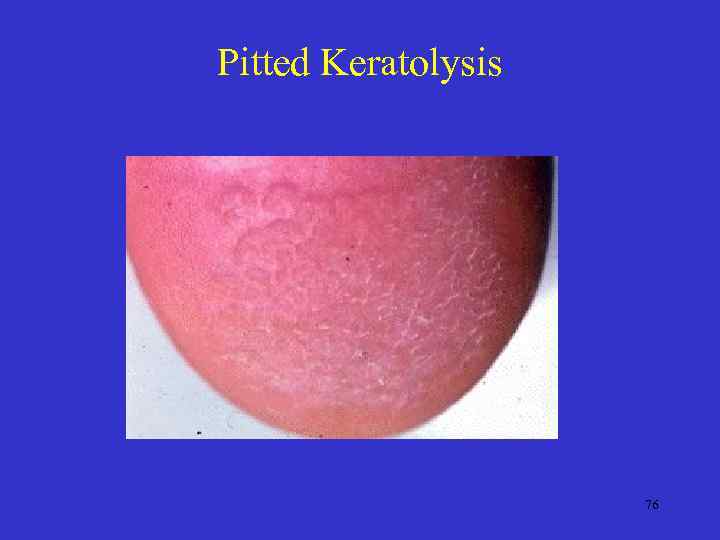
Pitted Keratolysis 76
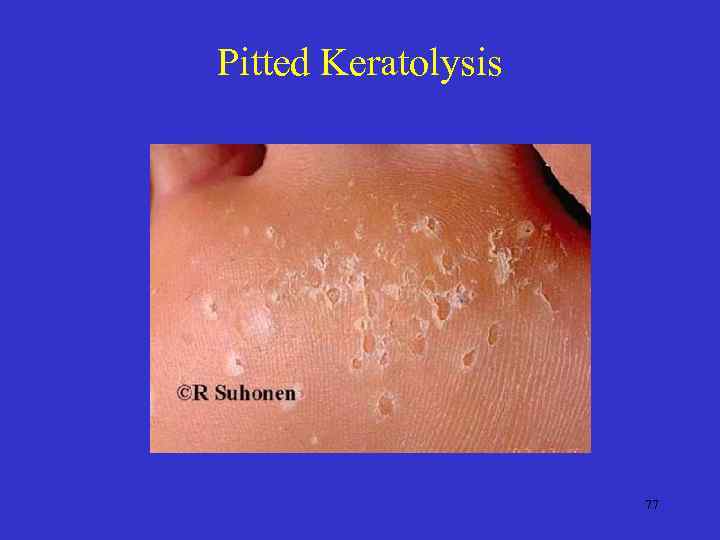
Pitted Keratolysis 77
Gas Gangrene • • Presentation: Several hours after a patient receives a deep laceration, severe pain and wound site crepitance develop as well as fever, chills and prostration. A mousy odor is characteristic. Etiology: (2 types) 1. Clostridium types: perfringens, oedematiens, septicum and haemolyticum. Acute onset ! 2. Peptostreptococcus. Delayed onset up to several days. • Treatment: – Clostridium: Wide debridement and PCN G, hyperbaric – Peptostreptococcus: Surgical debridement limited to glossy necrotic muscle. 78

Gas Gangrene 79
Chronic Undermining Burrowing Ulcers ( Meleney’s Gangrene) • Presentation: Pt who recently (1 -2 wks) underwent surgical drainage of a peritoneal or lung abscess develops carbunculoid appearance at the sutures or wound site. Pain is excruciating. • The lesion then differentiates into three zones: 1. outer zone - bright red, 2. middle zone - dusky purple, 3. inner zone - gangrenous with central areas of granulation tissue. 80
Chronic Undermining Burrowing Ulcers • Etiology: Peptostreptococcus in periphery. S. Aureus or Enterobacteriaceae in zone of gangrene. – Bacterial synergetic gangrene • Treatment: Wide excision with ABX (PCN and aminoglycoside). 81
Fournier’s Gangrene of the Penis and Scrotum • Presentation: Gangrenous infection of penis, scrotum or perineum which spreads along fascial planes. • Etiology: Group A Strep or mixed organism. • Ages 20 -50 • Culture for aerobic and anaerobic organisms. • Treatment: ABX as indicated. 82
Bacterial Infections Chapter 14.ppt