4ceb1e600715d1085771f973dc998dab.ppt
- Количество слайдов: 128
Bacteria They are prokaryotic microorganisms which can be spheroidal (coccus), rod / cylindrical (bacillus) and spirillar (spirochetes) They are the causative agents of many human diseases
Bacterial species
Some of the important specific bacterial infections TUBERCULOSIS SYPHILIS ACTINOMYCOSIS SCARLET FEVER NOMA LEPROSY DYPHTHERIA CAT – SCRATCH DISEASE PYOGENIC GRANULOMA
TUBERCULOSIS
v Tuberculosis is a chronic systemic infectious disease of worldwide prevalence. v It is a granulomatous infection and is caused by Mycobacterium tuberculosis or rarely by Mycobacterium bovis v Incidence of tuberculosis has declined greatly v In patients with AIDS, M. avium intercellulare is a common cause of opportunistic infections
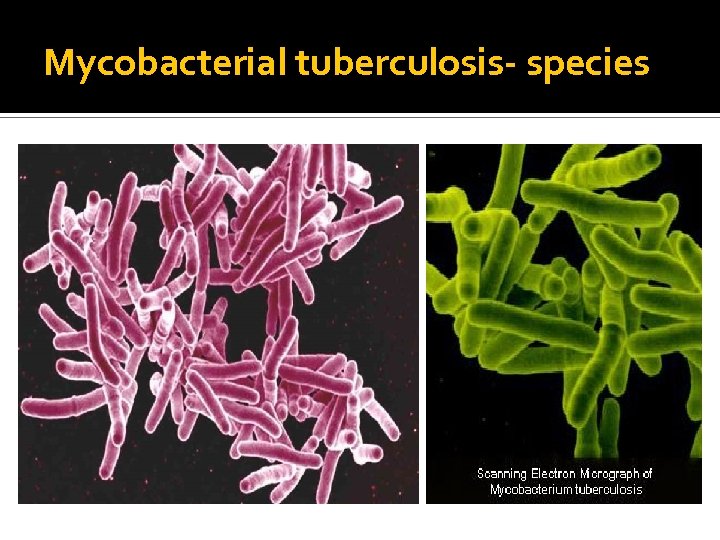
Mycobacterial tuberculosis- species
Pathogenesis v Caused by mycobacterium tuberculosis which is aerobic, slender, non-motile, non-spore forming, rod shaped, acid fast organism v Mode of spread: droplet infection v Since TB spread through droplet infection, optimal conditions for transmission include: Overcrowding Poor personal hygiene Poor public hygiene
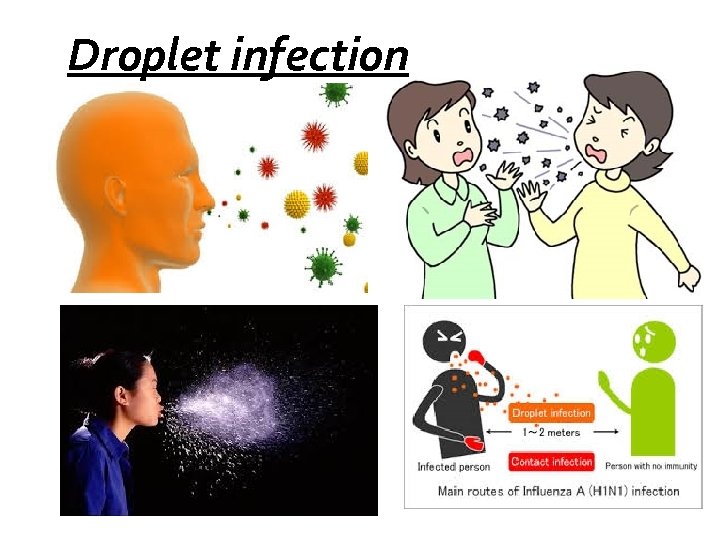
Droplet infection
Contributing factors v Social issues: poverty, overcrowding issues v Political issues: war time, resettlement, immigration v Health issues: malnutrition, drug abuse, HIV infection, immunosuppression, v Economic issues: drug cost, health care issues housing, case identification and management v Microbial: drug resistance
v Patients with the active disease bacilli into the air by: v Coughing/Sneezing/Shouting v Any other way that expels into the air expel the bacilli v Once inhaled by a tuberculin free person, the bacilli multiply in 4 -6 weeks and spreads throughout the body. The bacilli implant in areas of high partial pressure of oxygen: v Lung v Renal cortex
v This is known as the Primary Tuberculosis. The lesion will heal and a scar will appear in the infected loci. v The bacteria at this time goes into a dormant state v When a person's immune system is depressed, a secondary reactivation occurs and is called Secondary Tuberculosis. v Diffuse disseminated infection through vascular channels may occur and has been termed “Miliary Tuberculosis”.
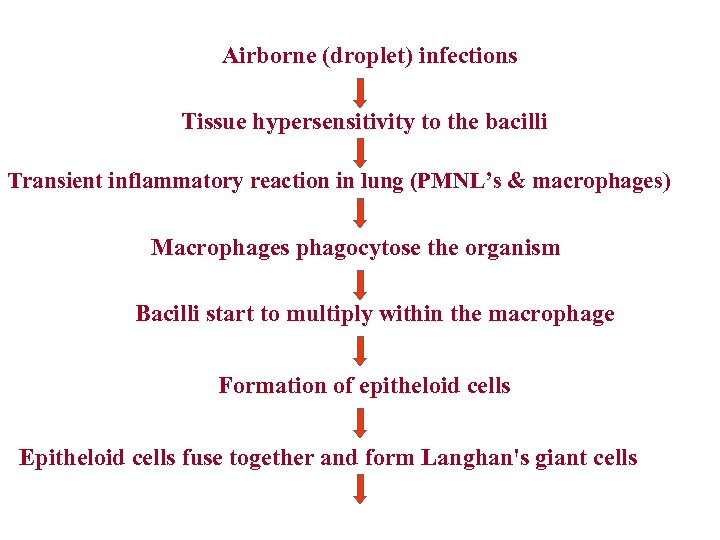
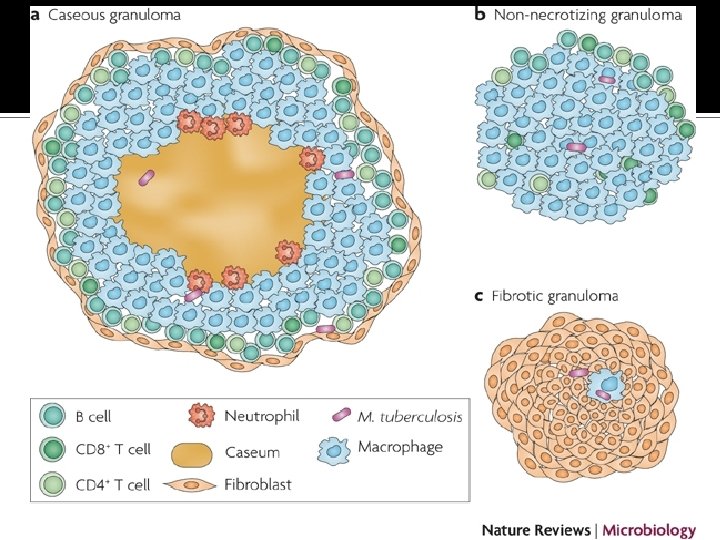
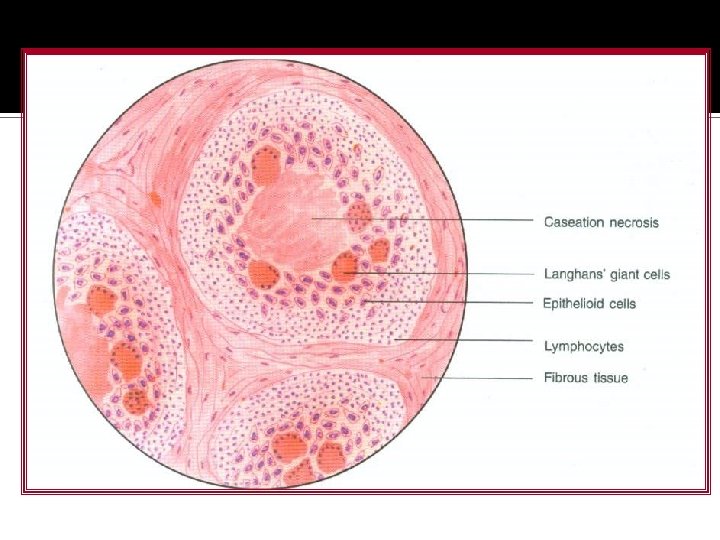
Airborne (droplet) infections Tissue hypersensitivity to the bacilli Transient inflammatory reaction in lung (PMNL’s & macrophages) Macrophages phagocytose the organism Bacilli start to multiply within the macrophage Formation of epitheloid cells Epitheloid cells fuse together and form Langhan's giant cells
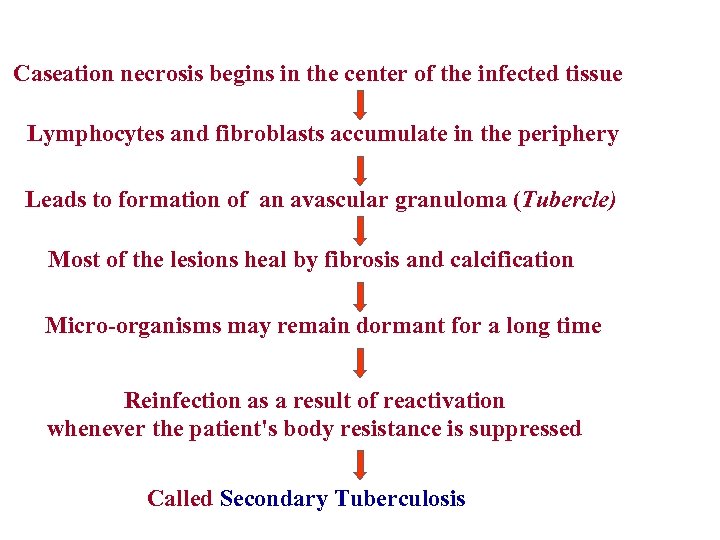
Caseation necrosis begins in the center of the infected tissue Lymphocytes and fibroblasts accumulate in the periphery Leads to formation of an avascular granuloma (Tubercle) Most of the lesions heal by fibrosis and calcification Micro-organisms may remain dormant for a long time Reinfection as a result of reactivation whenever the patient's body resistance is suppressed Called Secondary Tuberculosis
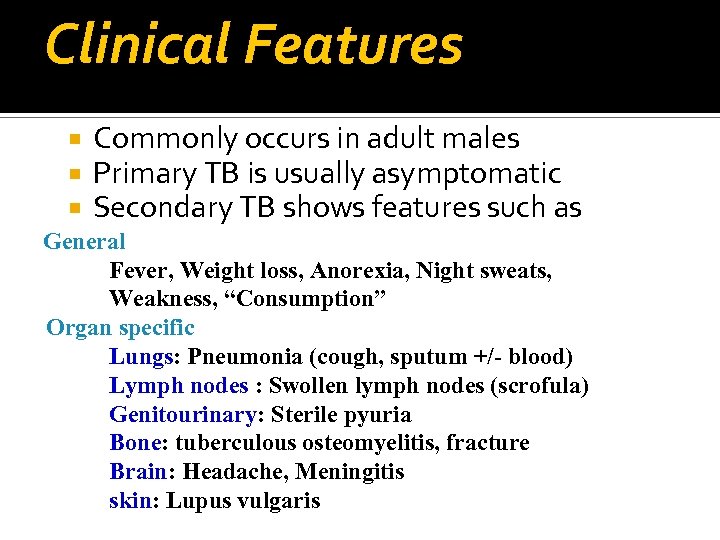
Clinical Features Commonly occurs in adult males Primary TB is usually asymptomatic Secondary TB shows features such as General Fever, Weight loss, Anorexia, Night sweats, Weakness, “Consumption” Organ specific Lungs: Pneumonia (cough, sputum +/- blood) Lymph nodes : Swollen lymph nodes (scrofula) Genitourinary: Sterile pyuria Bone: tuberculous osteomyelitis, fracture Brain: Headache, Meningitis skin: Lupus vulgaris
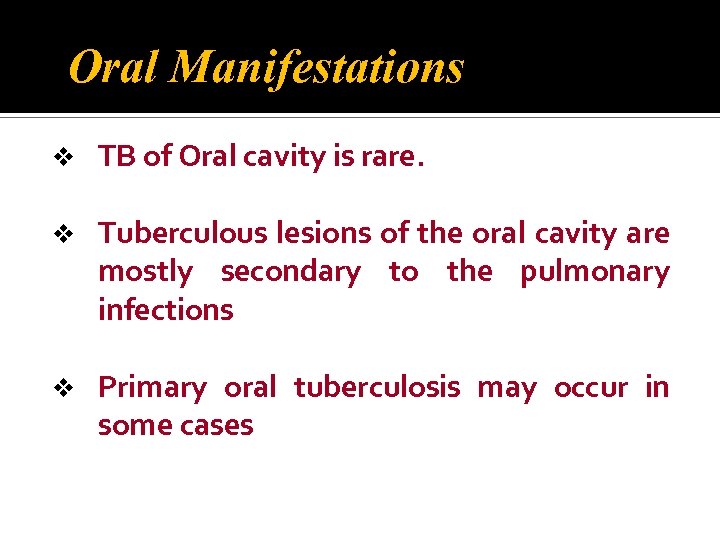
Oral Manifestations v TB of Oral cavity is rare. v Tuberculous lesions of the oral cavity are mostly secondary to the pulmonary infections v Primary oral tuberculosis may occur in some cases
v Intact oral mucosa does not permit tuberculous bacilli to enter into the tissue. v Pre-existing oral lesions may facilitate the entry of these organisms into various oral structures (oral ulcers, periodontitis, dental abscess, cyst, granuloma & leukoplakia ) v Organisms can also reach through hematogenous route to sub mucosa, subsequently proliferate & ulcerate the mucosa.
Dentist may get infected by contact with infected persons v The important tuberculous lesions of the oral cavity are v. Tuberculous ulcers v. Tuberculous gingivitis v. Tuberculous osteomyelitis v. Tuberculosis of the salivary glands v v May also produce nodules, vesicles, fissures, plaques, granulomas or verrucal-papillary lesions
v Tubercular ulcers v Single or multiple ulcers which are irregular , superficial or deep, painful & tend to increase slowly in size. v Have a granulating floor with minimum induration and surrounding mucosa is inflamed and edematous v May occur in any intraoral site, however tongue is the most common site. (Palate, buccal mucosa, gingiva, lips, alveolar ridge and vestibules may also be affected).
v Tubercular granuloma v Seen as soft, non-tender swelling v May occur in any intraoral site, palate is the most common site. v May develop in the periapical region of a grossly decayed tooth due to the entry of organism through the pulp canal- Tubercular periapical granuloma / tuberculoma v Tubercular Gingivitis Small granulating ulcers or erosive lesions with concomitant gingival hyperplasia
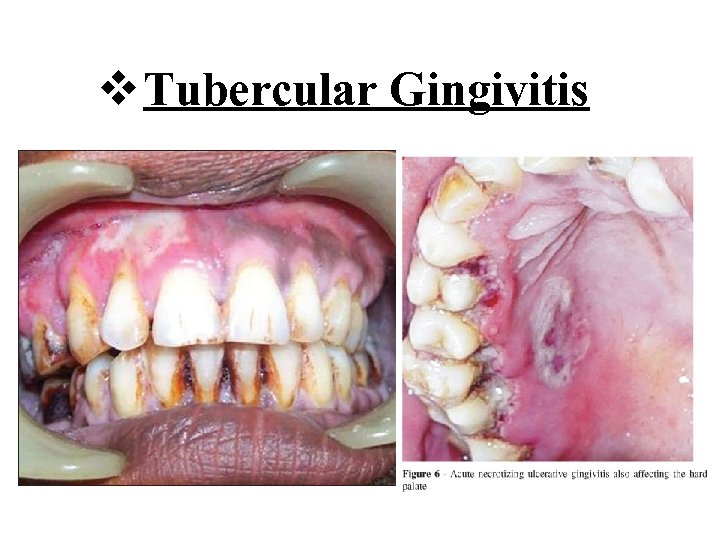
v Tubercular Gingivitis
v Tuberculous osteomyelitis v. Develop due to entry of organisms through decayed tooth or due to hematogenous spread. v Pain, swelling, sinus/fistula formation, trismus, paresthesia. v Tuberculosis of salivary gland v Generalized glandular swelling or abscess formation along with pain, facial palsy & fistula formation
v Scrofula v. Enlarged oropharyngeal lymphoid tissue with involvement of cervical lymph nodes. Caseous necrosis &numerous draining fistula through overlying skin Lupus vulgaris – Tuberculous involvement of skin
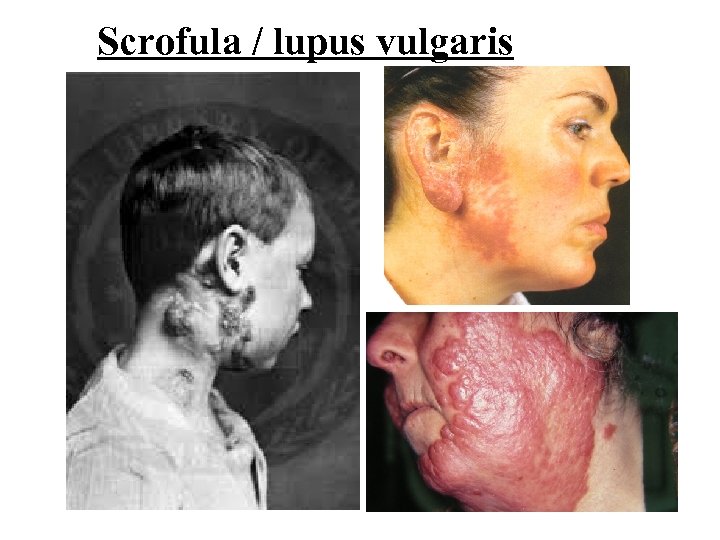
Scrofula / lupus vulgaris

Histopathology
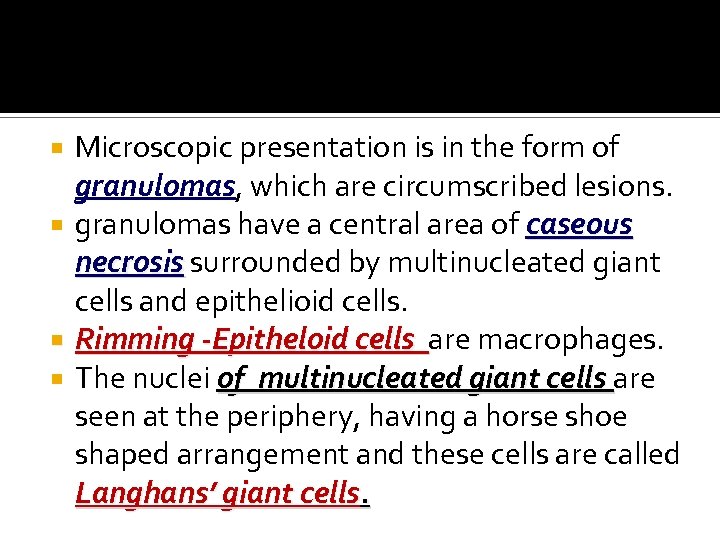
Microscopic presentation is in the form of granulomas, which are circumscribed lesions. granulomas have a central area of caseous necrosis surrounded by multinucleated giant cells and epithelioid cells. Rimming -Epitheloid cells are macrophages. The nuclei of multinucleated giant cells are seen at the periphery, having a horse shoe shaped arrangement and these cells are called Langhans’ giant cells.
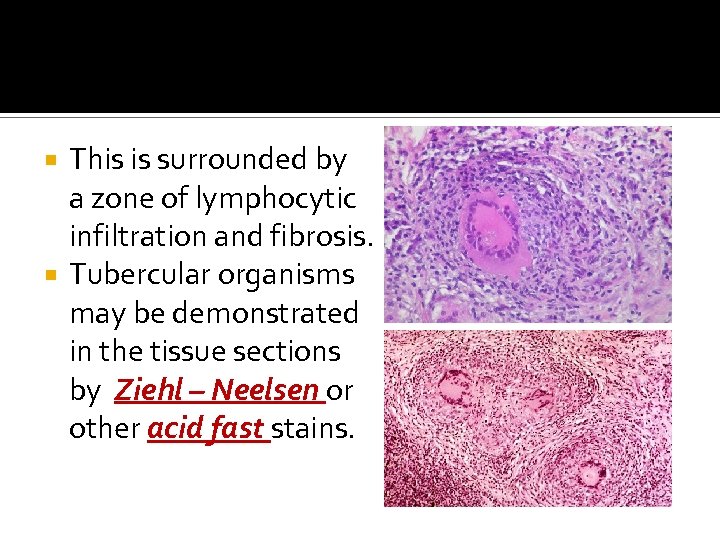
This is surrounded by a zone of lymphocytic infiltration and fibrosis. Tubercular organisms may be demonstrated in the tissue sections by Ziehl – Neelsen or other acid fast stains.
Investigations v v v v Staining of the smear prepared from sputum by Ziehl-Neelsen stain Chest radiograph Bacterial culture in Lowenstein-Jensen media (materials used for culture may be sputum, laryngeal swab, gastric lavage, urine, cerebrospinal fluid and pus, etc. ) Animal inoculation Histopathology Tuberculin test / Mantoux test Enzyme-linked immunosorbent assay (ELi. SA) test PCR (polymerase chain reaction)
Treatment By antitubercular drugs in different regimens
Historical Perspective It was first described in the 1500’s Also called as LUES Was known as “The Great Imitator” Imitator because so many of the signs and symptoms are indistinguishable from those of other diseases
Syphilis is a sexually transmitted disease (STD) caused by a microscopic bacterium called the Treponema pallidum, which enters the blood pallidum stream and infects the entire body. Syphilis has an incubation period of 1 -13 weeks before any signs or symptoms. The disease is generally classified into two: Acquired syphilis Congenital syphilis
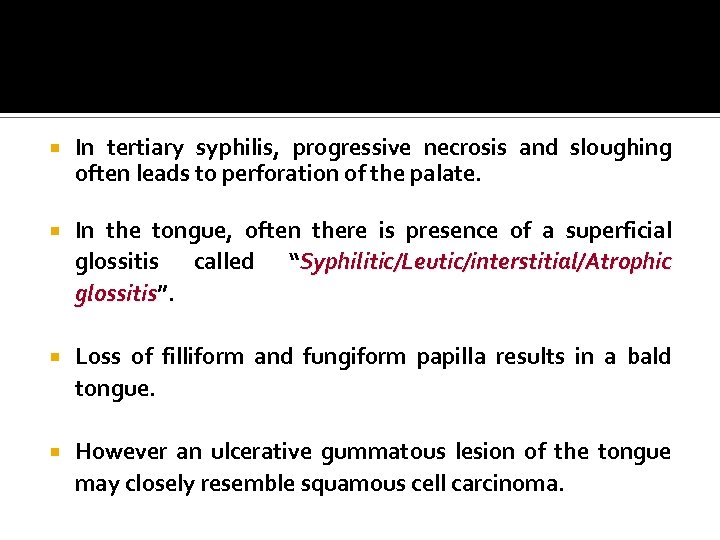
4 Stages of Syphilis Acquired syphilis Primary Stage Secondary Stage Latent Stage Tertiary Stage
Acquired Syphilis Is acquired from an infected person It can be either through Careless handling of the infected patients by the health professionals Sexual contact with an infected partner Drug abusers Manifests in four stages: 1. Primary syphilis 2. Secondary syphilis 3. Latent syphilis 4. Tertiary (late) syphilis
Primary Syphilis Develops at the site of inoculation approximately 3 weeks after infection Clinical symptoms appear at the site of inoculation male and female genitalia extra genital site like-fingers, oral region, perianal region & nipples, etc. (at these sites the spirochetes undergo rapid replication and enter into the lymphatics or blood stream)
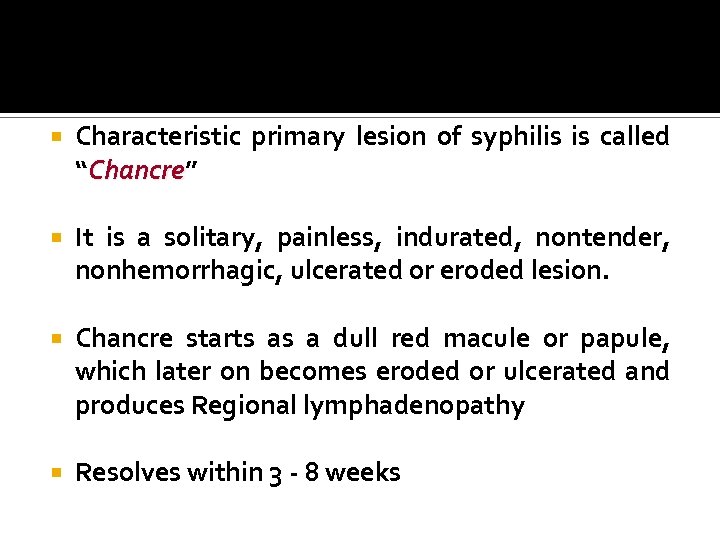
Characteristic primary lesion of syphilis is called “Chancre” Chancre It is a solitary, painless, indurated, nontender, nonhemorrhagic, ulcerated or eroded lesion. Chancre starts as a dull red macule or papule, which later on becomes eroded or ulcerated and produces Regional lymphadenopathy Resolves within 3 - 8 weeks
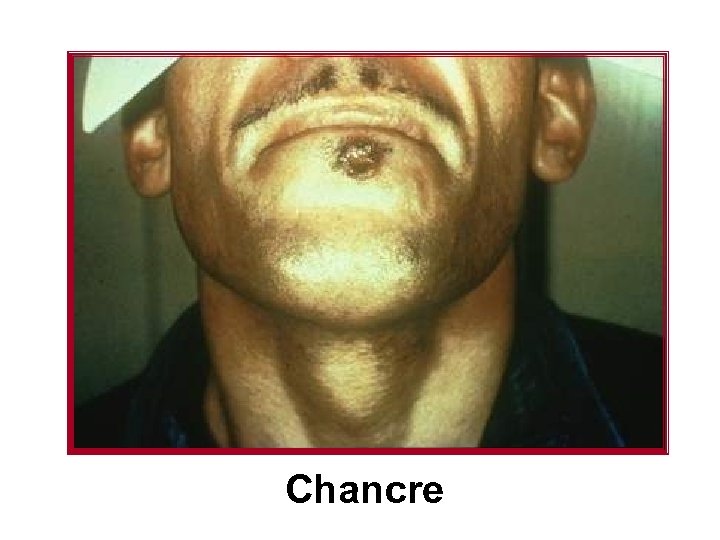
Chancre

Primary Syphilis: Oral manifestations Chancre occurs on the lips, tongue, palate, gingiva, uvula and tonsils May be painful due to secondary infection and are highly contagious in nature Chancres are ulcerated, indurated lesions covered by a grayish white membrane Often mistaken for an early carcinoma
Tongue lesions- seen on the lateral surface of the anterior two-third area or on the dorsal surface and often there is enlargement of the folate papilla. Tonsils show edema, redness and surface erosions or ulcerations. Lymph nodes are enlarged bilaterally, these are painless and rubbery in consistency Heals by scarring within 3 -6 weeks time
Secondary Syphilis Also called Metastatic Stage Appears in about 6 -8 weeks after the appearance of the primary chancre Occurs due to the generalized hematogenous dissemination of the infection in the body Characterized by skin lesions, mucosal lesions, few constitutional symptoms and generalized lymphadenopathy
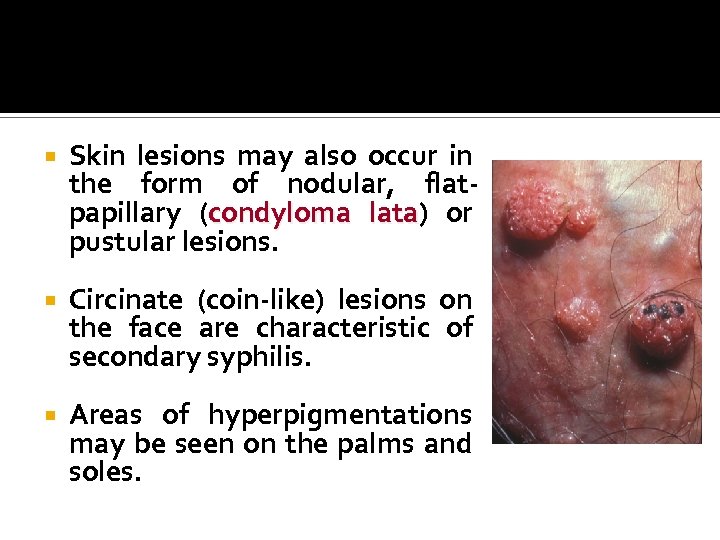
Skin lesions may also occur in the form of nodular, flatpapillary (condyloma lata) or lata pustular lesions. Circinate (coin-like) lesions on the face are characteristic of secondary syphilis. Areas of hyperpigmentations may be seen on the palms and soles.
Constitutional symptoms with secondary syphilis include-headache, anorexia, fever, joint and muscle pain, laryngitis and pharyngitis, etc. Generalized lymphadenopathy is common and the nodes are painless, discrete and not fixed to the surrounding tissues. With or without treatment secondary lesions usually heal within 2 -4 weeks time At times in immunocompromised patients , it become wide spread & is referred to as ‘ Leus Maligna’
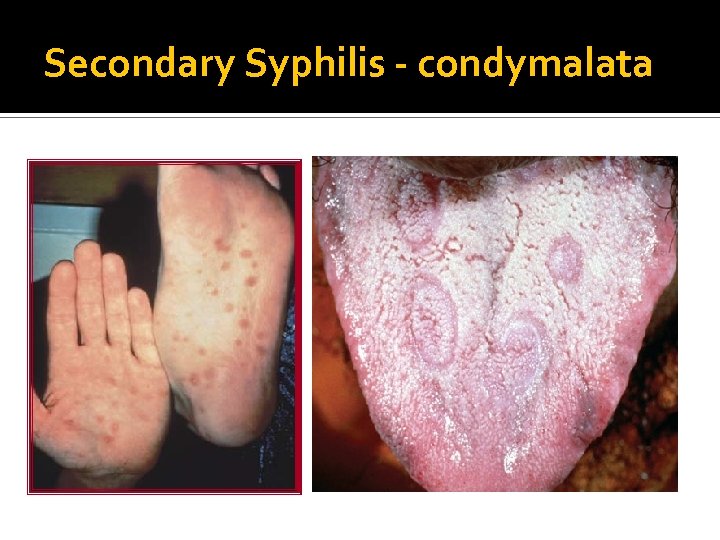
Secondary Syphilis - condymalata


Leus Maligna’
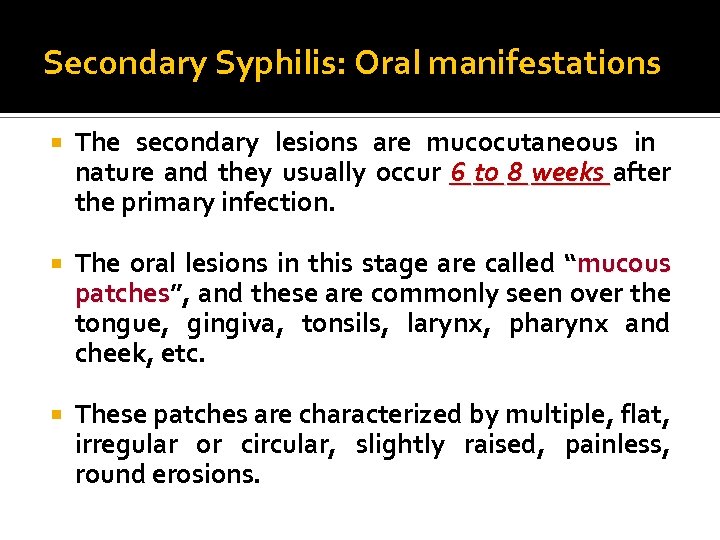
Secondary Syphilis: Oral manifestations The secondary lesions are mucocutaneous in nature and they usually occur 6 to 8 weeks after the primary infection. The oral lesions in this stage are called “mucous patches”, and these are commonly seen over the patches tongue, gingiva, tonsils, larynx, pharynx and cheek, etc. These patches are characterized by multiple, flat, irregular or circular, slightly raised, painless, round erosions.
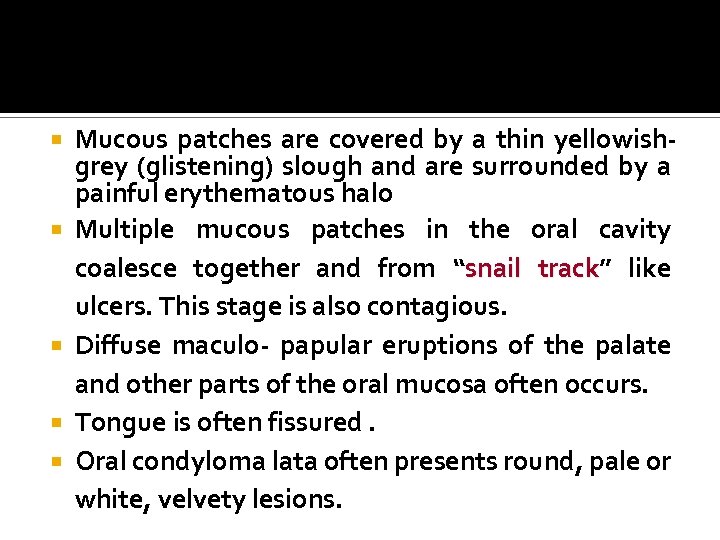
Mucous patches are covered by a thin yellowishgrey (glistening) slough and are surrounded by a painful erythematous halo Multiple mucous patches in the oral cavity coalesce together and from “snail track” like track ulcers. This stage is also contagious. Diffuse maculo- papular eruptions of the palate and other parts of the oral mucosa often occurs. Tongue is often fissured. Oral condyloma lata often presents round, pale or white, velvety lesions.
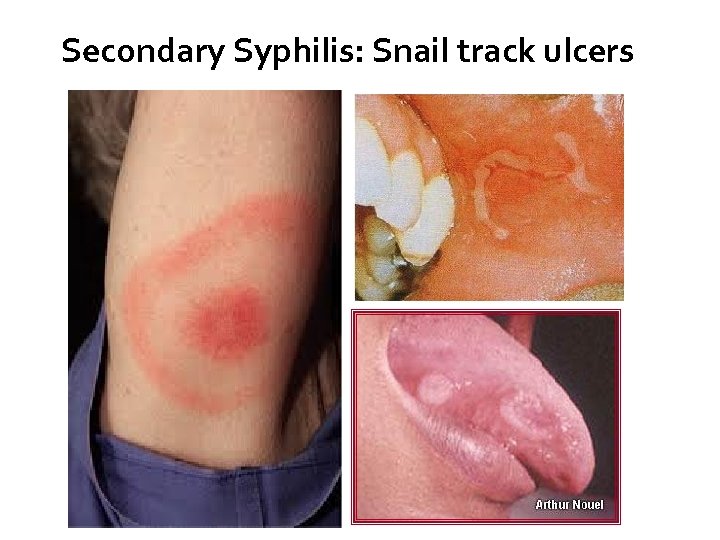
Secondary Syphilis: Snail track ulcers
Latent Syphilis Called the Hidden Stage Begins when the Secondary symptoms disappear The bacteria begins to infest the bone marrow, lymph glands, vital organs, and the central nervous system It may last up to a month or a lifetime 1/3 of the cases left untreated will proceed to tertiary stage

Latent Syphilis
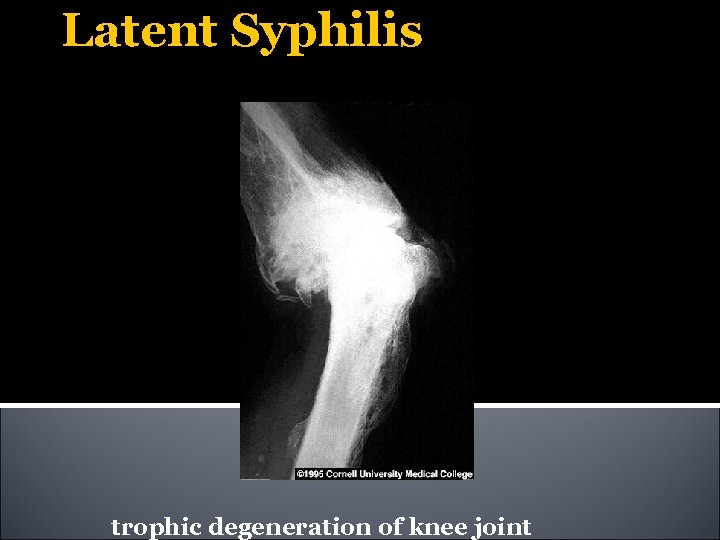
Latent Syphilis trophic degeneration of knee joint
Tertiary (Late) Syphilis Occurs about 5 -10 years after the primary infections and it affects nearly every organs of the body It mainly affects skin, mucous membrane, CNS & CVS Typical lesions of tertiary syphilis is called " Gumma", which is a localized, chronic Gumma granulomatous lesion having either nodular or ulcerated surface. Granulomatous ulcerative lesion often appears as a “punched-out” ulcer, having vertical walls and a dull red granulomatous base with an irregular outline.
Skin lesions heal very slowly and often they leave "tissue paper" like scars. Tertiary syphilis occurring in pregnancy often results in congenital syphilis of the newborn The most serious complication of tertiary syphilis is the destruction of the walls of large blood vessels, resulting in aneurysm and cardiac insufficiency. Involvement of central nervous system (neurosyphilis) results in generalized paresis, dementia and strokes.

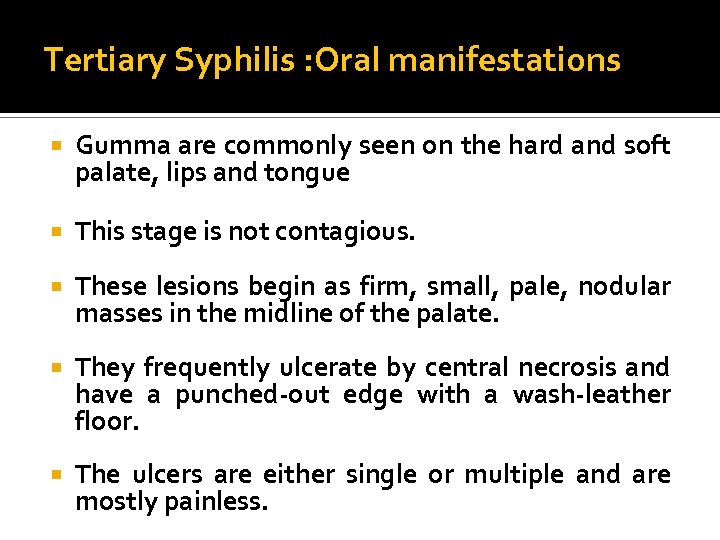
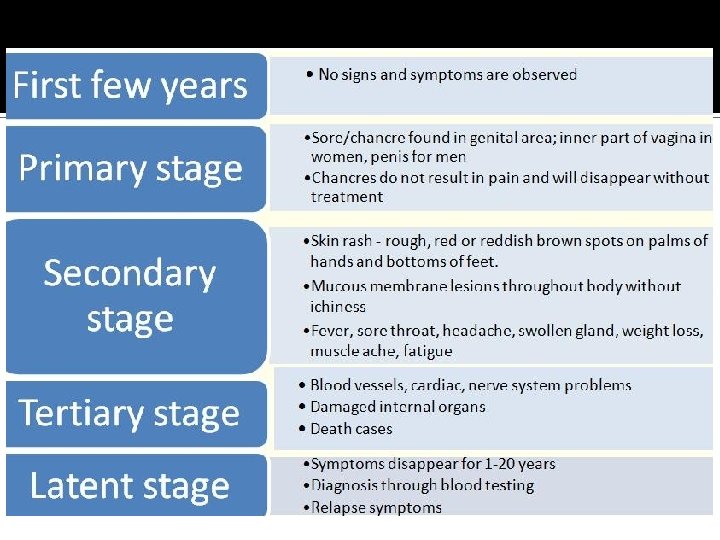
Tertiary Syphilis : Oral manifestations Gumma are commonly seen on the hard and soft palate, lips and tongue This stage is not contagious. These lesions begin as firm, small, pale, nodular masses in the midline of the palate. They frequently ulcerate by central necrosis and have a punched-out edge with a wash-leather floor. The ulcers are either single or multiple and are mostly painless.
In tertiary syphilis, progressive necrosis and sloughing often leads to perforation of the palate. In the tongue, often there is presence of a superficial glossitis called “Syphilitic/Leutic/interstitial/Atrophic glossitis”. glossitis Loss of filliform and fungiform papilla results in a bald tongue. However an ulcerative gummatous lesion of the tongue may closely resemble squamous cell carcinoma.
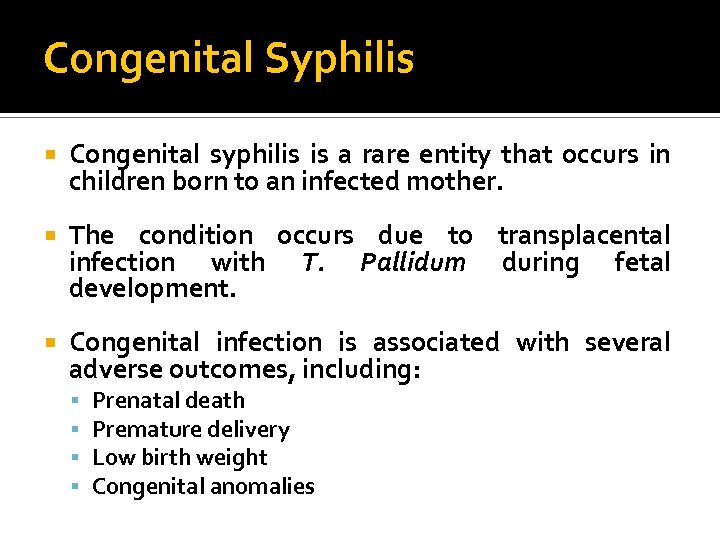
Congenital Syphilis Congenital syphilis is a rare entity that occurs in children born to an infected mother. The condition occurs due to transplacental infection with T. Pallidum during fetal development. Congenital infection is associated with several adverse outcomes, including: Prenatal death Premature delivery Low birth weight Congenital anomalies
Two-thirds of live-born neonates with Congenital syphilis are asymptomatic at birth. Overt infection can manifest in the fetus, the newborn, or later in childhood. The infant may have many or even no signs until 6 -8 weeks of life (delayed form). Clinical manifestations after birth are divided arbitrarily into: - Early CS (<=2 years of age) - Late CS ( >2 years of age)
Clinical Manifestations of Early Congenital syphilis Condyloma Lata Maculopapular rash Hepatosplenomegaly Jaundice due to the hepatitis Anemia Osteochondritis Pseudoparalysis Lymphadenopathy Mucous patches

Clinical Manifestations of Late Congenital syphilis Frontal bossing Saddle nose Short maxilla High -arched palate Relative prognathism of mandible Hutchinson's tooth Mulberry molars Hutchinson's incisors
Interstitial keratitis Eighth nerve deafness Rhagades Premature perioral fissuring Higoumenaki's sign Enlargement of clavicle adjacent to the sternum Saber shin Anterior bowing of tibia as a result of periostitis Scaphoid scapulae Concavity of vertebral border of the scapulae Clutton's joint Painless synovitis and enlargement of joints, usually the knee
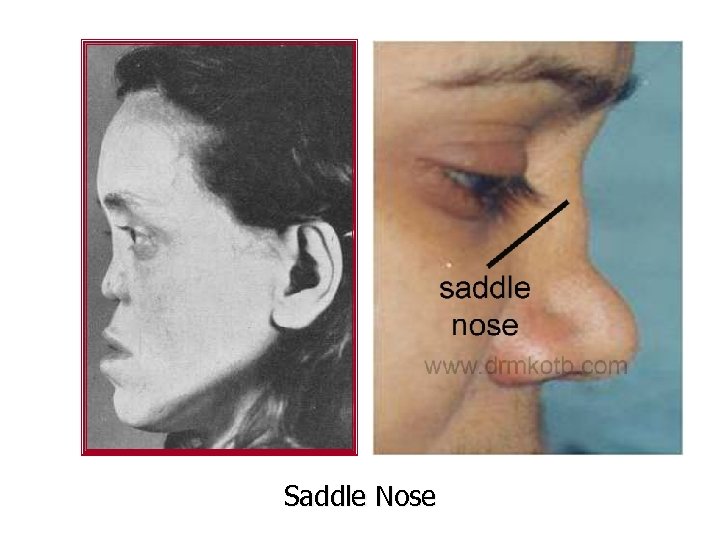
Saddle Nose
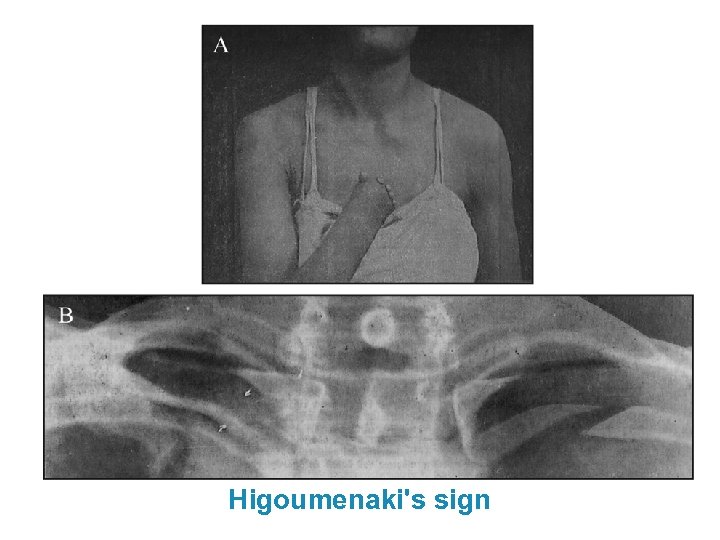
Higoumenaki's sign
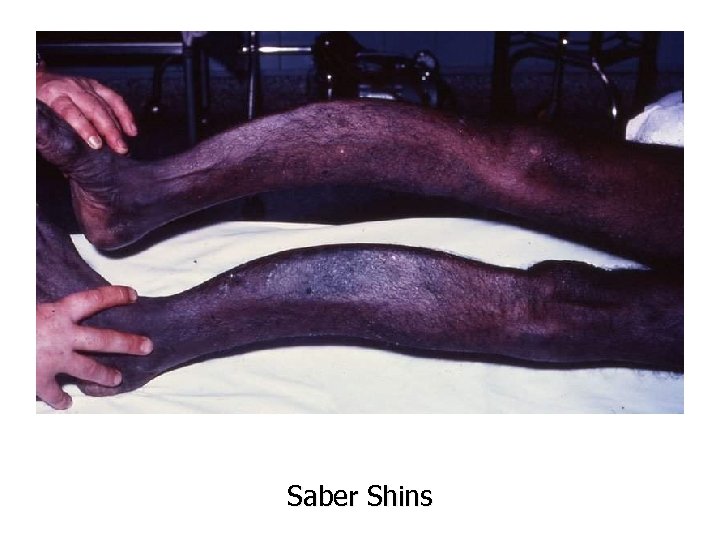
Saber Shins
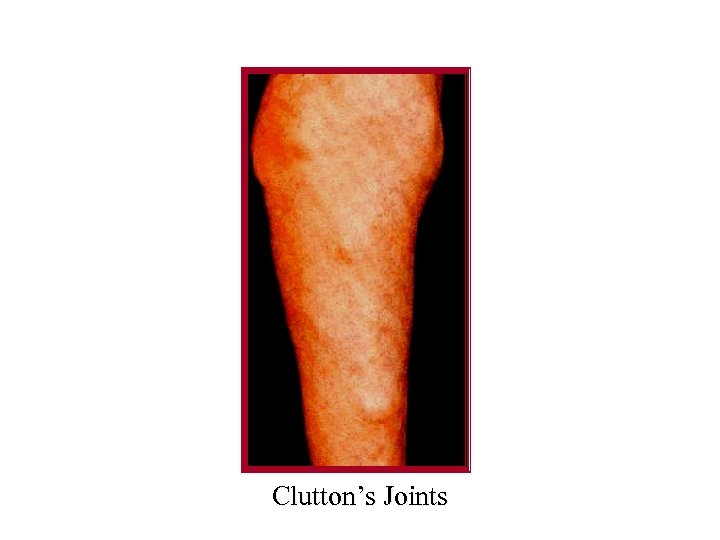
Clutton’s Joints

https: //classconnection. s 3. amazonaws. com/5 11/flashcards/3339511/jpg/median_rhomboid _glossitis-1454437 EBE 81 F 8381 A 3. jpg
Hutchinson's triad Described by Sir Jonathan Hutchinson in 1858. Defined the following three pathognomonic diagnostic features Hutchinson's teeth Ocular interstitial keratitis Eighth nerve deafness Few patients exhibit all three features
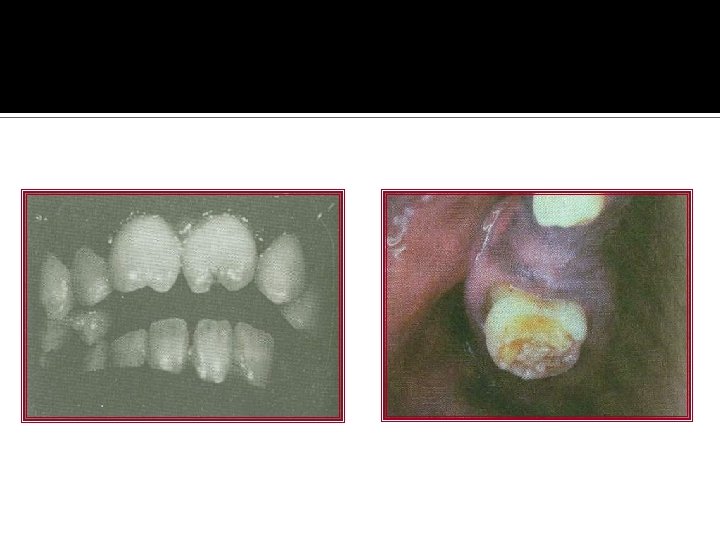
Hutchinson's teeth The infection alters the formation of both the anterior teeth (Hutchinson's incisors) and the incisors posterior dentition (Mulberry molars, Fournier's molars, Moon's molars). molars Hutchinson's incisors exhibit their greatest mesiodistal width in the middle third of the crown. The incisal third tapers to the incisal edge, and the resulting tooth resembles a straightedge screwdriver The middle lobe is affected. The incisal edge often exhibits a central hypoplastic notch.
Mulberry molars taper toward the occlusal surface with a constricted grinding surface. The occlusal anatomy is abnormal, with numerous disorganized globular projections that resemble the surface of a mulberry

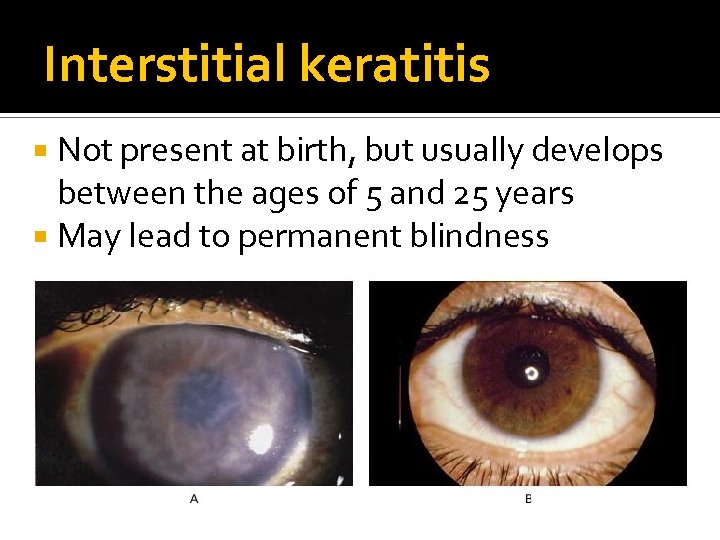
Interstitial keratitis Not present at birth, but usually develops between the ages of 5 and 25 years May lead to permanent blindness

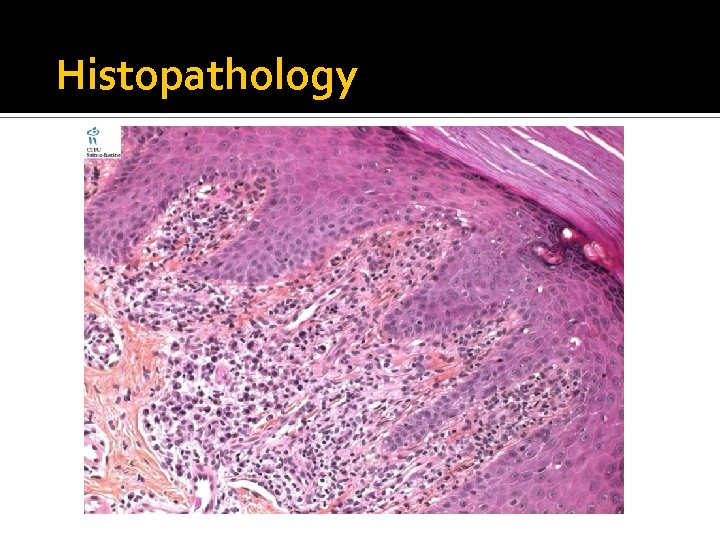
Histopathology Histopathologic picture of the oral lesions - not specific. During the first two stages, the pattern is similar The surface epithelium is ulcerated in 10 lesions & may be ulcerated/hyperplastic in the 20 stage. The underlying lamina propria may demonstrate an increase in the number of vascular channels, and an intense chronic inflammatory reaction. The infiltrate is composed predominantly of lymphocytes and plasma cells and often demonstrates a perivascular pattern.
Histopathology Oral tertiary lesions typically exhibit surface ulceration, with peripheral pseudo epitheliomatous hyperplasia. The underlying inflammatory infiltrate usually demonstrates foci of granulomatous inflammation with well-circumscribed collections of histiocytes and multi-nucleated giant cells. Even with special stains, the organisms are hard to demonstrate in the third stage
Histopathology
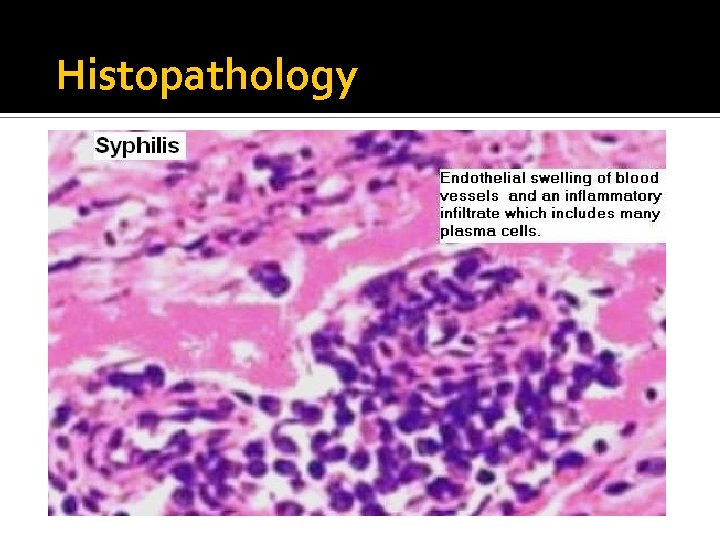
Histopathology
Diagnosis Detection of bacteria in smear by dark ground illumination microscopy Bacterial culture in artificial media. Serological tests Wasserman reaction, Khan test, Venereal disease research laboratory (VDRL) test, Rapid Plasma Reagin (RPR) test, T pallidum hemagglutination assay (TPHA) & Fluorescent treponemal antibody absorption(FTA-ABS) ELISA. Histopathology.
Treatment Penicillin- In high doses Erythromycin or tetracycline – In case of patients allergic to penicillin Blood tests - to make sure the infection has been eliminated. Tertiary syphilis is incurable
ACTINOMYCOSIS Actinomycosis is a chronic granulomatous, suppurative and fibrosing infection. Although the term actinomycosis seems to imply a fungal infection, it is an infection of filamentous, branching, gram-positive anaerobic, non acid fast bacteria Actinomyces-israelii A viscosus A naeslundii A odontolyticus A, meyeri A. bovis
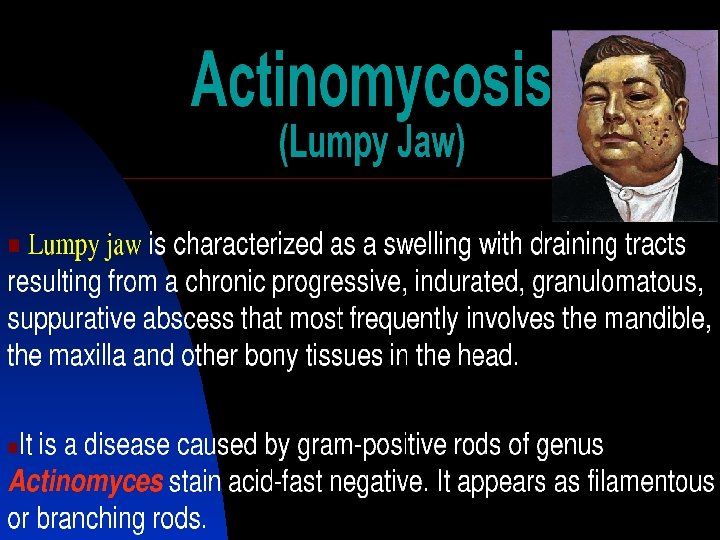
The microorganisms are normal inhabitants of the oral cavity Sites of colonization in healthy patients include the tonsillar crypts, dental plaque and calculus, carious dentin, gingival sulci, and periodontal pockets. Takes entry into the tissues during trauma or tooth extraction to produce infection Occurs in three forms: Cervicofacial (commonest form) Abdominal Pulmonary actinomycosis
Pathogenesis The organisms enter tissue through an area of prior trauma or soft tissue injury, periodontal pocket, extraction socket, or infected tonsil. The infection does not spread along the typical facial plain and usually disregards the normal lymphatic and vascular routes. Direct extension soft tissue is seen producing indurated swellings which become fluctuant and later organisms drain through multiple sinuses. Lymph nodes become involved only if they are in the path of the process. Lymphadenopathy associated due to secondary infections
Clinical Features Cervicofacial Age: disease occurs mostly in the fourth and fifth decade of life. Sex: More prevalent among males. Site: The soft tissues of the submandibular, submental, and cheek areas are common areas of involvement, with the area overlying the angle being the most frequently affected site.
The organism enters tissue through an area of prior trauma or soft tissue injury, periodontal pocket, extraction socket, or infected tonsil The infection does not spread along the typical facial plain and usually do not take normal lymphatic and vascular routes Direct extension through soft tissue is seen and lymph nodes become involved only if they are in the path of the process. Lymphadenopathy associated with this disease may be due to secondary infections caused by some other organisms.
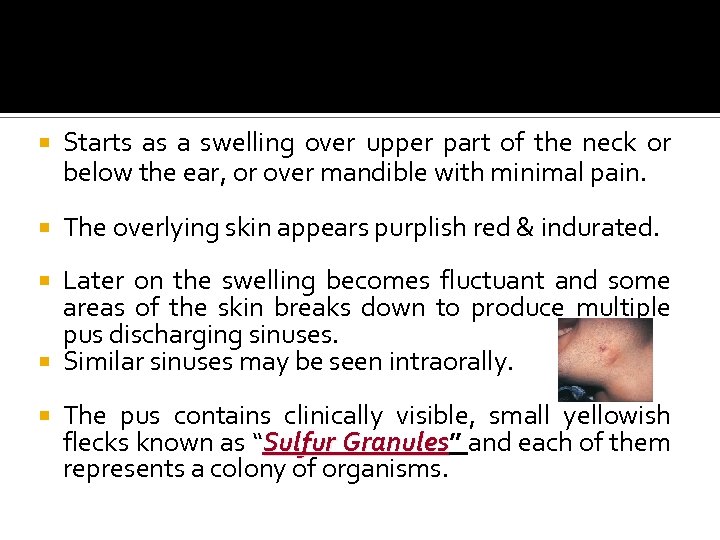
Starts as a swelling over upper part of the neck or below the ear, or over mandible with minimal pain. The overlying skin appears purplish red & indurated. Later on the swelling becomes fluctuant and some areas of the skin breaks down to produce multiple pus discharging sinuses. Similar sinuses may be seen intraorally. The pus contains clinically visible, small yellowish flecks known as “Sulfur Granules” and each of them Granules represents a colony of organisms.


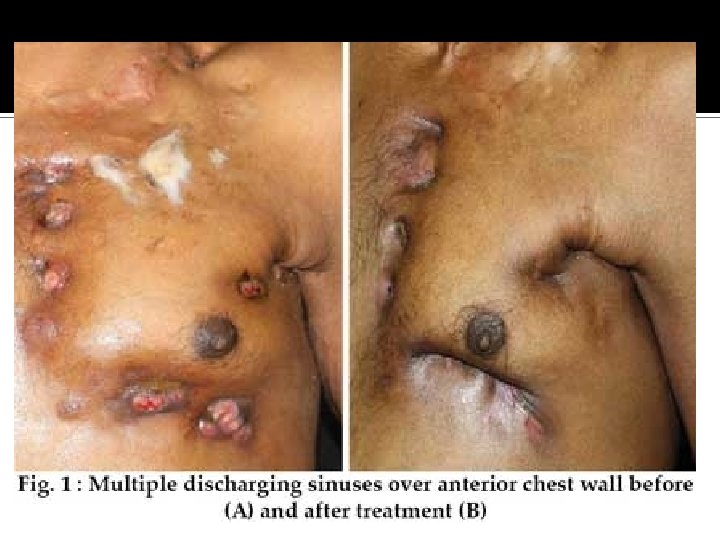
The pus discharging sinuses heal up, but later on, some new sinuses appear in the region and the process continues for years and causes great deal of scarring and disfigurement of the skin. Involvement of the jaw bones by this disease often results in chronic osteomyelitis Lesions localize at the apices of teeth and may simulate periapical granulomas or cyst
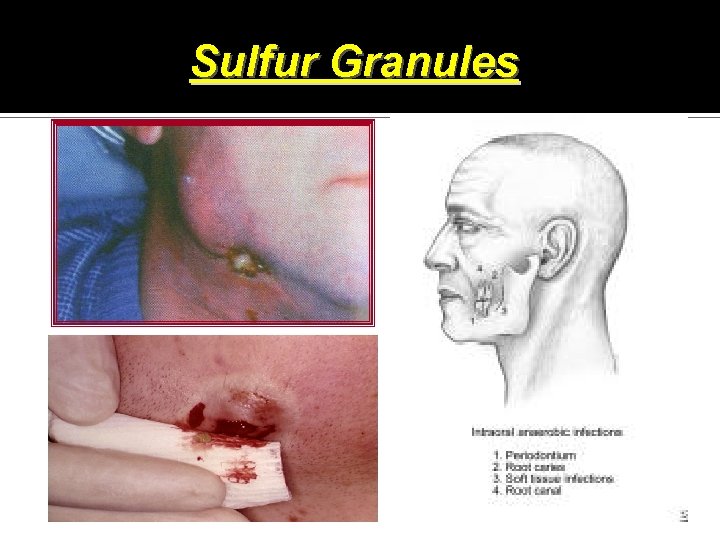
Sulfur Granules
Abdominal Extremely severe form High mortality rate Exhibit as a mass fixed to the underlying skin or as abscess involving any organ Accompanied by symptoms such as fever, chills, nausia, vomiting etc THORACIC FORM Fever & chills with productive cough and pleural pain
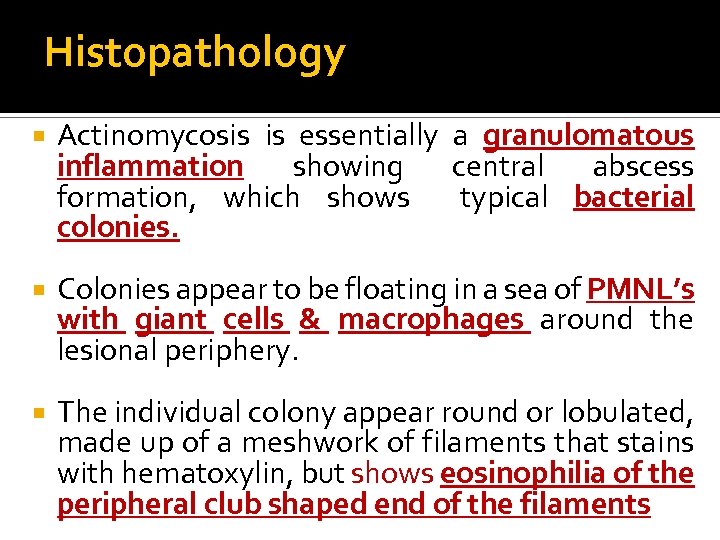
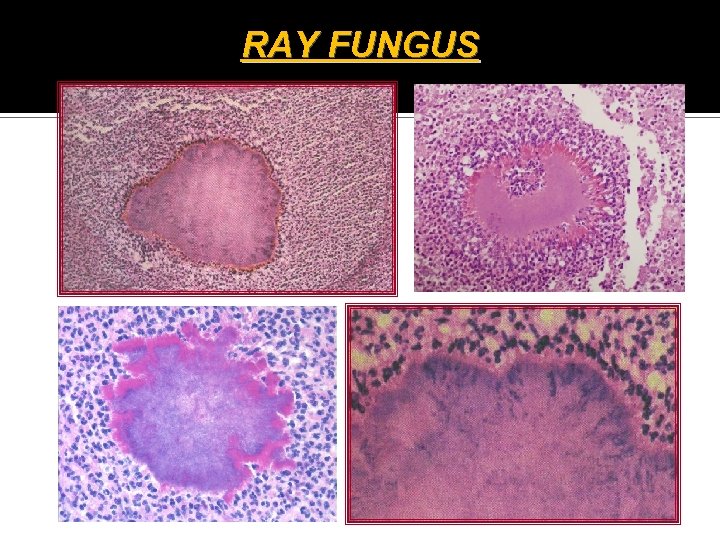
Histopathology Actinomycosis is essentially a granulomatous inflammation showing central abscess formation, which shows typical bacterial colonies. Colonies appear to be floating in a sea of PMNL’s with giant cells & macrophages around the lesional periphery. The individual colony appear round or lobulated, made up of a meshwork of filaments that stains with hematoxylin, but shows eosinophilia of the peripheral club shaped end of the filaments
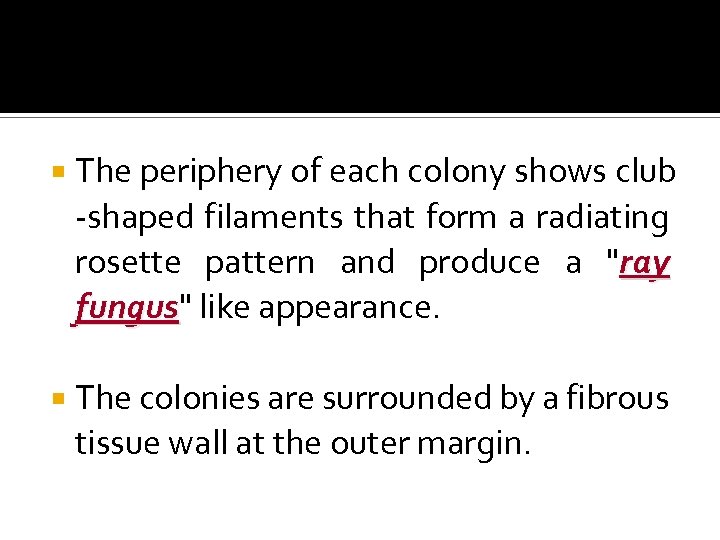
The periphery of each colony shows club -shaped filaments that form a radiating rosette pattern and produce a "ray fungus" like appearance. fungus The colonies are surrounded by a fibrous tissue wall at the outer margin.
RAY FUNGUS
Diagnosis Culturing of organisms Histopathological diagnosis Immunofluorescent techniques
Treatment High doses of any of the drugs like-penicillin, cephalosporin, clindamycin and lincomycin, etc.
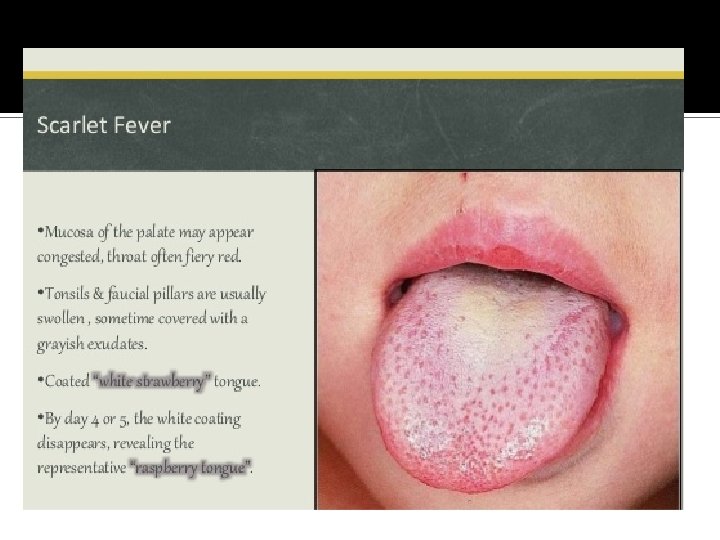
SCARLET FEVER Scarlet fever is a rare specific bacterial disease caused by Group A, β-hemolytic streptococcus It commonly occurs in children during winter months. The disease begins as streptococcal tonsillitis with pharyngitis in which the organisms elaborate an erythrogenic toxin The toxin attacks the blood vessels and cause the characteristic skin rash
Clinical Features Incubation period ranges from 1 -7 days Significant clinical findings: Fever, Enanthem & Exanthem Also seen are headache, vomiting, tonsillitis, pharyngitis and cervical lymphadenopathy, etc. Fever develops abruptly around second day Temperature peaks around 1030 & returns to normal within 3 days
A diffuse, bright red skin rash appears on the second or third day of the disease, that starts on the chest and gradually spreads to the other body surfaces. The skin rash is particularly more noticeable in areas of pressure & skin folds. Characteristic skin rash is referred to as “ Sunburn with goose pimples”. pimples Skin of the trunk & extremities have a Sand paper texture
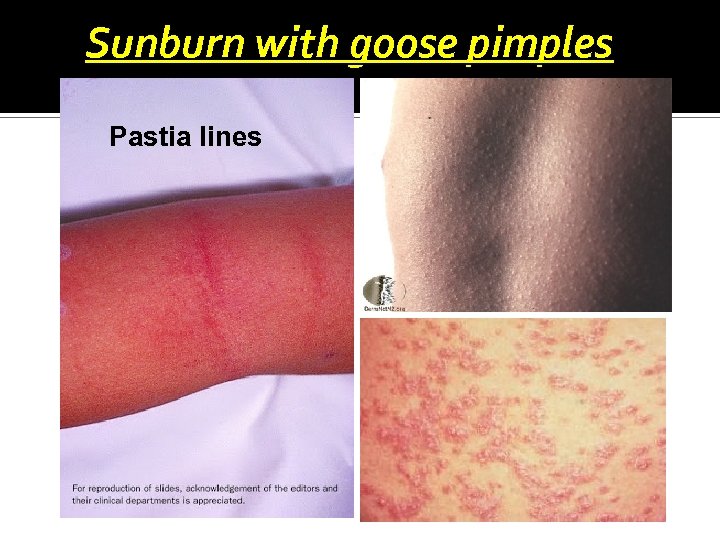
Sunburn with goose pimples Pastia lines
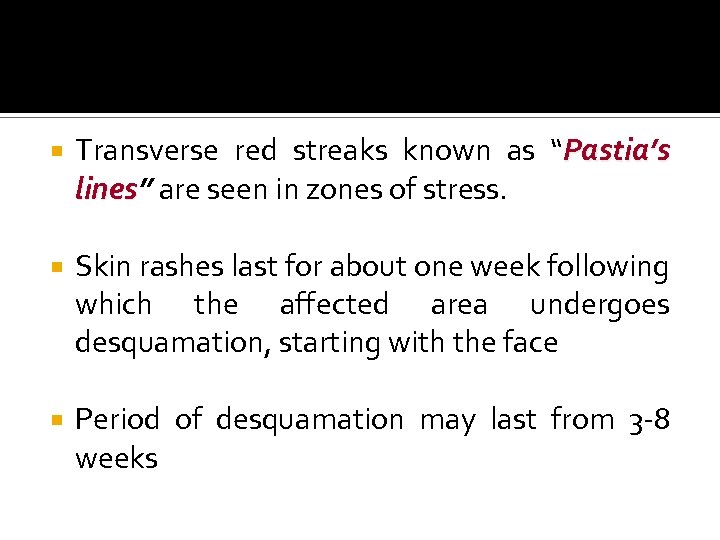
Transverse red streaks known as “Pastia’s lines” are seen in zones of stress. lines Skin rashes last for about one week following which the affected area undergoes desquamation, starting with the face Period of desquamation may last from 3 -8 weeks
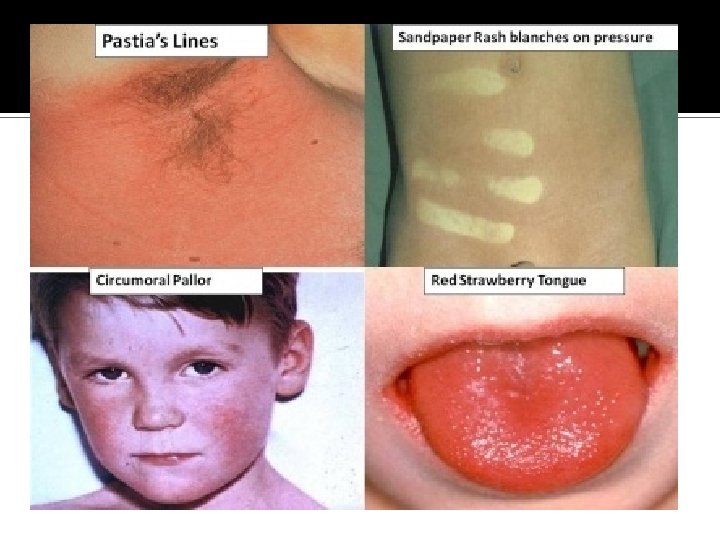
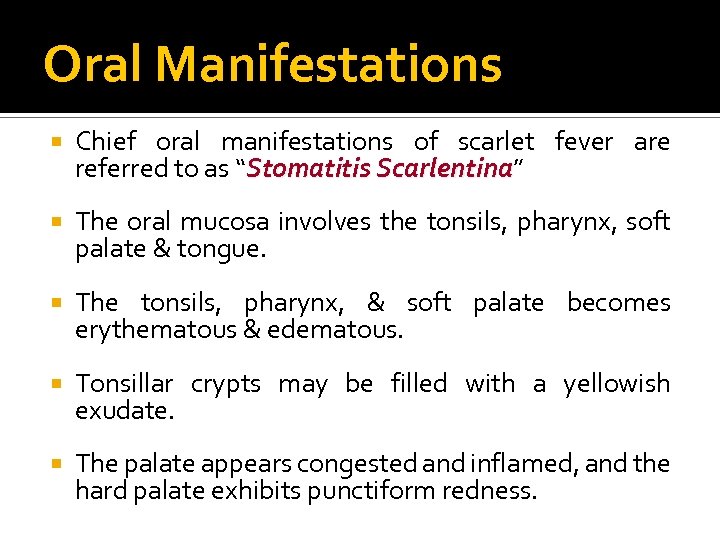
Oral Manifestations Chief oral manifestations of scarlet fever are referred to as “Stomatitis Scarlentina” Scarlentina The oral mucosa involves the tonsils, pharynx, soft palate & tongue. The tonsils, pharynx, & soft palate becomes erythematous & edematous. Tonsillar crypts may be filled with a yellowish exudate. The palate appears congested and inflamed, and the hard palate exhibits punctiform redness.
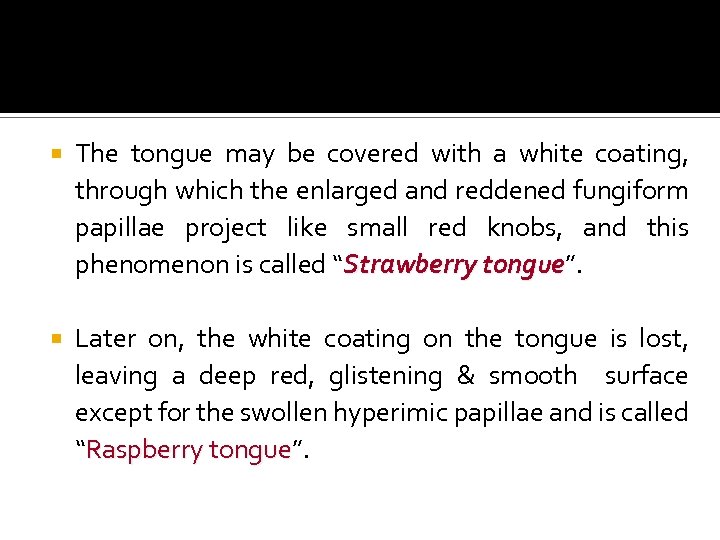
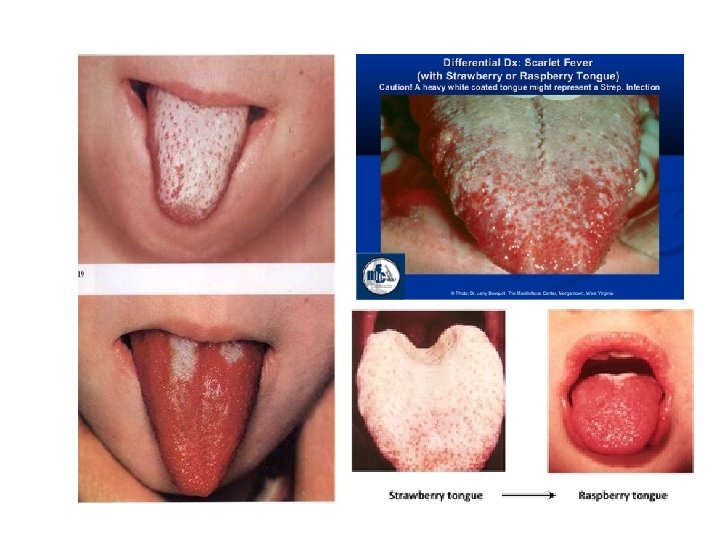
The tongue may be covered with a white coating, through which the enlarged and reddened fungiform papillae project like small red knobs, and this phenomenon is called “Strawberry tongue”. tongue Later on, the white coating on the tongue is lost, leaving a deep red, glistening & smooth surface except for the swollen hyperimic papillae and is called “Raspberry tongue”. tongue
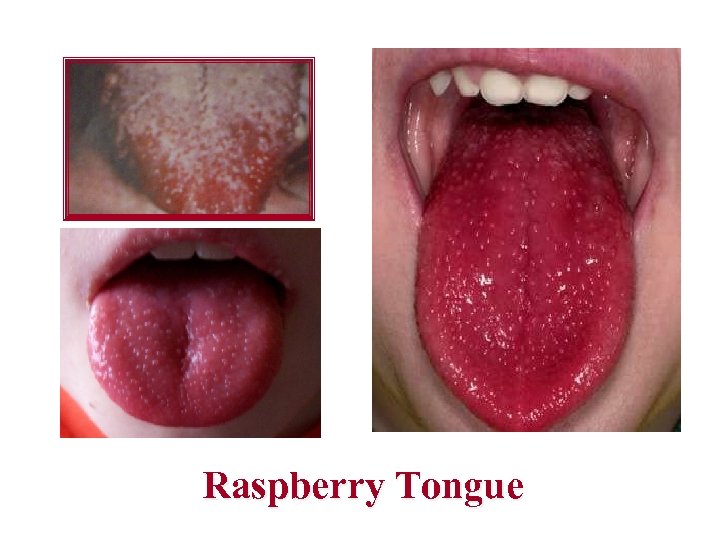
Raspberry Tongue
Treatment Administration of penicillin or erythromycin. With appropriate treatment prognosis is excellent. No available methods for prevention
NOMA Also called as “Cancrum oris; Gangrenous stomatitis & Necrotizing stomatitis” stomatitis Derived from the Greek word “Nomein” meaning "to Nomein devour. " devour Rapidly progressing, gangrene of the oral & facial tissues that occurs in debilitated or nutritionally deficient persons. An opportunistic infection caused by components of the normal oral flora that becomes pathogenic during periods of compromised immune status.
Main causative organisms are Fusobacterium necrophorum or F. nucleatum & Prevotella intermedia. They interact with one or more other bacterial organisms, of which the most commonly implicated are Borrelia vincenti, S. aureus, & Non hemolytic Streptococcus species. May be considered as a secondary complication of a systemic disease rather than a primary disease.
Predisposing factors include: Poverty Malnutrition or dehydration Poor oral hygiene Poor sanitation proximity to livestock Recent debilitating illness Immunodeficiency disorder
Clinical Features In many instances. the infection begins as necrotizing ulcerative gingivitis (NUG). May be considered as an extension of necrotizing ulcerative gingivitis Often begins on the gingiva as NUG, which may extends to involve the adjacent soft tissue by ganngrenous necrosis and forms areas called necrotizing ulcerative mucositis
Typically arises in children aged 1 to 10 years A line of demarcation develops between the healthy tissue & dead tissue Jaw is exposed as large masses of tissue sloughs out Commencement of gangrene is denoted by blackening of the skin. Fetid odor, significant pain, fever, malaise & regional lymphadenopathy are typical.
A related disorder, “Noma Neonatorum”, Neonatorum” arises in the first month of life in low-birth weight infants who also demonstrate malnutrition and frequently a debilitating illness These patients almost always have infection with Pseudomonas aeruginosa. often aeruginosa combined with E. coli, Kiebsiella species, or Staphylococcus species
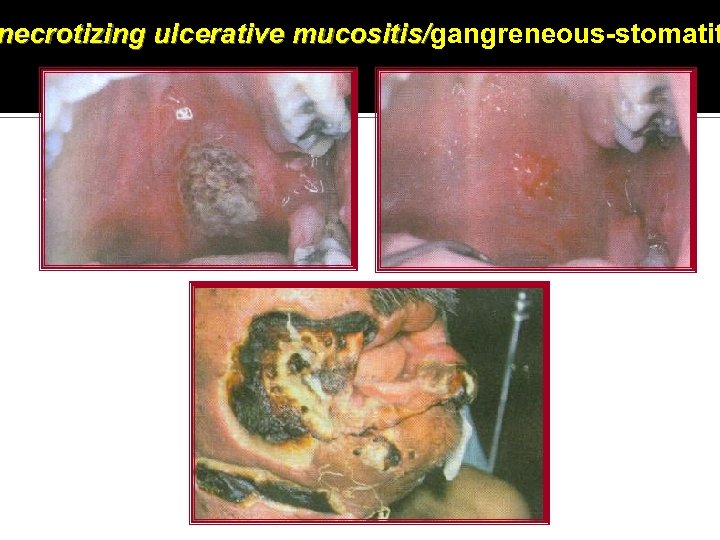
necrotizing ulcerative mucositis/gangreneous-stomatit mucositis/
Complications Severe facial disfigurement Death, as a result of Toxemia Pneumonia Diarrhea

THANK YOU
4ceb1e600715d1085771f973dc998dab.ppt