df116ec3b7b1097a58f6f2c58298baf7.ppt
- Количество слайдов: 110
Back to the Future: Returning to Accountability and Social Responsibility www. ruralmedicaleducation. org Robert C. Bowman, M. D. rcbowman@atsu. edu
This Presentation Given in Honor of West Virginia School of Osteopathic Medicine and its Distinguished and Retiring President Olen E. Jones, Ph. D West Virginia Osteopathic is number one in rural, rural underserved, and total underserved percentages of graduates in the United States u Presentation given at Lewisburg WV in February of 2008 u
Pipeline Issues

All we need to know about Primary Care Capacity is in this picture Redirection of the stream flow u Control valve u Natural tendencies with gravity u Leaks u Needs for maintenance and support u Delivery of primary care work, shaped long before the water enters the turbine u

Pipeline Issues Control Valve - Policy Primary Care Workforce Years Downhill Maintenance Needs Leaks Redirection – Admission and Training
Primary Care Capacity The US fails to admit and train for primary care u The US closes the control valve to primary care u The natural tendencies of those admitted and health policies are major medical center careers u Leaks – even those admitted and trained primary care leak out with poor maintenance and support u Delivery of primary care work is diverted before, during, and after medical education u Basic aspects of primary care escape awareness u
A Season of Accountability and Social Responsibility Was requested by AAMC Chair, Dean of Baylor William T. Butler in 1991 u Dr. Butler’s request as a leader in medicine and medical education was largely ignored, making it still relevant today u The lessons involved a return to awareness u Dr. Butler began with relevant press clippings u
1990 and 1991 Headlines Newsweek: The Revolution in Medicine u Fortune: Taking on Public Enemy No. 1 (health costs) u The New York Times: Ringing: Health Care Alarm u Business & Health: Physician, Cut Thy Costs u Nation’s Business: Curbing Costs of Health u The New York Times: Demands to Fix US Health Care Reach a Crescendo u Newsweek: Milking the Laboratories for Dollars – The Overhead Mess u
A Season of Accountability and Social Responsibility Raised Concerns regarding the supply of generalists, u salaries and support for primary care, u student debt, u the cost of delivering care u rural and underserved distributions u
Butler and the Admiral Stockdale paradox (from Good to Great by Jim Collins) Face the brutal truth of a bad situation but u Faith that you will prevail in the end u We fail to face the brutal truth u We clearly know what needs to be done but fail to do it u We lack faith, except for a few locations u
The Ultimate Accountability and Social Responsibility Efforts u Match medical school efforts to state and national needs for all peoples u Have been consistently successful u Have been documented in 4 letter words RPAP, PSAP, AHEC, RHOP, WAMI u Have been largely ignored by the nation u The Best Effort took 5 letters – WVSOM
An approach to training and retaining primary care physicians in rural Appalachia Feb 1993 Academic Medicine - WVSOM Roberts, A. u Foster, R. u Dennis, M. u Davis, L. u Wells, J. u Bodemuller, M. F. u Bailey, C. A. u
How West Virginia School of Osteopathic Medicine achieves its mission of providing rural primary care physicians Stookey, Baker, Nimitz u J Am Osteopathic Association u November 2000 u
6 Factors from Roberts Study 1993 Focused Achievable Mission u Multistate Educational Exchange u Personalized and interactive recruiting, admission, and placement processes aimed to attract nontraditional, rural students; u Rural Training u Dedicated to Medical Education u Freestanding School in a Rural Environment u
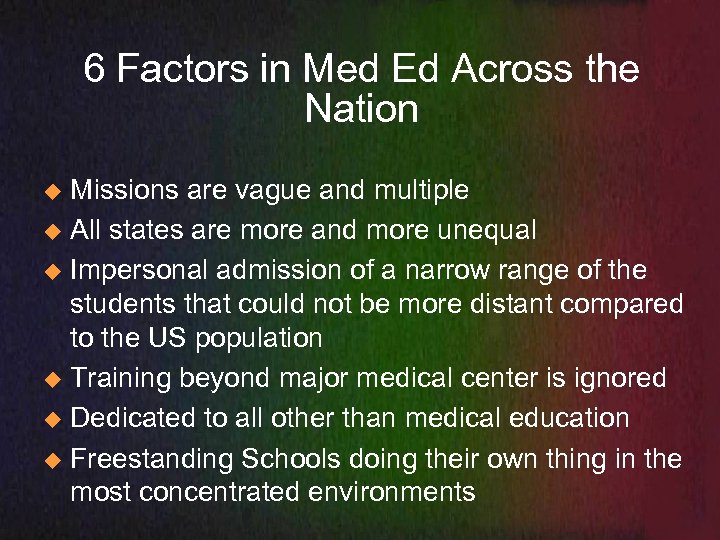
6 Factors in Med Ed Across the Nation Missions are vague and multiple u All states are more and more unequal u Impersonal admission of a narrow range of the students that could not be more distant compared to the US population u Training beyond major medical center is ignored u Dedicated to all other than medical education u Freestanding Schools doing their own thing in the most concentrated environments u
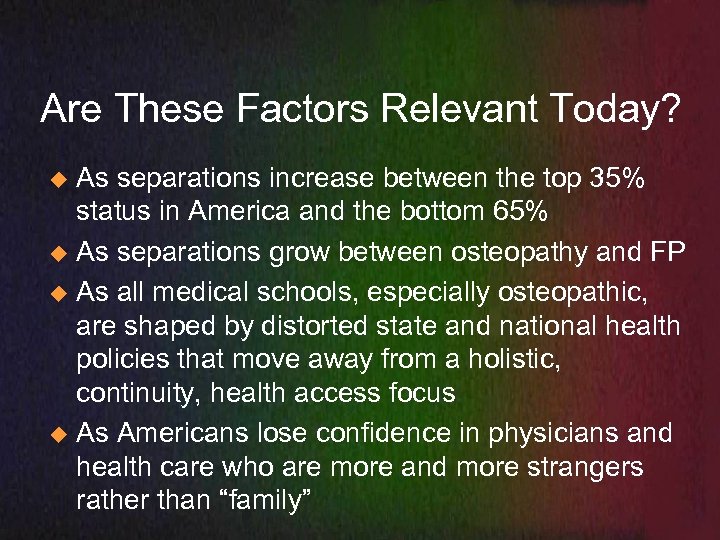
Are These Factors Relevant Today? As separations increase between the top 35% status in America and the bottom 65% u As separations grow between osteopathy and FP u As all medical schools, especially osteopathic, are shaped by distorted state and national health policies that move away from a holistic, continuity, health access focus u As Americans lose confidence in physicians and health care who are more and more strangers rather than “family” u
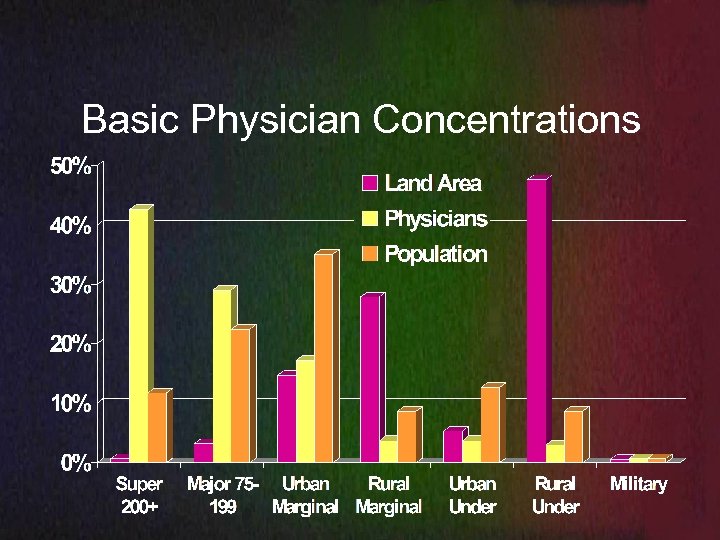
Basic Physician Concentrations
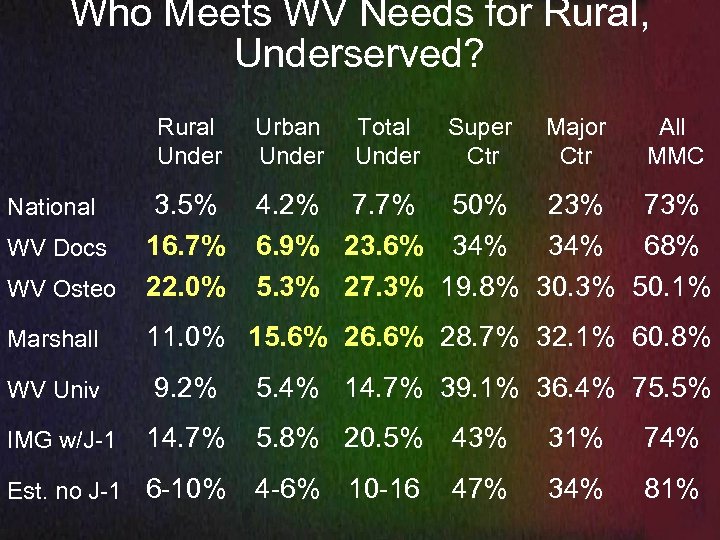
Who Meets WV Needs for Rural, Underserved? Rural Under Urban Under Total Under Super Ctr Major Ctr All MMC WV Osteo 3. 5% 16. 7% 22. 0% Marshall 11. 0% 15. 6% 26. 6% 28. 7% 32. 1% 60. 8% National WV Docs 4. 2% 7. 7% 50% 23% 73% 6. 9% 23. 6% 34% 68% 5. 3% 27. 3% 19. 8% 30. 3% 50. 1% 9. 2% 5. 4% 14. 7% 39. 1% 36. 4% 75. 5% 14. 7% 5. 8% 20. 5% 43% 31% 74% Est. no J-1 6 -10% 4 -6% 10 -16 47% 34% 81% WV Univ IMG w/J-1
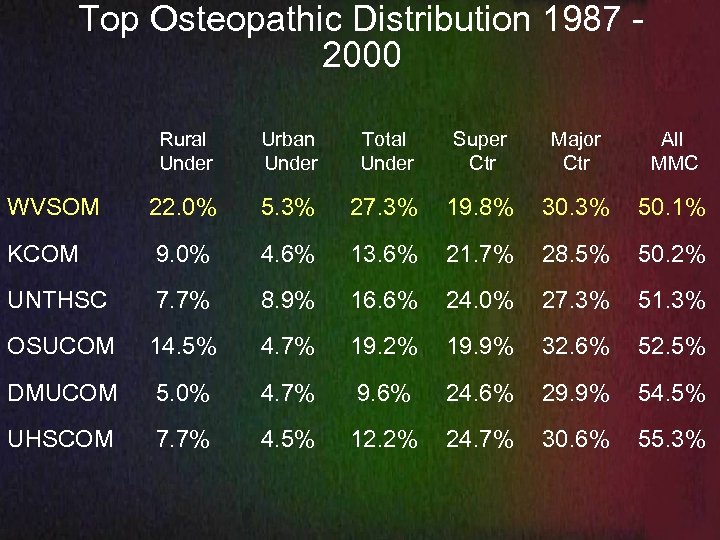
Top Osteopathic Distribution 1987 2000 Rural Under Urban Under Total Under Super Ctr Major Ctr All MMC WVSOM 22. 0% 5. 3% 27. 3% 19. 8% 30. 3% 50. 1% KCOM 9. 0% 4. 6% 13. 6% 21. 7% 28. 5% 50. 2% UNTHSC 7. 7% 8. 9% 16. 6% 24. 0% 27. 3% 51. 3% OSUCOM 14. 5% 4. 7% 19. 2% 19. 9% 32. 6% 52. 5% DMUCOM 5. 0% 4. 7% 9. 6% 24. 6% 29. 9% 54. 5% UHSCOM 7. 7% 4. 5% 12. 2% 24. 7% 30. 6% 55. 3%
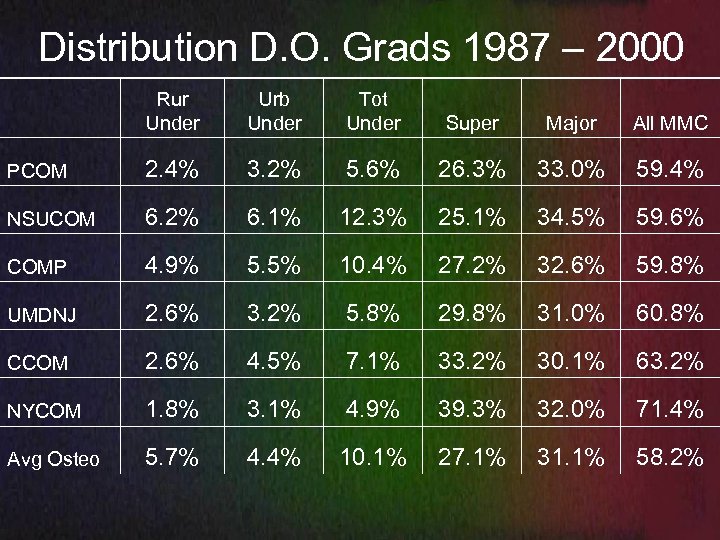
Distribution D. O. Grads 1987 – 2000 Rur Under Urb Under Tot Under Super Major All MMC PCOM 2. 4% 3. 2% 5. 6% 26. 3% 33. 0% 59. 4% NSUCOM 6. 2% 6. 1% 12. 3% 25. 1% 34. 5% 59. 6% COMP 4. 9% 5. 5% 10. 4% 27. 2% 32. 6% 59. 8% UMDNJ 2. 6% 3. 2% 5. 8% 29. 8% 31. 0% 60. 8% CCOM 2. 6% 4. 5% 7. 1% 33. 2% 30. 1% 63. 2% NYCOM 1. 8% 3. 1% 4. 9% 39. 3% 32. 0% 71. 4% Avg Osteo 5. 7% 4. 4% 10. 1% 27. 1% 31. 1% 58. 2%
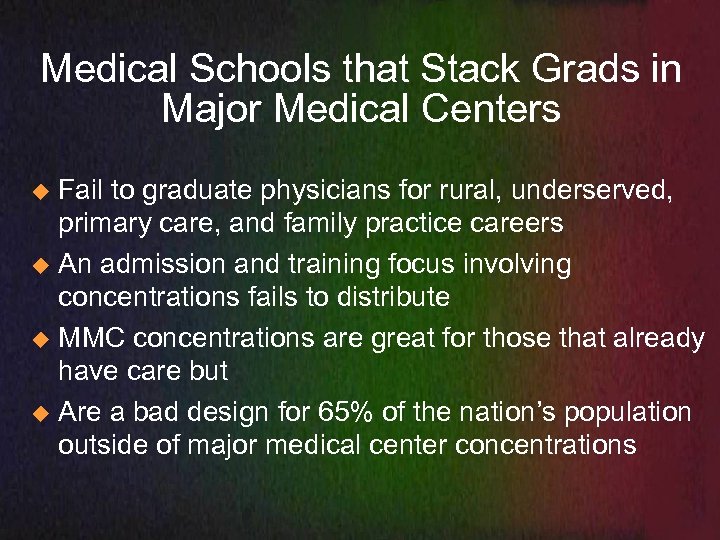
Medical Schools that Stack Grads in Major Medical Centers Fail to graduate physicians for rural, underserved, primary care, and family practice careers u An admission and training focus involving concentrations fails to distribute u MMC concentrations are great for those that already have care but u Are a bad design for 65% of the nation’s population outside of major medical center concentrations u
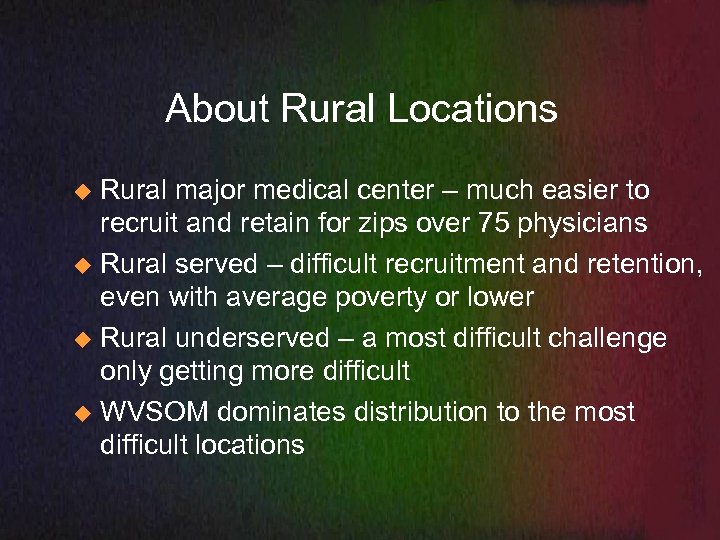
About Rural Locations Rural major medical center – much easier to recruit and retain for zips over 75 physicians u Rural served – difficult recruitment and retention, even with average poverty or lower u Rural underserved – a most difficult challenge only getting more difficult u WVSOM dominates distribution to the most difficult locations u
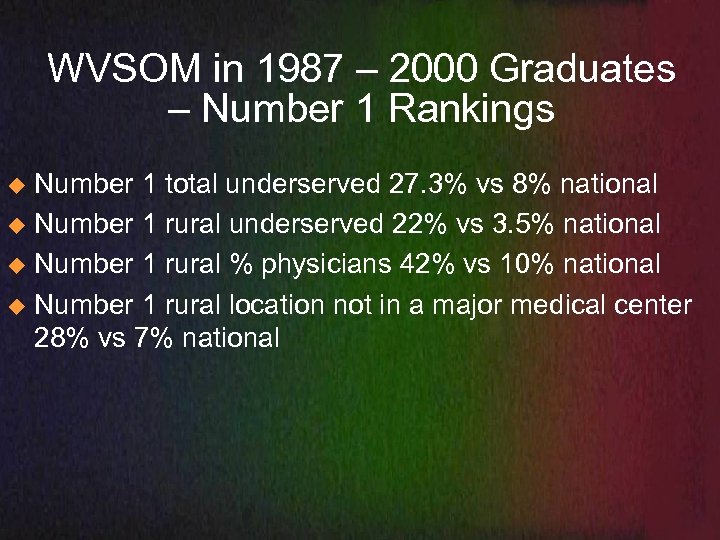
WVSOM in 1987 – 2000 Graduates – Number 1 Rankings Number 1 total underserved 27. 3% vs 8% national u Number 1 rural underserved 22% vs 3. 5% national u Number 1 rural % physicians 42% vs 10% national u Number 1 rural location not in a major medical center 28% vs 7% national u
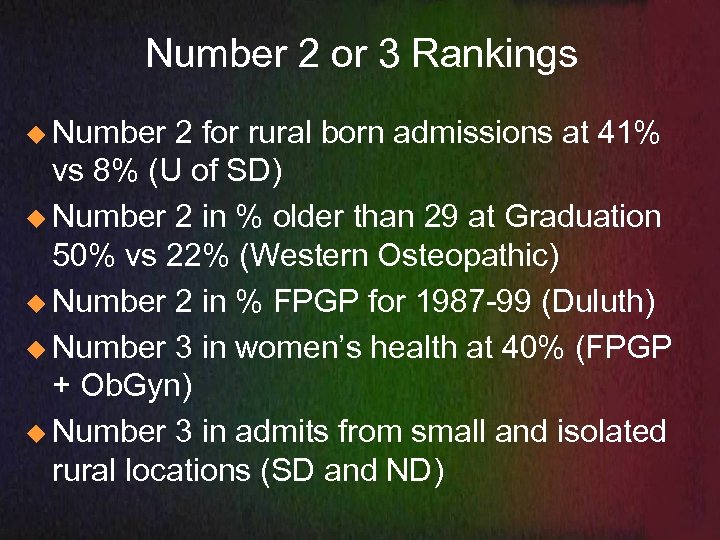
Number 2 or 3 Rankings u Number 2 for rural born admissions at 41% vs 8% (U of SD) u Number 2 in % older than 29 at Graduation 50% vs 22% (Western Osteopathic) u Number 2 in % FPGP for 1987 -99 (Duluth) u Number 3 in women’s health at 40% (FPGP + Ob. Gyn) u Number 3 in admits from small and isolated rural locations (SD and ND)
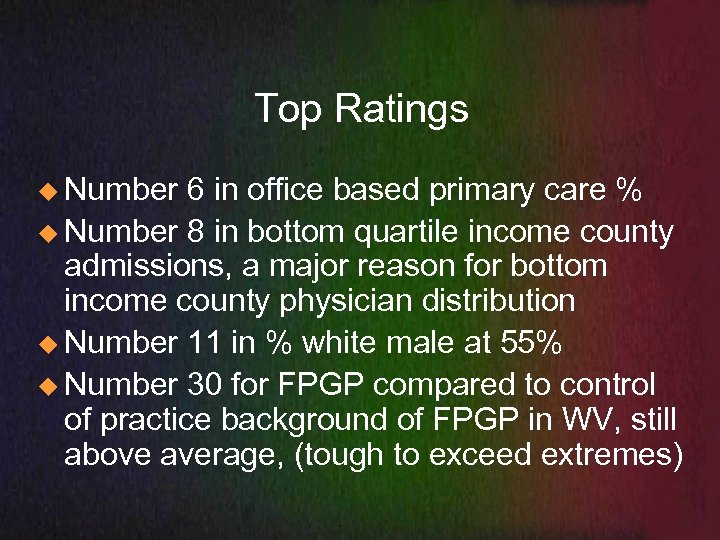
Top Ratings u Number 6 in office based primary care % u Number 8 in bottom quartile income county admissions, a major reason for bottom income county physician distribution u Number 11 in % white male at 55% u Number 30 for FPGP compared to control of practice background of FPGP in WV, still above average, (tough to exceed extremes)
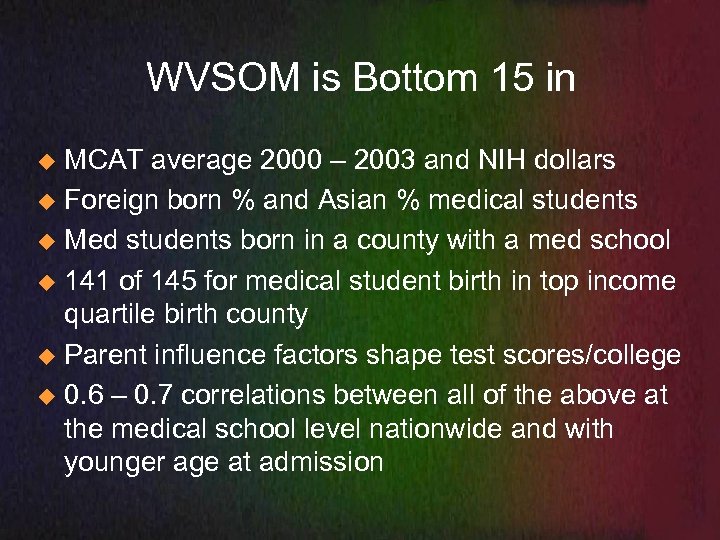
WVSOM is Bottom 15 in MCAT average 2000 – 2003 and NIH dollars u Foreign born % and Asian % medical students u Med students born in a county with a med school u 141 of 145 for medical student birth in top income quartile birth county u Parent influence factors shape test scores/college u 0. 6 – 0. 7 correlations between all of the above at the medical school level nationwide and with younger age at admission u
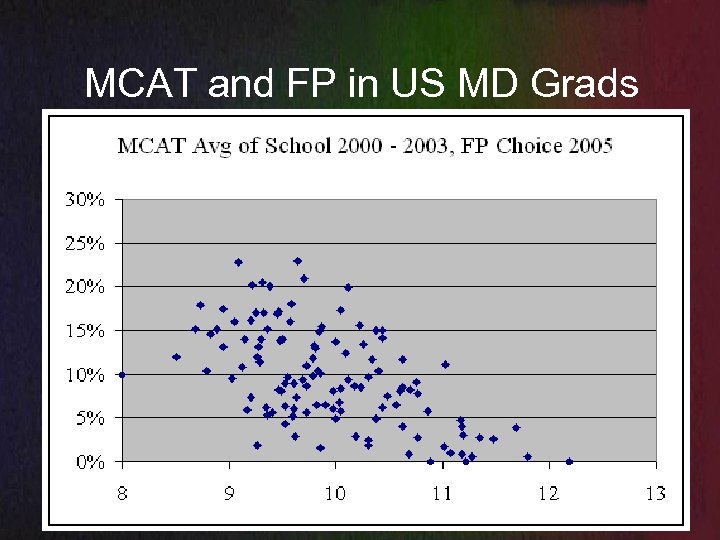
MCAT and FP in US MD Grads
MCAT Not associated with better physicians, a measure of parents u A measure of lower service orientation, lower FP choice, lower distribution, higher boards, greater subspecialty rates u Possibly a measure of less empathy and less satisfaction with a medical career u
MCAT – Good test, but… u u u Speeded test, according to Ellen Julian the test fails without having too many questions to answer, 20 – 40 more minutes and lost discrimination Especially tough on different language and fluency in Spanish perhaps the top factor in urban underserved distribution Barely can compensate for the single minimal change of gender difference forcing changes in number of questions and order of test to compensate for female gender, may work against certain people
Admission Probabilities Blacks and rural born half the probability of admission u Black males and rural males half probability of admission compared to black or rural females u Hispanic at 20% of national average u
Top Admissions - Children of Concentration urban, income, professional parents, medical u All ethnicities and races that share the same characteristics u Asian Indian 10 times, Asian 3 times u Born in a medical school county – 1. 5 – 2 times u All with lowest or lower family practice choice u Major medical center children, not likely to distribute u
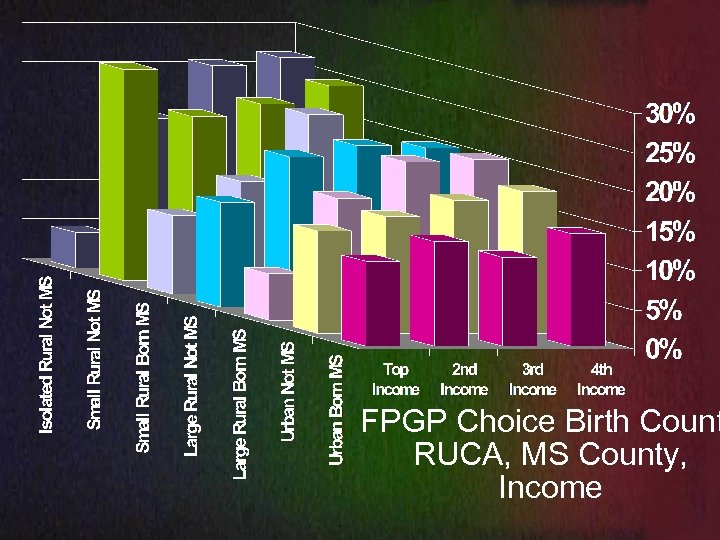
FPGP Choice Birth Count RUCA, MS County, Income
MCAT – Focus Has Been Consistently Exclusion Attrition reduction for 80 years – Mc. Gaghie/JAMA u Sensitive for risk of medical school failure in standard student populations (elite), but not even specific in standard student populations u Sensitivity and specificity fails miserably in populations that vary from the elite who take the test and set the standard for admission, especially in multiple dimensions or in a major area such as language. u
Top Scoring Medical Schools Fewest who are truly representative of the nation u Fewest rural or “diverse” and even these are often children of professionals u Admit Children of Concentration u Environments - Hundreds of physicians at a site with only 4% family physicians and 20% primary care, lowest in the nation u
Translation WVSOM admits students who reflect the population of the United States and West Virginia and graduates those most needed by the state and the United States u Schools that concentrate children of higher status parents admit children who are least representative u Mismatches result in poor distribution, poor quality, higher costs, less empathy, less service orientation, and other problem areas u
Differences Distributional schools have admissions, training, and graduate distributions that closely reflect the population of the United States in multiple dimensions u Concentrational schools admit the most concentrated, train in concentrations, and concentrate graduates, these all represent the most different medical students, training locations, and graduate locations compared to the population of the United States u
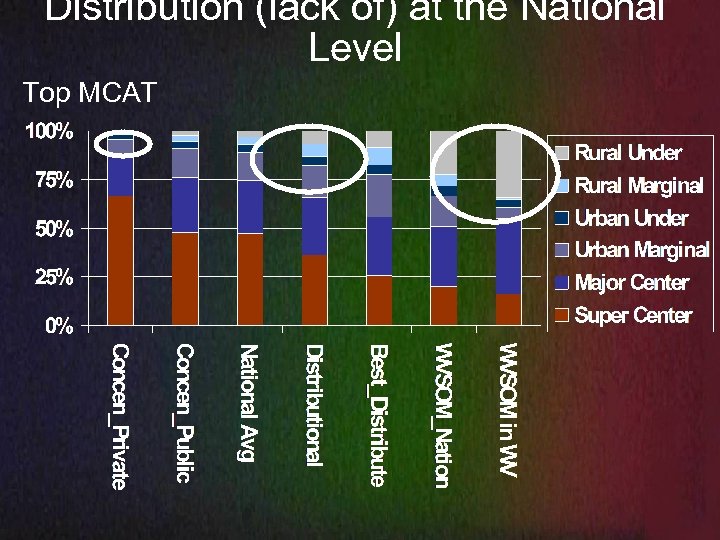
Distribution (lack of) at the National Level Top MCAT
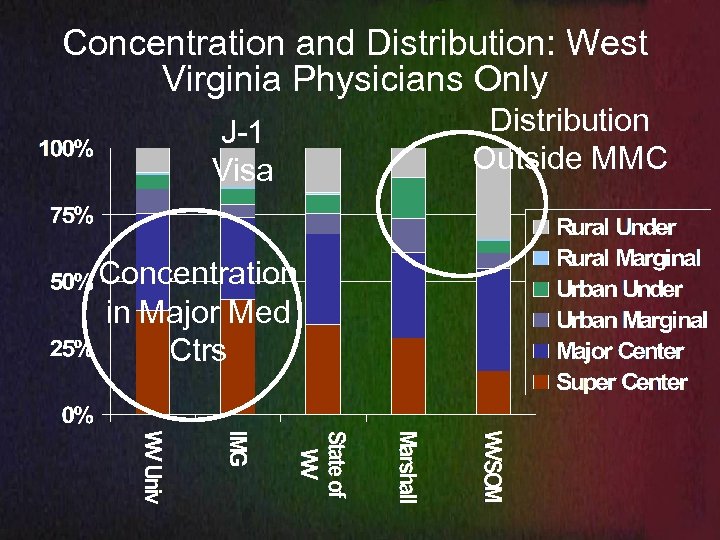
Concentration and Distribution: West Virginia Physicians Only J-1 Visa Concentration in Major Med Ctrs Distribution Outside MMC
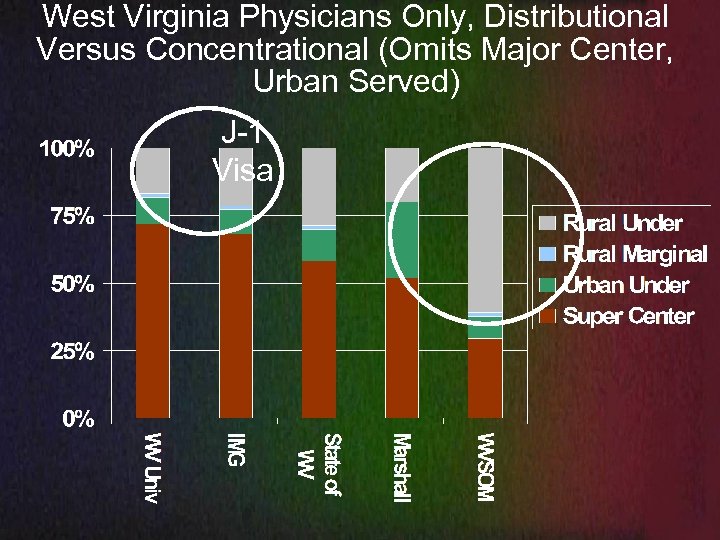
West Virginia Physicians Only, Distributional Versus Concentrational (Omits Major Center, Urban Served) J-1 Visa
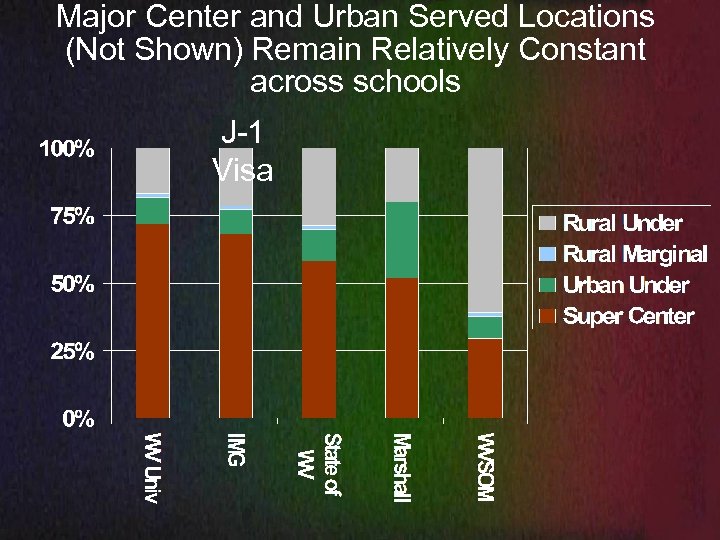
Major Center and Urban Served Locations (Not Shown) Remain Relatively Constant across schools J-1 Visa
WVSOM Took a Risk u Mission u Admissions u Rural Training u Remaining dedicated to medical education
The State of WV Made an Investment
There Was Outstanding Success u Poorly appreciated by a distorted sense of values in America
But Can WVSOM Resist The National Changes? Record low levels of FP choice in MD and DO grads u Down to 8% rural born admissions u Highest status replacing middle and lower income status in admission u Least distributional replacing the most distributional u
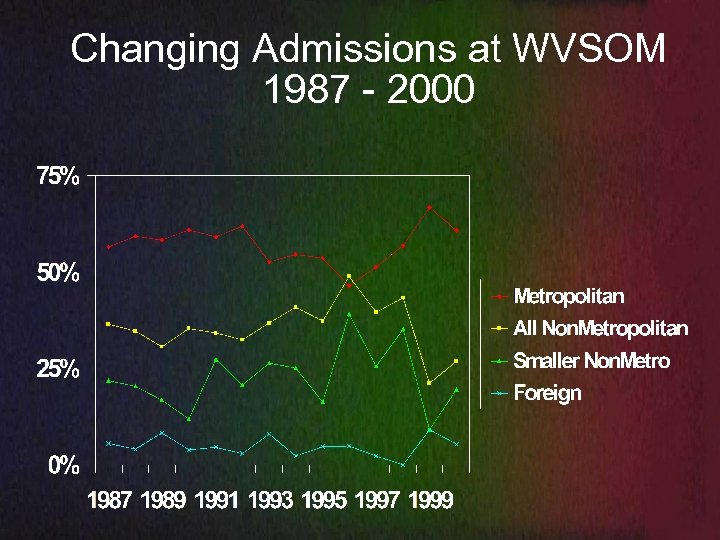
Changing Admissions at WVSOM 1987 - 2000
Admissions Can Change, Leadership Can Change
Why the WVSOM Mission Is More Important Because the nation is admitting and training fewer who will serve in the most needed careers and locations u Because the national health policies fail, leaving only admission and training to carry the incredibly difficult burden of fighting health policy u Because policy is melting away primary care in all forms u
Sadly WVSOM might look better, because the nation’s medical schools are worse
Changes in Primary Care Declines in All Forms % remaining in PC
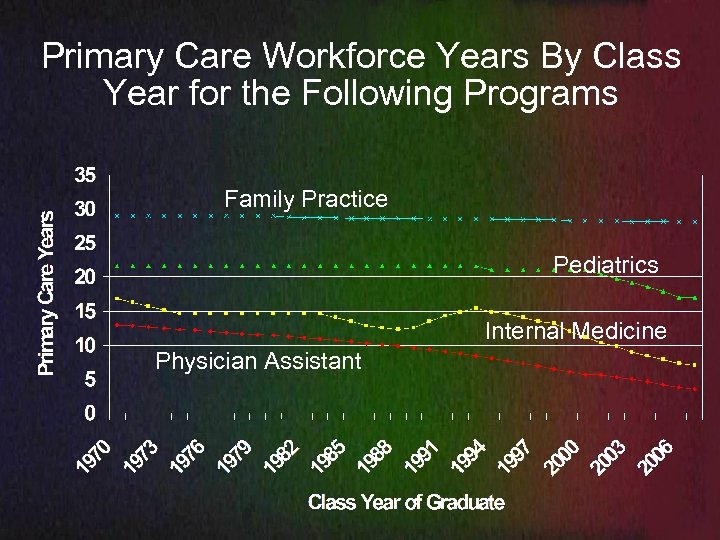
Primary Care Workforce Years By Class Year for the Following Programs Family Practice Pediatrics Internal Medicine Physician Assistant
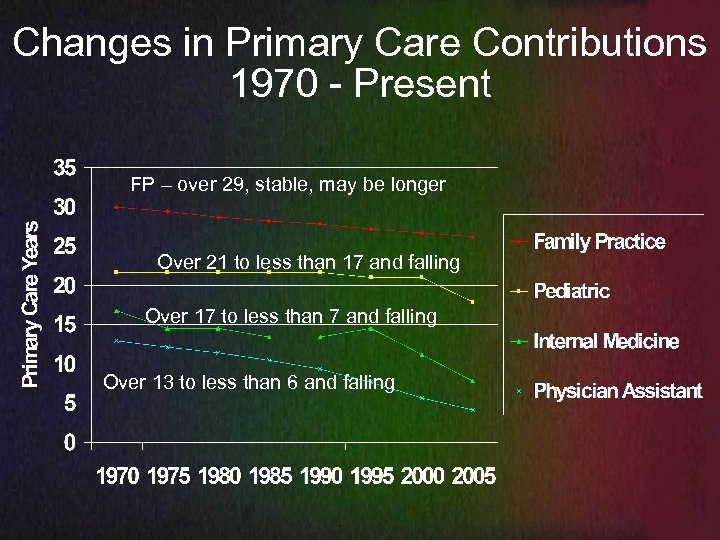
Changes in Primary Care Contributions 1970 - Present FP – over 29, stable, may be longer Over 21 to less than 17 and falling Over 17 to less than 7 and falling Over 13 to less than 6 and falling
Family Practice Will Soon Be the Only Majority Primary Care Source Pediatrics reduced 40% u Internal medicine cut in half u Nurse practitioners down to less than 40% in primary care u Physician assistants down to less than 35% in primary care u FP impacted at the only possible point for a permanent primary care source – before the choice is made, once committed, 30 yrs of primary care on average u
PC Bad News – Share is declining in all others Really bad news u FP from US MD and DO grads at record lows u NP and PA and IM and PD at record low in retention at graduation u NP and PA at record low primary care after graduation and decreasing yearly u Hospitalist, urgent, emergent, locums actively tapping in to primary care pool u
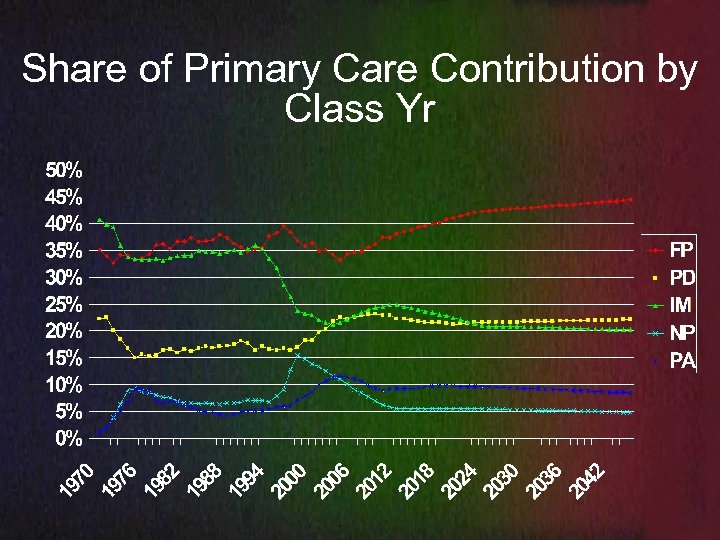
Share of Primary Care Contribution by Class Yr
If You Allow Market Forces Shaping of Education, Higher Education, and Medical Education to Reign u You get concentrations of physicians in major medical center careers and locations u You get medical students that are easy to teach, but they may never learn the most important parts of medicine u You get medical training separate from life and health experience, dis-
If You Allow Market Forces Education, Market Forces Higher Education, and Market Forces Medical Education to Reign You get medical students that may or may not deal with adversity well, as they have rarely been tested u You get physicians who share little in common with their patients or with the nurses and staff actually delivering the health care u You concentrate cost, quality, and access problems u
Concentrational Medical Schools Access the most lines of funding and the highest levels of funding in each line u Help create shortages and then want special funding u Fail to admit/train those that would be rural specialists u Help create shortages in women’s health u Desire special funding to deliver geriatrics in places with the fewest elderly and with the fewest physicians delivering primary care to the elderly u
If You Work Hard to Admit and Train u For family practice and rural – you will get rural and underserved and primary care and the most lasting policy resistant form of primary care - FP u Plus women’s health u Plus mental health u Plus geriatrics….
If You Work Hard to Admit and Train u For primary care – you get urban underserved and primary care, u Except more and more IM and PD residency grads are specializing now with lower and lower primary care, rural, and underserved yield u Except only half of IMGs remain in the US in active practice and J-1 declining
Those who distribute – Masterfile, all class years, all types of US Medical Schools Those born outside of concentrations u Basically lower and middle income people and children not from professionals and physicians u Rural born a bonus, but mainly not “children of concentration” u Older - barriers of education, income, parents u Scores that reflect most needed origins, backgrounds, distributions u Family physicians – 2 X – 4 X greater distribution u
The schools that aim for distributional status u Will accomplish health access goals, u Will also distribute rural specialists, u Will address women’s health, u Will deliver the most geriatric care u Without costly special programs!!!
Distributional Focus or Just Another Part of the Problem
Additional Notes and Slides for Small Group Discussion
Physician Distribution by Concentration New PDC Coding u Physicians concentrate not by geography but by concentrations of physicians u Integrates concentrations, income, poverty, RUCA coding u
PDC Coding – Inside and Outside Inside major medical centers – zip codes with 75 or more physicians – about 75% of physicians u Outside – all other locations u Urban served and underserved u Rural served and underserved u Underserved is 19% poverty or more or a zip code with a CHC, NHSC, whole county u Served – not MMC, not underserved u
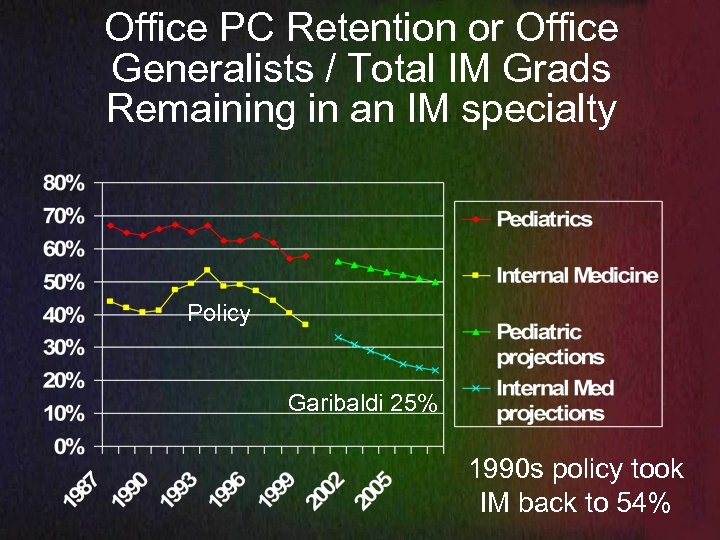
Office PC Retention or Office Generalists / Total IM Grads Remaining in an IM specialty Policy Garibaldi 25% 1990 s policy took IM back to 54%
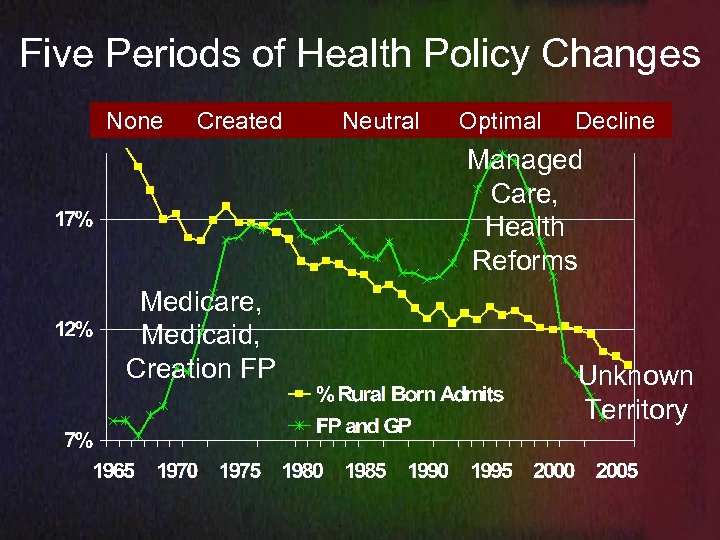
Five Periods of Health Policy Changes None Created Neutral Optimal Decline Managed Care, Health Reforms Medicare, Medicaid, Creation FP Unknown Territory
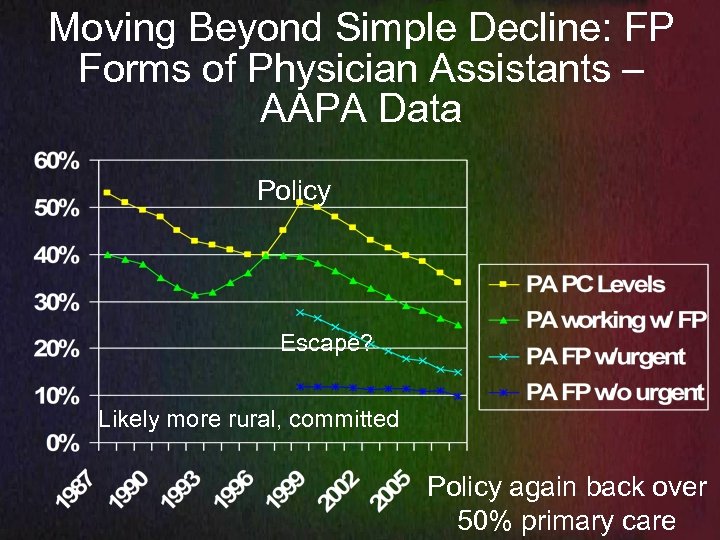
Moving Beyond Simple Decline: FP Forms of Physician Assistants – AAPA Data Policy Escape? Likely more rural, committed Policy again back over 50% primary care
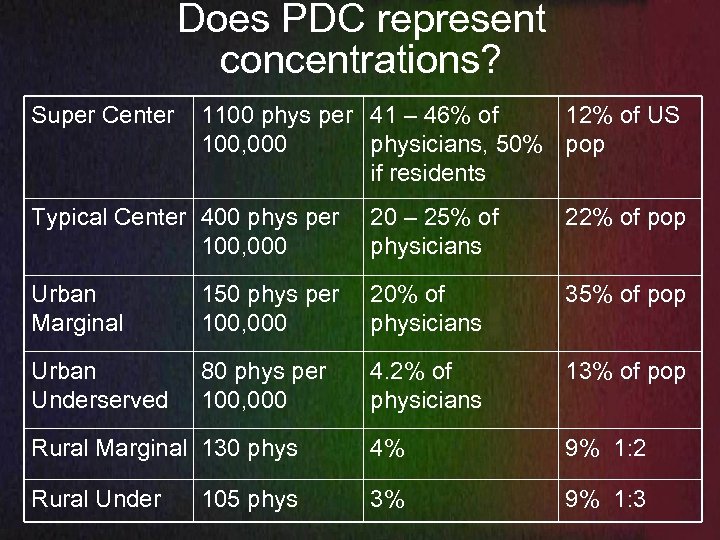
Does PDC represent concentrations? Super Center 1100 phys per 41 – 46% of 12% of US 100, 000 physicians, 50% pop if residents Typical Center 400 phys per 100, 000 20 – 25% of physicians 22% of pop Urban Marginal 150 phys per 100, 000 20% of physicians 35% of pop Urban Underserved 80 phys per 100, 000 4. 2% of physicians 13% of pop Rural Marginal 130 phys 4% 9% 1: 2 Rural Under 3% 9% 1: 3 105 phys
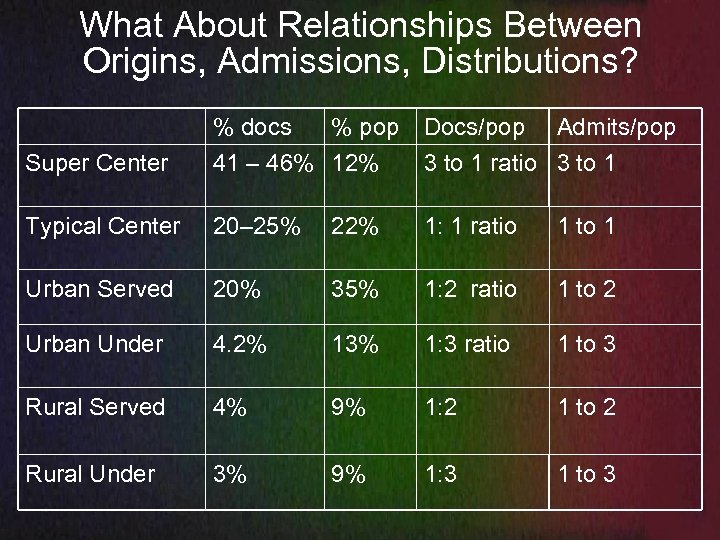
What About Relationships Between Origins, Admissions, Distributions? % docs % pop Docs/pop Admits/pop Super Center 41 – 46% 12% 3 to 1 ratio 3 to 1 Typical Center 20– 25% 22% 1: 1 ratio 1 to 1 Urban Served 20% 35% 1: 2 ratio 1 to 2 Urban Under 4. 2% 13% 1: 3 ratio 1 to 3 Rural Served 4% 9% 1: 2 1 to 2 Rural Under 3% 9% 1: 3 1 to 3
Similar Ratios: Current policies, practices, market forces Shape birth to admission education and opportunity: who gets admitted u Shape training: focus, distractions from teaching, few teachers, passive med ed u Shape health policy: who is hired u Shape physician distribution: who can be supported especially outside of major centers u
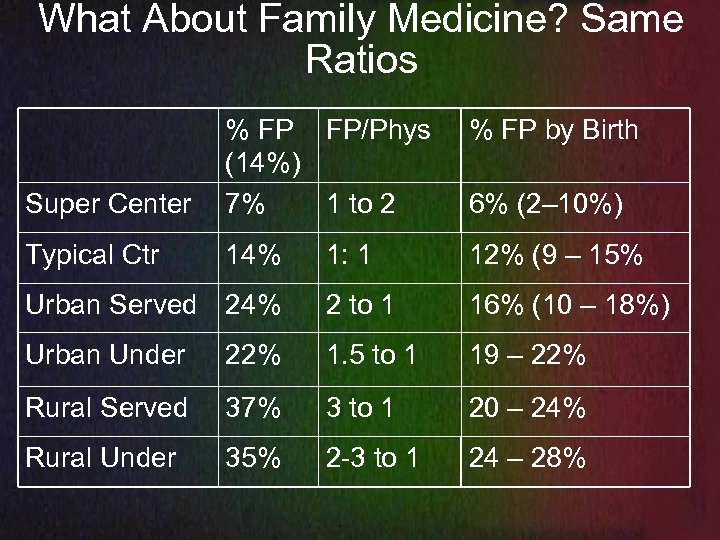
What About Family Medicine? Same Ratios % FP by Birth Super Center % FP FP/Phys (14%) 7% 1 to 2 Typical Ctr 14% 1: 1 12% (9 – 15% Urban Served 24% 2 to 1 16% (10 – 18%) Urban Under 22% 1. 5 to 1 19 – 22% Rural Served 37% 3 to 1 20 – 24% Rural Under 35% 2 -3 to 1 24 – 28% 6% (2– 10%)
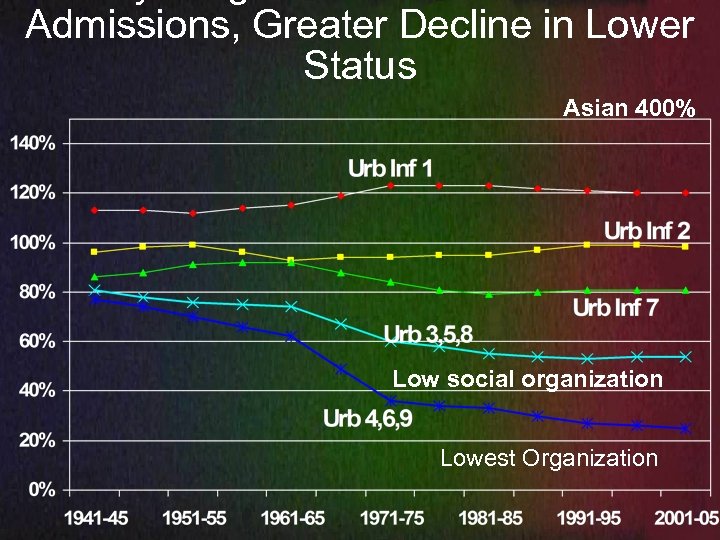
Admissions, Greater Decline in Lower Status Asian 400% Low social organization Lowest Organization
Reflection Points - What happens When a medical school maintains admissions patterns? u When a state does not allow lower and middle income and rural areas to deteriorate in education and college preparation u With the GI bill, 60 s and 70 s education efforts, or broader admissions (1990 s) u
Admission Ratios Compare the particularly birth origin group as a percentage of the US medical students u To the percentage of that group in the US population u 22% of medical students Asian divided by 4% of the US population Asian is 5. 5 times or 550%, 91% for White, 50% for African American or Rural Born u Changes over the decades compared u
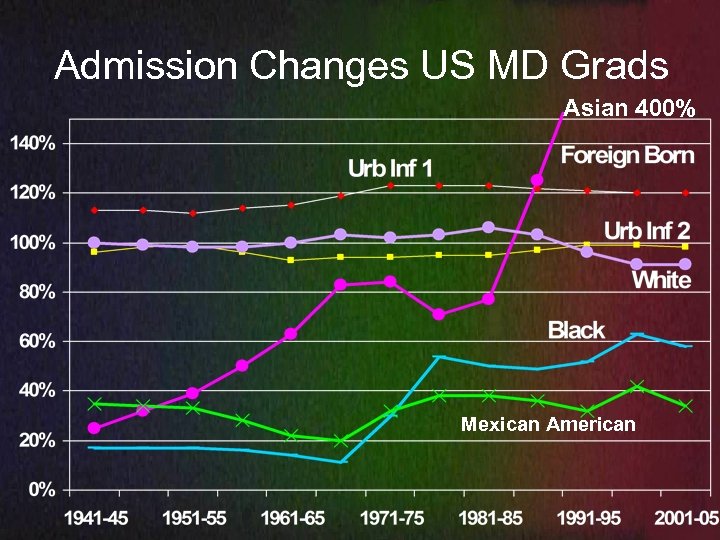
Admission Changes US MD Grads Asian 400% Mexican American
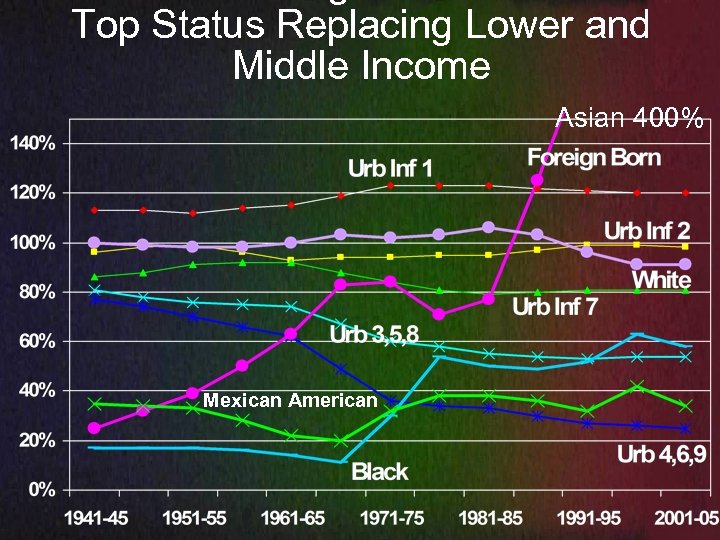
Top Status Replacing Lower and Middle Income Asian 400% Mexican American
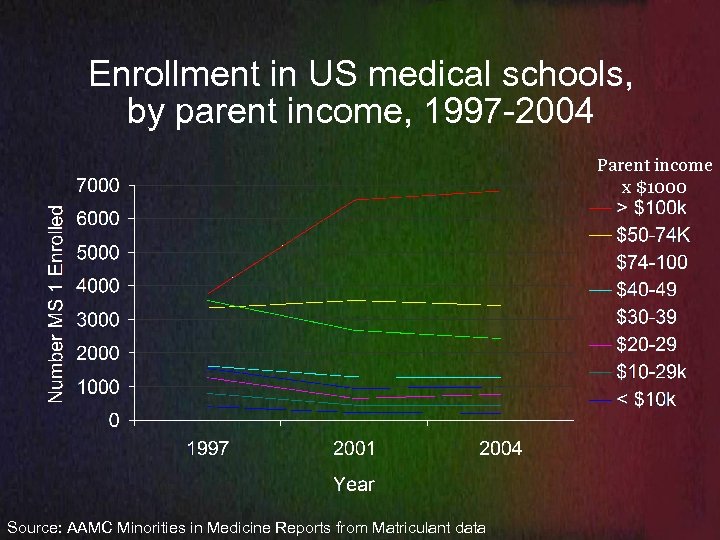
Enrollment in US medical schools, by parent income, 1997 -2004 Parent income x $1000 Source: AAMC Minorities in Medicine Reports from Matriculant data
Admission Impacts: Children of Concentration 1. 5 to 10 times Probability of admission 65% from the top 20% status, children of concentration, children of professions, top education, private schools, top ranking schools u Strength – organization, scores, academics u Weakness – lack of awareness, true integration and understanding, of those who are different and those who suffer, lack empathy u Exceptions – The rich can also suffer u
Admission Impacts: Children of Distribution 0. 2 – 0. 5 the probability of admission u u Not children of professionals, older, average scores, late bloomers, increasing trajectory as they “catch up” to those with birth and parent advantages Strength – people skills and orientation, service orientation, life experiences, have overcome obstacles, have dealt with uncertainty and unknown often without support Weaknesses – lack of organization, personal barriers Exceptions – Not all who appear to be children of distribution, are
Characteristics of Schools/Physicians Over 80% Found in Major Medical Centers Most urban born from highest income counties or Asian or foreign born who were raised in the same locations and have the same parents u Top MCAT medical schools u Lowest FP choice – less than 2% for Asian Indian u Lowest PC contribution u Fewest rural born, lower income, middle income u Born in highest income counties with med schools u Top probability of admission, lowest probability of distribution, FP, primary care u
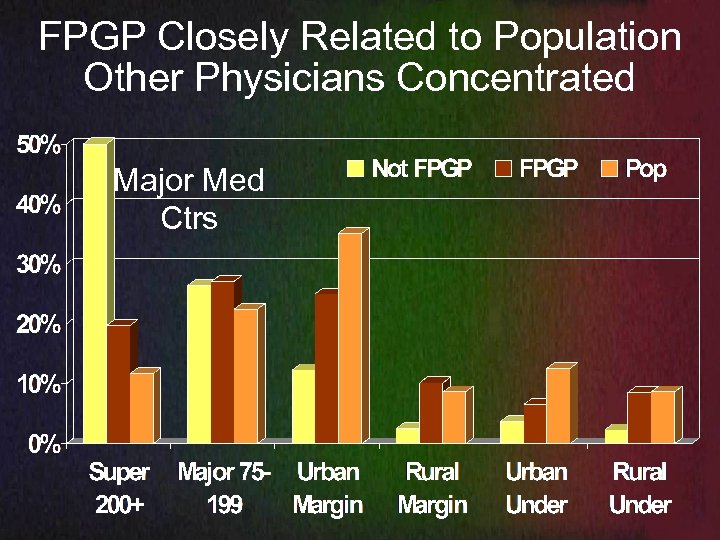
FPGP Closely Related to Population Other Physicians Concentrated Major Med Ctrs
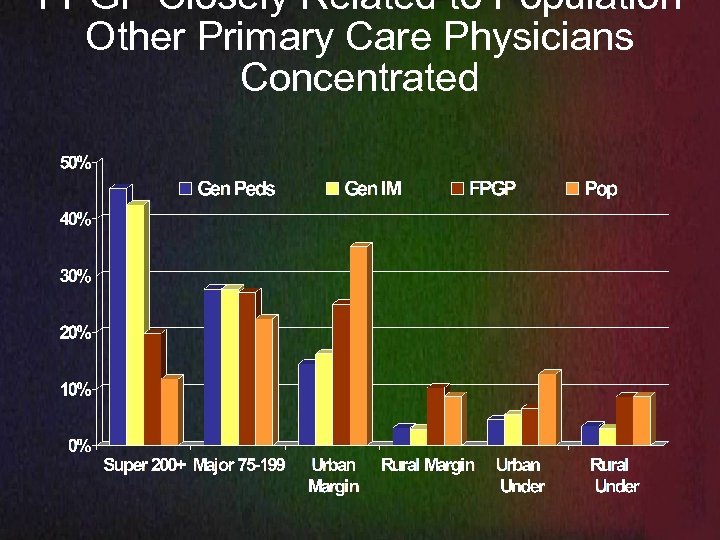
FPGP Closely Related to Population Other Primary Care Physicians Concentrated
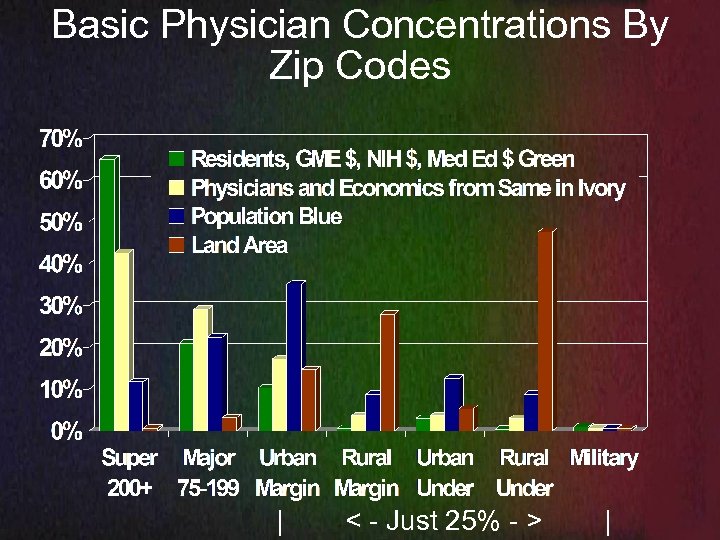
Basic Physician Concentrations By Zip Codes | < - Just 25% - > |
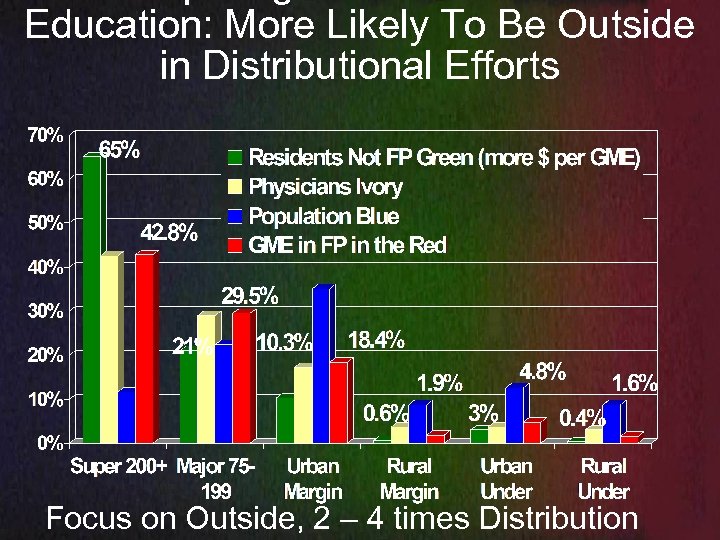
Education: More Likely To Be Outside in Distributional Efforts Focus on Outside, 2 – 4 times Distribution
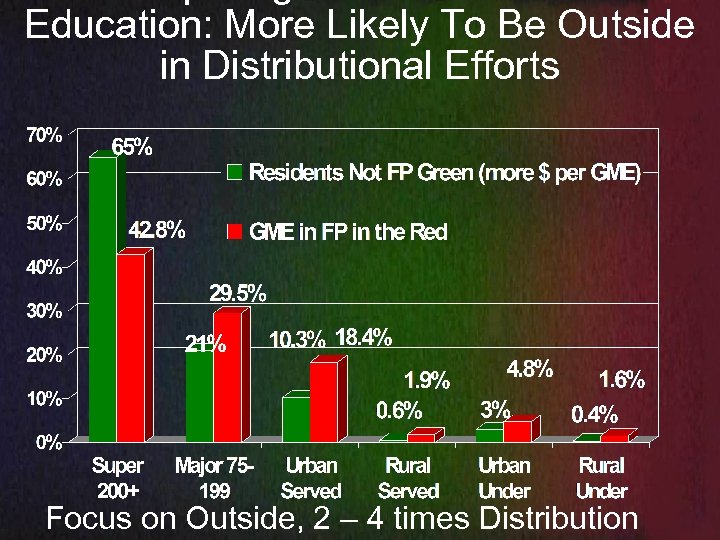
Education: More Likely To Be Outside in Distributional Efforts Focus on Outside, 2 – 4 times Distribution
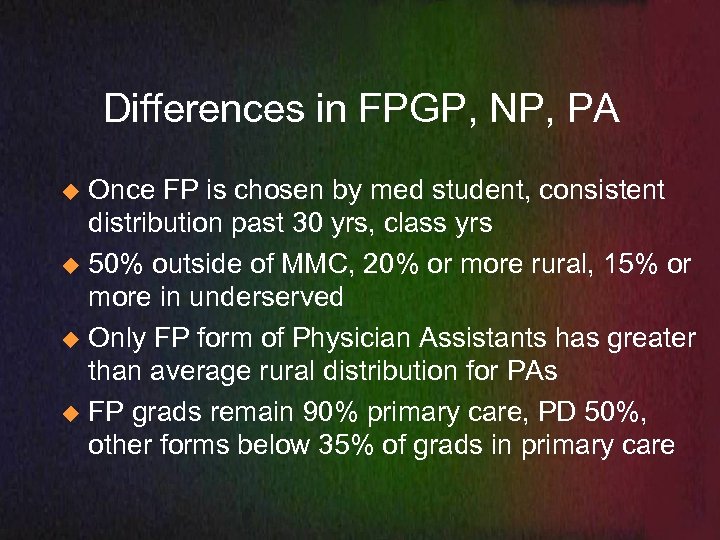
Differences in FPGP, NP, PA Once FP is chosen by med student, consistent distribution past 30 yrs, class yrs u 50% outside of MMC, 20% or more rural, 15% or more in underserved u Only FP form of Physician Assistants has greater than average rural distribution for PAs u FP grads remain 90% primary care, PD 50%, other forms below 35% of grads in primary care u
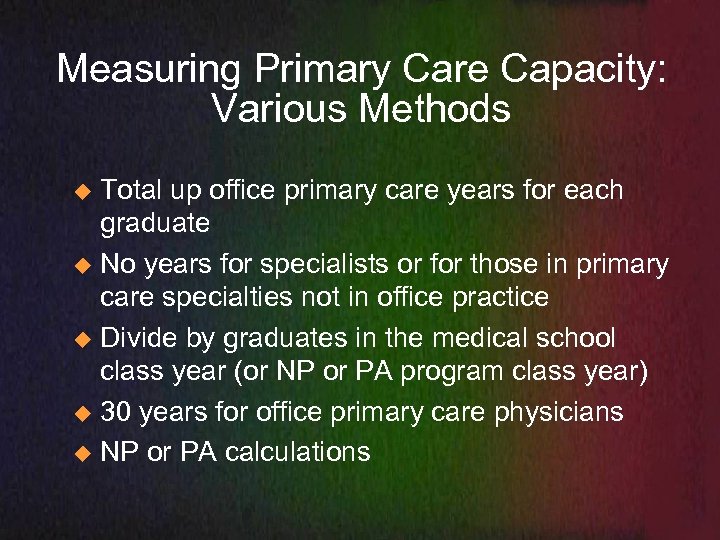
Measuring Primary Care Capacity: Various Methods Total up office primary care years for each graduate u No years for specialists or for those in primary care specialties not in office practice u Divide by graduates in the medical school class year (or NP or PA program class year) u 30 years for office primary care physicians u NP or PA calculations u

Primary Care Workforce Yrs: Association data, Masterfile, Garibaldi, Goolsby, HRSA Grad NP PA FP IM PD % PC 0. 35 0. 33 0. 9 0. 25 0. 55 Career 24 yr 35 yr Activity 0. 70 0. 8 0. 93 Volume 0. 5 0. 75 1 0. 86 0. 95 PC yrs 2. 94 6. 93 29. 30 7. 00 17. 01 Rural PC Yrs 0. 59 1. 39 5. 86 0. 62 1. 39 Underserved PC 0. 44 1. 04 4. 40 0. 57 1. 45
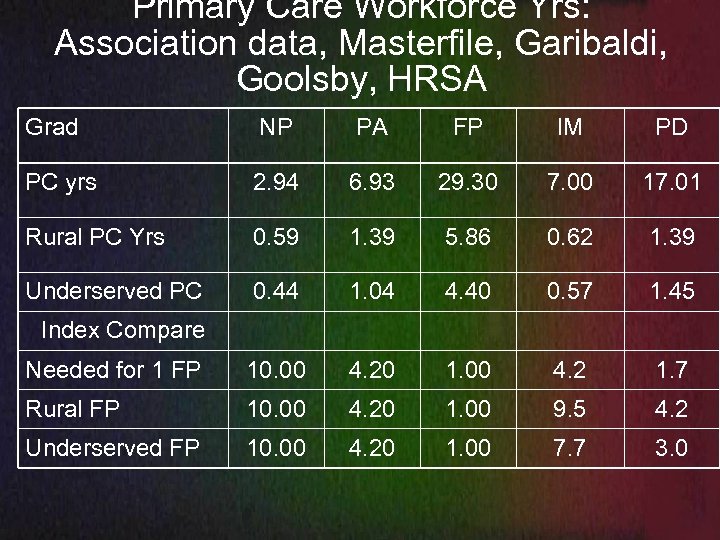
Primary Care Workforce Yrs: Association data, Masterfile, Garibaldi, Goolsby, HRSA Grad NP PA FP IM PD PC yrs 2. 94 6. 93 29. 30 7. 00 17. 01 Rural PC Yrs 0. 59 1. 39 5. 86 0. 62 1. 39 Underserved PC 0. 44 1. 04 4. 40 0. 57 1. 45 Needed for 1 FP 10. 00 4. 20 1. 00 4. 2 1. 7 Rural FP 10. 00 4. 20 1. 00 9. 5 4. 2 Underserved FP 10. 00 4. 20 1. 00 7. 7 3. 0 Index Compare
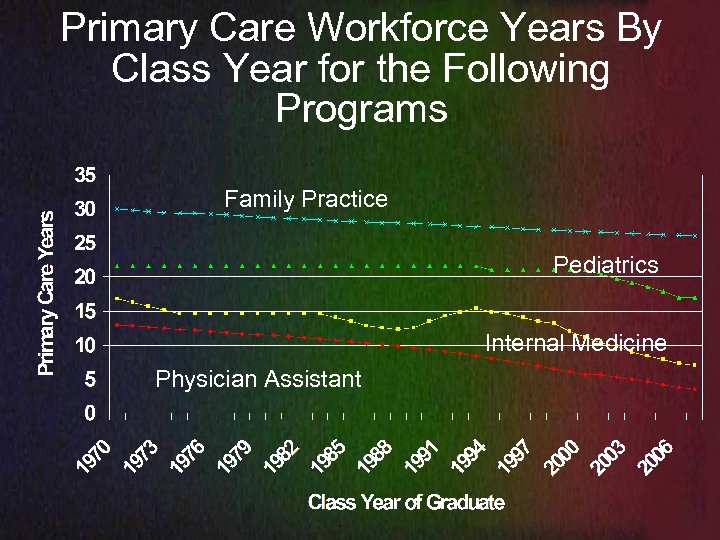
Primary Care Workforce Years By Class Year for the Following Programs Family Practice Pediatrics Internal Medicine Physician Assistant
Primary Care Workforce Year Changes Same contributions from family physicians u Internal medicine residents cut in half and still falling, interrupted only by policy change u Pediatrics down 30% u Takes 3 – 4 PAs to provide the same primary care u NP contributions down to 3 – 5 years per graduate – 65% lost to specialization, 25% inactive, half the PC volume of an FP, 15% in administration, multiple locations, poor utilization u
Family Practice and Urban Underserved for 1987 – 2000 medical school grads all sources National average – 4% physicians urban underserved u Top ranking MCAT schools 2% - 3% u IM or PD US MD grad – 3% u FP grads – 6 – 9% u Top school UAG Guadalajara number 1 in urban underserved at 22% and number 2 in total underserved with not a small contribution of 85 total physicians a year to the US u
Above Average Urban Underserved Osteo IM, PD, Ob-Gyn at 4 – 5%, FP 5. 6% u International grad IM or PD – 6% - J-1 driven u Asian or foreign born FP – 7% u All FP – 8% u Urban Underserved US pop - 12. 6% u Black or Hispanic FP – 16 - 22% u Inner city FP training (often CHC) – 15 - 25% u UAG Guadalajara – 22% for all grads in US u
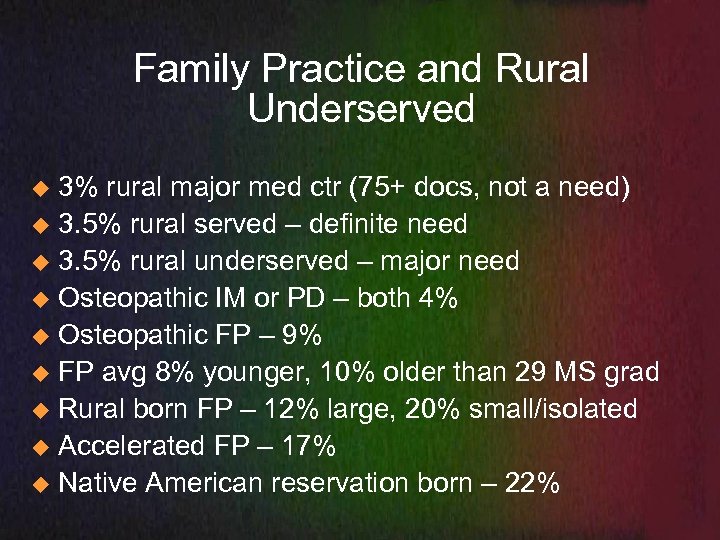
Family Practice and Rural Underserved 3% rural major med ctr (75+ docs, not a need) u 3. 5% rural served – definite need u 3. 5% rural underserved – major need u Osteopathic IM or PD – both 4% u Osteopathic FP – 9% u FP avg 8% younger, 10% older than 29 MS grad u Rural born FP – 12% large, 20% small/isolated u Accelerated FP – 17% u Native American reservation born – 22% u
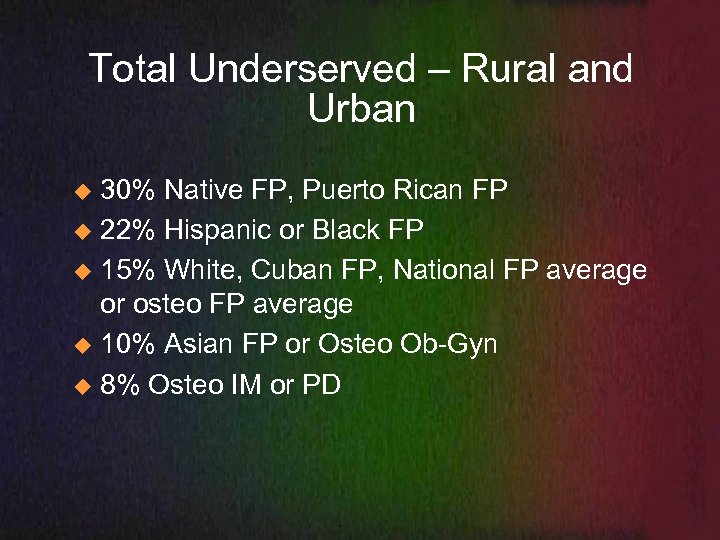
Total Underserved – Rural and Urban 30% Native FP, Puerto Rican FP u 22% Hispanic or Black FP u 15% White, Cuban FP, National FP average or osteo FP average u 10% Asian FP or Osteo Ob-Gyn u 8% Osteo IM or PD u
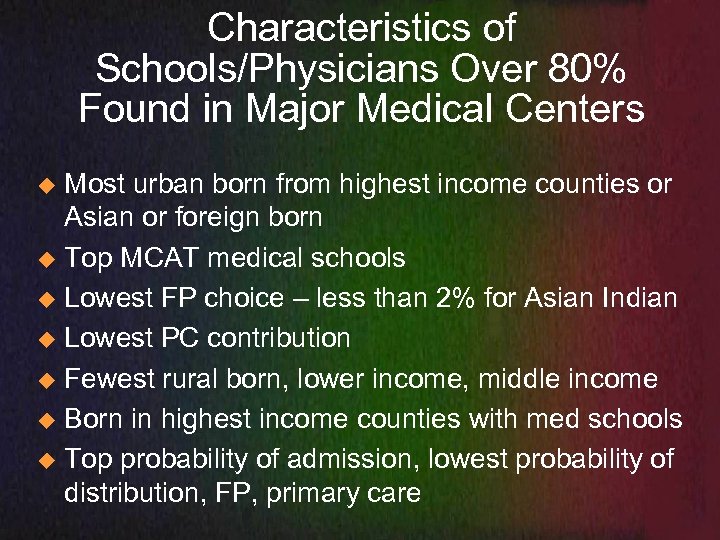
Characteristics of Schools/Physicians Over 80% Found in Major Medical Centers Most urban born from highest income counties or Asian or foreign born u Top MCAT medical schools u Lowest FP choice – less than 2% for Asian Indian u Lowest PC contribution u Fewest rural born, lower income, middle income u Born in highest income counties with med schools u Top probability of admission, lowest probability of distribution, FP, primary care u
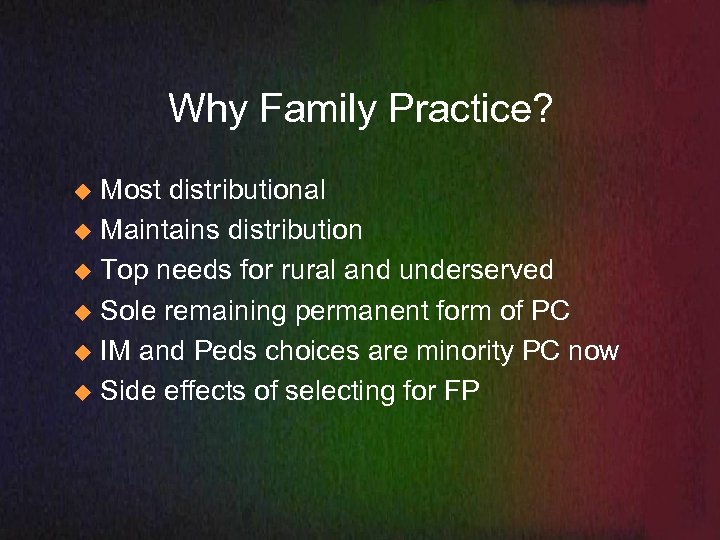
Why Family Practice? Most distributional u Maintains distribution u Top needs for rural and underserved u Sole remaining permanent form of PC u IM and Peds choices are minority PC now u Side effects of selecting for FP u
Side Effects of Selecting for FP Older – more psychiatrists, office primary care, rural, underserved, plus FP increase u Lower and middle income – PC, rural, underserved, women’s health u Lower scoring – same as above u Rural born – same as above u Born outside medical school county (proxy for parents not professionals - same u
Family Practice – 1997 – 2003 Residency Grads 98% still in FP, no decrease for earlier grads u 90% primary care, 2 – 4% each in teaching, military, research, administration, hospital u
Family Practice 53% outside major med ctrs, 60% osteo FP u 2 – 4 times more likely to be found outside u Specialties not family physicians are 3 times more likely to be found inside u Office IM and Office Peds – 70% inside, higher if considering all generalists, higher for hospital based and subspecialties u
Multiplier effects, controlling for origins and training sites FP Doubles urban underserved u FP Triples rural, all location types u FP Quadruples rural underserved, isolated rural, whole county PC shortage, CHC location, rural CHC location even higher u
Compromise on Mission, FP emphasis Graduates leave the state u Graduates do not address primary care needs u Graduates do not address rural and rural underserved needs u Graduates do IM or Peds and most specialize u
Procedural Focus in FP, Urban and Rural Women’s health, ultrasound, deliveries, colpo, scopes, minor surgery u Ventura, Tacoma, Wichita KS, Ramona/Bartlesville u Waco, Corpus Christi, John Peter Smith, Lisa Nash DO Galveston, u Scottsbluff, NE CHC, Pete Johnson, DO neuro u North Platte, and Lincoln NE, Shreveport, Nashville, Mad River Ohio, Western MA, Maine FP, u Rural FP sites in NM, WY, MT, ID, WI, NC, SC u
100 Osteopathic Family Physicians 2900 primary care workforce years u 1800 PC years outside of major centers u 500 - 600 underserved PC years u
Why Family Medicine: the CHC Component Rosenblatt, Hart in JAMA u Family physicians were 50% of CHC docs u Number 2 only to RNs u More than all other physician specialties combined and 61% in rural CHC u 4 – 5 times odds ratios compared to others u
Why FM: Poverty/Shortage Areas Family physicians are 1. 8 times more likely to be found in urban underserved zip codes u FPs are 3. 5 times more likely to be found in rural served, rural underserved locations u Underserved locations have 19% poverty or a CHC, NHSC site, whole county u FPs dominate whole county shortage and isolated locations with 4 times odds ratios u
Family Physicians and Major Medical Centers Are Oil and Water – Why they seek their own place FPs are only 47% located in zips of 75 or more physicians, only 40% for osteopathic FP u 60% of osteopathic FPs are found in the places most needed with 65% of the population. u Only 10 – 25% of specialty physicians are outside of major medical centers to serve 65% of the population in 96% of the land area u
Why Family Medicine Summary Most resistant to current health policy moving all other PC forms away from primary care, rural, CHC, distribution outside MMC u Optimal training - full scope family medicine u FM training – more likely to be outside MMC u FM docs 2 – 4 times more likely outside u Health policy drives family physicians where we want physicians, others less able to adapt u
df116ec3b7b1097a58f6f2c58298baf7.ppt