0e2adfefc55a2774e604aa5bb175ddbc.ppt
- Количество слайдов: 35
 Avoiding diarrhea: epidemiology and prevention Patrick Keller Aye Otubu Alex Doyal Adam Froyum Roise 26 April 2007
Avoiding diarrhea: epidemiology and prevention Patrick Keller Aye Otubu Alex Doyal Adam Froyum Roise 26 April 2007
 Outline Ø Developing world: Cholera Ø Cruise ships: Norovirus Ø Hiking: Giardia and Cryptosporidium Ø Friends: Shigella
Outline Ø Developing world: Cholera Ø Cruise ships: Norovirus Ø Hiking: Giardia and Cryptosporidium Ø Friends: Shigella
 Cholera An acute diarrheal illness caused by bacterium vibrio cholerae The most severe diarrheal disease
Cholera An acute diarrheal illness caused by bacterium vibrio cholerae The most severe diarrheal disease
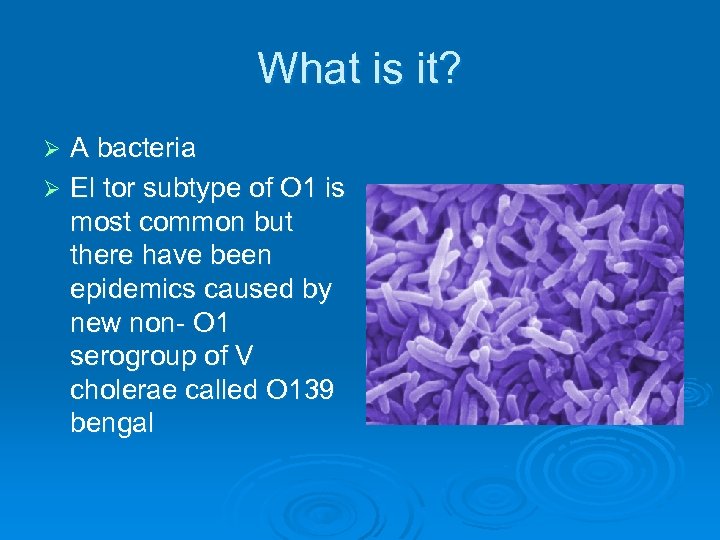 What is it? A bacteria Ø El tor subtype of O 1 is most common but there have been epidemics caused by new non- O 1 serogroup of V cholerae called O 139 bengal Ø
What is it? A bacteria Ø El tor subtype of O 1 is most common but there have been epidemics caused by new non- O 1 serogroup of V cholerae called O 139 bengal Ø
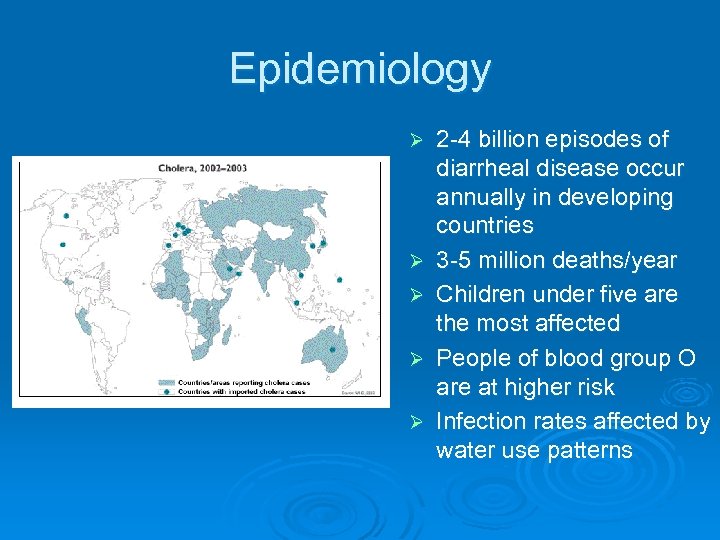 Epidemiology Ø Ø Ø 2 -4 billion episodes of diarrheal disease occur annually in developing countries 3 -5 million deaths/year Children under five are the most affected People of blood group O are at higher risk Infection rates affected by water use patterns
Epidemiology Ø Ø Ø 2 -4 billion episodes of diarrheal disease occur annually in developing countries 3 -5 million deaths/year Children under five are the most affected People of blood group O are at higher risk Infection rates affected by water use patterns
 How do you get it? Ø Ø Ø Classically a water borne disease causing bacteria. Eating or drinking contaminated food or water containing vibrio cholerae bacteria Contaminated food and not water a more likely source in developed countries. Sensitive to climate and grows rapidly in warmer environmental temps. Humans are the main reservoir. Shell fish and plankton are the only animal reservoirs. The natural habitat is believed to be the Ganges in Bangladesh
How do you get it? Ø Ø Ø Classically a water borne disease causing bacteria. Eating or drinking contaminated food or water containing vibrio cholerae bacteria Contaminated food and not water a more likely source in developed countries. Sensitive to climate and grows rapidly in warmer environmental temps. Humans are the main reservoir. Shell fish and plankton are the only animal reservoirs. The natural habitat is believed to be the Ganges in Bangladesh
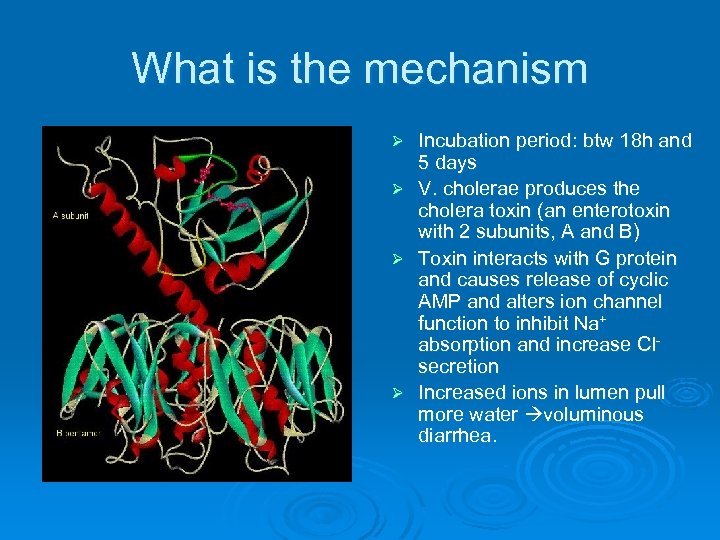 What is the mechanism Incubation period: btw 18 h and 5 days Ø V. cholerae produces the cholera toxin (an enterotoxin with 2 subunits, A and B) Ø Toxin interacts with G protein and causes release of cyclic AMP and alters ion channel function to inhibit Na+ absorption and increase Cl- secretion Ø Increased ions in lumen pull more water voluminous diarrhea. Ø
What is the mechanism Incubation period: btw 18 h and 5 days Ø V. cholerae produces the cholera toxin (an enterotoxin with 2 subunits, A and B) Ø Toxin interacts with G protein and causes release of cyclic AMP and alters ion channel function to inhibit Na+ absorption and increase Cl- secretion Ø Increased ions in lumen pull more water voluminous diarrhea. Ø
 What are the signs and symptoms? Ø Ø Ø Ø General stomach upset Massive watery “rice water” diarrhea (up to 20 liters/day) Muscle and stomach cramps Vomiting Fever (early on) Can progress from 1 st liquid stool to shock within 4 -6 hrs without treatment, and death within 18 -24 hrs. (Typical presentation is severe diarrhea but most people with cholera infection have no symptoms or mild diarrhea)
What are the signs and symptoms? Ø Ø Ø Ø General stomach upset Massive watery “rice water” diarrhea (up to 20 liters/day) Muscle and stomach cramps Vomiting Fever (early on) Can progress from 1 st liquid stool to shock within 4 -6 hrs without treatment, and death within 18 -24 hrs. (Typical presentation is severe diarrhea but most people with cholera infection have no symptoms or mild diarrhea)
 Signs and symptoms cont’ Poor skin turgor Ø Wrinkled skin Ø Sunken eyes Ø Restlessness and thirst Ø Apathy and LOC Ø
Signs and symptoms cont’ Poor skin turgor Ø Wrinkled skin Ø Sunken eyes Ø Restlessness and thirst Ø Apathy and LOC Ø
 Complications Acute renal failure Ø Electrolyte imbalance (esp. K+) Ø Severe hypoglycemia Ø Miscarriage of premature delivery in pregnant women Ø
Complications Acute renal failure Ø Electrolyte imbalance (esp. K+) Ø Severe hypoglycemia Ø Miscarriage of premature delivery in pregnant women Ø
 Treatment Aggressive Rehydration Ø Electrolyte replacement Ø ORT (1 tsp salt +8 tsp sugar in 1 liter Ø of clean/boiled water) IV therapy Ø Tetracycline, Cipro- may Ø reduce the duration of symptoms; resistance becoming apparent Ø Death rate without treatment is 50% and decreases to less than 1% with tx
Treatment Aggressive Rehydration Ø Electrolyte replacement Ø ORT (1 tsp salt +8 tsp sugar in 1 liter Ø of clean/boiled water) IV therapy Ø Tetracycline, Cipro- may Ø reduce the duration of symptoms; resistance becoming apparent Ø Death rate without treatment is 50% and decreases to less than 1% with tx
 Prevention Ø Clean Water-sterilization, boiling, chlorination, or good municipal water treatment Ø Sanitation-proper disposal of waste Ø Cook foods properly-esp high risk foods Ø Health education through mass media Ø Oral Vaccine (Dukoral) licensed and available in other countries, but not recommeded by CDC to travelers
Prevention Ø Clean Water-sterilization, boiling, chlorination, or good municipal water treatment Ø Sanitation-proper disposal of waste Ø Cook foods properly-esp high risk foods Ø Health education through mass media Ø Oral Vaccine (Dukoral) licensed and available in other countries, but not recommeded by CDC to travelers
 Foods to Avoid Ø Raw vegetables -Epidemic in Zambia in 2003 Ø Shellfish - oysters (concentrate the amount of vibrios)
Foods to Avoid Ø Raw vegetables -Epidemic in Zambia in 2003 Ø Shellfish - oysters (concentrate the amount of vibrios)
 References CDC. Cholera epidemic associated with raw vegetables--Lusaka, Zambia, 2003 -2004. MMWR Morb Mortal Wkly Rep. 2004 Sep 3; 53(34): 783 -6. Ø Sack DA, Sack RB, Nair GB, Siddique AK. Cholera. Lancet 2004; 363: 223 -33. Ø Morris JG. Clin Infect Dis. 2003 Jul 15; 37(2): 27280. Cholera and other types of vibriosis: a story of human pandemics and oysters on the half shell Ø
References CDC. Cholera epidemic associated with raw vegetables--Lusaka, Zambia, 2003 -2004. MMWR Morb Mortal Wkly Rep. 2004 Sep 3; 53(34): 783 -6. Ø Sack DA, Sack RB, Nair GB, Siddique AK. Cholera. Lancet 2004; 363: 223 -33. Ø Morris JG. Clin Infect Dis. 2003 Jul 15; 37(2): 27280. Cholera and other types of vibriosis: a story of human pandemics and oysters on the half shell Ø
 Cruise ship diarrhea
Cruise ship diarrhea
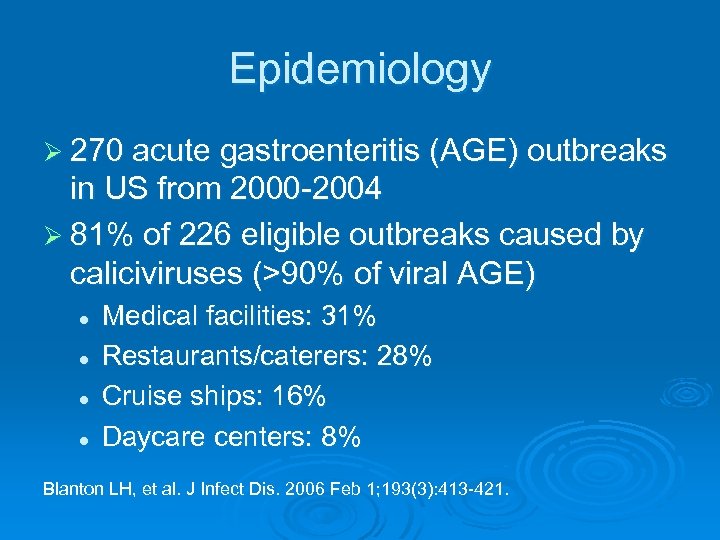 Epidemiology Ø 270 acute gastroenteritis (AGE) outbreaks in US from 2000 -2004 Ø 81% of 226 eligible outbreaks caused by caliciviruses (>90% of viral AGE) l l Medical facilities: 31% Restaurants/caterers: 28% Cruise ships: 16% Daycare centers: 8% Blanton LH, et al. J Infect Dis. 2006 Feb 1; 193(3): 413 -421.
Epidemiology Ø 270 acute gastroenteritis (AGE) outbreaks in US from 2000 -2004 Ø 81% of 226 eligible outbreaks caused by caliciviruses (>90% of viral AGE) l l Medical facilities: 31% Restaurants/caterers: 28% Cruise ships: 16% Daycare centers: 8% Blanton LH, et al. J Infect Dis. 2006 Feb 1; 193(3): 413 -421.
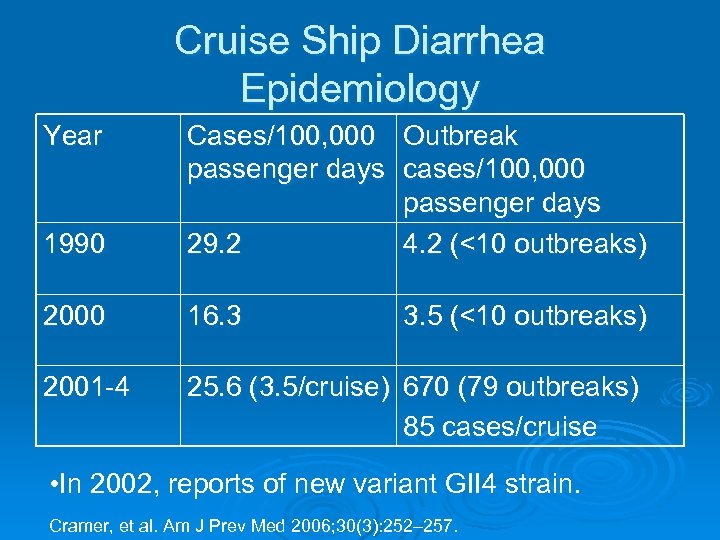 Cruise Ship Diarrhea Epidemiology Year 1990 Cases/100, 000 Outbreak passenger days cases/100, 000 passenger days 29. 2 4. 2 (<10 outbreaks) 2000 16. 3 2001 -4 25. 6 (3. 5/cruise) 670 (79 outbreaks) 85 cases/cruise 3. 5 (<10 outbreaks) • In 2002, reports of new variant GII 4 strain. Cramer, et al. Am J Prev Med 2006; 30(3): 252– 257.
Cruise Ship Diarrhea Epidemiology Year 1990 Cases/100, 000 Outbreak passenger days cases/100, 000 passenger days 29. 2 4. 2 (<10 outbreaks) 2000 16. 3 2001 -4 25. 6 (3. 5/cruise) 670 (79 outbreaks) 85 cases/cruise 3. 5 (<10 outbreaks) • In 2002, reports of new variant GII 4 strain. Cramer, et al. Am J Prev Med 2006; 30(3): 252– 257.
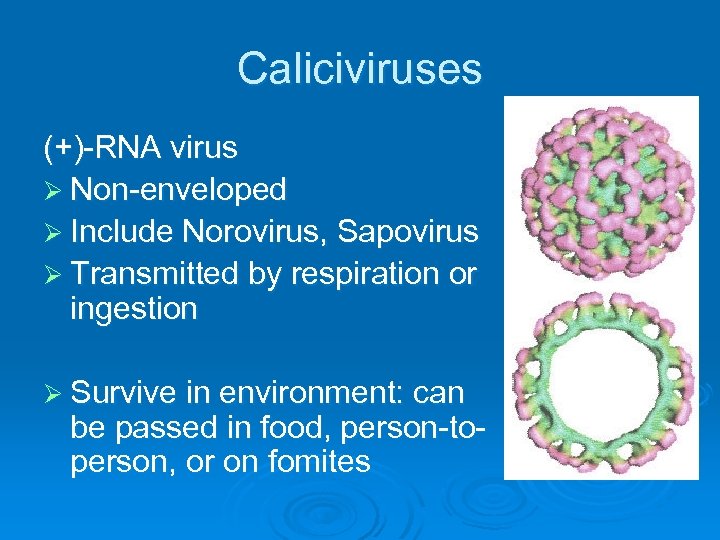 Caliciviruses (+)-RNA virus Ø Non-enveloped Ø Include Norovirus, Sapovirus Ø Transmitted by respiration or ingestion Ø Survive in environment: can be passed in food, person-toperson, or on fomites
Caliciviruses (+)-RNA virus Ø Non-enveloped Ø Include Norovirus, Sapovirus Ø Transmitted by respiration or ingestion Ø Survive in environment: can be passed in food, person-toperson, or on fomites
 Presentation Ø Incubation period: 1 -2 days Ø 1 st sign: abdominal cramps/nausea Ø Most have vomiting, diarrhea, or both Ø 1/5 have systemic symptoms Ø Duration 1 -3 days; self-limiting / supporting treatment / rehydration Ø Diarrhea: moderate (4 -8 stools per day), non-bloody, no mucus, not inflammatory/no WBCs
Presentation Ø Incubation period: 1 -2 days Ø 1 st sign: abdominal cramps/nausea Ø Most have vomiting, diarrhea, or both Ø 1/5 have systemic symptoms Ø Duration 1 -3 days; self-limiting / supporting treatment / rehydration Ø Diarrhea: moderate (4 -8 stools per day), non-bloody, no mucus, not inflammatory/no WBCs
 Prevention Ø CDC’s Vessel Sanitation Program l l l Started in 1975 Twice annual, unannounced inspections on ships with international itineraries at US ports 2001: implemented GISS (electronic gastrointestinal illness surveilance system) B/t 2001 -4, 4% of ships failed. http: //www. cdc. gov/nceh/vsp/default. htm
Prevention Ø CDC’s Vessel Sanitation Program l l l Started in 1975 Twice annual, unannounced inspections on ships with international itineraries at US ports 2001: implemented GISS (electronic gastrointestinal illness surveilance system) B/t 2001 -4, 4% of ships failed. http: //www. cdc. gov/nceh/vsp/default. htm
 Prevention Ø Things associated w/ outbreaks l l l Ø Things not associated with outbreaks l Ø Smaller ship Smaller fleet Older ships VSP score/performance Things associated with transmission during an outbreak l l Having a vomiting cabin mate Often initially food born, but then multiple routes, especially person-to person Isakbaeva, et al. , Emerging Infectious Diseases. 2005, 11(1); 154 -7.
Prevention Ø Things associated w/ outbreaks l l l Ø Things not associated with outbreaks l Ø Smaller ship Smaller fleet Older ships VSP score/performance Things associated with transmission during an outbreak l l Having a vomiting cabin mate Often initially food born, but then multiple routes, especially person-to person Isakbaeva, et al. , Emerging Infectious Diseases. 2005, 11(1); 154 -7.
 What you need to know Ø Risk of AGE on a cruise ship: <1% Ø Percent of cruise-ship physician caseload occupied by diarrhea: <10%. Ø But with >10 million passengers a year = lots of diarrhea. So… l l l Wash your hands often. Avoid sick people (e. g. cabin mates) and “vomit squad” Look up your cruises inspection score.
What you need to know Ø Risk of AGE on a cruise ship: <1% Ø Percent of cruise-ship physician caseload occupied by diarrhea: <10%. Ø But with >10 million passengers a year = lots of diarrhea. So… l l l Wash your hands often. Avoid sick people (e. g. cabin mates) and “vomit squad” Look up your cruises inspection score.
 Drink the water here: And you can TROT all the way home!
Drink the water here: And you can TROT all the way home!
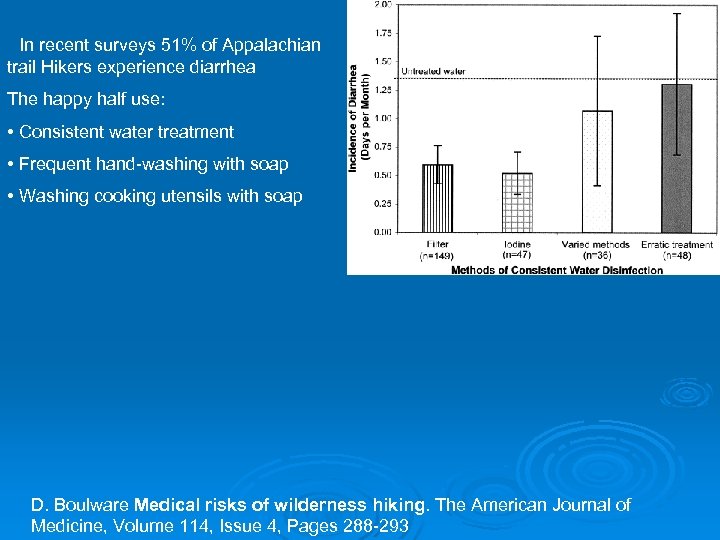 • In recent surveys 51% of Appalachian trail Hikers experience diarrhea The happy half use: • Consistent water treatment • Frequent hand-washing with soap • Washing cooking utensils with soap D. Boulware Medical risks of wilderness hiking. The American Journal of Medicine, Volume 114, Issue 4, Pages 288 -293
• In recent surveys 51% of Appalachian trail Hikers experience diarrhea The happy half use: • Consistent water treatment • Frequent hand-washing with soap • Washing cooking utensils with soap D. Boulware Medical risks of wilderness hiking. The American Journal of Medicine, Volume 114, Issue 4, Pages 288 -293
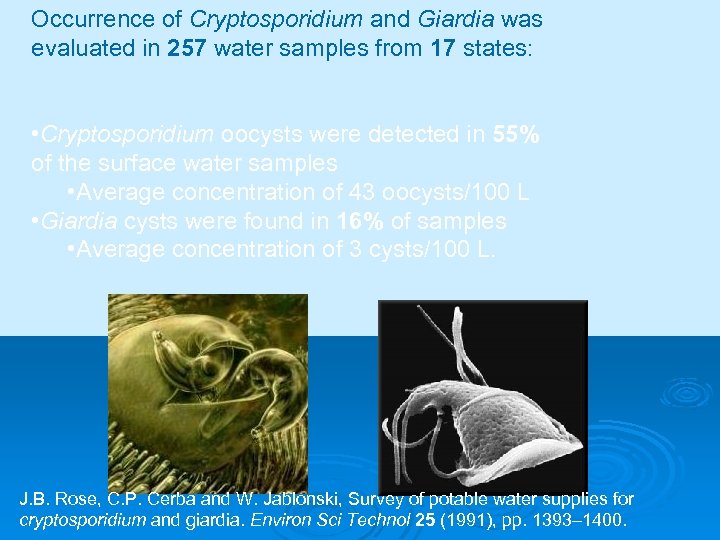 Occurrence of Cryptosporidium and Giardia was evaluated in 257 water samples from 17 states: • Cryptosporidium oocysts were detected in 55% of the surface water samples • Average concentration of 43 oocysts/100 L • Giardia cysts were found in 16% of samples • Average concentration of 3 cysts/100 L. J. B. Rose, C. P. Cerba and W. Jablonski, Survey of potable water supplies for cryptosporidium and giardia. Environ Sci Technol 25 (1991), pp. 1393– 1400.
Occurrence of Cryptosporidium and Giardia was evaluated in 257 water samples from 17 states: • Cryptosporidium oocysts were detected in 55% of the surface water samples • Average concentration of 43 oocysts/100 L • Giardia cysts were found in 16% of samples • Average concentration of 3 cysts/100 L. J. B. Rose, C. P. Cerba and W. Jablonski, Survey of potable water supplies for cryptosporidium and giardia. Environ Sci Technol 25 (1991), pp. 1393– 1400.
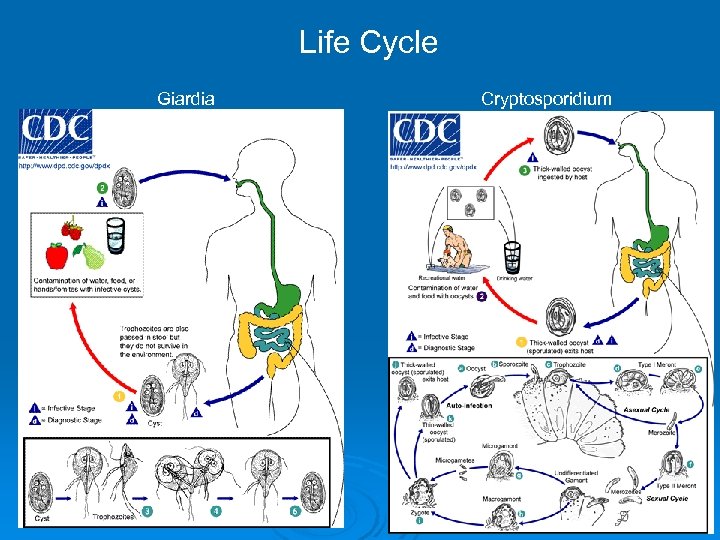 Life Cycle Giardia Cryptosporidium
Life Cycle Giardia Cryptosporidium
 Prevention • Cryptosporidium form oocysts between 4 to 7 microns in size. • Giardia cysts are 6 to 10 microns (One micron is one thousandth of a millimetre). • Cryptosporidium is not killed by normal chlorination and is only made harmless by long exposure to concentrated ultra violet light or specialized chemical treatment, Giardia is killed by long contact with chlorine or long exposure to concentrated UV light. • The most successful method of removing oocysts from a water supply is by filtration through microstrainers or cartridge filters. (1 micron absolute) http: //www. drinking-water. co. uk/information%20 sheets/cryptosporidium. htm
Prevention • Cryptosporidium form oocysts between 4 to 7 microns in size. • Giardia cysts are 6 to 10 microns (One micron is one thousandth of a millimetre). • Cryptosporidium is not killed by normal chlorination and is only made harmless by long exposure to concentrated ultra violet light or specialized chemical treatment, Giardia is killed by long contact with chlorine or long exposure to concentrated UV light. • The most successful method of removing oocysts from a water supply is by filtration through microstrainers or cartridge filters. (1 micron absolute) http: //www. drinking-water. co. uk/information%20 sheets/cryptosporidium. htm
 Treatment Giardiasis treatment Cryptosporidiosis treatment • Metronidazole • Supportive unless immunocompromised • some other antimicrobials as well • Treat Giardiasis because chronic infection – also examine close contacts and treat if found. www. emedicine. com/emerg/topic 215. htm, and med/topic 484. htm
Treatment Giardiasis treatment Cryptosporidiosis treatment • Metronidazole • Supportive unless immunocompromised • some other antimicrobials as well • Treat Giardiasis because chronic infection – also examine close contacts and treat if found. www. emedicine. com/emerg/topic 215. htm, and med/topic 484. htm
 Shigella My favourite bloody diarrhea
Shigella My favourite bloody diarrhea
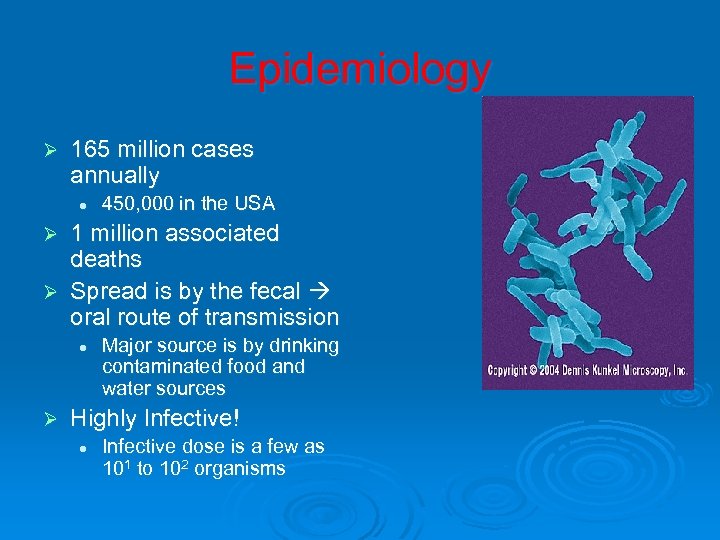 Epidemiology Ø 165 million cases annually l 450, 000 in the USA 1 million associated deaths Ø Spread is by the fecal oral route of transmission Ø l Ø Major source is by drinking contaminated food and water sources Highly Infective! l Infective dose is a few as 101 to 102 organisms
Epidemiology Ø 165 million cases annually l 450, 000 in the USA 1 million associated deaths Ø Spread is by the fecal oral route of transmission Ø l Ø Major source is by drinking contaminated food and water sources Highly Infective! l Infective dose is a few as 101 to 102 organisms
 Pathogenesis Shigella highly infective b/c resistant to natural defensive stomach acid Ø Bugs phagocytosed by intestinal epithelium Ø Once inside of the cell, the bug spreads directly from cell to cell Ø Actin spear Ø
Pathogenesis Shigella highly infective b/c resistant to natural defensive stomach acid Ø Bugs phagocytosed by intestinal epithelium Ø Once inside of the cell, the bug spreads directly from cell to cell Ø Actin spear Ø
 Clinical Manifestations Ø Incubation of 1 -7 days Ø Symptoms l l High fever Abdominal cramps Bloody diarrhea Vomiting
Clinical Manifestations Ø Incubation of 1 -7 days Ø Symptoms l l High fever Abdominal cramps Bloody diarrhea Vomiting
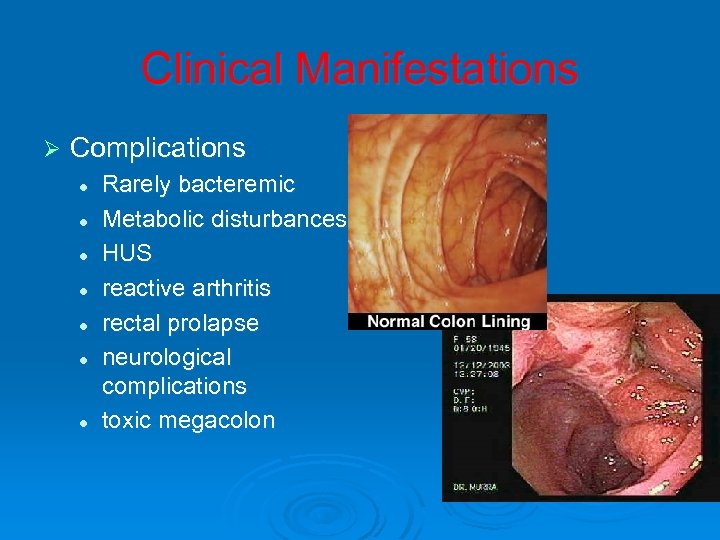 Clinical Manifestations Ø Complications l l l l Rarely bacteremic Metabolic disturbances HUS reactive arthritis rectal prolapse neurological complications toxic megacolon
Clinical Manifestations Ø Complications l l l l Rarely bacteremic Metabolic disturbances HUS reactive arthritis rectal prolapse neurological complications toxic megacolon
 Treatment Break the cycle of the“ 5 -Fs” Ø Best treatment is prevention Ø l Meta analysis showed 59% reduction in incidence with handwashing • Curtis, Cairncross. Lancet Infect Dis 2003 May; 3(5): 275 -81 Ø No effective treatment l Self limiting disease, course usually 7 days Cipro and Septra have been shown to decrease fever by 1 -2 days Ø No vaccine currently available; in development Ø
Treatment Break the cycle of the“ 5 -Fs” Ø Best treatment is prevention Ø l Meta analysis showed 59% reduction in incidence with handwashing • Curtis, Cairncross. Lancet Infect Dis 2003 May; 3(5): 275 -81 Ø No effective treatment l Self limiting disease, course usually 7 days Cipro and Septra have been shown to decrease fever by 1 -2 days Ø No vaccine currently available; in development Ø
 Questions?
Questions?


