0d9ecd653fbd780b5757a15942f92416.ppt
- Количество слайдов: 37
Atrial Fibrillation RACHEAL JAMES HEART RHYTHM SPECIALIST NURSE UHW
The Role of the Heart Rhythm Specialist Nurse It is now widely recognised within our trust that the skills and expertise the Heart Rhythm Specialist Nurses bring to arrhythmia services are extremely valuable. The role of the specialist arrhythmia nurse is diverse and varies dependent on local service needs Roles include caring for patients with Atrial Fibrillation, Device therapy (ICD or CRT-D), syncope and screening for SCD relatives
Journey of Heart Rhythm Specialist Nurse Qualified as Registered Nurse October 1996 9 Years Acute Cardiology Experience on Coronary Care Unit at University Hospital of Wales 3 Years Experience on the Cardiac Day Case Unit – Cardiology and Electrophysiology intervention 4 Years Heart Rhythm Specialist Nurse Currently attending the MSc “Advanced Programme” at Cardiff University Independent Prescriber MSc Arrhythmia Management Module
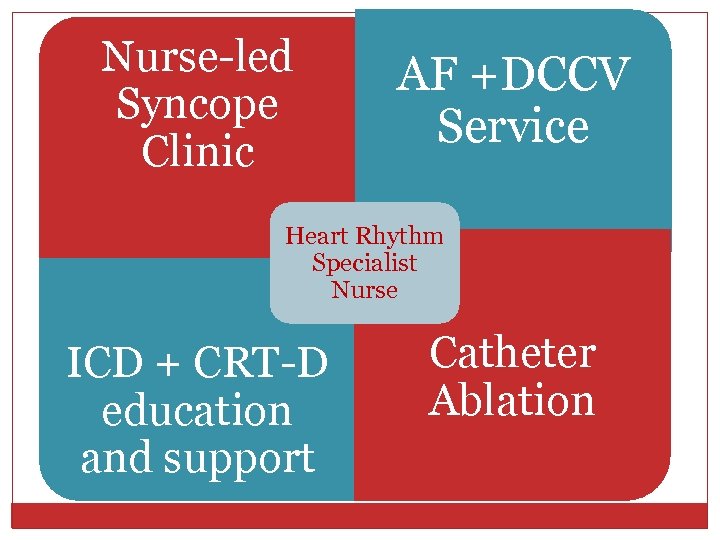
Nurse-led Syncope Clinic AF +DCCV Service Heart Rhythm Specialist Nurse ICD + CRT-D education and support Catheter Ablation
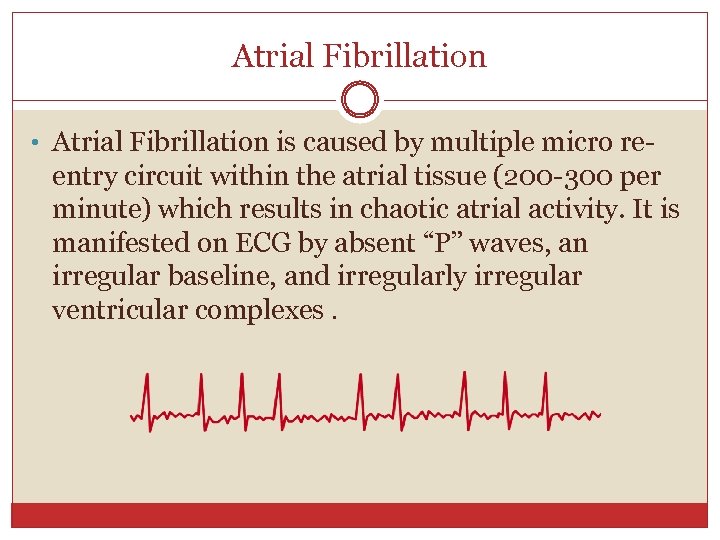
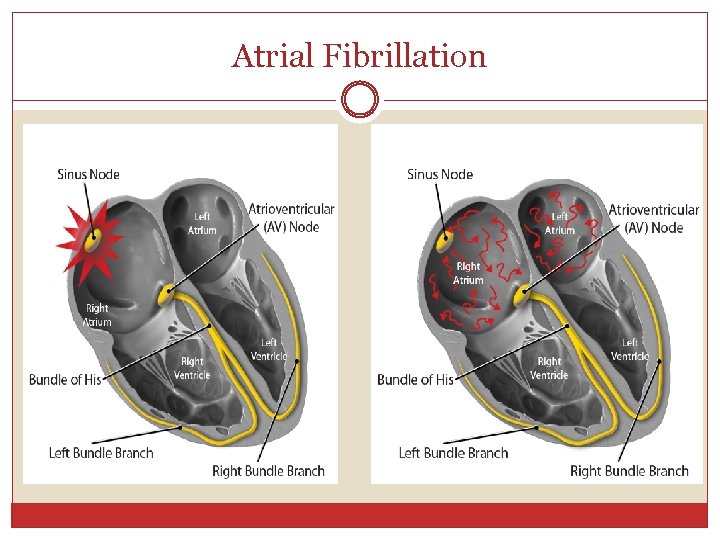
Atrial Fibrillation • Atrial Fibrillation is caused by multiple micro re- entry circuit within the atrial tissue (200 -300 per minute) which results in chaotic atrial activity. It is manifested on ECG by absent “P” waves, an irregular baseline, and irregularly irregular ventricular complexes.
Atrial Fibrillation
Risks factors for Atrial Fibrillation Hypertension Coronary artery disease Heart Failure Hyperthyroidism Rheumatic heart disease-valvular defects Obesity Alcohol
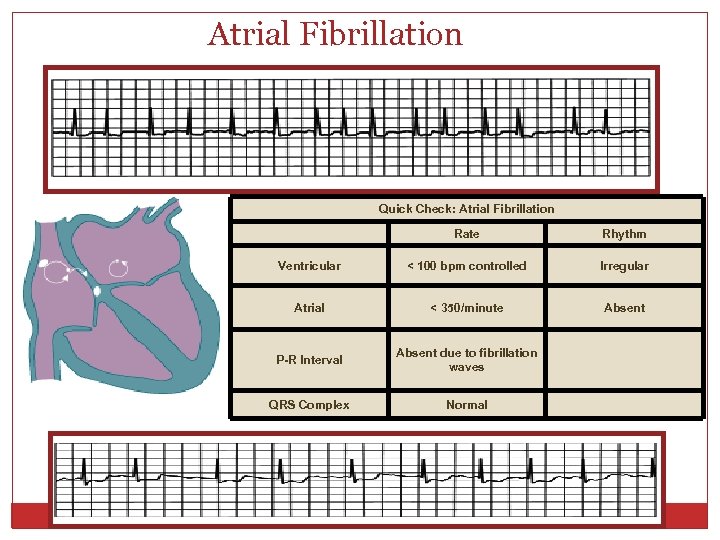
Atrial Fibrillation Quick Check: Atrial Fibrillation Rate Rhythm Ventricular < 100 bpm controlled Irregular Atrial < 350/minute Absent P-R Interval Absent due to fibrillation waves QRS Complex Normal
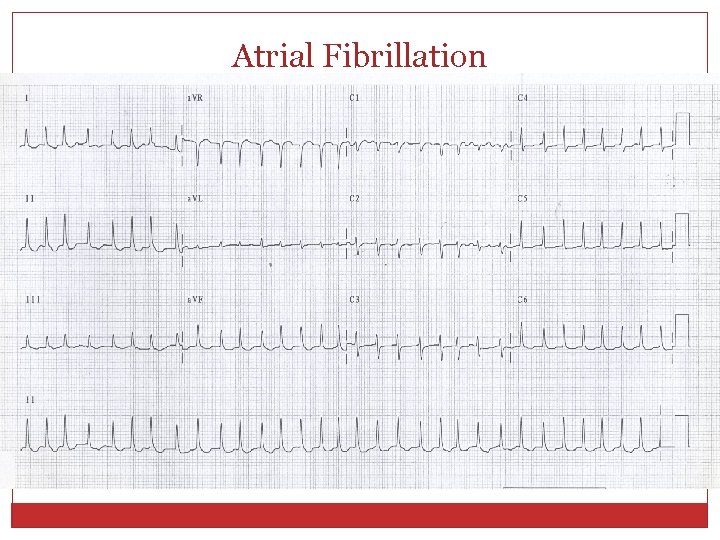
Atrial Fibrillation
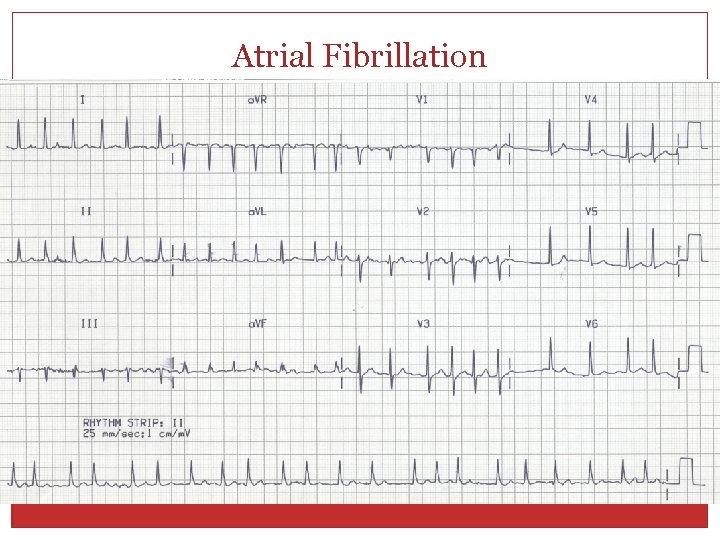
Atrial Fibrillation
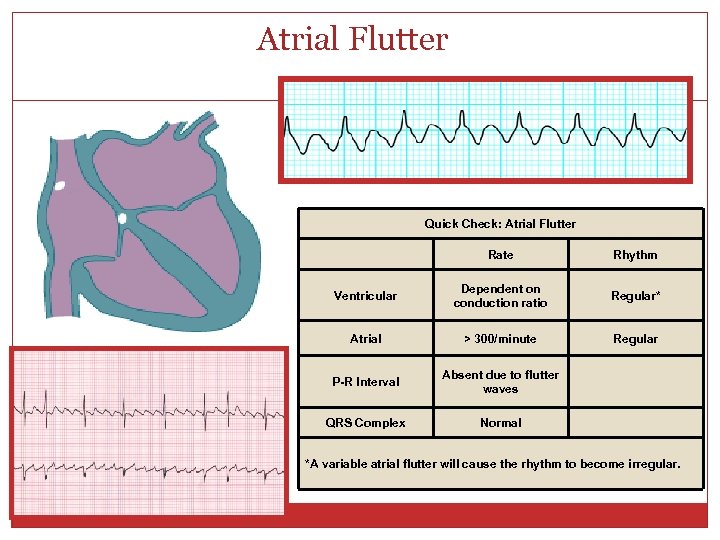
Atrial Flutter Quick Check: Atrial Flutter Rate Rhythm Ventricular Dependent on conduction ratio Regular* Atrial > 300/minute Regular P-R Interval Absent due to flutter waves QRS Complex Normal *A variable atrial flutter will cause the rhythm to become irregular.
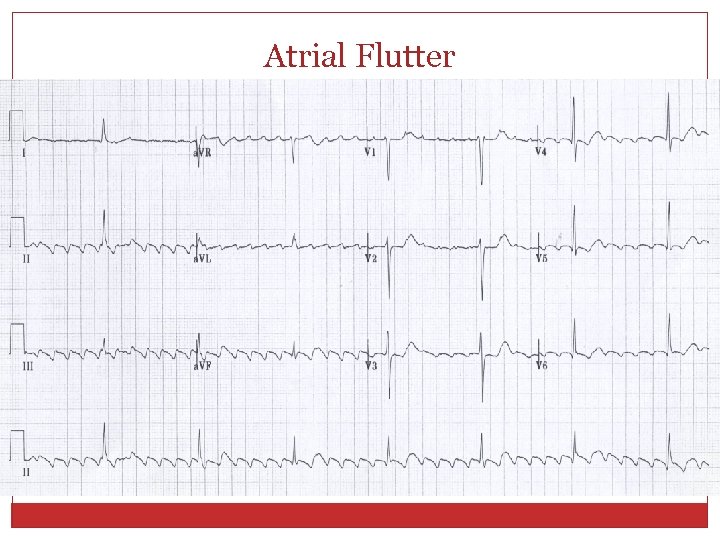
Atrial Flutter
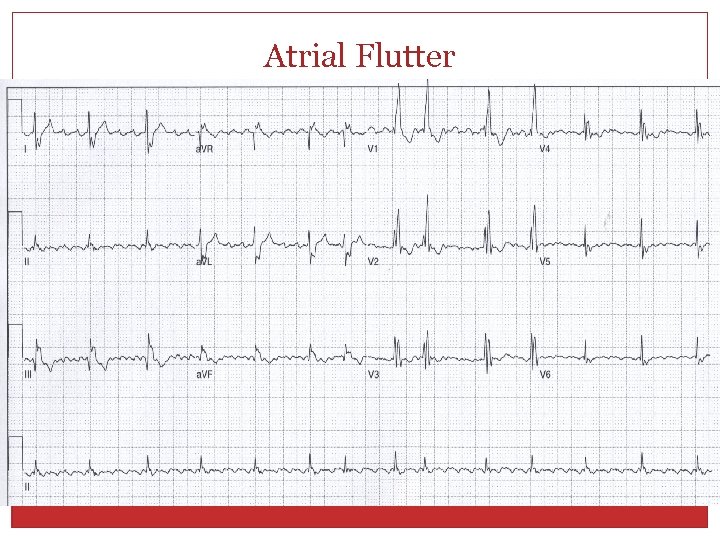
Atrial Flutter
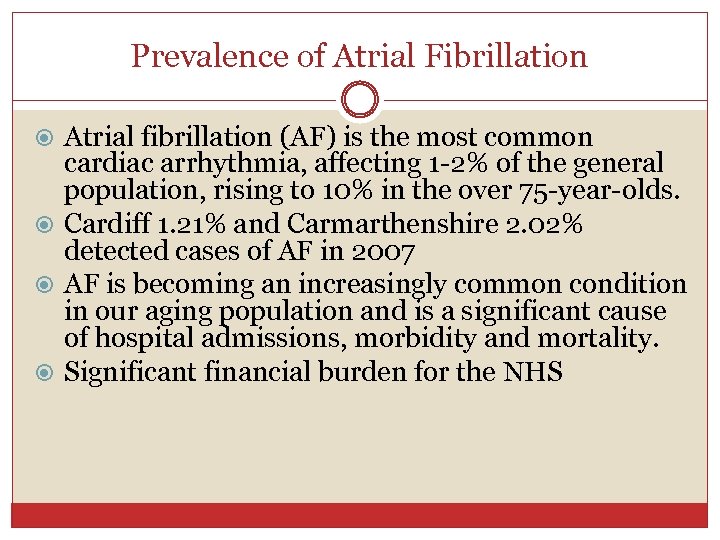
Prevalence of Atrial Fibrillation Atrial fibrillation (AF) is the most common cardiac arrhythmia, affecting 1 -2% of the general population, rising to 10% in the over 75 -year-olds. Cardiff 1. 21% and Carmarthenshire 2. 02% detected cases of AF in 2007 AF is becoming an increasingly common condition in our aging population and is a significant cause of hospital admissions, morbidity and mortality. Significant financial burden for the NHS
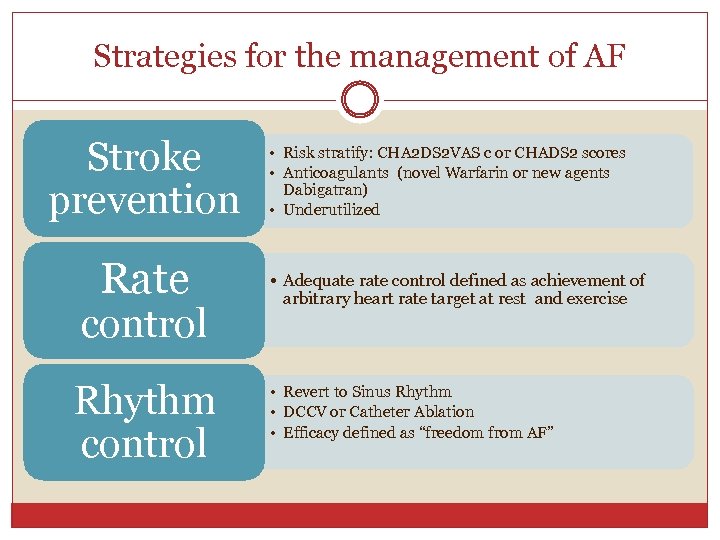
Strategies for the management of AF Stroke prevention Rate control Rhythm control • Risk stratify: CHA 2 DS 2 VAS c or CHADS 2 scores • Anticoagulants (novel Warfarin or new agents Dabigatran) • Underutilized • Adequate rate control defined as achievement of arbitrary heart rate target at rest and exercise • Revert to Sinus Rhythm • DCCV or Catheter Ablation • Efficacy defined as “freedom from AF”
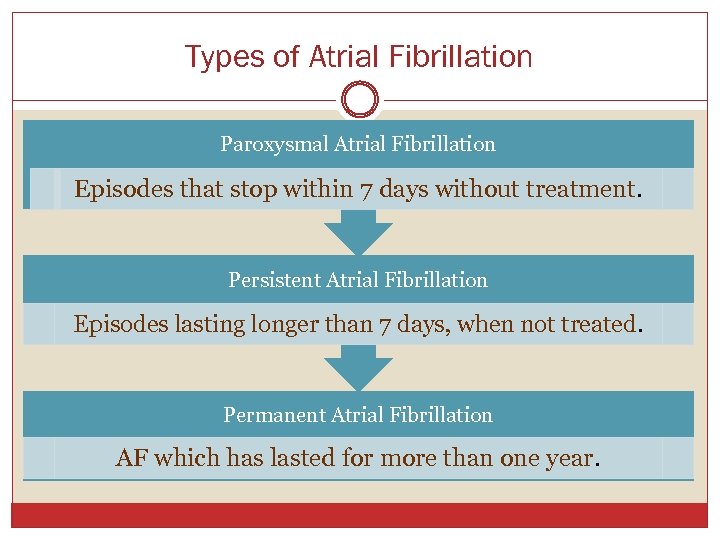
Types of Atrial Fibrillation Paroxysmal Atrial Fibrillation Episodes that stop within 7 days without treatment. Persistent Atrial Fibrillation Episodes lasting longer than 7 days, when not treated. Permanent Atrial Fibrillation AF which has lasted for more than one year.
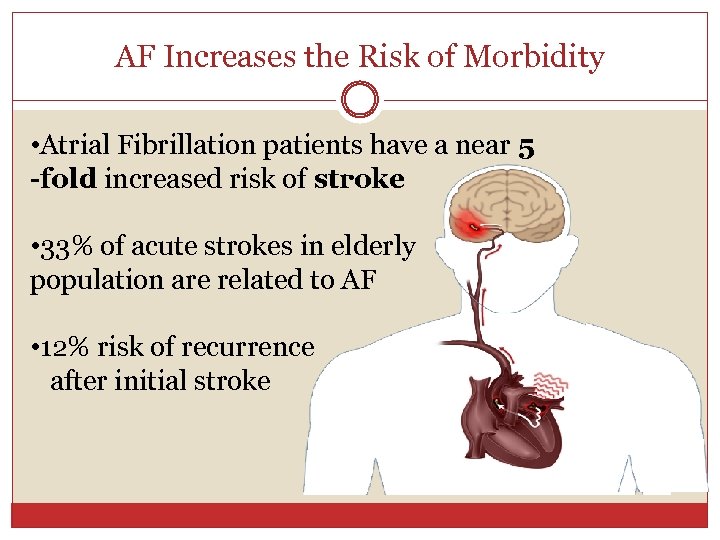
AF Increases the Risk of Morbidity • Atrial Fibrillation patients have a near 5 -fold increased risk of stroke • 33% of acute strokes in elderly population are related to AF • 12% risk of recurrence after initial stroke
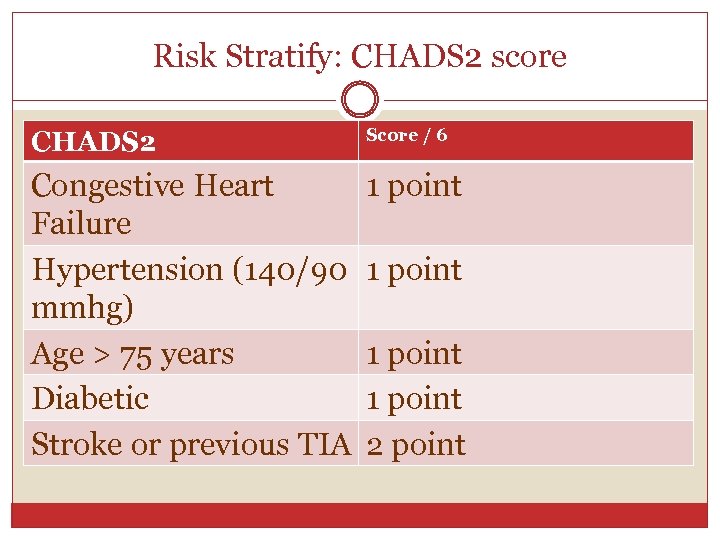
Risk Stratify: CHADS 2 score CHADS 2 Score / 6 Congestive Heart Failure Hypertension (140/90 mmhg) Age > 75 years Diabetic Stroke or previous TIA 1 point 2 point
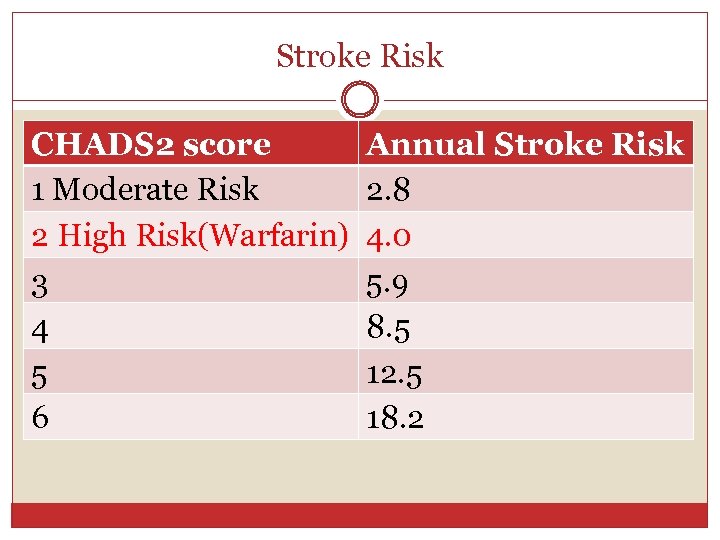
Stroke Risk CHADS 2 score 1 Moderate Risk 2 High Risk(Warfarin) 3 4 5 6 Annual Stroke Risk 2. 8 4. 0 5. 9 8. 5 12. 5 18. 2
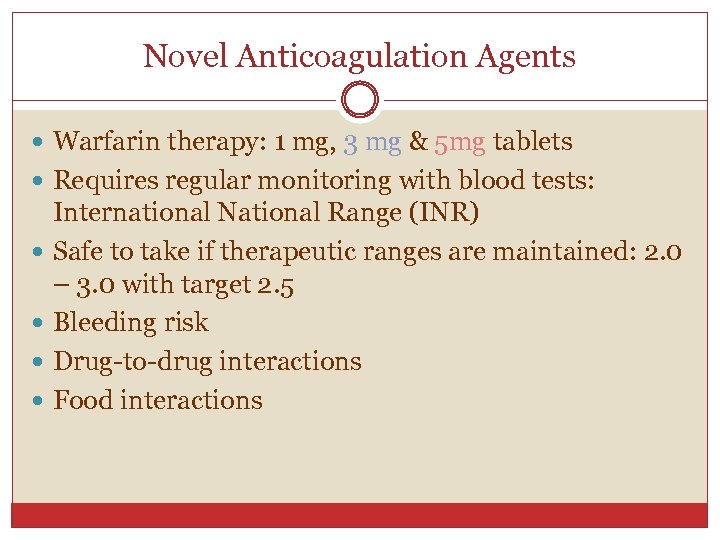
Novel Anticoagulation Agents Warfarin therapy: 1 mg, 3 mg & 5 mg tablets Requires regular monitoring with blood tests: International National Range (INR) Safe to take if therapeutic ranges are maintained: 2. 0 – 3. 0 with target 2. 5 Bleeding risk Drug-to-drug interactions Food interactions
New Anticoagulation agent Prevention of stroke in adults with non-valvular atrial fibrillation with 1 or more risk factors: Previous stroke, TIA or systemic embolism (SEE) Left ventricular ejection fraction (LVEF) <40% Symptomatic heart failure (NYHA) class >2 Age> 75 years Age >65 years associated with one of the following: diabetes mellitus, coronary artery disease or hypertension
New Anticoagulation Agents Dabigatran: 110 mg & 150 mg (BD) Rapid onset of action: 2 hours No dietary restrictions No requirement for routine coagulation (INR) monitoring Main side-effect: Dyspepsia
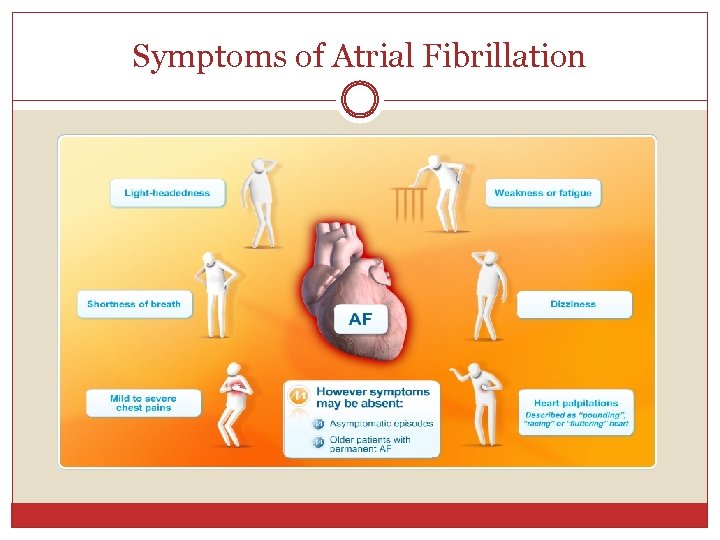
Symptoms of Atrial Fibrillation
Rate Control: Slow ventricular rate The latest ESC guidelines state that it is reasonable to initiate treatment with a rate control protocol aimed at a resting heart rate of <110 beats per minute. When symptoms persist a stricter rate control strategy should aim at achieving a resting heart rate <80 beats per minute and a heart rate during moderate exercise <110 beats per minute. First-line therapies for pharmacological control of heart rate include beta-blockers, calcium channel blockers and digitalis, which can be used either alone or in combination Unfortunately many of the side-effects from antiarrhythmic medications are intolerable
Rhythm Control: Restore Sinus Rhythm Direct Current Cardioversion (DCCV): Synchronized electrical cardioversion using biphasic defibrillator A synchronized shock via 2 pads with selected amount of electric current over a predefined number of milliseconds at the optimal moment in the cardiac cycle. • Timing the shock to the R wave prevents the delivery of the shock during the vulnerable period (or relative refractory period) R wave of the QRS complex on the ECG. • Reduce risk of inducing Ventricular Fibrillation
Rhythm Control: Restore Sinus Rhythm • Heart Rhythm Specialist Nurse accepts direct referrals for DCCV service – suitability? ? ? Currently 45 patients on waiting list 3 -4 DCCV each week (170 -180 a year) Initiates anticoagulation – Warfarin Therapy and coordinates therapeutic ranges pre DCCV Direct contact in symptoms change or relapse back into AF post PVI or DCCV
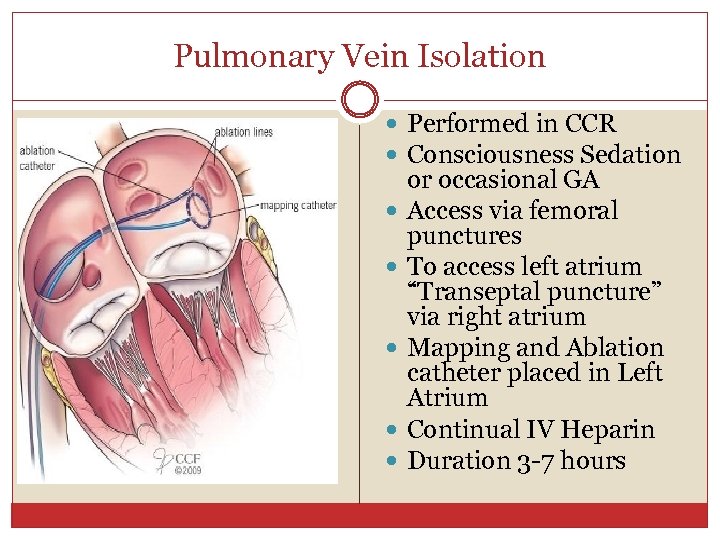
Pulmonary Vein Isolation Performed in CCR Consciousness Sedation or occasional GA Access via femoral punctures To access left atrium “Transeptal puncture” via right atrium Mapping and Ablation catheter placed in Left Atrium Continual IV Heparin Duration 3 -7 hours
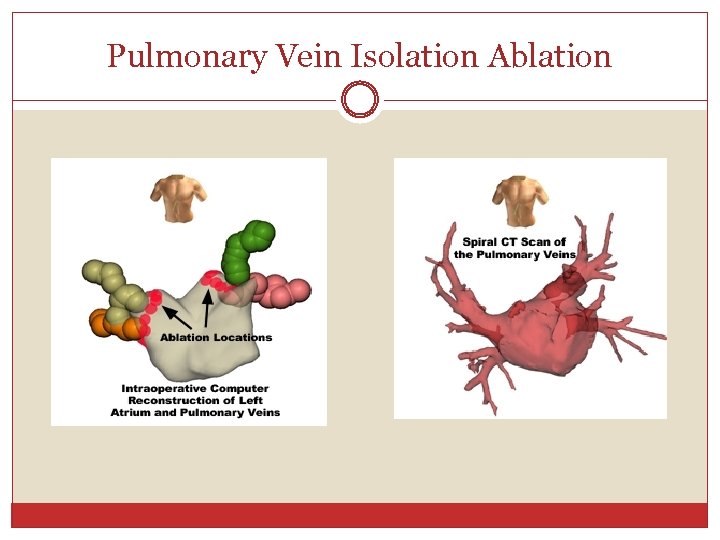
Pulmonary Vein Isolation Ablation
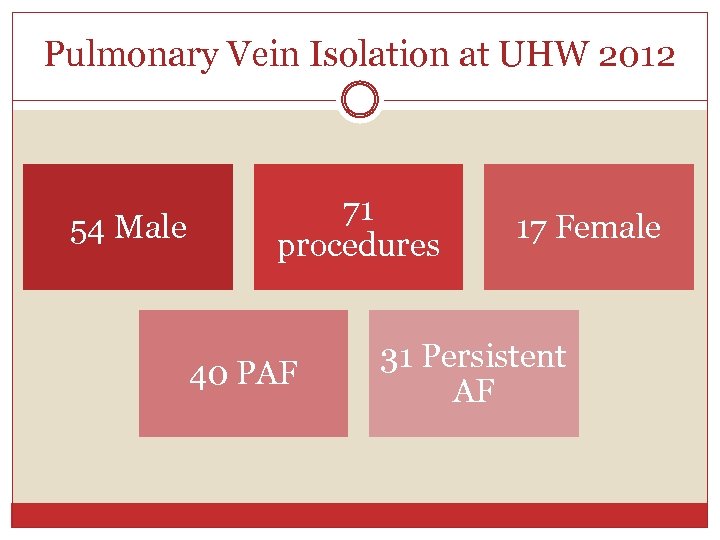
Pulmonary Vein Isolation at UHW 2012 54 Male 71 procedures 40 PAF 17 Female 31 Persistent AF
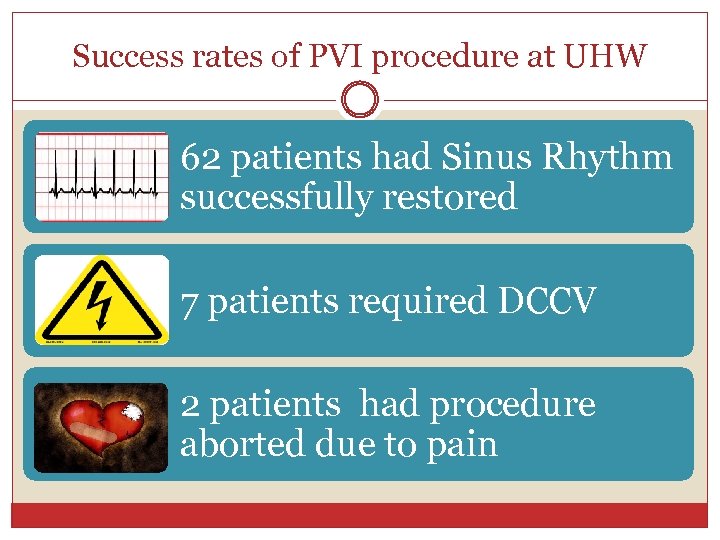
Success rates of PVI procedure at UHW 62 patients had Sinus Rhythm successfully restored 7 patients required DCCV 2 patients had procedure aborted due to pain
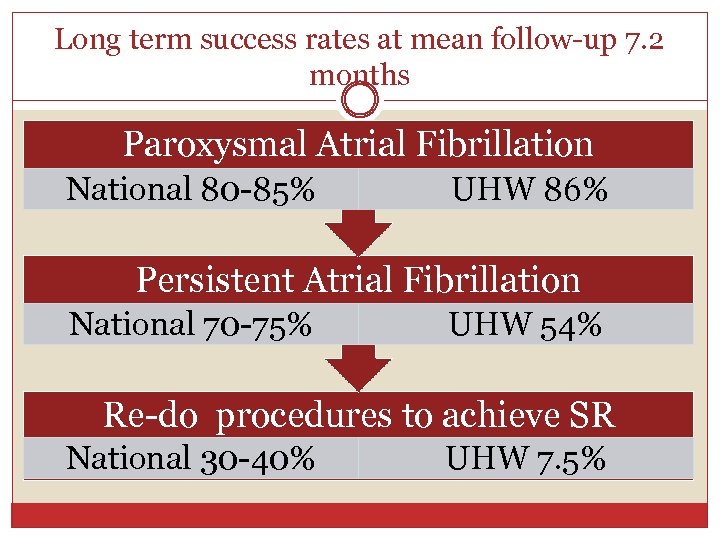
Long term success rates at mean follow-up 7. 2 months Paroxysmal Atrial Fibrillation National 80 -85% UHW 86% Persistent Atrial Fibrillation National 70 -75% UHW 54% Re-do procedures to achieve SR National 30 -40% UHW 7. 5%
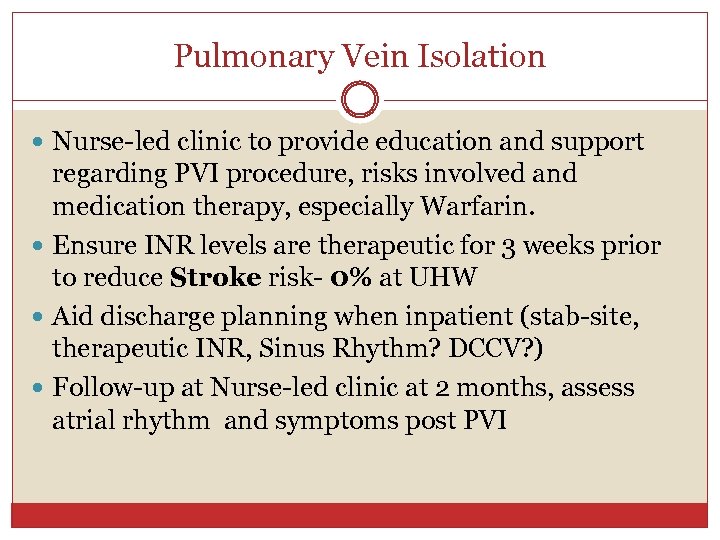
Pulmonary Vein Isolation Nurse-led clinic to provide education and support regarding PVI procedure, risks involved and medication therapy, especially Warfarin. Ensure INR levels are therapeutic for 3 weeks prior to reduce Stroke risk- 0% at UHW Aid discharge planning when inpatient (stab-site, therapeutic INR, Sinus Rhythm? DCCV? ) Follow-up at Nurse-led clinic at 2 months, assess atrial rhythm and symptoms post PVI
Pulmonary Vein Isolation Independent Prescriber to restart or titrate anti arrhythmic drugs if relapsed back into AF. Arrange DCCV if relapsed into persistent AF Direct access via telephone-anxious patients awaiting a very complex procedure-lots of questions. Recovery not always straightforward- prone to bouts of AF post PVI-doesn’t mean PVI unsuccessful. Main link between Consultant, GP, secretary and patient.
Support from Arrhythmia Charities British Heart Foundation & Atrial Fibrillation Association Raise Awareness of Atrial Fibrillation Arrhythmia Alliance (AA) Provide education and support for AF patients – information sheets and leaflets
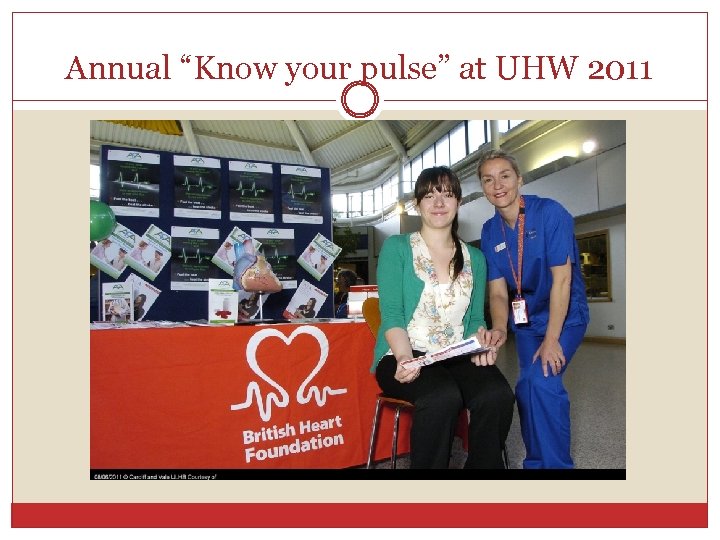
Annual “Know your pulse” at UHW 2011
Thank You Any Questions? ? ?
0d9ecd653fbd780b5757a15942f92416.ppt