s-110606075809-phpapp01.ppt
- Количество слайдов: 48
ATHEROSCLEROSIS MORPHOLOGY & COMPLICATIONS -S. SHRINATH 83 Batch.
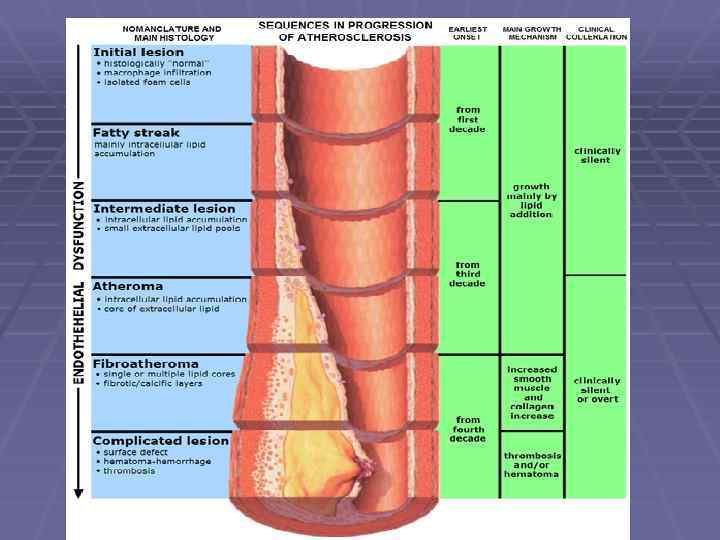
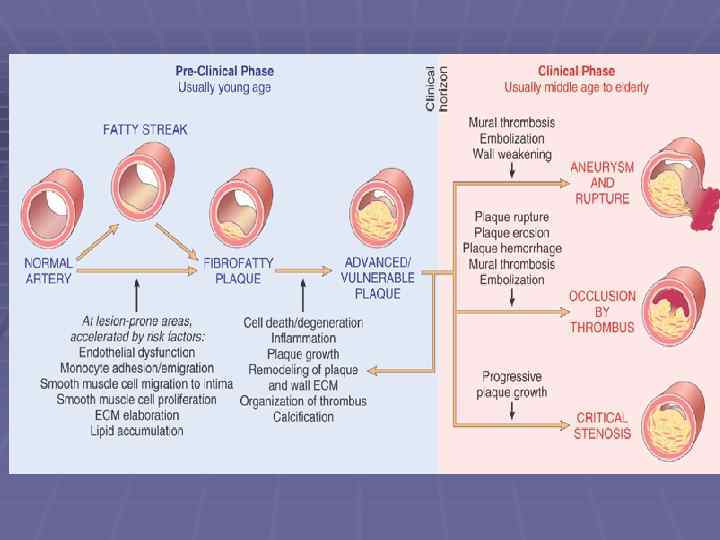
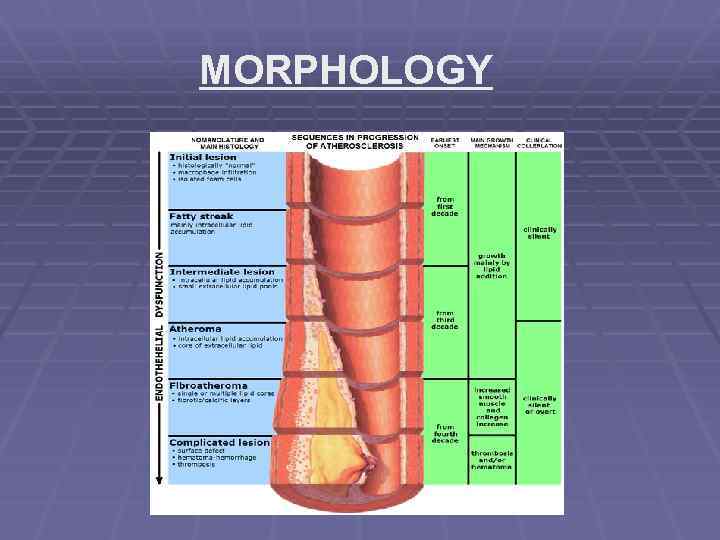
MORPHOLOGY §FATTY STREAK §ATHEROSCLEROTIC PLAQUE
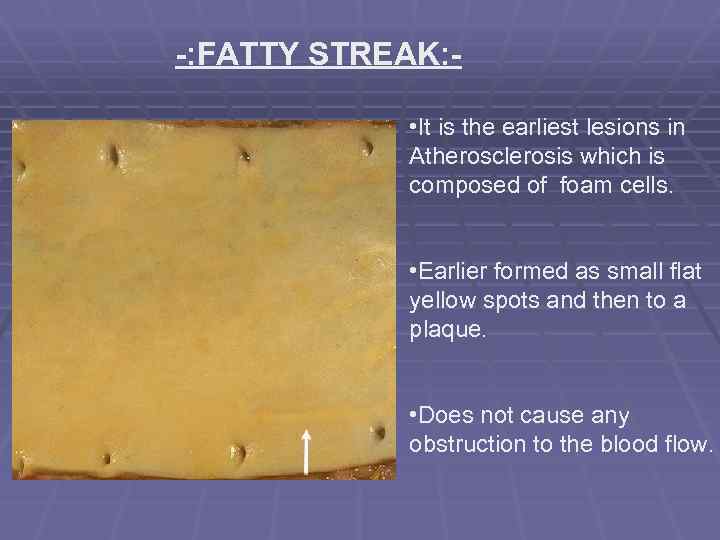
-: FATTY STREAK: • It is the earliest lesions in Atherosclerosis which is composed of foam cells. • Earlier formed as small flat yellow spots and then to a plaque. • Does not cause any obstruction to the blood flow.
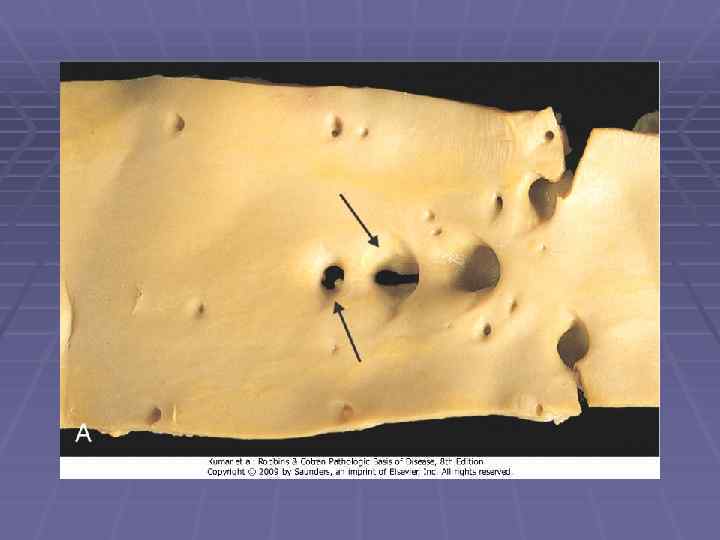
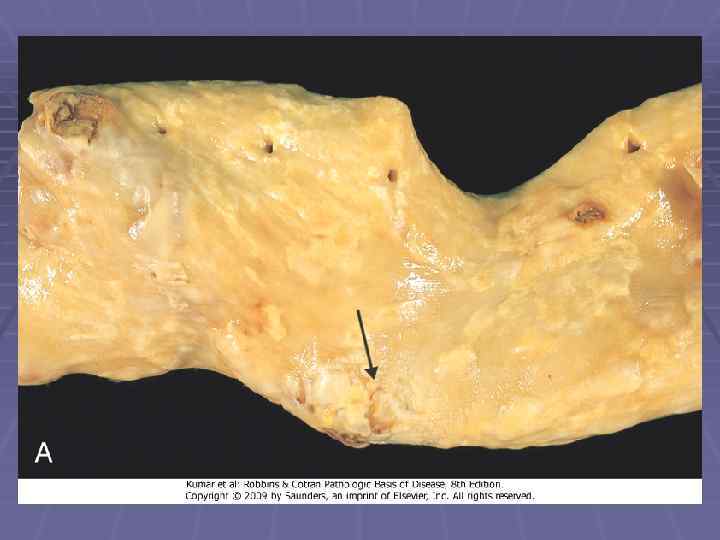
-: ATHEROSCLEROTIC PLAQUE: • Intimal thickening and lipid accumulation. • Lodged in the lumen of the artery (0. 3 -1. 5 cm in dia). • Grossly they appear as white to yellow patches. • Lesions are mostly eccentric but rarely circumferential. • Local flow disturbances –increased susceptibility to plaque formation.
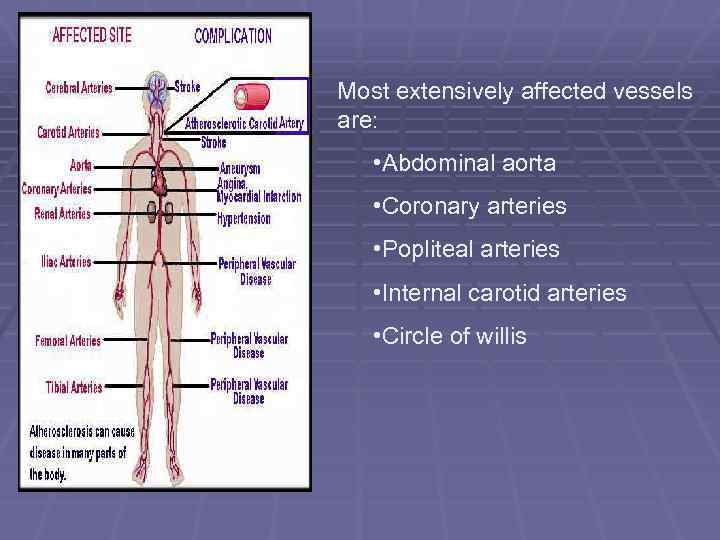
Most extensively affected vessels are: • Abdominal aorta • Coronary arteries • Popliteal arteries • Internal carotid arteries • Circle of willis
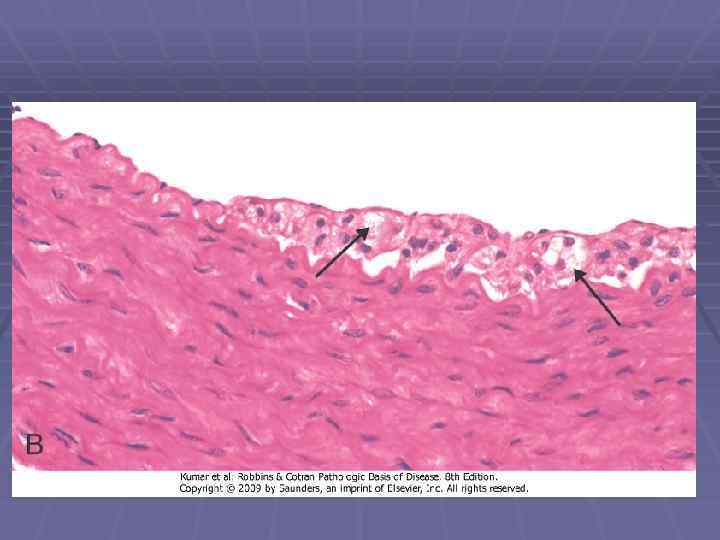
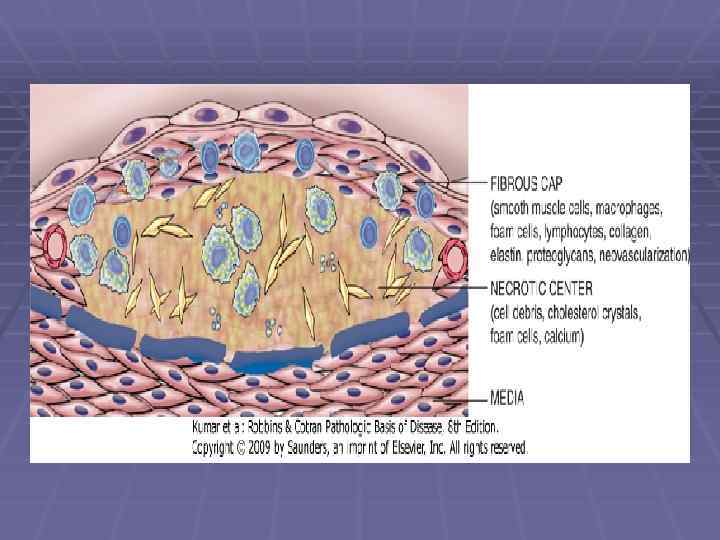
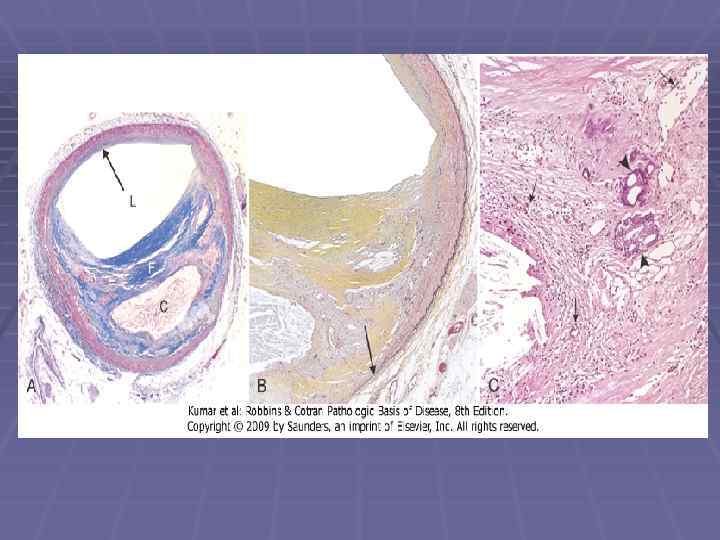
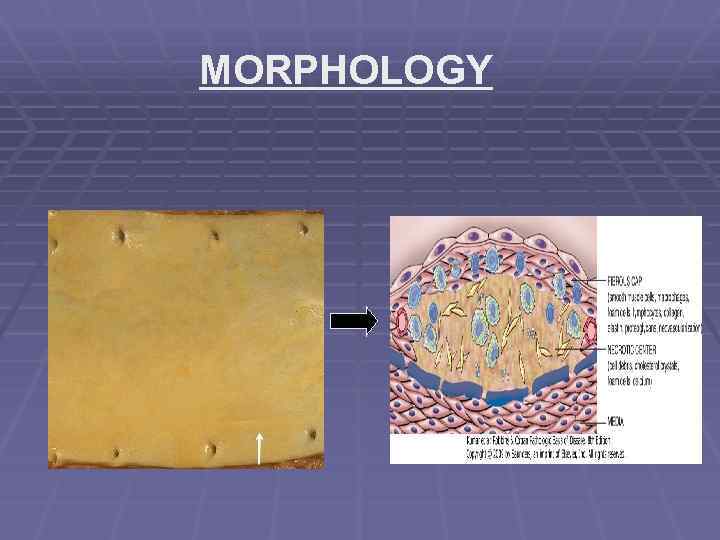
Components of Plaque: Cells • T-cells • Smooth muscle cells • Macrophages. ECM • Collagen • Elastic fibers • Proteoglycans Lipids • Intracellular and extracellular.
-: DESCRIPTION – PLAQUE: • Typically composed of superficial composed fibrous cap (smooth muscle cells and collagen). • Beneath it contains cellular area. • Deeply containing lipid core, cell debris, foam cells, fibrin, thrombus, plasma proteins. • Periphery shows neovascularisation.
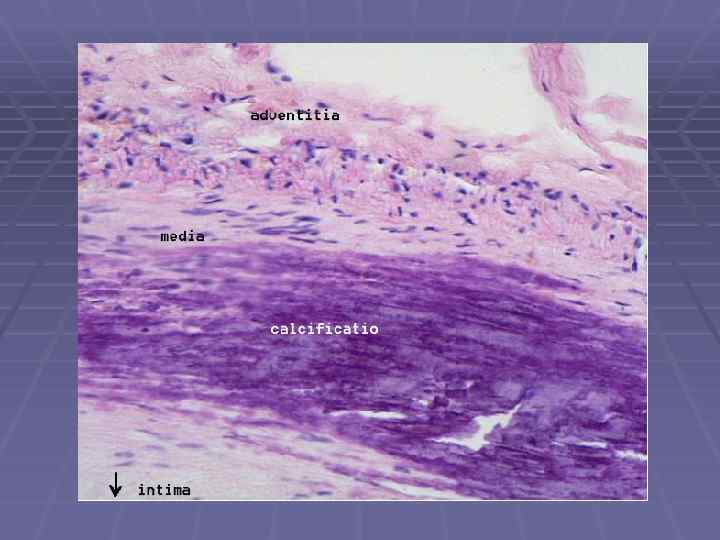
-: NATURE OF THE PLAQUE: ØProgressively enlarges due to: - • Cell death and degeneration. • Synthesis and remodeling of collagen. • Organization of thrombus. ØOften undergo calcification.
CHANGES IN THE ATHEROSCLEROTIC PLAQUE • Rupture , erosion , ulceration. • Hemorrhage into a plaque. • Atheroembolism. • Aneurysm formation.
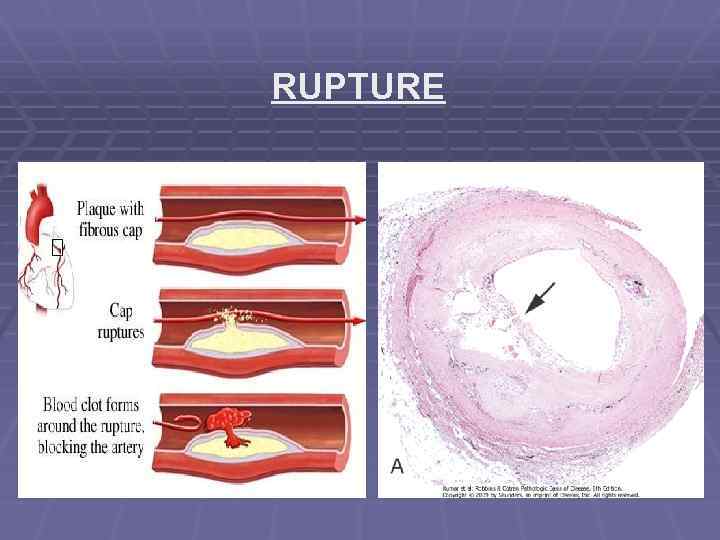
RUPTURE
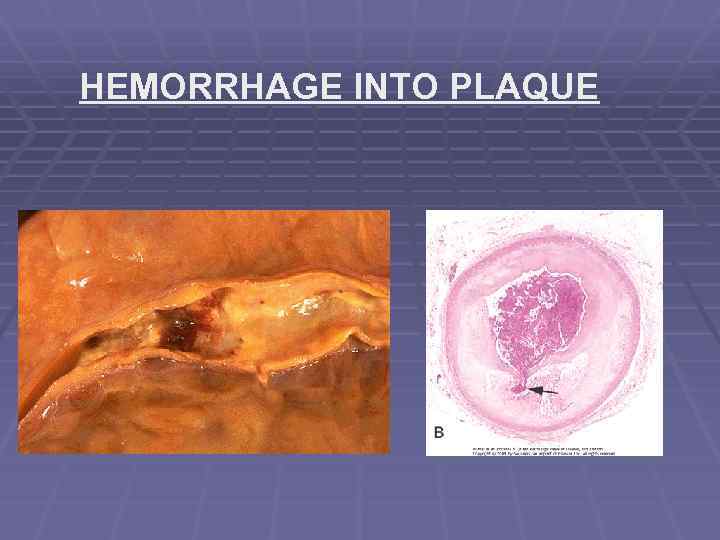
HEMORRHAGE INTO PLAQUE
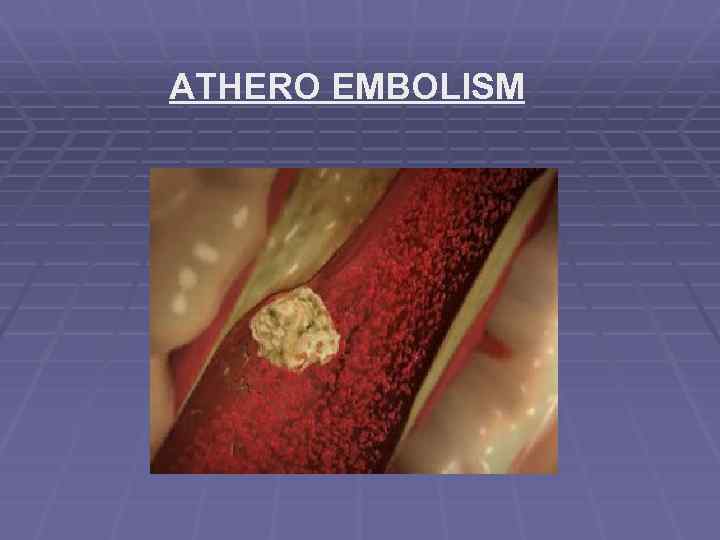
ATHERO EMBOLISM
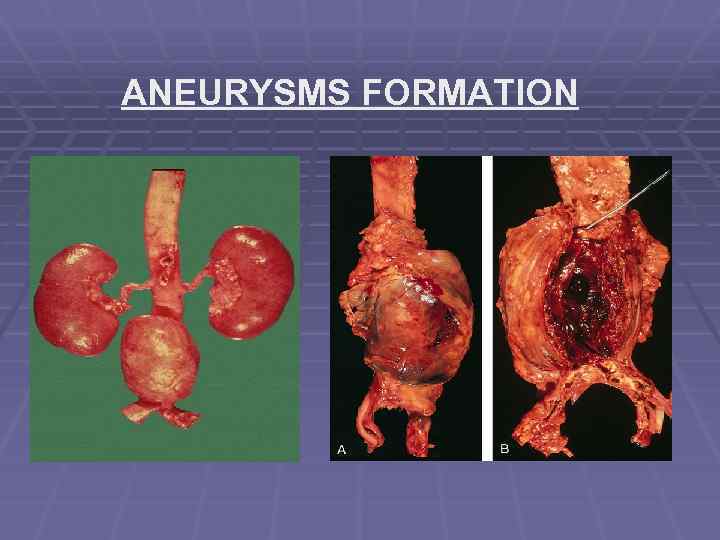
ANEURYSMS FORMATION

COMPLICATIONS
-: COMPLICATIONS: • Myocardial infarction • Cerebral infarction (stroke). • Aneurysm • Peripheral vascular disease (PVD).
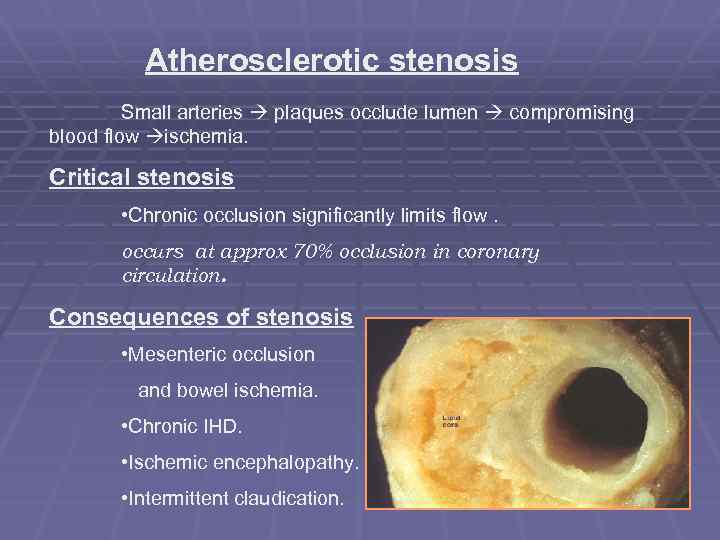
Atherosclerotic stenosis Small arteries plaques occlude lumen compromising blood flow ischemia. Critical stenosis • Chronic occlusion significantly limits flow. occurs at approx 70% occlusion in coronary circulation. Consequences of stenosis • Mesenteric occlusion and bowel ischemia. • Chronic IHD. • Ischemic encephalopathy. • Intermittent claudication.
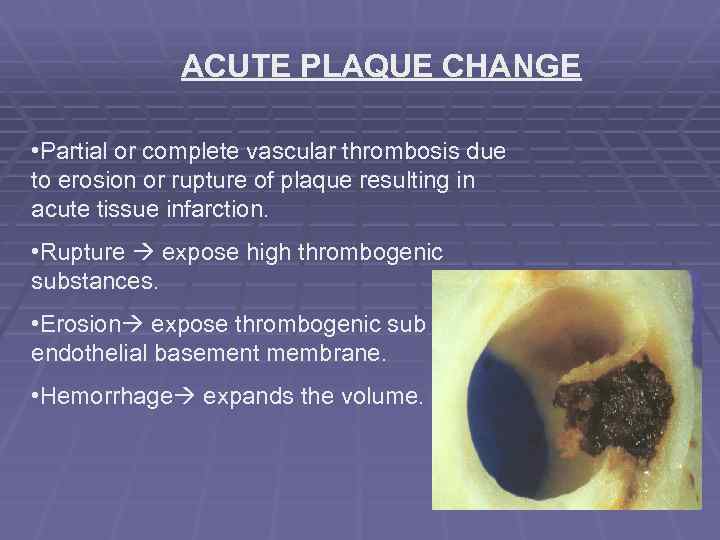
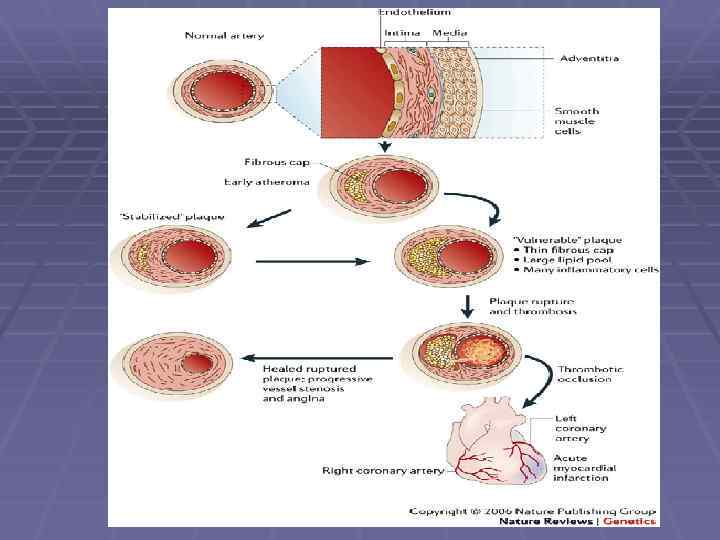
ACUTE PLAQUE CHANGE • Partial or complete vascular thrombosis due to erosion or rupture of plaque resulting in acute tissue infarction. • Rupture expose high thrombogenic substances. • Erosion expose thrombogenic sub endothelial basement membrane. • Hemorrhage expands the volume.
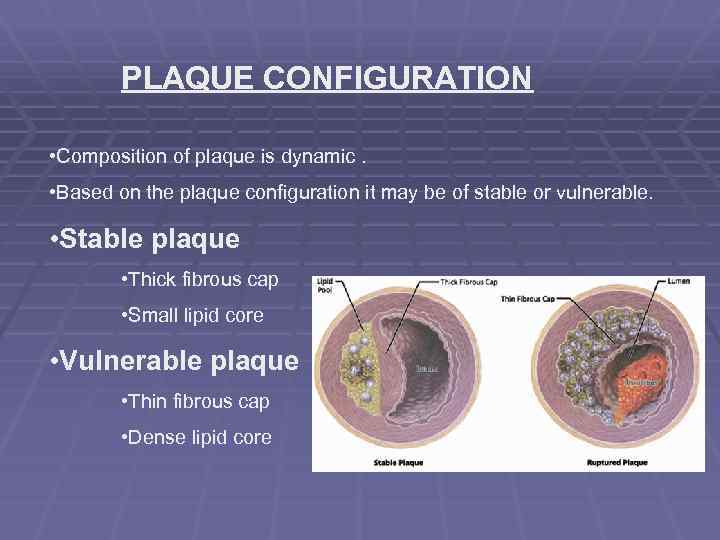
PLAQUE CONFIGURATION • Composition of plaque is dynamic. • Based on the plaque configuration it may be of stable or vulnerable. • Stable plaque • Thick fibrous cap • Small lipid core • Vulnerable plaque • Thin fibrous cap • Dense lipid core
EVENTS TRIGGERING CHANGES IN PLAQUE CONFIGURATION INTRINSIC FACTORS - plaque structure and composition Fibrous cap • Collagen (produced by smooth cells). • Collagen turnover is regulated by • Matrix metalloproteinase (macrophages within plaque), • Tissue inhibitors of metalloproteinase (endothelial cells, smooth muscle cells) EXTRINSIC FACTORS -BP and platelet activity. • adrenergic stimulation increase BP increasing physical stress.
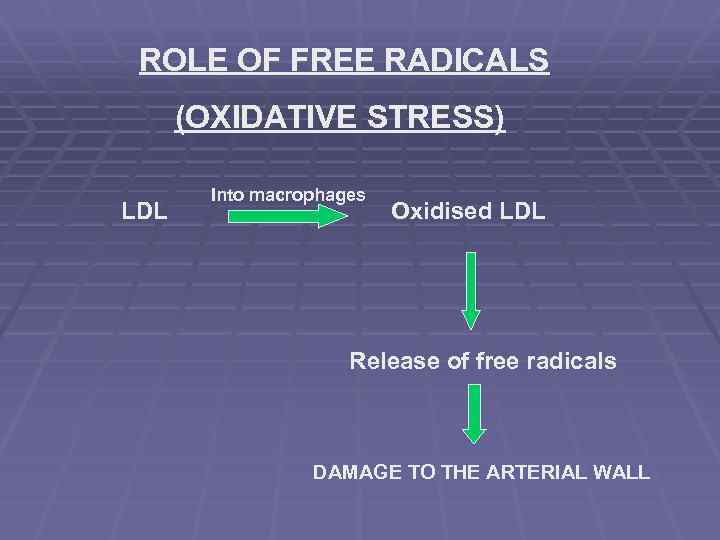
ROLE OF FREE RADICALS (OXIDATIVE STRESS) LDL Into macrophages Oxidised LDL Release of free radicals DAMAGE TO THE ARTERIAL WALL
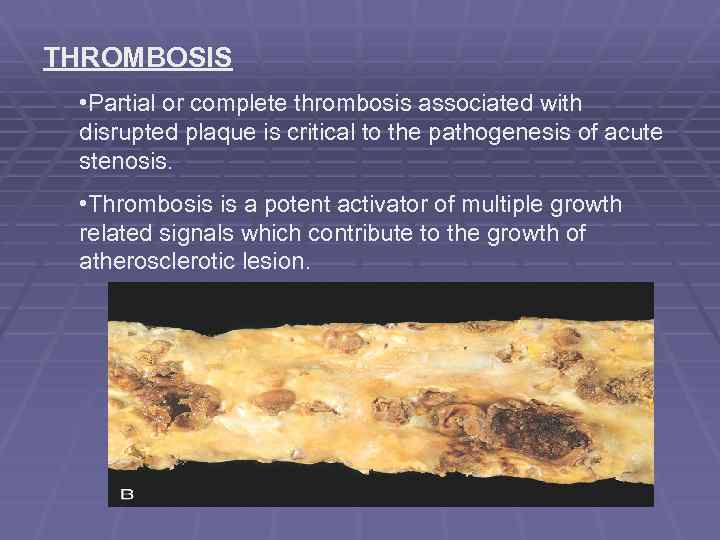
THROMBOSIS • Partial or complete thrombosis associated with disrupted plaque is critical to the pathogenesis of acute stenosis. • Thrombosis is a potent activator of multiple growth related signals which contribute to the growth of atherosclerotic lesion.
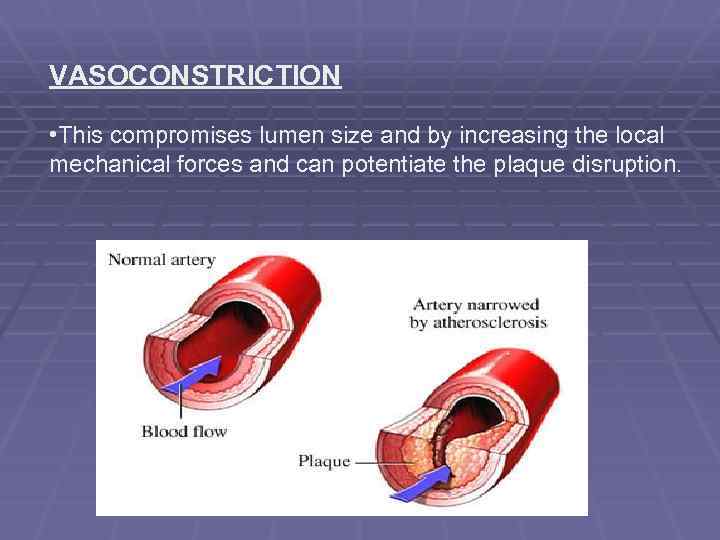
VASOCONSTRICTION • This compromises lumen size and by increasing the local mechanical forces and can potentiate the plaque disruption.
CLINICAL FEATURES ON CORONARY ARTERIES: • Angina • Hyperhidrosis • Shortness of breath • Palpitations • Tachycardia • Weakness or dizziness • Nausea ON CAROTID ARTERIES: • Transient ischemic attacks • Dizziness , Confusion , Fainting , Coma • Loss of eyesight • Hemiplegia.
ON PERIPHERAL ARTERIES: • Claudication is the most common symptom of this condition. • Pain • Coolness, numbness • Poor healing of wounds • Ulcers leading to Gangrene formation • Black discoloration

DIAGNOSIS
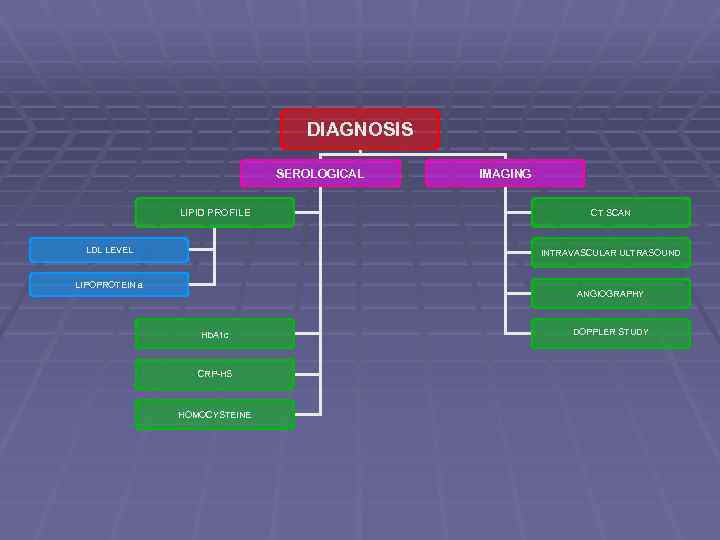
DIAGNOSIS SEROLOGICAL LIPID PROFILE LDL LEVEL IMAGING CT SCAN INTRAVASCULAR ULTRASOUND LIPOPROTEIN a ANGIOGRAPHY Hb. A 1 c CRP-HS HOMOCYSTEINE DOPPLER STUDY

TREATMENT
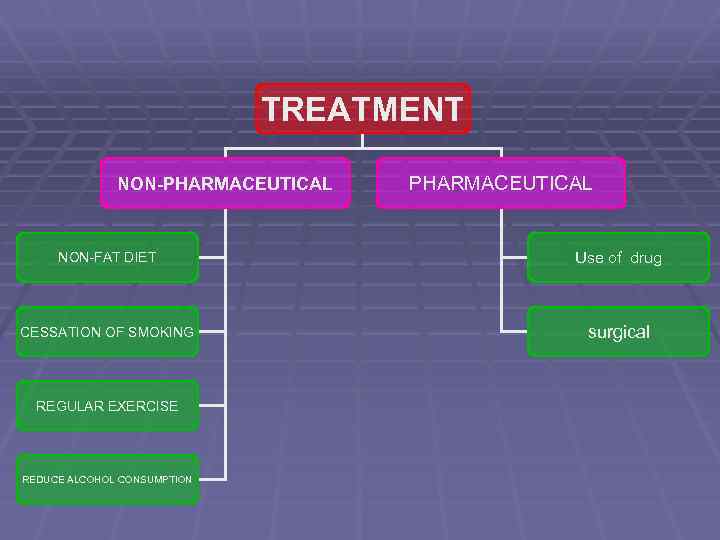
TREATMENT NON-PHARMACEUTICAL NON-FAT DIET Use of drug CESSATION OF SMOKING surgical REGULAR EXERCISE REDUCE ALCOHOL CONSUMPTION
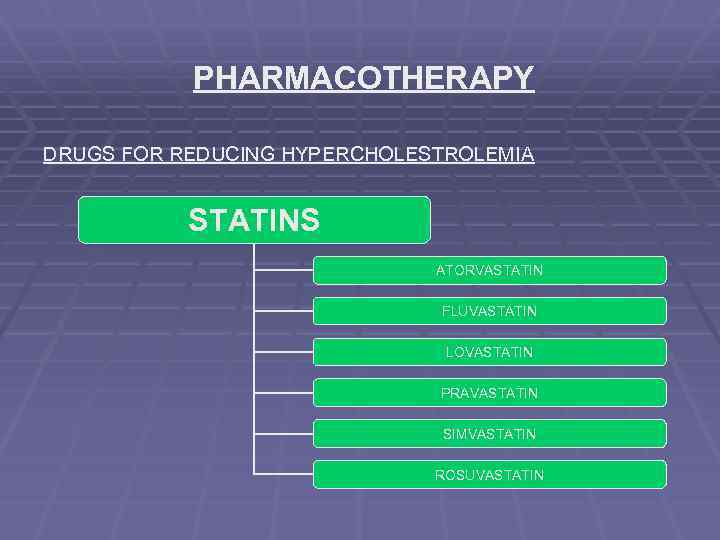
PHARMACOTHERAPY DRUGS FOR REDUCING HYPERCHOLESTROLEMIA STATINS ATORVASTATIN FLUVASTATIN LOVASTATIN PRAVASTATIN SIMVASTATIN ROSUVASTATIN
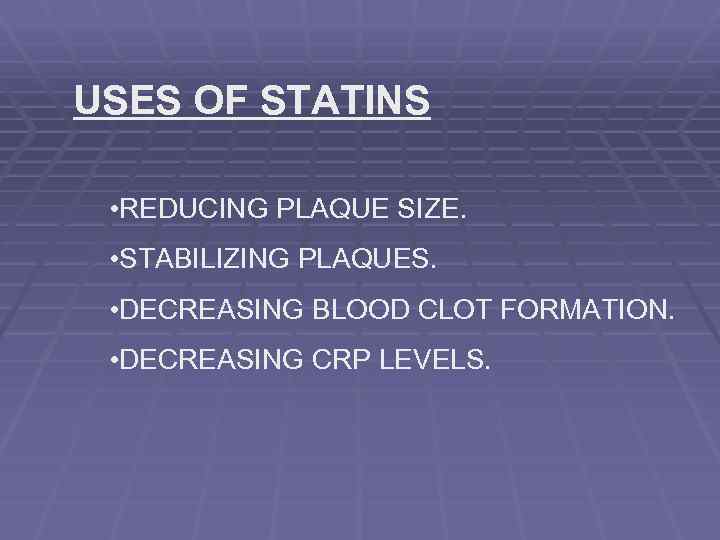
USES OF STATINS • REDUCING PLAQUE SIZE. • STABILIZING PLAQUES. • DECREASING BLOOD CLOT FORMATION. • DECREASING CRP LEVELS.
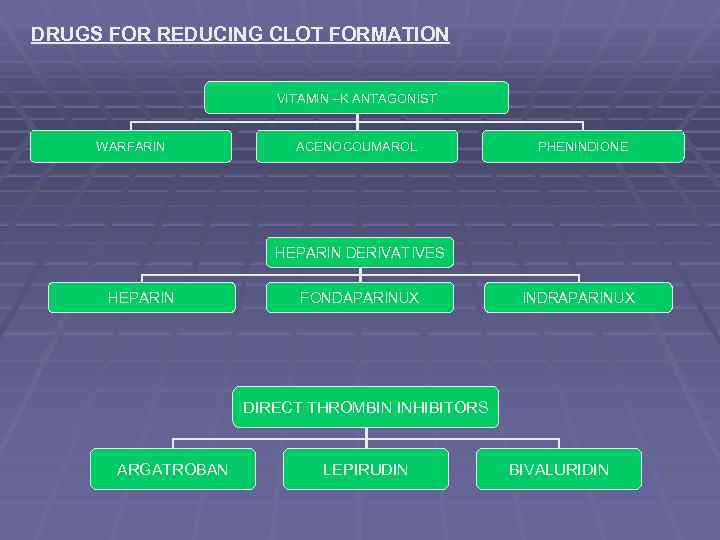
DRUGS FOR REDUCING CLOT FORMATION VITAMIN –K ANTAGONIST WARFARIN ACENOCOUMAROL PHENINDIONE HEPARIN DERIVATIVES HEPARIN FONDAPARINUX INDRAPARINUX DIRECT THROMBIN INHIBITORS ARGATROBAN LEPIRUDIN BIVALURIDIN
THE DRUGS THAT BREAKSDOWN THE BLOOD CLOT tissue plasminogen activator t-PA: alteplase (Activase) reteplase (Retavase) tenecteplase (TNKase) antistreplase (Eminase) streptokinase (Kabikinase, Streptase) urokinase (Abbokinase)
SURGICAL INTERVENTION • BALOON ANGIOPLASTY AND STENTING • ATHERECTOMY • SURGICAL BYPASS • ENDATERECTOMY

SUMMARY
MORPHOLOGY
MORPHOLOGY
COMPLICATIONS PERIPHERAL VASCULAR DISEASE MYOCARDIAL INFARCTION STROKE ANEURYSM FORMATION
COMPLICATIONS Atherosclerotic stenosis • Critical stenosis • Consequences of stenosis Acute plaque change • Stable plaque & vulnerable plaque • Factors that bring about the Change.

THANK YOU
s-110606075809-phpapp01.ppt