atherosclerosis-1231171492027331-2.ppt
- Количество слайдов: 36
 Atherosclerosis
Atherosclerosis
 Introduction l l A disease of the intima of large arteries Major degenerative disease of arteries Atherosclerotic lesions produce luminal narrowing, thrombosis, embolization, and occulation. Characterized by local accumulation of lipid in the vessel wall located either in the extracellular matrix or inside foam cells.
Introduction l l A disease of the intima of large arteries Major degenerative disease of arteries Atherosclerotic lesions produce luminal narrowing, thrombosis, embolization, and occulation. Characterized by local accumulation of lipid in the vessel wall located either in the extracellular matrix or inside foam cells.
 Thories of atherogenesis l l l Lipid insudation hypothesis Encrustation hypothesis Monoclonal hypothesis Infectious hypothesis Intima cell mass hypothesis Injury hypothesis
Thories of atherogenesis l l l Lipid insudation hypothesis Encrustation hypothesis Monoclonal hypothesis Infectious hypothesis Intima cell mass hypothesis Injury hypothesis
 Pathology
Pathology
 Pathologic hallmark l l l Atherosclerotic plaque Major components of plaque: smooth muscle cells, connective tissue (matrix), lipid, and inflammatory cells (predominantly macrophages) The presence of lipid within these lesions is a prominent distinguishing feature in comparison to other arteriopathies.
Pathologic hallmark l l l Atherosclerotic plaque Major components of plaque: smooth muscle cells, connective tissue (matrix), lipid, and inflammatory cells (predominantly macrophages) The presence of lipid within these lesions is a prominent distinguishing feature in comparison to other arteriopathies.
 Position of lesion l l commonly involved the infrarenal abdominal aorta, iliofemoral arteries (especially the superficial femoral artery), popliteal arteries, carotid bifurcation, and proximal coronary arteries Upper extremity vessels, as well as the common carotid, renal, and mesenteric arteries (beyond their origins), are also usually spared.
Position of lesion l l commonly involved the infrarenal abdominal aorta, iliofemoral arteries (especially the superficial femoral artery), popliteal arteries, carotid bifurcation, and proximal coronary arteries Upper extremity vessels, as well as the common carotid, renal, and mesenteric arteries (beyond their origins), are also usually spared.
 Risk Factors l Major Hyperlipidemia Ø Cigarette smoking Ø Hypertension Ø Diabetes Ø Positive family history Ø Hyperfibrinogenemia Ø Age Ø Homocysteinemia Ø
Risk Factors l Major Hyperlipidemia Ø Cigarette smoking Ø Hypertension Ø Diabetes Ø Positive family history Ø Hyperfibrinogenemia Ø Age Ø Homocysteinemia Ø
 Hypercholesterolemia l Studies have demonstrated a strong positive correlation between atherosclerotic cardiovascular disease and elevated total and LDL cholesterol and an equally strong negative correlation with HDL levels.
Hypercholesterolemia l Studies have demonstrated a strong positive correlation between atherosclerotic cardiovascular disease and elevated total and LDL cholesterol and an equally strong negative correlation with HDL levels.
 Cigarette smoking l The mechanism for the effects of smoking is likely to involve direct toxicity of tobacco metabolites on the vascular endothelium, probably by creating oxidant stress.
Cigarette smoking l The mechanism for the effects of smoking is likely to involve direct toxicity of tobacco metabolites on the vascular endothelium, probably by creating oxidant stress.
 Hypertension l another important independent risk factor for coronary atherosclerosis, with a continuous increase in relative risk associated with each increment of pressure.
Hypertension l another important independent risk factor for coronary atherosclerosis, with a continuous increase in relative risk associated with each increment of pressure.
 Diabetes l Diabetic patients are also at markedly increased risk for atherosclerosis, often manifesting a particularly virulent form of the disease, leading to higher rates of myocardial events, stroke, and amputation.
Diabetes l Diabetic patients are also at markedly increased risk for atherosclerosis, often manifesting a particularly virulent form of the disease, leading to higher rates of myocardial events, stroke, and amputation.
 Risk Factors l Minor Obesity ü Excessive alcohol use ü Sedentary lifestyle ü Male gender ü Hypercoagulable status ü Race ü
Risk Factors l Minor Obesity ü Excessive alcohol use ü Sedentary lifestyle ü Male gender ü Hypercoagulable status ü Race ü
 Clinical presentation l l l Arterial insufficiency Aneurysm formation embolism
Clinical presentation l l l Arterial insufficiency Aneurysm formation embolism
 Peripheral arterial insufficiency l Atherosclerotic plagues become large enough to narrow the arterial lumen and cause atherosclerosis occlusion
Peripheral arterial insufficiency l Atherosclerotic plagues become large enough to narrow the arterial lumen and cause atherosclerosis occlusion
 Definition l a complex, chronic inflammatory process that affects the elastic and muscular arteries. l Atherosclerotic plaques continuous progression and secondary thrombosis cause stricture or obstruction of arteries and often results in chronic or acute ischemic symptoms of lower limbs
Definition l a complex, chronic inflammatory process that affects the elastic and muscular arteries. l Atherosclerotic plaques continuous progression and secondary thrombosis cause stricture or obstruction of arteries and often results in chronic or acute ischemic symptoms of lower limbs
 Pathophysiology l Atherosclerotic plaques are dynamic lesions that may undergo progression or regression over time. Similarly, the underlying arterial wall also undergoes adaptive remodeling. l Arterial enlargement is a well-established feature of atherosclerosis and often results in relative preservation of luminal area until plaque volume reaches a threshold size (approximately 40% stenosis) beyond which compensation fails and lumen narrowing becomes progressive.
Pathophysiology l Atherosclerotic plaques are dynamic lesions that may undergo progression or regression over time. Similarly, the underlying arterial wall also undergoes adaptive remodeling. l Arterial enlargement is a well-established feature of atherosclerosis and often results in relative preservation of luminal area until plaque volume reaches a threshold size (approximately 40% stenosis) beyond which compensation fails and lumen narrowing becomes progressive.
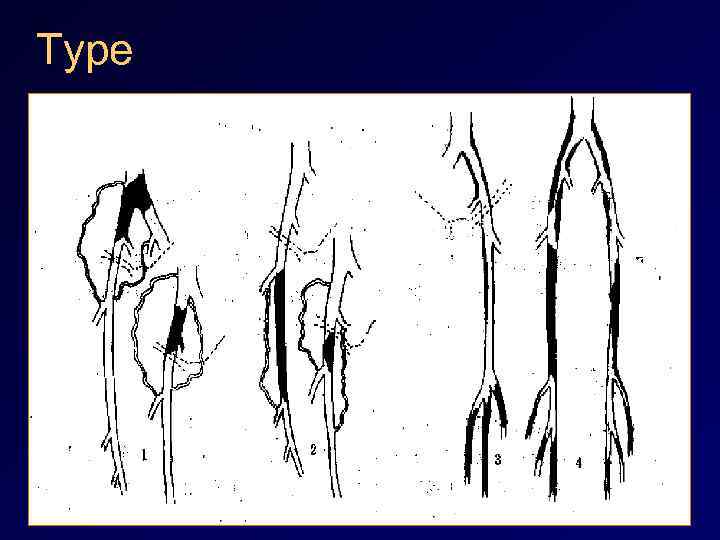 Type
Type
 Clinical manifestation l Intermittent claudication l Decreased amplitude of the pulses l Pallor of foot on elevation l Ischemic rest pain l Ulceration/ nonhealing of wounds l Atrophy and gangrene l Low ankel-brachial index (ABI)
Clinical manifestation l Intermittent claudication l Decreased amplitude of the pulses l Pallor of foot on elevation l Ischemic rest pain l Ulceration/ nonhealing of wounds l Atrophy and gangrene l Low ankel-brachial index (ABI)
 Intermittent claudication l l l Pain or fatigue in muscles of the lower extremity caused by walking and relieved by rest Typically, symptoms are completely relieved after 2 -5 minutes of inactivity Reproducible Does not occur at rest Commonly occurs in the calf muscles
Intermittent claudication l l l Pain or fatigue in muscles of the lower extremity caused by walking and relieved by rest Typically, symptoms are completely relieved after 2 -5 minutes of inactivity Reproducible Does not occur at rest Commonly occurs in the calf muscles
 Ischemic rest pain l l l Caused by ischemic neuritis and tissue necrosis Indicate an advanced stage of ischemia Localized to the vicinity of an ischemic ulcer or pregangrenous toe Aggravated by elevation of the extremity Relieved sometimes when patients stand erect, as gravity aids the delivery of arterial blood
Ischemic rest pain l l l Caused by ischemic neuritis and tissue necrosis Indicate an advanced stage of ischemia Localized to the vicinity of an ischemic ulcer or pregangrenous toe Aggravated by elevation of the extremity Relieved sometimes when patients stand erect, as gravity aids the delivery of arterial blood
 Ankel-brachial index (ABI) l l Determined by dividing the pressure obtained at the ankle by the brachial arterial pressure Normally, the ABI is 1. 0 or greater A value below 1. 0 indicates occlusive disease proximal to the point of measurement Rest pain usually appears when the ratio is 0. 3 or lower
Ankel-brachial index (ABI) l l Determined by dividing the pressure obtained at the ankle by the brachial arterial pressure Normally, the ABI is 1. 0 or greater A value below 1. 0 indicates occlusive disease proximal to the point of measurement Rest pain usually appears when the ratio is 0. 3 or lower
 Diagnosis l Noninvasive Hemodynamic Assessment ü segmental pressure technique ü Exercise (treadmill) testing ü Limb plethysmography l Doppler and Duplex Ultrasonography l Computed tomography angiography (CTA) l Magnetic resonance angiography (MRA) l Digital subtraction angiography (DSA)
Diagnosis l Noninvasive Hemodynamic Assessment ü segmental pressure technique ü Exercise (treadmill) testing ü Limb plethysmography l Doppler and Duplex Ultrasonography l Computed tomography angiography (CTA) l Magnetic resonance angiography (MRA) l Digital subtraction angiography (DSA)





 Treatment
Treatment
 Nonoperative treatment l l Lipid-lowering therapy Antiaggregation therapy ü Low MW dextrans: 500 ml iv qd ü Aispirin Antispasmodic, nacotic and artery dilated drugs ü Morphine and dolantin ü Sympathetic nerve blocker such as phentolamine ü PGE 1 Thrombolytic therapy ü urokinase
Nonoperative treatment l l Lipid-lowering therapy Antiaggregation therapy ü Low MW dextrans: 500 ml iv qd ü Aispirin Antispasmodic, nacotic and artery dilated drugs ü Morphine and dolantin ü Sympathetic nerve blocker such as phentolamine ü PGE 1 Thrombolytic therapy ü urokinase
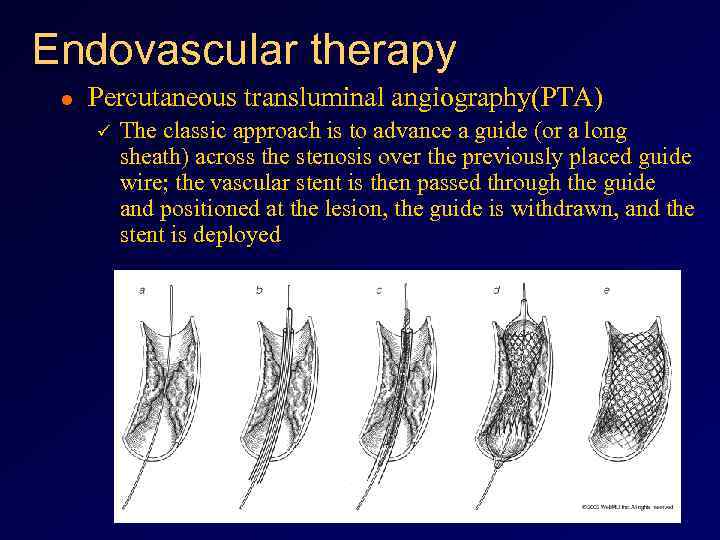 Endovascular therapy l Percutaneous transluminal angiography(PTA) ü The classic approach is to advance a guide (or a long sheath) across the stenosis over the previously placed guide wire; the vascular stent is then passed through the guide and positioned at the lesion, the guide is withdrawn, and the stent is deployed
Endovascular therapy l Percutaneous transluminal angiography(PTA) ü The classic approach is to advance a guide (or a long sheath) across the stenosis over the previously placed guide wire; the vascular stent is then passed through the guide and positioned at the lesion, the guide is withdrawn, and the stent is deployed
 Surgical treatment Endarterectomy l Angioplasty l Bypass grafting l Lumbar sympathectomy l Amputation l
Surgical treatment Endarterectomy l Angioplasty l Bypass grafting l Lumbar sympathectomy l Amputation l







