87ac868f6268d4c67d9729bd7bcbcaf5.ppt
- Количество слайдов: 52
Asthma By Ass. Prof. Dr. Abdul Hameed Al Qaseer
Asthma is a chronic inflammatory disease of airways that is characterized by increased responsiveness of the tracheobronchial tree to a multiplicity of stimuli. It is manifested physiologically by a widespread narrowing of the air passages , which may be relieved spontaneously or as a result of therapy, & clinically by paroxysms of dyspnea , cough , & wheezing.
Prevalence of Asthma is a very common disease. Current estimates suggest that 300 millions people world-wide suffer from asthma & additional 100 millions may be diagnosed with asthma by 2025. The prevalence of asthma is rising in many parts of the world e. g. in US the prevalence increased from 4 -5% to ~ 10 -12% of adult & 15% of children. The prevalence of asthma in UK ~ 7% in adults. There is no study to estimate the real prevalence in IRAQ !!
Prevalence ( cont. ): The mean prevalence of asthma in Middle East is about 5. 8%. In Kuwait 8. 5% ; Iran 5. 5% ; Turkey 7. 4% ; Saudi Arabia 5. 6%. Asthma more common in children , about One –half of cases develop before age 10. Another 1 3 occur before 40.
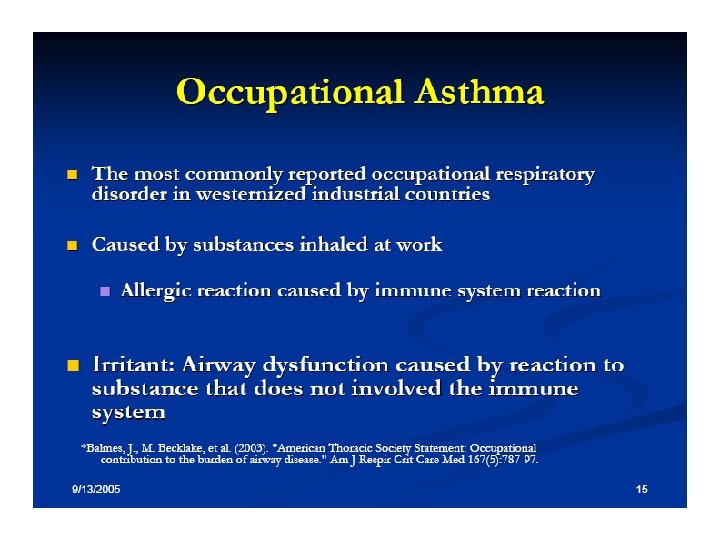
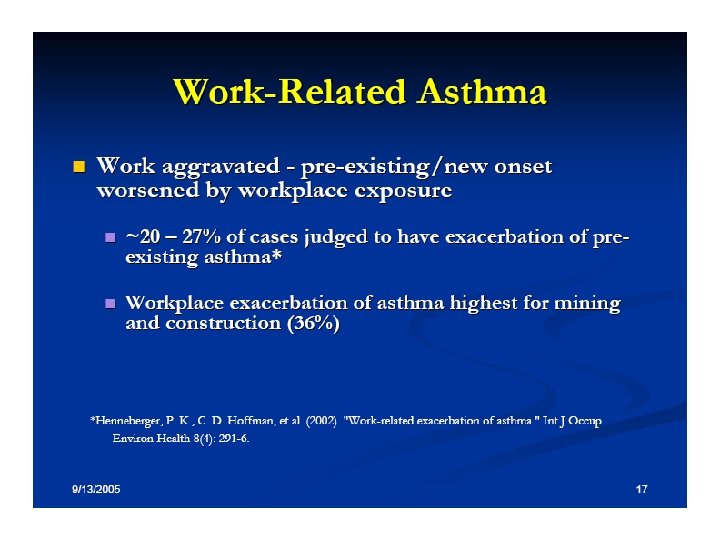
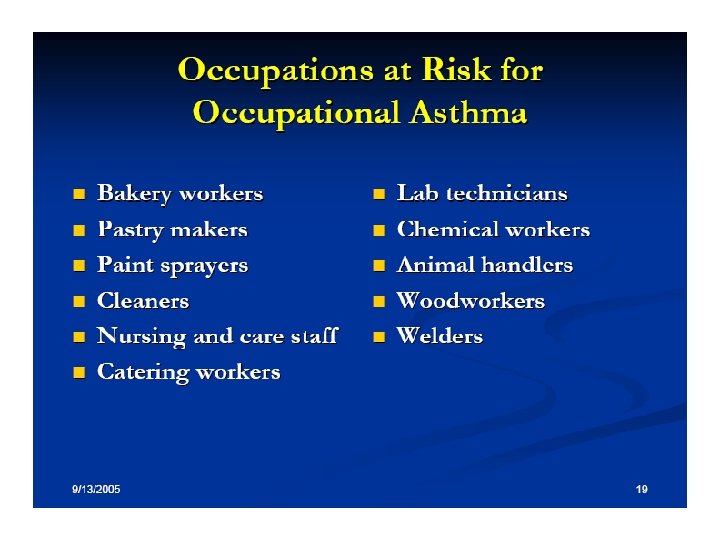
Etiology Of Asthma is a heterogeneous disease, genetic & environmental factors play a role. Environmental factors , such as viruses , occupational exposure , & allergens contribute to its initiation & continuance.
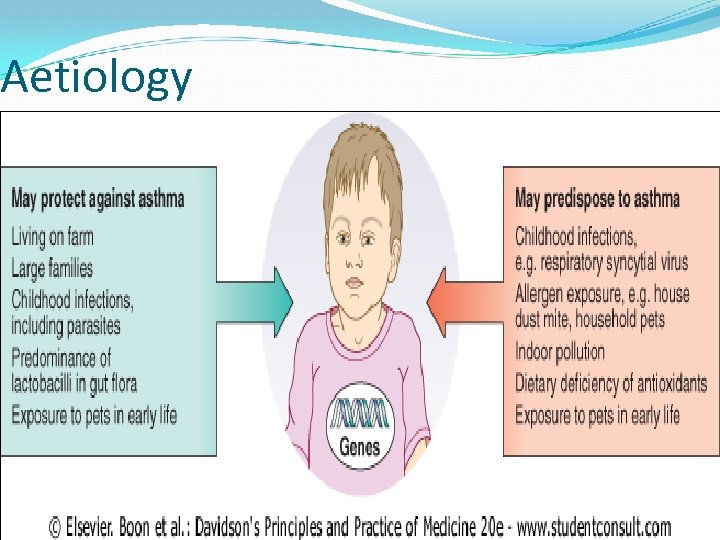
Aetiology
Classification Of Asthma 1. Allergic asthma ( atopic)( extrinsic) It is often associated with a personal &or family history of allergic disease + increased level of Ig. E in serum & or positive response to provocation test. It is usually early –onset & typically episodic. 2. Idiosyncratic asthma (non- atopic ) (intrinsic): 3. Many patients have disease not fit clearly into either of the above ( mixed group).
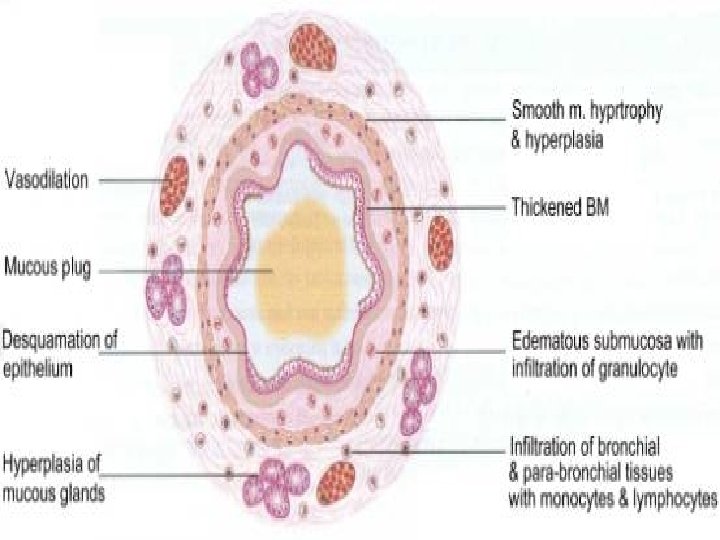
Pathogenesis Of Asthma results from a state of persistent subacute inflam mation of the airways. The airways are edematous & infiltrated with eosinophils( which seems to play an important role), neutrophils , & lymphocytes. Physiologic & clinical features of asthma derive from an interaction among the resident & infiltrating cells in the airways.
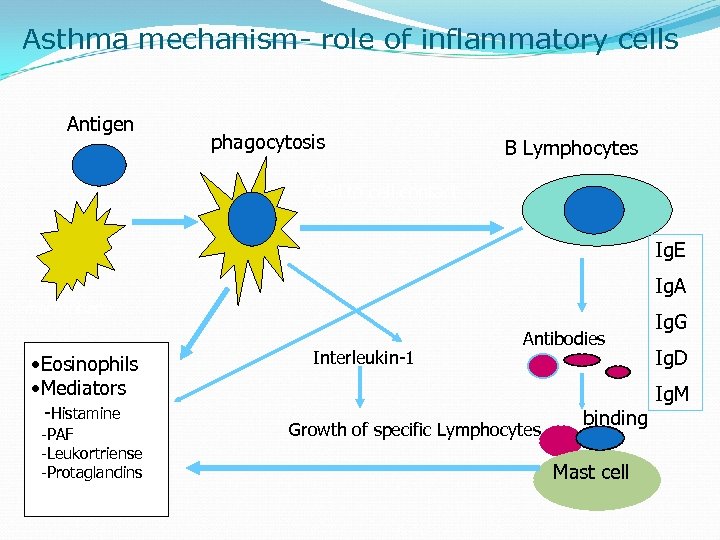
Asthma mechanism- role of inflammatory cells Antigen phagocytosis B Lymphocytes Cell to cell contact Ig. E Ig. A macrophage • Eosinophils • Mediators -Histamine -PAF -Leukortriense -Protaglandins Interleukin-1 Antibodies Growth of specific Lymphocytes binding Mast cell Ig. G Ig. D Ig. M
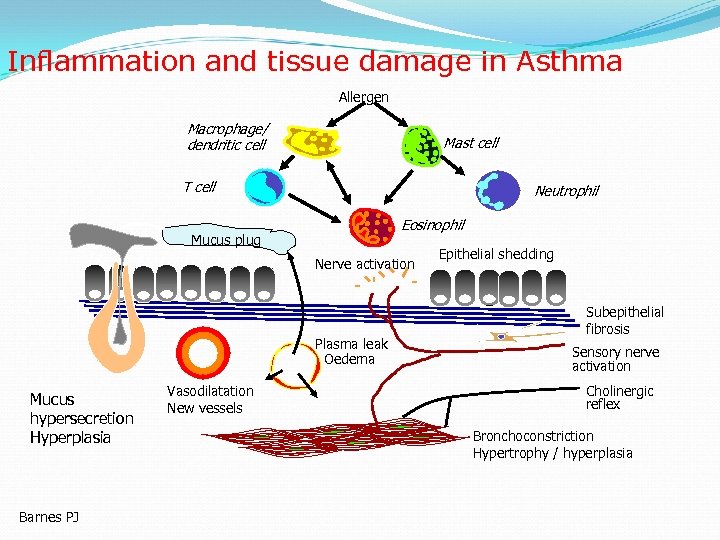
Inflammation and tissue damage in Asthma Allergen Macrophage/ dendritic cell Mast cell T cell Neutrophil Eosinophil Mucus plug Nerve activation Plasma leak Oedema Mucus hypersecretion Hyperplasia Barnes PJ Vasodilatation New vessels Epithelial shedding Subepithelial fibrosis Sensory nerve activation Cholinergic reflex Bronchoconstriction Hypertrophy / hyperplasia
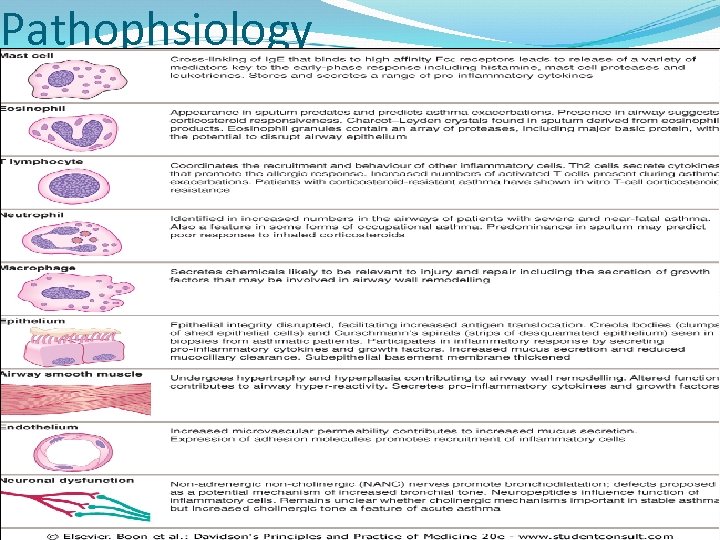
Pathophsiology
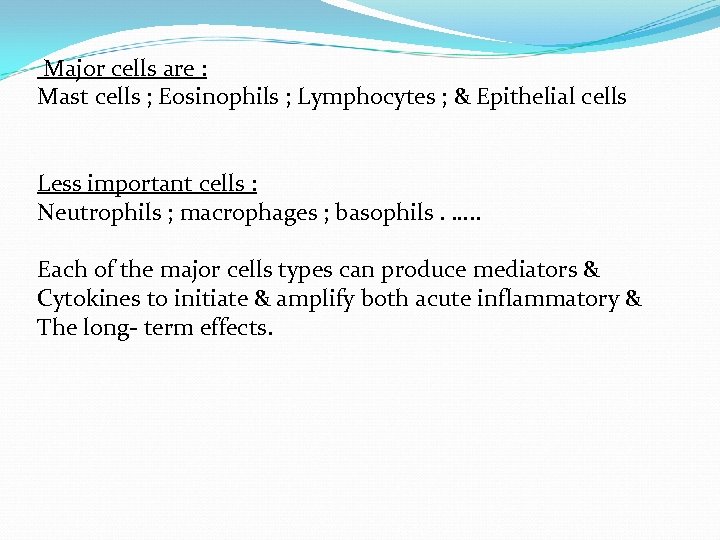
Major cells are : Mast cells ; Eosinophils ; Lymphocytes ; & Epithelial cells Less important cells : Neutrophils ; macrophages ; basophils. …. . Each of the major cells types can produce mediators & Cytokines to initiate & amplify both acute inflammatory & The long- term effects.
Mediators Histamine Leukotrienes Prostaglandins Thromboxane PAF Bradykinins Tachykinins Endothelins & Others
Mediators released produce an intense , immediate inflammatory reaction involving : 1. 2. 3. 4. 5. 6. Bronchoconstruction Vascular congestion Edema formation Increased mucus production Impaired mucociliary transport. Structural changes ( fibrosis , sm hyperplasia , angiogenesis , mucus hyperplasia)
Stimuli That Incite Asthma 1. 2. 3. 4. 5. 6. 7. Allergens: Pharmacologic Stimuli : Environment & Air Pollution : Occupational Factors : Infections : Exercise: Emotional : Coexisting conditions that can aggravate asthma like : 1. Rhinitis 2. sinusitis 3. GERD.
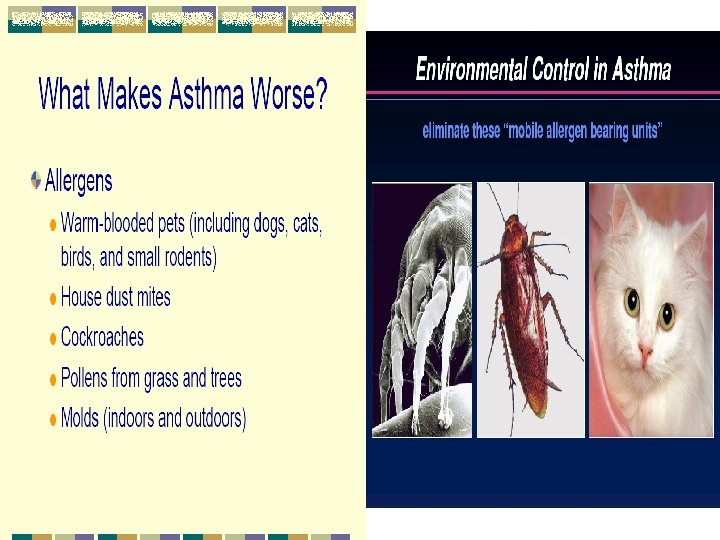
Allergens : Most of the allergens that provoke asthma are airborne. Immune mechanisms appear to be causally Related to the development of asthma in 2535% of all cases & contributory in ~ another 1 3. Important allergen such as house dusts mites, cat's allergen & pets , cockroach allergen. Smoking increase the risk of asthma (~ 4 x).
Aspirin-sensitive asthma Aspirin & other NSAID can result in asthma exacerbation in Some (~10%) patients. Most of such patients have severe Asthma & nasal polyps. The affected patients develop rhinorrhea & nasal congestion. They may benefit from leukotriene modifying agents. Other drugs e. g. B- blockers.
Exercise – induced Asthma Exercise is common precipitant of acute episodes of asthma. Typically the attacks follow exertion & do not occur during it. Short sprints are more likely to induce the episodes. The challenge test consist of a short ( 6 -8 min) exercise , & Spirometry is checked before & at 0, 5, 10, 15, 20, or 30 min. After exercise. A 20% decrease in FEV 1 confirms the Dx. Approximately 10% of the athletes on U. S. Olympic teams in recent years had exercise- induced asthma. It dose not evoke any long – term squeal , nor dose it incr ease airway reactivity.
Infections : Respiratory infections are the most common stimuli that evoke acute exacerbations of asthma Viruses & not bacteria are the major stimuli. In children RCV & parainfluenza virus are most important. In older children & adult , rhinovirus & influenza virus are the commonest.
Clinical Presentation Of Asthma Triad of cough + dyspnea + wheezing usually episodic. 2. Dry cough. 3. Exertional syspnea. 4. Asymptomatic 1.
DIAGNOSIS OF ASTHMA
Clinical features in adults that influence the probability of asthma ( from BTS 2008) MORE THAN ONE OF THE FOLLOWING SYMPTOMS : Wheeze , breathlessness , chest tightness , & cough , particularly if : * symptoms worse at night early morning * symptoms in response to exercise , allergens & cold air. * symptoms after taking aspirin or B-blockers.
History of atopic disorders. Family history of asthma or atopic disorders. Widespread wheeze on auscultation. Otherwise unexplained low FEV 1 or PEF. Otherwise unexplained peripheral eosinophilia.
Making a diagnosis of asthma -----------------------Compatible clinical history + ether or. FEV 1 >= 15% ( & 200 ml) increase following bronchodilator trial of corticosteroids. > 20% diurnal variation on > 3 days in a week for 2 weeks on PEF diary. FEV 1 >= 15 % decrease after 6 min of exercise --------------------------------GINA accepts an increased FEV 1 12%
Peak flow(PEFR) measurement The fastest flow rate of air during a forced expiration PEFR = 600 L/min in healthy adult male = 450 L /min in healthy female & children AM-PM variation in healthy person < 20% PEFM, easy to use, repeatable, inexpensive
Importance of long term peak flow measurements To establish diagnosis and treatment To assess severity of an exacerbation To assess response to treatment To evaluate how well asthma is controlled To alert patient to need for possible change in treatment
Other Diagnostic methods Enhanced bronchoconstriction( AHR) to a variety of direct Or indirect stimuli e. g. 1. Exercise 2. Cold air 3. Dusts , smoke , & chemicals. 4. Histamine & methacholine ( provocative test). 5. Challenge test using adenosine ( may be more specific).
Other investigations: 1. 2. 3. 4. 5. 6. Eosinophilia( sputum or blood) Ig. E ( total or specific). Skin tests Pulmonary function test ( for Dx & evaluations) CXR ABG.
Differential Diagnosis Of Asthma COMMON : 1. Acute bronchitis 2. Aspiration( foreign body) 3. Bronchial stenosis 4. Cardiac failure 5. Chronic bronchitis 6. Cystic fibrosis 7. Eosinophilic pneumonias
D. Dx ( cont. ) Uncommon : 1. Airway obstruction e. g. external or internal 2. Carcinoid syndrome 3. Pulmonary embolism 4. Systemic vasculitis 5. Endobronchial sarcoid 6. Systemic mastocytosis.
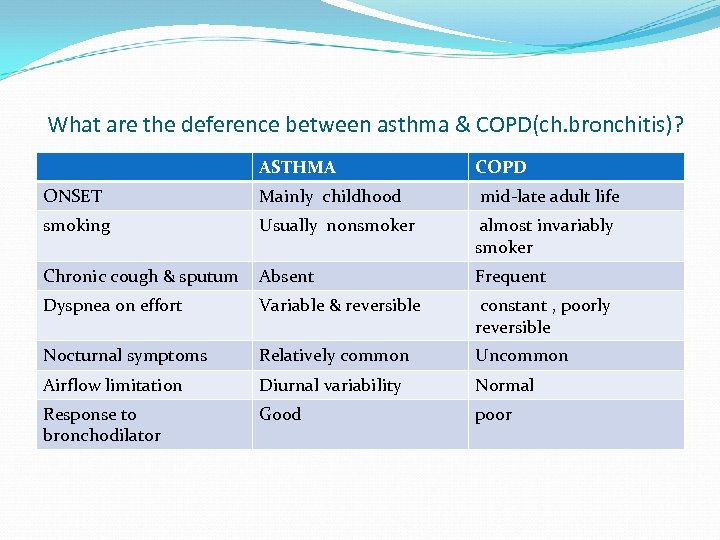
What are the deference between asthma & COPD(ch. bronchitis)? ASTHMA COPD ONSET Mainly childhood mid-late adult life smoking Usually nonsmoker almost invariably smoker Chronic cough & sputum Absent Frequent Dyspnea on effort Variable & reversible constant , poorly reversible Nocturnal symptoms Relatively common Uncommon Airflow limitation Diurnal variability Normal Response to bronchodilator Good poor
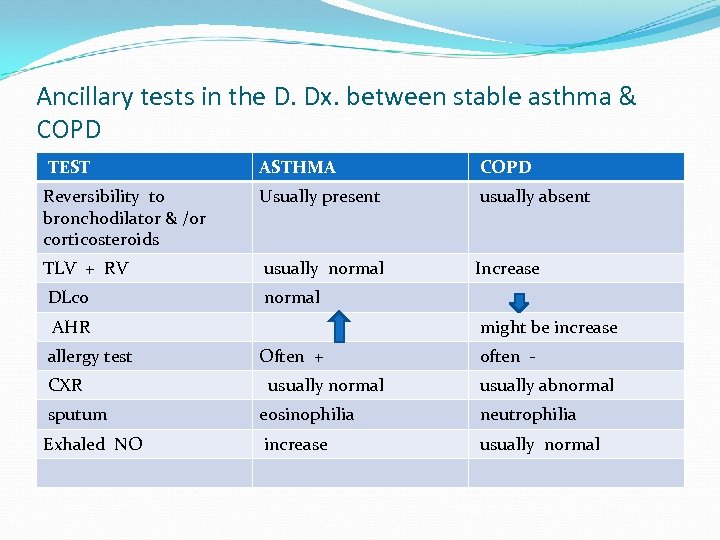
Ancillary tests in the D. Dx. between stable asthma & COPD TEST ASTHMA COPD Reversibility to bronchodilator & /or corticosteroids Usually present usually absent TLV + RV usually normal Increase DLco normal AHR allergy test CXR might be increase Often + usually normal often usually abnormal sputum eosinophilia neutrophilia Exhaled NO increase usually normal
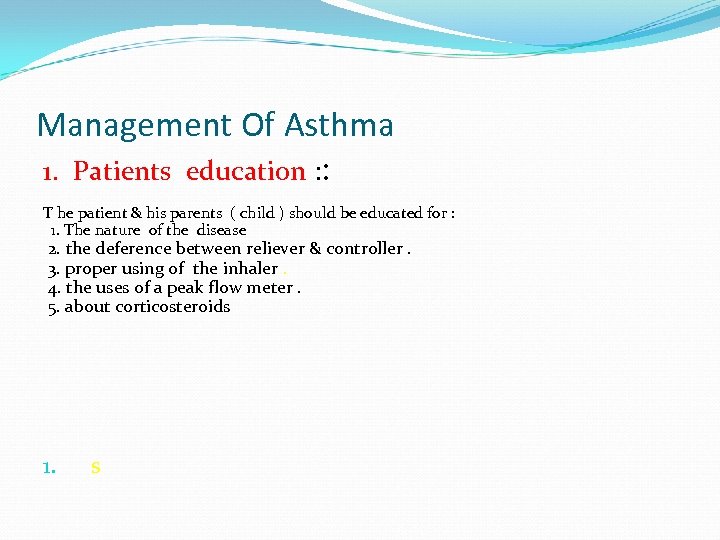
Management Of Asthma 1. Patients education : : T he patient & his parents ( child ) should be educated for : 1. The nature of the disease 2. the deference between reliever & controller. 3. proper using of the inhaler. 4. the uses of a peak flow meter. 5. about corticosteroids 1. s
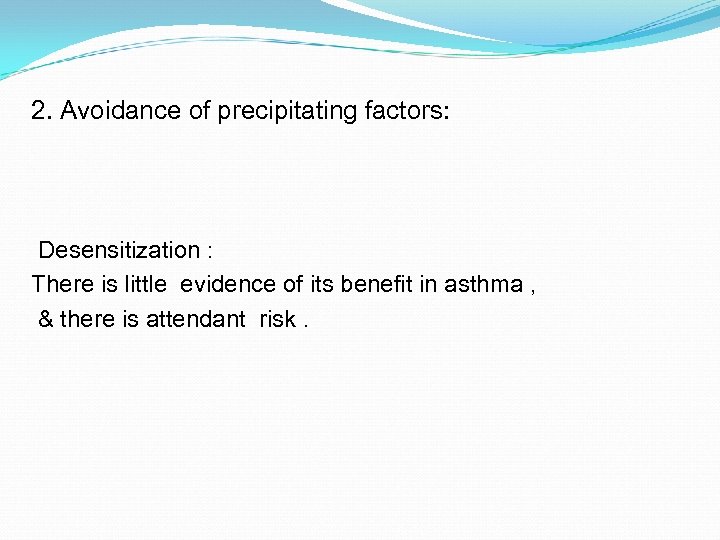
2. Avoidance of precipitating factors: Desensitization : There is little evidence of its benefit in asthma , & there is attendant risk.
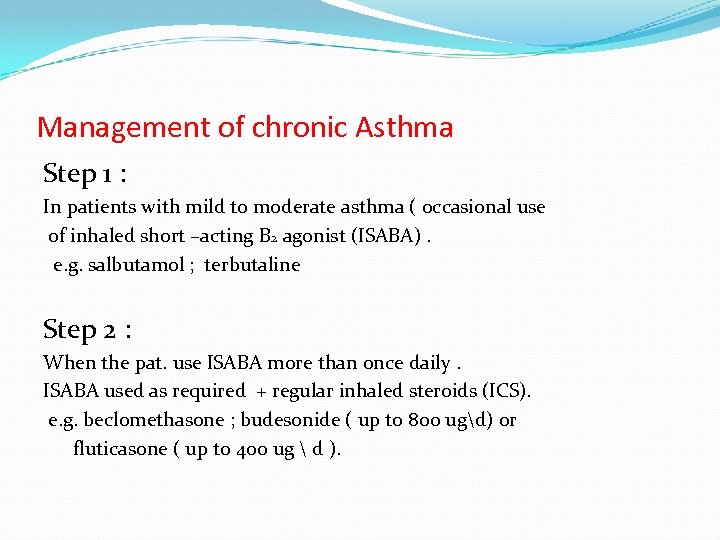
Management of chronic Asthma Step 1 : In patients with mild to moderate asthma ( occasional use of inhaled short –acting B 2 agonist (ISABA). e. g. salbutamol ; terbutaline Step 2 : When the pat. use ISABA more than once daily. ISABA used as required + regular inhaled steroids (ICS). e. g. beclomethasone ; budesonide ( up to 800 ugd) or fluticasone ( up to 400 ug d ).
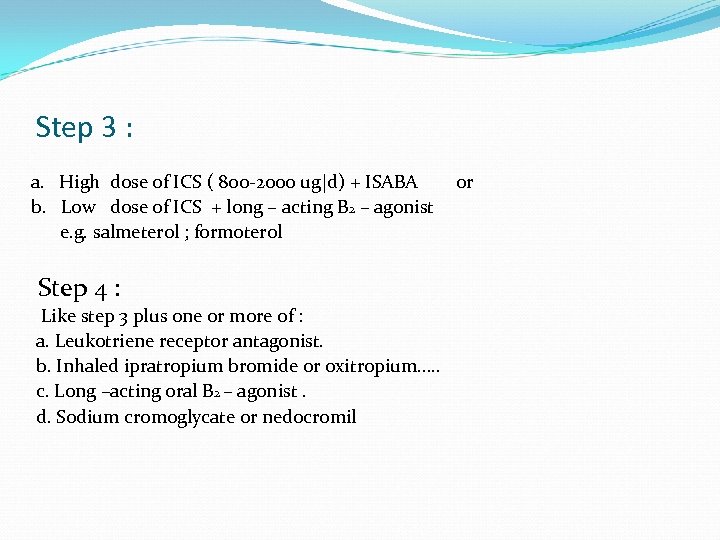
Step 3 : a. High dose of ICS ( 800 -2000 ug|d) + ISABA b. Low dose of ICS + long – acting B 2 – agonist e. g. salmeterol ; formoterol Step 4 : Like step 3 plus one or more of : a. Leukotriene receptor antagonist. b. Inhaled ipratropium bromide or oxitropium…. . c. Long –acting oral B 2 – agonist. d. Sodium cromoglycate or nedocromil or
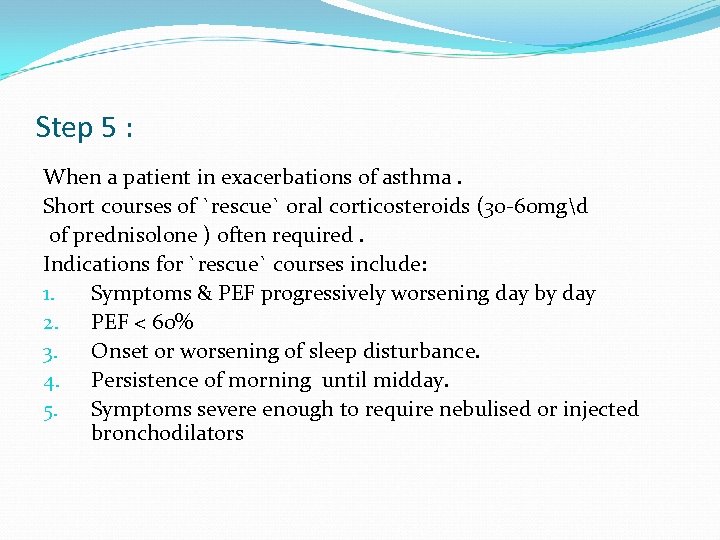
Step 5 : When a patient in exacerbations of asthma. Short courses of `rescue` oral corticosteroids (30 -60 mgd of prednisolone ) often required. Indications for `rescue` courses include: 1. Symptoms & PEF progressively worsening day by day 2. PEF < 60% 3. Onset or worsening of sleep disturbance. 4. Persistence of morning until midday. 5. Symptoms severe enough to require nebulised or injected bronchodilators
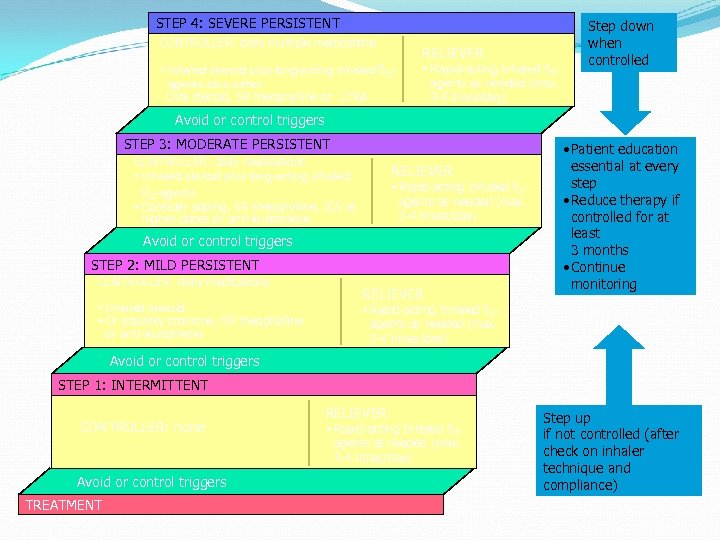
STEP 4: SEVERE PERSISTENT CONTROLLER: daily multiple medications RELIEVER • Inhaled steroid plus long-acting inhaled ß 2 agents plus either Oral steroid, SR theophylline or LTRA • Rapid-acting Inhaled ß 2 agents as needed (max. 3 -4 times/day) Step down when controlled Avoid or control triggers STEP 3: MODERATE PERSISTENT CONTROLLER: daily medications • Inhaled steroid plus long-acting inhaled ß 2 -agents • Consider adding, SR theophylline, ICS at higher doses or anti-leukotriene RELIEVER • Rapid-acting Inhaled ß 2 agents as needed (max. 3 -4 times/day) Avoid or control triggers STEP 2: MILD PERSISTENT CONTROLLER: daily medications • Inhaled steroid • Or possibly cromone, SR theophylline or anti-leukotriene RELIEVER • Patient education essential at every step • Reduce therapy if controlled for at least 3 months • Continue monitoring • Rapid-acting Inhaled ß 2 agents as needed (max. 3 -4 times/day) Avoid or control triggers STEP 1: INTERMITTENT CONTROLLER: none Avoid or control triggers TREATMENT RELIEVER • Rapid-acting Inhaled ß 2 agents as needed (max. 3 -4 times/day) Step up if not controlled (after check on inhaler technique and compliance)

Why don’t patients comply with treatment? Drug factors Difficulties with inhaler devices Too complex regimen e. g multiple doses or multiple drugs Side effects Cost of medication Dislike of medication(taste, odour or shape) Distant health services and pharmacies Non drug factors Misunderstanding or lack of instructions Dissatisfaction with health care professionals Poor supervision, training or follow-up Inappropriate expectations underestimation of severity Cultural issues Fear of addiction Attitude toward ill health religious issues
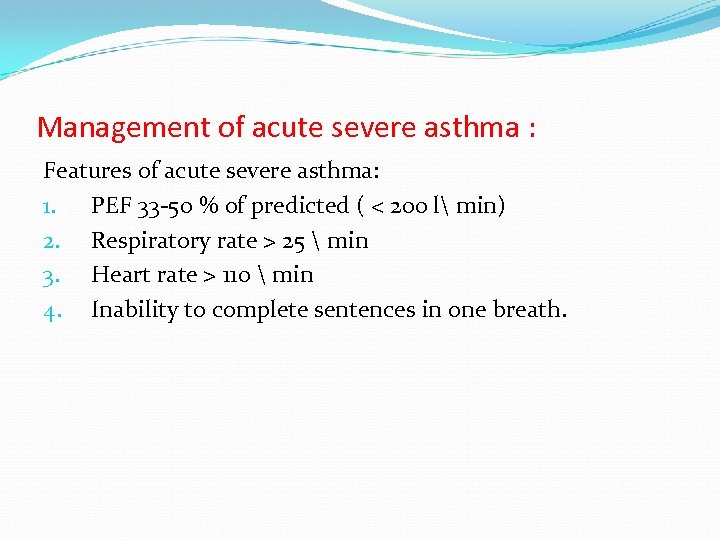
Management of acute severe asthma : Features of acute severe asthma: 1. PEF 33 -50 % of predicted ( < 200 l min) 2. Respiratory rate > 25 min 3. Heart rate > 110 min 4. Inability to complete sentences in one breath.
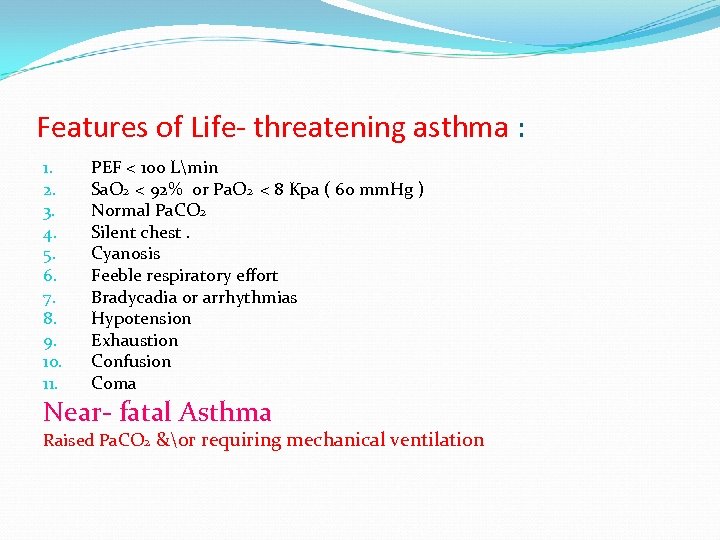
Features of Life- threatening asthma : 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. PEF < 100 Lmin Sa. O 2 < 92% or Pa. O 2 < 8 Kpa ( 60 mm. Hg ) Normal Pa. CO 2 Silent chest. Cyanosis Feeble respiratory effort Bradycadia or arrhythmias Hypotension Exhaustion Confusion Coma Near- fatal Asthma Raised Pa. CO 2 &or requiring mechanical ventilation
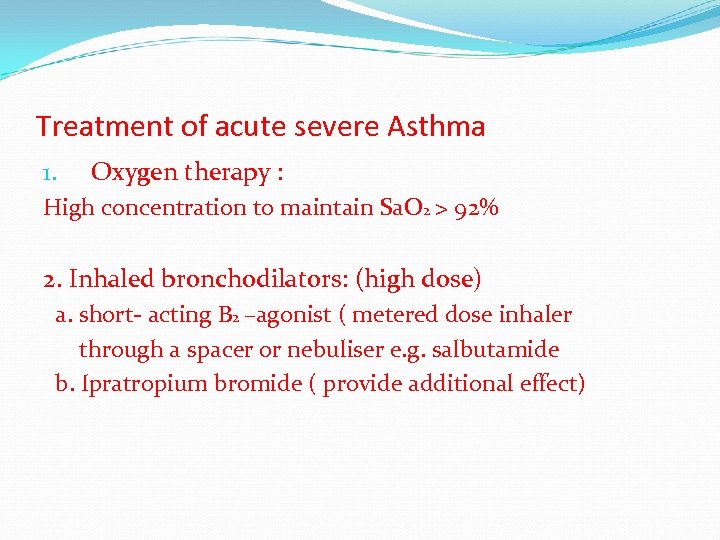
Treatment of acute severe Asthma 1. Oxygen therapy : High concentration to maintain Sa. O 2 > 92% 2. Inhaled bronchodilators: (high dose) a. short- acting B 2 –agonist ( metered dose inhaler through a spacer or nebuliser e. g. salbutamide b. Ipratropium bromide ( provide additional effect)
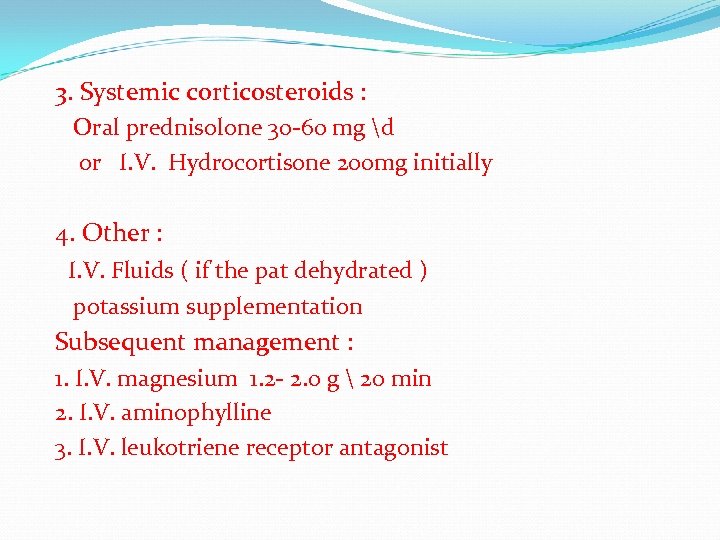
3. Systemic corticosteroids : Oral prednisolone 30 -60 mg d or I. V. Hydrocortisone 200 mg initially 4. Other : I. V. Fluids ( if the pat dehydrated ) potassium supplementation Subsequent management : 1. I. V. magnesium 1. 2 - 2. 0 g 20 min 2. I. V. aminophylline 3. I. V. leukotriene receptor antagonist
Monitoring of the patients 1. 2. 3. 4. PEF every 15 -30 min Pulse oximetry Arterial blood gases (ABG) CXR
Indications for assisted ventilation 1. 2. 3. Coma Respiratory arrest Deterioration of ABG Pa. O 2 < 8 Kpa Pa CO 2 > 6 kpa low PH 4. Exhaustion ; confusion ; drowsiness
Thank You
87ac868f6268d4c67d9729bd7bcbcaf5.ppt