c15dc76e2f02f47a89577b2201619bf3.ppt
- Количество слайдов: 21
 ASTHMA AND COPD 2015 Dr Dhaher Jameel Salih Al-habbo FRCP London UK Assistant Professor Department of Medicine. College of Mdicine University of Mosul
ASTHMA AND COPD 2015 Dr Dhaher Jameel Salih Al-habbo FRCP London UK Assistant Professor Department of Medicine. College of Mdicine University of Mosul
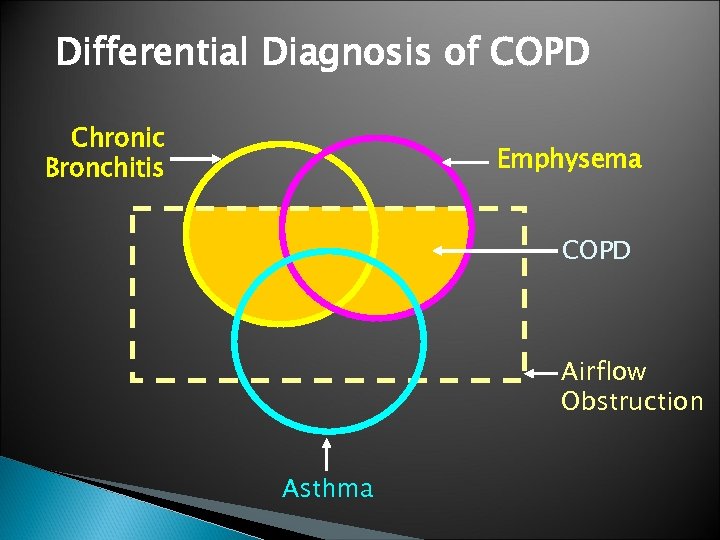 Differential Diagnosis of COPD Chronic Bronchitis Emphysema COPD Airflow Obstruction Asthma
Differential Diagnosis of COPD Chronic Bronchitis Emphysema COPD Airflow Obstruction Asthma
 asthma and allergic asthma
asthma and allergic asthma
 Asthma Chronic Inflammatory disorder of Bronchi characterized by , Episodic, reversable Brochospasm resulting from an exagurated Bronchconsrector response to a various stimuli(allergy). Affects 10% of children& 5 -7% adults
Asthma Chronic Inflammatory disorder of Bronchi characterized by , Episodic, reversable Brochospasm resulting from an exagurated Bronchconsrector response to a various stimuli(allergy). Affects 10% of children& 5 -7% adults
 Pathophysiology; Genetic susceptibility 1 -Childhood asthma occurs in atopic individuals who produce Ig. E on exposure to small amounts of common antigen. 2 -Asthma in adults is called non-atopic, intrinsic or late-onset asthma. 3 -First degree relatives of asthmatics have higher prevalence for asthma.
Pathophysiology; Genetic susceptibility 1 -Childhood asthma occurs in atopic individuals who produce Ig. E on exposure to small amounts of common antigen. 2 -Asthma in adults is called non-atopic, intrinsic or late-onset asthma. 3 -First degree relatives of asthmatics have higher prevalence for asthma.
 Pathophysiology; Environmental factors 1 -Indoor environment and childhood exposure to allergen is very important in determining sensitization. 2 -House dust mites and pet-derived allergens are wide spread in houses. 3 -Fungal spores, cockroach antigens and nitrogen dioxide (gas cockers). Environmental factors ; Out door like ; ozone, sulphur dioxide and air-borne particles, smoking, Drugs and infection.
Pathophysiology; Environmental factors 1 -Indoor environment and childhood exposure to allergen is very important in determining sensitization. 2 -House dust mites and pet-derived allergens are wide spread in houses. 3 -Fungal spores, cockroach antigens and nitrogen dioxide (gas cockers). Environmental factors ; Out door like ; ozone, sulphur dioxide and air-borne particles, smoking, Drugs and infection.
 Asthma Pathogenetic Types Extrinsic (Allergic/Immune) ◦ Atopic - Ig. E ◦ Occupational - Ig. G ◦ A. Bronchopulomonary Aspergillosis - Ig. E Intrinsic (Non immune) ◦ Aspirin induced ◦ Infections induced
Asthma Pathogenetic Types Extrinsic (Allergic/Immune) ◦ Atopic - Ig. E ◦ Occupational - Ig. G ◦ A. Bronchopulomonary Aspergillosis - Ig. E Intrinsic (Non immune) ◦ Aspirin induced ◦ Infections induced
 Pathology Inhaled allergen rapidly interacts with mucosal mast cells (Ig. E-Dependent mechanism). This will results in histamine and leukotrienes release leading to bronchoconstriction. Airway edema, increased volume and size of sub mucosal glands. desquamation of airway epithelial cells.
Pathology Inhaled allergen rapidly interacts with mucosal mast cells (Ig. E-Dependent mechanism). This will results in histamine and leukotrienes release leading to bronchoconstriction. Airway edema, increased volume and size of sub mucosal glands. desquamation of airway epithelial cells.
 Clinical features 1 -Wheeze, breathlessness, cough, and sensation of chest tightness usually episodic especially in children and atopic. 2 -chronic and persistent wheeze is more common in older non-atopic patients with adult asthma and it may be difficult to be differentiated from COPD.
Clinical features 1 -Wheeze, breathlessness, cough, and sensation of chest tightness usually episodic especially in children and atopic. 2 -chronic and persistent wheeze is more common in older non-atopic patients with adult asthma and it may be difficult to be differentiated from COPD.
 Clinical features cont… 3 -Typically, there is diurnal variation in symptoms and peak expiratory flow measurement being worse in the early morning. Cough and wheeze usually disturb the patient sleep (Nocturnal asthma). There may be cough with no wheezes (cough variant asthma). 4 -Symptoms may provoked by exercise (exercise-induced asthma).
Clinical features cont… 3 -Typically, there is diurnal variation in symptoms and peak expiratory flow measurement being worse in the early morning. Cough and wheeze usually disturb the patient sleep (Nocturnal asthma). There may be cough with no wheezes (cough variant asthma). 4 -Symptoms may provoked by exercise (exercise-induced asthma).
 Clinical features cont… 5 -Acute sever asthma: Patient usually extremely distressed, using accessory muscles of respiration, the chest is inflated and the patient is tachypnoeic. Pulsus paradoxus (loss of pulse pressure on inspiration due to reduce cardiac return due to sever hyperinflation) and sweating. Central cyanosis in sever cases with silent chest and bradycardia.
Clinical features cont… 5 -Acute sever asthma: Patient usually extremely distressed, using accessory muscles of respiration, the chest is inflated and the patient is tachypnoeic. Pulsus paradoxus (loss of pulse pressure on inspiration due to reduce cardiac return due to sever hyperinflation) and sweating. Central cyanosis in sever cases with silent chest and bradycardia.
 Investigations Spirometric measurement of FEV 1/VC ratio or PEF before and after bronchodilators provide reliable indication of the degree of airflow obstruction, relation to exercise &the reversibility after bronchodilators. Radiological. Arterial Blood Gas analysis(ABGA)
Investigations Spirometric measurement of FEV 1/VC ratio or PEF before and after bronchodilators provide reliable indication of the degree of airflow obstruction, relation to exercise &the reversibility after bronchodilators. Radiological. Arterial Blood Gas analysis(ABGA)
 Management 1 -Patient education: A-The patient should be able to differentiate between reliever (bronchodilators) and preventer (anti-inflammatory) medications B-The patient should be fully capable of using the inhaler devices. C- The patient should be fully capable of using the peak flow meter, to understand the readings, to determine his personal best measurement and to record all these information in his personal action plan.
Management 1 -Patient education: A-The patient should be able to differentiate between reliever (bronchodilators) and preventer (anti-inflammatory) medications B-The patient should be fully capable of using the inhaler devices. C- The patient should be fully capable of using the peak flow meter, to understand the readings, to determine his personal best measurement and to record all these information in his personal action plan.
 Rescue short-course oral corticosteroid treatment The rescue course is in the form of *- 30 -60 mg prednisolone orally daily *-Continue as single morning dose until 2 days after good control of the symptoms. *-Tapering the dose to withdraw is required only if we continue treatment for 3 weeks and more.
Rescue short-course oral corticosteroid treatment The rescue course is in the form of *- 30 -60 mg prednisolone orally daily *-Continue as single morning dose until 2 days after good control of the symptoms. *-Tapering the dose to withdraw is required only if we continue treatment for 3 weeks and more.
 Immediate treatment of Acute sever Asthma A- Oxygen should be given at the highest concentration. To maintain a Pa. O 2 of >8. 5 -9 KPa. B-High dose of inhaled 2 -adrenoceptor agonist nebulised using oxygen (salbutamol 2. 5 -5 mgor terbutaline 5 -10 mg) repeated within 30 minutes if necessary. Inhaled 2 -adrenoceptor agonist can be given out side hospital by large volume spacers. C-Systemic steroids; 30 -60 mg prednisolone orally or intravenous 200 mg hydrocortisone.
Immediate treatment of Acute sever Asthma A- Oxygen should be given at the highest concentration. To maintain a Pa. O 2 of >8. 5 -9 KPa. B-High dose of inhaled 2 -adrenoceptor agonist nebulised using oxygen (salbutamol 2. 5 -5 mgor terbutaline 5 -10 mg) repeated within 30 minutes if necessary. Inhaled 2 -adrenoceptor agonist can be given out side hospital by large volume spacers. C-Systemic steroids; 30 -60 mg prednisolone orally or intravenous 200 mg hydrocortisone.
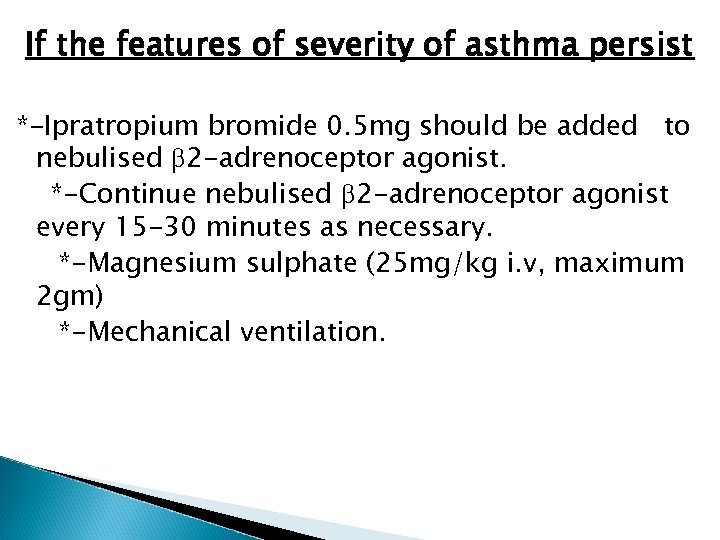 If the features of severity of asthma persist *-Ipratropium bromide 0. 5 mg should be added to nebulised 2 -adrenoceptor agonist. *-Continue nebulised 2 -adrenoceptor agonist every 15 -30 minutes as necessary. *-Magnesium sulphate (25 mg/kg i. v, maximum 2 gm) *-Mechanical ventilation.
If the features of severity of asthma persist *-Ipratropium bromide 0. 5 mg should be added to nebulised 2 -adrenoceptor agonist. *-Continue nebulised 2 -adrenoceptor agonist every 15 -30 minutes as necessary. *-Magnesium sulphate (25 mg/kg i. v, maximum 2 gm) *-Mechanical ventilation.
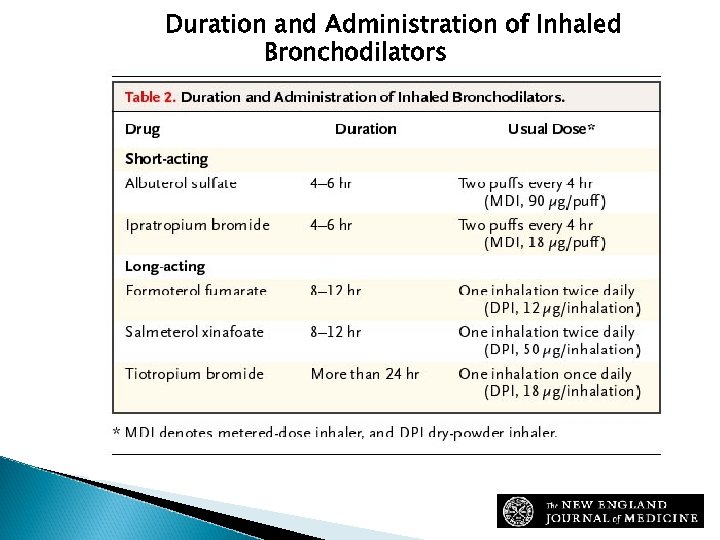 Duration and Administration of Inhaled Bronchodilators Sutherland, E. R. et al. N Engl J Med 2004; 350: 2689 -2697
Duration and Administration of Inhaled Bronchodilators Sutherland, E. R. et al. N Engl J Med 2004; 350: 2689 -2697





