d79d451800186794fd0cb1328cac9f66.ppt
- Количество слайдов: 35
Asthma and Bronchiectasis Branislava Milenkovic Professor of Internal/Respiratory Medicine, University of Belgrade Deputy Director of Clinic for Pulmonary Diseases, Clinical Center of Serbia, Belgrade, Serbia
Disclosures 2010 - 2017 Branislava Milenkovic Lectures: Astra. Zeneca, Boehringer Ingelheim, Chiesi, Glaxo. Smith. Kline, Novartis, Takeda, TEVA Consultancy or national/regional Advisory Boards: Astra. Zeneca, Boehringer Ingelheim, Glaxo. Smith. Kline, Novartis Educational programmes: no Industry-sponsored grants (Institution): no
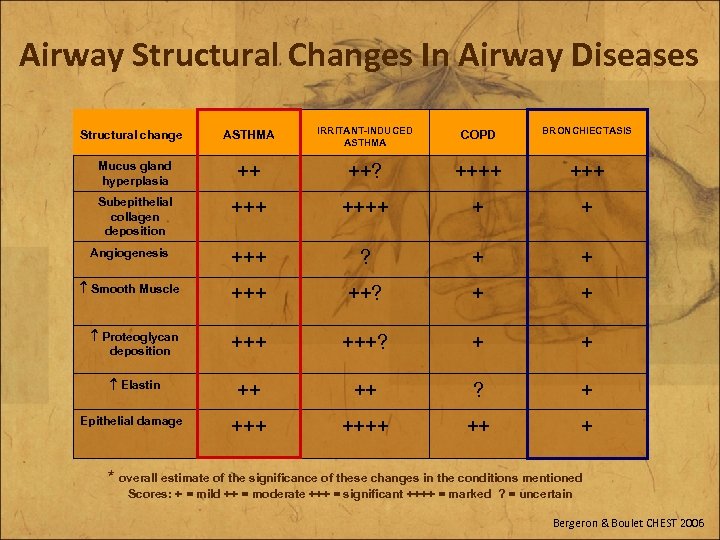
Airway Structural Changes In Airway Diseases ASTHMA IRRITANT-INDUCED ASTHMA COPD BRONCHIECTASIS ++ ++? ++++ +++ + + Angiogenesis +++ ? + + Smooth Muscle +++ ++? + + Proteoglycan deposition +++? + + Elastin ++ ++ ? + ++++ ++ + Structural change Mucus gland hyperplasia Subepithelial collagen deposition Epithelial damage * overall estimate of the significance of these changes in the conditions mentioned Scores: + = mild ++ = moderate +++ = significant ++++ = marked ? = uncertain Bergeron & Boulet CHEST 2006
• Bronchiectasis (and asthma) • Asthma (and bronchiectasis) Asthma Bronchiectasis
Bronchiectasis - Comorbidities • Common among bronchiectasis patients at any stage of the disease • Limited data regarding prevalence and impact on disease outcomes • Single disease approach ineffective • Given ageing population, number of comorbidities likely to increase • Associated increase in healthcare costs Adapted from Do. H document: A framework of principles for system wide action on comorbidity
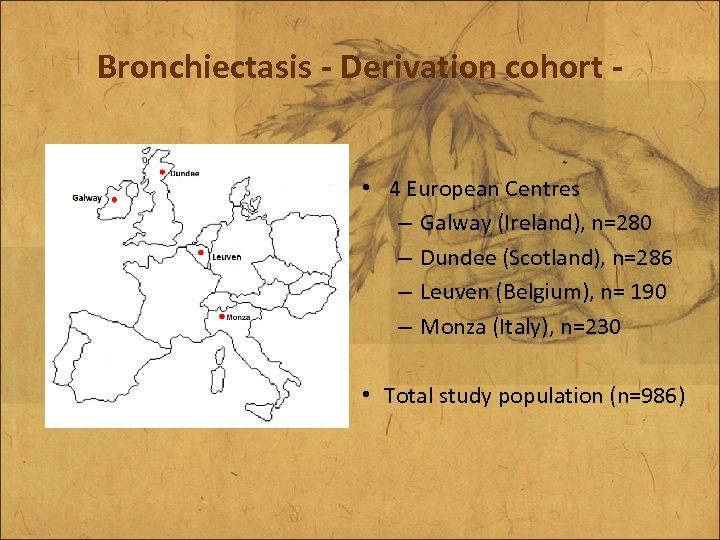
Bronchiectasis - Derivation cohort • 4 European Centres – Galway (Ireland), n=280 – Dundee (Scotland), n=286 – Leuven (Belgium), n= 190 – Monza (Italy), n=230 • Total study population (n=986)
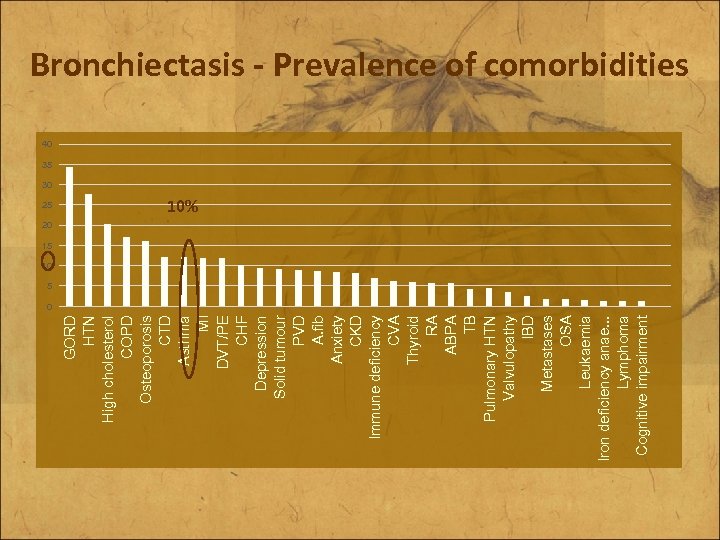
25 GORD HTN High cholesterol COPD Osteoporosis CTD Asthma MI DVT/PE CHF Depression Solid tumour PVD A. fib Anxiety CKD Immune deficiency CVA Thyroid RA ABPA TB Pulmonary HTN Valvulopathy IBD Metastases OSA Leukaemia Iron deficiency anae. . . Lymphoma Cognitive impairment Bronchiectasis - Prevalence of comorbidities 40 35 30 10% 20 15 10 5 0
Bronchiectasis (and asthma) A woman with intractable asthma E-mail: branislava. milenkovic@kcs. ac. rs
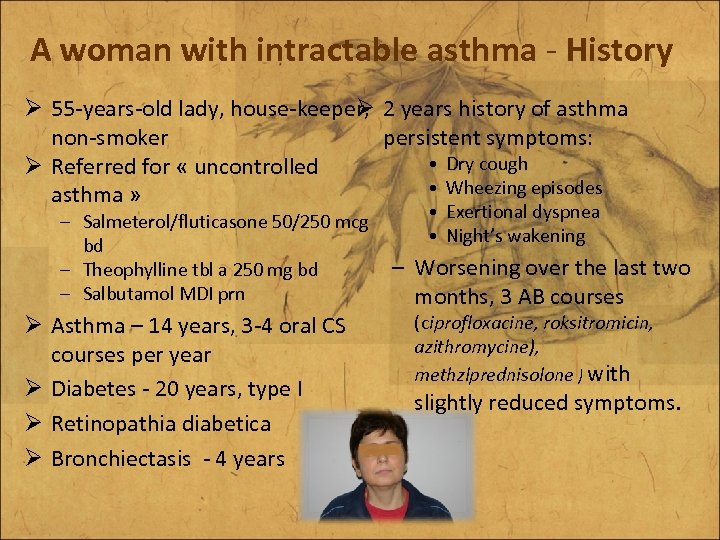
A woman with intractable asthma - History Ø 55 -years-old lady, house-keeper, 2 years history of asthma Ø non-smoker persistent symptoms: • Dry cough Ø Referred for « uncontrolled • Wheezing episodes asthma » • Exertional dyspnea – Salmeterol/fluticasone 50/250 mcg • Night’s wakening bd – Worsening over the last two – Theophylline tbl a 250 mg bd – Salbutamol MDI prn months, 3 AB courses (ciprofloxacine, roksitromicin, Ø Asthma – 14 years, 3 -4 oral CS azithromycine), courses per year methzlprednisolone ) with Ø Diabetes - 20 years, type I Ø Retinopathia diabetica Ø Bronchiectasis - 4 years slightly reduced symptoms.
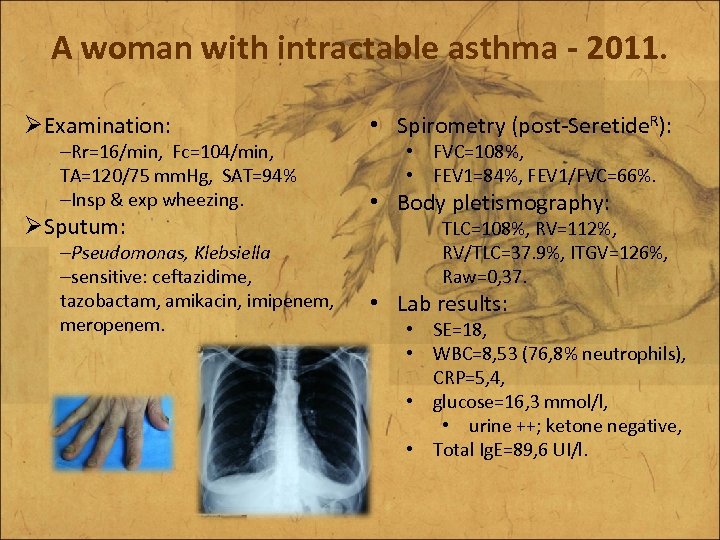
A woman with intractable asthma - 2011. ØExamination: –Rr=16/min, Fc=104/min, TA=120/75 mm. Hg, SAT=94% –Insp & exp wheezing. ØSputum: –Pseudomonas, Klebsiella –sensitive: ceftazidime, tazobactam, amikacin, imipenem, meropenem. • Spirometry (post-Seretide. R): • FVC=108%, • FEV 1=84%, FEV 1/FVC=66%. • Body pletismography: TLC=108%, RV=112%, RV/TLC=37. 9%, ITGV=126%, Raw=0, 37. • Lab results: • SE=18, • WBC=8, 53 (76, 8% neutrophils), CRP=5, 4, • glucose=16, 3 mmol/l, • urine ++; ketone negative, • Total Ig. E=89, 6 UI/l.
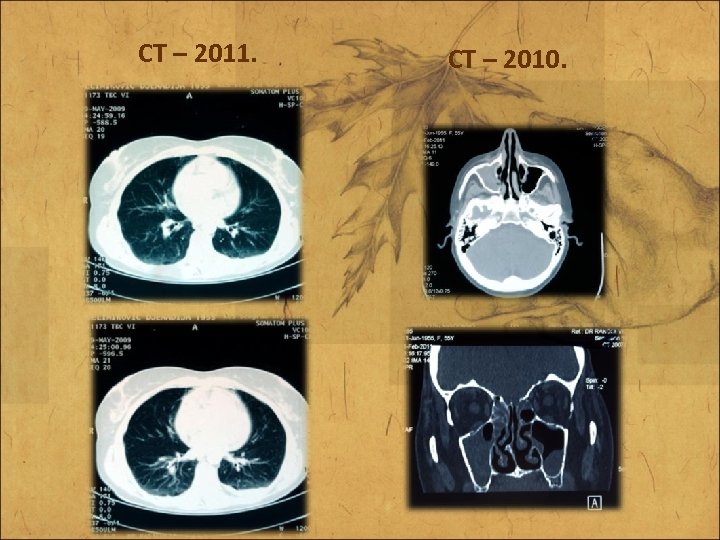
CT – 2011. CT – 2010.
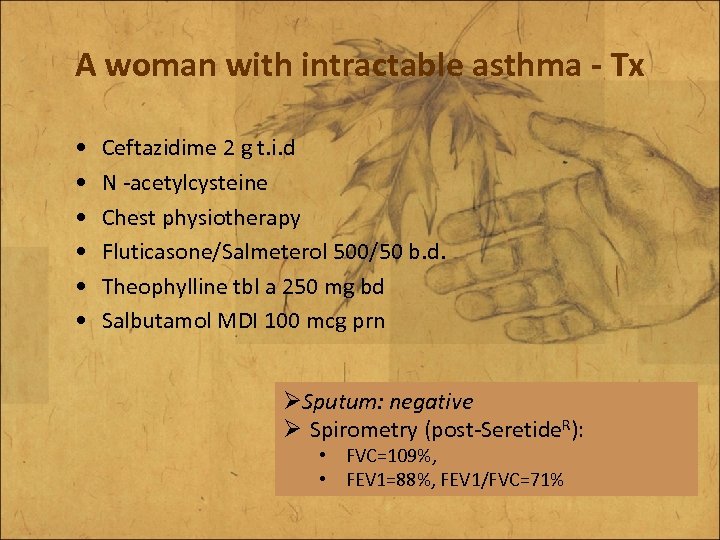
A woman with intractable asthma - Tx • • • Ceftazidime 2 g t. i. d N -acetylcysteine Chest physiotherapy Fluticasone/Salmeterol 500/50 b. d. Theophylline tbl a 250 mg bd Salbutamol MDI 100 mcg prn ØSputum: negative Ø Spirometry (post-Seretide. R): • FVC=109%, • FEV 1=88%, FEV 1/FVC=71%
Severe Asthma Phenotype? Difficult to Treat Asthma? ERS/ATS Task Force ERJ 2013.
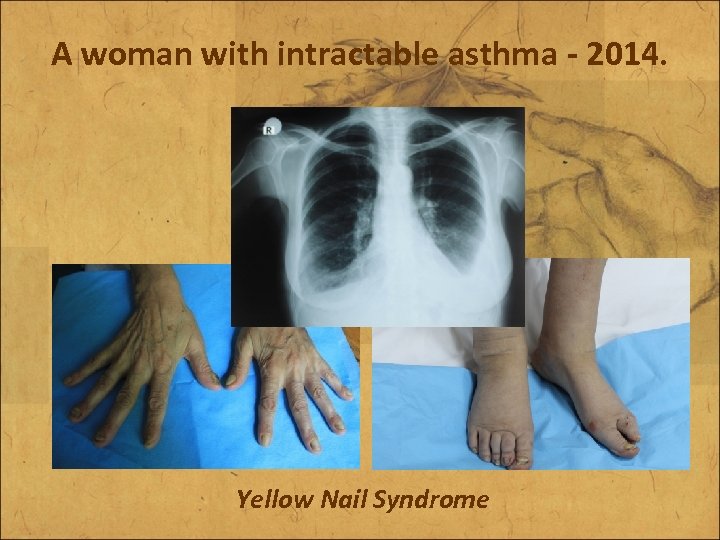
A woman with intractable asthma - 2014. Yellow Nail Syndrome
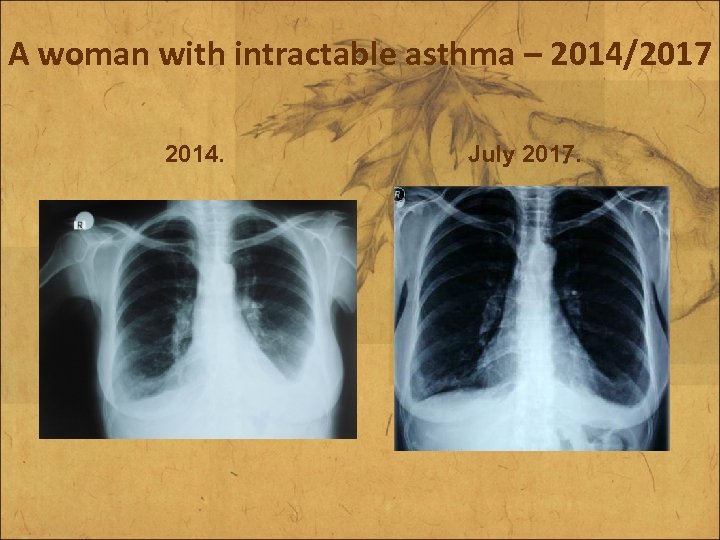
A woman with intractable asthma – 2014/2017 2014. July 2017.
• Asthma (and bronchiectasis) • Bronchiectasis (and asthma) Asthma Bronchiectasis
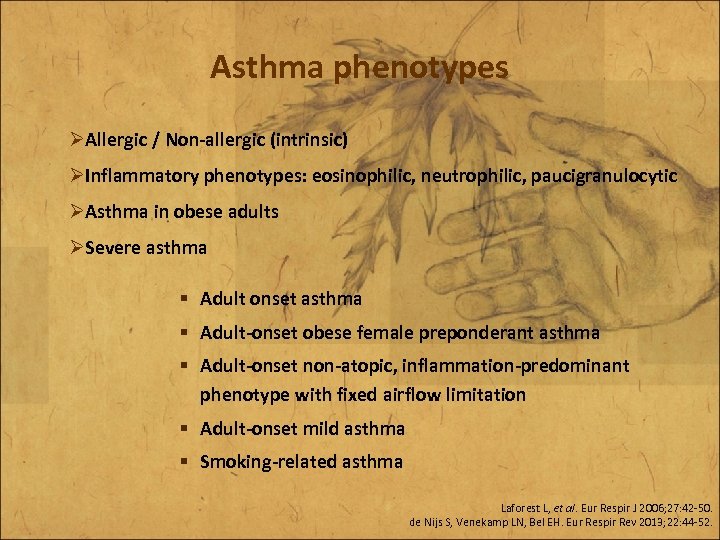
Asthma phenotypes ØAllergic / Non-allergic (intrinsic) ØInflammatory phenotypes: eosinophilic, neutrophilic, paucigranulocytic ØAsthma in obese adults ØSevere asthma § Adult onset asthma § Adult-onset obese female preponderant asthma § Adult-onset non-atopic, inflammation-predominant phenotype with fixed airflow limitation § Adult-onset mild asthma § Smoking-related asthma Laforest L, et al. Eur Respir J 2006; 27: 42 -50. de Nijs S, Venekamp LN, Bel EH. Eur Respir Rev 2013; 22: 44 -52.
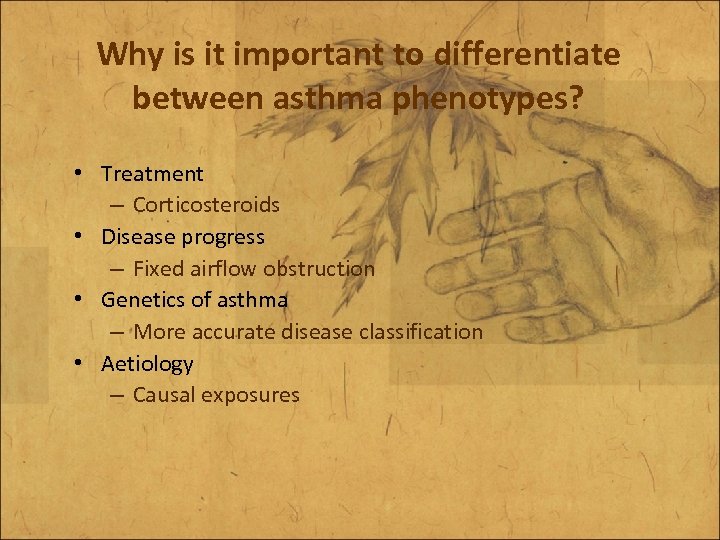
Why is it important to differentiate between asthma phenotypes? • Treatment – Corticosteroids • Disease progress – Fixed airflow obstruction • Genetics of asthma – More accurate disease classification • Aetiology – Causal exposures
Asthma (and Bronchiectasis) A woman with intractable asthma E-mail: branislava. milenkovic@kcs. ac. rs
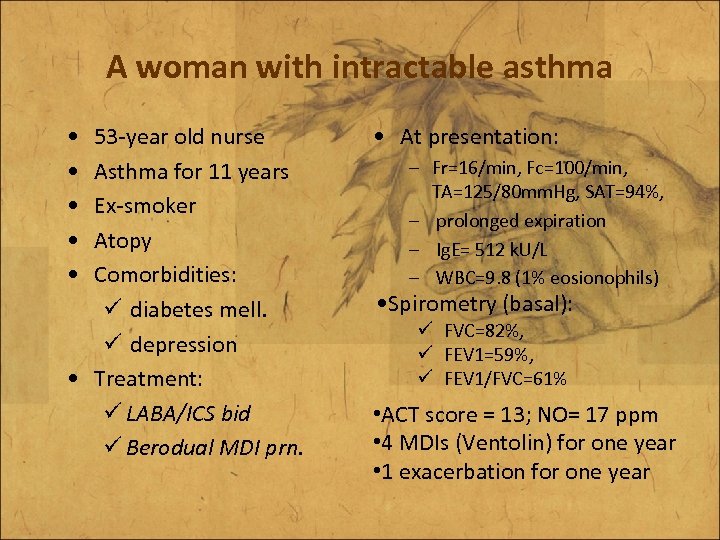
A woman with intractable asthma • • • 53 -year old nurse Asthma for 11 years Ex-smoker Atopy Comorbidities: ü diabetes mell. ü depression • Treatment: ü LABA/ICS bid ü Berodual MDI prn. • At presentation: – Fr=16/min, Fc=100/min, TA=125/80 mm. Hg, SAT=94%, – prolonged expiration – Ig. E= 512 k. U/L – WBC=9. 8 (1% eosionophils) • Spirometry (basal): ü FVC=82%, ü FEV 1=59%, ü FEV 1/FVC=61% • ACT score = 13; NO= 17 ppm • 4 MDIs (Ventolin) for one year • 1 exacerbation for one year
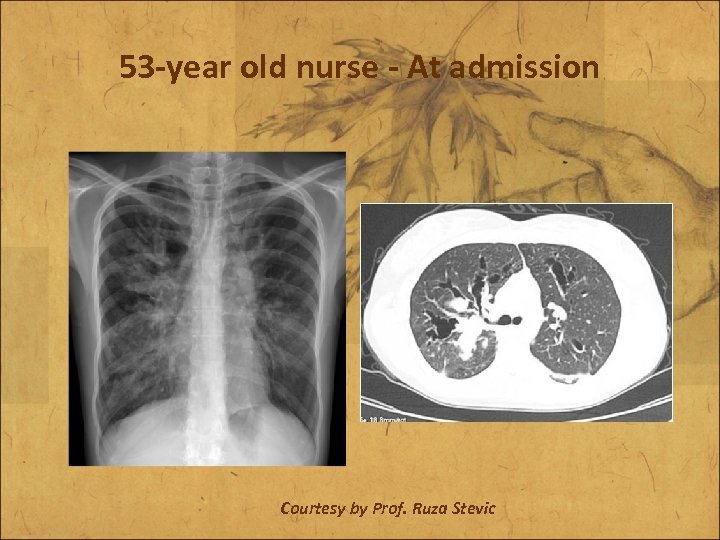
53 -year old nurse - At admission Courtesy by Prof. Ruza Stevic
Minimal Diagnostic Criteria for ABPA-Central Bronchiectasis • Asthma • Central bronchiectasis • Immediate cutaneous reactivity to Aspergillus species or A. fumigatus • Elevated total serum Ig. E (>417 k. U/L) - 512 k. U/L • Elevated serum Ig. E-A. fumigatus and or Ig. G-A. fumigatus compared to sera from prick positive patients with asthma • Inspisated mucus difficult to remove during bronchoscopy.
Classification of ABPA • ABPA with central bronchiectasis …. . ABPA-CB • ABPA without bronchiectasis…………. ABPA-S • ABPA with “other radiologic findings”. . ABPA-ORF • ABPA is classified into 5 stages for ABPA-CB and 4 stages for ABPA-Seropositive • Patients can change stages over time in either direction except if stage 5 (end stage- fibrocavitary) Ricketti AJ, Greenberger PA et al Arch Int Med 1983; 143: 1553
Treatment Options • Oral Corticosteroids • Anti-fungals • Immunomodulators • TREAT the ASTHMA and CO-MORBIDITIES • CONSIDER ENVIRONMENTAL SOURCES Cochrane Review Wark PAB et al 2004
Prednisone as Monotherapy • 0. 5 mg/kg/each am for 2 weeks then on alterate mornings for 2 months…. Tapered prednisone • Repeat HRCT examination • Repeat total Ig. E (should decline at least by 33%) • Environmental exposures to molds-inquire re home and workplace for obvious sources Ricketti AJ, Greenberger PA et al Arch Int Med 1983; 143: 1553 ---Cochrane Review Wark PAB et al 2004
Antifungals • Oral (itraconazole, voriconazole, posaconazole) • Adverse effects of itraconazole… – gastrointestinal intolerance, – lfts, – headache, – peripheral neuropathy, – sleep disturbance…. and – inhibition of cyp 3 a 4 dependent hepatic metabolism (increases concentration of prednisolone (not prednisone) and inhaled budesonide and fluticasone causing HPA suppression) Ricketti AJ, Greenberger PA et al Arch Int Med 1983; 143: 1553 ---Cochrane Review Wark PAB et al 2004
53 -year old nurse Prednisone Plus Itraconazole • 0. 5 mg/kg/each am for 2 weeks then on alterate mornings for 2 months…. Tapered prednisone • Plus Itraconazole 400 mg daily for 16 weeks • Repeat HRCT examination • Repeat total Ig. E (should decline at least by 33%) • Environmental exposures to molds-inquire home and workplace for obvious sources
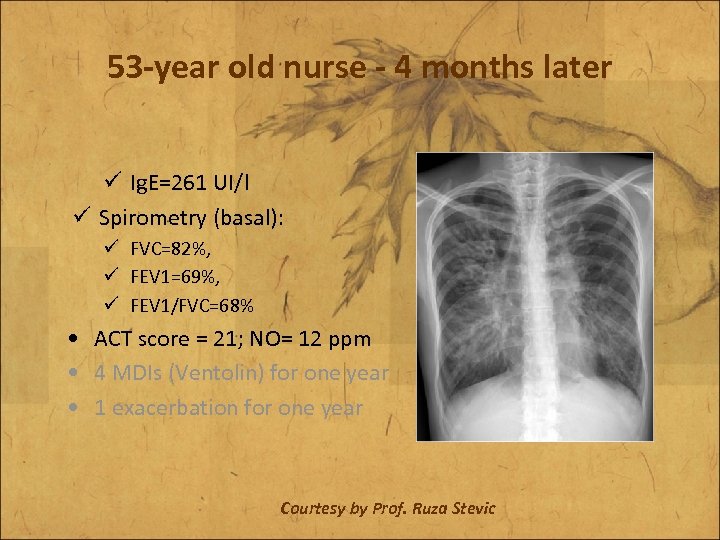
53 -year old nurse - 4 months later ü Ig. E=261 UI/l ü Spirometry (basal): ü FVC=82%, ü FEV 1=69%, ü FEV 1/FVC=68% • ACT score = 21; NO= 12 ppm • 4 MDIs (Ventolin) for one year • 1 exacerbation for one year Courtesy by Prof. Ruza Stevic
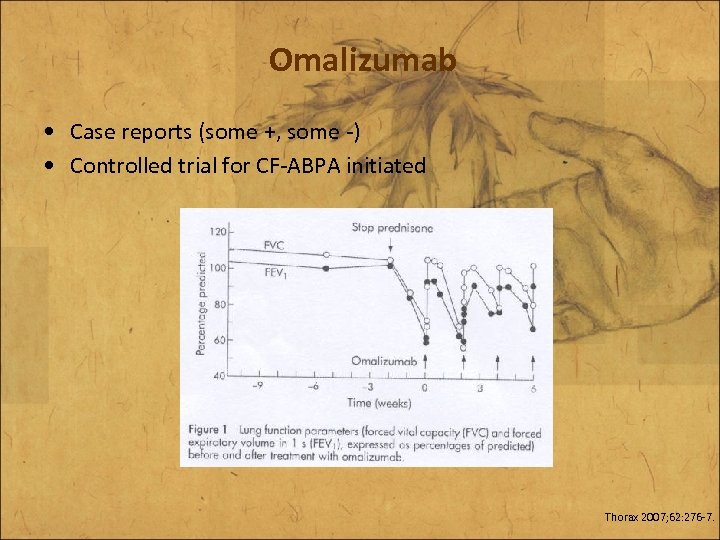
Omalizumab • Case reports (some +, some -) • Controlled trial for CF-ABPA initiated Thorax 2007; 62: 276 -7.
Fungal sensitisation (Allergy SPT) is common in patients with life-threatening asthma in USA O'Hollaren et al New Engl J Med 1991; 324: 359 Fungal sensitisation is common in patients with life-threatening asthma in New Zealand Poole PJ, Black PN Allergy 2000; 55: 501
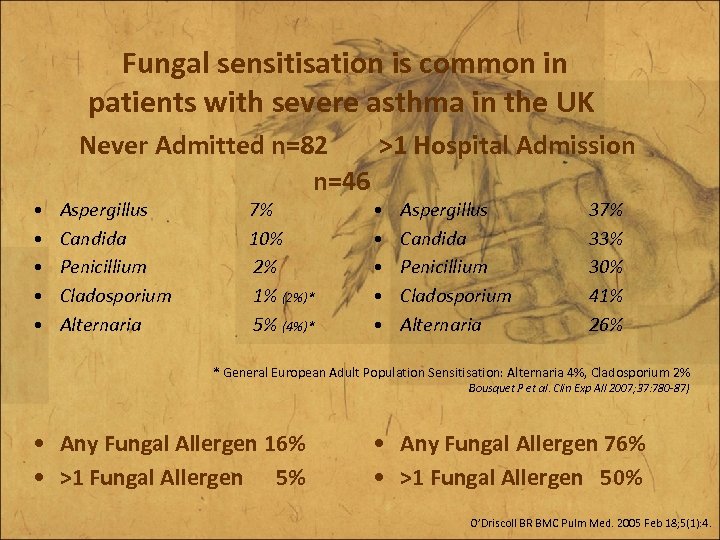
Fungal sensitisation is common in patients with severe asthma in the UK • • • Never Admitted n=82 >1 Hospital Admission n=46 Aspergillus Candida Penicillium Cladosporium Alternaria 7% 10% 2% 1% (2%)* 5% (4%)* • • • Aspergillus Candida Penicillium Cladosporium Alternaria 37% 33% 30% 41% 26% * General European Adult Population Sensitisation: Alternaria 4%, Cladosporium 2% Bousquet P et al. Clin Exp All 2007; 37: 780 -87) • Any Fungal Allergen 16% • >1 Fungal Allergen 5% • Any Fungal Allergen 76% • >1 Fungal Allergen 50% O’Driscoll BR BMC Pulm Med. 2005 Feb 18; 5(1): 4.
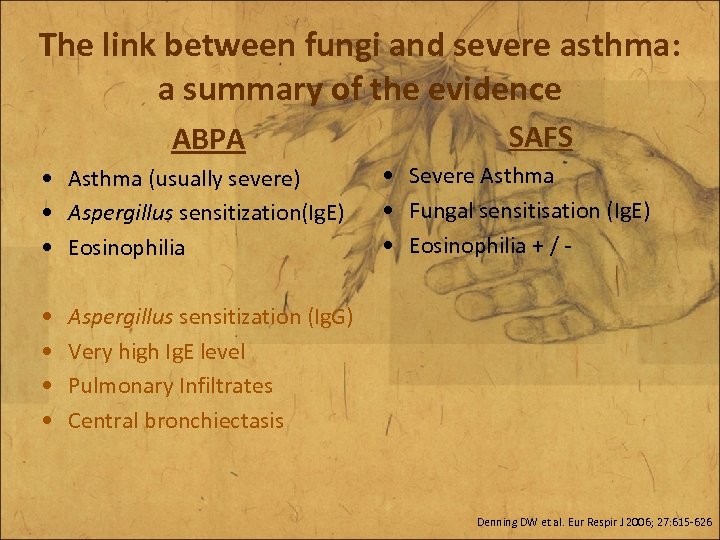
The link between fungi and severe asthma: a summary of the evidence ABPA • Asthma (usually severe) • Aspergillus sensitization(Ig. E) • Eosinophilia • • SAFS • Severe Asthma • Fungal sensitisation (Ig. E) • Eosinophilia + / - Aspergillus sensitization (Ig. G) Very high Ig. E level Pulmonary Infiltrates Central bronchiectasis Denning DW et al. Eur Respir J 2006; 27: 615 -626
The Fungal Asthma Sensitization Trial (FAST) study • Atopy to fungal and non-fungal allergens is very common in severe asthma in North West England • SPT and RAST tests can identify fungal sensitisation • At present, it remains necessary to undertake both tests to identify all cases of fungal sensitisation • This may have therapeutic implications (ABPA and SAFS) Denning DW et al Am J Resp Crit Care Med 2008; In press
• Asthma (and bronchiectasis) • Bronchiectasis (and asthma) Asthma Bronchiectasis
d79d451800186794fd0cb1328cac9f66.ppt