a61a6949bda551df39821f33a5ad7996.ppt
- Количество слайдов: 18
 Association for Real Change – Here to Stay Research & Development Project Consensus Building Event – West Midlands @ Birmingham Voluntary Services Centre
Association for Real Change – Here to Stay Research & Development Project Consensus Building Event – West Midlands @ Birmingham Voluntary Services Centre
 Are we nearly there yet?
Are we nearly there yet?
 MME # PLD l Similarities and differences l l l l Stigma Exclusion Information/ Communication Poor access to services Poor outcomes from using services Difficulties enjoying good health Can you have TWO disadvantages?
MME # PLD l Similarities and differences l l l l Stigma Exclusion Information/ Communication Poor access to services Poor outcomes from using services Difficulties enjoying good health Can you have TWO disadvantages?
 Outline Agenda (things to discuss) l l l access to services experiences of people using services outcomes of support for people with learning disabilities from ethnic minority and new migrant communities. l The ‘double whammy’ or in academic talk – “Intersectional disadvantages” – is it because… l How do we address these challenges?
Outline Agenda (things to discuss) l l l access to services experiences of people using services outcomes of support for people with learning disabilities from ethnic minority and new migrant communities. l The ‘double whammy’ or in academic talk – “Intersectional disadvantages” – is it because… l How do we address these challenges?
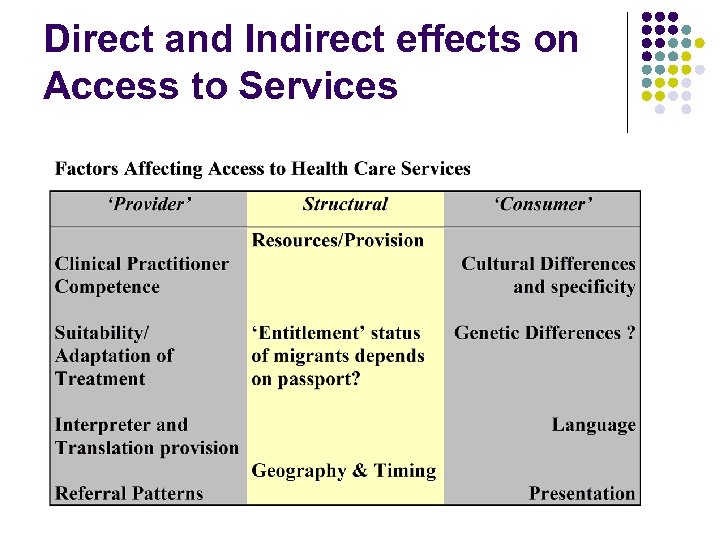 Direct and Indirect effects on Access to Services
Direct and Indirect effects on Access to Services
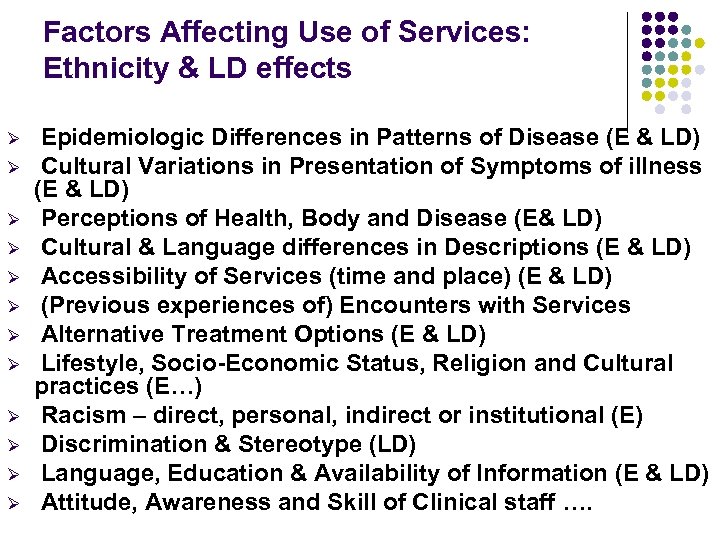 Factors Affecting Use of Services: Ethnicity & LD effects Ø Ø Ø Epidemiologic Differences in Patterns of Disease (E & LD) Cultural Variations in Presentation of Symptoms of illness (E & LD) Perceptions of Health, Body and Disease (E& LD) Cultural & Language differences in Descriptions (E & LD) Accessibility of Services (time and place) (E & LD) (Previous experiences of) Encounters with Services Alternative Treatment Options (E & LD) Lifestyle, Socio-Economic Status, Religion and Cultural practices (E…) Racism – direct, personal, indirect or institutional (E) Discrimination & Stereotype (LD) Language, Education & Availability of Information (E & LD) Attitude, Awareness and Skill of Clinical staff ….
Factors Affecting Use of Services: Ethnicity & LD effects Ø Ø Ø Epidemiologic Differences in Patterns of Disease (E & LD) Cultural Variations in Presentation of Symptoms of illness (E & LD) Perceptions of Health, Body and Disease (E& LD) Cultural & Language differences in Descriptions (E & LD) Accessibility of Services (time and place) (E & LD) (Previous experiences of) Encounters with Services Alternative Treatment Options (E & LD) Lifestyle, Socio-Economic Status, Religion and Cultural practices (E…) Racism – direct, personal, indirect or institutional (E) Discrimination & Stereotype (LD) Language, Education & Availability of Information (E & LD) Attitude, Awareness and Skill of Clinical staff ….
 Differential Outcomes of people using services of getting treatment / services l May arise from Access to Services (e. g. effects of late presentation) May arise from Suitability of treatment May arise from Quality of care given l Need to be monitored and evaluated. l l
Differential Outcomes of people using services of getting treatment / services l May arise from Access to Services (e. g. effects of late presentation) May arise from Suitability of treatment May arise from Quality of care given l Need to be monitored and evaluated. l l
 A short history of the encounter with Diversity & Health in Britain l l l l ‘Port Health’ – Protection & Exoticism Essential ‘manpower’ (Powell, Rhondda, etc) Race Relations and Regulation (Toleration? ) Acceptance and grudging awareness (Toolkits) Increasing recognition – public health & equality Legislation, extension/dilution & confusion Human Rights – and Competition over priority …. (cut backs? )
A short history of the encounter with Diversity & Health in Britain l l l l ‘Port Health’ – Protection & Exoticism Essential ‘manpower’ (Powell, Rhondda, etc) Race Relations and Regulation (Toleration? ) Acceptance and grudging awareness (Toolkits) Increasing recognition – public health & equality Legislation, extension/dilution & confusion Human Rights – and Competition over priority …. (cut backs? )
 Phases of Training or Policy in ‘ethnicity’ …. (LD also has history!) l l Racism Awareness Training (Katz 1978) (RAT) Transcultural Nursing (Leininger) (“CAT”? ) The ‘Fact. File’ (criticised by Culley 2000) Cultural safety (NZ: Papps & Ramsden 1996) Some other alternatives: l Culturally & Linguistically Appropriate Standards (CLAS) (USA – see Diversity Rx; Like 2008) l Racial Justice Approaches l Anti-discriminatory Practice l Cultural sensitivity. .
Phases of Training or Policy in ‘ethnicity’ …. (LD also has history!) l l Racism Awareness Training (Katz 1978) (RAT) Transcultural Nursing (Leininger) (“CAT”? ) The ‘Fact. File’ (criticised by Culley 2000) Cultural safety (NZ: Papps & Ramsden 1996) Some other alternatives: l Culturally & Linguistically Appropriate Standards (CLAS) (USA – see Diversity Rx; Like 2008) l Racial Justice Approaches l Anti-discriminatory Practice l Cultural sensitivity. .
 What sort of Equality / Diversity do we seek l “The NHS provides a comprehensive service, available to all irrespective of gender, race, disability, age, sexual orientation, religion or belief. It has a duty to each and every individual that it serves and must respect their human rights. At the same time, it has a wider social duty to promote equality through the services it provides and to pay particular attention to groups or sections of society where improvements in health and life expectancy are not keeping pace with the rest of the population. ” NHS Constitution 2009
What sort of Equality / Diversity do we seek l “The NHS provides a comprehensive service, available to all irrespective of gender, race, disability, age, sexual orientation, religion or belief. It has a duty to each and every individual that it serves and must respect their human rights. At the same time, it has a wider social duty to promote equality through the services it provides and to pay particular attention to groups or sections of society where improvements in health and life expectancy are not keeping pace with the rest of the population. ” NHS Constitution 2009
 The Will must be there too: The Expressed Aim l l The NHS Commissioning Board will have an explicit duty to promote equality and tackle inequalities in access to healthcare. - DH 2010 Equity & Excellence: Liberating the NHS “Equality must lie at the heart of the NHS - its values, processes and behaviours - if we are to create a service that is personal, fair and diverse, that meets the needs of every patient and all staff” Sir David Nicholson, NHS Chief Executive and Chair of NHS Equality & Diversity Council - The Equality Delivery System for the NHS July 2011 l l The National Charter for Inclusion (2011) – www. givingusavoice. org. uk Valuing People Now & Framework for Action on Ethnicity (2011) – www. valuingpeoplenow. dh. gov. uk
The Will must be there too: The Expressed Aim l l The NHS Commissioning Board will have an explicit duty to promote equality and tackle inequalities in access to healthcare. - DH 2010 Equity & Excellence: Liberating the NHS “Equality must lie at the heart of the NHS - its values, processes and behaviours - if we are to create a service that is personal, fair and diverse, that meets the needs of every patient and all staff” Sir David Nicholson, NHS Chief Executive and Chair of NHS Equality & Diversity Council - The Equality Delivery System for the NHS July 2011 l l The National Charter for Inclusion (2011) – www. givingusavoice. org. uk Valuing People Now & Framework for Action on Ethnicity (2011) – www. valuingpeoplenow. dh. gov. uk
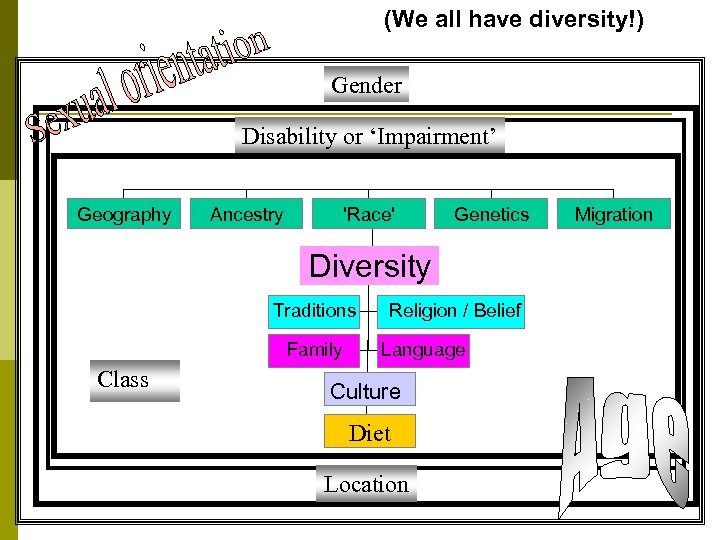 (We all have diversity!) Gender Disability or ‘Impairment’ Geography Ancestry 'Race' Genetics Diversity Traditions Family Class Religion / Belief Language Culture Diet Location Migration
(We all have diversity!) Gender Disability or ‘Impairment’ Geography Ancestry 'Race' Genetics Diversity Traditions Family Class Religion / Belief Language Culture Diet Location Migration
 All professionals have an obligation as Individuals: l To know l And to act l And to recognise that they already deal with clinical complexity so what’s so hard about social complexity? ? ? i. e. Diversity is or should be a ‘key skill’/ core competence But what about the Organisation (NHS etc) … l
All professionals have an obligation as Individuals: l To know l And to act l And to recognise that they already deal with clinical complexity so what’s so hard about social complexity? ? ? i. e. Diversity is or should be a ‘key skill’/ core competence But what about the Organisation (NHS etc) … l
 What might a Culturally Competent Organisation look like? l l l l a degree of respect for cultural traditions and diversity, a preparedness to work alongside community-based groups, and to learn about cultures, languages, religions and dietary restrictions having access to ‘expert’ knowledge from within the community (such as chaplaincy and interpreter support) and lists of contacts within those communities, an awareness of cultural calendars, so festivals and days of religious obligation could be recognised and when appropriate, celebrated together. Hospitals and primary care teams would monitor their own activity and be aware when specific minority groups were disadvantaged or failing to receive particular services, so that action could be taken to remedy inequalities that were detected (Johnson Chirico Scott Pawar 2000) (Bedford &Luton)
What might a Culturally Competent Organisation look like? l l l l a degree of respect for cultural traditions and diversity, a preparedness to work alongside community-based groups, and to learn about cultures, languages, religions and dietary restrictions having access to ‘expert’ knowledge from within the community (such as chaplaincy and interpreter support) and lists of contacts within those communities, an awareness of cultural calendars, so festivals and days of religious obligation could be recognised and when appropriate, celebrated together. Hospitals and primary care teams would monitor their own activity and be aware when specific minority groups were disadvantaged or failing to receive particular services, so that action could be taken to remedy inequalities that were detected (Johnson Chirico Scott Pawar 2000) (Bedford &Luton)
 The Equality Delivery System for the NHS (2011) Endorsed by the NHS Commissioning Board Business Plan April 2012 Making Sure Everyone Counts
The Equality Delivery System for the NHS (2011) Endorsed by the NHS Commissioning Board Business Plan April 2012 Making Sure Everyone Counts
 Conclusion l l Professionals cannot expect sameness in their practice: one of the benefits and challenges of the autonomy afforded to professionals is the expectation that they will be able to respond appropriately to situations for which their initial training may not have prepared them, ‘Life long learning’ and continual professional development and policy making must parallel and complement the changing nature of cultures and the needs and aspirations of people of diverse backgrounds as they too ‘integrate’ or develop within a society that does not merely tolerate, but actively encourages and celebrates, diversity as a resource to meet and overcome new challenges. (Williams & Johnson 2010)
Conclusion l l Professionals cannot expect sameness in their practice: one of the benefits and challenges of the autonomy afforded to professionals is the expectation that they will be able to respond appropriately to situations for which their initial training may not have prepared them, ‘Life long learning’ and continual professional development and policy making must parallel and complement the changing nature of cultures and the needs and aspirations of people of diverse backgrounds as they too ‘integrate’ or develop within a society that does not merely tolerate, but actively encourages and celebrates, diversity as a resource to meet and overcome new challenges. (Williams & Johnson 2010)
 Selected References l l l Johnson M, Chirico S, Scott M, Pawar A 2000 The Toolbox: Culturally Competent Organisations, Services and Care Pathways Bedford: Bedfordshire Health Promotion Agency Katz, JH, 1978, White Awareness: a handbook for Anti Racism Training, Oklahoma: University of Oklahoma Press. Koskinen, L, Abdelhamid, P, & Likitalo, L, 2008, ‘The simulation method for learning cultural awareness in nursing’, Diversity in Health and Social Care, Vol. 5, pt. 1, pp. 55 -63. Campinha-Bacote, J, 2003, ‘Cultural desire: the key to unlocking cultural competence’, Journal of Nursing Education, Vol. 42, pt. 6, pp. 239. Williams C, Johnson MRD 2010 Race and Ethnicity in a Welfare Society Open University Press/ Mc. Graw Hill
Selected References l l l Johnson M, Chirico S, Scott M, Pawar A 2000 The Toolbox: Culturally Competent Organisations, Services and Care Pathways Bedford: Bedfordshire Health Promotion Agency Katz, JH, 1978, White Awareness: a handbook for Anti Racism Training, Oklahoma: University of Oklahoma Press. Koskinen, L, Abdelhamid, P, & Likitalo, L, 2008, ‘The simulation method for learning cultural awareness in nursing’, Diversity in Health and Social Care, Vol. 5, pt. 1, pp. 55 -63. Campinha-Bacote, J, 2003, ‘Cultural desire: the key to unlocking cultural competence’, Journal of Nursing Education, Vol. 42, pt. 6, pp. 239. Williams C, Johnson MRD 2010 Race and Ethnicity in a Welfare Society Open University Press/ Mc. Graw Hill
 More references l l l Like RC, 2008, Culturally competent medicine: an American perspective, Diversity in Health & Social Care, Vol. 5, pt. 2, pp. 83 -86. Papps E, & Ramsden I, 1996, ‘Cultural safety in nursing: the New Zealand experience’, International Journal for Quality in Health Care, Vol. 8, pt. 5, pp. 491 -497 Culley L, 2000, Working with diversity: Beyond the factfile, In: Davies, C, Finlay, L, & Bullman, A, Changing practice in health and social care, London: Sage/ Open University. (pp. 131 -42) l Papadopoulos I, Tilki M, Lees S 2004 Promoting cultural competence in healthcare through a research-based intervention in the UK DHC 1, 2 pp. 107 -116 l O'Boyle-Duggan Marie; Johnson Tony 2013 The last great civil rights issue? Attitudes towards and treatment of people with a learning disability Diversity & Equality in Health & Care 10, 2 pp. 69 -71 (Guest editorial)
More references l l l Like RC, 2008, Culturally competent medicine: an American perspective, Diversity in Health & Social Care, Vol. 5, pt. 2, pp. 83 -86. Papps E, & Ramsden I, 1996, ‘Cultural safety in nursing: the New Zealand experience’, International Journal for Quality in Health Care, Vol. 8, pt. 5, pp. 491 -497 Culley L, 2000, Working with diversity: Beyond the factfile, In: Davies, C, Finlay, L, & Bullman, A, Changing practice in health and social care, London: Sage/ Open University. (pp. 131 -42) l Papadopoulos I, Tilki M, Lees S 2004 Promoting cultural competence in healthcare through a research-based intervention in the UK DHC 1, 2 pp. 107 -116 l O'Boyle-Duggan Marie; Johnson Tony 2013 The last great civil rights issue? Attitudes towards and treatment of people with a learning disability Diversity & Equality in Health & Care 10, 2 pp. 69 -71 (Guest editorial)


