7510f2cfad9b2d267917db1107c43089.ppt
- Количество слайдов: 76
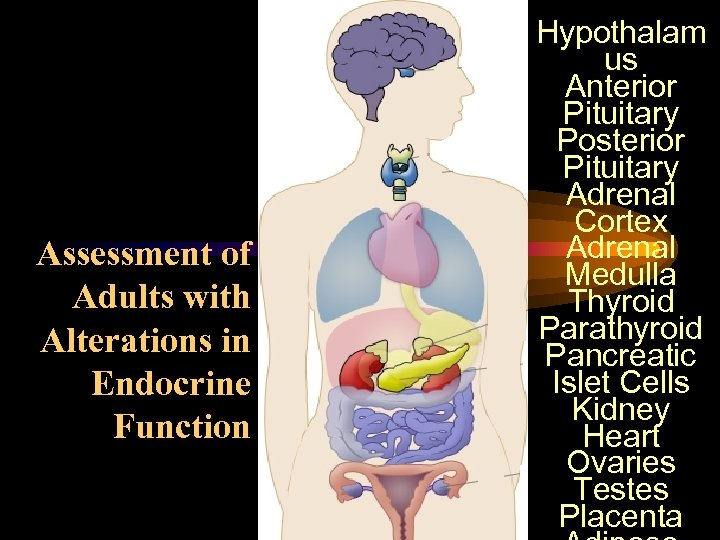 Assessment of Adults with Alterations in Endocrine Function Hypothalam us Anterior Pituitary Posterior Pituitary Adrenal Cortex Adrenal Medulla Thyroid Parathyroid Pancreatic Islet Cells Kidney Heart Ovaries Testes Placenta
Assessment of Adults with Alterations in Endocrine Function Hypothalam us Anterior Pituitary Posterior Pituitary Adrenal Cortex Adrenal Medulla Thyroid Parathyroid Pancreatic Islet Cells Kidney Heart Ovaries Testes Placenta
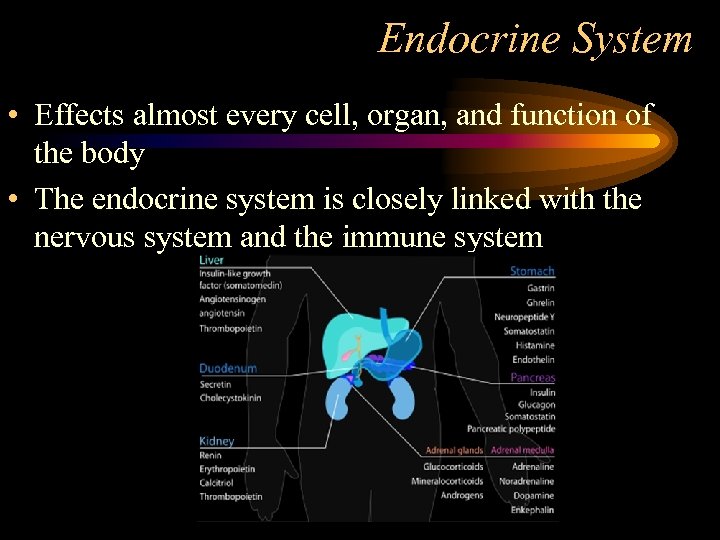 Endocrine System • Effects almost every cell, organ, and function of the body • The endocrine system is closely linked with the nervous system and the immune system
Endocrine System • Effects almost every cell, organ, and function of the body • The endocrine system is closely linked with the nervous system and the immune system
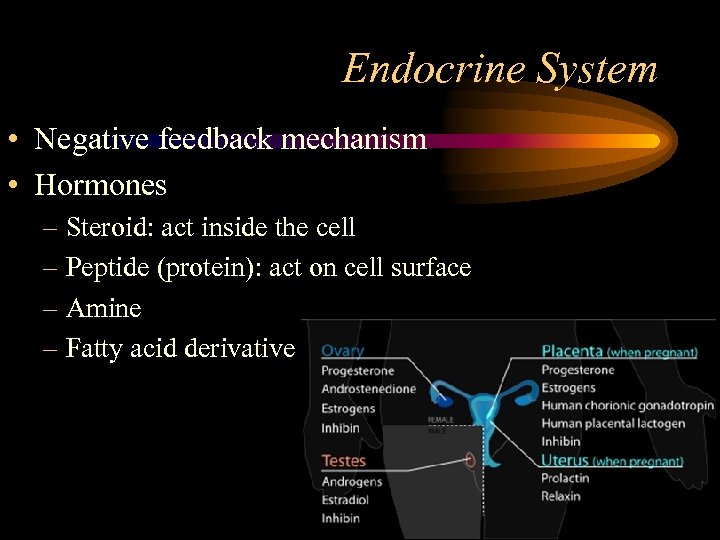 Endocrine System • Negative feedback mechanism • Hormones – Steroid: act inside the cell – Peptide (protein): act on cell surface – Amine – Fatty acid derivative
Endocrine System • Negative feedback mechanism • Hormones – Steroid: act inside the cell – Peptide (protein): act on cell surface – Amine – Fatty acid derivative
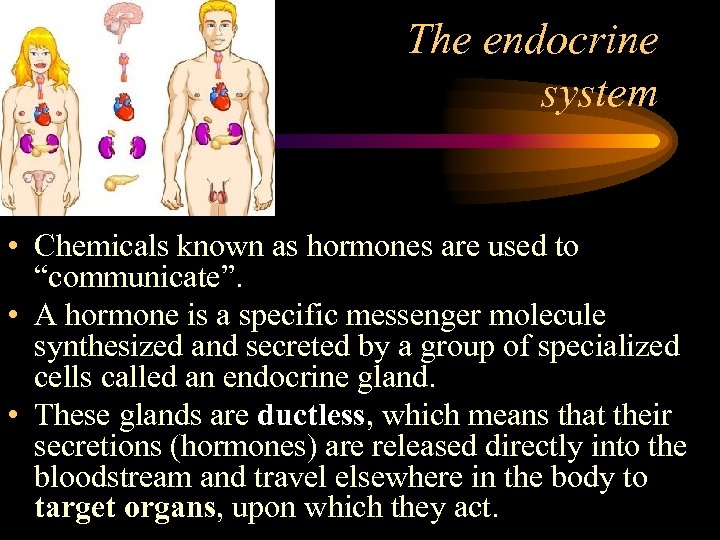 The endocrine system • Chemicals known as hormones are used to “communicate”. • A hormone is a specific messenger molecule synthesized and secreted by a group of specialized cells called an endocrine gland. • These glands are ductless, which means that their secretions (hormones) are released directly into the bloodstream and travel elsewhere in the body to target organs, upon which they act.
The endocrine system • Chemicals known as hormones are used to “communicate”. • A hormone is a specific messenger molecule synthesized and secreted by a group of specialized cells called an endocrine gland. • These glands are ductless, which means that their secretions (hormones) are released directly into the bloodstream and travel elsewhere in the body to target organs, upon which they act.
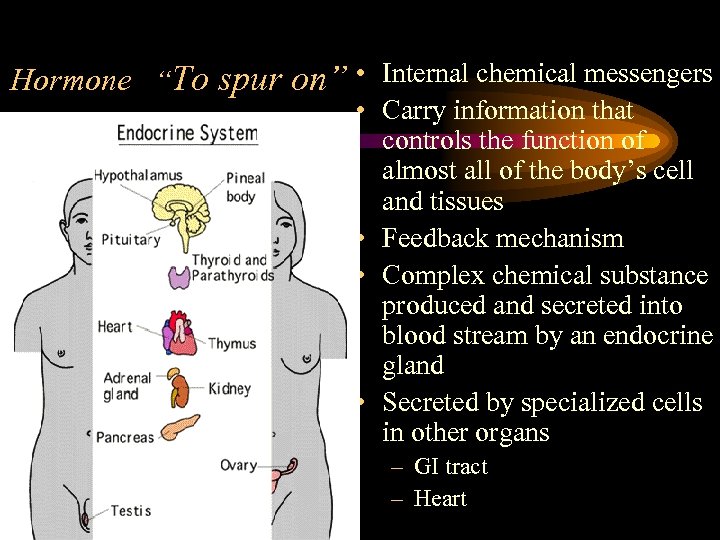 Hormone “To spur on” • Internal chemical messengers • Carry information that controls the function of almost all of the body’s cell and tissues • Feedback mechanism • Complex chemical substance produced and secreted into blood stream by an endocrine gland • Secreted by specialized cells in other organs – GI tract – Heart
Hormone “To spur on” • Internal chemical messengers • Carry information that controls the function of almost all of the body’s cell and tissues • Feedback mechanism • Complex chemical substance produced and secreted into blood stream by an endocrine gland • Secreted by specialized cells in other organs – GI tract – Heart
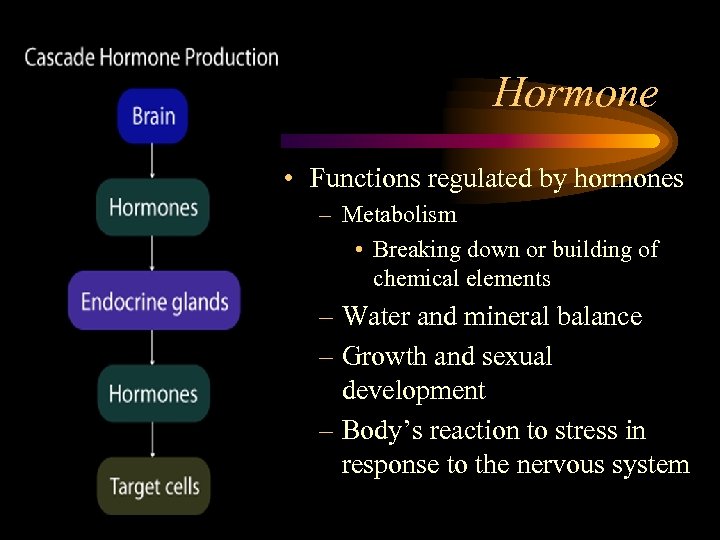 Hormone • Functions regulated by hormones – Metabolism • Breaking down or building of chemical elements – Water and mineral balance – Growth and sexual development – Body’s reaction to stress in response to the nervous system
Hormone • Functions regulated by hormones – Metabolism • Breaking down or building of chemical elements – Water and mineral balance – Growth and sexual development – Body’s reaction to stress in response to the nervous system
 Hormone Action Integrate the activities of widely separated organs Effects of nervous system appear rapidly and are short-lived Endocrine effects are slow to appear, longerlasting, and usually occur at distant target sites
Hormone Action Integrate the activities of widely separated organs Effects of nervous system appear rapidly and are short-lived Endocrine effects are slow to appear, longerlasting, and usually occur at distant target sites
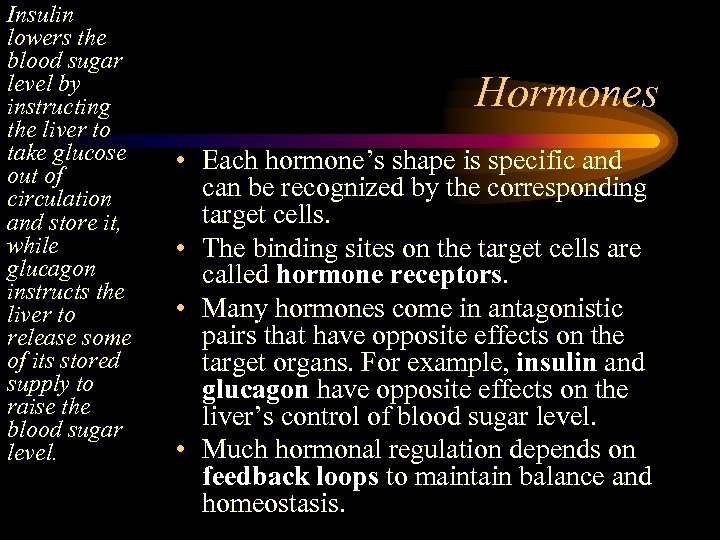 Insulin lowers the blood sugar level by instructing the liver to take glucose out of circulation and store it, while glucagon instructs the liver to release some of its stored supply to raise the blood sugar level. Hormones • Each hormone’s shape is specific and can be recognized by the corresponding target cells. • The binding sites on the target cells are called hormone receptors. • Many hormones come in antagonistic pairs that have opposite effects on the target organs. For example, insulin and glucagon have opposite effects on the liver’s control of blood sugar level. • Much hormonal regulation depends on feedback loops to maintain balance and homeostasis.
Insulin lowers the blood sugar level by instructing the liver to take glucose out of circulation and store it, while glucagon instructs the liver to release some of its stored supply to raise the blood sugar level. Hormones • Each hormone’s shape is specific and can be recognized by the corresponding target cells. • The binding sites on the target cells are called hormone receptors. • Many hormones come in antagonistic pairs that have opposite effects on the target organs. For example, insulin and glucagon have opposite effects on the liver’s control of blood sugar level. • Much hormonal regulation depends on feedback loops to maintain balance and homeostasis.
 Assessment of the Endocrine System • A wide variety of signs and symptoms may occur with endocrine disorders • More general manifestations • Changes in energy level and fatigue common • Ask about energy level • Ask about ability to perform ADL • Ask about changes in heat and cold tolerance • Changes in weight • Changes in sexual function or secondary sex characteristics • Changes in mood, memory, ability to concentrate
Assessment of the Endocrine System • A wide variety of signs and symptoms may occur with endocrine disorders • More general manifestations • Changes in energy level and fatigue common • Ask about energy level • Ask about ability to perform ADL • Ask about changes in heat and cold tolerance • Changes in weight • Changes in sexual function or secondary sex characteristics • Changes in mood, memory, ability to concentrate
 Assessment of the Endocrine System • Changes in skin texture (for hypo or hyperthyroid conditions) • Eye changes (exophthalmos with Hyperthyroidism – Grave’s disease) • Changes in physical appearance (facial hair in women, “moon face”, “buffalo hump”, thinning of skin, obesity of the trunk and thinness of the extremities, increased size of feet and hands, edema) may signify disorders of the thyroid, adrenal cortex, or pituitary gland. • Vital signs measured and compared
Assessment of the Endocrine System • Changes in skin texture (for hypo or hyperthyroid conditions) • Eye changes (exophthalmos with Hyperthyroidism – Grave’s disease) • Changes in physical appearance (facial hair in women, “moon face”, “buffalo hump”, thinning of skin, obesity of the trunk and thinness of the extremities, increased size of feet and hands, edema) may signify disorders of the thyroid, adrenal cortex, or pituitary gland. • Vital signs measured and compared
 • Nursing history Nursing Assessment – Patient history • Pertinent past and present history of endocrine problems • Onset sudden or gradual • Impact on activities • Changes in energy levels • Elimination patterns • Changes in nutritional status • GI disturbances • Sexual and reproductive function disturbances • Changes in physical characteristics
• Nursing history Nursing Assessment – Patient history • Pertinent past and present history of endocrine problems • Onset sudden or gradual • Impact on activities • Changes in energy levels • Elimination patterns • Changes in nutritional status • GI disturbances • Sexual and reproductive function disturbances • Changes in physical characteristics
 – Family history Nursing Assessment • Diabetes mellitus • Thyroid disorders • Any other endocrine disorder – Social history • Coping skills • Support systems • Health-related beliefs • Infertility • Impotence • Medication
– Family history Nursing Assessment • Diabetes mellitus • Thyroid disorders • Any other endocrine disorder – Social history • Coping skills • Support systems • Health-related beliefs • Infertility • Impotence • Medication
 Nursing Assessment • Physical Assessment – Inspection • General appearance in relationship to age – Height – Weight – Fat distribution – Muscle mass
Nursing Assessment • Physical Assessment – Inspection • General appearance in relationship to age – Height – Weight – Fat distribution – Muscle mass
 Nursing Assessment • Skin abnormalities – Skin color, hyper- or hypo pigmentation – Bruising, petechiae • Edema • Hair distribution • Nails
Nursing Assessment • Skin abnormalities – Skin color, hyper- or hypo pigmentation – Bruising, petechiae • Edema • Hair distribution • Nails
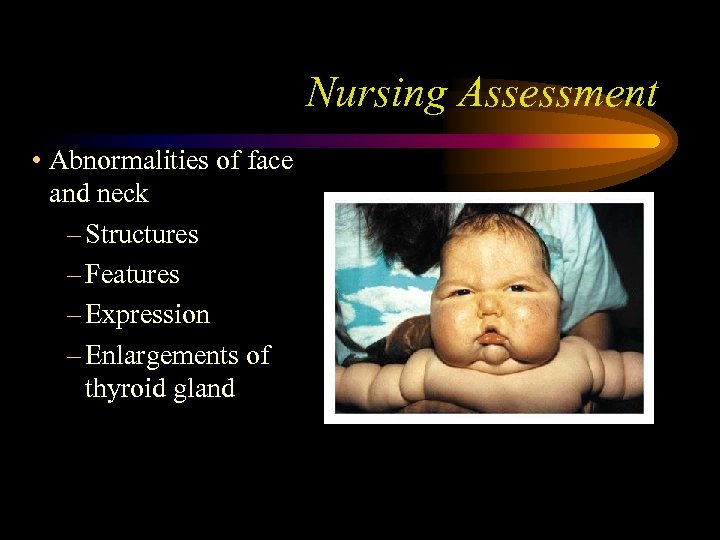 Nursing Assessment • Abnormalities of face and neck – Structures – Features – Expression – Enlargements of thyroid gland
Nursing Assessment • Abnormalities of face and neck – Structures – Features – Expression – Enlargements of thyroid gland
 Nursing Assessment • Abnormalities of trunk – Truncal obesity – Supraclavicular fat pads – Buffalo hump – Secondary sexual characteristics
Nursing Assessment • Abnormalities of trunk – Truncal obesity – Supraclavicular fat pads – Buffalo hump – Secondary sexual characteristics
 Nursing Assessment • Genitalia – Size of external genitalia – Distribution and quantity of pubic hair
Nursing Assessment • Genitalia – Size of external genitalia – Distribution and quantity of pubic hair
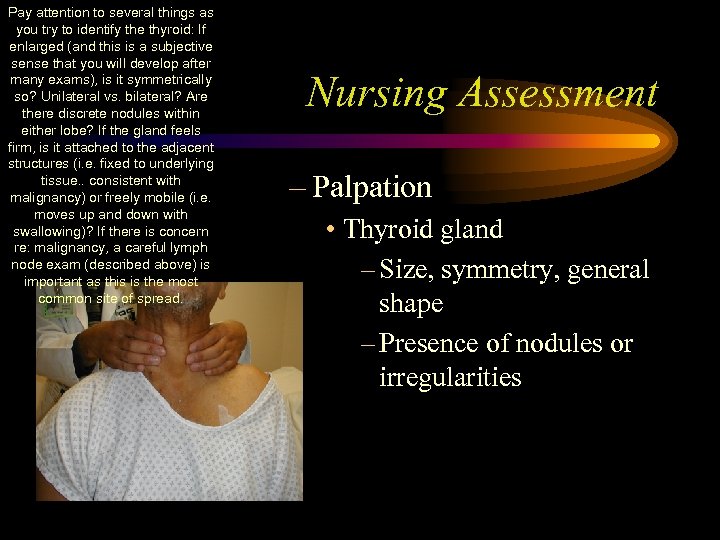 Pay attention to several things as you try to identify the thyroid: If enlarged (and this is a subjective sense that you will develop after many exams), is it symmetrically so? Unilateral vs. bilateral? Are there discrete nodules within either lobe? If the gland feels firm, is it attached to the adjacent structures (i. e. fixed to underlying tissue. . consistent with malignancy) or freely mobile (i. e. moves up and down with swallowing)? If there is concern re: malignancy, a careful lymph node exam (described above) is important as this is the most common site of spread. Nursing Assessment – Palpation • Thyroid gland – Size, symmetry, general shape – Presence of nodules or irregularities
Pay attention to several things as you try to identify the thyroid: If enlarged (and this is a subjective sense that you will develop after many exams), is it symmetrically so? Unilateral vs. bilateral? Are there discrete nodules within either lobe? If the gland feels firm, is it attached to the adjacent structures (i. e. fixed to underlying tissue. . consistent with malignancy) or freely mobile (i. e. moves up and down with swallowing)? If there is concern re: malignancy, a careful lymph node exam (described above) is important as this is the most common site of spread. Nursing Assessment – Palpation • Thyroid gland – Size, symmetry, general shape – Presence of nodules or irregularities
 Nursing Assessment • Behavioral changes – Agitation – Nervousness – Flat affect – Lack of concern about personal appearance
Nursing Assessment • Behavioral changes – Agitation – Nervousness – Flat affect – Lack of concern about personal appearance
 Nursing Assessment • Diagnostic Studies – Laboratory test essential component in diagnostic phase of endocrine dysfunction assessment – Hormonal blood levels do not always fall in distinct normal and abnormal categories – In suspected endocrine gland under activity, a stimulus is sometimes given to ascertain if a normal response is possible - stimulation testing
Nursing Assessment • Diagnostic Studies – Laboratory test essential component in diagnostic phase of endocrine dysfunction assessment – Hormonal blood levels do not always fall in distinct normal and abnormal categories – In suspected endocrine gland under activity, a stimulus is sometimes given to ascertain if a normal response is possible - stimulation testing
 Diagnostic Evaluation • Blood tests – Hormone blood levels • Hyper or hypo function – Autoantibodies • Assesses effect of hormones on other substances – (ex: effect of insulin on blood glucose) – Radioimmunoassays • Radioisotope-labeled antigen • Measures level of hormones and other substances
Diagnostic Evaluation • Blood tests – Hormone blood levels • Hyper or hypo function – Autoantibodies • Assesses effect of hormones on other substances – (ex: effect of insulin on blood glucose) – Radioimmunoassays • Radioisotope-labeled antigen • Measures level of hormones and other substances
 Diagnostic Evaluation • Urine tests – Hormone excreted – 24 hour test • (ex: measuring free catecholamines for suspected pheochromocytoma ) • Stimulation and suppression tests – Determines how endocrine gland responds to administration of stimulating hormone normally produced or released by the hypothalamus or pituitary gland – Checking the negative feedback mechanisms
Diagnostic Evaluation • Urine tests – Hormone excreted – 24 hour test • (ex: measuring free catecholamines for suspected pheochromocytoma ) • Stimulation and suppression tests – Determines how endocrine gland responds to administration of stimulating hormone normally produced or released by the hypothalamus or pituitary gland – Checking the negative feedback mechanisms
 Nursing Assessment • Radiographic exams – MRI, CT, PET, DEXA – especially of head, are used for visualization of sella turcica – CAT scans may determined extent of growth of a gland or tumor gland – Needle biopsy used to determine composition of thyroid nodules
Nursing Assessment • Radiographic exams – MRI, CT, PET, DEXA – especially of head, are used for visualization of sella turcica – CAT scans may determined extent of growth of a gland or tumor gland – Needle biopsy used to determine composition of thyroid nodules
 Nursing Assessment • Genetic Screening – Advent of DNA testing – Any gene mutation
Nursing Assessment • Genetic Screening – Advent of DNA testing – Any gene mutation
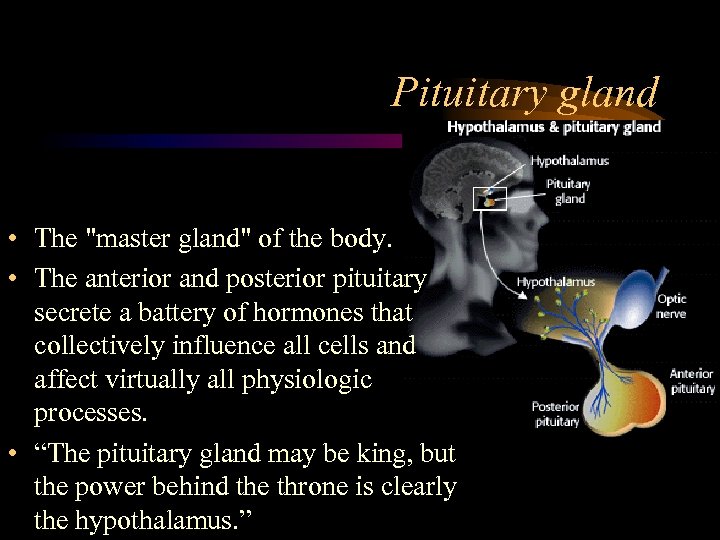 Pituitary gland • The "master gland" of the body. • The anterior and posterior pituitary secrete a battery of hormones that collectively influence all cells and affect virtually all physiologic processes. • “The pituitary gland may be king, but the power behind the throne is clearly the hypothalamus. ”
Pituitary gland • The "master gland" of the body. • The anterior and posterior pituitary secrete a battery of hormones that collectively influence all cells and affect virtually all physiologic processes. • “The pituitary gland may be king, but the power behind the throne is clearly the hypothalamus. ”
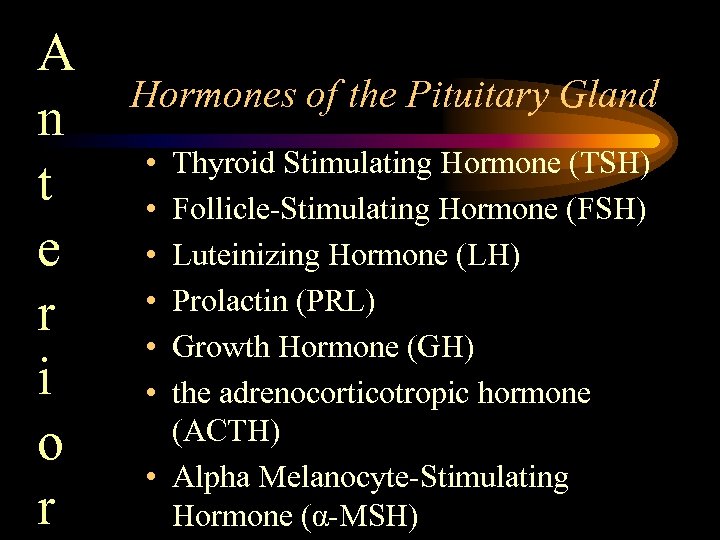 A n t e r i o r Hormones of the Pituitary Gland • • • Thyroid Stimulating Hormone (TSH) Follicle-Stimulating Hormone (FSH) Luteinizing Hormone (LH) Prolactin (PRL) Growth Hormone (GH) the adrenocorticotropic hormone (ACTH) • Alpha Melanocyte-Stimulating Hormone (α-MSH)
A n t e r i o r Hormones of the Pituitary Gland • • • Thyroid Stimulating Hormone (TSH) Follicle-Stimulating Hormone (FSH) Luteinizing Hormone (LH) Prolactin (PRL) Growth Hormone (GH) the adrenocorticotropic hormone (ACTH) • Alpha Melanocyte-Stimulating Hormone (α-MSH)
 Pituitary Gland (Master Gland) Abnormalties occur with under secretion and over secretion of the hormones secreted by this gland • Anterior – Hyperpituitarism • an over-secretion generally of prolactin or growth hormone. Most commonly caused by a benign tumor, such as adenoma
Pituitary Gland (Master Gland) Abnormalties occur with under secretion and over secretion of the hormones secreted by this gland • Anterior – Hyperpituitarism • an over-secretion generally of prolactin or growth hormone. Most commonly caused by a benign tumor, such as adenoma
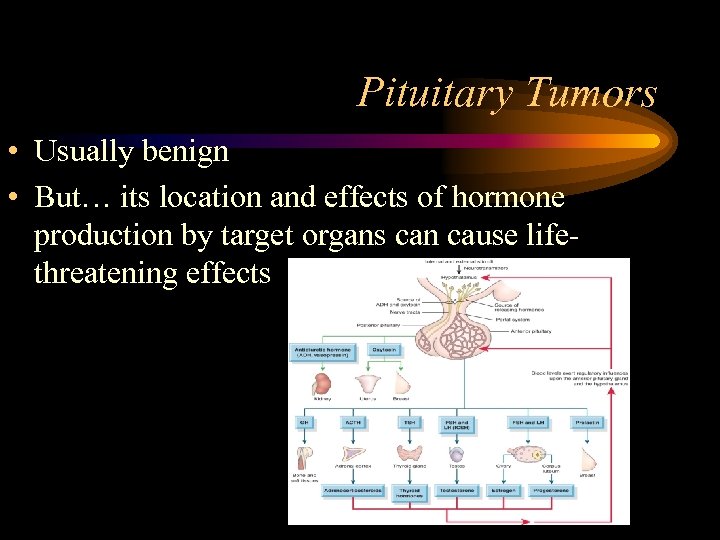 Pituitary Tumors • Usually benign • But… its location and effects of hormone production by target organs can cause lifethreatening effects
Pituitary Tumors • Usually benign • But… its location and effects of hormone production by target organs can cause lifethreatening effects
 Pituitary Gland • Tumors (continued) – Giantism – Cushing’s syndrome • Chromophobic tumors – Do not produce hormones – Destroy rest of pituitary gland – Obese, somulent, fine scanty hair, soft skin, Headaches, no libido, pasty complexion and blindness – Polyuria, polyphagia, decreased MR, and subnormal body temperature
Pituitary Gland • Tumors (continued) – Giantism – Cushing’s syndrome • Chromophobic tumors – Do not produce hormones – Destroy rest of pituitary gland – Obese, somulent, fine scanty hair, soft skin, Headaches, no libido, pasty complexion and blindness – Polyuria, polyphagia, decreased MR, and subnormal body temperature
 Pituitary Tumors • Assessment – Careful history and physical examination – Visual acuity/ visual fields – CT and MRI – Serum levels of pituitary hormones – Measurement of target organs
Pituitary Tumors • Assessment – Careful history and physical examination – Visual acuity/ visual fields – CT and MRI – Serum levels of pituitary hormones – Measurement of target organs
 Pituitary Tumors • Medical Management – Surgical removal (hypophysectomy) – Sterotactic Radiation – Parlodel (bromocriptine) • Dopamine antagonist – Sandostatin • Synthetic analogue of GH
Pituitary Tumors • Medical Management – Surgical removal (hypophysectomy) – Sterotactic Radiation – Parlodel (bromocriptine) • Dopamine antagonist – Sandostatin • Synthetic analogue of GH
 Pituitary Tumors • Surgical Management – Surgical removal (hypophysectomy) – Treatment of choice for patients with excessive ACTH (Cushing’s) by Pituitary gland – Palliative measure to relieve bone pain from metastatic lesions of breast/ prostate
Pituitary Tumors • Surgical Management – Surgical removal (hypophysectomy) – Treatment of choice for patients with excessive ACTH (Cushing’s) by Pituitary gland – Palliative measure to relieve bone pain from metastatic lesions of breast/ prostate

 NURSING MANAGEMENTPRE OPERATIVE CARE • Assess the patient knowledge and understanding of the planned operative procedure. • Obtain a health history and physical assessment. • Explain necessary postoperative activity restriction.
NURSING MANAGEMENTPRE OPERATIVE CARE • Assess the patient knowledge and understanding of the planned operative procedure. • Obtain a health history and physical assessment. • Explain necessary postoperative activity restriction.
 PRE OPERATIVE CARE • Teach respiratory hygiene procedures such as coughing, and deep breathing exercise • Administer intravenous antibiotic as ordered. • Keep patient NBM.
PRE OPERATIVE CARE • Teach respiratory hygiene procedures such as coughing, and deep breathing exercise • Administer intravenous antibiotic as ordered. • Keep patient NBM.
 Complications • • • Hypopituitarism. Cerebrospinal fluid (CSF) leakage. Infection. Bleeding. Nasal septal perforation. Visual impairment. Incomplete tumor removal. Diabetic Insipidus
Complications • • • Hypopituitarism. Cerebrospinal fluid (CSF) leakage. Infection. Bleeding. Nasal septal perforation. Visual impairment. Incomplete tumor removal. Diabetic Insipidus
 Nursing Care • Monitor vital signs. • Provide bed rest. • Assess nasal drip pad (“moustache” dressing) frequently for blood or clear fluid. • Encourage the patient to use the straw for drinking any fluid. • Frequent oral hygiene and a cool vaporizer mist. • Avoid toothbrushing for 10 days. • Administer analgesic to reduce pain as ordered
Nursing Care • Monitor vital signs. • Provide bed rest. • Assess nasal drip pad (“moustache” dressing) frequently for blood or clear fluid. • Encourage the patient to use the straw for drinking any fluid. • Frequent oral hygiene and a cool vaporizer mist. • Avoid toothbrushing for 10 days. • Administer analgesic to reduce pain as ordered
 Treatment • Treatment Hormone replacement therapy – Glucocorticoids – Growth hormone – Vasopressin – Is usually free of complications. Glucocorticoids replacement require careful dose adjustments during stressful events.
Treatment • Treatment Hormone replacement therapy – Glucocorticoids – Growth hormone – Vasopressin – Is usually free of complications. Glucocorticoids replacement require careful dose adjustments during stressful events.
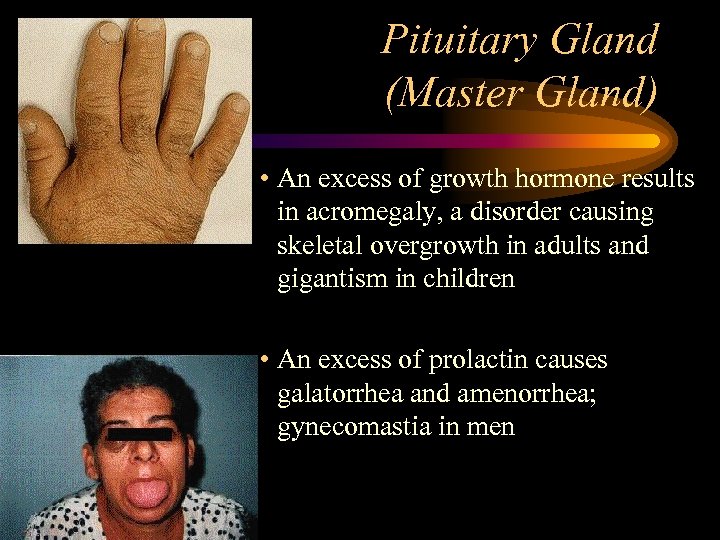 Pituitary Gland (Master Gland) • An excess of growth hormone results in acromegaly, a disorder causing skeletal overgrowth in adults and gigantism in children • An excess of prolactin causes galatorrhea and amenorrhea; gynecomastia in men
Pituitary Gland (Master Gland) • An excess of growth hormone results in acromegaly, a disorder causing skeletal overgrowth in adults and gigantism in children • An excess of prolactin causes galatorrhea and amenorrhea; gynecomastia in men
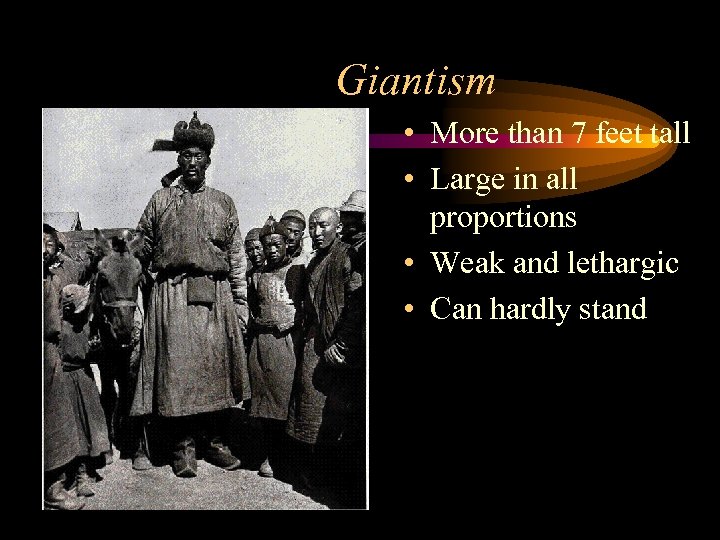 Giantism • More than 7 feet tall • Large in all proportions • Weak and lethargic • Can hardly stand
Giantism • More than 7 feet tall • Large in all proportions • Weak and lethargic • Can hardly stand
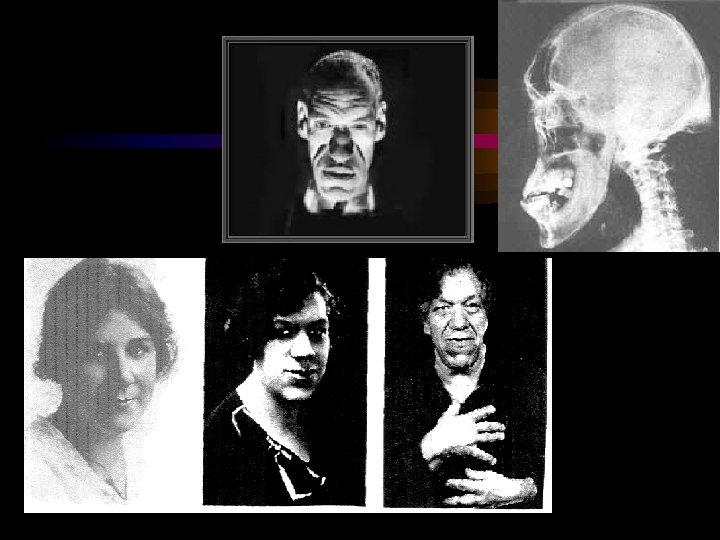
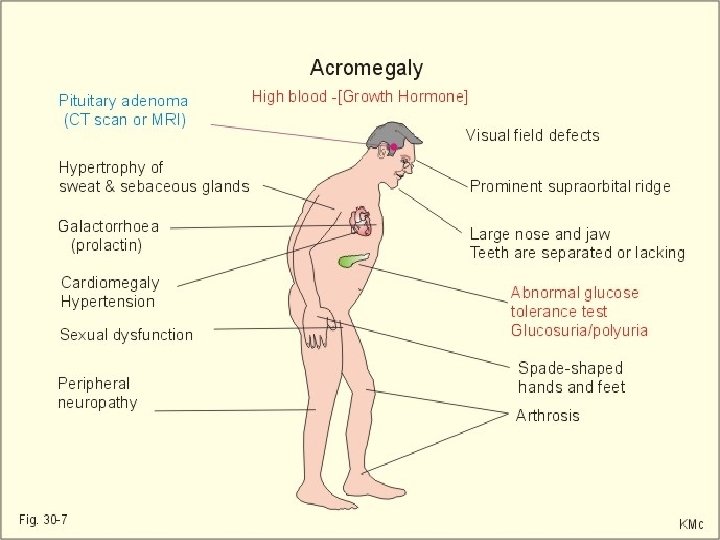
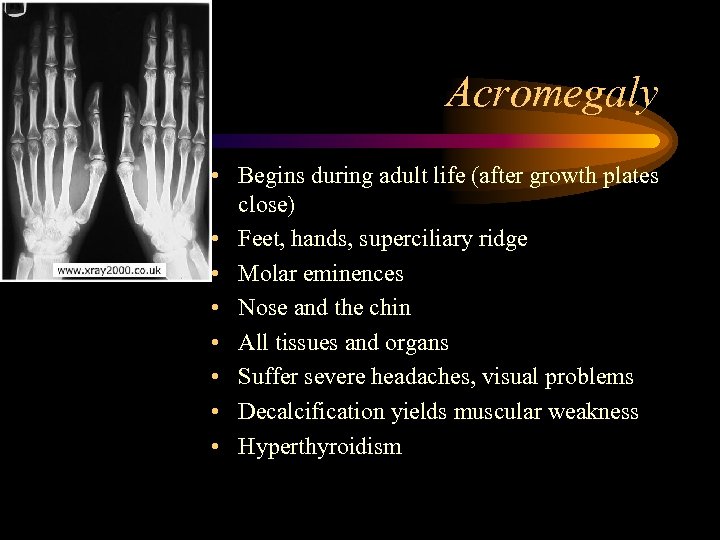 Acromegaly • Begins during adult life (after growth plates close) • Feet, hands, superciliary ridge • Molar eminences • Nose and the chin • All tissues and organs • Suffer severe headaches, visual problems • Decalcification yields muscular weakness • Hyperthyroidism
Acromegaly • Begins during adult life (after growth plates close) • Feet, hands, superciliary ridge • Molar eminences • Nose and the chin • All tissues and organs • Suffer severe headaches, visual problems • Decalcification yields muscular weakness • Hyperthyroidism
 • Goal – Reduce GH production • Drug Therapy – Bromocriptine (Parlodel) – Shrinks tumor before surgery – Octreotide (Sandostatin) – Synthetic brain hormone – Stops GH production • Radiation Therapy Treatment of Acromegaly
• Goal – Reduce GH production • Drug Therapy – Bromocriptine (Parlodel) – Shrinks tumor before surgery – Octreotide (Sandostatin) – Synthetic brain hormone – Stops GH production • Radiation Therapy Treatment of Acromegaly
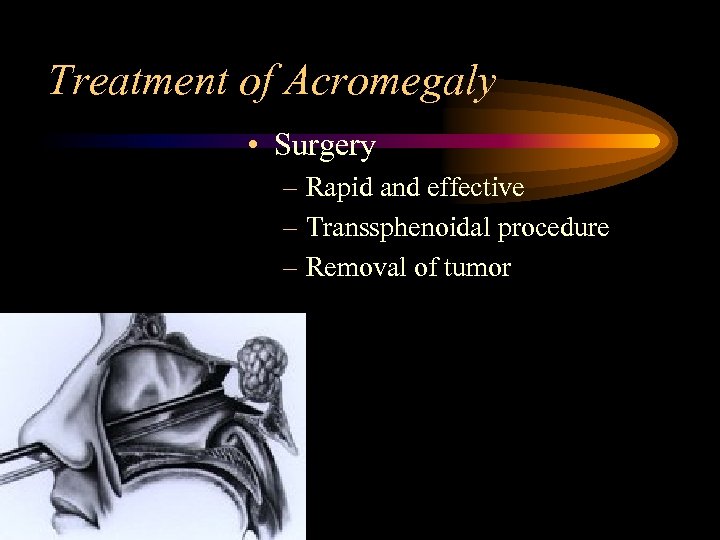 Treatment of Acromegaly • Surgery – Rapid and effective – Transsphenoidal procedure – Removal of tumor
Treatment of Acromegaly • Surgery – Rapid and effective – Transsphenoidal procedure – Removal of tumor
 Pituitary Gland (Master Gland) – Hypopituitarism – a deficiency of a single hormone or all of pituitary hormones may be caused by primary pituitary tumors, surgery of pituitary gland, or infection. – Growth hormone deficiency as a child results in dwarfism
Pituitary Gland (Master Gland) – Hypopituitarism – a deficiency of a single hormone or all of pituitary hormones may be caused by primary pituitary tumors, surgery of pituitary gland, or infection. – Growth hormone deficiency as a child results in dwarfism
 Pituitary Gland (Master Gland) – Management • Hyperpituitarism is often treated with medication to suppress hormone secretion whiles hypopituitarism can be treated with hormone replacement therapy • When anterior pituitary problem is secondary to tumor, a surgical procedure such as a hypophysectomy may be warranted
Pituitary Gland (Master Gland) – Management • Hyperpituitarism is often treated with medication to suppress hormone secretion whiles hypopituitarism can be treated with hormone replacement therapy • When anterior pituitary problem is secondary to tumor, a surgical procedure such as a hypophysectomy may be warranted
 Pituitary Gland (Master Gland) • Posterior – damage to posterior pituitary will result in changed in secretion of two hormones in stores and releases, ADH and oxytocin
Pituitary Gland (Master Gland) • Posterior – damage to posterior pituitary will result in changed in secretion of two hormones in stores and releases, ADH and oxytocin
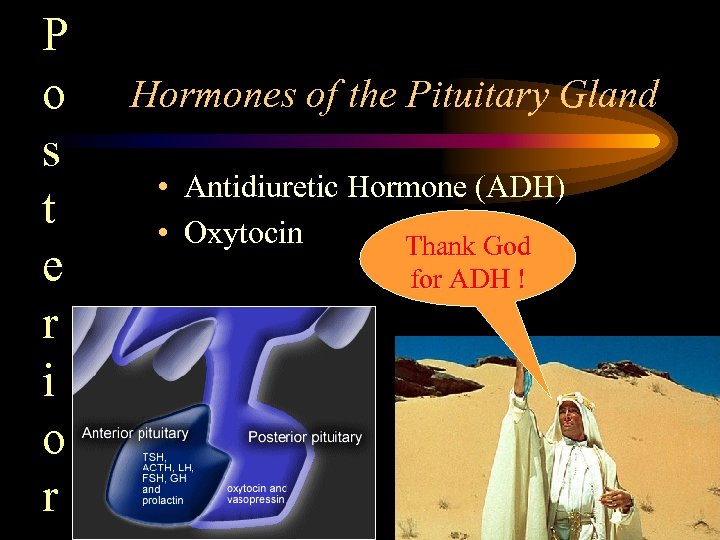 P o s t e r i o r Hormones of the Pituitary Gland • Antidiuretic Hormone (ADH) • Oxytocin Thank God for ADH !
P o s t e r i o r Hormones of the Pituitary Gland • Antidiuretic Hormone (ADH) • Oxytocin Thank God for ADH !
 Diabetes Insipidus • DI is a clinical condition due to a deficit of ADH or due to the kidney’s resistance to the effects of ADH. • DI may be central (neurogenic) or nephrogenic. • DI may be a transient or a permanent condition.
Diabetes Insipidus • DI is a clinical condition due to a deficit of ADH or due to the kidney’s resistance to the effects of ADH. • DI may be central (neurogenic) or nephrogenic. • DI may be a transient or a permanent condition.
 Diabetes Insipidus • ADH insufficiency causes diabetes Insipidus – Primary DI is result of defect in the posterior pituitary gland itself – Secondary DI is result of a defect of hypothalamus or pituitary stalk – Deficient production of vasopressin – Management • Replace ADH with drugs such as (DDAVP) Desmopressin, lypressin, and Clofibrate (diuretic effect from a hypolipedemic) • Adequate fluid replacement • Correct underlying problem
Diabetes Insipidus • ADH insufficiency causes diabetes Insipidus – Primary DI is result of defect in the posterior pituitary gland itself – Secondary DI is result of a defect of hypothalamus or pituitary stalk – Deficient production of vasopressin – Management • Replace ADH with drugs such as (DDAVP) Desmopressin, lypressin, and Clofibrate (diuretic effect from a hypolipedemic) • Adequate fluid replacement • Correct underlying problem
 Etiologies of DI • CNS disorders that damage or create pressure in the area of the hypothalamus, pituitary stalk, or posterior pituitary gland • Head Injuries • CNS infections • Intraventricular Hemorrhage • Neurosurgical Procedures: common postoperatively with resection of craniopharyngiomas, pituitary gland tumors, or suprasellar tumors. • Associated with certain drugs: Ethanol, phenytoin, halothane, opiate antagonists, lithium
Etiologies of DI • CNS disorders that damage or create pressure in the area of the hypothalamus, pituitary stalk, or posterior pituitary gland • Head Injuries • CNS infections • Intraventricular Hemorrhage • Neurosurgical Procedures: common postoperatively with resection of craniopharyngiomas, pituitary gland tumors, or suprasellar tumors. • Associated with certain drugs: Ethanol, phenytoin, halothane, opiate antagonists, lithium
 Signs and Symptoms of DI • • • POLYURIA- first sign Low Urine osmolality (less than 100 -200 m. Osm/L) Urine specific gravity <1. 010 Hypernatremia (serum sodium greater than 145 m. Eq/L) Serum hyperosmolar (greater than 300 m. Osm/L) Thirst, polydipsia Irritability or mental status changes Dehydration Shock
Signs and Symptoms of DI • • • POLYURIA- first sign Low Urine osmolality (less than 100 -200 m. Osm/L) Urine specific gravity <1. 010 Hypernatremia (serum sodium greater than 145 m. Eq/L) Serum hyperosmolar (greater than 300 m. Osm/L) Thirst, polydipsia Irritability or mental status changes Dehydration Shock
 Clinical Management of DI • Goal is to prevent circulatory failure and hyperosmolar encephalopathy. • Replace volume deficit and ongoing losses • Replace ADH • Close monitoring of serum and urine lytes/osmolality
Clinical Management of DI • Goal is to prevent circulatory failure and hyperosmolar encephalopathy. • Replace volume deficit and ongoing losses • Replace ADH • Close monitoring of serum and urine lytes/osmolality
 Fluid Replacement • Correct Hypernatremia slowly • Bolus with NS if hypotensive • Volume deficit replaced over 24 to 48 hours • Replace ongoing urine losses
Fluid Replacement • Correct Hypernatremia slowly • Bolus with NS if hypotensive • Volume deficit replaced over 24 to 48 hours • Replace ongoing urine losses
 Vasopressin • Available IV, subcutaneous, and intranasal forms • DDAVP given intranasally • Pitressin IV • Therapeutic effect: increase in specific gravity and decrease in urine output within 1 hour of dose.
Vasopressin • Available IV, subcutaneous, and intranasal forms • DDAVP given intranasally • Pitressin IV • Therapeutic effect: increase in specific gravity and decrease in urine output within 1 hour of dose.
 Nursing Management • • Close monitoring of intake and output Frequent hemodynamic monitoring Frequent Neuro assessments Serial labs: urine specific gravity and osmolality, Serum sodium and osmolality
Nursing Management • • Close monitoring of intake and output Frequent hemodynamic monitoring Frequent Neuro assessments Serial labs: urine specific gravity and osmolality, Serum sodium and osmolality
 Complications • • Cardiac collapse Shock Cerebral Edema Herniation Death Electrolyte imbalances Water intoxication and fluid overload
Complications • • Cardiac collapse Shock Cerebral Edema Herniation Death Electrolyte imbalances Water intoxication and fluid overload
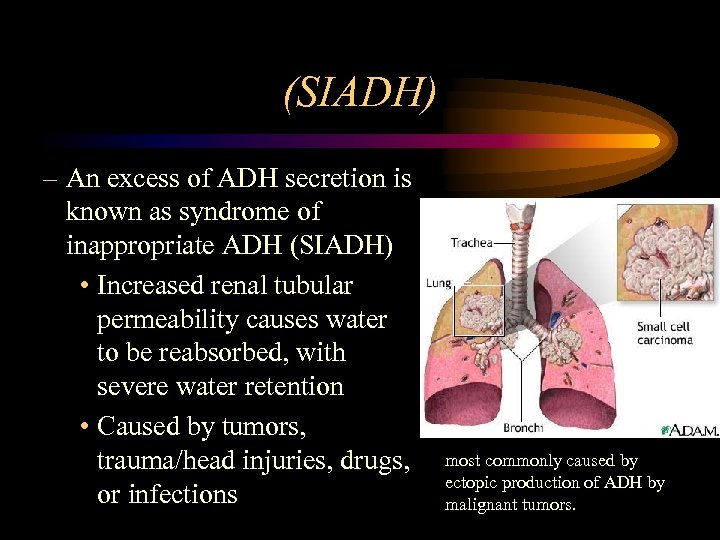 (SIADH) – An excess of ADH secretion is known as syndrome of inappropriate ADH (SIADH) • Increased renal tubular permeability causes water to be reabsorbed, with severe water retention • Caused by tumors, trauma/head injuries, drugs, or infections most commonly caused by ectopic production of ADH by malignant tumors.
(SIADH) – An excess of ADH secretion is known as syndrome of inappropriate ADH (SIADH) • Increased renal tubular permeability causes water to be reabsorbed, with severe water retention • Caused by tumors, trauma/head injuries, drugs, or infections most commonly caused by ectopic production of ADH by malignant tumors.
 Syndrome of Inappropriate Anti. Diuretic Hormone • SIADH is a clinical condition involving and excess of ADH secretion. • The patient is hyponatremic with a low serum Osmolality, which normally would inhibit ADH secretion.
Syndrome of Inappropriate Anti. Diuretic Hormone • SIADH is a clinical condition involving and excess of ADH secretion. • The patient is hyponatremic with a low serum Osmolality, which normally would inhibit ADH secretion.
 Etiology of SIADH • • • Head Trauma Cerebral Tumors Meningitis Cerebral Hemorrhage Pulmonary Diseases Chronically ill or malnourished children Spinal surgery BMT or Stem Cell Transplants Medications Positive pressure ventilation
Etiology of SIADH • • • Head Trauma Cerebral Tumors Meningitis Cerebral Hemorrhage Pulmonary Diseases Chronically ill or malnourished children Spinal surgery BMT or Stem Cell Transplants Medications Positive pressure ventilation
 Signs and Symptoms of SIADH • Low urine output in absence of hypovolemia • Hyponatremia (serum sodium<135 m. Eq/L) • Low Serum osmolality (<285 m. Osm/L) • High urine specific gravity (>1. 020) • Nausea and vomiting • Mental status changes
Signs and Symptoms of SIADH • Low urine output in absence of hypovolemia • Hyponatremia (serum sodium<135 m. Eq/L) • Low Serum osmolality (<285 m. Osm/L) • High urine specific gravity (>1. 020) • Nausea and vomiting • Mental status changes
 Clinical Management • • Normalize serum sodium over 24 to 48 hours Normalize serum osmolality Correct excess extravascular fluid volume Prevent neurological sequelae Restrict fluids 3% Na. Cl Loop diuretics
Clinical Management • • Normalize serum sodium over 24 to 48 hours Normalize serum osmolality Correct excess extravascular fluid volume Prevent neurological sequelae Restrict fluids 3% Na. Cl Loop diuretics
 Nursing Management • • • Close monitoring of intake and output Maintain fluid Restriction Frequent Hemodynamic monitoring Frequent Neuro assessments Serial labs: serum electrolytes, serum osmolality, specific gravity
Nursing Management • • • Close monitoring of intake and output Maintain fluid Restriction Frequent Hemodynamic monitoring Frequent Neuro assessments Serial labs: serum electrolytes, serum osmolality, specific gravity
 SIADH • Pulmonary-related conditions – Pneumonia – positive pressure ventilation • Pharmacologic agents – general anesthetics – thiazine diuretics – oral hypoglycemics – chemotherapeutic agents – analgesics are also
SIADH • Pulmonary-related conditions – Pneumonia – positive pressure ventilation • Pharmacologic agents – general anesthetics – thiazine diuretics – oral hypoglycemics – chemotherapeutic agents – analgesics are also
 Complications • • • Seizures Cerebral edema Cerebral hemorrhage Pulmonary edema Muscle cramps or weakness
Complications • • • Seizures Cerebral edema Cerebral hemorrhage Pulmonary edema Muscle cramps or weakness
 Triphasic response post Neurosurgery • Transient DI 12 -48 hours postop • SIADH after transient DI phase lasting up to 10 days postop • Permanent DI
Triphasic response post Neurosurgery • Transient DI 12 -48 hours postop • SIADH after transient DI phase lasting up to 10 days postop • Permanent DI
 Pituitary Gland (Master Gland) • Management of SIADH – Alleviate underlying cause – Restrict fluid intake, use of diuretics – Use of tricyclic antidepressants and demeclocycline HCL may inhibit the renal effect ADH – ADH is essential to the fluid balance of the body since it regulates urinary output – Patient and family will require encouragement and support in dealing with each disease rate
Pituitary Gland (Master Gland) • Management of SIADH – Alleviate underlying cause – Restrict fluid intake, use of diuretics – Use of tricyclic antidepressants and demeclocycline HCL may inhibit the renal effect ADH – ADH is essential to the fluid balance of the body since it regulates urinary output – Patient and family will require encouragement and support in dealing with each disease rate
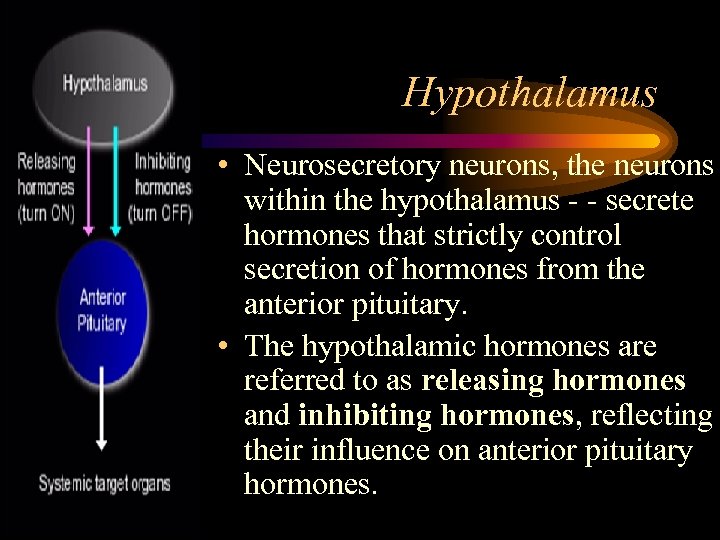 Hypothalamus • Neurosecretory neurons, the neurons within the hypothalamus - - secrete hormones that strictly control secretion of hormones from the anterior pituitary. • The hypothalamic hormones are referred to as releasing hormones and inhibiting hormones, reflecting their influence on anterior pituitary hormones.
Hypothalamus • Neurosecretory neurons, the neurons within the hypothalamus - - secrete hormones that strictly control secretion of hormones from the anterior pituitary. • The hypothalamic hormones are referred to as releasing hormones and inhibiting hormones, reflecting their influence on anterior pituitary hormones.
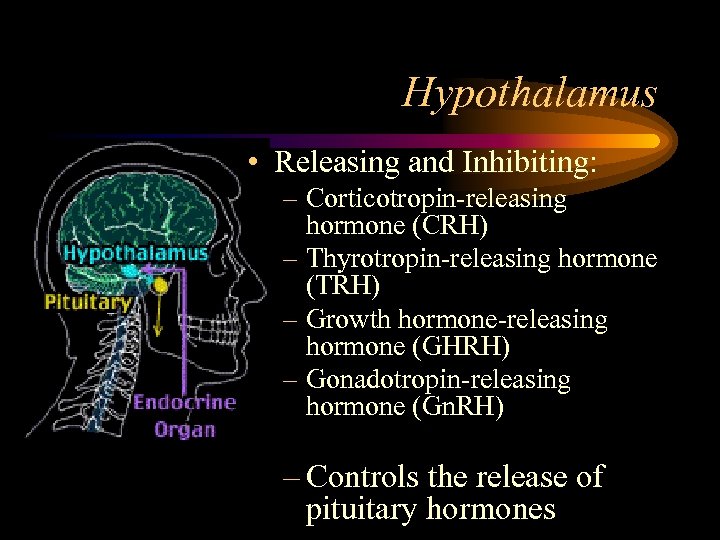 Hypothalamus • Releasing and Inhibiting: – Corticotropin-releasing hormone (CRH) – Thyrotropin-releasing hormone (TRH) – Growth hormone-releasing hormone (GHRH) – Gonadotropin-releasing hormone (Gn. RH) – Controls the release of pituitary hormones
Hypothalamus • Releasing and Inhibiting: – Corticotropin-releasing hormone (CRH) – Thyrotropin-releasing hormone (TRH) – Growth hormone-releasing hormone (GHRH) – Gonadotropin-releasing hormone (Gn. RH) – Controls the release of pituitary hormones
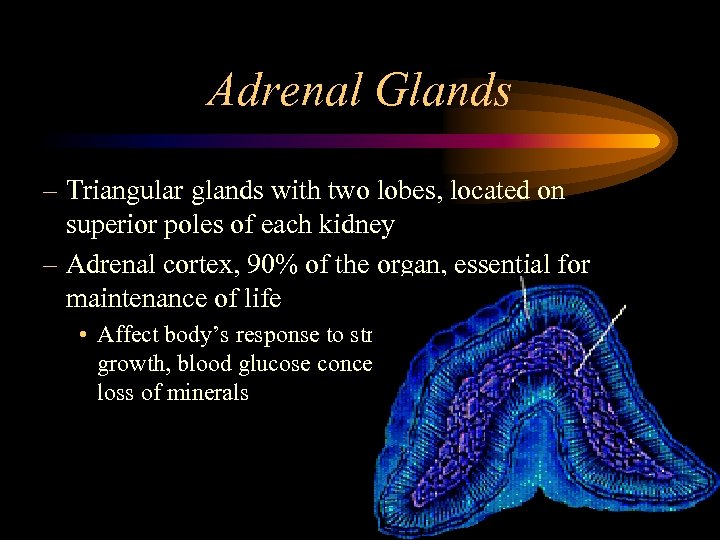 Adrenal Glands – Triangular glands with two lobes, located on superior poles of each kidney – Adrenal cortex, 90% of the organ, essential for maintenance of life • Affect body’s response to stress, metabolic rate, growth, blood glucose concentration, retention and loss of minerals
Adrenal Glands – Triangular glands with two lobes, located on superior poles of each kidney – Adrenal cortex, 90% of the organ, essential for maintenance of life • Affect body’s response to stress, metabolic rate, growth, blood glucose concentration, retention and loss of minerals
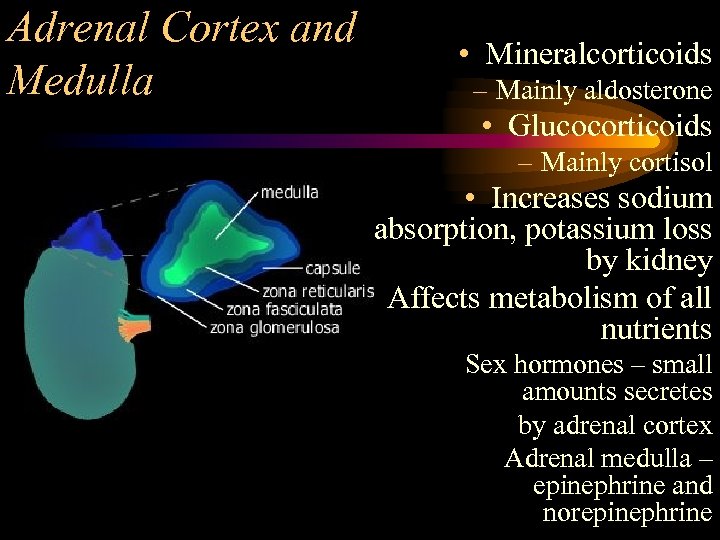 Adrenal Cortex and Medulla • Mineralcorticoids – Mainly aldosterone • Glucocorticoids – Mainly cortisol • Increases sodium absorption, potassium loss by kidney • Affects metabolism of all nutrients Sex hormones – small amounts secretes by adrenal cortex Adrenal medulla – epinephrine and norepinephrine
Adrenal Cortex and Medulla • Mineralcorticoids – Mainly aldosterone • Glucocorticoids – Mainly cortisol • Increases sodium absorption, potassium loss by kidney • Affects metabolism of all nutrients Sex hormones – small amounts secretes by adrenal cortex Adrenal medulla – epinephrine and norepinephrine
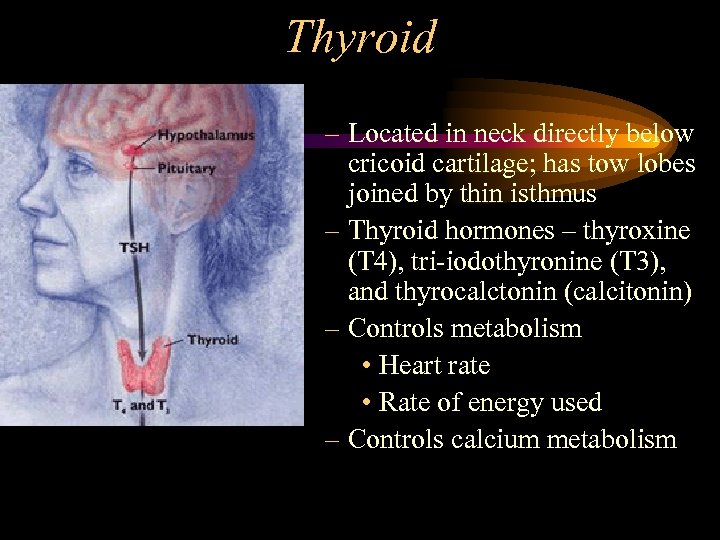 Thyroid – Located in neck directly below cricoid cartilage; has tow lobes joined by thin isthmus – Thyroid hormones – thyroxine (T 4), tri-iodothyronine (T 3), and thyrocalctonin (calcitonin) – Controls metabolism • Heart rate • Rate of energy used – Controls calcium metabolism
Thyroid – Located in neck directly below cricoid cartilage; has tow lobes joined by thin isthmus – Thyroid hormones – thyroxine (T 4), tri-iodothyronine (T 3), and thyrocalctonin (calcitonin) – Controls metabolism • Heart rate • Rate of energy used – Controls calcium metabolism
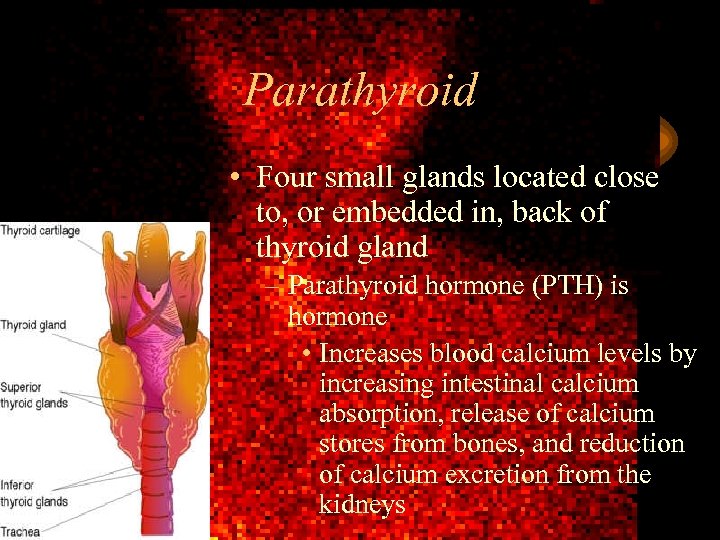 Parathyroid • Four small glands located close to, or embedded in, back of thyroid gland – Parathyroid hormone (PTH) is hormone • Increases blood calcium levels by increasing intestinal calcium absorption, release of calcium stores from bones, and reduction of calcium excretion from the kidneys
Parathyroid • Four small glands located close to, or embedded in, back of thyroid gland – Parathyroid hormone (PTH) is hormone • Increases blood calcium levels by increasing intestinal calcium absorption, release of calcium stores from bones, and reduction of calcium excretion from the kidneys
 • Place retroperitoneally behind the stomach Pancre as – Has both endocrine and exocrine functions – Islets of Langerhans’ cells • throughout pancreas • Alpha cells which secrete glucagon – Increase glucose concentration in blood • Beta cells which secrete insulin – Lower blood glucose • Delta cells which secrete somatostatin – Regulate other pancreatic hormones
• Place retroperitoneally behind the stomach Pancre as – Has both endocrine and exocrine functions – Islets of Langerhans’ cells • throughout pancreas • Alpha cells which secrete glucagon – Increase glucose concentration in blood • Beta cells which secrete insulin – Lower blood glucose • Delta cells which secrete somatostatin – Regulate other pancreatic hormones
 The End
The End


