7afe03c94eac90fc4c0c4a3bfaf7d586.ppt
- Количество слайдов: 1
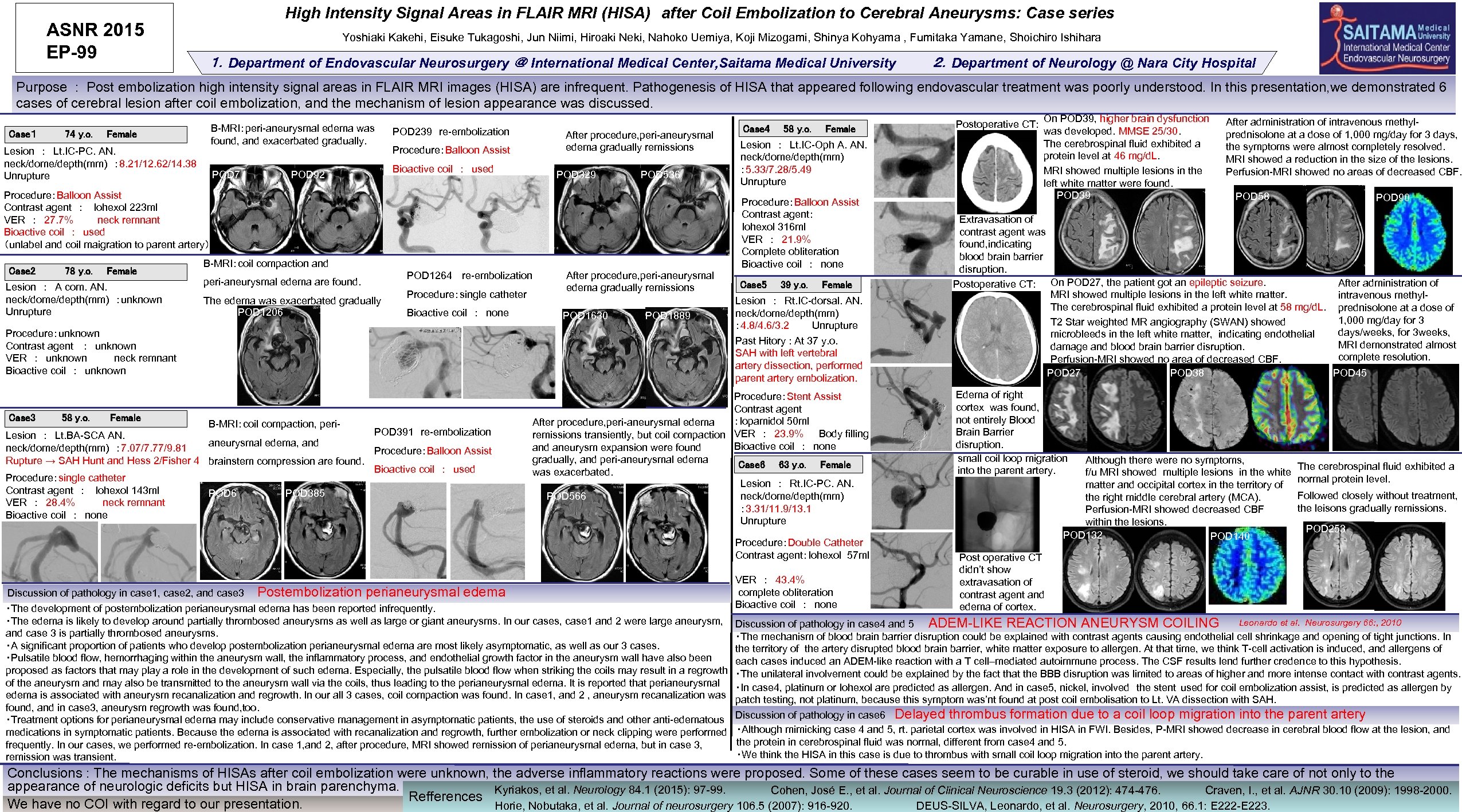 ASNR 2015 EP-99 High Intensity Signal Areas in FLAIR MRI (HISA) after Coil Embolization to Cerebral Aneurysms: Case series Yoshiaki Kakehi, Eisuke Tukagoshi, Jun Niimi, Hiroaki Neki, Nahoko Uemiya, Koji Mizogami, Shinya Kohyama , Fumitaka Yamane, Shoichiro Ishihara 1.Department of Endovascular Neurosurgery @ International Medical Center, Saitama Medical University 2.Department of Neurology @ Nara City Hospital Purpose : Post embolization high intensity signal areas in FLAIR MRI images (HISA) are infrequent. Pathogenesis of HISA that appeared following endovascular treatment was poorly understood. In this presentation, we demonstrated 6 cases of cerebral lesion after coil embolization, and the mechanism of lesion appearance was discussed. B-MRI:peri-aneurysmal edema was found, and exacerbated gradually. Case1 74 y. o. Female Lesion : Lt. IC-PC. AN. neck/dome/depth(mm) : 8. 21/12. 62/14. 38 Unrupture POD 7 POD 92 POD 239 re-embolization After procedure, peri-aneurysmal edema gradually remissions POD 329 POD 536 Procedure:Balloon Assist Bioactive coil : used Procedure:Balloon Assist Contrast agent : Iohexol 223 ml VER : 27. 7% neck remnant Bioactive coil : used (unlabel and coil maigration to parent artery) Case 2 78 y. o. Female Lesion : A com. AN. neck/dome/depth(mm) :unknown Unrupture 頭部MRI:白質病変やや軽減 B-MRI:coil compaction and peri-aneurysmal edema are found. The edema was exacerbated gradually POD 1206 POD 1264 re-embolization Procedure:single catheter Bioactive coil : none After procedure, peri-aneurysmal edema gradually remissions POD 1630 POD 1889 Procedure:unknown Contrast agent : unknown VER : unknown neck remnant Bioactive coil : unknown Case 3 58 y. o. Female B-MRI:coil compaction, peri- POD 391 re-embolization Lesion : Lt. BA-SCA AN. aneurysmal edema, and neck/dome/depth(mm) : 7. 07/7. 77/9. 81 Procedure:Balloon Assist Rupture → SAH Hunt and Hess 2/Fisher 4 brainstem compression are found. Bioactive coil : used Procedure:single catheter Contrast agent : Iohexol 143 ml POD 6 POD 385 VER : 28. 4% neck remnant Bioactive coil : none Case 4 58 y. o. Female Lesion : Lt. IC-Oph A. AN. neck/dome/depth(mm) : 5. 33/7. 28/5. 49 Unrupture Procedure:Balloon Assist Contrast agent: Iohexol 316 ml VER : 21. 9% Complete obliteration Bioactive coil : none Case 5 39 y. o. Female Lesion : Rt. IC-dorsal. AN. neck/dome/depth(mm) : 4. 8/4. 6/3. 2 Unrupture Past Hitory : At 37 y. o. SAH with left vertebral artery dissection, performed parent artery embolization. Procedure:Stent Assist Contrast agent :Iopamidol 50 ml After procedure, peri-aneurysmal edema remissions transiently, but coil compaction VER : 23. 9% Body filling Bioactive coil : none and aneurysm expansion were found gradually, and peri-aneurysmal edema Case 6 63 y. o. Female was exacerbated. Lesion : Rt. IC-PC. AN. neck/dome/depth(mm) POD 566 : 3. 31/11. 9/13. 1 Unrupture Discussion of pathology in case 1, case 2, and case 3 Postembolization perianeurysmal edema ・The development of postembolization perianeurysmal edema has been reported infrequently. ・The edema is likely to develop around partially thrombosed aneurysms as well as large or giant aneurysms. In our cases, case 1 and 2 were large aneurysm, and case 3 is partially thrombosed aneurysms. ・A significant proportion of patients who develop postembolization perianeurysmal edema are most likely asymptomatic, as well as our 3 cases. ・Pulsatile blood flow, hemorrhaging within the aneurysm wall, the inflammatory process, and endothelial growth factor in the aneurysm wall have also been proposed as factors that may play a role in the development of such edema. Especially, the pulsatile blood flow when striking the coils may result in a regrowth of the aneurysm and may also be transmitted to the aneurysm wall via the coils, thus leading to the perianeurysmal edema. It is reported that perianeurysmal edema is associated with aneurysm recanalization and regrowth. In our all 3 cases, coil compaction was found. In case 1, and 2 , aneurysm recanalization was found, and in case 3, aneurysm regrowth was found, too. ・Treatment options for perianeurysmal edema may include conservative management in asymptomatic patients, the use of steroids and other anti-edematous medications in symptomatic patients. Because the edema is associated with recanalization and regrowth, further embolization or neck clipping were performed frequently. In our cases, we performed re-embolization. In case 1, and 2, after procedure, MRI showed remission of perianeurysmal edema, but in case 3, remission was transient. Procedure:Double Catheter Contrast agent:Iohexol 57 ml VER : 43. 4% complete obliteration Bioactive coil : none Postoperative CT: On POD 39, higher brain dysfunction was developed. MMSE 25/30. The cerebrospinal fluid exhibited a protein level at 46 mg/d. L. MRI showed multiple lesions in the left white matter were found. POD 39 After administration of intravenous methylprednisolone at a dose of 1, 000 mg/day for 3 days, the symptoms were almost completely resolved. MRI showed a reduction in the size of the lesions. Perfusion-MRI showed no areas of decreased CBF. POD 58 POD 90 Extravasation of contrast agent was found, indicating blood brain barrier disruption. After administration of Postoperative CT: On POD 27, the patient got an epileptic seizure. MRI showed multiple lesions in the left white matter. intravenous methyl. The cerebrospinal fluid exhibited a protein level at 58 mg/d. L. prednisolone at a dose of 1, 000 mg/day for 3 T 2 Star weighted MR angiography (SWAN) showed days/weeks, for 3 weeks, microbleeds in the left white matter, indicating endothelial MRI demonstrated almost damage and blood brain barrier disruption. complete resolution. Perfusion-MRI showed no area of decreased CBF. POD 27 POD 38 POD 45 Edema of right cortex was found, not entirely Blood Brain Barrier disruption. small coil loop migration into the parent artery. Although there were no symptoms, f/u MRI showed multiple lesions in the white matter and occipital cortex in the territory of the right middle cerebral artery (MCA). Perfusion-MRI showed decreased CBF within the lesions. POD 132 POD 140 The cerebrospinal fluid exhibited a normal protein level. Followed closely without treatment, the leisons gradually remissions. POD 253 Post operative CT didn’t show extravasation of contrast agent and edema of cortex. Leonardo et al. Neurosurgery 66: , 2010 Discussion of pathology in case 4 and 5 ADEM-LIKE REACTION ANEURYSM COILING ・The mechanism of blood brain barrier disruption could be explained with contrast agents causing endothelial cell shrinkage and opening of tight junctions. In the territory of the artery disrupted blood brain barrier, white matter exposure to allergen. At that time, we think T-cell activation is induced, and allergens of each cases induced an ADEM-like reaction with a T cell–mediated autoimmune process. The CSF results lend further credence to this hypothesis. ・The unilateral involvement could be explained by the fact that the BBB disruption was limited to areas of higher and more intense contact with contrast agents. ・In case 4, platinum or Iohexol are predicted as allergen. And in case 5, nickel, involved the stent used for coil embolization assist, is predicted as allergen by patch testing, not platinum, because this symptom was’nt found at post coil embolisation to Lt. VA dissection with SAH. Discussion of pathology in case 6 Delayed thrombus formation due to a coil loop migration into the parent artery ・Although mimicking case 4 and 5, rt. parietal cortex was involved in HISA in FWI. Besides, P-MRI showed decrease in cerebral blood flow at the lesion, and the protein in cerebrospinal fluid was normal, different from case 4 and 5. ・We think the HISA in this case is due to thrombus with small coil loop migration into the parent artery. Conclusions : The mechanisms of HISAs after coil embolization were unknown, the adverse inflammatory reactions were proposed. Some of these cases seem to be curable in use of steroid, we should take care of not only to the appearance of neurologic deficits but HISA in brain parenchyma. Kyriakos, et al. Neurology 84. 1 (2015): 97 -99. Cohen, José E. , et al. Journal of Clinical Neuroscience 19. 3 (2012): 474 -476. Craven, I. , et al. AJNR 30. 10 (2009): 1998 -2000. Refferences We have no COI with regard to our presentation. Horie, Nobutaka, et al. Journal of neurosurgery 106. 5 (2007): 916 -920. DEUS-SILVA, Leonardo, et al. Neurosurgery, 2010, 66. 1: E 222 -E 223.
ASNR 2015 EP-99 High Intensity Signal Areas in FLAIR MRI (HISA) after Coil Embolization to Cerebral Aneurysms: Case series Yoshiaki Kakehi, Eisuke Tukagoshi, Jun Niimi, Hiroaki Neki, Nahoko Uemiya, Koji Mizogami, Shinya Kohyama , Fumitaka Yamane, Shoichiro Ishihara 1.Department of Endovascular Neurosurgery @ International Medical Center, Saitama Medical University 2.Department of Neurology @ Nara City Hospital Purpose : Post embolization high intensity signal areas in FLAIR MRI images (HISA) are infrequent. Pathogenesis of HISA that appeared following endovascular treatment was poorly understood. In this presentation, we demonstrated 6 cases of cerebral lesion after coil embolization, and the mechanism of lesion appearance was discussed. B-MRI:peri-aneurysmal edema was found, and exacerbated gradually. Case1 74 y. o. Female Lesion : Lt. IC-PC. AN. neck/dome/depth(mm) : 8. 21/12. 62/14. 38 Unrupture POD 7 POD 92 POD 239 re-embolization After procedure, peri-aneurysmal edema gradually remissions POD 329 POD 536 Procedure:Balloon Assist Bioactive coil : used Procedure:Balloon Assist Contrast agent : Iohexol 223 ml VER : 27. 7% neck remnant Bioactive coil : used (unlabel and coil maigration to parent artery) Case 2 78 y. o. Female Lesion : A com. AN. neck/dome/depth(mm) :unknown Unrupture 頭部MRI:白質病変やや軽減 B-MRI:coil compaction and peri-aneurysmal edema are found. The edema was exacerbated gradually POD 1206 POD 1264 re-embolization Procedure:single catheter Bioactive coil : none After procedure, peri-aneurysmal edema gradually remissions POD 1630 POD 1889 Procedure:unknown Contrast agent : unknown VER : unknown neck remnant Bioactive coil : unknown Case 3 58 y. o. Female B-MRI:coil compaction, peri- POD 391 re-embolization Lesion : Lt. BA-SCA AN. aneurysmal edema, and neck/dome/depth(mm) : 7. 07/7. 77/9. 81 Procedure:Balloon Assist Rupture → SAH Hunt and Hess 2/Fisher 4 brainstem compression are found. Bioactive coil : used Procedure:single catheter Contrast agent : Iohexol 143 ml POD 6 POD 385 VER : 28. 4% neck remnant Bioactive coil : none Case 4 58 y. o. Female Lesion : Lt. IC-Oph A. AN. neck/dome/depth(mm) : 5. 33/7. 28/5. 49 Unrupture Procedure:Balloon Assist Contrast agent: Iohexol 316 ml VER : 21. 9% Complete obliteration Bioactive coil : none Case 5 39 y. o. Female Lesion : Rt. IC-dorsal. AN. neck/dome/depth(mm) : 4. 8/4. 6/3. 2 Unrupture Past Hitory : At 37 y. o. SAH with left vertebral artery dissection, performed parent artery embolization. Procedure:Stent Assist Contrast agent :Iopamidol 50 ml After procedure, peri-aneurysmal edema remissions transiently, but coil compaction VER : 23. 9% Body filling Bioactive coil : none and aneurysm expansion were found gradually, and peri-aneurysmal edema Case 6 63 y. o. Female was exacerbated. Lesion : Rt. IC-PC. AN. neck/dome/depth(mm) POD 566 : 3. 31/11. 9/13. 1 Unrupture Discussion of pathology in case 1, case 2, and case 3 Postembolization perianeurysmal edema ・The development of postembolization perianeurysmal edema has been reported infrequently. ・The edema is likely to develop around partially thrombosed aneurysms as well as large or giant aneurysms. In our cases, case 1 and 2 were large aneurysm, and case 3 is partially thrombosed aneurysms. ・A significant proportion of patients who develop postembolization perianeurysmal edema are most likely asymptomatic, as well as our 3 cases. ・Pulsatile blood flow, hemorrhaging within the aneurysm wall, the inflammatory process, and endothelial growth factor in the aneurysm wall have also been proposed as factors that may play a role in the development of such edema. Especially, the pulsatile blood flow when striking the coils may result in a regrowth of the aneurysm and may also be transmitted to the aneurysm wall via the coils, thus leading to the perianeurysmal edema. It is reported that perianeurysmal edema is associated with aneurysm recanalization and regrowth. In our all 3 cases, coil compaction was found. In case 1, and 2 , aneurysm recanalization was found, and in case 3, aneurysm regrowth was found, too. ・Treatment options for perianeurysmal edema may include conservative management in asymptomatic patients, the use of steroids and other anti-edematous medications in symptomatic patients. Because the edema is associated with recanalization and regrowth, further embolization or neck clipping were performed frequently. In our cases, we performed re-embolization. In case 1, and 2, after procedure, MRI showed remission of perianeurysmal edema, but in case 3, remission was transient. Procedure:Double Catheter Contrast agent:Iohexol 57 ml VER : 43. 4% complete obliteration Bioactive coil : none Postoperative CT: On POD 39, higher brain dysfunction was developed. MMSE 25/30. The cerebrospinal fluid exhibited a protein level at 46 mg/d. L. MRI showed multiple lesions in the left white matter were found. POD 39 After administration of intravenous methylprednisolone at a dose of 1, 000 mg/day for 3 days, the symptoms were almost completely resolved. MRI showed a reduction in the size of the lesions. Perfusion-MRI showed no areas of decreased CBF. POD 58 POD 90 Extravasation of contrast agent was found, indicating blood brain barrier disruption. After administration of Postoperative CT: On POD 27, the patient got an epileptic seizure. MRI showed multiple lesions in the left white matter. intravenous methyl. The cerebrospinal fluid exhibited a protein level at 58 mg/d. L. prednisolone at a dose of 1, 000 mg/day for 3 T 2 Star weighted MR angiography (SWAN) showed days/weeks, for 3 weeks, microbleeds in the left white matter, indicating endothelial MRI demonstrated almost damage and blood brain barrier disruption. complete resolution. Perfusion-MRI showed no area of decreased CBF. POD 27 POD 38 POD 45 Edema of right cortex was found, not entirely Blood Brain Barrier disruption. small coil loop migration into the parent artery. Although there were no symptoms, f/u MRI showed multiple lesions in the white matter and occipital cortex in the territory of the right middle cerebral artery (MCA). Perfusion-MRI showed decreased CBF within the lesions. POD 132 POD 140 The cerebrospinal fluid exhibited a normal protein level. Followed closely without treatment, the leisons gradually remissions. POD 253 Post operative CT didn’t show extravasation of contrast agent and edema of cortex. Leonardo et al. Neurosurgery 66: , 2010 Discussion of pathology in case 4 and 5 ADEM-LIKE REACTION ANEURYSM COILING ・The mechanism of blood brain barrier disruption could be explained with contrast agents causing endothelial cell shrinkage and opening of tight junctions. In the territory of the artery disrupted blood brain barrier, white matter exposure to allergen. At that time, we think T-cell activation is induced, and allergens of each cases induced an ADEM-like reaction with a T cell–mediated autoimmune process. The CSF results lend further credence to this hypothesis. ・The unilateral involvement could be explained by the fact that the BBB disruption was limited to areas of higher and more intense contact with contrast agents. ・In case 4, platinum or Iohexol are predicted as allergen. And in case 5, nickel, involved the stent used for coil embolization assist, is predicted as allergen by patch testing, not platinum, because this symptom was’nt found at post coil embolisation to Lt. VA dissection with SAH. Discussion of pathology in case 6 Delayed thrombus formation due to a coil loop migration into the parent artery ・Although mimicking case 4 and 5, rt. parietal cortex was involved in HISA in FWI. Besides, P-MRI showed decrease in cerebral blood flow at the lesion, and the protein in cerebrospinal fluid was normal, different from case 4 and 5. ・We think the HISA in this case is due to thrombus with small coil loop migration into the parent artery. Conclusions : The mechanisms of HISAs after coil embolization were unknown, the adverse inflammatory reactions were proposed. Some of these cases seem to be curable in use of steroid, we should take care of not only to the appearance of neurologic deficits but HISA in brain parenchyma. Kyriakos, et al. Neurology 84. 1 (2015): 97 -99. Cohen, José E. , et al. Journal of Clinical Neuroscience 19. 3 (2012): 474 -476. Craven, I. , et al. AJNR 30. 10 (2009): 1998 -2000. Refferences We have no COI with regard to our presentation. Horie, Nobutaka, et al. Journal of neurosurgery 106. 5 (2007): 916 -920. DEUS-SILVA, Leonardo, et al. Neurosurgery, 2010, 66. 1: E 222 -E 223.


