ARTICULAR SYSTEM2.ppt
- Количество слайдов: 61
 ARTICULAR SYSTEM GENERAL INFORMATION
ARTICULAR SYSTEM GENERAL INFORMATION
 PLAN: 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. Development of joints. Classification of bone articulations. Continuous bone articulations. Synovial joints. The most typical features of the joints. Accessory structures of joints. Congruent and incongruent joints. Movements in the joints. Classification of the joints based on the number of articulating surfaces. Classification of the joints based on the shape of articulating surfaces. Clinical applications.
PLAN: 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. Development of joints. Classification of bone articulations. Continuous bone articulations. Synovial joints. The most typical features of the joints. Accessory structures of joints. Congruent and incongruent joints. Movements in the joints. Classification of the joints based on the number of articulating surfaces. Classification of the joints based on the shape of articulating surfaces. Clinical applications.
 Development of joints Embryonic development of the joints is greatly dependent on the bone development. In the areas, where discontinuous articulations will form between the developing bones, the mesenchyme is resorbed in the center of the primordium forming a cleft like cavity of the future joint. On the contrary, peripheral regions of the mesenchyme, which surround the cavity, condense, giving rise to the fibrous capsule and ligaments of the joint. Cartilaginous epiphyses ossify in such away that a thin layer of articular cartilage remains on their surfaces for life, which provides the smoothness of articular surfaces.
Development of joints Embryonic development of the joints is greatly dependent on the bone development. In the areas, where discontinuous articulations will form between the developing bones, the mesenchyme is resorbed in the center of the primordium forming a cleft like cavity of the future joint. On the contrary, peripheral regions of the mesenchyme, which surround the cavity, condense, giving rise to the fibrous capsule and ligaments of the joint. Cartilaginous epiphyses ossify in such away that a thin layer of articular cartilage remains on their surfaces for life, which provides the smoothness of articular surfaces.
 CLASSIFICATION OF BONE ARTICULATIONS n n n Continuous articulations(synarthroses) are characterized by the presence of an uninterrupted articulating tissue connective, cartilaginous, or osseous. Such articulations are either slightly movable or completely fixed. Discontinuous (synovial) articulations contain a cavity lined with the synovial membrane. They possess a great mobility. They are called joints. Intermediate forms between the continuous and discontinuous articulations are symphyses (or hemiarthroses). They are represented by the cartilaginous articulations with the cleft like cavity lacking a fibrous capsule and without synovial membrane.
CLASSIFICATION OF BONE ARTICULATIONS n n n Continuous articulations(synarthroses) are characterized by the presence of an uninterrupted articulating tissue connective, cartilaginous, or osseous. Such articulations are either slightly movable or completely fixed. Discontinuous (synovial) articulations contain a cavity lined with the synovial membrane. They possess a great mobility. They are called joints. Intermediate forms between the continuous and discontinuous articulations are symphyses (or hemiarthroses). They are represented by the cartilaginous articulations with the cleft like cavity lacking a fibrous capsule and without synovial membrane.
 CONTINUOUS BONE ARTICULATIONS Depending on the tissue type, which articulates two bones, continuous articulations are divided into n fibrous, syndesmoses, n cartilaginous, synchondroses, n osseous, synostoses.
CONTINUOUS BONE ARTICULATIONS Depending on the tissue type, which articulates two bones, continuous articulations are divided into n fibrous, syndesmoses, n cartilaginous, synchondroses, n osseous, synostoses.
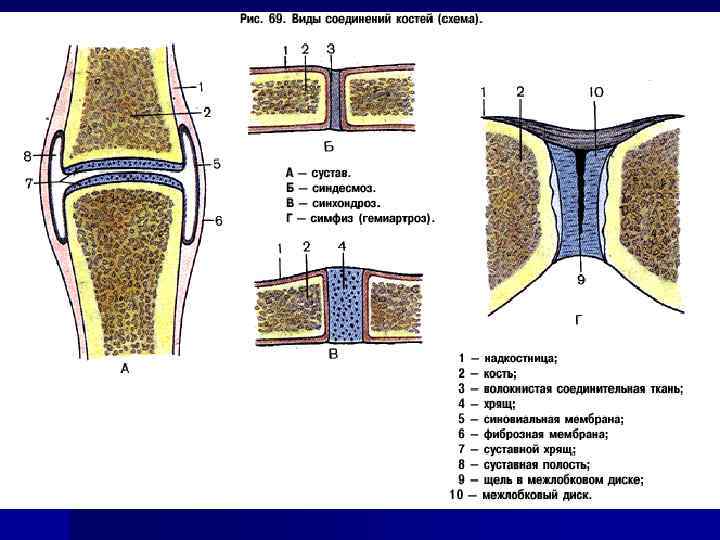
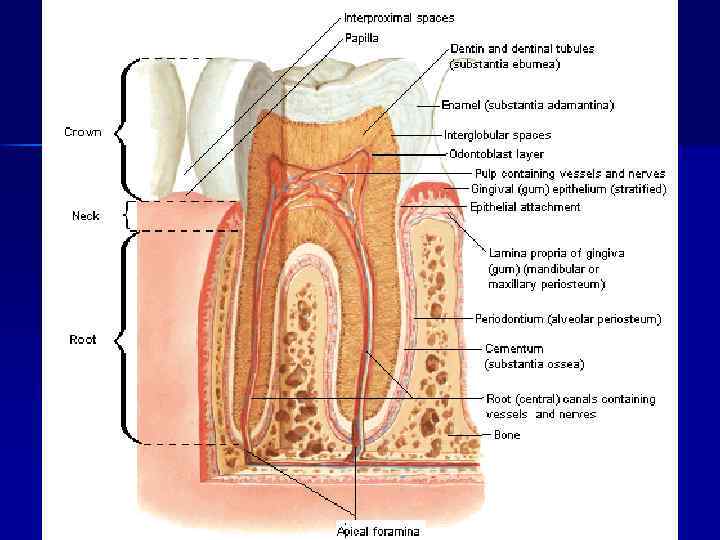
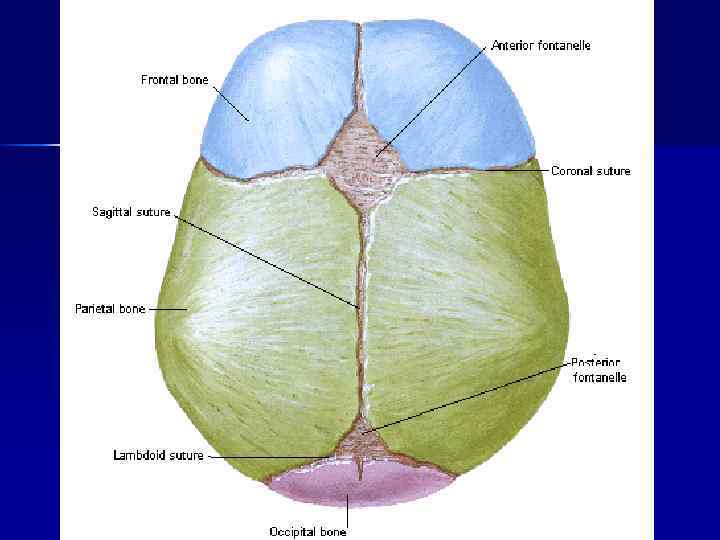
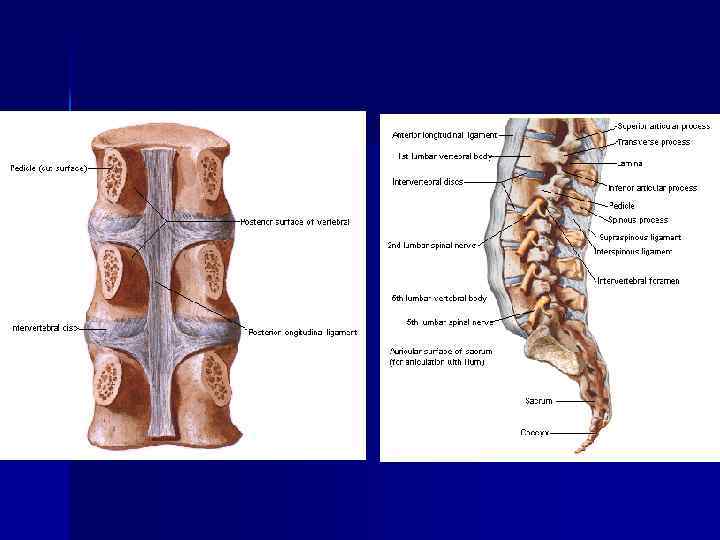
 Syndesmoses, syndesmosis, (juncturae fibrosae) are formed from the fibrous connective tissue and are divided into the following groups: n gomphosis, dentoalveolar syndesmosis, a fibrous articulation n sutures, sutura, fibrous articulations between the bones of the skull, which n fontanelles, fonticuli, between bones of skull of the new born; n interosseous membranes, membranae interosseae; n ligaments, ligamenta, most of the ligaments consist of a dense regular between the periodontium of alveolar socket and the root of the tooth; contain a thin layer of connective tissue; connective tissue. Fibers in the ligaments run obliquely and cross over like in the rope. Therefore, ligaments are quite resilient. Collagen fibers of the ligaments, besides resiliency, provide great elasticity. Some ligaments, besides collagen fibers, contain a considerable amount of elastic tissue yellow in color. They are characterized by lower resilience but greater elasticity. They perform a shock absorbing function (e. g. yellow ligaments of the vertebral column). Because of their low resilience, elastic ligaments are not very common in the body.
Syndesmoses, syndesmosis, (juncturae fibrosae) are formed from the fibrous connective tissue and are divided into the following groups: n gomphosis, dentoalveolar syndesmosis, a fibrous articulation n sutures, sutura, fibrous articulations between the bones of the skull, which n fontanelles, fonticuli, between bones of skull of the new born; n interosseous membranes, membranae interosseae; n ligaments, ligamenta, most of the ligaments consist of a dense regular between the periodontium of alveolar socket and the root of the tooth; contain a thin layer of connective tissue; connective tissue. Fibers in the ligaments run obliquely and cross over like in the rope. Therefore, ligaments are quite resilient. Collagen fibers of the ligaments, besides resiliency, provide great elasticity. Some ligaments, besides collagen fibers, contain a considerable amount of elastic tissue yellow in color. They are characterized by lower resilience but greater elasticity. They perform a shock absorbing function (e. g. yellow ligaments of the vertebral column). Because of their low resilience, elastic ligaments are not very common in the body.
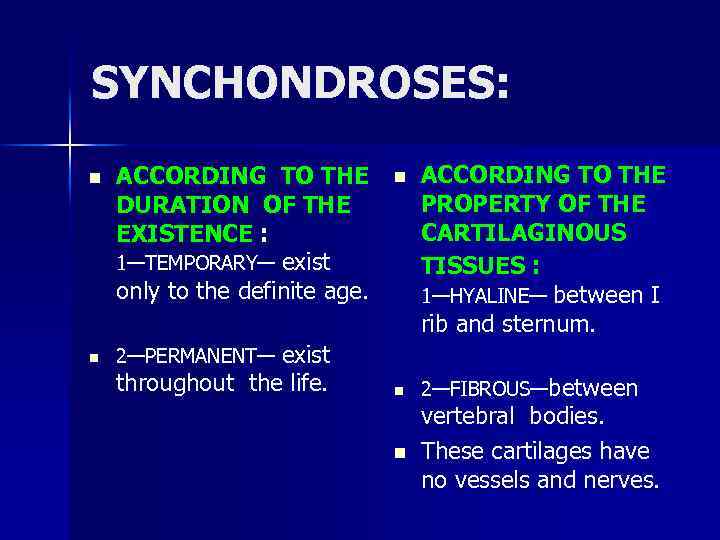 SYNCHONDROSES: n n ACCORDING TO THE PROPERTY OF THE DURATION OF THE EXISTENCE : CARTILAGINOUS 1—TEMPORARY— exist TISSUES : only to the definite age. 1—HYALINE— between I rib and sternum. 2—PERMANENT— exist throughout the life. n 2—FIBROUS—between vertebral bodies. n These cartilages have no vessels and nerves.
SYNCHONDROSES: n n ACCORDING TO THE PROPERTY OF THE DURATION OF THE EXISTENCE : CARTILAGINOUS 1—TEMPORARY— exist TISSUES : only to the definite age. 1—HYALINE— between I rib and sternum. 2—PERMANENT— exist throughout the life. n 2—FIBROUS—between vertebral bodies. n These cartilages have no vessels and nerves.
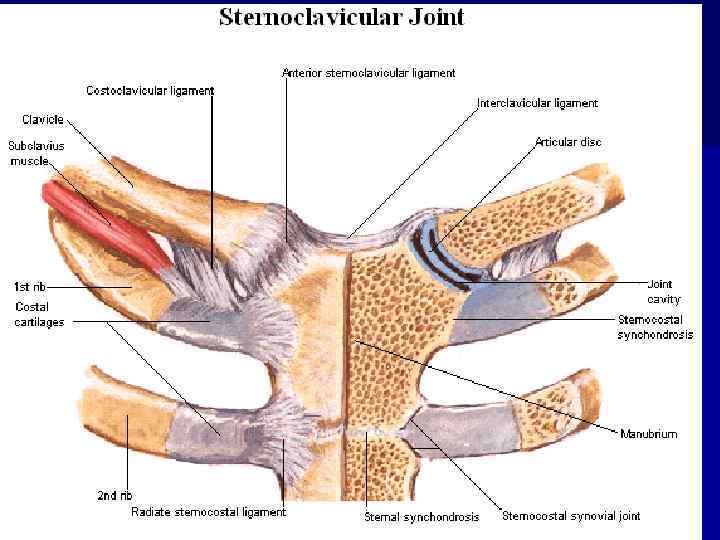
 When ossified, synchondrosis can be transformed into the osseous articulation synostosis (synostosis). Synostoses or bone articulations (junctura ossea) is contiguous joining of bones by means of bone tissue, for instance, synostoses between three bones of the hip bone in an adult.
When ossified, synchondrosis can be transformed into the osseous articulation synostosis (synostosis). Synostoses or bone articulations (junctura ossea) is contiguous joining of bones by means of bone tissue, for instance, synostoses between three bones of the hip bone in an adult.
 SYNOVIAL JOINTS The synovial articulations (juncturae synoviales, articulatio, diarthrosis) are discontinuous joints characterized by the presence of the synovial membrane. They are also characterized by a variety of movement amplitudes. Consequently these joints are most common in higher vertebrates and humans.
SYNOVIAL JOINTS The synovial articulations (juncturae synoviales, articulatio, diarthrosis) are discontinuous joints characterized by the presence of the synovial membrane. They are also characterized by a variety of movement amplitudes. Consequently these joints are most common in higher vertebrates and humans.
 THE MOST TYPICAL FEATURES OF THE JOINTS Each joint possesses four basic elements: n articular surfaces, facies articulares; n articular capsule, capsula articularis; n articular cavity, cavitas articularis hermetically sealed, cleft like cavity; between the articulating bones. n synovial fluid
THE MOST TYPICAL FEATURES OF THE JOINTS Each joint possesses four basic elements: n articular surfaces, facies articulares; n articular capsule, capsula articularis; n articular cavity, cavitas articularis hermetically sealed, cleft like cavity; between the articulating bones. n synovial fluid
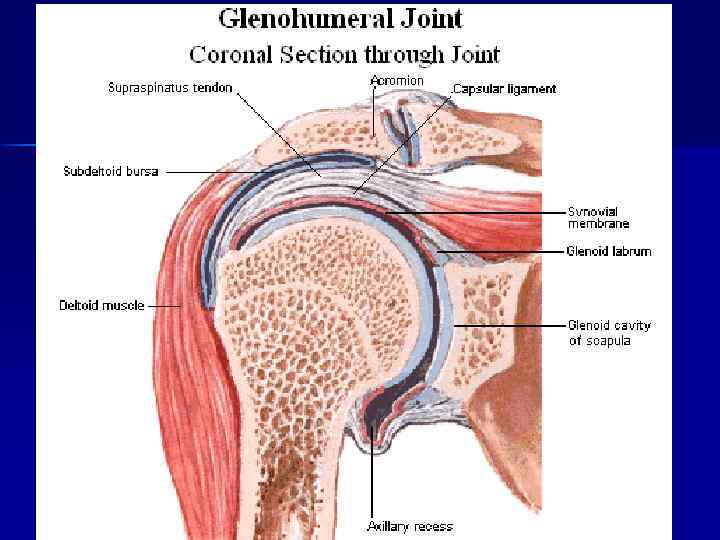
 Articular surfaces. The articular surfaces of the bones are covered with the hyaline cartilage (sometimes fibrous), which is 2. 5 mm thick on average. The thickness of the cartilage depends on the amount of compression experienced by the joint. The surface of the cartilage is not covered with the perichondrium. The surface is smooth lubricated with the synovial fluid which reduces friction to minimum and facilitates the movement. Articular capsule. The capsule of the joint attaches to the edges of articular surfaces or somewhat over them. The articular capsule hermetically seals the articular cavity and consists of two layers external fibrous layer, membrana fibrosa, and internal synovial layer, membrana synovialis. n n The fibrous layer of the capsule has a mechanical function. It consists of bundles of resilient connective tissue fibers, which attach to the bone penetrating it in the form of Sharpie's fibers. Synovial membrane. This layer of the articular capsule is a thin connective tissue membrane, which is lined on the inside with squamous synovial cells of mesenchymatous origin. Consequently, the synovial membrane can form folds and protrusions.
Articular surfaces. The articular surfaces of the bones are covered with the hyaline cartilage (sometimes fibrous), which is 2. 5 mm thick on average. The thickness of the cartilage depends on the amount of compression experienced by the joint. The surface of the cartilage is not covered with the perichondrium. The surface is smooth lubricated with the synovial fluid which reduces friction to minimum and facilitates the movement. Articular capsule. The capsule of the joint attaches to the edges of articular surfaces or somewhat over them. The articular capsule hermetically seals the articular cavity and consists of two layers external fibrous layer, membrana fibrosa, and internal synovial layer, membrana synovialis. n n The fibrous layer of the capsule has a mechanical function. It consists of bundles of resilient connective tissue fibers, which attach to the bone penetrating it in the form of Sharpie's fibers. Synovial membrane. This layer of the articular capsule is a thin connective tissue membrane, which is lined on the inside with squamous synovial cells of mesenchymatous origin. Consequently, the synovial membrane can form folds and protrusions.
 n n Synovial folds and bursae. The synovial membrane is well developed and, in the majority of the joints forms large folds, plicae synoviales, which contain adipose tissue. They go into the articular cavity, filling its potential spaces and forming cushions, which absorb shock during motion. In certain regions, most frequently in the areas of muscular tendons, the synovial membrane protrudes through the clefts in the fibrous layer and forms synovial bursae. They serve to reduce friction during tendons' movement and can be attributed to the accessory muscular apparatus. Synovial villi. The synovial layer bears numerous, microscopic, synovial villi, villi synoviales, which significantly increase its surface area, contain capillary networks, and produce the synovial fluid. n Synovial fluid. In the articular cavity there is a small amount of pale, thick, synovial fluid. It is produced by the synovial membrane. The synovial fluid lubricates the articular surfaces and reduces friction between them. n Synovial cavity. Under normal circumstances, the synovial cavity is a thin cleft, bounded by the synovial membrane and the articular surfaces. Between the latter, there is a thin layer of synovial fluid, which separates articulating surfaces. In the pathological processes, the synovial cavity can accumulate large amounts of inflammatory liquid and greatly increases in size.
n n Synovial folds and bursae. The synovial membrane is well developed and, in the majority of the joints forms large folds, plicae synoviales, which contain adipose tissue. They go into the articular cavity, filling its potential spaces and forming cushions, which absorb shock during motion. In certain regions, most frequently in the areas of muscular tendons, the synovial membrane protrudes through the clefts in the fibrous layer and forms synovial bursae. They serve to reduce friction during tendons' movement and can be attributed to the accessory muscular apparatus. Synovial villi. The synovial layer bears numerous, microscopic, synovial villi, villi synoviales, which significantly increase its surface area, contain capillary networks, and produce the synovial fluid. n Synovial fluid. In the articular cavity there is a small amount of pale, thick, synovial fluid. It is produced by the synovial membrane. The synovial fluid lubricates the articular surfaces and reduces friction between them. n Synovial cavity. Under normal circumstances, the synovial cavity is a thin cleft, bounded by the synovial membrane and the articular surfaces. Between the latter, there is a thin layer of synovial fluid, which separates articulating surfaces. In the pathological processes, the synovial cavity can accumulate large amounts of inflammatory liquid and greatly increases in size.
 Accessory structures of joints Synovial joints may possess several accessory elements, which facilitate movement to a certain extent: n n articular disc, discus articularis, a cartilaginous plate, which completely separates the joint into two regions; articular meniscus, meniscus articularis, cartilaginous semilunar plate, which partially separates the synovial cavity; articular lip, labrum articularis, a cartilaginous rim or lip, which deepens the articular socket; intraarticular ligaments, ligg. intraarticularia, connect bones within the joint; they are covered with the synovial membrane. Auxiliary strengthening apparatus of joints – ligaments and tendons of muscles. There are extra articular and intra articular ligaments, covered by synovial membranes.
Accessory structures of joints Synovial joints may possess several accessory elements, which facilitate movement to a certain extent: n n articular disc, discus articularis, a cartilaginous plate, which completely separates the joint into two regions; articular meniscus, meniscus articularis, cartilaginous semilunar plate, which partially separates the synovial cavity; articular lip, labrum articularis, a cartilaginous rim or lip, which deepens the articular socket; intraarticular ligaments, ligg. intraarticularia, connect bones within the joint; they are covered with the synovial membrane. Auxiliary strengthening apparatus of joints – ligaments and tendons of muscles. There are extra articular and intra articular ligaments, covered by synovial membranes.
 Factors, which aid in the stabilization of articular surfaces: n n n The fibrous capsule, which is reinforced by the ligaments; Muscles, which surround the joint and actively hold the bones together due to a constant muscle tone; Molecular attraction of articular surfaces, lubricated by the synovial fluid.
Factors, which aid in the stabilization of articular surfaces: n n n The fibrous capsule, which is reinforced by the ligaments; Muscles, which surround the joint and actively hold the bones together due to a constant muscle tone; Molecular attraction of articular surfaces, lubricated by the synovial fluid.
 Congruent and incongruent joints In those cases, when articulating surfaces entirely correspond to each other and appear as imprints of one another, joints are called congruent (congruo correspond). In such joints, articular surfaces are tightly joined together as, for example, in the hip joint, in which movements are largely restricted. Incongruent joints have a greater degree of freedom in their movements due to the incomplete correspondence of the articulating surfaces. These joints possess accessory structures such as disks, menisci, synovial folds, which fill the irregularities in the articular surfaces and smooth out their incongruence. The knee joint is an example of the incongruent joint.
Congruent and incongruent joints In those cases, when articulating surfaces entirely correspond to each other and appear as imprints of one another, joints are called congruent (congruo correspond). In such joints, articular surfaces are tightly joined together as, for example, in the hip joint, in which movements are largely restricted. Incongruent joints have a greater degree of freedom in their movements due to the incomplete correspondence of the articulating surfaces. These joints possess accessory structures such as disks, menisci, synovial folds, which fill the irregularities in the articular surfaces and smooth out their incongruence. The knee joint is an example of the incongruent joint.
 Movements in the joints n The frontal axis runs through the joint from right to left. Flexion (flexio) and extension (extensio) of the shoulder occur around the frontal axis. n The sagittal axis is drawn from front to back. Abduction (abductio) and adduction (adductio) of the shoulder occur around this axis. n The vertical axis runs through the joint and through the entire arm from the top to the bottom. Medial and lateral rotations (rotatio) of the humerus occur around this axis. n Circumduction (circumductio) takes place when the movement passes from one axis to another, as when the hand moves in a circular path. Circular movements are possible in multi axial and bi axial joints.
Movements in the joints n The frontal axis runs through the joint from right to left. Flexion (flexio) and extension (extensio) of the shoulder occur around the frontal axis. n The sagittal axis is drawn from front to back. Abduction (abductio) and adduction (adductio) of the shoulder occur around this axis. n The vertical axis runs through the joint and through the entire arm from the top to the bottom. Medial and lateral rotations (rotatio) of the humerus occur around this axis. n Circumduction (circumductio) takes place when the movement passes from one axis to another, as when the hand moves in a circular path. Circular movements are possible in multi axial and bi axial joints.
 CLASSIFICATION OF JOINTS Classification of the joints based on the number of articulating surfaces: n simple is composed of only two articulating surfaces; n compound contains more than two articulating surfaces; n complex joint if a joint contains articular discs or menisci, which divide it into two parts; n combined joints two isolated joints, in which movements occur simultaneously.
CLASSIFICATION OF JOINTS Classification of the joints based on the number of articulating surfaces: n simple is composed of only two articulating surfaces; n compound contains more than two articulating surfaces; n complex joint if a joint contains articular discs or menisci, which divide it into two parts; n combined joints two isolated joints, in which movements occur simultaneously.
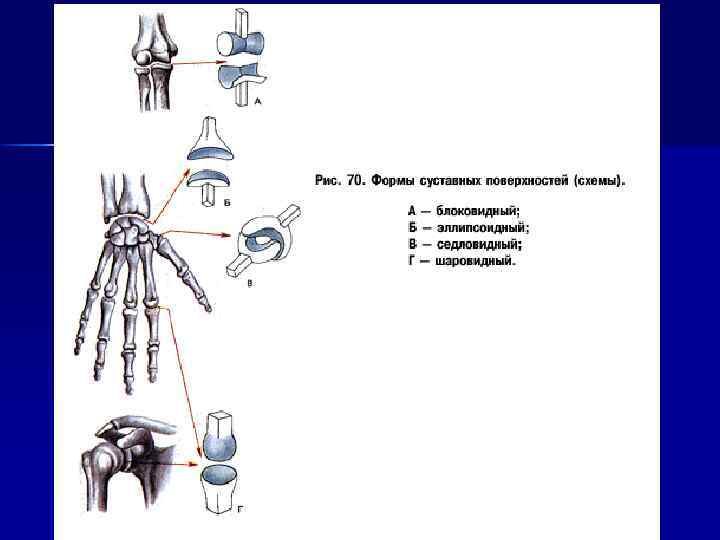
 Classification of the joints based on the shape of articulating surfaces: n n n Uni-axial joints Bi-axial joints Multi-axial joints
Classification of the joints based on the shape of articulating surfaces: n n n Uni-axial joints Bi-axial joints Multi-axial joints
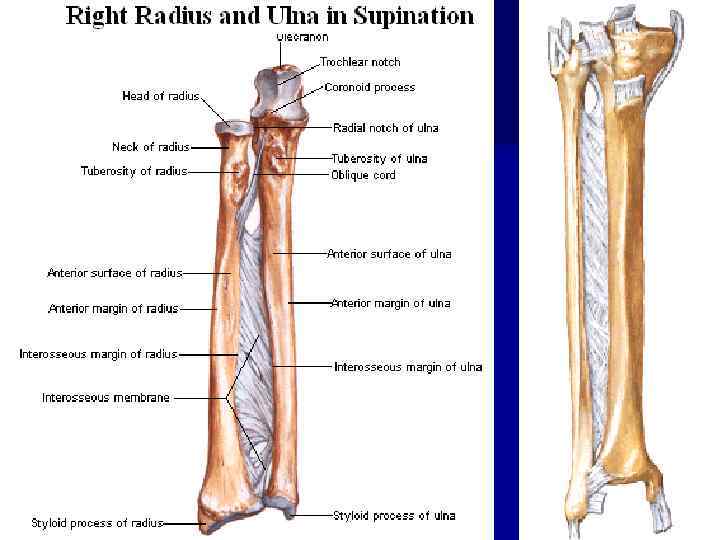
 Uni-axial joints. In these joints, movement is restricted to a single axis. There are two types of uni axial joints: n hinge joint, ginglymus, contains articulating surfaces, which resemble hinges (for example, interphalangeal joints of the hand foot); n pivot joint, art. trochoidea (art. cylindrica), a cylindrical joint, formed by the convex and concave articulating surfaces cylindrical in shape (for example, proximal and distal radio ulnar joints).
Uni-axial joints. In these joints, movement is restricted to a single axis. There are two types of uni axial joints: n hinge joint, ginglymus, contains articulating surfaces, which resemble hinges (for example, interphalangeal joints of the hand foot); n pivot joint, art. trochoidea (art. cylindrica), a cylindrical joint, formed by the convex and concave articulating surfaces cylindrical in shape (for example, proximal and distal radio ulnar joints).
 Bi-axial joints. These joints permit movements around two axes, which are perpendicular to each other. The following bi axial joints are distinguished based on their shape: n ellipsoid joint, art. ellipsoidea, contains elliptical (egg shaped) n bicondylar joint, art. bicondylaris, consists of a pair of convex, n saddle joint, art. sellaris, contains two articulating surfaces each of articulating surfaces (for example, radiocarpal joint); ellipsoid, articulating surfaces, which are rather prominent. Hence, they are known as condyles (for example, knee joint); which resembles a saddle (for example, carpometacarpal joint of the thumb).
Bi-axial joints. These joints permit movements around two axes, which are perpendicular to each other. The following bi axial joints are distinguished based on their shape: n ellipsoid joint, art. ellipsoidea, contains elliptical (egg shaped) n bicondylar joint, art. bicondylaris, consists of a pair of convex, n saddle joint, art. sellaris, contains two articulating surfaces each of articulating surfaces (for example, radiocarpal joint); ellipsoid, articulating surfaces, which are rather prominent. Hence, they are known as condyles (for example, knee joint); which resembles a saddle (for example, carpometacarpal joint of the thumb).
 Multi-axial joints include spheroidal joints and their variations. Even though, in principle, movements in these joints arc possible around multiple axes drawn through the joint, rotation occurs only around three axis: n spheroidal joint (ball-and-socket joint), art. spheroidea, consists of n plane joint, art. plana, contains two flat surfaces, which can be a globular head and a corresponding concavity. A typical example is the shoulder joint. Variation of the ball and socket joint is the cotyloid joint. Its head resides in a deep articular socket, consequently, it is known as the cup-like joint (art. cotylica); viewed as sur faces a sphere with a large diameter. Because of of the small size difference of both articulating surfaces, only slight translations are possible in plane joints (for example, sacroiliac joint).
Multi-axial joints include spheroidal joints and their variations. Even though, in principle, movements in these joints arc possible around multiple axes drawn through the joint, rotation occurs only around three axis: n spheroidal joint (ball-and-socket joint), art. spheroidea, consists of n plane joint, art. plana, contains two flat surfaces, which can be a globular head and a corresponding concavity. A typical example is the shoulder joint. Variation of the ball and socket joint is the cotyloid joint. Its head resides in a deep articular socket, consequently, it is known as the cup-like joint (art. cotylica); viewed as sur faces a sphere with a large diameter. Because of of the small size difference of both articulating surfaces, only slight translations are possible in plane joints (for example, sacroiliac joint).
 Clinical applications Pathological process can develop in the joints, among which infectious arthritis is the most common (particularly, rheumatic or tuberculous arthritis). Inflammations of the synovial membrane — synovitis and bursitis are also fairly common. Joint deformations, contraction of the synovial cleft, and restriction of movements accompanied by pain syndrome can occur as a consequence of degenerative changes (arthrosis). Traumas can cause various joint dislocations with stretched and ruptured ligaments. Physician of different specialties often have to deal with the diseases of joints.
Clinical applications Pathological process can develop in the joints, among which infectious arthritis is the most common (particularly, rheumatic or tuberculous arthritis). Inflammations of the synovial membrane — synovitis and bursitis are also fairly common. Joint deformations, contraction of the synovial cleft, and restriction of movements accompanied by pain syndrome can occur as a consequence of degenerative changes (arthrosis). Traumas can cause various joint dislocations with stretched and ruptured ligaments. Physician of different specialties often have to deal with the diseases of joints.
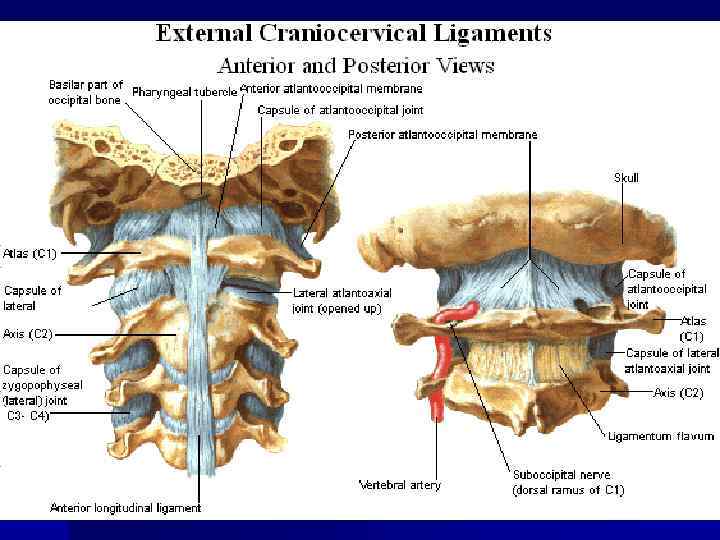
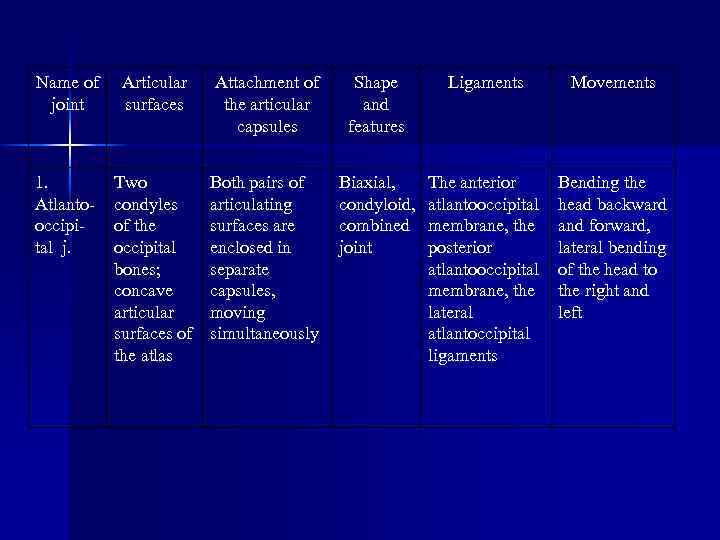 Name of joint Articular surfaces Attachment of the articular capsules Shape and features Ligaments Movements 1. Atlantooccipital j. Two condyles of the occipital bones; concave articular surfaces of the atlas Both pairs of articulating surfaces are enclosed in separate capsules, moving simultaneously Biaxial, condyloid, combined joint The anterior atlantooccipital membrane, the posterior atlantooccipital membrane, the lateral atlantoccipital ligaments Bending the head backward and forward, lateral bending of the head to the right and left
Name of joint Articular surfaces Attachment of the articular capsules Shape and features Ligaments Movements 1. Atlantooccipital j. Two condyles of the occipital bones; concave articular surfaces of the atlas Both pairs of articulating surfaces are enclosed in separate capsules, moving simultaneously Biaxial, condyloid, combined joint The anterior atlantooccipital membrane, the posterior atlantooccipital membrane, the lateral atlantoccipital ligaments Bending the head backward and forward, lateral bending of the head to the right and left
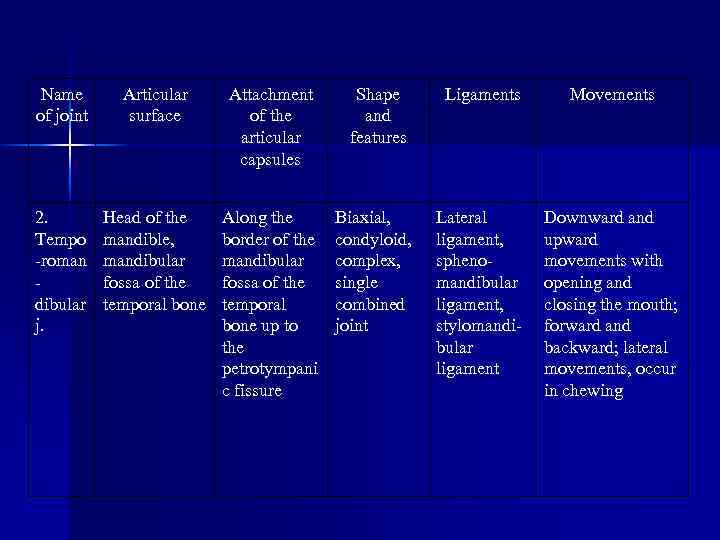 Name of joint Articular surface Attachment of the articular capsules Shape and features Ligaments Movements 2. Tempo -roman dibular j. Head of the mandible, mandibular fossa of the temporal bone Along the border of the mandibular fossa of the temporal bone up to the petrotympani c fissure Biaxial, condyloid, complex, single combined joint Lateral ligament, sphenomandibular ligament, stylomandibular ligament Downward and upward movements with opening and closing the mouth; forward and backward; lateral movements, occur in chewing
Name of joint Articular surface Attachment of the articular capsules Shape and features Ligaments Movements 2. Tempo -roman dibular j. Head of the mandible, mandibular fossa of the temporal bone Along the border of the mandibular fossa of the temporal bone up to the petrotympani c fissure Biaxial, condyloid, complex, single combined joint Lateral ligament, sphenomandibular ligament, stylomandibular ligament Downward and upward movements with opening and closing the mouth; forward and backward; lateral movements, occur in chewing
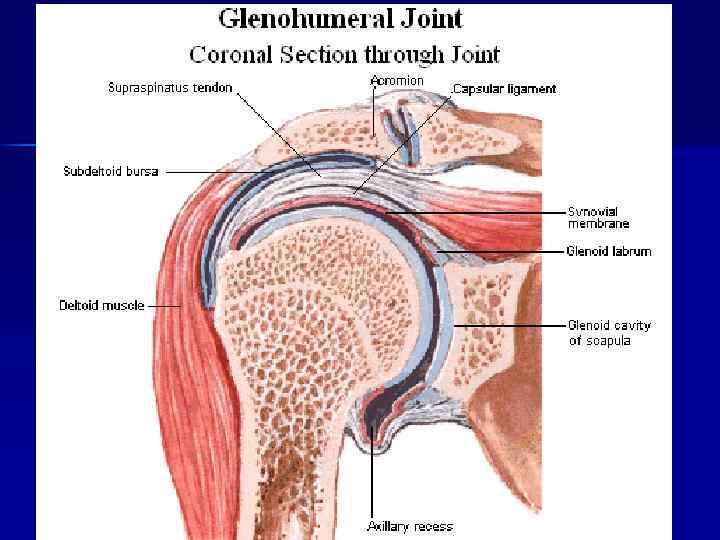
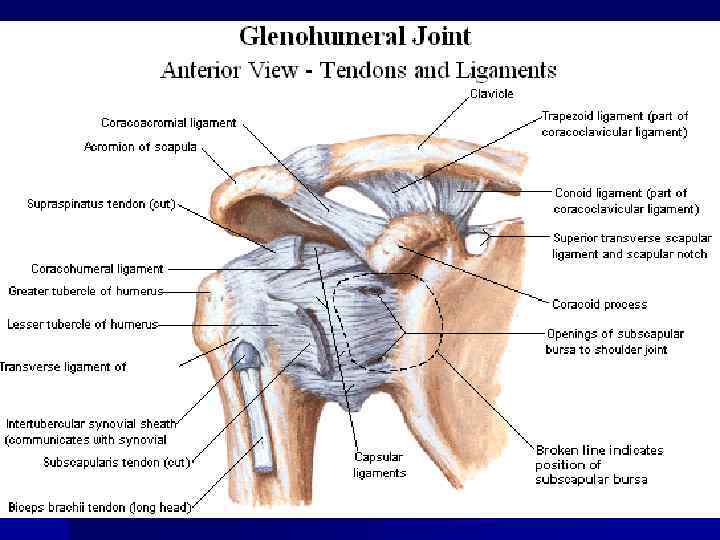
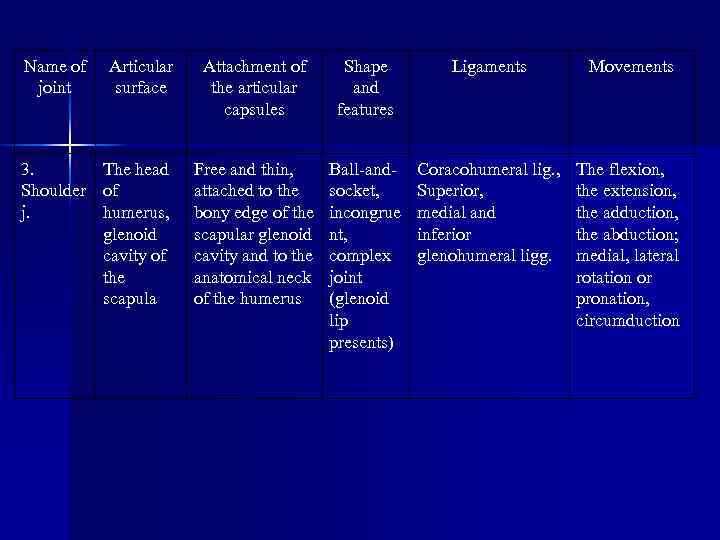 Name of joint Articular surface 3. The head Shoulder of j. humerus, glenoid cavity of the scapula Attachment of the articular capsules Shape and features Ligaments Movements Free and thin, attached to the bony edge of the scapular glenoid cavity and to the anatomical neck of the humerus Ball-andsocket, incongrue nt, complex joint (glenoid lip presents) Coracohumeral lig. , Superior, medial and inferior glenohumeral ligg. The flexion, the extension, the adduction, the abduction; medial, lateral rotation or pronation, circumduction
Name of joint Articular surface 3. The head Shoulder of j. humerus, glenoid cavity of the scapula Attachment of the articular capsules Shape and features Ligaments Movements Free and thin, attached to the bony edge of the scapular glenoid cavity and to the anatomical neck of the humerus Ball-andsocket, incongrue nt, complex joint (glenoid lip presents) Coracohumeral lig. , Superior, medial and inferior glenohumeral ligg. The flexion, the extension, the adduction, the abduction; medial, lateral rotation or pronation, circumduction
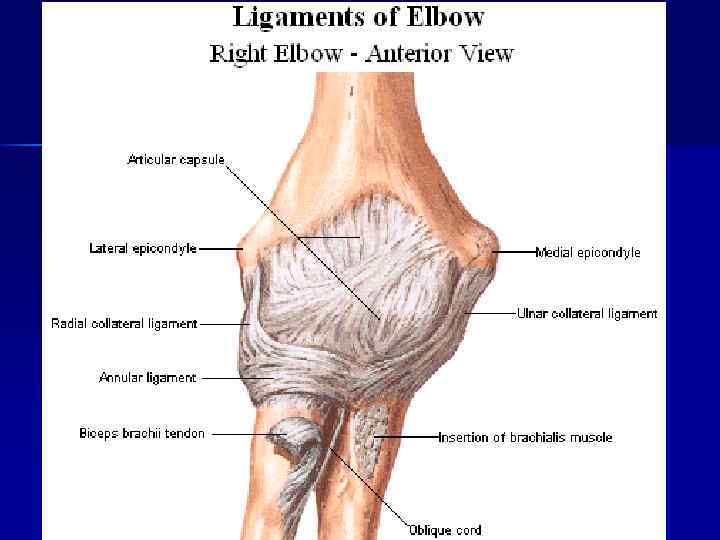
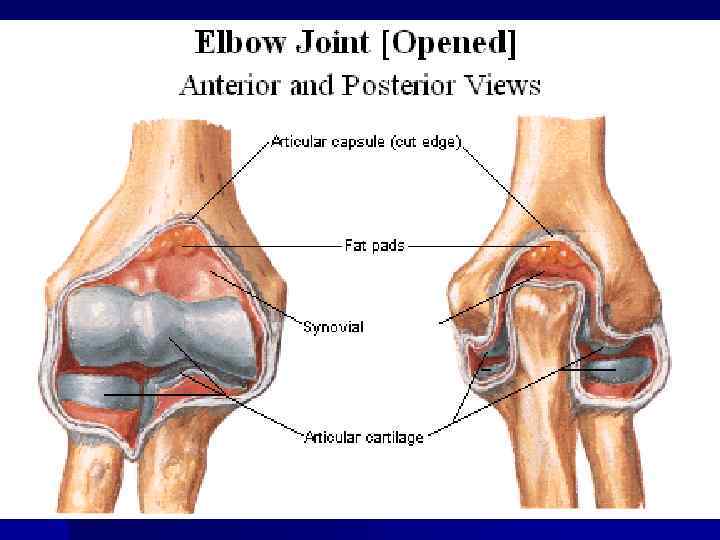
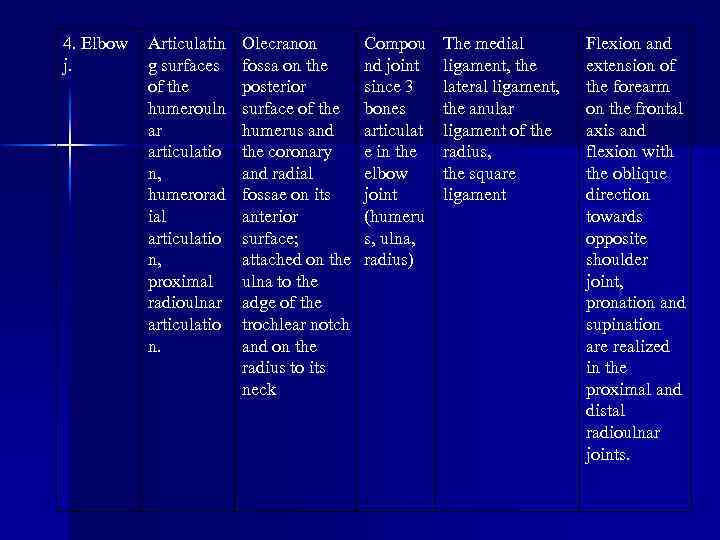 4. Elbow j. Articulatin g surfaces of the humerouln ar articulatio n, humerorad ial articulatio n, proximal radioulnar articulatio n. Olecranon fossa on the posterior surface of the humerus and the coronary and radial fossae on its anterior surface; attached on the ulna to the adge of the trochlear notch and on the radius to its neck Compou nd joint since 3 bones articulat e in the elbow joint (humeru s, ulna, radius) The medial ligament, the lateral ligament, the anular ligament of the radius, the square ligament Flexion and extension of the forearm on the frontal axis and flexion with the oblique direction towards opposite shoulder joint, pronation and supination are realized in the proximal and distal radioulnar joints.
4. Elbow j. Articulatin g surfaces of the humerouln ar articulatio n, humerorad ial articulatio n, proximal radioulnar articulatio n. Olecranon fossa on the posterior surface of the humerus and the coronary and radial fossae on its anterior surface; attached on the ulna to the adge of the trochlear notch and on the radius to its neck Compou nd joint since 3 bones articulat e in the elbow joint (humeru s, ulna, radius) The medial ligament, the lateral ligament, the anular ligament of the radius, the square ligament Flexion and extension of the forearm on the frontal axis and flexion with the oblique direction towards opposite shoulder joint, pronation and supination are realized in the proximal and distal radioulnar joints.
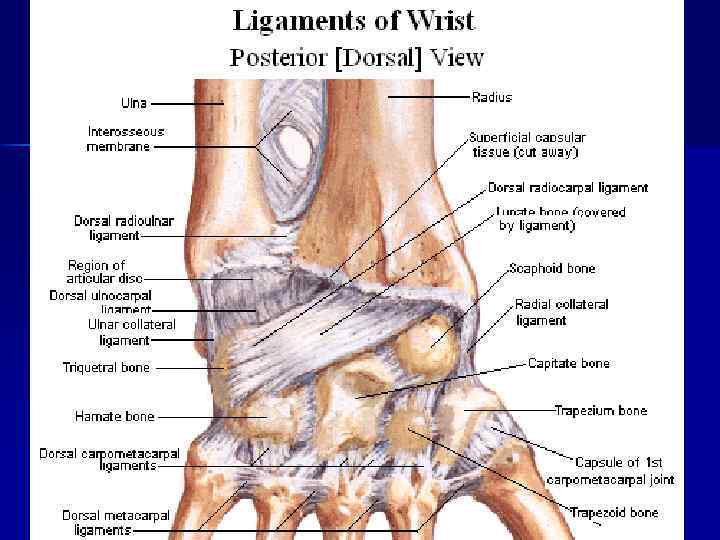
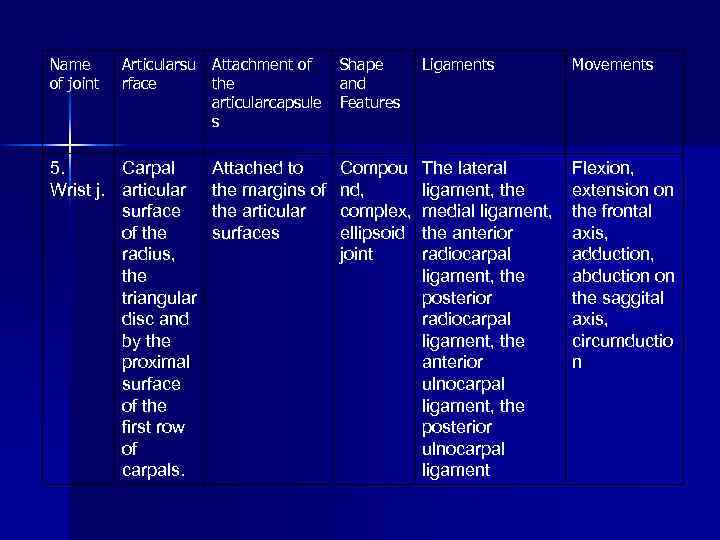 Name of joint Articularsu Attachment of rface the articularcapsule s 5. Carpal Wrist j. articular surface of the radius, the triangular disc and by the proximal surface of the first row of carpals. Attached to the margins of the articular surfaces Shape and Features Ligaments Movements Compou nd, complex, ellipsoid joint The lateral ligament, the medial ligament, the anterior radiocarpal ligament, the posterior radiocarpal ligament, the anterior ulnocarpal ligament, the posterior ulnocarpal ligament Flexion, extension on the frontal axis, adduction, abduction on the saggital axis, circumductio n
Name of joint Articularsu Attachment of rface the articularcapsule s 5. Carpal Wrist j. articular surface of the radius, the triangular disc and by the proximal surface of the first row of carpals. Attached to the margins of the articular surfaces Shape and Features Ligaments Movements Compou nd, complex, ellipsoid joint The lateral ligament, the medial ligament, the anterior radiocarpal ligament, the posterior radiocarpal ligament, the anterior ulnocarpal ligament, the posterior ulnocarpal ligament Flexion, extension on the frontal axis, adduction, abduction on the saggital axis, circumductio n
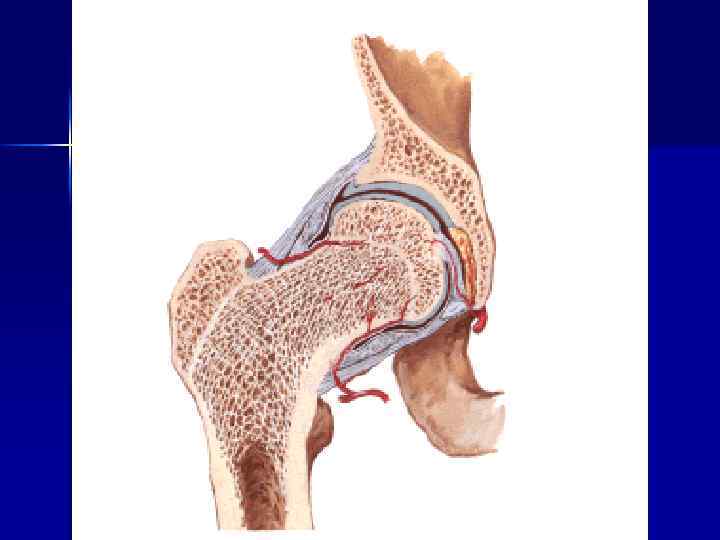
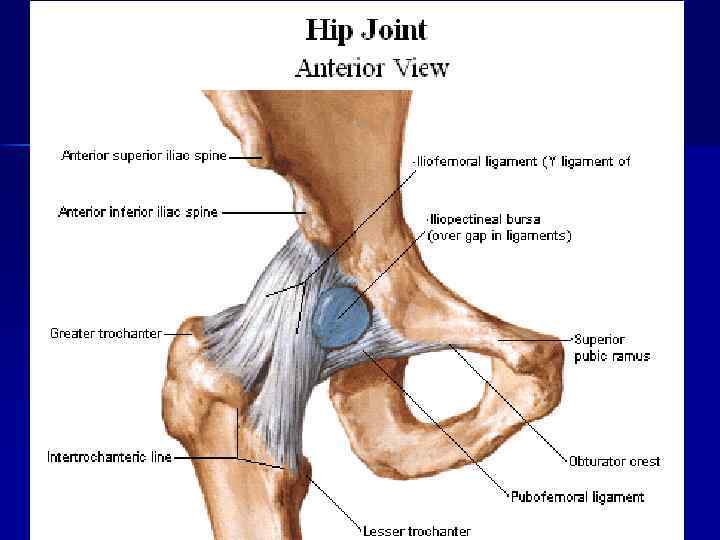
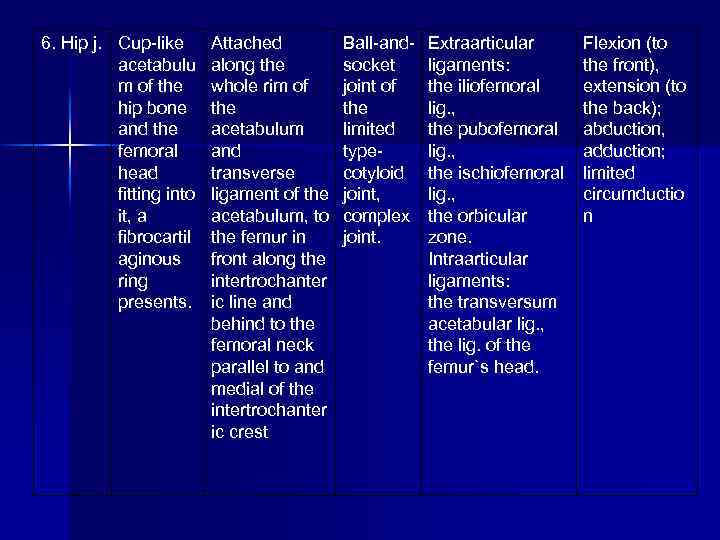 6. Hip j. Cup-like acetabulu m of the hip bone and the femoral head fitting into it, a fibrocartil aginous ring presents. Attached along the whole rim of the acetabulum and transverse ligament of the acetabulum, to the femur in front along the intertrochanter ic line and behind to the femoral neck parallel to and medial of the intertrochanter ic crest Ball-andsocket joint of the limited typecotyloid joint, complex joint. Extraarticular ligaments: the iliofemoral lig. , the pubofemoral lig. , the ischiofemoral lig. , the orbicular zone. Intraarticular ligaments: the transversum acetabular lig. , the lig. of the femur`s head. Flexion (to the front), extension (to the back); abduction, adduction; limited circumductio n
6. Hip j. Cup-like acetabulu m of the hip bone and the femoral head fitting into it, a fibrocartil aginous ring presents. Attached along the whole rim of the acetabulum and transverse ligament of the acetabulum, to the femur in front along the intertrochanter ic line and behind to the femoral neck parallel to and medial of the intertrochanter ic crest Ball-andsocket joint of the limited typecotyloid joint, complex joint. Extraarticular ligaments: the iliofemoral lig. , the pubofemoral lig. , the ischiofemoral lig. , the orbicular zone. Intraarticular ligaments: the transversum acetabular lig. , the lig. of the femur`s head. Flexion (to the front), extension (to the back); abduction, adduction; limited circumductio n
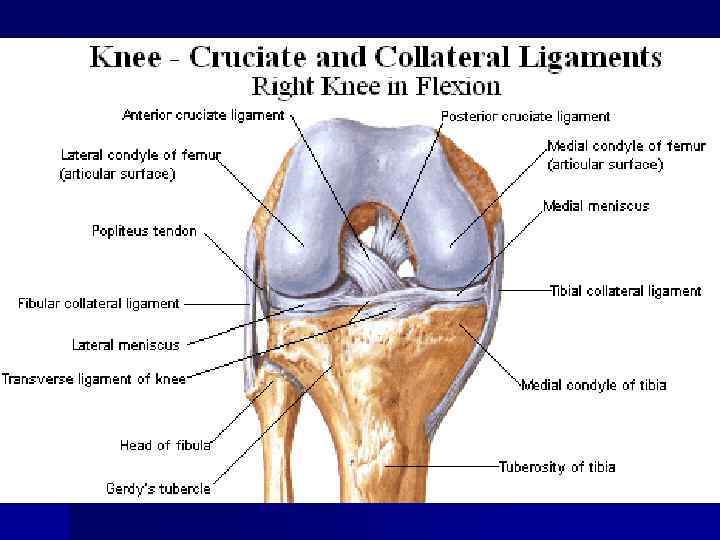
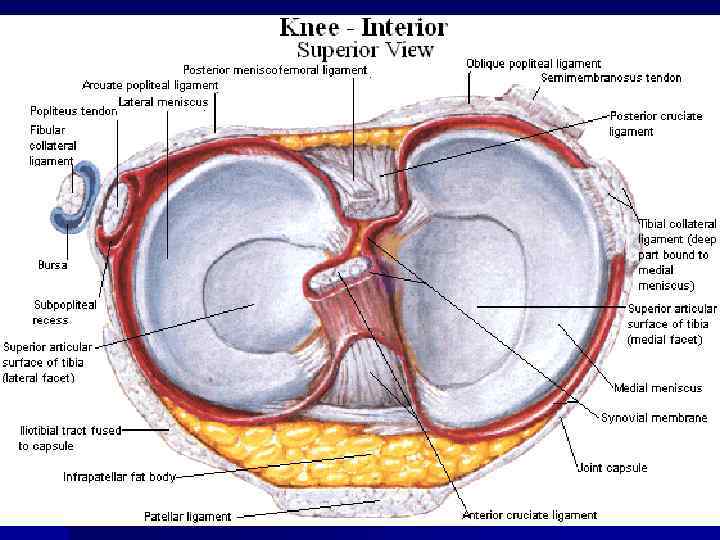
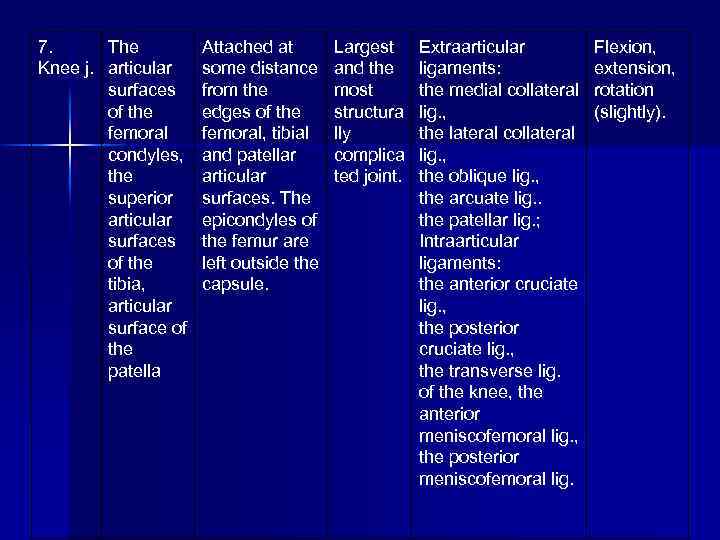 7. The Knee j. articular surfaces of the femoral condyles, the superior articular surfaces of the tibia, articular surface of the patella Attached at some distance from the edges of the femoral, tibial and patellar articular surfaces. The epicondyles of the femur are left outside the capsule. Largest and the most structura lly complica ted joint. Extraarticular ligaments: the medial collateral lig. , the lateral collateral lig. , the oblique lig. , the arcuate lig. . the patellar lig. ; Intraarticular ligaments: the anterior cruciate lig. , the posterior cruciate lig. , the transverse lig. of the knee, the anterior meniscofemoral lig. , the posterior meniscofemoral lig. Flexion, extension, rotation (slightly).
7. The Knee j. articular surfaces of the femoral condyles, the superior articular surfaces of the tibia, articular surface of the patella Attached at some distance from the edges of the femoral, tibial and patellar articular surfaces. The epicondyles of the femur are left outside the capsule. Largest and the most structura lly complica ted joint. Extraarticular ligaments: the medial collateral lig. , the lateral collateral lig. , the oblique lig. , the arcuate lig. . the patellar lig. ; Intraarticular ligaments: the anterior cruciate lig. , the posterior cruciate lig. , the transverse lig. of the knee, the anterior meniscofemoral lig. , the posterior meniscofemoral lig. Flexion, extension, rotation (slightly).
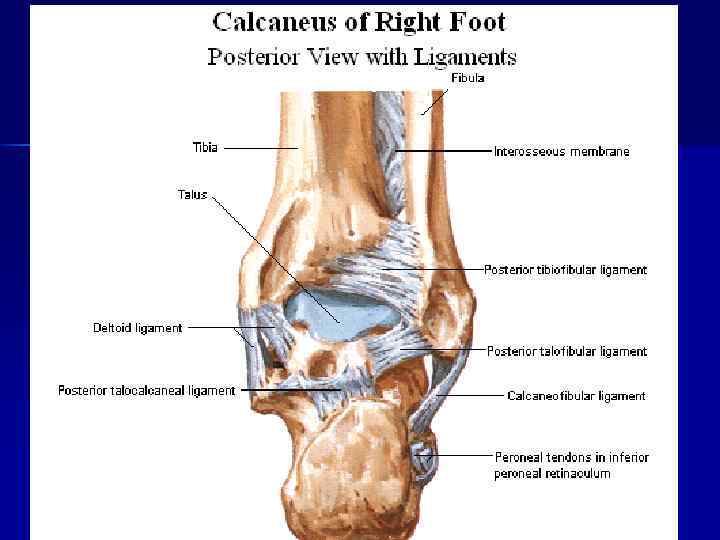
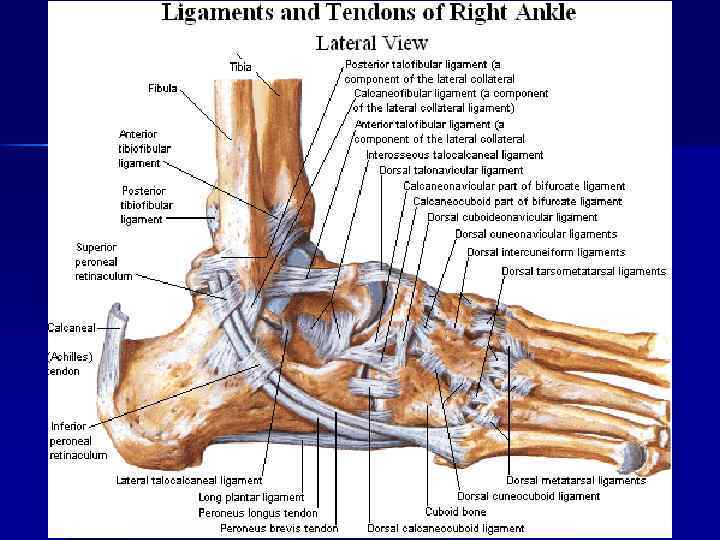
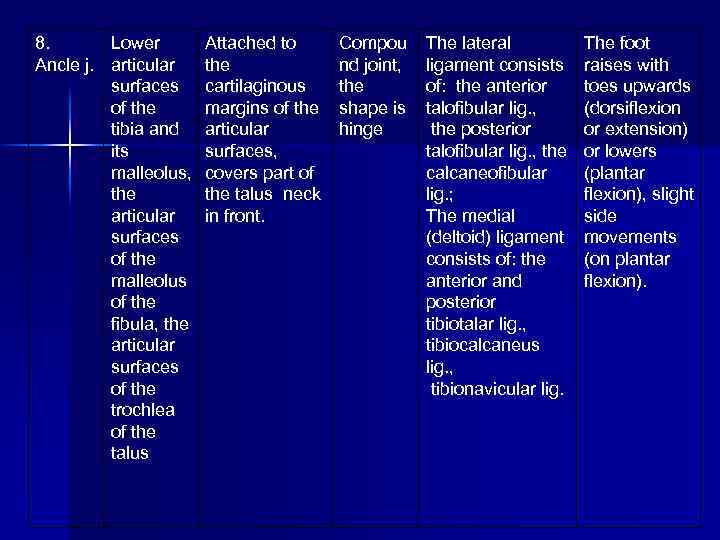 8. Lower Ancle j. articular surfaces of the tibia and its malleolus, the articular surfaces of the malleolus of the fibula, the articular surfaces of the trochlea of the talus Attached to the cartilaginous margins of the articular surfaces, covers part of the talus neck in front. Compou nd joint, the shape is hinge The lateral ligament consists of: the anterior talofibular lig. , the posterior talofibular lig. , the calcaneofibular lig. ; The medial (deltoid) ligament consists of: the anterior and posterior tibiotalar lig. , tibiocalcaneus lig. , tibionavicular lig. The foot raises with toes upwards (dorsiflexion or extension) or lowers (plantar flexion), slight side movements (on plantar flexion).
8. Lower Ancle j. articular surfaces of the tibia and its malleolus, the articular surfaces of the malleolus of the fibula, the articular surfaces of the trochlea of the talus Attached to the cartilaginous margins of the articular surfaces, covers part of the talus neck in front. Compou nd joint, the shape is hinge The lateral ligament consists of: the anterior talofibular lig. , the posterior talofibular lig. , the calcaneofibular lig. ; The medial (deltoid) ligament consists of: the anterior and posterior tibiotalar lig. , tibiocalcaneus lig. , tibionavicular lig. The foot raises with toes upwards (dorsiflexion or extension) or lowers (plantar flexion), slight side movements (on plantar flexion).
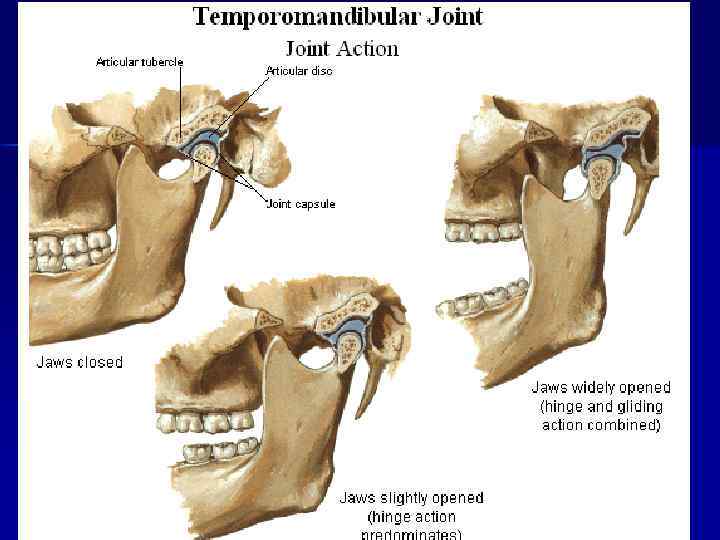
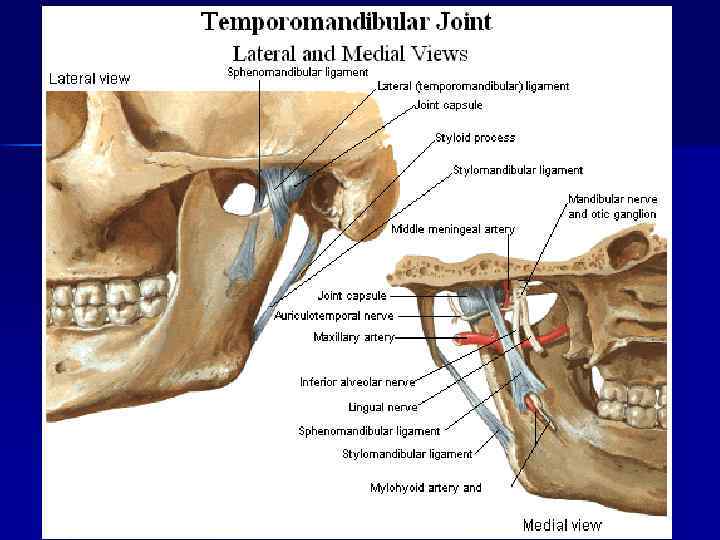
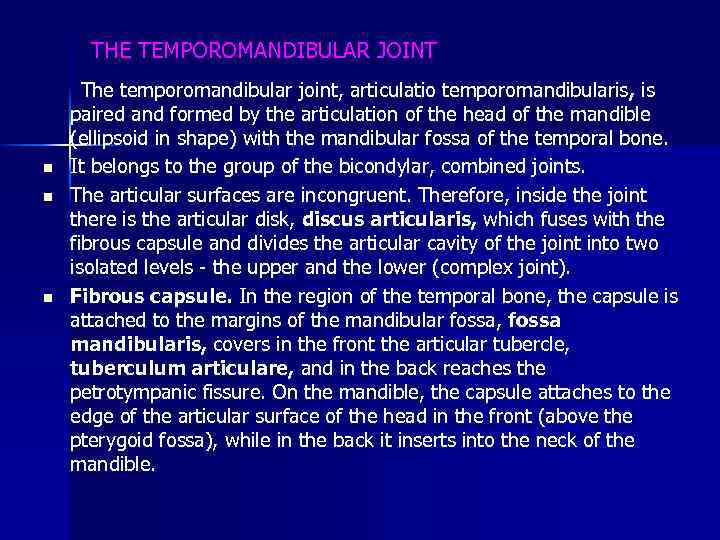 THE TEMPOROMANDIBULAR JOINT The temporomandibular joint, articulatio temporomandibularis , is paired and formed by the articulation of the head of the mandible (ellipsoid in shape) with the mandibular fossa of the temporal bone. n It belongs to the group of the bicondylar, combined joints. n The articular surfaces are incongruent. Therefore, inside the joint there is the articular disk, discus articularis, which fuses with the fibrous capsule and divides the articular cavity of the joint into two isolated levels the upper and the lower (complex joint). n Fibrous capsule. In the region of the temporal bone, the capsule is attached to the margins of the mandibular fossa, fossa mandibularis, covers in the front the articular tubercle, tuberculum articulare, and in the back reaches the petrotympanic fissure. On the mandible, the capsule attaches to the edge of the articular surface of the head in the front (above the pterygoid fossa), while in the back it inserts into the neck of the mandible.
THE TEMPOROMANDIBULAR JOINT The temporomandibular joint, articulatio temporomandibularis , is paired and formed by the articulation of the head of the mandible (ellipsoid in shape) with the mandibular fossa of the temporal bone. n It belongs to the group of the bicondylar, combined joints. n The articular surfaces are incongruent. Therefore, inside the joint there is the articular disk, discus articularis, which fuses with the fibrous capsule and divides the articular cavity of the joint into two isolated levels the upper and the lower (complex joint). n Fibrous capsule. In the region of the temporal bone, the capsule is attached to the margins of the mandibular fossa, fossa mandibularis, covers in the front the articular tubercle, tuberculum articulare, and in the back reaches the petrotympanic fissure. On the mandible, the capsule attaches to the edge of the articular surface of the head in the front (above the pterygoid fossa), while in the back it inserts into the neck of the mandible.
 n n n n Ligaments. The capsule is reinforced by the lateral ligament, lig. laterale, whose fibers run obliquely from the zygomatic process of the temporal bono to the neck of the mandible. Importantly, (ho following fasciae (ligaments) thicken in order to stabilize the mandible: 1) lig. stylomandibular, which runs from the styloid process of the temporal bone to the posterior angle of the mandible; 2) lig. sphenomandibulare, which extends from the spine of the sphenoid towards the lingula of the mandible. Movements. The temporomandibular joint permits the following movements: 1) elevation and depression of themandible occurs around the frontal axis in the lower level of the joint. When the mandible is exceedingly depressed, the articular disk with the head of the mandible may be displaced onto the articular tubercle; 2) protrusion of the mandible occurs in the upper level of the joint in such a way that the head together with the articular disk are drawn onto the articular tubercle; 3) lateral movements of the mandible occur such that on one side the head remains in the fossa, whereas on the opposite side it: is drawn onto the articular tubercle together with the articular disc.
n n n n Ligaments. The capsule is reinforced by the lateral ligament, lig. laterale, whose fibers run obliquely from the zygomatic process of the temporal bono to the neck of the mandible. Importantly, (ho following fasciae (ligaments) thicken in order to stabilize the mandible: 1) lig. stylomandibular, which runs from the styloid process of the temporal bone to the posterior angle of the mandible; 2) lig. sphenomandibulare, which extends from the spine of the sphenoid towards the lingula of the mandible. Movements. The temporomandibular joint permits the following movements: 1) elevation and depression of themandible occurs around the frontal axis in the lower level of the joint. When the mandible is exceedingly depressed, the articular disk with the head of the mandible may be displaced onto the articular tubercle; 2) protrusion of the mandible occurs in the upper level of the joint in such a way that the head together with the articular disk are drawn onto the articular tubercle; 3) lateral movements of the mandible occur such that on one side the head remains in the fossa, whereas on the opposite side it: is drawn onto the articular tubercle together with the articular disc.
 MASTICATORY MUSCLES The masticatory muscles are derived from the common mesenchymatous primordium of the first visceral (mandibular) arch, which is associated with the third branch of the trigeminal nerve. All of the masticatory muscles (four) act on the temporomandibular joint and move the mandible. They can be divided into the superficial and deep muscles. THE SUPERFICIAL MASTICATORY MUSCLES Masseter, m. masseter. Origin: zygomatic arch. Insertion: masseteric tuberosity and angle of the mandible. It consists of two parts — superficial (pars superficialis) and deep (pars profunda). Action. Elevates the mandible; the superficial part protracts the mandible. Temporalis, m. temporalis. Origin: temporal and parietal bones, temporal fascia. Insertion: coronoid process of the mandible. The muscle fills the temporal fossa. It is flat and fan shaped. The ante rior fibers of the temporalis are directed vertically, middle fibers — obliquely, and posterior fibers — almost horizontally. The fibers of the muscle converge below forming a thick tendon, which runs underneath the zygomatic arch and inserts into the coronoid process. Action. Elevates and retracts the mandible.
MASTICATORY MUSCLES The masticatory muscles are derived from the common mesenchymatous primordium of the first visceral (mandibular) arch, which is associated with the third branch of the trigeminal nerve. All of the masticatory muscles (four) act on the temporomandibular joint and move the mandible. They can be divided into the superficial and deep muscles. THE SUPERFICIAL MASTICATORY MUSCLES Masseter, m. masseter. Origin: zygomatic arch. Insertion: masseteric tuberosity and angle of the mandible. It consists of two parts — superficial (pars superficialis) and deep (pars profunda). Action. Elevates the mandible; the superficial part protracts the mandible. Temporalis, m. temporalis. Origin: temporal and parietal bones, temporal fascia. Insertion: coronoid process of the mandible. The muscle fills the temporal fossa. It is flat and fan shaped. The ante rior fibers of the temporalis are directed vertically, middle fibers — obliquely, and posterior fibers — almost horizontally. The fibers of the muscle converge below forming a thick tendon, which runs underneath the zygomatic arch and inserts into the coronoid process. Action. Elevates and retracts the mandible.
 THE DEEP MASTICATORY MUSCLES Medial pterygoid, m. pterygoideus medialis. Origin: pterygoid fossa of the pterygoid process. Insertion: pterygoid tuberosity of the mandible. Action. Elevates and pulls the mandible to the side. When the muscle contracts on both sides, it protracts the mandible. Lateral pterygoid, m. pterygoideus lateralis. Origin: arises by two heads: from the infratemporal crest of the sphenoid bone (upper head) and lateral plate of the pterygoid process (lower head). Insertion: pterygoid fossa of the neck of the mandible and capsule of the temporomandibular joint. The muscle is triangular in shape. Its fibers are directed backward and laterally. It lies deep in the infratemporal fossa covered by the zygomatic arch and the ramus of the mandible as well as by the temporal muscle. Action. In unilateral contraction, the muscle moves the mandible to the opposite side; when the lateral pterygoid muscles of the two sides act together they protrude the mandible. Nerve supply of the masticatory muscles. All masticatory muscles arc supplied by the third branch of the trigeminal nerve.
THE DEEP MASTICATORY MUSCLES Medial pterygoid, m. pterygoideus medialis. Origin: pterygoid fossa of the pterygoid process. Insertion: pterygoid tuberosity of the mandible. Action. Elevates and pulls the mandible to the side. When the muscle contracts on both sides, it protracts the mandible. Lateral pterygoid, m. pterygoideus lateralis. Origin: arises by two heads: from the infratemporal crest of the sphenoid bone (upper head) and lateral plate of the pterygoid process (lower head). Insertion: pterygoid fossa of the neck of the mandible and capsule of the temporomandibular joint. The muscle is triangular in shape. Its fibers are directed backward and laterally. It lies deep in the infratemporal fossa covered by the zygomatic arch and the ramus of the mandible as well as by the temporal muscle. Action. In unilateral contraction, the muscle moves the mandible to the opposite side; when the lateral pterygoid muscles of the two sides act together they protrude the mandible. Nerve supply of the masticatory muscles. All masticatory muscles arc supplied by the third branch of the trigeminal nerve.
 Muscles of the neck Is divided into three groups: - Superficial - medial or muscles of the hyoid bone - deep Superficial Muscles of the neck 1. The platysma is subcutaneous muscle, which attached from the 2 rib to the mandible. Action: - pulling the skin of the neck; - depress the angle of the mouth. 2. The sternocleidomastoid muscle lies under the platysma. Attached: - the hilt of sternum - the sternal and of the clavicle - the mastoid process - the superior nuchae line. Action: - hold the head in a vertical position
Muscles of the neck Is divided into three groups: - Superficial - medial or muscles of the hyoid bone - deep Superficial Muscles of the neck 1. The platysma is subcutaneous muscle, which attached from the 2 rib to the mandible. Action: - pulling the skin of the neck; - depress the angle of the mouth. 2. The sternocleidomastoid muscle lies under the platysma. Attached: - the hilt of sternum - the sternal and of the clavicle - the mastoid process - the superior nuchae line. Action: - hold the head in a vertical position
 Middle muscles of the neck Is divided into 2 groups: - above the hyoid bone and below. Muscles located above the hyoid bone 1. The mylohyoid muscle is flat, connected to the mylohyoid muscle. 2. The digastric muscle consists of two bellies. Anterior arises from the digastrics fossa, posterior – the mastoid process. 3. The stylohyoid muscle – the styloid process of temporal bone. 4. The geniohyoid muscle – lies above the mylohoid muscle on the mental spine of mandible.
Middle muscles of the neck Is divided into 2 groups: - above the hyoid bone and below. Muscles located above the hyoid bone 1. The mylohyoid muscle is flat, connected to the mylohyoid muscle. 2. The digastric muscle consists of two bellies. Anterior arises from the digastrics fossa, posterior – the mastoid process. 3. The stylohyoid muscle – the styloid process of temporal bone. 4. The geniohyoid muscle – lies above the mylohoid muscle on the mental spine of mandible.
 Muscles located below the hyoid bone 1. The sternohyoid muscle attached the hilt of the sternum, sterna and of the clavicle. Action: - pulls the hyoid bone downwards. 2. The sternothyroid muscle: - lies under the sternohyoid muscle, lowers the larynx. 3. The thyrohyoid muscle is continuated of the sternothyroid muscle, pulls the larynx upwards. 4. The omohyoid muscle – consists of two bellies, inferior and superior. Inferior arises of the subscapular notch and connected with superior belly. Action: pulls the hyoid bone downwards.
Muscles located below the hyoid bone 1. The sternohyoid muscle attached the hilt of the sternum, sterna and of the clavicle. Action: - pulls the hyoid bone downwards. 2. The sternothyroid muscle: - lies under the sternohyoid muscle, lowers the larynx. 3. The thyrohyoid muscle is continuated of the sternothyroid muscle, pulls the larynx upwards. 4. The omohyoid muscle – consists of two bellies, inferior and superior. Inferior arises of the subscapular notch and connected with superior belly. Action: pulls the hyoid bone downwards.
 The Deep muscles of the neck Is divided into three groups: - lateral, attached to the ribs - prevertebral - suboccipital The Deep lateral muscles of the neck 1. The anterior scalene muscle 2. The medius scalene muscle 3. The posterior scalene muscle They attached the transverse processes of the cervical vertebrae. Action: raises the upper ribs, inspiration muscles. The Deep prevertebral muscles of the neck 1. The long muscle of the neck 2. The long muscle of the head Action: flex the head forward and laterally The Deep suboccipital muscles of the neck 1, 2. The anterior and lateral straight muscles of the head – flex the head forward, spine – laterally. 3, 4. The obliquus capitis superior and inferior muscles 5, 6. The greater and lesser straight muscles Action: rotate the head and pull it backwards.
The Deep muscles of the neck Is divided into three groups: - lateral, attached to the ribs - prevertebral - suboccipital The Deep lateral muscles of the neck 1. The anterior scalene muscle 2. The medius scalene muscle 3. The posterior scalene muscle They attached the transverse processes of the cervical vertebrae. Action: raises the upper ribs, inspiration muscles. The Deep prevertebral muscles of the neck 1. The long muscle of the neck 2. The long muscle of the head Action: flex the head forward and laterally The Deep suboccipital muscles of the neck 1, 2. The anterior and lateral straight muscles of the head – flex the head forward, spine – laterally. 3, 4. The obliquus capitis superior and inferior muscles 5, 6. The greater and lesser straight muscles Action: rotate the head and pull it backwards.
 THE END THANK FOR YOUR ATTENTION
THE END THANK FOR YOUR ATTENTION


