505450eab73b233fb6a8186509e4fdd8.ppt
- Количество слайдов: 176
 Articles from the past year or so that may change your practice Mark Graber, MD FACEP Professor Christopher Hogrefe, MD Assistant Professor Departments of Family and Emergency Medicine University of Iowa Carver College of Medicine
Articles from the past year or so that may change your practice Mark Graber, MD FACEP Professor Christopher Hogrefe, MD Assistant Professor Departments of Family and Emergency Medicine University of Iowa Carver College of Medicine
 Sacred Cows
Sacred Cows

 Quassem et al. Appropriate Use of Screening and Diagnostic Tests to Foster High-Value, Cost-Conscious Care. Ann Intern Med. 2012; 156: 147 -149. How can we reduce health care costs by using only high value screening and diagnostic tests?
Quassem et al. Appropriate Use of Screening and Diagnostic Tests to Foster High-Value, Cost-Conscious Care. Ann Intern Med. 2012; 156: 147 -149. How can we reduce health care costs by using only high value screening and diagnostic tests?
 • Delphi technique in which “experts” come to a consensus on each item.
• Delphi technique in which “experts” come to a consensus on each item.
 BOGSAT
BOGSAT
 GOBSAT
GOBSAT
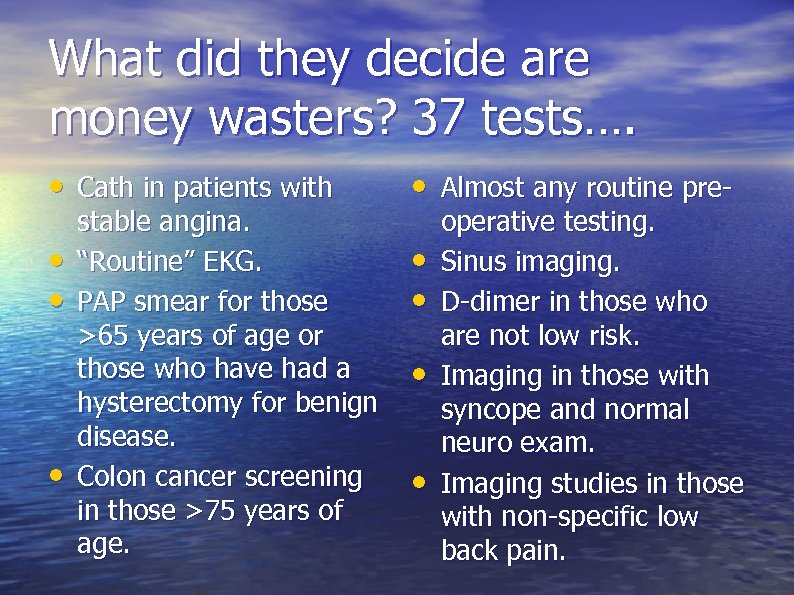 What did they decide are money wasters? 37 tests…. • Cath in patients with • Almost any routine pre- • • • stable angina. “Routine” EKG. PAP smear for those >65 years of age or those who have had a hysterectomy for benign disease. Colon cancer screening in those >75 years of age. • • operative testing. Sinus imaging. D-dimer in those who are not low risk. Imaging in those with syncope and normal neuro exam. Imaging studies in those with non-specific low back pain.
What did they decide are money wasters? 37 tests…. • Cath in patients with • Almost any routine pre- • • • stable angina. “Routine” EKG. PAP smear for those >65 years of age or those who have had a hysterectomy for benign disease. Colon cancer screening in those >75 years of age. • • operative testing. Sinus imaging. D-dimer in those who are not low risk. Imaging in those with syncope and normal neuro exam. Imaging studies in those with non-specific low back pain.
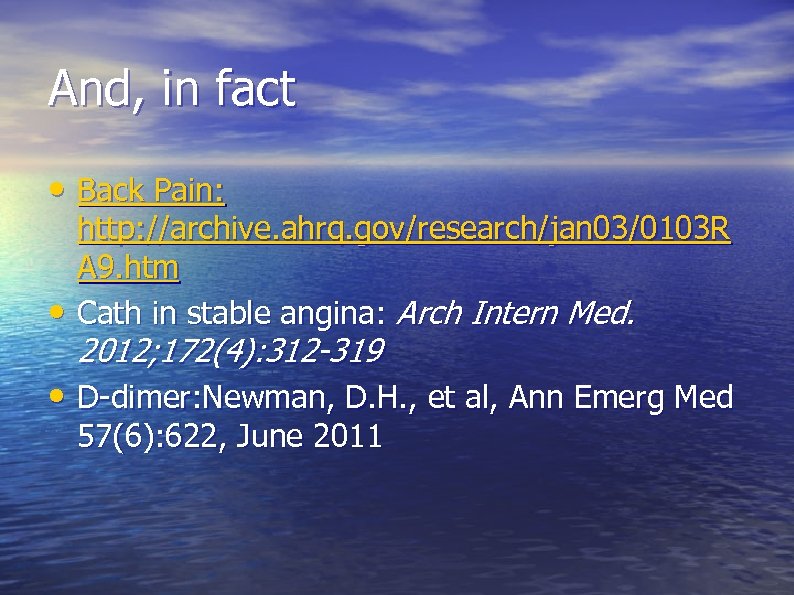 And, in fact • Back Pain: • http: //archive. ahrq. gov/research/jan 03/0103 R A 9. htm Cath in stable angina: Arch Intern Med. 2012; 172(4): 312 -319 • D-dimer: Newman, D. H. , et al, Ann Emerg Med 57(6): 622, June 2011
And, in fact • Back Pain: • http: //archive. ahrq. gov/research/jan 03/0103 R A 9. htm Cath in stable angina: Arch Intern Med. 2012; 172(4): 312 -319 • D-dimer: Newman, D. H. , et al, Ann Emerg Med 57(6): 622, June 2011
 Schjerning Olsen A-M et al. Duration of treatment with nonsteroidal anti-inflammatory drugs and impact on risk of death and recurrent myocardial infarction in patients with prior myocardial infarction: A nationwide cohort study. Circulation 2011 May 24; 123: 2226. C
Schjerning Olsen A-M et al. Duration of treatment with nonsteroidal anti-inflammatory drugs and impact on risk of death and recurrent myocardial infarction in patients with prior myocardial infarction: A nationwide cohort study. Circulation 2011 May 24; 123: 2226. C
 Even short term NSAIDS lead in increased Cardiovascular Risk • >83, 000 Danish Registry • Mean age 68, 63% men • Looked at hospitalization after FIRST MI in relationship to NSAIDS • So…these patients had known CAD • 42% received an NSAID • 42% of the whole cohort had death or recurrent MI
Even short term NSAIDS lead in increased Cardiovascular Risk • >83, 000 Danish Registry • Mean age 68, 63% men • Looked at hospitalization after FIRST MI in relationship to NSAIDS • So…these patients had known CAD • 42% received an NSAID • 42% of the whole cohort had death or recurrent MI
 • Hazard Ratio for MI in 1 st week of NSAID use: 1. 45 (45% increase) • Hazard Ratio going forward >90 days: 1. 55 (55% increase) • All NSAIDS except Naproxen (statistical fluke? ? ) Naproxen does seem to be the drug of choice, though.
• Hazard Ratio for MI in 1 st week of NSAID use: 1. 45 (45% increase) • Hazard Ratio going forward >90 days: 1. 55 (55% increase) • All NSAIDS except Naproxen (statistical fluke? ? ) Naproxen does seem to be the drug of choice, though.
 Bangalore S et al. Angiotensin receptor blockers and risk of myocardial infarction: Meta-analyses and trial sequential analyses of 147 020 patients from randomised trials. BMJ 2011 Apr 26; 342: d 2234. (http: //dx. doi. org/10. 1136/bmj. d 2234)
Bangalore S et al. Angiotensin receptor blockers and risk of myocardial infarction: Meta-analyses and trial sequential analyses of 147 020 patients from randomised trials. BMJ 2011 Apr 26; 342: d 2234. (http: //dx. doi. org/10. 1136/bmj. d 2234)

 We know not all BP lowering is equal. ALLHAT, Beta-blockers, alphablockers
We know not all BP lowering is equal. ALLHAT, Beta-blockers, alphablockers
 What we know • ARBS don’t decrease mortality in those with diabetic nephropathy. BMJ 2004 Oct 9; 329: 828 -31 • Some hint ARBS worsen cardiovascular outcomes. • „The ARBS-MI Paradox“
What we know • ARBS don’t decrease mortality in those with diabetic nephropathy. BMJ 2004 Oct 9; 329: 828 -31 • Some hint ARBS worsen cardiovascular outcomes. • „The ARBS-MI Paradox“
 This Study • Well done meta-analysis of 37 trials (with 39 arms) of ARBs vs Placebo or active drug for HTN • 147, 000 patients total. 3. 3 year follow-up • Sensitivity analysis: highest bias and lowest bias studies came to same conclusion. • Good homogeneity of studies
This Study • Well done meta-analysis of 37 trials (with 39 arms) of ARBs vs Placebo or active drug for HTN • 147, 000 patients total. 3. 3 year follow-up • Sensitivity analysis: highest bias and lowest bias studies came to same conclusion. • Good homogeneity of studies
 • What did they find? – Lower risk of stroke (RR reduction 10%) – Lower heart failure (RR reduction 13%) – Lower risk of diabetes (RR reduction 15%) • But wait for it….
• What did they find? – Lower risk of stroke (RR reduction 10%) – Lower heart failure (RR reduction 13%) – Lower risk of diabetes (RR reduction 15%) • But wait for it….
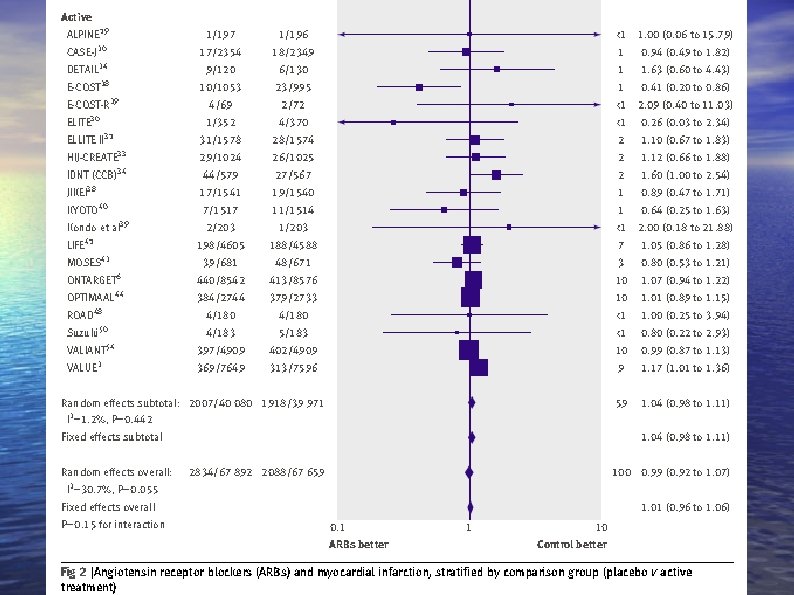
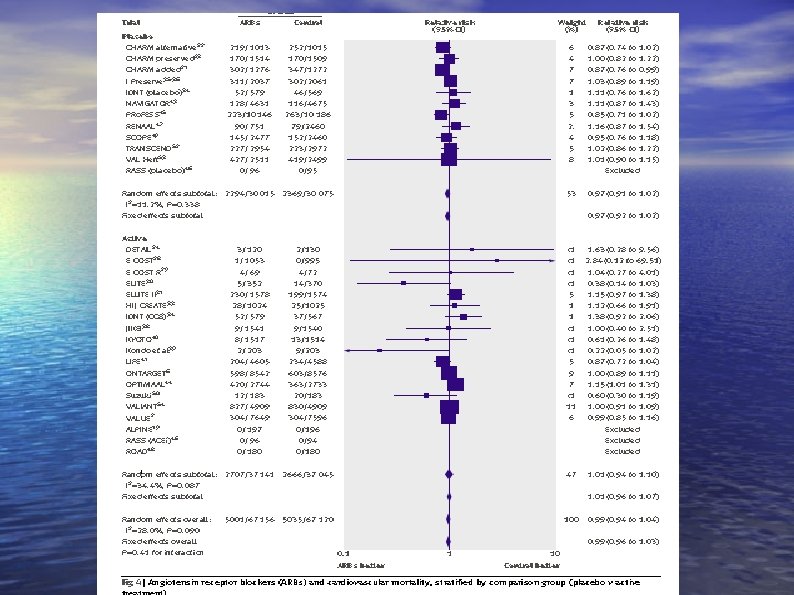
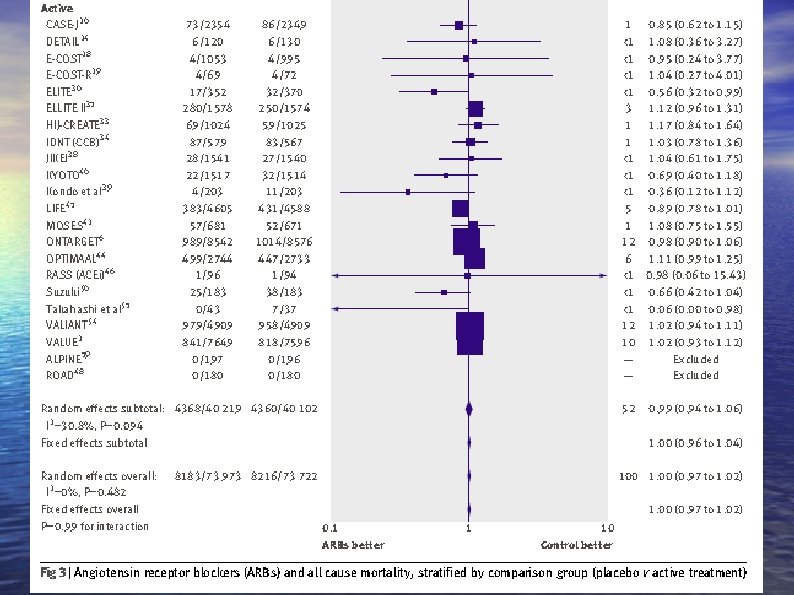
 But wait for it…. • BMJ editors say, based on the data: – “Despite lower blood pressure with angiotensin receptor blockers when compared with placebo, there also was no detectable beneficial effect for the outcome of myocardial infarction or cardiovascular mortality. ” • No benefit in overall mortality. • QED. Use something else.
But wait for it…. • BMJ editors say, based on the data: – “Despite lower blood pressure with angiotensin receptor blockers when compared with placebo, there also was no detectable beneficial effect for the outcome of myocardial infarction or cardiovascular mortality. ” • No benefit in overall mortality. • QED. Use something else.
 Well done meta-analysis • Did not get unpublished data but this would likely have supported their conclusion (un-spinable studies critical of ARBs likely would not see the light of day). • Good homogeneity
Well done meta-analysis • Did not get unpublished data but this would likely have supported their conclusion (un-spinable studies critical of ARBs likely would not see the light of day). • Good homogeneity
 Do nothing which is of no use. Miyamoto Musashi
Do nothing which is of no use. Miyamoto Musashi
 Howard R, et al. Donepezil and Memantine for Moderate-to-Severe Alzheimer's Disease. N Engl J Med 2012; 366: 893. Does memantine add anything to donepezil for moderate to severe Alzheimer’s disease?
Howard R, et al. Donepezil and Memantine for Moderate-to-Severe Alzheimer's Disease. N Engl J Med 2012; 366: 893. Does memantine add anything to donepezil for moderate to severe Alzheimer’s disease?
 Previous Literature • NNT 12 • No important positive outcomes (time to nursing home, ability to do ADLs, etc. ) • Donepezil not effective in minimal cognitive impairment • Cholinesterase inhibitors for patients with Alzheimer’s disease: • systematic review of randomized trials, BMJ 2005; 331; 321 -327 Doody RS et al. Donepezil treatment of patients with MCI: A 48 -week randomized, placebo-controlled trial. Neurology 2009 May 5; 72: 1555.
Previous Literature • NNT 12 • No important positive outcomes (time to nursing home, ability to do ADLs, etc. ) • Donepezil not effective in minimal cognitive impairment • Cholinesterase inhibitors for patients with Alzheimer’s disease: • systematic review of randomized trials, BMJ 2005; 331; 321 -327 Doody RS et al. Donepezil treatment of patients with MCI: A 48 -week randomized, placebo-controlled trial. Neurology 2009 May 5; 72: 1555.
 • 285 Patients randomized • Double-blind, randomized, 2 x 2 factorial design study of donepezil +/- memantine vs placebo for moderate-to-severe community-dwelling patients with probable Alzheimer dementia. • Outcome: Mini mental status exam: 0 -30 • Bristol ADL Scale: 0 -60
• 285 Patients randomized • Double-blind, randomized, 2 x 2 factorial design study of donepezil +/- memantine vs placebo for moderate-to-severe community-dwelling patients with probable Alzheimer dementia. • Outcome: Mini mental status exam: 0 -30 • Bristol ADL Scale: 0 -60
 Outcome • MMSE: Memantine+ donezapil vs. placebo + donezapil: 1. 2 • BALDS: Memantine + donezapil vs. placebo + donepazil: 1. 5 points • MMSE: donepazil vs. placebo: 1. 9 points • BALDS: donepazil vs placebo: 3. 0 points
Outcome • MMSE: Memantine+ donezapil vs. placebo + donezapil: 1. 2 • BALDS: Memantine + donezapil vs. placebo + donepazil: 1. 5 points • MMSE: donepazil vs. placebo: 1. 9 points • BALDS: donepazil vs placebo: 3. 0 points
 • Their conclusions: – Memantine adds nothing to donepazil- I’ll buy that – Donepazil has “significant functional benefit” over placebo- Not so fast
• Their conclusions: – Memantine adds nothing to donepazil- I’ll buy that – Donepazil has “significant functional benefit” over placebo- Not so fast
 Hmmm… • They decided arbitrarily that clinically “significant” was 1. 4 on the MMSE and 3. 5 points on BALDS based on – …. . 0. 4 SD from baseline…. – …the response seen from 127 patients. • Nowhere does this say anything about clinically detectable differences.
Hmmm… • They decided arbitrarily that clinically “significant” was 1. 4 on the MMSE and 3. 5 points on BALDS based on – …. . 0. 4 SD from baseline…. – …the response seen from 127 patients. • Nowhere does this say anything about clinically detectable differences.
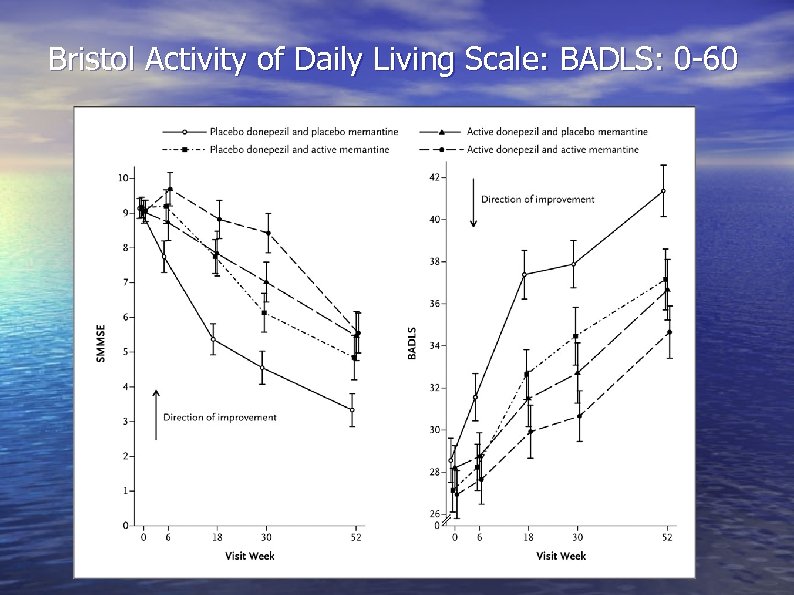 Bristol Activity of Daily Living Scale: BADLS: 0 -60
Bristol Activity of Daily Living Scale: BADLS: 0 -60
 No difference between donepazil + memantine vs. donepazil alone. • What do we take from this? – The combination of donepezil and memantine for moderate-to-severe AD is not beneficial. – The discontinuation rates of dementia medications are high. – The “clinically significant” benefit is marginal. – If you start donepezil (or another ACh. E inhibitor) for dementia, it’s reasonable to continue it through the course of the disease (or not…you could argue either point with this article).
No difference between donepazil + memantine vs. donepazil alone. • What do we take from this? – The combination of donepezil and memantine for moderate-to-severe AD is not beneficial. – The discontinuation rates of dementia medications are high. – The “clinically significant” benefit is marginal. – If you start donepezil (or another ACh. E inhibitor) for dementia, it’s reasonable to continue it through the course of the disease (or not…you could argue either point with this article).
 Zeiger RS et al. Daily or intermittent budesonide in preschool children with recurrent wheezing. N Engl J Med 2011 Nov 24; 365: 1990 c
Zeiger RS et al. Daily or intermittent budesonide in preschool children with recurrent wheezing. N Engl J Med 2011 Nov 24; 365: 1990 c
 What we know… • Oral steroids for acute exacerbations often cause behavioural problems in children. • 1 mg/kg/d is as good as 2 mg/kg/d • Chest 2002; 122; 624 -628 DOI 10. 1378/chest. 122. 2. 624 • Treating those that wheeze with URIs at the start of the URI is helpful
What we know… • Oral steroids for acute exacerbations often cause behavioural problems in children. • 1 mg/kg/d is as good as 2 mg/kg/d • Chest 2002; 122; 624 -628 DOI 10. 1378/chest. 122. 2. 624 • Treating those that wheeze with URIs at the start of the URI is helpful
 This article. . • Compared 278 children age 12 -53 months randomized to: – Low dose budesonide daily (0. 5 mg BID) – High dose budesonide 1 mg BID for 7 days at onset of wheezing or URI symptoms • These were all children who had required oral glucocorticoid therapy, ED visit (? ? ), hospitalization
This article. . • Compared 278 children age 12 -53 months randomized to: – Low dose budesonide daily (0. 5 mg BID) – High dose budesonide 1 mg BID for 7 days at onset of wheezing or URI symptoms • These were all children who had required oral glucocorticoid therapy, ED visit (? ? ), hospitalization
 Outcome • No difference in need for oral glucocorticoids • No difference in time to first exacerbation • No difference in growth, etc. • No difference in treatment failure • 104 mg less budesonide in intermittent group
Outcome • No difference in need for oral glucocorticoids • No difference in time to first exacerbation • No difference in growth, etc. • No difference in treatment failure • 104 mg less budesonide in intermittent group
 So what do I take from this? • Am I ready to stop controlled meds on my asthma patients? NO. • But for those who we only burst with steroids for a URI this is an acceptable option.
So what do I take from this? • Am I ready to stop controlled meds on my asthma patients? NO. • But for those who we only burst with steroids for a URI this is an acceptable option.
 Calcium and Bisphonates are killing me…. .
Calcium and Bisphonates are killing me…. .
 Park-Wyllie LY et al. Bisphonate use and the risk of subtrochanteric or femoral shaft fractures in older women. JAMA 2011 Feb 23; 305: 783 And Schilcher J et al. Bisphonate use and atypical fractures of the femoral shaft. N Engl J Med 2011 May 5; 364: 1728
Park-Wyllie LY et al. Bisphonate use and the risk of subtrochanteric or femoral shaft fractures in older women. JAMA 2011 Feb 23; 305: 783 And Schilcher J et al. Bisphonate use and atypical fractures of the femoral shaft. N Engl J Med 2011 May 5; 364: 1728
 What we know… • Bisphonates reduce bone remodeling
What we know… • Bisphonates reduce bone remodeling
 First study • Population based, nested, case control study • 716 women over age 68 who were taking a bisphonate and had an atypical hip fracture over 7 years. • 3580 controls on bisphonates but with no fracture
First study • Population based, nested, case control study • 716 women over age 68 who were taking a bisphonate and had an atypical hip fracture over 7 years. • 3580 controls on bisphonates but with no fracture
 • “Long term” versus transient bisphonate use associated with “atypical” hip fracture OR of 2. 74 for fracture. • 2 of 1000 women so absolute risk is low. • Still reduced “typical” hip fractures that were much more common
• “Long term” versus transient bisphonate use associated with “atypical” hip fracture OR of 2. 74 for fracture. • 2 of 1000 women so absolute risk is low. • Still reduced “typical” hip fractures that were much more common
 Next study • Sweden. Looked all hip fractures in 2008 • Total of 1271 fractures • Of these, 59 were “atypical” • Relative Risk for atypical fracture with bisphonate use was 47. 3 • But…still only 5 more per 10, 000 patientyears
Next study • Sweden. Looked all hip fractures in 2008 • Total of 1271 fractures • Of these, 59 were “atypical” • Relative Risk for atypical fracture with bisphonate use was 47. 3 • But…still only 5 more per 10, 000 patientyears
 • 78% of “atypical” fractures had used bisphonates • 10% of controls had used bisphonates • Likelihood went up with duration of bisphonate use
• 78% of “atypical” fractures had used bisphonates • 10% of controls had used bisphonates • Likelihood went up with duration of bisphonate use
 Should we have a drug holiday at 5 years? In whom should we continue the drug?
Should we have a drug holiday at 5 years? In whom should we continue the drug?
 Finally some guide: opinion only, though. N Engl J Med 2012; 366: 2048 -2051 May 31, 2012 N Engl J Med 2012; 366: 2051 -2053 May 31, 2012 • Patients with low bone-mineral density at the femoral neck (T score below -2. 5) following 3 to 5 years' of treatment have the highest risk for vertebral fracture and seem to benefit most from treatment continuation.
Finally some guide: opinion only, though. N Engl J Med 2012; 366: 2048 -2051 May 31, 2012 N Engl J Med 2012; 366: 2051 -2053 May 31, 2012 • Patients with low bone-mineral density at the femoral neck (T score below -2. 5) following 3 to 5 years' of treatment have the highest risk for vertebral fracture and seem to benefit most from treatment continuation.
 • Those with existing vertebral fractures who • have T scores below -2. 0 may also benefit. Those with femoral neck T scores above -2. 0 have low vertebral fracture risk and are not likely to benefit.
• Those with existing vertebral fractures who • have T scores below -2. 0 may also benefit. Those with femoral neck T scores above -2. 0 have low vertebral fracture risk and are not likely to benefit.
 OK. We solved that problem. What about calcium?
OK. We solved that problem. What about calcium?
 Li K, Kaaks R, et al. Associations of dietary calcium intake and calcium supplementation with myocardial infarction and stroke risk and overall cardiovascular mortality in the Heidelberg cohort of the European Prospective Investigation into Cancer and Nutrition study (EPIC-Heidelberg). Heart 2012; 98: 920 -925 So what about this calcium and heart attack thing anyway?
Li K, Kaaks R, et al. Associations of dietary calcium intake and calcium supplementation with myocardial infarction and stroke risk and overall cardiovascular mortality in the Heidelberg cohort of the European Prospective Investigation into Cancer and Nutrition study (EPIC-Heidelberg). Heart 2012; 98: 920 -925 So what about this calcium and heart attack thing anyway?
 • 25, 540 local residents, who were then aged 35 -64 years • Free of CVD at baseline – excluded participants with: MI, stroke, or transient ischaemic attack (but not angina, etc. ) • Used a validated food frequency questionnaire.
• 25, 540 local residents, who were then aged 35 -64 years • Free of CVD at baseline – excluded participants with: MI, stroke, or transient ischaemic attack (but not angina, etc. ) • Used a validated food frequency questionnaire.
 For calcium supplements… • Cardiovascular events diagnosed by: – Patient report – Family report (if dead) – Verified by death records or medical records • MI, stroke, overall CVD • Recent calcium use defined as in past 4 weeks, where ‘regularly’ was defined as daily use for at least 1 week or non-daily use of at least five doses on a regular basis.
For calcium supplements… • Cardiovascular events diagnosed by: – Patient report – Family report (if dead) – Verified by death records or medical records • MI, stroke, overall CVD • Recent calcium use defined as in past 4 weeks, where ‘regularly’ was defined as daily use for at least 1 week or non-daily use of at least five doses on a regular basis.
 • Logistic regression to adjust for confounders • Ran 4 different models. • 11 year follow-up
• Logistic regression to adjust for confounders • Ran 4 different models. • 11 year follow-up
 • 354 MI and 260 stroke cases and 267 CVD deaths. • Users of calcium supplements and MI: – HR 1. 86 (95% CI 1. 17 to 2. 96) – Calcium supplement only users HR 2. 39 (95% CI 1. 12 -to 5. 12)
• 354 MI and 260 stroke cases and 267 CVD deaths. • Users of calcium supplements and MI: – HR 1. 86 (95% CI 1. 17 to 2. 96) – Calcium supplement only users HR 2. 39 (95% CI 1. 12 -to 5. 12)
 But… • “Most recent but not the cumulative calcium only supplementation was significantly positively associated with MI risk (HR=2. 17; 95% CI 1. 06 to 4. 42). ” • They also didn’t collect data on cumulative dose (only frequency).
But… • “Most recent but not the cumulative calcium only supplementation was significantly positively associated with MI risk (HR=2. 17; 95% CI 1. 06 to 4. 42). ” • They also didn’t collect data on cumulative dose (only frequency).
 Huh? • Recent but not cumulative calcium supplement dose associated with CAD (? ? !) – This would seem to undermine the proposed mechanism of increased plaque formation • No change in stroke risk or overall CVD • • mortality Of course, reported as 86% increase in MI Absolute risk very low. – Out of 25, 000+ participants: 354 MI and 260 stroke cases and 267 CVD deaths.
Huh? • Recent but not cumulative calcium supplement dose associated with CAD (? ? !) – This would seem to undermine the proposed mechanism of increased plaque formation • No change in stroke risk or overall CVD • • mortality Of course, reported as 86% increase in MI Absolute risk very low. – Out of 25, 000+ participants: 354 MI and 260 stroke cases and 267 CVD deaths.
 Warensjo E et al. Dietary calcium intake and risk of fracture and osteoporosis prospective longitudinal cohort study BMJ 2011; 342: d 1473 doi: 10. 1136/bmj. d 1473 (Published 24 May 2011)
Warensjo E et al. Dietary calcium intake and risk of fracture and osteoporosis prospective longitudinal cohort study BMJ 2011; 342: d 1473 doi: 10. 1136/bmj. d 1473 (Published 24 May 2011)
 Second study • • • Cohort study of 61, 433 women born 1914 -1948. Study started 1987 and was of fracture risk. Based on the Swedish Mammography Cohort 5022 in the sub-cohort that looked at Dexa scans. Followed for 19 years. Calcium intake as reported by patients.
Second study • • • Cohort study of 61, 433 women born 1914 -1948. Study started 1987 and was of fracture risk. Based on the Swedish Mammography Cohort 5022 in the sub-cohort that looked at Dexa scans. Followed for 19 years. Calcium intake as reported by patients.
 • Calcium intake of 750 mg-882 mg/day (second quintile) was as good at preventing fractures and osteoporosis as were higher levels of calcium intake. • In fact, highest quintile had Hazard ratio = 1. 19 (95%CI 1. 06 -1. 32) for hip Fx.
• Calcium intake of 750 mg-882 mg/day (second quintile) was as good at preventing fractures and osteoporosis as were higher levels of calcium intake. • In fact, highest quintile had Hazard ratio = 1. 19 (95%CI 1. 06 -1. 32) for hip Fx.
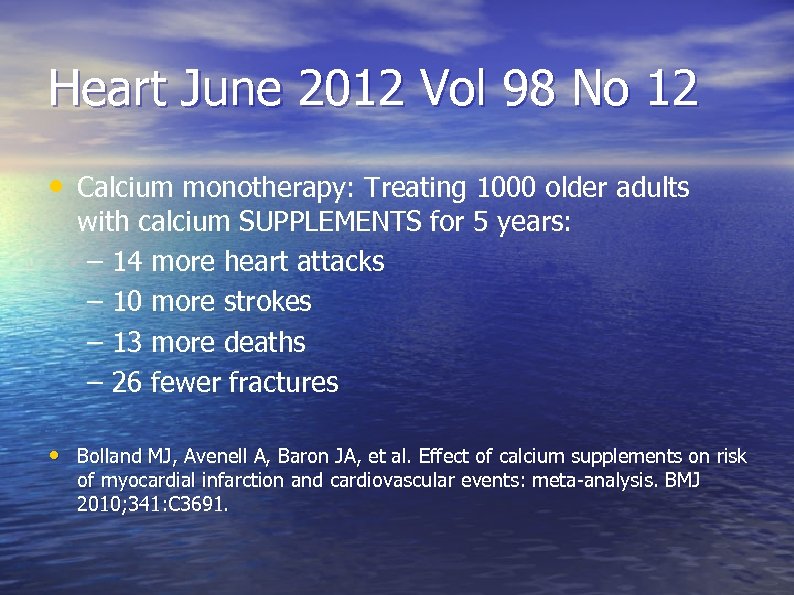 Heart June 2012 Vol 98 No 12 • Calcium monotherapy: Treating 1000 older adults with calcium SUPPLEMENTS for 5 years: – 14 more heart attacks – 10 more strokes – 13 more deaths – 26 fewer fractures • Bolland MJ, Avenell A, Baron JA, et al. Effect of calcium supplements on risk of myocardial infarction and cardiovascular events: meta-analysis. BMJ 2010; 341: C 3691.
Heart June 2012 Vol 98 No 12 • Calcium monotherapy: Treating 1000 older adults with calcium SUPPLEMENTS for 5 years: – 14 more heart attacks – 10 more strokes – 13 more deaths – 26 fewer fractures • Bolland MJ, Avenell A, Baron JA, et al. Effect of calcium supplements on risk of myocardial infarction and cardiovascular events: meta-analysis. BMJ 2010; 341: C 3691.
 Luckily, AHRQ and USPSTF to the rescue….
Luckily, AHRQ and USPSTF to the rescue….
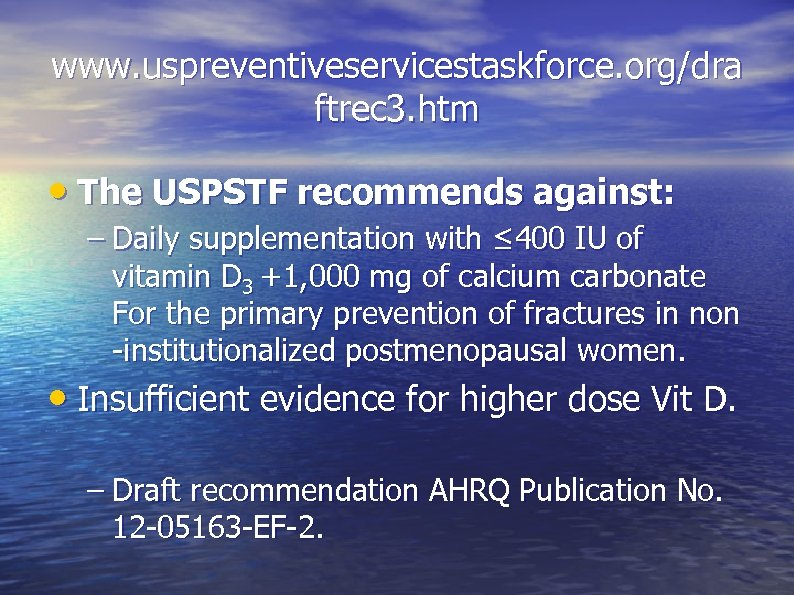 www. uspreventiveservicestaskforce. org/dra ftrec 3. htm • The USPSTF recommends against: – Daily supplementation with ≤ 400 IU of vitamin D 3 +1, 000 mg of calcium carbonate For the primary prevention of fractures in non -institutionalized postmenopausal women. • Insufficient evidence for higher dose Vit D. – Draft recommendation AHRQ Publication No. 12 -05163 -EF-2.
www. uspreventiveservicestaskforce. org/dra ftrec 3. htm • The USPSTF recommends against: – Daily supplementation with ≤ 400 IU of vitamin D 3 +1, 000 mg of calcium carbonate For the primary prevention of fractures in non -institutionalized postmenopausal women. • Insufficient evidence for higher dose Vit D. – Draft recommendation AHRQ Publication No. 12 -05163 -EF-2.
 Search for the holy grail of treating back pain.
Search for the holy grail of treating back pain.
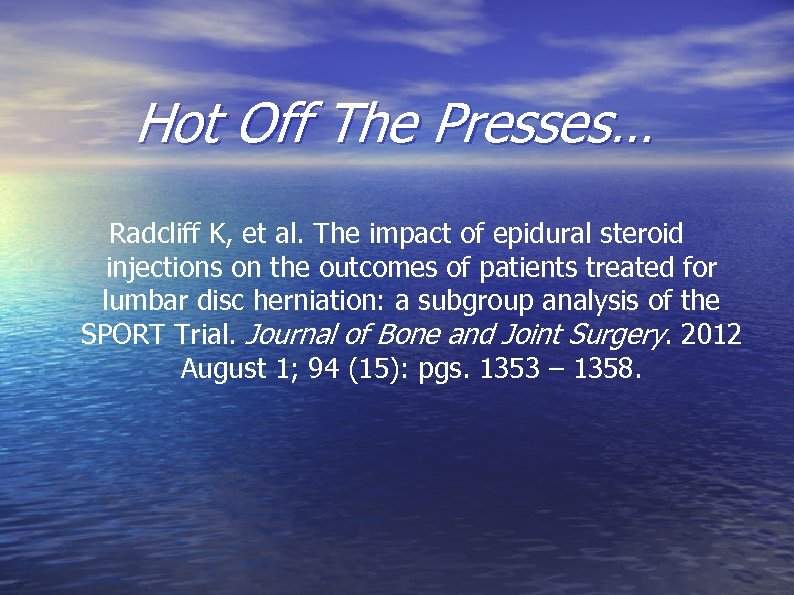 Hot Off The Presses… Radcliff K, et al. The impact of epidural steroid injections on the outcomes of patients treated for lumbar disc herniation: a subgroup analysis of the SPORT Trial. Journal of Bone and Joint Surgery. 2012 August 1; 94 (15): pgs. 1353 – 1358.
Hot Off The Presses… Radcliff K, et al. The impact of epidural steroid injections on the outcomes of patients treated for lumbar disc herniation: a subgroup analysis of the SPORT Trial. Journal of Bone and Joint Surgery. 2012 August 1; 94 (15): pgs. 1353 – 1358.
 The Nitty Gritty • A subgroup analysis of a prospective, multicenter study of operative versus nonoperative treatment of lumbar interverterbral disc herniation. • 154 patients who received epidural steroid injections during the SPORT trial (with no previous injections) vs. 453 patients who never received an injection (before or during the SPORT trial).
The Nitty Gritty • A subgroup analysis of a prospective, multicenter study of operative versus nonoperative treatment of lumbar interverterbral disc herniation. • 154 patients who received epidural steroid injections during the SPORT trial (with no previous injections) vs. 453 patients who never received an injection (before or during the SPORT trial).
 Gauging Success (or Failure) • Compared both primary and secondary outcomes at four years and the rates of surgical/non-surgical treatments. • Primary outcomes = bodily pain, physical function, and physical/mental component summary. • Secondary outcomes = self-reported improvement, work status, and satisfaction.
Gauging Success (or Failure) • Compared both primary and secondary outcomes at four years and the rates of surgical/non-surgical treatments. • Primary outcomes = bodily pain, physical function, and physical/mental component summary. • Secondary outcomes = self-reported improvement, work status, and satisfaction.
 The Bottom Line • Patients with lumbar disc herniation treated with epidural steroid injections had no improvement in short and/or long-term outcomes. • However, there was an increased prevalence of crossover to non-surgical treatment. • Confounded by a preference for surgical avoidance.
The Bottom Line • Patients with lumbar disc herniation treated with epidural steroid injections had no improvement in short and/or long-term outcomes. • However, there was an increased prevalence of crossover to non-surgical treatment. • Confounded by a preference for surgical avoidance.
 Other references of randomized studies that come to the same conclusion • Cohen SP et al. Epidural steroids, etanercept, or • saline in subacute sciatica: A multicenter, randomized trial. Ann Intern Med 2012 Apr 17; 156: 551. (http: //www. annals. org/content/156/8/551. full) Cohen SP. Epidural steroid injections for low back pain. BMJ 2011 Sep 13; 343: d 5310. (http: //dx. doi. org/10. 1136/bmj. d 5310)
Other references of randomized studies that come to the same conclusion • Cohen SP et al. Epidural steroids, etanercept, or • saline in subacute sciatica: A multicenter, randomized trial. Ann Intern Med 2012 Apr 17; 156: 551. (http: //www. annals. org/content/156/8/551. full) Cohen SP. Epidural steroid injections for low back pain. BMJ 2011 Sep 13; 343: d 5310. (http: //dx. doi. org/10. 1136/bmj. d 5310)
 And Thus… What is a provider to do?
And Thus… What is a provider to do?
 Stergiopoulos K and Brown DL. , Initial Coronary Stent Implantation With Medical Therapy vs Medical Therapy Alone for Stable Coronary Artery Disease Arch Intern Med 2012 Feb 27; 172: 312.
Stergiopoulos K and Brown DL. , Initial Coronary Stent Implantation With Medical Therapy vs Medical Therapy Alone for Stable Coronary Artery Disease Arch Intern Med 2012 Feb 27; 172: 312.
 Sisyphus trying to get physicians to act rationally
Sisyphus trying to get physicians to act rationally
 What we know • COURAGE trial supported by AHRQ showed no benefit to stenting versus optimal medical management. N Engl J Med 2007; 356: 1503 -1516 April 12, 2007 • We also know that this hasn’t changed practices. Borden WB et al. JAMA 2011 May 11; 305: 1882.
What we know • COURAGE trial supported by AHRQ showed no benefit to stenting versus optimal medical management. N Engl J Med 2007; 356: 1503 -1516 April 12, 2007 • We also know that this hasn’t changed practices. Borden WB et al. JAMA 2011 May 11; 305: 1882.
 Why another meta-analysis • Prior meta-analyses included patients who had simple balloon angioplasty and who did not have the current standard of care for optimum medical therapy.
Why another meta-analysis • Prior meta-analyses included patients who had simple balloon angioplasty and who did not have the current standard of care for optimum medical therapy.
 This study • 8 trials with 7229 patients using patient level data • 3 studies stable patients after MI • 5 studies stable angina with some sort of provocative test • Follow-up was 4. 3 years
This study • 8 trials with 7229 patients using patient level data • 3 studies stable patients after MI • 5 studies stable angina with some sort of provocative test • Follow-up was 4. 3 years
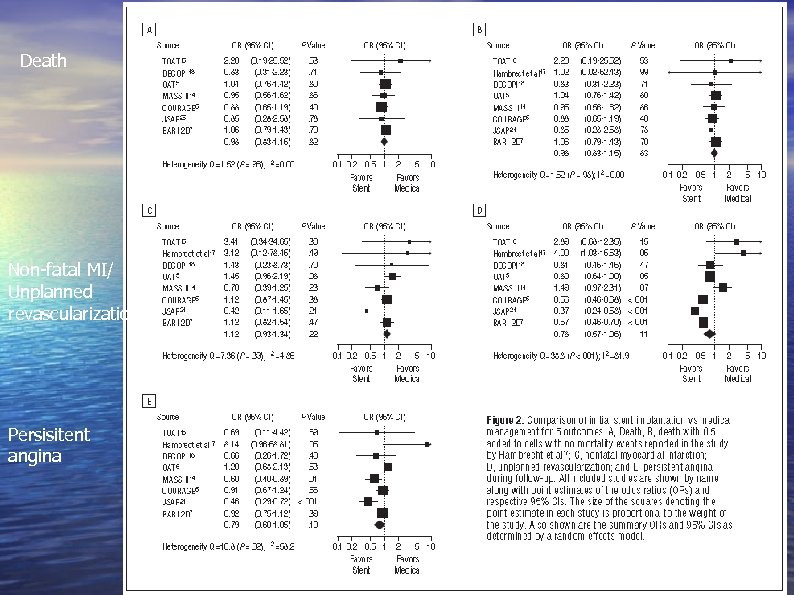 Death Non-fatal MI/ Unplanned revascularization Persisitent angina
Death Non-fatal MI/ Unplanned revascularization Persisitent angina
 Results in numbers: • Death (all cause): 8. 9% vs. 9. 1% (OR 0. 98 95% CI • • • 0. 84 -1. 16) Non-fatal MI: 8. 9% vs. 8. 1% (OR 1. 12 95% CI. 931. 34) Unplanned revasc: 21. 4% and 30. 7% (OR, 0. 78; 95% CI, 0. 57 -1. 06 favoring stent Persistent angina, 29% and 33% (OR, 0. 80; 95% CI, 0. 60 -1. 05).
Results in numbers: • Death (all cause): 8. 9% vs. 9. 1% (OR 0. 98 95% CI • • • 0. 84 -1. 16) Non-fatal MI: 8. 9% vs. 8. 1% (OR 1. 12 95% CI. 931. 34) Unplanned revasc: 21. 4% and 30. 7% (OR, 0. 78; 95% CI, 0. 57 -1. 06 favoring stent Persistent angina, 29% and 33% (OR, 0. 80; 95% CI, 0. 60 -1. 05).
 Editorial: ARCH INTERN MED/VOL 172 (NO. 4), 320 FEB 27, 2012 • Reducing even 1/3 of the caths would save $6 billion to $8 billion annually • “While physicians outwardly worship at the altar of evidence-based medicine, in reality, we more often tend to practice selective evidence-based medicine by adopting and embracing those trials and studies with results that reinforce our existing clinical practice preferences or biases…. . ”
Editorial: ARCH INTERN MED/VOL 172 (NO. 4), 320 FEB 27, 2012 • Reducing even 1/3 of the caths would save $6 billion to $8 billion annually • “While physicians outwardly worship at the altar of evidence-based medicine, in reality, we more often tend to practice selective evidence-based medicine by adopting and embracing those trials and studies with results that reinforce our existing clinical practice preferences or biases…. . ”
 Diabetes
Diabetes
 More confusion…
More confusion…
 Farmer AJ et al. Meta-analysis of individual patient data in randomised trials of self monitoring of blood glucose in people with non-insulin treated type 2 diabetes. BMJ 2012 Feb 27; 344: e 486. The issue: does home glucose monitoring help to improve overall glucose control?
Farmer AJ et al. Meta-analysis of individual patient data in randomised trials of self monitoring of blood glucose in people with non-insulin treated type 2 diabetes. BMJ 2012 Feb 27; 344: e 486. The issue: does home glucose monitoring help to improve overall glucose control?
 • The study: 6 randomized trials with > • 2, 500 participants. A ”useful” intervention should decrease Hb. A 1 c by at least 0. 5%
• The study: 6 randomized trials with > • 2, 500 participants. A ”useful” intervention should decrease Hb. A 1 c by at least 0. 5%
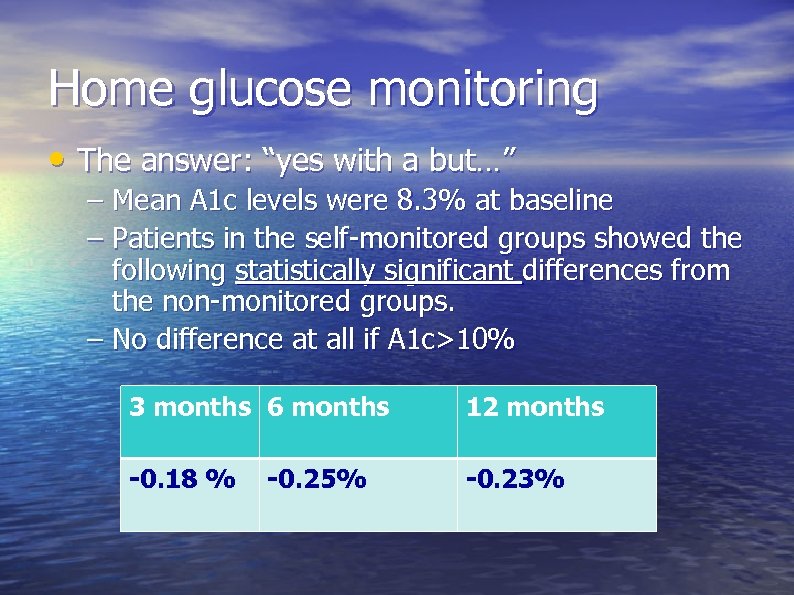 Home glucose monitoring • The answer: “yes with a but…” – Mean A 1 c levels were 8. 3% at baseline – Patients in the self-monitored groups showed the following statistically significant differences from the non-monitored groups. – No difference at all if A 1 c>10% 3 months 6 months 12 months -0. 18 % -0. 23% -0. 25%
Home glucose monitoring • The answer: “yes with a but…” – Mean A 1 c levels were 8. 3% at baseline – Patients in the self-monitored groups showed the following statistically significant differences from the non-monitored groups. – No difference at all if A 1 c>10% 3 months 6 months 12 months -0. 18 % -0. 23% -0. 25%
 Home glucose monitoring • What do we take from this? – Home glucose monitoring does little to improve overall glucose control in those not taking insulin. – Home glucose monitoring is necessary for patients on insulin or who have hypoglycemic episodes (or at least we don’t have data to say otherwise…. )
Home glucose monitoring • What do we take from this? – Home glucose monitoring does little to improve overall glucose control in those not taking insulin. – Home glucose monitoring is necessary for patients on insulin or who have hypoglycemic episodes (or at least we don’t have data to say otherwise…. )
 What else do we already know… • Tight blood pressure control does not make any difference in those with preexisitng disease. • • • The ACCORD Study Group. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med 2010 Mar 14; [e-pub ahead of print]. (http: //dx. doi. org/10. 1056/NEJMoa 1001286) • JAMA. 2010; 304(1): 61 -68. doi: 10. 1001/jama. 2010. 884
What else do we already know… • Tight blood pressure control does not make any difference in those with preexisitng disease. • • • The ACCORD Study Group. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med 2010 Mar 14; [e-pub ahead of print]. (http: //dx. doi. org/10. 1056/NEJMoa 1001286) • JAMA. 2010; 304(1): 61 -68. doi: 10. 1001/jama. 2010. 884
 How about tight glucose control? ACCORD study group. Long-Term Effects of Intensive Glucose Lowering on Cardiovascular Outcomes. N Engl J Med 2011; 364: 818 -28.
How about tight glucose control? ACCORD study group. Long-Term Effects of Intensive Glucose Lowering on Cardiovascular Outcomes. N Engl J Med 2011; 364: 818 -28.
 • 77 clinical sites • Age 40 -79, DM type II, A 1 c 7. 5% or > • Randomly assigned to intensive control – Hb. A 1 c goal 6% – Hb. A 1 c goal 7%-7. 9% • Approx 5000 in each group
• 77 clinical sites • Age 40 -79, DM type II, A 1 c 7. 5% or > • Randomly assigned to intensive control – Hb. A 1 c goal 6% – Hb. A 1 c goal 7%-7. 9% • Approx 5000 in each group
 • Terminated intensive control arm early (3. 7 years) – Maybe longer follow-up would change outcome adverse events may cluster as years progress? ? • Non-fatal MI lower in intensive group (1. 08% vs. • 1. 35%, HR 0. 79 (95% CI 0. 66 -0. 95) at time of transition Fatal Cardiovascular disease higher (not statistically significant early on but…. ) – By end of study was statistically significant
• Terminated intensive control arm early (3. 7 years) – Maybe longer follow-up would change outcome adverse events may cluster as years progress? ? • Non-fatal MI lower in intensive group (1. 08% vs. • 1. 35%, HR 0. 79 (95% CI 0. 66 -0. 95) at time of transition Fatal Cardiovascular disease higher (not statistically significant early on but…. ) – By end of study was statistically significant
 • 21% higher all-cause mortality HR 1. 42 vs. 1. 16 (95% CI 1. 02 -1. 44) • Not the cleanest study: included interventions for BP, • • triglycerides, lipids. No interaction between these and primary outcome except… Intensive glucose control + intensive BP control = worse outcomes.
• 21% higher all-cause mortality HR 1. 42 vs. 1. 16 (95% CI 1. 02 -1. 44) • Not the cleanest study: included interventions for BP, • • triglycerides, lipids. No interaction between these and primary outcome except… Intensive glucose control + intensive BP control = worse outcomes.
 This shouldn’t be surprising. Large British study of tight control showed only difference was in retinopathy and then only with metformin.
This shouldn’t be surprising. Large British study of tight control showed only difference was in retinopathy and then only with metformin.
 Tight control may not change renal outcomes. Arch Intern Med. 2012; 172(10): 761 -769. doi: 10. 1001/archinternmed. 2011. 2230
Tight control may not change renal outcomes. Arch Intern Med. 2012; 172(10): 761 -769. doi: 10. 1001/archinternmed. 2011. 2230
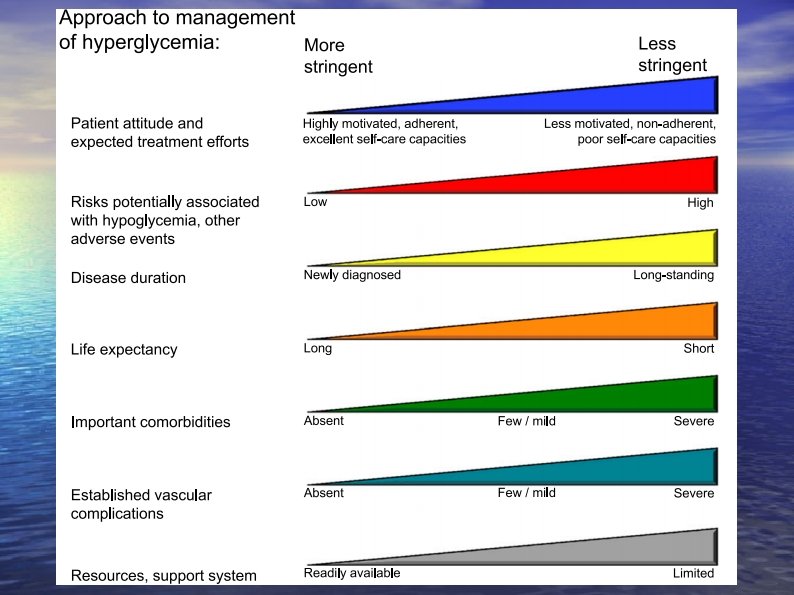
 Amazingly, the ADA agrees. Position Statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD)Published online before print April 19, 2012, doi: 10. 2337/dc 12 -0413 Diabetes Care April 19, 2012 http: //care. diabetesjournals. org/content/early/2012/04/17/dc 120413. full. pdf+html • Up to Hb. A 1 c of 8% is OK and maybe 8. 5%
Amazingly, the ADA agrees. Position Statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD)Published online before print April 19, 2012, doi: 10. 2337/dc 12 -0413 Diabetes Care April 19, 2012 http: //care. diabetesjournals. org/content/early/2012/04/17/dc 120413. full. pdf+html • Up to Hb. A 1 c of 8% is OK and maybe 8. 5%
 Implications for quality measures?
Implications for quality measures?
 Kavousi M et al. Evaluation of newer risk markers for coronary heart disease risk classification: A cohort study. Ann Intern Med 2012 Mar 20; 156: 438. (http: //www. annals. org/content/156/6/438. full) Do any of the new risk markers (such as CRP) add anything to the prediction of CAD risk? c
Kavousi M et al. Evaluation of newer risk markers for coronary heart disease risk classification: A cohort study. Ann Intern Med 2012 Mar 20; 156: 438. (http: //www. annals. org/content/156/6/438. full) Do any of the new risk markers (such as CRP) add anything to the prediction of CAD risk? c
 • Data that were collected prospectively from the Rotterdam Study of almost 6000 asymptomatic community-dwelling participants (mean age, 69) without known CHD.
• Data that were collected prospectively from the Rotterdam Study of almost 6000 asymptomatic community-dwelling participants (mean age, 69) without known CHD.
 Looked at the following: • Prohormone brain-type • • • natriuretic peptide (NTpro. BNP) von Willebrand factor antigen Fibrinogen C-reactive protein (CRP) Pulse wave velocity Homocysteine • • • Uric acid Glomerular filtration rate Leukocyte count, Coronary artery calcium score (CAC) Carotid intima–media thickness, Presence of peripheral artery disease,
Looked at the following: • Prohormone brain-type • • • natriuretic peptide (NTpro. BNP) von Willebrand factor antigen Fibrinogen C-reactive protein (CRP) Pulse wave velocity Homocysteine • • • Uric acid Glomerular filtration rate Leukocyte count, Coronary artery calcium score (CAC) Carotid intima–media thickness, Presence of peripheral artery disease,
 Weakness • Only half of the participants were evaluated for CAC and CRP.
Weakness • Only half of the participants were evaluated for CAC and CRP.
 Controlled for Framingham Risk Score • Only two markers increased the hazard ratio by 2 or more. • NT-pro. BNP: HR: 2. 5 • Coronary artery calcium score: HR 6. 2 • So now that we can predict, what can we do to prevent?
Controlled for Framingham Risk Score • Only two markers increased the hazard ratio by 2 or more. • NT-pro. BNP: HR: 2. 5 • Coronary artery calcium score: HR 6. 2 • So now that we can predict, what can we do to prevent?
 News about statins • FDA has changed some if its recommendations and warnings about HMG-Co. A-reductase inhibitors (“statins”). • http: //www. fda. gov/Drugs/Drug. Safety/uc m 293101. htm c
News about statins • FDA has changed some if its recommendations and warnings about HMG-Co. A-reductase inhibitors (“statins”). • http: //www. fda. gov/Drugs/Drug. Safety/uc m 293101. htm c
 News about statins • Liver enzymes every year? – Nah… – Routine periodic testing of liver enzymes is neither necessary for safe statin use nor effective for identifying rare liver toxicity early. – New recommendation, to quote the FDA: “before starting statin therapy and as clinically indicated thereafter”.
News about statins • Liver enzymes every year? – Nah… – Routine periodic testing of liver enzymes is neither necessary for safe statin use nor effective for identifying rare liver toxicity early. – New recommendation, to quote the FDA: “before starting statin therapy and as clinically indicated thereafter”.
 News about statins • What about memory and blood sugar concerns? • FDA states that non-serious and reversible cognitive changes have been associated with statin use (AERS data). – Observational and prospective studies have not found this association (*). • FDA states that elevations in glucose and A 1 c levels have been associated with statin use. – Relative risk of new onset DM in patients on statins ranges from 9 – 13% and appears real (+).
News about statins • What about memory and blood sugar concerns? • FDA states that non-serious and reversible cognitive changes have been associated with statin use (AERS data). – Observational and prospective studies have not found this association (*). • FDA states that elevations in glucose and A 1 c levels have been associated with statin use. – Relative risk of new onset DM in patients on statins ranges from 9 – 13% and appears real (+).
 • What do we learn from this? – Skip the “annual ALT” for statin monitoring. It just leads to more incidental findings of abnormal LFT’s. – Watch for the development of DM in those at risk patients on statins. However, the small increased risk of DM does not outweigh the benefits of appropriate statin use. – Cognitive changes are highly subjective and potentially due to myriad causes. Use this warning with caution.
• What do we learn from this? – Skip the “annual ALT” for statin monitoring. It just leads to more incidental findings of abnormal LFT’s. – Watch for the development of DM in those at risk patients on statins. However, the small increased risk of DM does not outweigh the benefits of appropriate statin use. – Cognitive changes are highly subjective and potentially due to myriad causes. Use this warning with caution.
 Po Lai Yau et al Impairments in Adolescence Obesity and Metabolic Syndrome and Functional and Structural Brain September 3, 2012 http: //pediatrics. aappublications. org/conte nt/early/2012/08/28/peds. 2012 -0324
Po Lai Yau et al Impairments in Adolescence Obesity and Metabolic Syndrome and Functional and Structural Brain September 3, 2012 http: //pediatrics. aappublications. org/conte nt/early/2012/08/28/peds. 2012 -0324
 What we already know: • Metabolic syndrome is associated with neurocognitive imparements in adults. • Metabolic syndrome is being seen with increasing frequency in children. • This has not been looked at in children (until now). Gatto NM, et al. Metabolic syndrome and cognitive function in healthy middleaged and older adults without diabetes. Neuropsychol Dev Cogn B Aging Neuropsychol Cogn. 2008; 15(5): 627– 641
What we already know: • Metabolic syndrome is associated with neurocognitive imparements in adults. • Metabolic syndrome is being seen with increasing frequency in children. • This has not been looked at in children (until now). Gatto NM, et al. Metabolic syndrome and cognitive function in healthy middleaged and older adults without diabetes. Neuropsychol Dev Cogn B Aging Neuropsychol Cogn. 2008; 15(5): 627– 641
 The group • Defined metabolic syndrome as: – Increased insulin levels – ATP III definition of HTN and obesity – National Health and Nutrition Examination Survey (NHANES) for triglycerides – Stringent adult levels for HDL • Need 3/5 to define adolescent Met Syn
The group • Defined metabolic syndrome as: – Increased insulin levels – ATP III definition of HTN and obesity – National Health and Nutrition Examination Survey (NHANES) for triglycerides – Stringent adult levels for HDL • Need 3/5 to define adolescent Met Syn
 • Age 14 -20 • Exclusion criteria – DM 2 – Any significant medical problems – Tanner stage <4 – Depression or use of psychoactive drugs – Hx learning disability – Pregnancy – MRI abnormality
• Age 14 -20 • Exclusion criteria – DM 2 – Any significant medical problems – Tanner stage <4 – Depression or use of psychoactive drugs – Hx learning disability – Pregnancy – MRI abnormality
 • Screened 129 – 18 excluded (DM, did not meet criteria, 6 failed to complete screening) • 49 with met syn • 62 without met syn
• Screened 129 – 18 excluded (DM, did not meet criteria, 6 failed to complete screening) • 49 with met syn • 62 without met syn
 • Standardized tests – Tested IQ, academic achievement, memory skills and executive functioning, ability to pay attention – MRI (I don’t pretend to understand this methodology)
• Standardized tests – Tested IQ, academic achievement, memory skills and executive functioning, ability to pay attention – MRI (I don’t pretend to understand this methodology)
 Results • Both groups balanced in socioeconomic status, ethnicity, gender • Cohen Effect Size • 0. 2 to 0. 3: Small • 0. 5: Medium • 0. 8 and greater: large
Results • Both groups balanced in socioeconomic status, ethnicity, gender • Cohen Effect Size • 0. 2 to 0. 3: Small • 0. 5: Medium • 0. 8 and greater: large
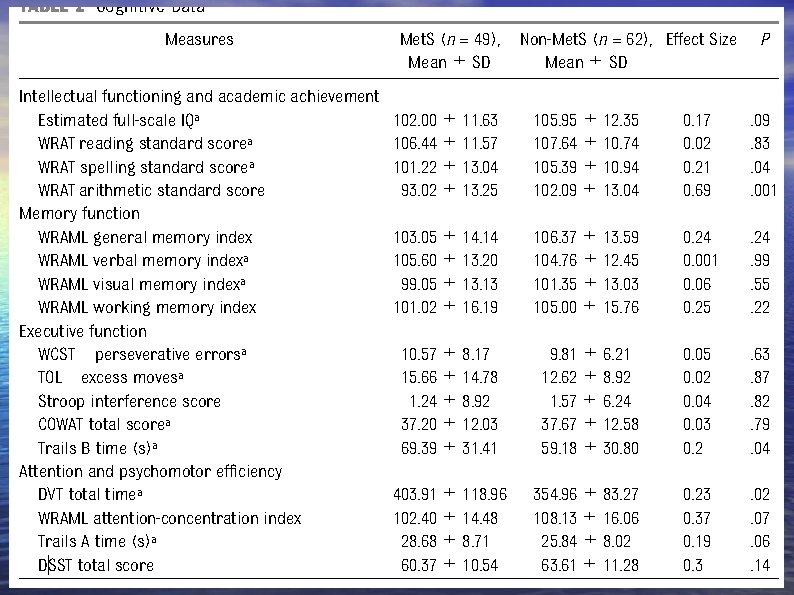
 Problems • Didn’t do Bonferroni correction • Small sample size (may actually be bigger differences based on effect sizes). • Association does not equal causality. – Is it reversible? Is it cause and effect or does decreased intellect cause overeating and Met Syn? • Very small absolute differences: is it important?
Problems • Didn’t do Bonferroni correction • Small sample size (may actually be bigger differences based on effect sizes). • Association does not equal causality. – Is it reversible? Is it cause and effect or does decreased intellect cause overeating and Met Syn? • Very small absolute differences: is it important?
 Good stuff • “Dose response effect”: Level of functioning decreased with increasing number of Met Syn criteria. • Same found in DM 2 in adolescents but more pronounced
Good stuff • “Dose response effect”: Level of functioning decreased with increasing number of Met Syn criteria. • Same found in DM 2 in adolescents but more pronounced
 Jha AK et al. The long-term effect of premier pay for performance on patient outcomes. N Engl J Med 2012 Mar 28; [e-pub ahead of print]. (http: //dx. doi. org/10. 1056/NEJMsa 1112351) Does “improvement” in process translate into improvement in patient outcomes?
Jha AK et al. The long-term effect of premier pay for performance on patient outcomes. N Engl J Med 2012 Mar 28; [e-pub ahead of print]. (http: //dx. doi. org/10. 1056/NEJMsa 1112351) Does “improvement” in process translate into improvement in patient outcomes?
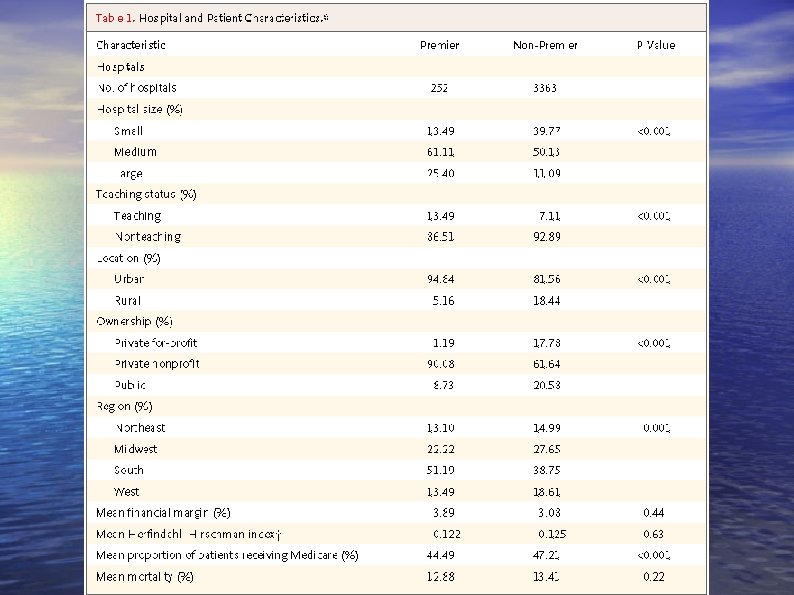
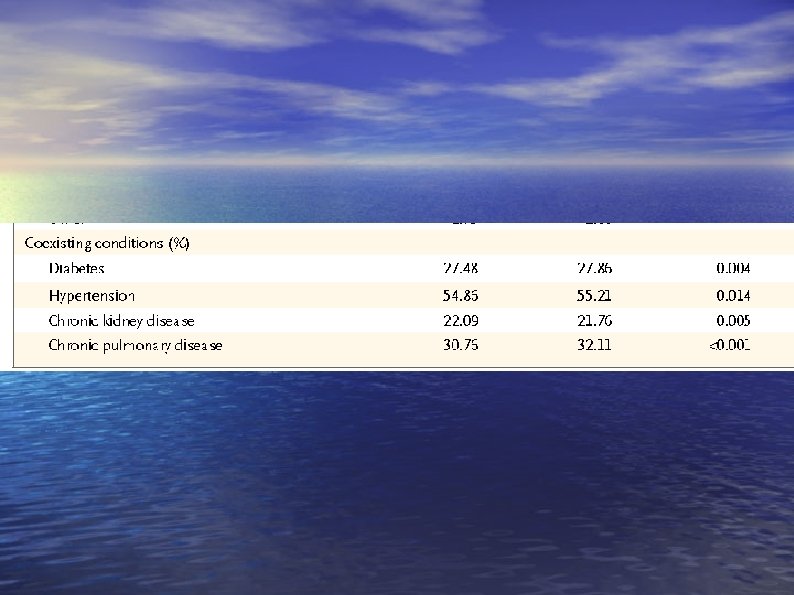
 • Medicare data for 250 hospitals participating in Medicare's Premier Hospital Quality Incentive Demonstration • 3300 hospitals that participated in public reporting alone (non-Premier). • Used Medicare part data 2002 -2009
• Medicare data for 250 hospitals participating in Medicare's Premier Hospital Quality Incentive Demonstration • 3300 hospitals that participated in public reporting alone (non-Premier). • Used Medicare part data 2002 -2009
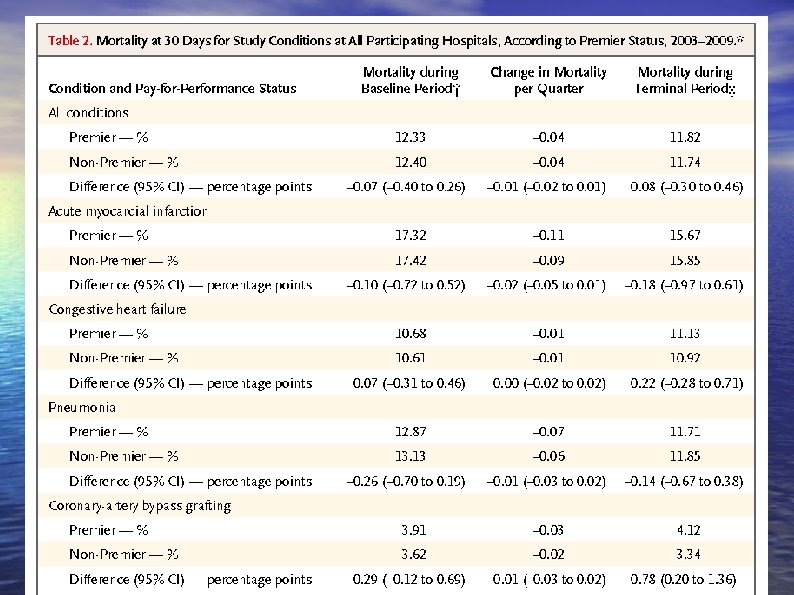
 6 million patients • Two diagnoses linked to incentives – Acute myocardial infarction – Coronary-artery bypass grafting • Two diagnoses not linked to incentives – Congestive heart failure – Pneumonia or who underwent
6 million patients • Two diagnoses linked to incentives – Acute myocardial infarction – Coronary-artery bypass grafting • Two diagnoses not linked to incentives – Congestive heart failure – Pneumonia or who underwent
 • Outcome was death • Did multivariate analysis to control for confounders: 5 models • Looked at staffing rates, rural vs urban, ownership, financial margins, etc. • Adjusted risk of death for 29 conditions
• Outcome was death • Did multivariate analysis to control for confounders: 5 models • Looked at staffing rates, rural vs urban, ownership, financial margins, etc. • Adjusted risk of death for 29 conditions
 Results • No difference in mortality between participating and non-participating hospitals. • Baseline: 12. 33% vs. 12. 40% (95% CI 0. 4, 0. 26) • Outcome: 11. 82% vs. 11. 74% (95% CI 0. 30 -0. 46)
Results • No difference in mortality between participating and non-participating hospitals. • Baseline: 12. 33% vs. 12. 40% (95% CI 0. 4, 0. 26) • Outcome: 11. 82% vs. 11. 74% (95% CI 0. 30 -0. 46)
 • Improvement in mortality at the same rate. • How about CABG? – Higher mortality at premier hospitals – 4. 12% vs. 3. 34% (95% CI 0. 2%-1. 36%)
• Improvement in mortality at the same rate. • How about CABG? – Higher mortality at premier hospitals – 4. 12% vs. 3. 34% (95% CI 0. 2%-1. 36%)
 We know guidelines work. What is the problem here?
We know guidelines work. What is the problem here?
 Heterogenous patients/hospitals. Maybe wrong quality measures.
Heterogenous patients/hospitals. Maybe wrong quality measures.
 But it does make the point that simple pay for performance likely doesn’t work well
But it does make the point that simple pay for performance likely doesn’t work well
 J Emerg Med. 2011 Mar; 40(3): 262 -6. Post Concussion syndrome is common. c And sticks around for a while
J Emerg Med. 2011 Mar; 40(3): 262 -6. Post Concussion syndrome is common. c And sticks around for a while
 Postconcussion syndrome • Concussion does not equal LOC • Concussion = any neurologic dysfunction after head injury. • 94 patients in two Canadian EDS. • Inclusion criteria – Any sx – GCS =15
Postconcussion syndrome • Concussion does not equal LOC • Concussion = any neurologic dysfunction after head injury. • 94 patients in two Canadian EDS. • Inclusion criteria – Any sx – GCS =15
 • Not necessarily your ordinary patient with minor head trauma – Were allowed hospitalization and <20 minutes LOC. • BUT – Only 17% had CT scans – All were discharged from the ED • So, were essentially the people we see.
• Not necessarily your ordinary patient with minor head trauma – Were allowed hospitalization and <20 minutes LOC. • BUT – Only 17% had CT scans – All were discharged from the ED • So, were essentially the people we see.
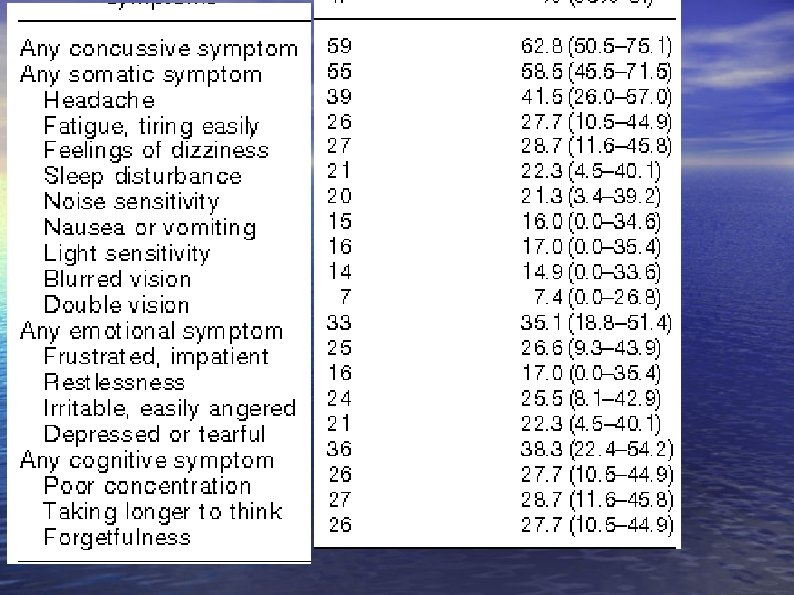
 Used a validated scale • 68/94 concussive symptoms at baseline • 59/94 (63%) still had sx at one month
Used a validated scale • 68/94 concussive symptoms at baseline • 59/94 (63%) still had sx at one month
 What is (unfortunately) “new” in Breast Cancer Treatment? Jeevan R. et al. Reoperation rates after breast conserving surgery forbreast cancer among women in England: retrospectivestudy of hospital episode statistics BMJ 2012; 345: e 4505 doi: 10. 1136/bmj. e 4505 and Mc. Cahill LE et al. Variability in reexcision following breast conservation surgery. JAMA 2012 Feb 1; 307: 467.
What is (unfortunately) “new” in Breast Cancer Treatment? Jeevan R. et al. Reoperation rates after breast conserving surgery forbreast cancer among women in England: retrospectivestudy of hospital episode statistics BMJ 2012; 345: e 4505 doi: 10. 1136/bmj. e 4505 and Mc. Cahill LE et al. Variability in reexcision following breast conservation surgery. JAMA 2012 Feb 1; 307: 467.
 Question: What percentage of patients with breast conserving therapy need a second operation? What percent need it and don’t get it?
Question: What percentage of patients with breast conserving therapy need a second operation? What percent need it and don’t get it?
 The JAMA article • 2206 women with invasive breast cancer who underwent open biopsy or partial breast conserving therapy. • 23% needed a second surgery on the same breast (bad). • 311 with positive margins did not undergo a second procedure (14%).
The JAMA article • 2206 women with invasive breast cancer who underwent open biopsy or partial breast conserving therapy. • 23% needed a second surgery on the same breast (bad). • 311 with positive margins did not undergo a second procedure (14%).
 • Total mastectomy on second surgery about 1/2: 9% • Limited to 4 institutions…… • BMJ article: 55, 297 women – All adult women in Britain undergoing breast conserving mastectomy from April 2005 March 2008
• Total mastectomy on second surgery about 1/2: 9% • Limited to 4 institutions…… • BMJ article: 55, 297 women – All adult women in Britain undergoing breast conserving mastectomy from April 2005 March 2008
 • 11 032 (20. 0%, 95% CI: 19. 6% to 20. 3%) had second surgery. • Interestingly: – Carcinoma-in-situ: 30% ( adjusted odds ratio 1. 9, 95% CI 1. 8 to 2. 0) – Locally invasive disease: 18% ( • 11% breast conserving, 7% total mastectomy.
• 11 032 (20. 0%, 95% CI: 19. 6% to 20. 3%) had second surgery. • Interestingly: – Carcinoma-in-situ: 30% ( adjusted odds ratio 1. 9, 95% CI 1. 8 to 2. 0) – Locally invasive disease: 18% ( • 11% breast conserving, 7% total mastectomy.
 What are the implications for informed consent? What are the implications for quality measures?
What are the implications for informed consent? What are the implications for quality measures?
 Saving money by treatment at home. First, new chest guidelines.
Saving money by treatment at home. First, new chest guidelines.
 You can use the cheap stuff without monitoring • “For outpatients with VTE treated with SC UFH, we suggest weight-adjusted dosing (first dose 333 units/kg, then 250 units/kg) without monitoring rather than fixed or weight-adjusted dosing with monitoring. ” • Chest. 2012; 141: 7 S-47 S.
You can use the cheap stuff without monitoring • “For outpatients with VTE treated with SC UFH, we suggest weight-adjusted dosing (first dose 333 units/kg, then 250 units/kg) without monitoring rather than fixed or weight-adjusted dosing with monitoring. ” • Chest. 2012; 141: 7 S-47 S.
 But is it safe? Aujesky D et al. Outpatient versus inpatient treatment for patients with acute pulmonary embolism: An international, open -label, randomised, non-inferiority trial. Lancet 2011 Jul 2; 378: 41. And J Thromb Haemost. 2011 Aug; 9(8): 1500 -7. doi: 10. 1111/j. 1538 -7836. 2011. 04388. x.
But is it safe? Aujesky D et al. Outpatient versus inpatient treatment for patients with acute pulmonary embolism: An international, open -label, randomised, non-inferiority trial. Lancet 2011 Jul 2; 378: 41. And J Thromb Haemost. 2011 Aug; 9(8): 1500 -7. doi: 10. 1111/j. 1538 -7836. 2011. 04388. x.
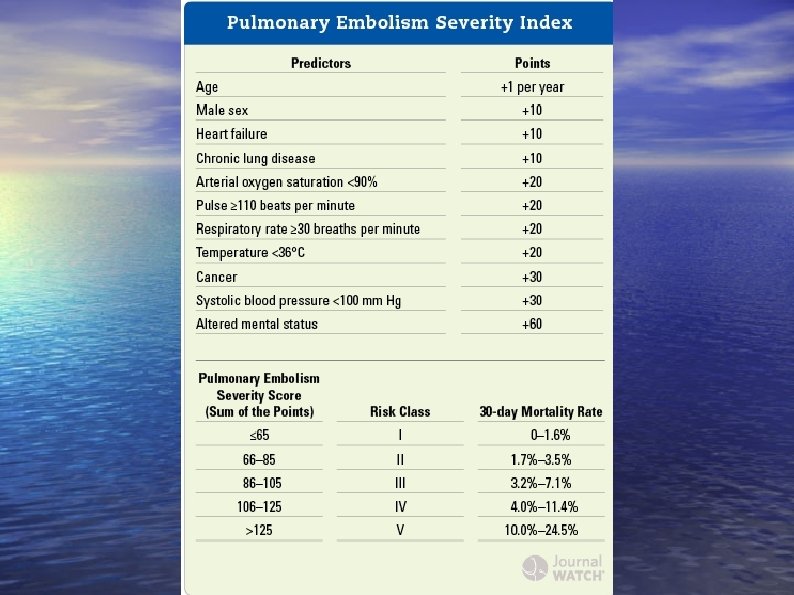
 • • • 19 Eds 171 outpatients 168 inpatients Open label, randomized, non-inferiority Patients had to have a risk of dying of less than 4% based on the PE Severity Index
• • • 19 Eds 171 outpatients 168 inpatients Open label, randomized, non-inferiority Patients had to have a risk of dying of less than 4% based on the PE Severity Index
 Exclusion criteria • O 2 sat <90% • BP <100 systolic • Chest pain requiring opioids • High risk of hemorrhage (recent stroke, bleed, • • • etc. ) Platelets < 75, 000 Cancer only 1% outpatients Cancer only 2% inpatients.
Exclusion criteria • O 2 sat <90% • BP <100 systolic • Chest pain requiring opioids • High risk of hemorrhage (recent stroke, bleed, • • • etc. ) Platelets < 75, 000 Cancer only 1% outpatients Cancer only 2% inpatients.
 • All got enoxaparin 1 mg/kg SQ followed by • • • warfarin at least 90 days 1 person in each group died. Neither from PE 1 person in outpatient group had recurrent disease. Bleeding in 3 outpatients (IM hematoma day 3 and day 13 and menorrhagia day 50) at day 13 and 50 not likely to be due to treatment
• All got enoxaparin 1 mg/kg SQ followed by • • • warfarin at least 90 days 1 person in each group died. Neither from PE 1 person in outpatient group had recurrent disease. Bleeding in 3 outpatients (IM hematoma day 3 and day 13 and menorrhagia day 50) at day 13 and 50 not likely to be due to treatment
 IT DOES MAKE THE POINT THAT OUTPATIENT TREATMENT IS SAFE…. AND THERE IS THIS…. . Büller HR et al. for the EINSTEIN–PE Investigators. Oral rivaroxaban for the treatment of symptomatic pulmonary embolism. N Engl J Med 2012 Mar 26
IT DOES MAKE THE POINT THAT OUTPATIENT TREATMENT IS SAFE…. AND THERE IS THIS…. . Büller HR et al. for the EINSTEIN–PE Investigators. Oral rivaroxaban for the treatment of symptomatic pulmonary embolism. N Engl J Med 2012 Mar 26
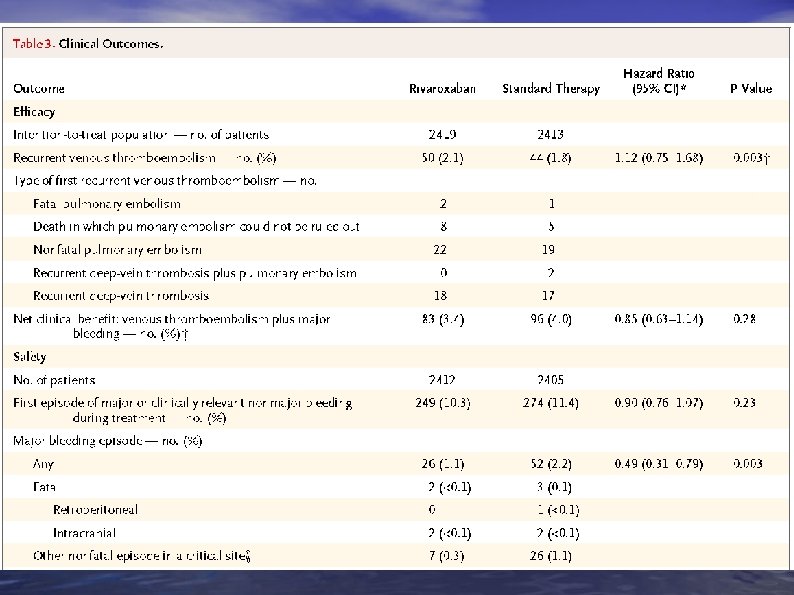
 Actually well done study. • Randomized 4833 to rivaroxaban or • • enoxaparin+ warfarin Randomized to 3, 6, or 12 months of drug. Actually were very good about calling death from PE
Actually well done study. • Randomized 4833 to rivaroxaban or • • enoxaparin+ warfarin Randomized to 3, 6, or 12 months of drug. Actually were very good about calling death from PE
 P value for non-inferiority
P value for non-inferiority
 Not FDA approved for this application. But look for it soon.
Not FDA approved for this application. But look for it soon.
 Eerenberg ES et al. Reversal of rivaroxaban and dabigatran by prothrombin complex concentrate: A randomized, placebo-controlled, crossover study in healthy subjects. Circulation 2011 Oct 4; 124: 1573. C
Eerenberg ES et al. Reversal of rivaroxaban and dabigatran by prothrombin complex concentrate: A randomized, placebo-controlled, crossover study in healthy subjects. Circulation 2011 Oct 4; 124: 1573. C
 What we know… • Both rivaroxaban and dabigatran are now approved for use in atrial fibrillation • Dabigatran is a direct thrombin inhibitor. • Rivaroxaban is a Factor Xa inhibitor • The downside is it has been “impossible” to reverse them
What we know… • Both rivaroxaban and dabigatran are now approved for use in atrial fibrillation • Dabigatran is a direct thrombin inhibitor. • Rivaroxaban is a Factor Xa inhibitor • The downside is it has been “impossible” to reverse them
 This study • Hypothesis: Prothrombin concentrates may reverse direct thrombin inhibitors and factor Xa inhibitors because they have a high concentration of factors II, VII, IX and X
This study • Hypothesis: Prothrombin concentrates may reverse direct thrombin inhibitors and factor Xa inhibitors because they have a high concentration of factors II, VII, IX and X
 • 12 healthy volunteers • Double blind crossover study • Treated with either drug for 2. 5 days • Hospitalized for Prothrombin complex concentrates IV • On a battery of tests there was reversal with rivaroxaban but not dabigatran. • Dabigatran is dialyzable (60%).
• 12 healthy volunteers • Double blind crossover study • Treated with either drug for 2. 5 days • Hospitalized for Prothrombin complex concentrates IV • On a battery of tests there was reversal with rivaroxaban but not dabigatran. • Dabigatran is dialyzable (60%).
 So what is the problem…. • 1) healthy patients • 2) did show effect on reversing bleeding…lab tests surrogate markers only. • 3) not exactly chronic use of the drugs.
So what is the problem…. • 1) healthy patients • 2) did show effect on reversing bleeding…lab tests surrogate markers only. • 3) not exactly chronic use of the drugs.
 Monitoring? ? • Dabigatran: ap. TT>2. 5 normal = over anticoagulation (? ? ) • Shoot for 1. 5 -2 X normal • Rivaroxaban: – Factor Xa levels – Elevated PT associated with drug concentrations.
Monitoring? ? • Dabigatran: ap. TT>2. 5 normal = over anticoagulation (? ? ) • Shoot for 1. 5 -2 X normal • Rivaroxaban: – Factor Xa levels – Elevated PT associated with drug concentrations.
 Turns out you can monitor dabigitran …. for a price Guess who sells the kit used for monitoring? ?
Turns out you can monitor dabigitran …. for a price Guess who sells the kit used for monitoring? ?
 Ecarin Clotting Time (ECT) • • • Monitoring for dabigatran. Not effected by other anticoagulants. Thrombin Time – Also used for monitoring direct thrombin inhibitors – Sensitive to other anticoagulants, though
Ecarin Clotting Time (ECT) • • • Monitoring for dabigatran. Not effected by other anticoagulants. Thrombin Time – Also used for monitoring direct thrombin inhibitors – Sensitive to other anticoagulants, though
 Bonus Topics
Bonus Topics
 Shingles Tseng HF et al. Herpes Zoster Vaccine in Older Adults and the Risk of Subsequent Herpes Zoster Disease. JAMA 2011; 305: 160.
Shingles Tseng HF et al. Herpes Zoster Vaccine in Older Adults and the Risk of Subsequent Herpes Zoster Disease. JAMA 2011; 305: 160.
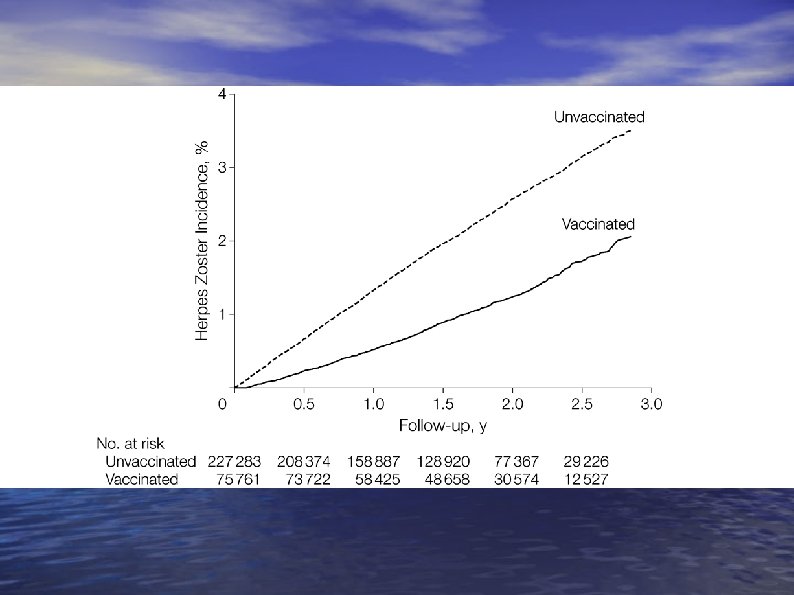
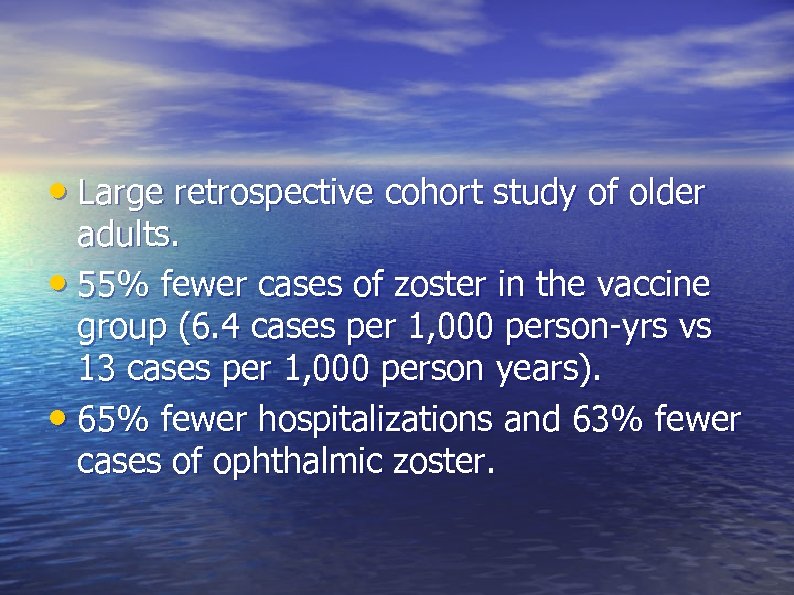 • Large retrospective cohort study of older adults. • 55% fewer cases of zoster in the vaccine group (6. 4 cases per 1, 000 person-yrs vs 13 cases per 1, 000 person years). • 65% fewer hospitalizations and 63% fewer cases of ophthalmic zoster.
• Large retrospective cohort study of older adults. • 55% fewer cases of zoster in the vaccine group (6. 4 cases per 1, 000 person-yrs vs 13 cases per 1, 000 person years). • 65% fewer hospitalizations and 63% fewer cases of ophthalmic zoster.
 Shingles • What do we take from this? – In the ‘real world’ the zoster vaccine works about as well as it did in the initial studies. – We can be confident in recommending the zoster vaccine for its efficacy (but cost is another matter…).
Shingles • What do we take from this? – In the ‘real world’ the zoster vaccine works about as well as it did in the initial studies. – We can be confident in recommending the zoster vaccine for its efficacy (but cost is another matter…).
 Not another infectious disease guideline! Urinary Tract Infection: Clinical Practice Guideline for the Diagnosis and Management of the Initial UTI in Febrile Infants and Children 2 to 24 Months SUBCOMMITTEE ON QUALITY IMPROVEMENT AND STEERING MANAGEMENT SUBCOMMITTEE ON URINARY TRACT INFECTION and STEERING Pediatrics; originally published online August 28, 2011; DOI: 10. 1542/peds. 2011 -1330 161
Not another infectious disease guideline! Urinary Tract Infection: Clinical Practice Guideline for the Diagnosis and Management of the Initial UTI in Febrile Infants and Children 2 to 24 Months SUBCOMMITTEE ON QUALITY IMPROVEMENT AND STEERING MANAGEMENT SUBCOMMITTEE ON URINARY TRACT INFECTION and STEERING Pediatrics; originally published online August 28, 2011; DOI: 10. 1542/peds. 2011 -1330 161
 What we know? • Treatment and diagnosis is all over the • • • place. Workup after 1 st episode? Workup after 2 nd episode? And what workup should be done. 162
What we know? • Treatment and diagnosis is all over the • • • place. Workup after 1 st episode? Workup after 2 nd episode? And what workup should be done. 162
 Some answers • Analysis of medical literature. • UTI defined as pyuria and at least 50, 000 cfu 163
Some answers • Analysis of medical literature. • UTI defined as pyuria and at least 50, 000 cfu 163
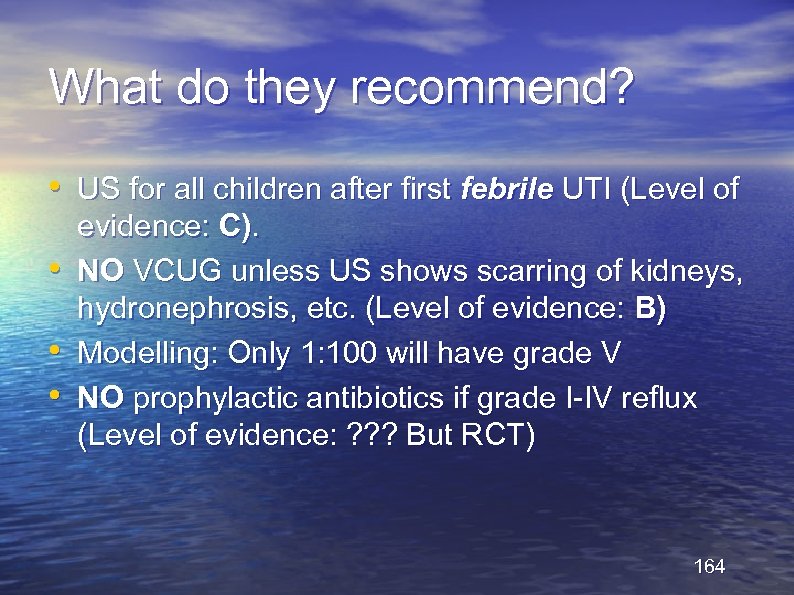 What do they recommend? • US for all children after first febrile UTI (Level of • • • evidence: C). NO VCUG unless US shows scarring of kidneys, hydronephrosis, etc. (Level of evidence: B) Modelling: Only 1: 100 will have grade V NO prophylactic antibiotics if grade I-IV reflux (Level of evidence: ? ? ? But RCT) 164
What do they recommend? • US for all children after first febrile UTI (Level of • • • evidence: C). NO VCUG unless US shows scarring of kidneys, hydronephrosis, etc. (Level of evidence: B) Modelling: Only 1: 100 will have grade V NO prophylactic antibiotics if grade I-IV reflux (Level of evidence: ? ? ? But RCT) 164
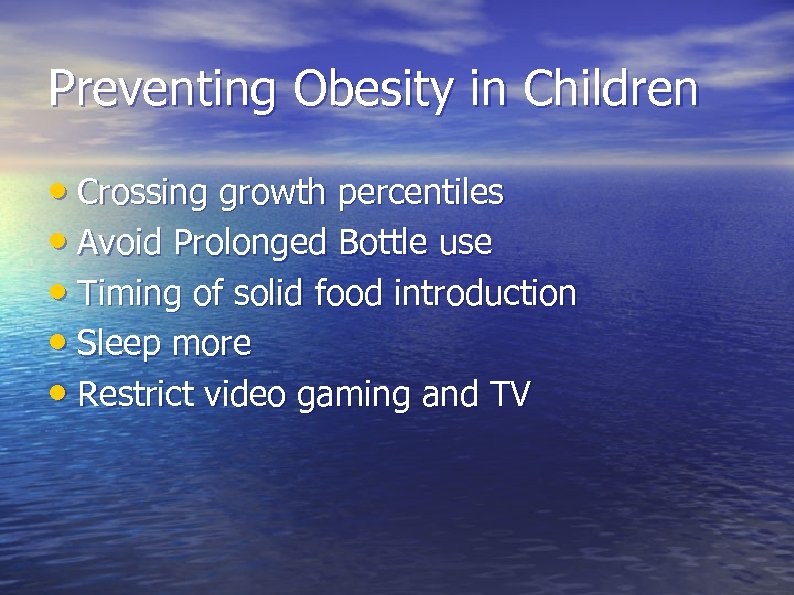 Preventing Obesity in Children • Crossing growth percentiles • Avoid Prolonged Bottle use • Timing of solid food introduction • Sleep more • Restrict video gaming and TV
Preventing Obesity in Children • Crossing growth percentiles • Avoid Prolonged Bottle use • Timing of solid food introduction • Sleep more • Restrict video gaming and TV
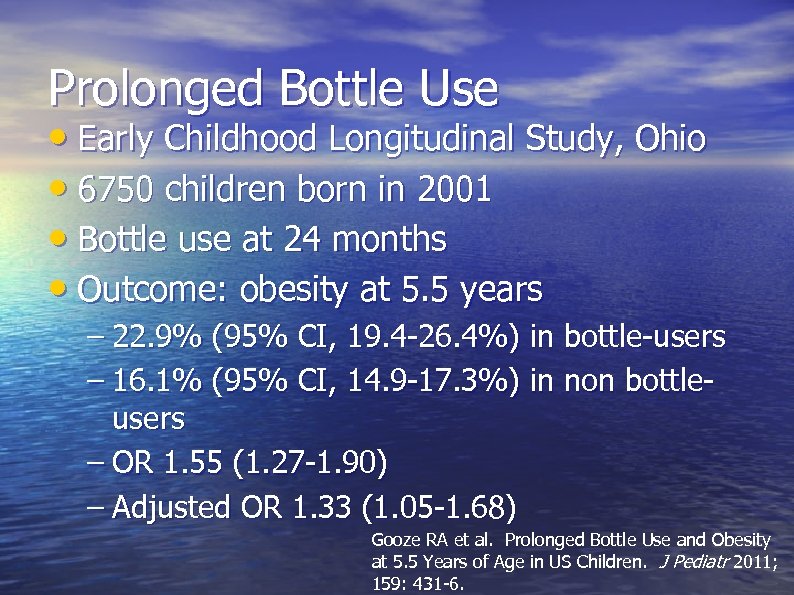 Prolonged Bottle Use • Early Childhood Longitudinal Study, Ohio • 6750 children born in 2001 • Bottle use at 24 months • Outcome: obesity at 5. 5 years – 22. 9% (95% CI, 19. 4 -26. 4%) in bottle-users – 16. 1% (95% CI, 14. 9 -17. 3%) in non bottleusers – OR 1. 55 (1. 27 -1. 90) – Adjusted OR 1. 33 (1. 05 -1. 68) Gooze RA et al. Prolonged Bottle Use and Obesity at 5. 5 Years of Age in US Children. J Pediatr 2011; 159: 431 -6.
Prolonged Bottle Use • Early Childhood Longitudinal Study, Ohio • 6750 children born in 2001 • Bottle use at 24 months • Outcome: obesity at 5. 5 years – 22. 9% (95% CI, 19. 4 -26. 4%) in bottle-users – 16. 1% (95% CI, 14. 9 -17. 3%) in non bottleusers – OR 1. 55 (1. 27 -1. 90) – Adjusted OR 1. 33 (1. 05 -1. 68) Gooze RA et al. Prolonged Bottle Use and Obesity at 5. 5 Years of Age in US Children. J Pediatr 2011; 159: 431 -6.
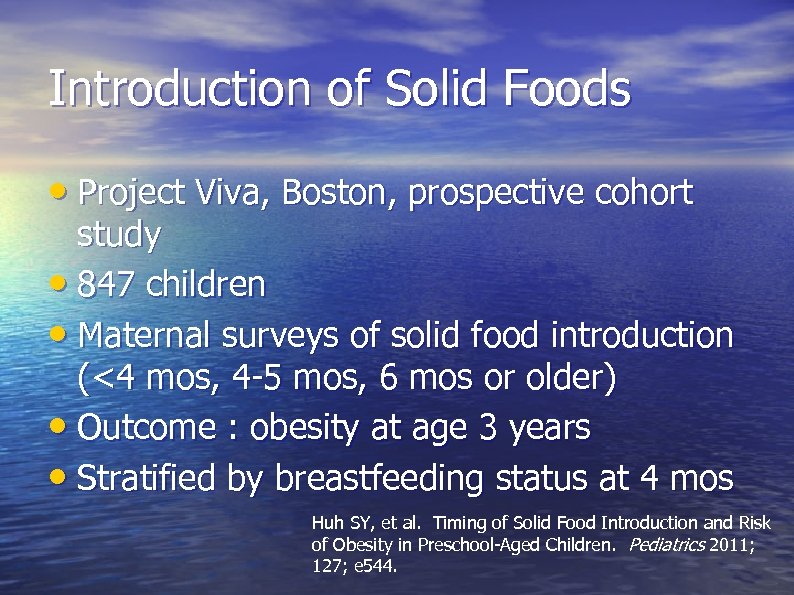 Introduction of Solid Foods • Project Viva, Boston, prospective cohort study • 847 children • Maternal surveys of solid food introduction (<4 mos, 4 -5 mos, 6 mos or older) • Outcome : obesity at age 3 years • Stratified by breastfeeding status at 4 mos Huh SY, et al. Timing of Solid Food Introduction and Risk of Obesity in Preschool-Aged Children. Pediatrics 2011; 127; e 544.
Introduction of Solid Foods • Project Viva, Boston, prospective cohort study • 847 children • Maternal surveys of solid food introduction (<4 mos, 4 -5 mos, 6 mos or older) • Outcome : obesity at age 3 years • Stratified by breastfeeding status at 4 mos Huh SY, et al. Timing of Solid Food Introduction and Risk of Obesity in Preschool-Aged Children. Pediatrics 2011; 127; e 544.
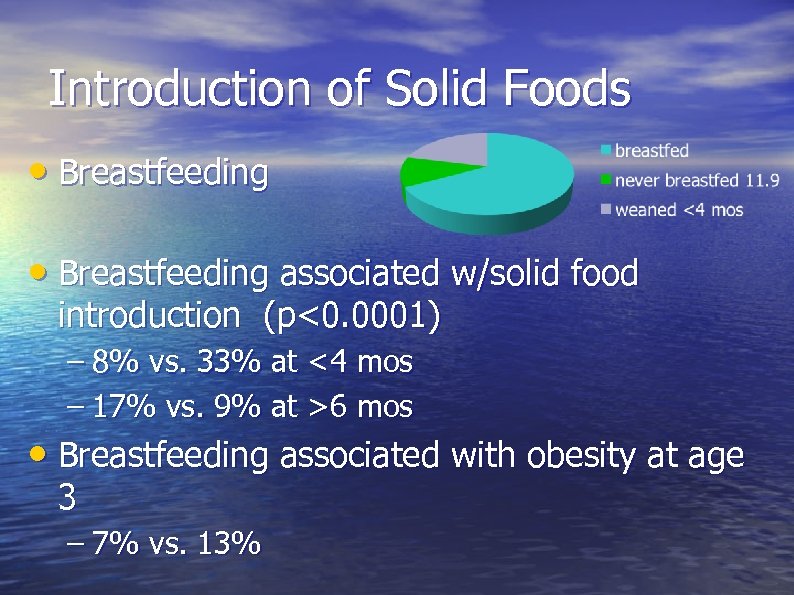 Introduction of Solid Foods • Breastfeeding associated w/solid food introduction (p<0. 0001) – 8% vs. 33% at <4 mos – 17% vs. 9% at >6 mos • Breastfeeding associated with obesity at age 3 – 7% vs. 13%
Introduction of Solid Foods • Breastfeeding associated w/solid food introduction (p<0. 0001) – 8% vs. 33% at <4 mos – 17% vs. 9% at >6 mos • Breastfeeding associated with obesity at age 3 – 7% vs. 13%
 Introduction of Solid Foods • Among breastfed infants, timing of solid foods was not associated with obesity at age 3 • Among formula-fed infants, early or late introduction was associated with – Obesity (OR 6. 3 for early) – Weight for age – BMI
Introduction of Solid Foods • Among breastfed infants, timing of solid foods was not associated with obesity at age 3 • Among formula-fed infants, early or late introduction was associated with – Obesity (OR 6. 3 for early) – Weight for age – BMI
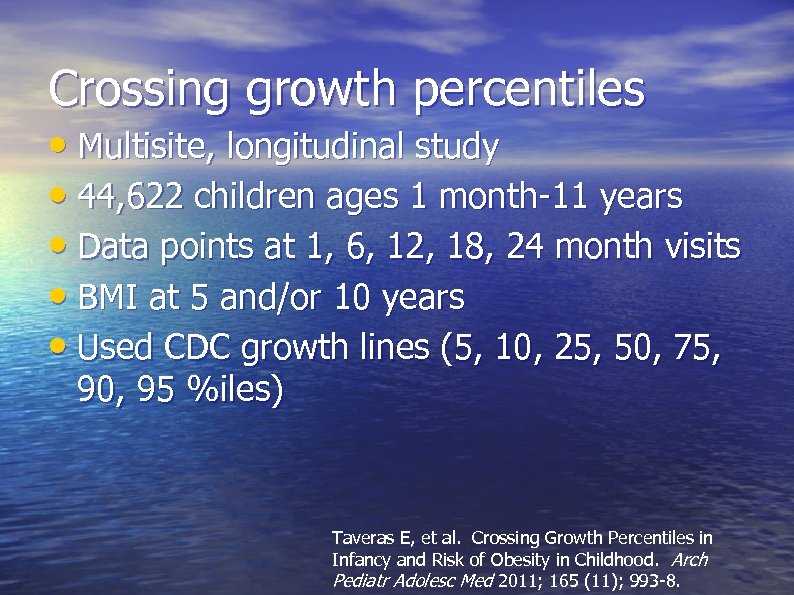 Crossing growth percentiles • Multisite, longitudinal study • 44, 622 children ages 1 month-11 years • Data points at 1, 6, 12, 18, 24 month visits • BMI at 5 and/or 10 years • Used CDC growth lines (5, 10, 25, 50, 75, 90, 95 %iles) Taveras E, et al. Crossing Growth Percentiles in Infancy and Risk of Obesity in Childhood. Arch Pediatr Adolesc Med 2011; 165 (11); 993 -8.
Crossing growth percentiles • Multisite, longitudinal study • 44, 622 children ages 1 month-11 years • Data points at 1, 6, 12, 18, 24 month visits • BMI at 5 and/or 10 years • Used CDC growth lines (5, 10, 25, 50, 75, 90, 95 %iles) Taveras E, et al. Crossing Growth Percentiles in Infancy and Risk of Obesity in Childhood. Arch Pediatr Adolesc Med 2011; 165 (11); 993 -8.
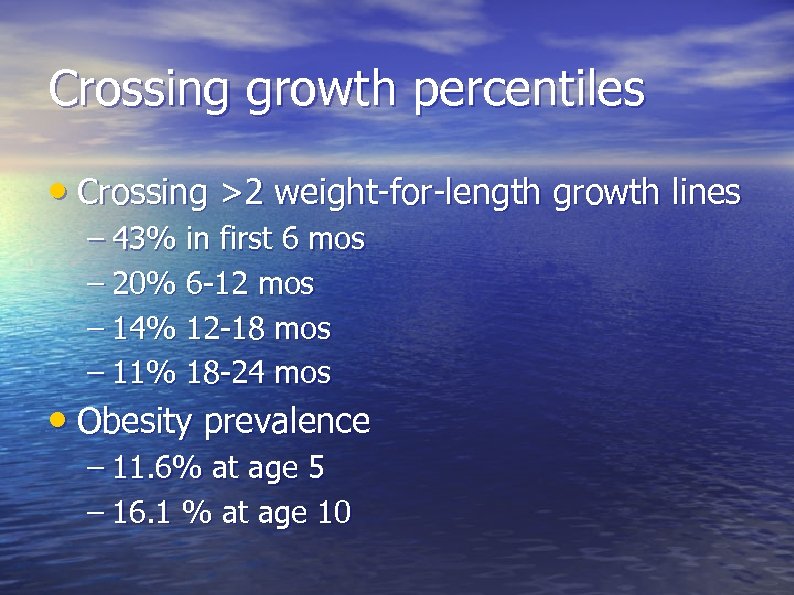 Crossing growth percentiles • Crossing >2 weight-for-length growth lines – 43% in first 6 mos – 20% 6 -12 mos – 14% 12 -18 mos – 11% 18 -24 mos • Obesity prevalence – 11. 6% at age 5 – 16. 1 % at age 10
Crossing growth percentiles • Crossing >2 weight-for-length growth lines – 43% in first 6 mos – 20% 6 -12 mos – 14% 12 -18 mos – 11% 18 -24 mos • Obesity prevalence – 11. 6% at age 5 – 16. 1 % at age 10
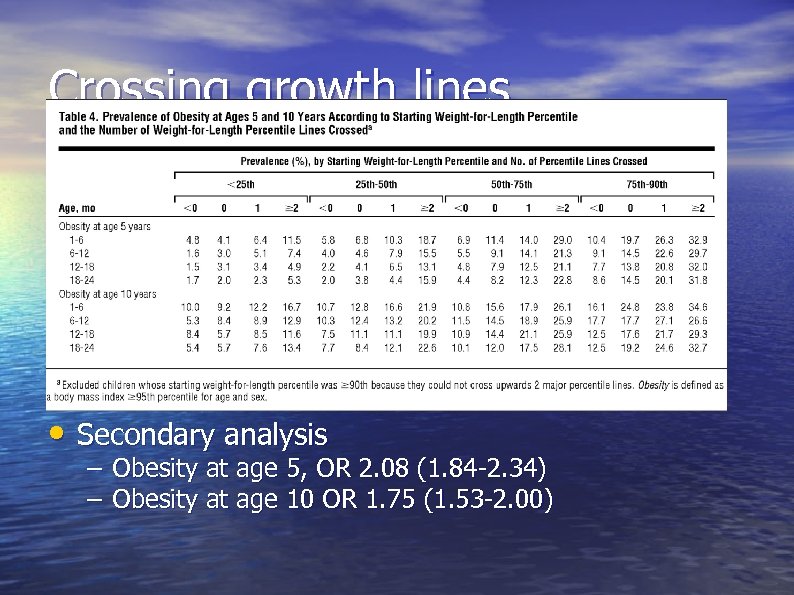 Crossing growth lines • Secondary analysis – Obesity at age 5, OR 2. 08 (1. 84 -2. 34) – Obesity at age 10 OR 1. 75 (1. 53 -2. 00)
Crossing growth lines • Secondary analysis – Obesity at age 5, OR 2. 08 (1. 84 -2. 34) – Obesity at age 10 OR 1. 75 (1. 53 -2. 00)
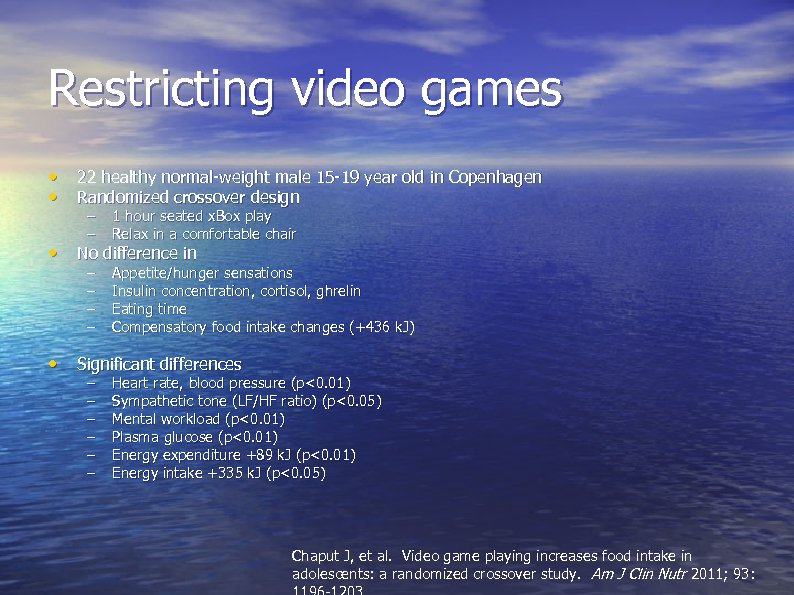 Restricting video games • 22 healthy normal-weight male 15 -19 year old in Copenhagen • Randomized crossover design – – 1 hour seated x. Box play Relax in a comfortable chair – – Appetite/hunger sensations Insulin concentration, cortisol, ghrelin Eating time Compensatory food intake changes (+436 k. J) • No difference in • Significant differences – – – Heart rate, blood pressure (p<0. 01) Sympathetic tone (LF/HF ratio) (p<0. 05) Mental workload (p<0. 01) Plasma glucose (p<0. 01) Energy expenditure +89 k. J (p<0. 01) Energy intake +335 k. J (p<0. 05) Chaput J, et al. Video game playing increases food intake in adolescents: a randomized crossover study. Am J Clin Nutr 2011; 93:
Restricting video games • 22 healthy normal-weight male 15 -19 year old in Copenhagen • Randomized crossover design – – 1 hour seated x. Box play Relax in a comfortable chair – – Appetite/hunger sensations Insulin concentration, cortisol, ghrelin Eating time Compensatory food intake changes (+436 k. J) • No difference in • Significant differences – – – Heart rate, blood pressure (p<0. 01) Sympathetic tone (LF/HF ratio) (p<0. 05) Mental workload (p<0. 01) Plasma glucose (p<0. 01) Energy expenditure +89 k. J (p<0. 01) Energy intake +335 k. J (p<0. 05) Chaput J, et al. Video game playing increases food intake in adolescents: a randomized crossover study. Am J Clin Nutr 2011; 93:
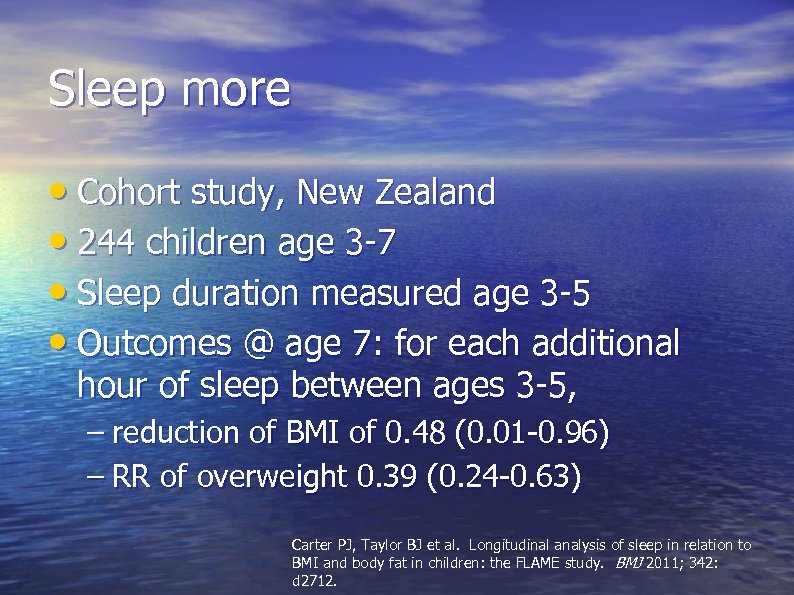 Sleep more • Cohort study, New Zealand • 244 children age 3 -7 • Sleep duration measured age 3 -5 • Outcomes @ age 7: for each additional hour of sleep between ages 3 -5, – reduction of BMI of 0. 48 (0. 01 -0. 96) – RR of overweight 0. 39 (0. 24 -0. 63) Carter PJ, Taylor BJ et al. Longitudinal analysis of sleep in relation to BMI and body fat in children: the FLAME study. BMJ 2011; 342: d 2712.
Sleep more • Cohort study, New Zealand • 244 children age 3 -7 • Sleep duration measured age 3 -5 • Outcomes @ age 7: for each additional hour of sleep between ages 3 -5, – reduction of BMI of 0. 48 (0. 01 -0. 96) – RR of overweight 0. 39 (0. 24 -0. 63) Carter PJ, Taylor BJ et al. Longitudinal analysis of sleep in relation to BMI and body fat in children: the FLAME study. BMJ 2011; 342: d 2712.
 What about beta-blockers in COPD?
What about beta-blockers in COPD?
 • • • 6000 COPD patients Retrospective cohort study 819 taking a beta-blocker Mean age 69 After 4. 4 year follow-up – 1/3 rd died – Beta blocker use associated with a 22% decrease in all cause mortality – No adverse effects on lung function • Other similar studies – BMJ 2011 May 10; 342: d 2549. (http: //dx. doi. org/10. 1136/bmj. d 2549) Rutten FH et al. β-blockers may reduce mortality and risk of exacerbations in patients with chronic obstructive pulmonary disease. Arch Intern Med 2010 May 24; 170: 880.
• • • 6000 COPD patients Retrospective cohort study 819 taking a beta-blocker Mean age 69 After 4. 4 year follow-up – 1/3 rd died – Beta blocker use associated with a 22% decrease in all cause mortality – No adverse effects on lung function • Other similar studies – BMJ 2011 May 10; 342: d 2549. (http: //dx. doi. org/10. 1136/bmj. d 2549) Rutten FH et al. β-blockers may reduce mortality and risk of exacerbations in patients with chronic obstructive pulmonary disease. Arch Intern Med 2010 May 24; 170: 880.
 Metformin causes B-12 deficiency • 390 patients randomized to Insulin + metformin or Metformin + placebo • 19% lower B 12 levels • 7% had true B 12 deficiency • 11% low B 12 levels • So, think about this as a cause of neuropathy in those on metformin BMJ 2010 May 20; 340: c 2181
Metformin causes B-12 deficiency • 390 patients randomized to Insulin + metformin or Metformin + placebo • 19% lower B 12 levels • 7% had true B 12 deficiency • 11% low B 12 levels • So, think about this as a cause of neuropathy in those on metformin BMJ 2010 May 20; 340: c 2181


