ed557cfcd329d4968861ef21d6d5de5b.ppt
- Количество слайдов: 33
 ARDS ----------------------------------------------------------- Ventilator Management Nimesh Mehta, MD Pulmonary and Critical Care Salem Pulmonary Associates
ARDS ----------------------------------------------------------- Ventilator Management Nimesh Mehta, MD Pulmonary and Critical Care Salem Pulmonary Associates
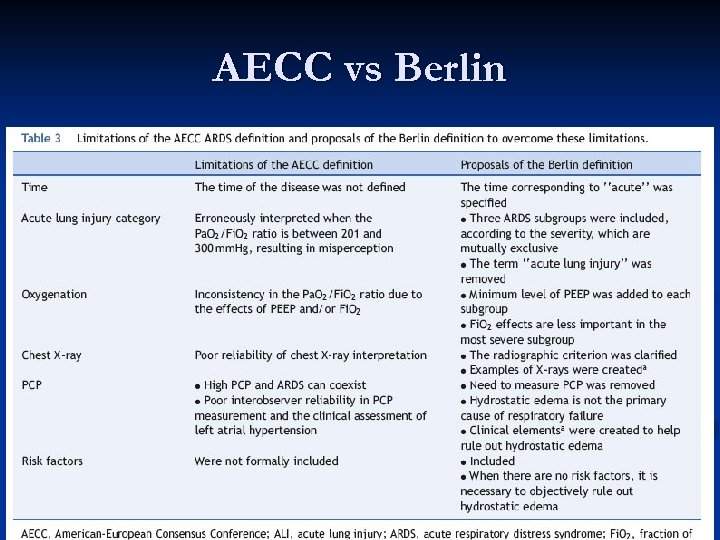 AECC vs Berlin
AECC vs Berlin
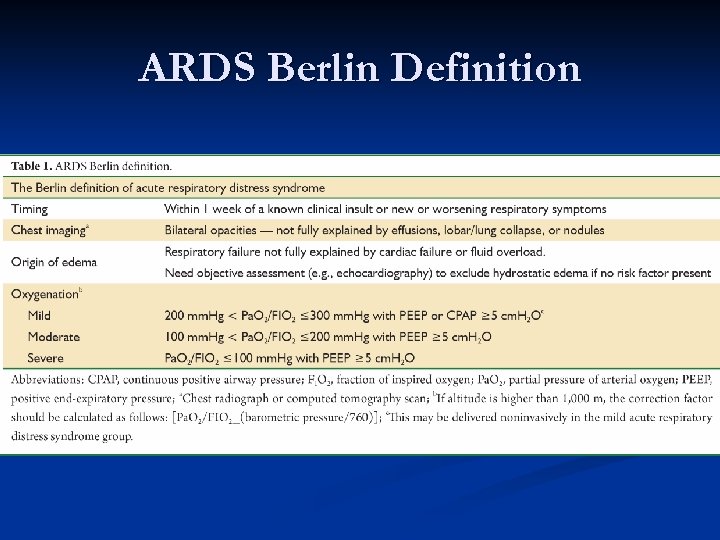 ARDS Berlin Definition
ARDS Berlin Definition
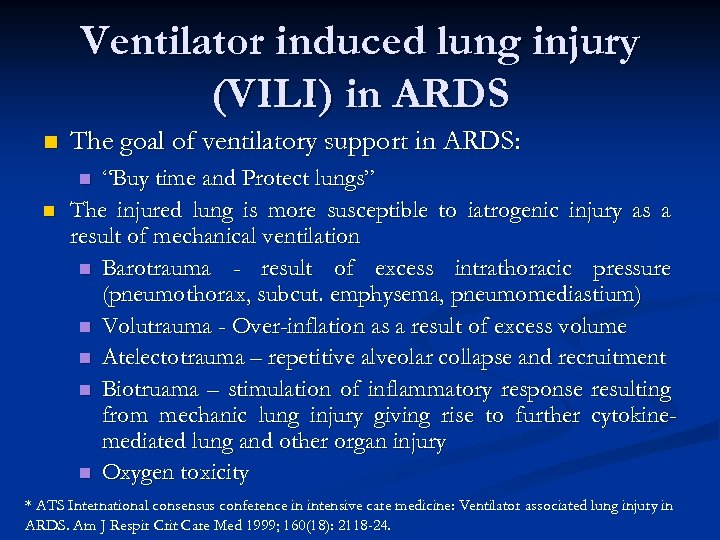 Ventilator induced lung injury (VILI) in ARDS n The goal of ventilatory support in ARDS: “Buy time and Protect lungs” The injured lung is more susceptible to iatrogenic injury as a result of mechanical ventilation n Barotrauma - result of excess intrathoracic pressure (pneumothorax, subcut. emphysema, pneumomediastium) n Volutrauma - Over-inflation as a result of excess volume n Atelectotrauma – repetitive alveolar collapse and recruitment n Biotruama – stimulation of inflammatory response resulting from mechanic lung injury giving rise to further cytokinemediated lung and other organ injury n Oxygen toxicity n n * ATS International consensus conference in intensive care medicine: Ventilator associated lung injury in ARDS. Am J Respir Crit Care Med 1999; 160(18): 2118 -24.
Ventilator induced lung injury (VILI) in ARDS n The goal of ventilatory support in ARDS: “Buy time and Protect lungs” The injured lung is more susceptible to iatrogenic injury as a result of mechanical ventilation n Barotrauma - result of excess intrathoracic pressure (pneumothorax, subcut. emphysema, pneumomediastium) n Volutrauma - Over-inflation as a result of excess volume n Atelectotrauma – repetitive alveolar collapse and recruitment n Biotruama – stimulation of inflammatory response resulting from mechanic lung injury giving rise to further cytokinemediated lung and other organ injury n Oxygen toxicity n n * ATS International consensus conference in intensive care medicine: Ventilator associated lung injury in ARDS. Am J Respir Crit Care Med 1999; 160(18): 2118 -24.
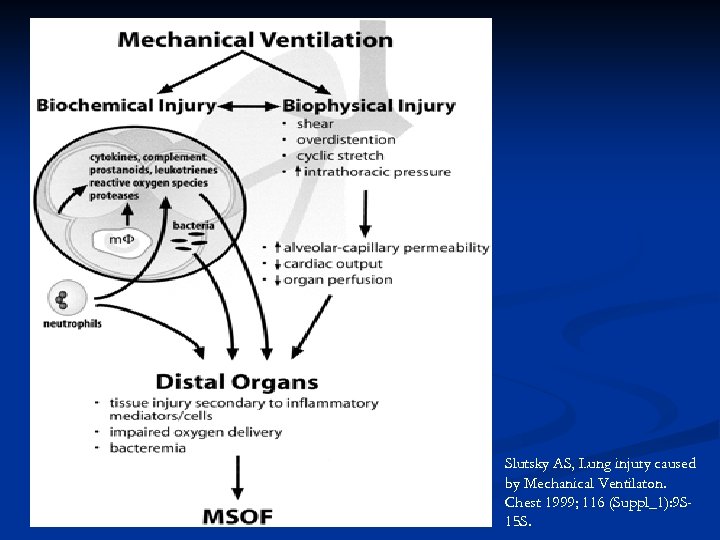 Slutsky AS, Lung injury caused by Mechanical Ventilaton. Chest 1999; 116 (Suppl_1): 9 S 15 S.
Slutsky AS, Lung injury caused by Mechanical Ventilaton. Chest 1999; 116 (Suppl_1): 9 S 15 S.
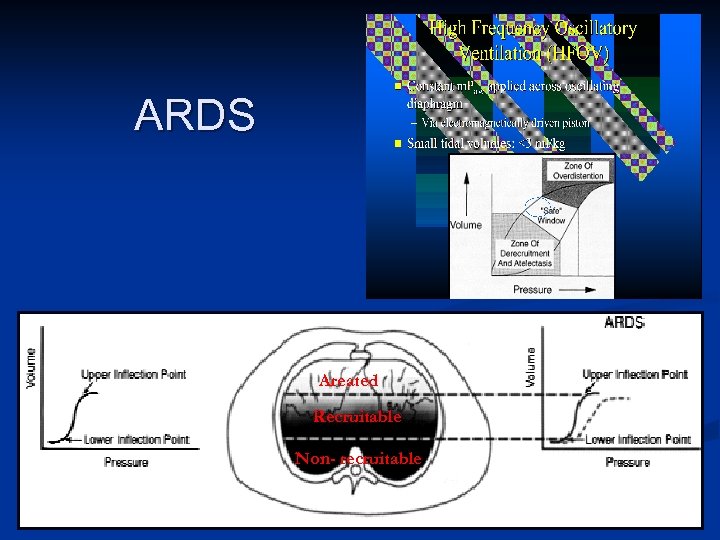 ARDS Areated Recruitable Non- recruitable
ARDS Areated Recruitable Non- recruitable
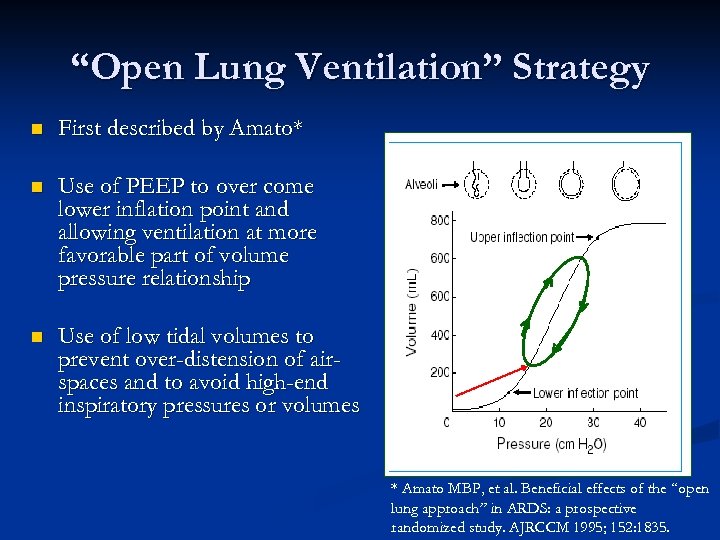 “Open Lung Ventilation” Strategy n First described by Amato* n Use of PEEP to over come lower inflation point and allowing ventilation at more favorable part of volume pressure relationship n Use of low tidal volumes to prevent over-distension of airspaces and to avoid high-end inspiratory pressures or volumes * Amato MBP, et al. Beneficial effects of the “open lung approach” in ARDS: a prospective randomized study. AJRCCM 1995; 152: 1835.
“Open Lung Ventilation” Strategy n First described by Amato* n Use of PEEP to over come lower inflation point and allowing ventilation at more favorable part of volume pressure relationship n Use of low tidal volumes to prevent over-distension of airspaces and to avoid high-end inspiratory pressures or volumes * Amato MBP, et al. Beneficial effects of the “open lung approach” in ARDS: a prospective randomized study. AJRCCM 1995; 152: 1835.
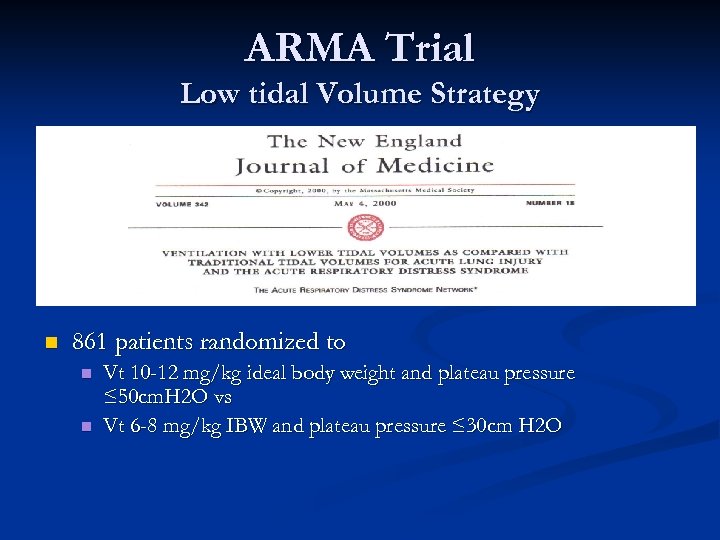 ARMA Trial Low tidal Volume Strategy n 861 patients randomized to n n Vt 10 -12 mg/kg ideal body weight and plateau pressure ≤ 50 cm. H 2 O vs Vt 6 -8 mg/kg IBW and plateau pressure ≤ 30 cm H 2 O
ARMA Trial Low tidal Volume Strategy n 861 patients randomized to n n Vt 10 -12 mg/kg ideal body weight and plateau pressure ≤ 50 cm. H 2 O vs Vt 6 -8 mg/kg IBW and plateau pressure ≤ 30 cm H 2 O
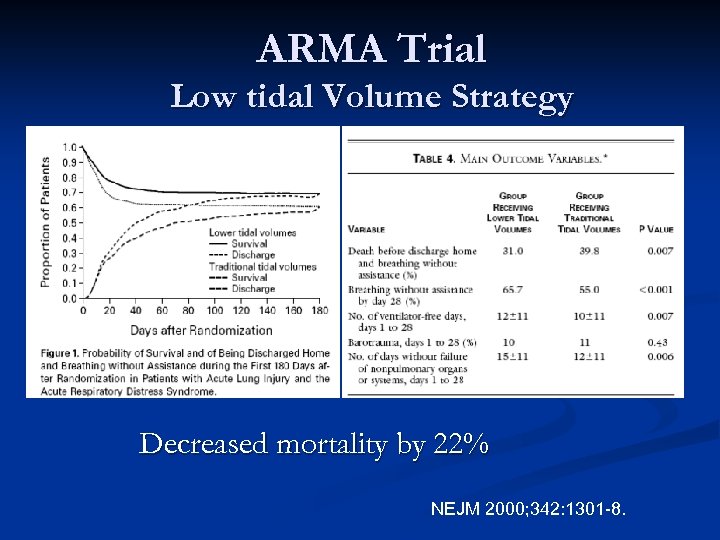 ARMA Trial Low tidal Volume Strategy Decreased mortality by 22% NEJM 2000; 342: 1301 -8.
ARMA Trial Low tidal Volume Strategy Decreased mortality by 22% NEJM 2000; 342: 1301 -8.
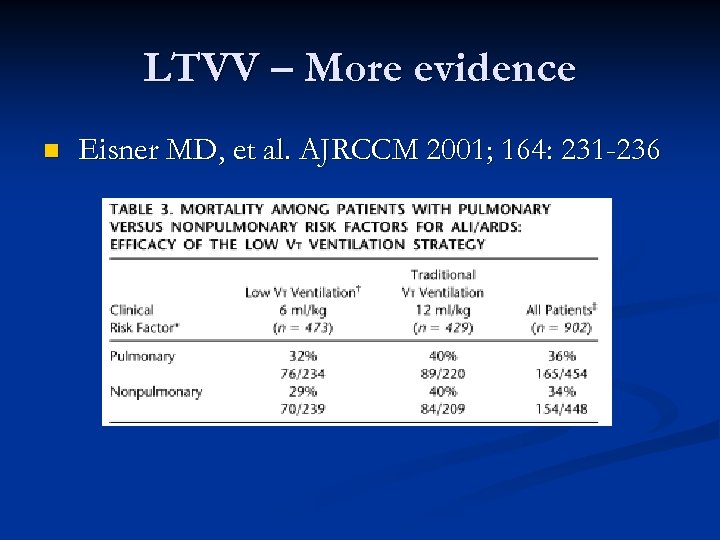 LTVV – More evidence n Eisner MD, et al. AJRCCM 2001; 164: 231 -236
LTVV – More evidence n Eisner MD, et al. AJRCCM 2001; 164: 231 -236
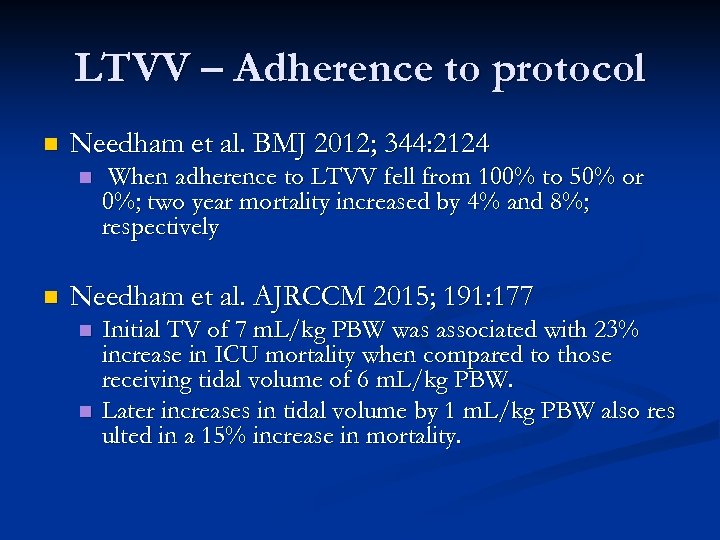 LTVV – Adherence to protocol n Needham et al. BMJ 2012; 344: 2124 n n When adherence to LTVV fell from 100% to 50% or 0%; two year mortality increased by 4% and 8%; respectively Needham et al. AJRCCM 2015; 191: 177 n n Initial TV of 7 m. L/kg PBW was associated with 23% increase in ICU mortality when compared to those receiving tidal volume of 6 m. L/kg PBW. Later increases in tidal volume by 1 m. L/kg PBW also res ulted in a 15% increase in mortality.
LTVV – Adherence to protocol n Needham et al. BMJ 2012; 344: 2124 n n When adherence to LTVV fell from 100% to 50% or 0%; two year mortality increased by 4% and 8%; respectively Needham et al. AJRCCM 2015; 191: 177 n n Initial TV of 7 m. L/kg PBW was associated with 23% increase in ICU mortality when compared to those receiving tidal volume of 6 m. L/kg PBW. Later increases in tidal volume by 1 m. L/kg PBW also res ulted in a 15% increase in mortality.
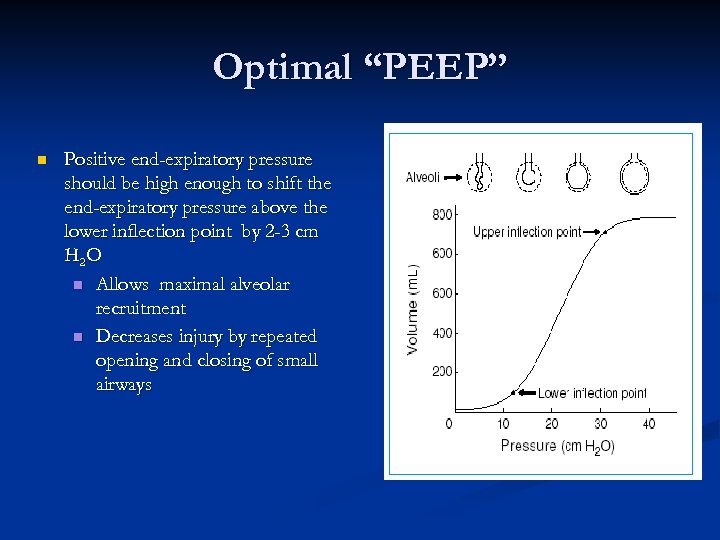 Optimal “PEEP” n Positive end-expiratory pressure should be high enough to shift the end-expiratory pressure above the lower inflection point by 2 -3 cm H 2 O n Allows maximal alveolar recruitment n Decreases injury by repeated opening and closing of small airways
Optimal “PEEP” n Positive end-expiratory pressure should be high enough to shift the end-expiratory pressure above the lower inflection point by 2 -3 cm H 2 O n Allows maximal alveolar recruitment n Decreases injury by repeated opening and closing of small airways
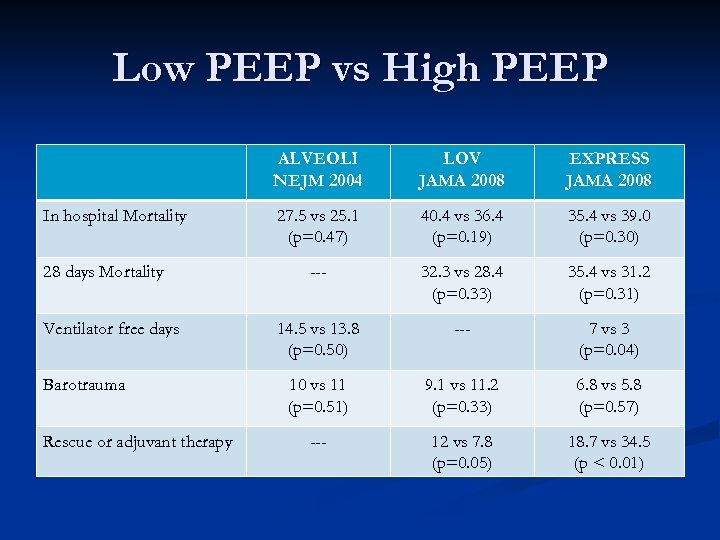 Low PEEP vs High PEEP ALVEOLI NEJM 2004 In hospital Mortality 28 days Mortality Ventilator free days Barotrauma Rescue or adjuvant therapy LOV JAMA 2008 EXPRESS JAMA 2008 27. 5 vs 25. 1 (p=0. 47) 40. 4 vs 36. 4 (p=0. 19) 35. 4 vs 39. 0 (p=0. 30) --- 32. 3 vs 28. 4 (p=0. 33) 35. 4 vs 31. 2 (p=0. 31) 14. 5 vs 13. 8 (p=0. 50) --- 7 vs 3 (p=0. 04) 10 vs 11 (p=0. 51) 9. 1 vs 11. 2 (p=0. 33) 6. 8 vs 5. 8 (p=0. 57) --- 12 vs 7. 8 (p=0. 05) 18. 7 vs 34. 5 (p < 0. 01)
Low PEEP vs High PEEP ALVEOLI NEJM 2004 In hospital Mortality 28 days Mortality Ventilator free days Barotrauma Rescue or adjuvant therapy LOV JAMA 2008 EXPRESS JAMA 2008 27. 5 vs 25. 1 (p=0. 47) 40. 4 vs 36. 4 (p=0. 19) 35. 4 vs 39. 0 (p=0. 30) --- 32. 3 vs 28. 4 (p=0. 33) 35. 4 vs 31. 2 (p=0. 31) 14. 5 vs 13. 8 (p=0. 50) --- 7 vs 3 (p=0. 04) 10 vs 11 (p=0. 51) 9. 1 vs 11. 2 (p=0. 33) 6. 8 vs 5. 8 (p=0. 57) --- 12 vs 7. 8 (p=0. 05) 18. 7 vs 34. 5 (p < 0. 01)
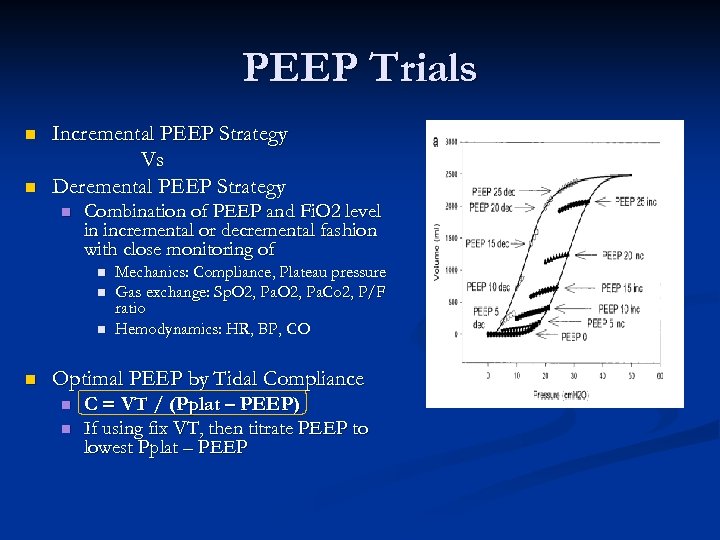 PEEP Trials n n Incremental PEEP Strategy Vs Deremental PEEP Strategy n Combination of PEEP and Fi. O 2 level in incremental or decremental fashion with close monitoring of n n Mechanics: Compliance, Plateau pressure Gas exchange: Sp. O 2, Pa. Co 2, P/F ratio Hemodynamics: HR, BP, CO Optimal PEEP by Tidal Compliance n n C = VT / (Pplat – PEEP) If using fix VT, then titrate PEEP to lowest Pplat – PEEP
PEEP Trials n n Incremental PEEP Strategy Vs Deremental PEEP Strategy n Combination of PEEP and Fi. O 2 level in incremental or decremental fashion with close monitoring of n n Mechanics: Compliance, Plateau pressure Gas exchange: Sp. O 2, Pa. Co 2, P/F ratio Hemodynamics: HR, BP, CO Optimal PEEP by Tidal Compliance n n C = VT / (Pplat – PEEP) If using fix VT, then titrate PEEP to lowest Pplat – PEEP
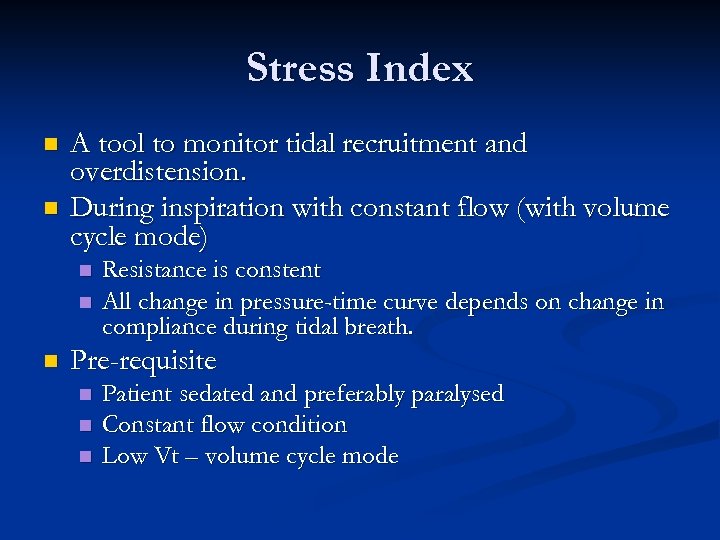 Stress Index n n A tool to monitor tidal recruitment and overdistension. During inspiration with constant flow (with volume cycle mode) n n n Resistance is constent All change in pressure-time curve depends on change in compliance during tidal breath. Pre-requisite n n n Patient sedated and preferably paralysed Constant flow condition Low Vt – volume cycle mode
Stress Index n n A tool to monitor tidal recruitment and overdistension. During inspiration with constant flow (with volume cycle mode) n n n Resistance is constent All change in pressure-time curve depends on change in compliance during tidal breath. Pre-requisite n n n Patient sedated and preferably paralysed Constant flow condition Low Vt – volume cycle mode
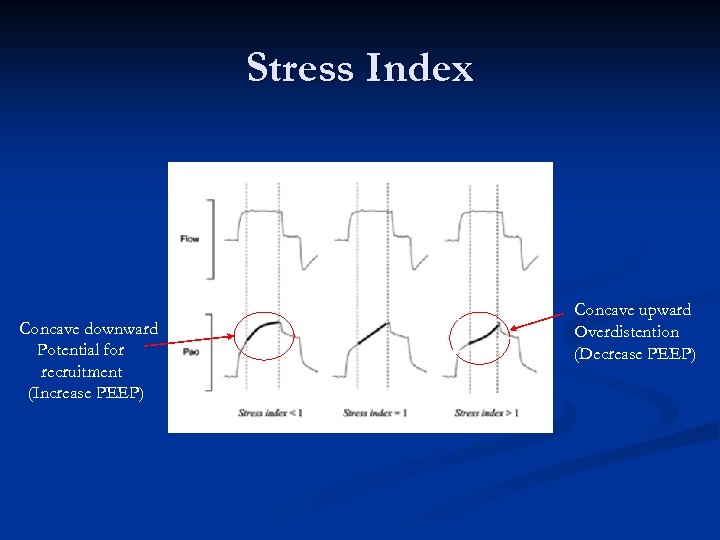 Stress Index Concave downward Potential for recruitment (Increase PEEP) Concave upward Overdistention (Decrease PEEP)
Stress Index Concave downward Potential for recruitment (Increase PEEP) Concave upward Overdistention (Decrease PEEP)
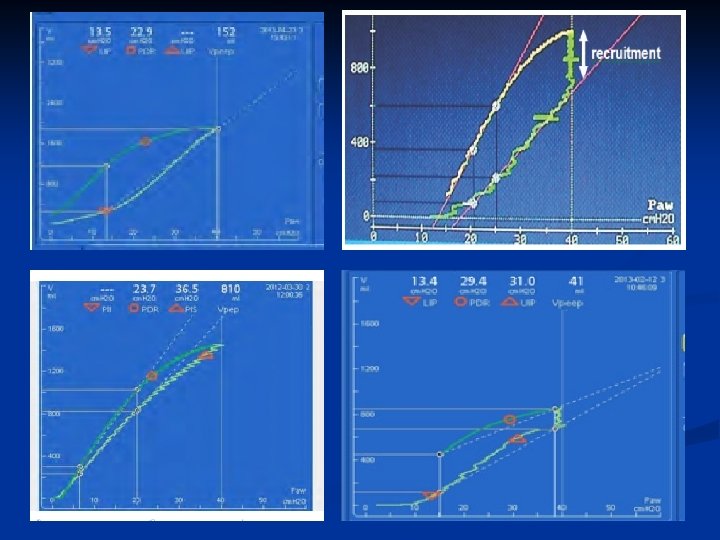
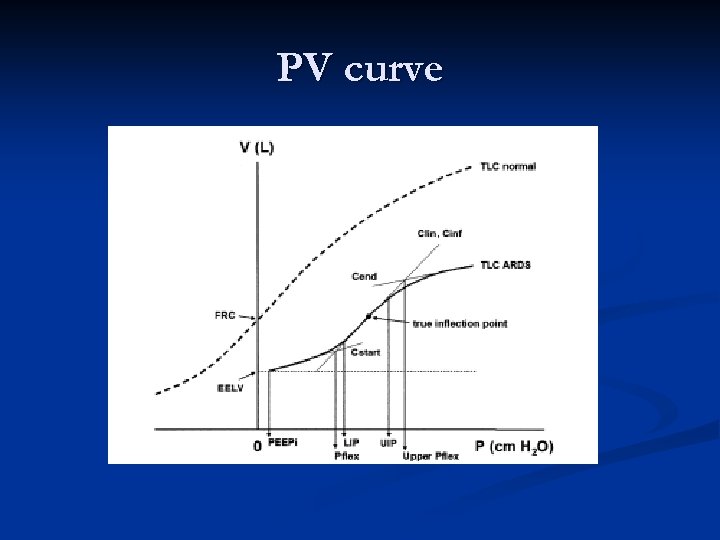 PV curve
PV curve
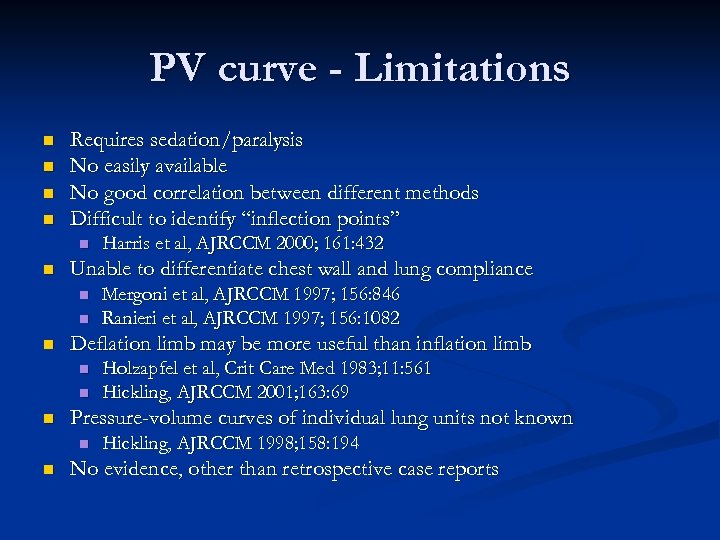 PV curve - Limitations n n Requires sedation/paralysis No easily available No good correlation between different methods Difficult to identify “inflection points” n n Unable to differentiate chest wall and lung compliance n n Holzapfel et al, Crit Care Med 1983; 11: 561 Hickling, AJRCCM 2001; 163: 69 Pressure-volume curves of individual lung units not known n n Mergoni et al, AJRCCM 1997; 156: 846 Ranieri et al, AJRCCM 1997; 156: 1082 Deflation limb may be more useful than inflation limb n n Harris et al, AJRCCM 2000; 161: 432 Hickling, AJRCCM 1998; 158: 194 No evidence, other than retrospective case reports
PV curve - Limitations n n Requires sedation/paralysis No easily available No good correlation between different methods Difficult to identify “inflection points” n n Unable to differentiate chest wall and lung compliance n n Holzapfel et al, Crit Care Med 1983; 11: 561 Hickling, AJRCCM 2001; 163: 69 Pressure-volume curves of individual lung units not known n n Mergoni et al, AJRCCM 1997; 156: 846 Ranieri et al, AJRCCM 1997; 156: 1082 Deflation limb may be more useful than inflation limb n n Harris et al, AJRCCM 2000; 161: 432 Hickling, AJRCCM 1998; 158: 194 No evidence, other than retrospective case reports
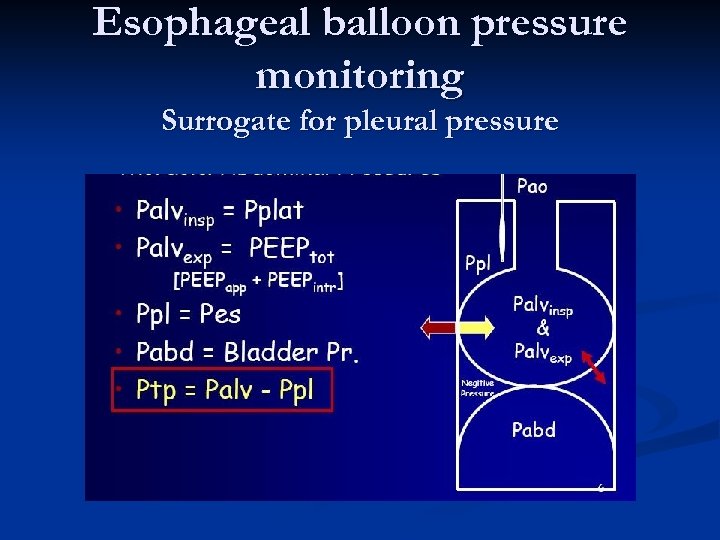 Esophageal balloon pressure monitoring Surrogate for pleural pressure
Esophageal balloon pressure monitoring Surrogate for pleural pressure
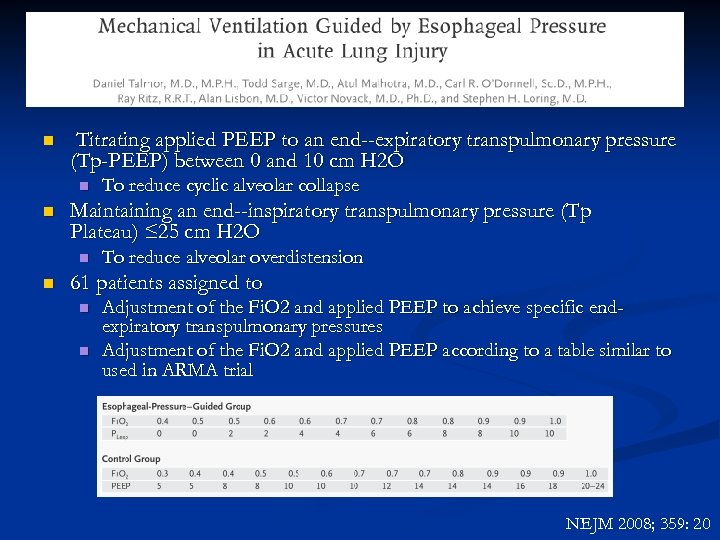 n Titrating applied PEEP to an end -expiratory transpulmonary pressure (Tp-PEEP) between 0 and 10 cm H 2 O n n Maintaining an end -inspiratory transpulmonary pressure (Tp Plateau) ≤ 25 cm H 2 O n n To reduce cyclic alveolar collapse To reduce alveolar overdistension 61 patients assigned to n n Adjustment of the Fi. O 2 and applied PEEP to achieve specific endexpiratory transpulmonary pressures Adjustment of the Fi. O 2 and applied PEEP according to a table similar to used in ARMA trial NEJM 2008; 359: 20
n Titrating applied PEEP to an end -expiratory transpulmonary pressure (Tp-PEEP) between 0 and 10 cm H 2 O n n Maintaining an end -inspiratory transpulmonary pressure (Tp Plateau) ≤ 25 cm H 2 O n n To reduce cyclic alveolar collapse To reduce alveolar overdistension 61 patients assigned to n n Adjustment of the Fi. O 2 and applied PEEP to achieve specific endexpiratory transpulmonary pressures Adjustment of the Fi. O 2 and applied PEEP according to a table similar to used in ARMA trial NEJM 2008; 359: 20
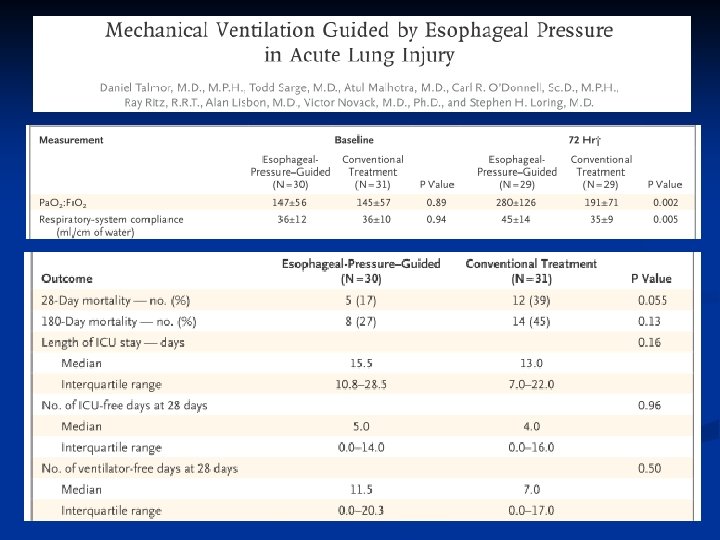
 Esophageal balloon pressure monitoring Limitations n Is it true representation of pleural pressure n n n Single trial to aim to look at only oxygenation n n Supine position Weight of mediastinum Heterogeneity of lung pathology Focal rather than global pleural pressure Malpositioning and changing positions. Using merely high PEEP has already shown similar results Approximately trans-pulmonary end-inspiratory pressure to 25 cm H 2 O n No evidence base.
Esophageal balloon pressure monitoring Limitations n Is it true representation of pleural pressure n n n Single trial to aim to look at only oxygenation n n Supine position Weight of mediastinum Heterogeneity of lung pathology Focal rather than global pleural pressure Malpositioning and changing positions. Using merely high PEEP has already shown similar results Approximately trans-pulmonary end-inspiratory pressure to 25 cm H 2 O n No evidence base.
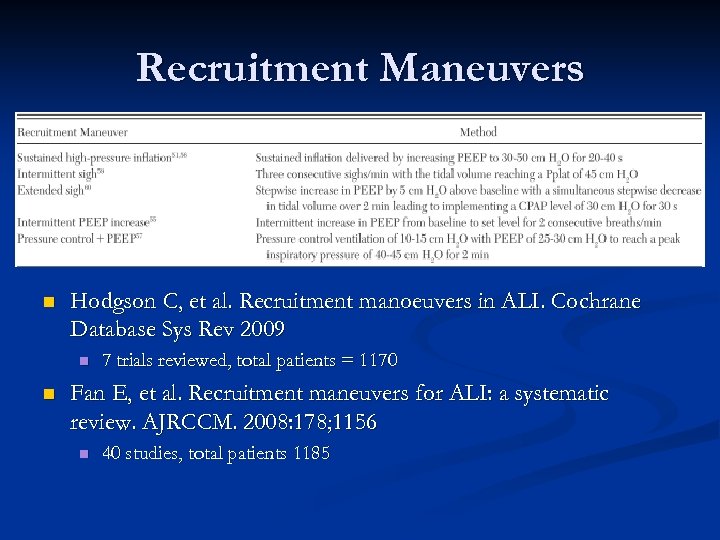 Recruitment Maneuvers n Hodgson C, et al. Recruitment manoeuvers in ALI. Cochrane Database Sys Rev 2009 n n 7 trials reviewed, total patients = 1170 Fan E, et al. Recruitment maneuvers for ALI: a systematic review. AJRCCM. 2008: 178; 1156 n 40 studies, total patients 1185
Recruitment Maneuvers n Hodgson C, et al. Recruitment manoeuvers in ALI. Cochrane Database Sys Rev 2009 n n 7 trials reviewed, total patients = 1170 Fan E, et al. Recruitment maneuvers for ALI: a systematic review. AJRCCM. 2008: 178; 1156 n 40 studies, total patients 1185
 Recruitment Maneuvers ~ Evidence based ~ n n n n n Did not differentiate between different RM strategies Improved oxygenation (did not persist) No change in ventilator parameter, except higher PEEP after RM No significant difference on 28 th day mortality No statistical difference in risk of barotrauma No significant changes in hemodynamic parameters after an RM. Hypotension (12%) and desaturation (9%) were the most common adverse events Only 1% patients had their RMs terminated prematurely due to adverse events. Current recommendation: to use after brief disconnection of patient from ventilator.
Recruitment Maneuvers ~ Evidence based ~ n n n n n Did not differentiate between different RM strategies Improved oxygenation (did not persist) No change in ventilator parameter, except higher PEEP after RM No significant difference on 28 th day mortality No statistical difference in risk of barotrauma No significant changes in hemodynamic parameters after an RM. Hypotension (12%) and desaturation (9%) were the most common adverse events Only 1% patients had their RMs terminated prematurely due to adverse events. Current recommendation: to use after brief disconnection of patient from ventilator.
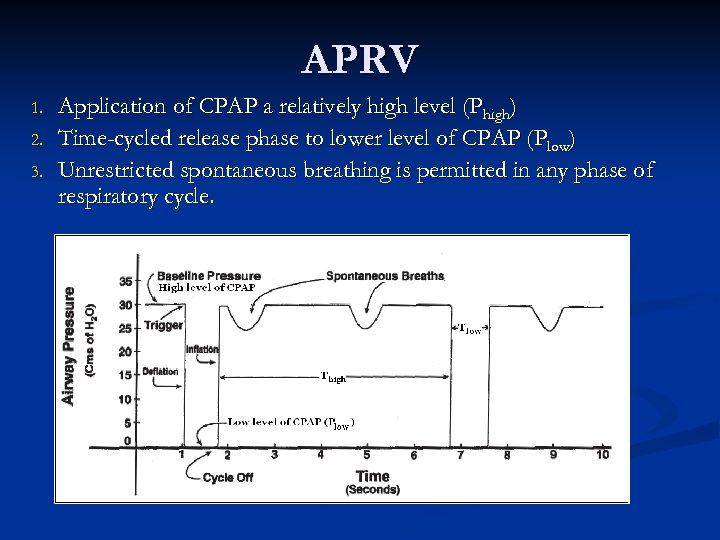 APRV 1. 2. 3. Application of CPAP a relatively high level (Phigh) Time-cycled release phase to lower level of CPAP (Plow) Unrestricted spontaneous breathing is permitted in any phase of respiratory cycle.
APRV 1. 2. 3. Application of CPAP a relatively high level (Phigh) Time-cycled release phase to lower level of CPAP (Plow) Unrestricted spontaneous breathing is permitted in any phase of respiratory cycle.
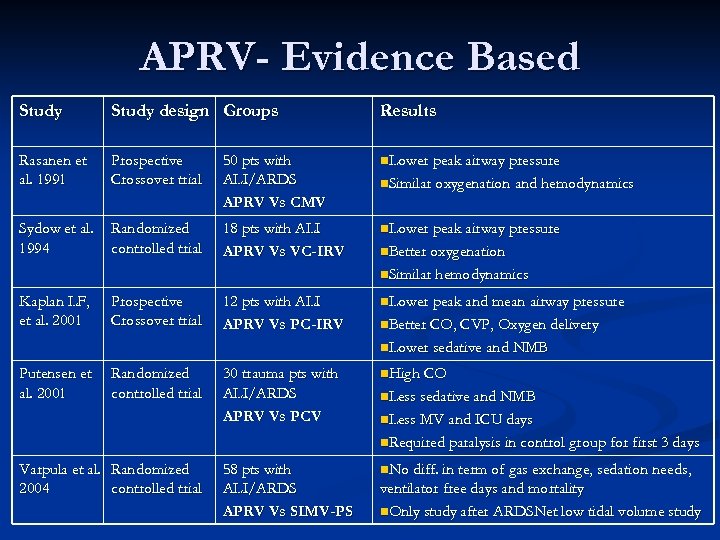 APRV- Evidence Based Study design Groups Results Rasanen et al. 1991 Prospective Crossover trial 50 pts with ALI/ARDS APRV Vs CMV n. Lower peak airway pressure Sydow et al. 1994 Randomized controlled trial 18 pts with ALI APRV Vs VC-IRV n. Lower peak airway pressure n. Similar oxygenation and hemodynamics n. Better oxygenation n. Similar hemodynamics Kaplan LF, et al. 2001 Prospective Crossover trial 12 pts with ALI APRV Vs PC-IRV n. Lower peak and mean airway pressure n. Better CO, CVP, Oxygen delivery n. Lower sedative and NMB Putensen et al. 2001 Randomized controlled trial 30 trauma pts with ALI/ARDS APRV Vs PCV n. High CO n. Less sedative and NMB n. Less MV and ICU days n. Required paralysis in control group for first 3 days Varpula et al. Randomized 2004 controlled trial 58 pts with ALI/ARDS APRV Vs SIMV-PS n. No diff. in term of gas exchange, sedation needs, ventilator free days and mortality n. Only study after ARDSNet low tidal volume study
APRV- Evidence Based Study design Groups Results Rasanen et al. 1991 Prospective Crossover trial 50 pts with ALI/ARDS APRV Vs CMV n. Lower peak airway pressure Sydow et al. 1994 Randomized controlled trial 18 pts with ALI APRV Vs VC-IRV n. Lower peak airway pressure n. Similar oxygenation and hemodynamics n. Better oxygenation n. Similar hemodynamics Kaplan LF, et al. 2001 Prospective Crossover trial 12 pts with ALI APRV Vs PC-IRV n. Lower peak and mean airway pressure n. Better CO, CVP, Oxygen delivery n. Lower sedative and NMB Putensen et al. 2001 Randomized controlled trial 30 trauma pts with ALI/ARDS APRV Vs PCV n. High CO n. Less sedative and NMB n. Less MV and ICU days n. Required paralysis in control group for first 3 days Varpula et al. Randomized 2004 controlled trial 58 pts with ALI/ARDS APRV Vs SIMV-PS n. No diff. in term of gas exchange, sedation needs, ventilator free days and mortality n. Only study after ARDSNet low tidal volume study
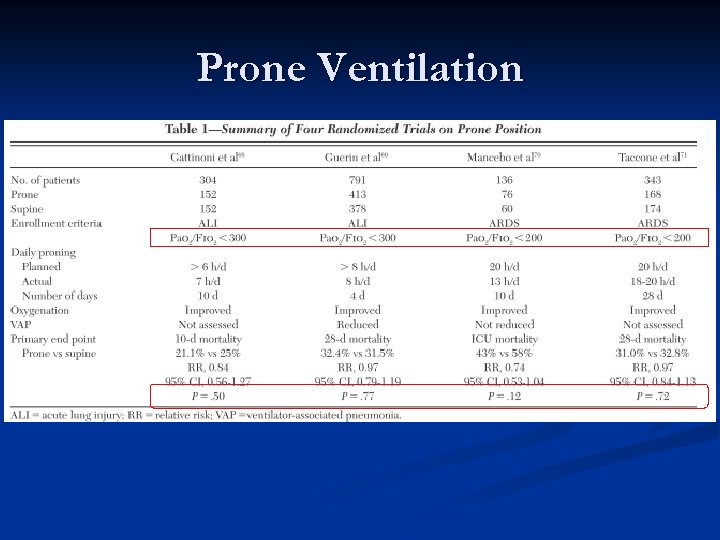 Prone Ventilation
Prone Ventilation
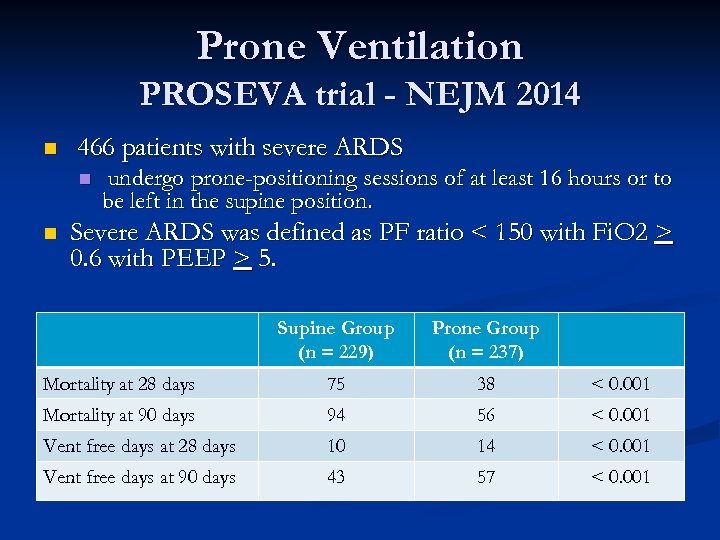 Prone Ventilation PROSEVA trial - NEJM 2014 n 466 patients with severe ARDS n n undergo prone-positioning sessions of at least 16 hours or to be left in the supine position. Severe ARDS was defined as PF ratio < 150 with Fi. O 2 > 0. 6 with PEEP > 5. Supine Group (n = 229) Prone Group (n = 237) Mortality at 28 days 75 38 < 0. 001 Mortality at 90 days 94 56 < 0. 001 Vent free days at 28 days 10 14 < 0. 001 Vent free days at 90 days 43 57 < 0. 001
Prone Ventilation PROSEVA trial - NEJM 2014 n 466 patients with severe ARDS n n undergo prone-positioning sessions of at least 16 hours or to be left in the supine position. Severe ARDS was defined as PF ratio < 150 with Fi. O 2 > 0. 6 with PEEP > 5. Supine Group (n = 229) Prone Group (n = 237) Mortality at 28 days 75 38 < 0. 001 Mortality at 90 days 94 56 < 0. 001 Vent free days at 28 days 10 14 < 0. 001 Vent free days at 90 days 43 57 < 0. 001
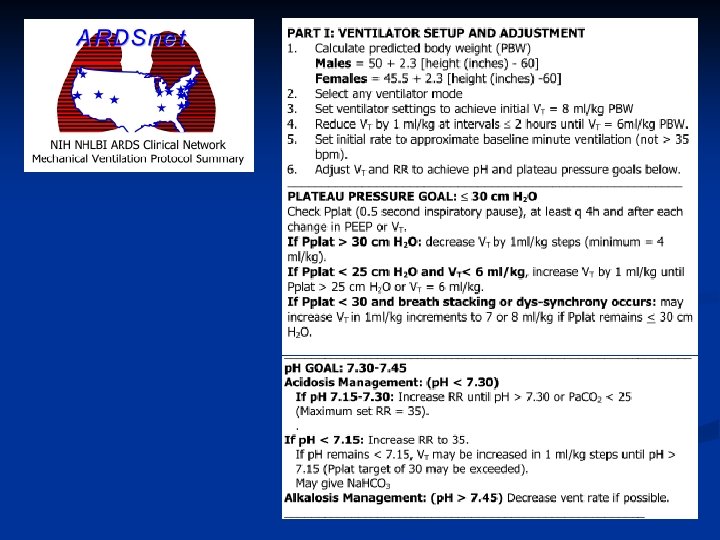
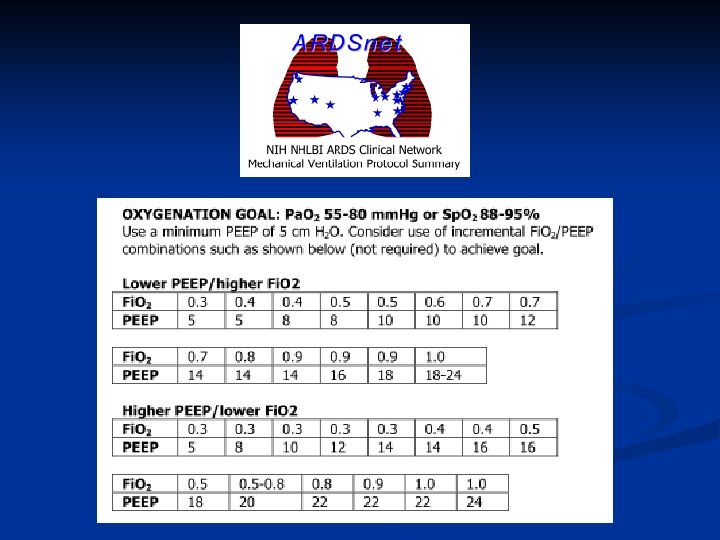
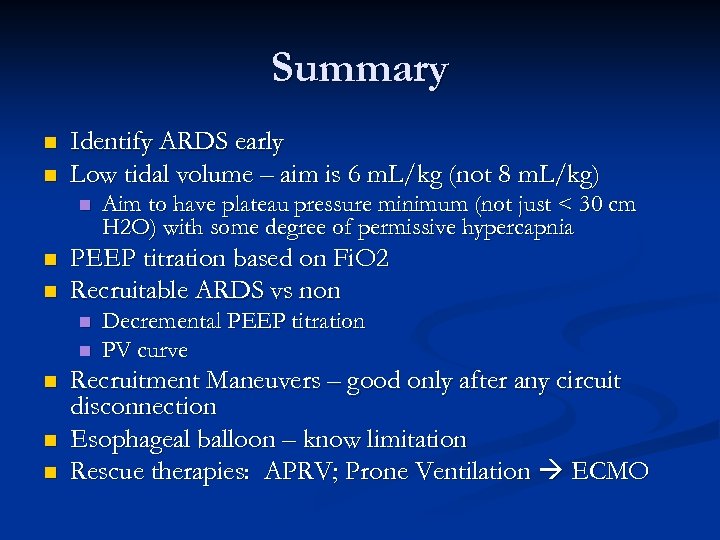 Summary n n Identify ARDS early Low tidal volume – aim is 6 m. L/kg (not 8 m. L/kg) n n n PEEP titration based on Fi. O 2 Recruitable ARDS vs non n n Aim to have plateau pressure minimum (not just < 30 cm H 2 O) with some degree of permissive hypercapnia Decremental PEEP titration PV curve Recruitment Maneuvers – good only after any circuit disconnection Esophageal balloon – know limitation Rescue therapies: APRV; Prone Ventilation ECMO
Summary n n Identify ARDS early Low tidal volume – aim is 6 m. L/kg (not 8 m. L/kg) n n n PEEP titration based on Fi. O 2 Recruitable ARDS vs non n n Aim to have plateau pressure minimum (not just < 30 cm H 2 O) with some degree of permissive hypercapnia Decremental PEEP titration PV curve Recruitment Maneuvers – good only after any circuit disconnection Esophageal balloon – know limitation Rescue therapies: APRV; Prone Ventilation ECMO
 Questions
Questions


