fa444e74b5b0ef6e1bc1b11895dada98.ppt
- Количество слайдов: 60
AR Systems, Inc Training Library Presents RAC ATTACK – A Guide to Successful Appeals “To Appeal or not to Appeal -A Strategic Decision” Instructor: Day Egusquiza, Pres AR Systems, Inc RAC 2011 1
RAC –The Recovery Audit Contractor: What’s a provider to do? Ø Ø Ø Ø Where are we today? – powerful updates Walking thru the process - defense /validation audits/moving forward Impact to departments –from letters to recoupment How will the recoupments work – automated vs complex Prevent the denial but know the Provider Options Tracking and trending 5 levels of appeal – decision points Balancing moving forward as well as looking back RAC 2011 2
Goal of the Audit Culture Ø To ensure billed services are reflected in the documentation in the record Ø To ensure billed services are in the medically correct setting for the pt’s condition Ø To ensure billed service reflect the ‘rules’ regarding billing for the specific service Ø To ensure documentation can support all billed services according to the payer rules. RAC 2011 3
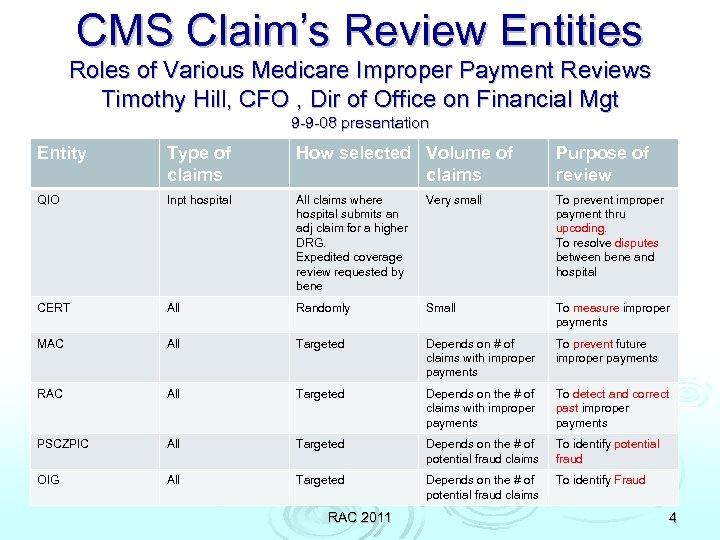
CMS Claim’s Review Entities Roles of Various Medicare Improper Payment Reviews Timothy Hill, CFO , Dir of Office on Financial Mgt 9 -9 -08 presentation Entity Type of claims How selected Volume of claims Purpose of review QIO Inpt hospital All claims where hospital submits an adj claim for a higher DRG. Expedited coverage review requested by bene Very small To prevent improper payment thru upcoding. To resolve disputes between bene and hospital CERT All Randomly Small To measure improper payments MAC All Targeted Depends on # of claims with improper payments To prevent future improper payments RAC All Targeted Depends on the # of claims with improper payments To detect and correct past improper payments PSCZPIC All Targeted Depends on the # of potential fraud claims To identify potential fraud OIG All Targeted Depends on the # of potential fraud claims To identify Fraud RAC 2011 4
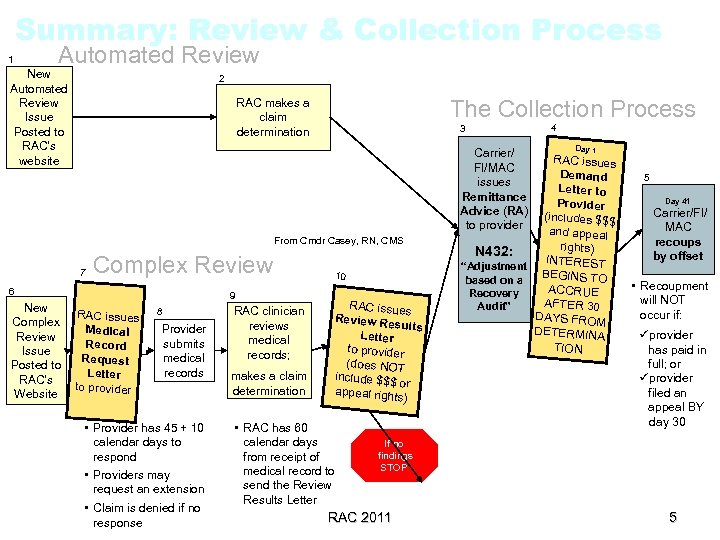
Summary: Review & Collection Process 1 Automated Review New Automated Review Issue Posted to RAC’s website 2 The Collection Process RAC makes a claim determination 3 Carrier/ FI/MAC issues Remittance Advice (RA) to provider From Cmdr Casey, RN, CMS 7 Complex Review 6 New Complex Review Issue Posted to RAC’s Website 9 RAC issues Medical Record Request Letter to provider 8 Provider submits medical records • Provider has 45 + 10 calendar days to respond • Providers may request an extension • Claim is denied if no response RAC clinician reviews medical records; makes a claim determination 10 RAC issues Review Re sults Letter to provider (does NOT include $$$ or appeal righ ts) • RAC has 60 calendar days from receipt of medical record to send the Review Results Letter 4 Day 1 RAC issues Demand Letter to Provider (includes $$$ and appeal rights) N 432: INTEREST “Adjustment BEGINS TO based on a ACCRUE Recovery AFTER 30 Audit” DAYS FROM DETERMINA TION 5 Day 41 Carrier/FI/ MAC recoups by offset • Recoupment will NOT occur if: üprovider has paid in full; or üprovider filed an appeal BY day 30 If no findings STOP RAC 2011 5 5
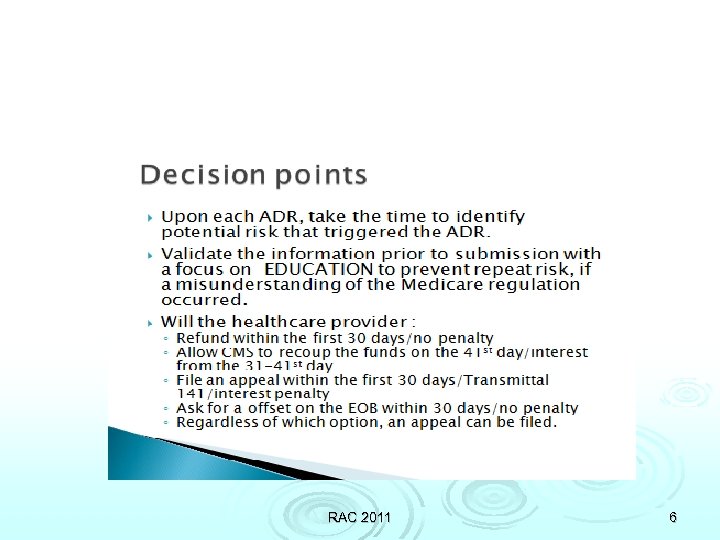
RAC 2011 6
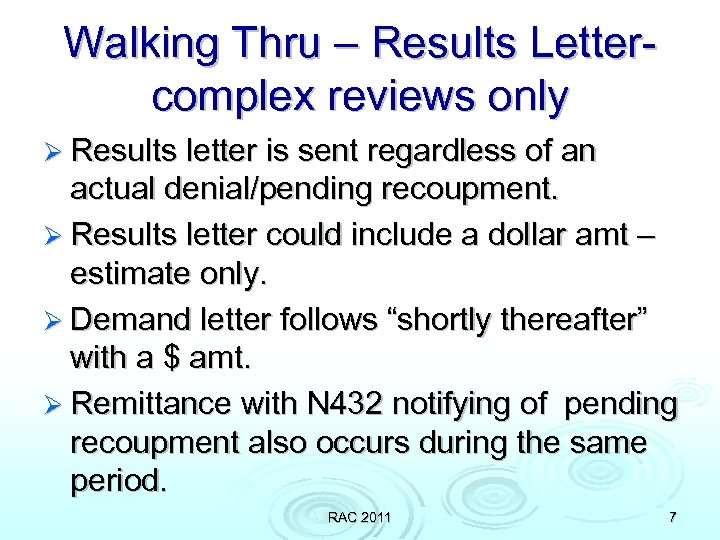
Walking Thru – Results Lettercomplex reviews only Ø Results letter is sent regardless of an actual denial/pending recoupment. Ø Results letter could include a dollar amt – estimate only. Ø Demand letter follows “shortly thereafter” with a $ amt. Ø Remittance with N 432 notifying of pending recoupment also occurs during the same period. RAC 2011 7
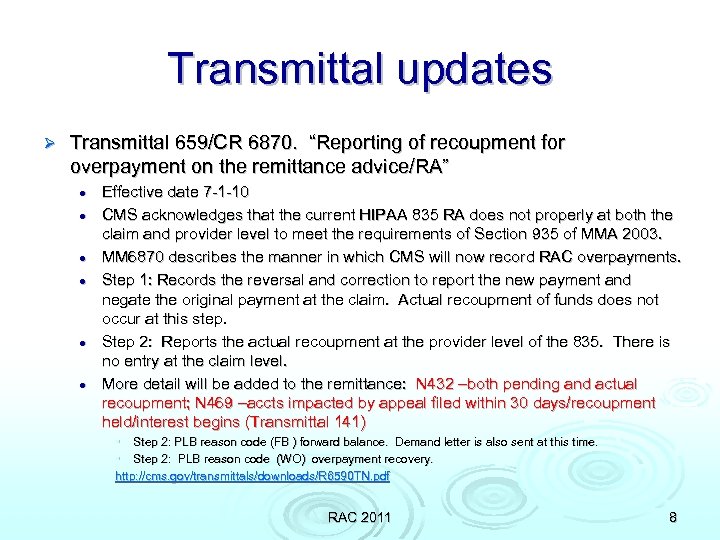
Transmittal updates Ø Transmittal 659/CR 6870. “Reporting of recoupment for overpayment on the remittance advice/RA” l l l Effective date 7 -1 -10 CMS acknowledges that the current HIPAA 835 RA does not properly at both the claim and provider level to meet the requirements of Section 935 of MMA 2003. MM 6870 describes the manner in which CMS will now record RAC overpayments. Step 1: Records the reversal and correction to report the new payment and negate the original payment at the claim. Actual recoupment of funds does not occur at this step. Step 2: Reports the actual recoupment at the provider level of the 835. There is no entry at the claim level. More detail will be added to the remittance: N 432 –both pending and actual recoupment; N 469 –accts impacted by appeal filed within 30 days/recoupment held/interest begins (Transmittal 141) • Step 2: PLB reason code (FB ) forward balance. Demand letter is also sent at this time. • Step 2: PLB reason code (WO) overpayment recovery. http: //cms. gov/transmittals/downloads/R 6590 TN. pdf RAC 2011 8
Sample DRG Results Letter 2010 RAC 2011 9
Pt specific results RAC 2011 10
Now you have the Demand RAC letter. . Ø Ø Ø Ø Review results of the initial validation review. Involve physician if necessary to assist in developing an appeal strategy. If no appeal is appropriate, flag the account for recoupment and monitor. Prepare a letter to send to the pt; watch for Medigap recoupment &/or refunds Determine rebilling potential for lesser services. Determine the value of using the informal 1 -40 day discussion period with the RAC. Determine to repay or request an Automatic Offset of amt to be recouped from the MAC within 30 days with no RAC 2011 11 interest.
Sample letter communication Dear pt Ø As part of ABC hospital’s commitment to compliance, we are continuously auditing to ensure accuracy and adherence to the Medicare regulations. Ø On (date), Medicare and ABC hospital had a dispute regarding your Ø ). (type of service Medicare has determined to take back the payment and therefore, we will be refunding your payment of $ (or indicate if the supplemental insurance will be refunded. ) Ø If you have any questions, please call our Medicare specialist, Susan Jones, at 1 -800 -happy hospital. We apologize for any confusion this may have caused. Ø Thank you for allowing ABC hospital to serve your health care needs. RAC 2010 12
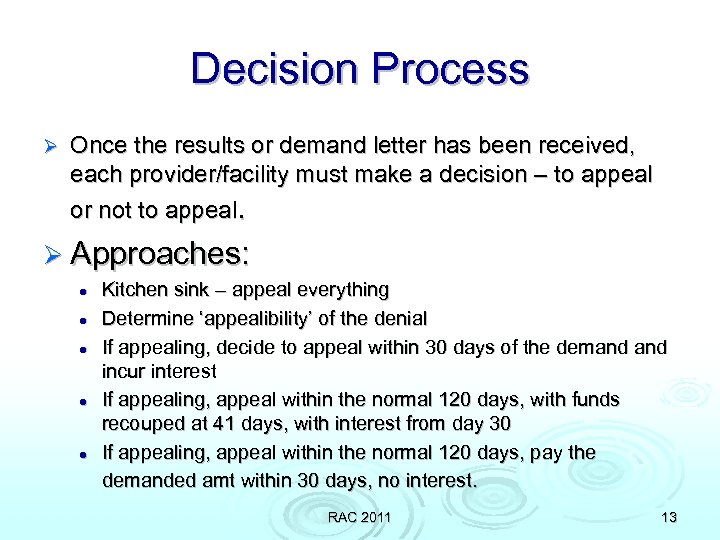
Decision Process Ø Once the results or demand letter has been received, each provider/facility must make a decision – to appeal or not to appeal. Ø Approaches: l l l Kitchen sink – appeal everything Determine ‘appealibility’ of the denial If appealing, decide to appeal within 30 days of the demand incur interest If appealing, appeal within the normal 120 days, with funds recouped at 41 days, with interest from day 30 If appealing, appeal within the normal 120 days, pay the demanded amt within 30 days, no interest. RAC 2011 13
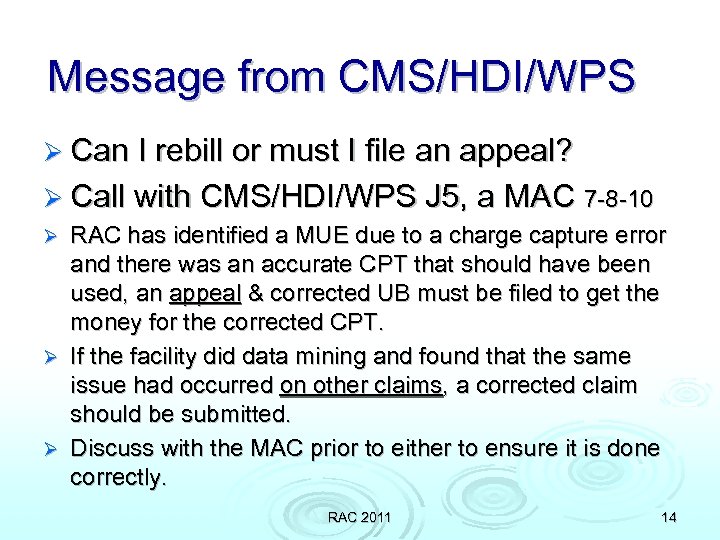
Message from CMS/HDI/WPS Ø Can I rebill or must I file an appeal? Ø Call with CMS/HDI/WPS J 5, a MAC 7 -8 -10 RAC has identified a MUE due to a charge capture error and there was an accurate CPT that should have been used, an appeal & corrected UB must be filed to get the money for the corrected CPT. Ø If the facility did data mining and found that the same issue had occurred on other claims, a corrected claim should be submitted. Ø Discuss with the MAC prior to either to ensure it is done correctly. Ø RAC 2011 14
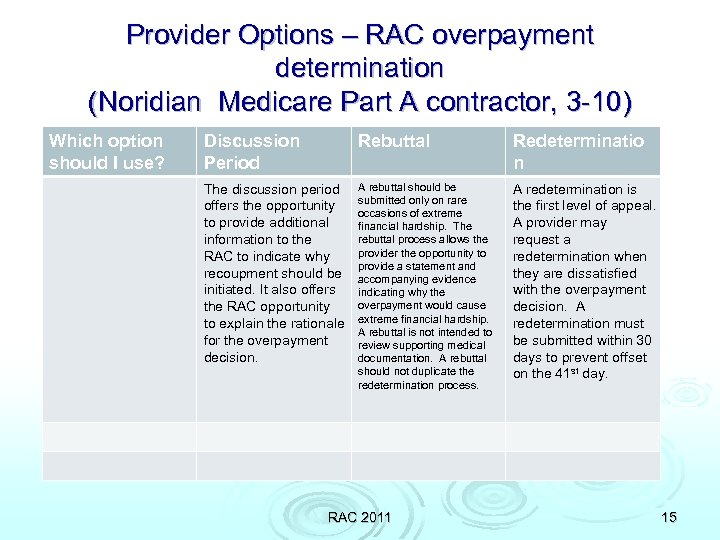
Provider Options – RAC overpayment determination (Noridian Medicare Part A contractor, 3 -10) Which option should I use? Discussion Period Rebuttal Redeterminatio n The discussion period offers the opportunity to provide additional information to the RAC to indicate why recoupment should be initiated. It also offers the RAC opportunity to explain the rationale for the overpayment decision. A rebuttal should be submitted only on rare occasions of extreme financial hardship. The rebuttal process allows the provider the opportunity to provide a statement and accompanying evidence indicating why the overpayment would cause extreme financial hardship. A rebuttal is not intended to review supporting medical documentation. A rebuttal should not duplicate the redetermination process. A redetermination is the first level of appeal. A provider may request a redetermination when they are dissatisfied with the overpayment decision. A redetermination must be submitted within 30 days to prevent offset on the 41 st day. RAC 2011 15
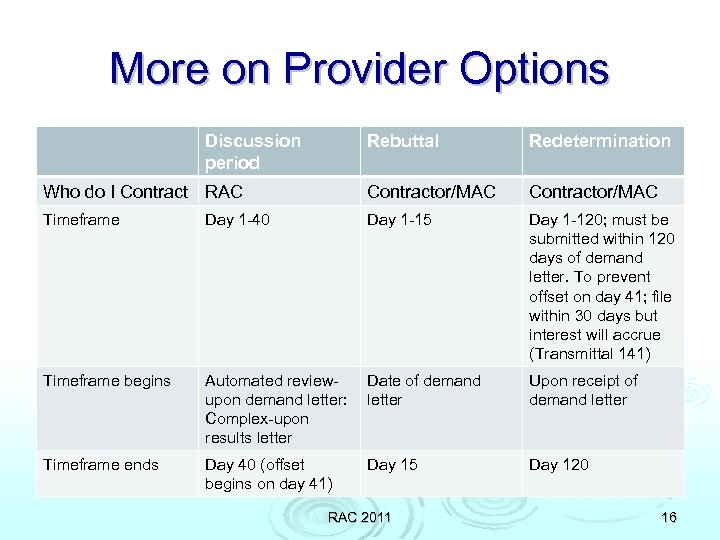
More on Provider Options Discussion period Rebuttal Redetermination Who do I Contract RAC Contractor/MAC Timeframe Day 1 -40 Day 1 -15 Day 1 -120; must be submitted within 120 days of demand letter. To prevent offset on day 41; file within 30 days but interest will accrue (Transmittal 141) Timeframe begins Automated reviewupon demand letter: Complex-upon results letter Date of demand letter Upon receipt of demand letter Timeframe ends Day 40 (offset begins on day 41) Day 15 Day 120 RAC 2011 16
New Appeal Transmittal Ø Transmittal 1762, CR 6377 Ø Ø Ø Ø July 2, 2009 www. cms. hhs. gov/transmittals/downloads/R 1762 CP. pdf Glossary of terms All appeals are on behalf of the beneficiary. “A provider or supplier may represent that beneficiary on the beneficiary’s behalf. No fee. CMS can assign liability to the pt if they ‘should have known’ noncoverage. Uncommon… “When an appellant requests a reconsideration with a QIC (level 2), the contractor (MAC/FI) must prepare and forward the case file to the QIC. “ Letter format for appeals Elements of each level of appeal RAC 2011 17
New Appeal Forms Ø Revision 12 -10 CMS has updated their Redetermination and Reconsideration Appeals forms. No change to ALJ form. http: //www. cms. gov/Org. Med. FFSAppeals/Downloads/CM S 20027 a. pdf Ø http: //www. cms. gov/Org. Med. FFSAppeals/Downloads/CM S 20033 a. pdf Ø Minor changes Ø RAC 2011 18
Understanding ‘interest’ NEW Transmittal 141, CR 6183, 9 -12 -08 “Limitation on Recoupment (935) “ Ø If the facility decides to appeal a RAC determination-understand the process: l l l If an appeal is filed within 30 days, the MAC/FI will not take back the funds. (Take back is immediate and will occur within 41 days of notice if no appeal. ) However, while the facility is going thru the numerous Medicare steps of appeal, interest will accrue on the amount that is being disputed. If the overpayment dispute is overturned at any level of the appeal process, the interest will be removed. If the overpayment dispute is not overturned, then the interest is left on the account. The overpayment take back will include the interest. There is an incentive to only appeal the determinations where there is a good reason to believe it will be overturned. “Punished’ for appealing all. (www. cms. hhs. gov/transmittals/downloads/R 141 FM. pdf) RAC 2011 19
Transmittal 141, CR 6183 Section 935/Medicare Modernization Act, 2003 “Limitation on Recoupment” Ø Overpayments that are subject to limitations on recoupment – appeals will suspend the recoupment. l l l Post-pay denials of claim under Part A and Part B MSP duplicate payment Both have demand letters Medicare will resume overpayment recoveries WITH INTEREST if the Medicare overpayment decision is upheld in the appeals process. www. cms. hhs. gov/transmittals/downloads/R 141 FM. pdf. MN 6183 is also available at this website. 9 -12 -08 RAC 2011 20
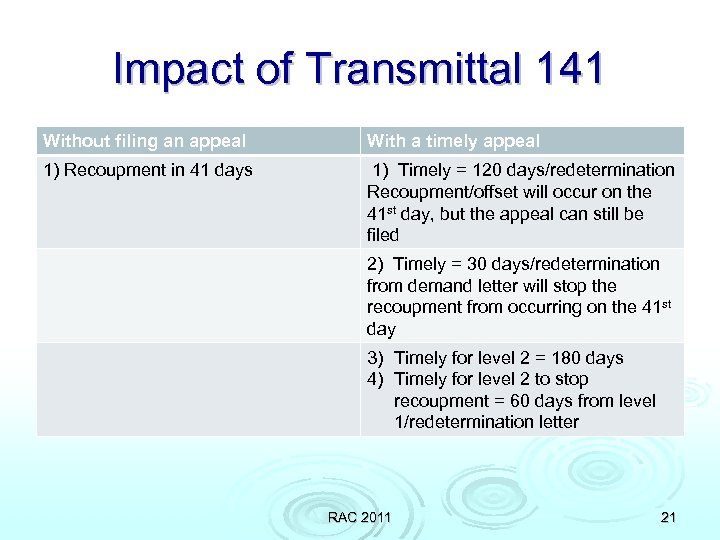
Impact of Transmittal 141 Without filing an appeal With a timely appeal 1) Recoupment in 41 days 1) Timely = 120 days/redetermination Recoupment/offset will occur on the 41 st day, but the appeal can still be filed 2) Timely = 30 days/redetermination from demand letter will stop the recoupment from occurring on the 41 st day 3) Timely for level 2 = 180 days 4) Timely for level 2 to stop recoupment = 60 days from level 1/redetermination letter RAC 2011 21
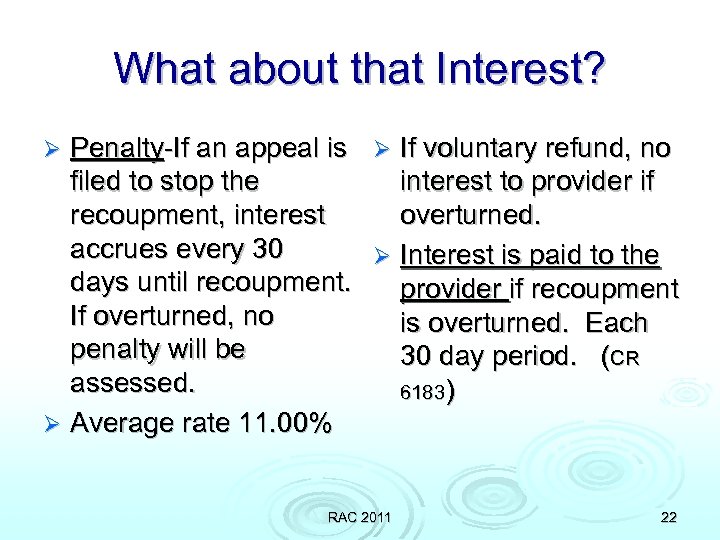
What about that Interest? Penalty-If an appeal is Ø If voluntary refund, no filed to stop the interest to provider if recoupment, interest overturned. accrues every 30 Ø Interest is paid to the days until recoupment. provider if recoupment If overturned, no is overturned. Each penalty will be 30 day period. (CR assessed. 6183) Ø Average rate 11. 00% Ø RAC 2011 22

RAC Appeal Process – Mirrors regular Medicare appeal levels with minor exceptions RAC 2011 23
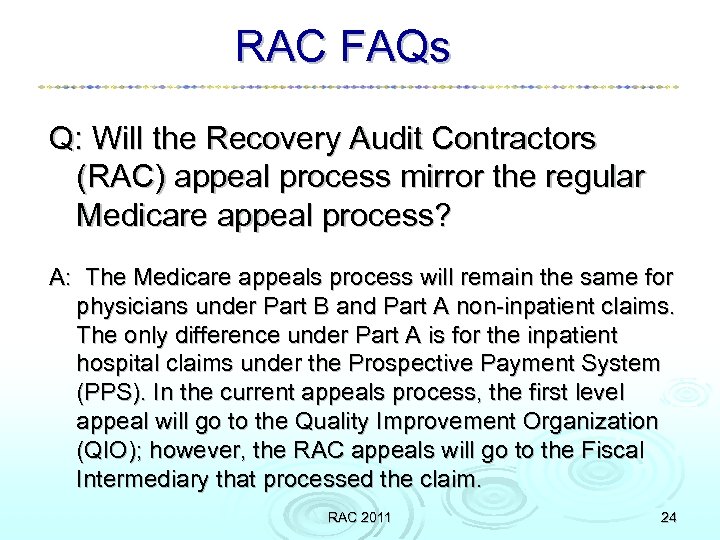
RAC FAQs Q: Will the Recovery Audit Contractors (RAC) appeal process mirror the regular Medicare appeal process? A: The Medicare appeals process will remain the same for physicians under Part B and Part A non-inpatient claims. The only difference under Part A is for the inpatient hospital claims under the Prospective Payment System (PPS). In the current appeals process, the first level appeal will go to the Quality Improvement Organization (QIO); however, the RAC appeals will go to the Fiscal Intermediary that processed the claim. RAC 2011 24
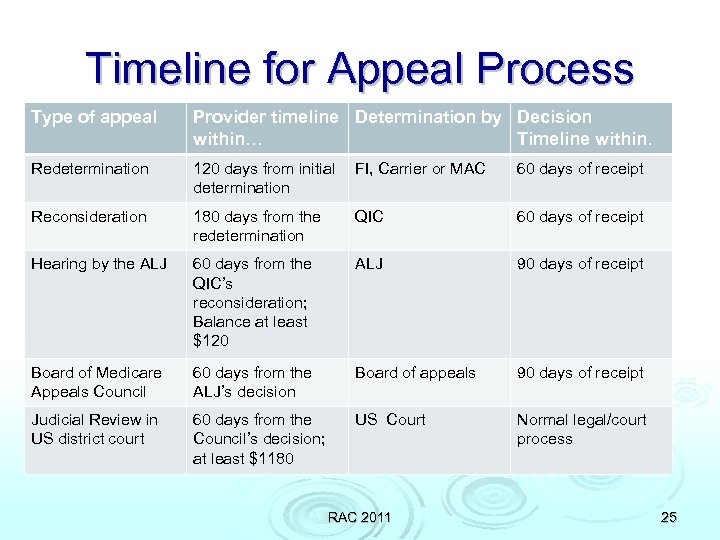
Timeline for Appeal Process Type of appeal Provider timeline Determination by Decision within… Timeline within. Redetermination 120 days from initial determination FI, Carrier or MAC 60 days of receipt Reconsideration 180 days from the redetermination QIC 60 days of receipt Hearing by the ALJ 60 days from the QIC’s reconsideration; Balance at least $120 ALJ 90 days of receipt Board of Medicare Appeals Council 60 days from the ALJ’s decision Board of appeals 90 days of receipt Judicial Review in US district court 60 days from the Council’s decision; at least $1180 US Court Normal legal/court process RAC 2011 25
RAC 2011 26
RAC 2011 27
RAC 2011 28
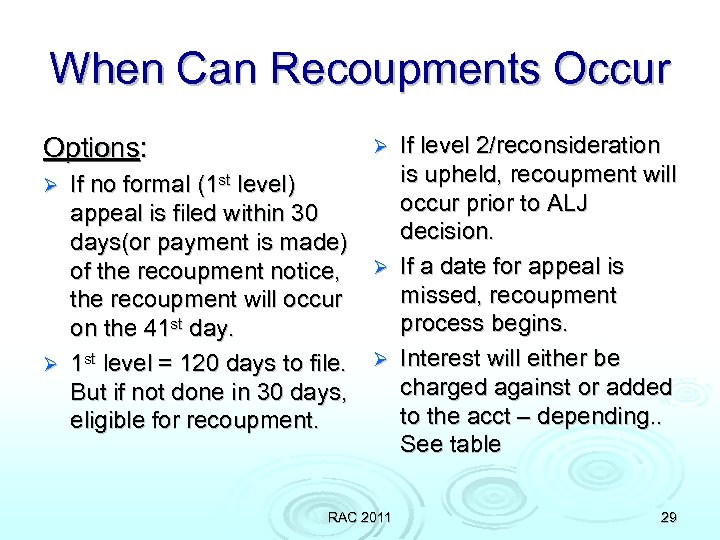
When Can Recoupments Occur Options: If no formal (1 st level) appeal is filed within 30 days(or payment is made) of the recoupment notice, the recoupment will occur on the 41 st day. Ø 1 st level = 120 days to file. But if not done in 30 days, eligible for recoupment. Ø If level 2/reconsideration is upheld, recoupment will occur prior to ALJ decision. Ø If a date for appeal is missed, recoupment process begins. Ø Interest will either be charged against or added to the acct – depending. . See table Ø RAC 2011 29
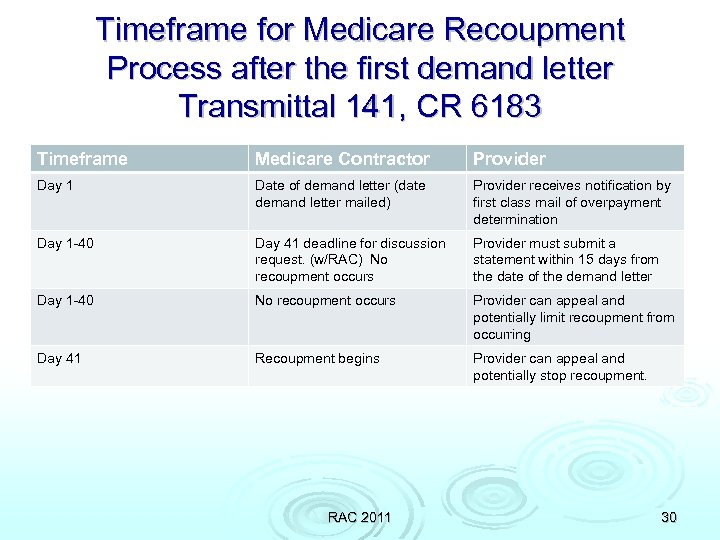
Timeframe for Medicare Recoupment Process after the first demand letter Transmittal 141, CR 6183 Timeframe Medicare Contractor Provider Day 1 Date of demand letter (date demand letter mailed) Provider receives notification by first class mail of overpayment determination Day 1 -40 Day 41 deadline for discussion request. (w/RAC) No recoupment occurs Provider must submit a statement within 15 days from the date of the demand letter Day 1 -40 No recoupment occurs Provider can appeal and potentially limit recoupment from occurring Day 41 Recoupment begins Provider can appeal and potentially stop recoupment. RAC 2011 30
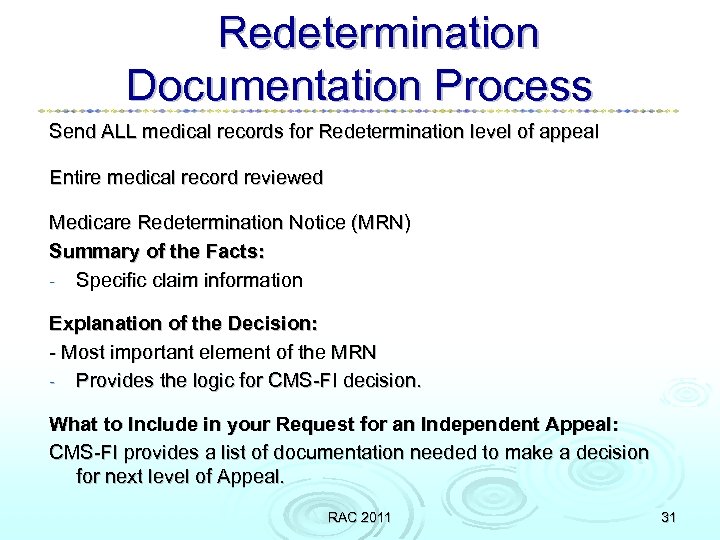
Redetermination Documentation Process Send ALL medical records for Redetermination level of appeal Entire medical record reviewed Medicare Redetermination Notice (MRN) Summary of the Facts: - Specific claim information Explanation of the Decision: - Most important element of the MRN - Provides the logic for CMS-FI decision. What to Include in your Request for an Independent Appeal: CMS-FI provides a list of documentation needed to make a decision for next level of Appeal. RAC 2011 31
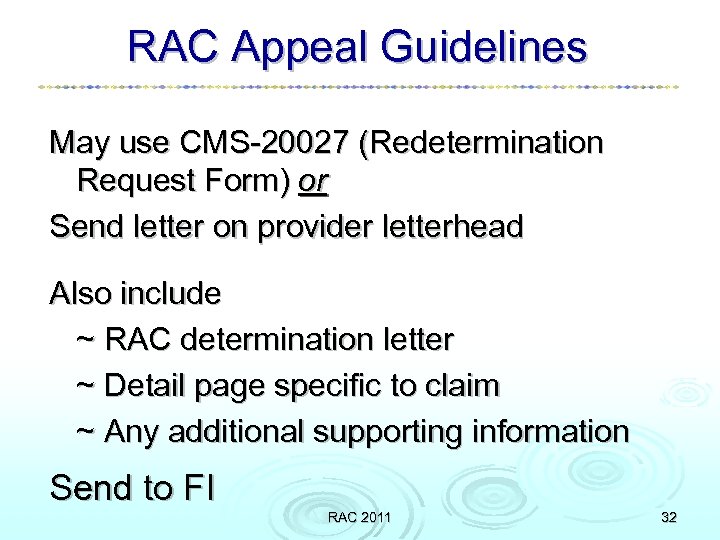
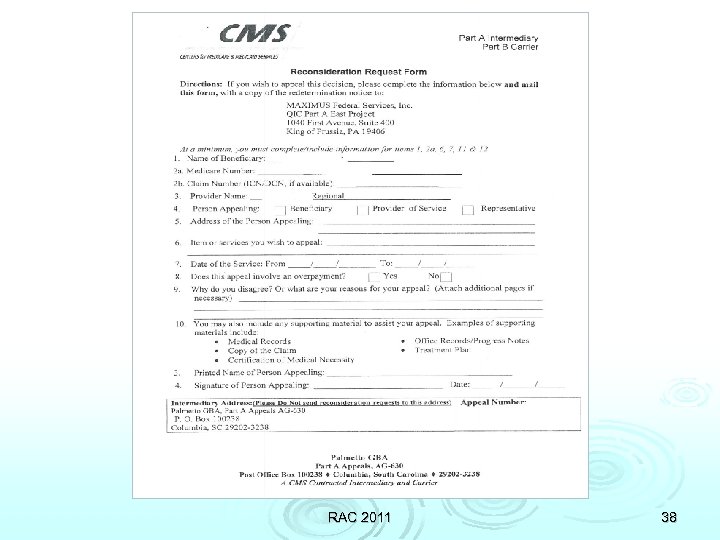
RAC Appeal Guidelines May use CMS-20027 (Redetermination Request Form) or Send letter on provider letterhead Also include ~ RAC determination letter ~ Detail page specific to claim ~ Any additional supporting information Send to FI RAC 2011 32
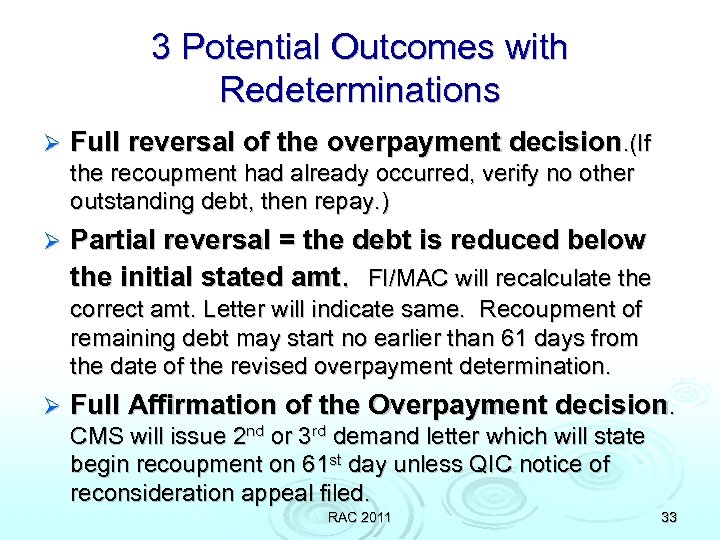
3 Potential Outcomes with Redeterminations Ø Full reversal of the overpayment decision. (If the recoupment had already occurred, verify no other outstanding debt, then repay. ) Ø Partial reversal = the debt is reduced below the initial stated amt. FI/MAC will recalculate the correct amt. Letter will indicate same. Recoupment of remaining debt may start no earlier than 61 days from the date of the revised overpayment determination. Ø Full Affirmation of the Overpayment decision. CMS will issue 2 nd or 3 rd demand letter which will state begin recoupment on 61 st day unless QIC notice of reconsideration appeal filed. RAC 2011 33
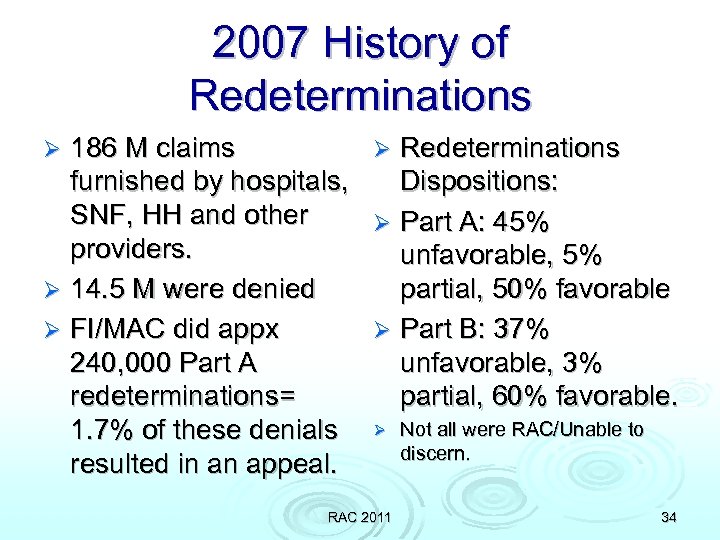
2007 History of Redeterminations 186 M claims Ø Redeterminations furnished by hospitals, Dispositions: SNF, HH and other Ø Part A: 45% providers. unfavorable, 5% Ø 14. 5 M were denied partial, 50% favorable Ø FI/MAC did appx Ø Part B: 37% 240, 000 Part A unfavorable, 3% redeterminations= partial, 60% favorable. 1. 7% of these denials Ø Not all were RAC/Unable to discern. resulted in an appeal. Ø RAC 2011 34
RAC 2011 35
RAC 2011 36
RAC 2011 37
RAC 2011 38
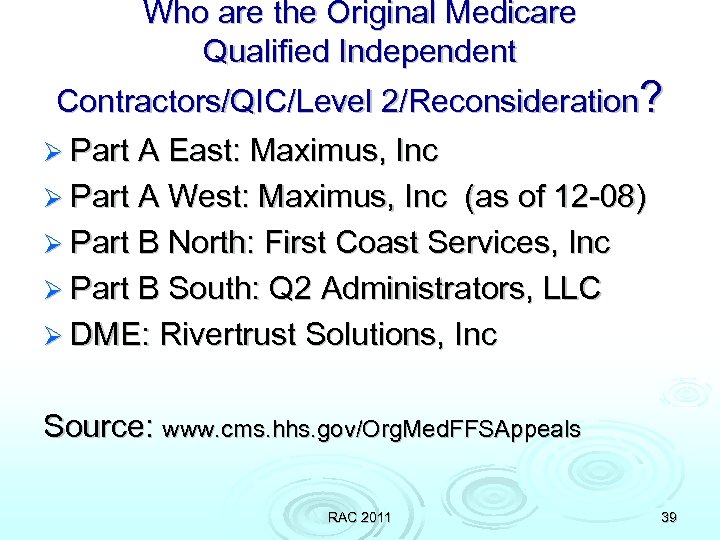
Who are the Original Medicare Qualified Independent Contractors/QIC/Level 2/Reconsideration? Ø Part A East: Maximus, Inc Ø Part A West: Maximus, Inc (as of 12 -08) Ø Part B North: First Coast Services, Inc Ø Part B South: Q 2 Administrators, LLC Ø DME: Rivertrust Solutions, Inc Source: www. cms. hhs. gov/Org. Med. FFSAppeals RAC 2011 39
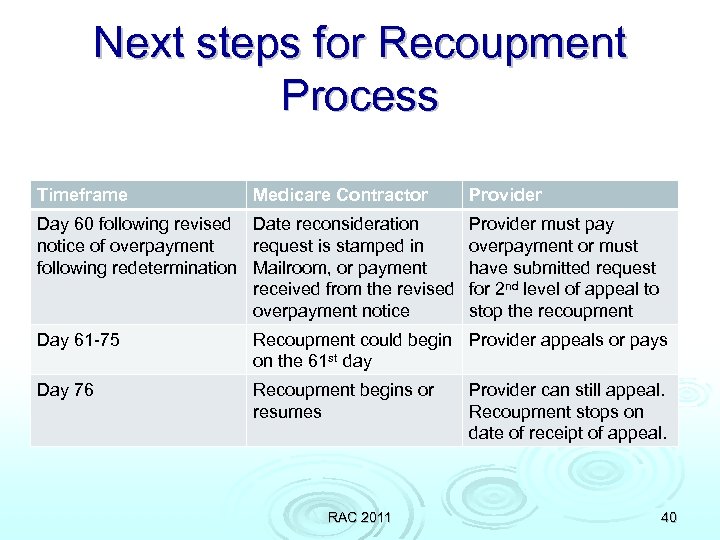
Next steps for Recoupment Process Timeframe Medicare Contractor Day 60 following revised Date reconsideration notice of overpayment request is stamped in following redetermination Mailroom, or payment received from the revised overpayment notice Provider must pay overpayment or must have submitted request for 2 nd level of appeal to stop the recoupment Day 61 -75 Recoupment could begin Provider appeals or pays on the 61 st day Day 76 Recoupment begins or resumes RAC 2011 Provider can still appeal. Recoupment stops on date of receipt of appeal. 40
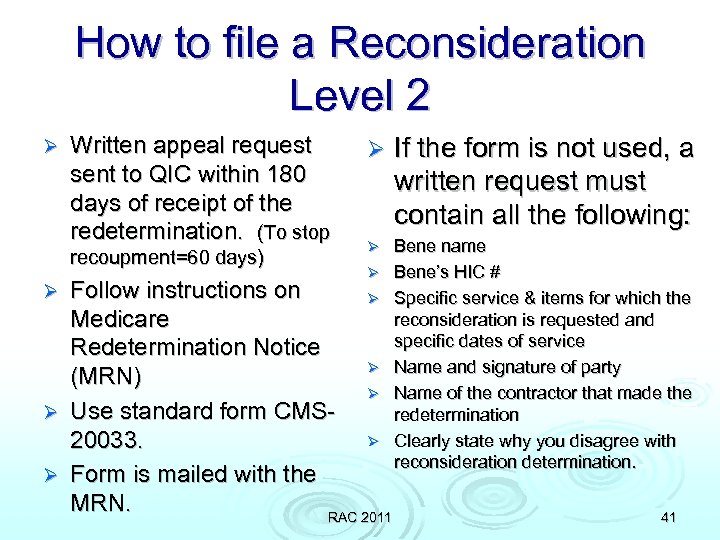
How to file a Reconsideration Level 2 Ø Written appeal request sent to QIC within 180 days of receipt of the redetermination. (To stop recoupment=60 days) Ø If the form is not used, a written request must contain all the following: Ø Bene name Bene’s HIC # Specific service & items for which the reconsideration is requested and specific dates of service Name and signature of party Name of the contractor that made the redetermination Clearly state why you disagree with reconsideration determination. Ø Follow instructions on Ø Medicare Redetermination Notice Ø (MRN) Ø Ø Use standard form CMSØ 20033. Ø Form is mailed with the MRN. RAC 2011 Ø 41
3 Potential Outcomes with Reconsiderations Full reversal – same as redeterminations Ø Partial reversal – this reduces the overpayment. QIC issue a revised demand letter or make appropriate payments if due of an underpayment amt. Recoupment will begin on the 30 th day from the date of the notice of the revised payment. Ø Affirmation – recoupment may resume on the 30 th calendar after the date of the notice of the reconsideration. Ø RAC 2011 42
2007 Reconsideration History QIC (Qualified Independent Contractors) processed appox 400, 000 appeals in 2007. Ø DME is separate. Ø Not all were RAC/unable to discern. Ø Reconsideration Dispositions: Ø Part A: 79% unfavorable, 3% partial, 18% favorable. Ø Part B: 64% unfavorable, 5% partial, 31% favorable. Ø RAC 2011 43
And then there was ALJ/Administrative Law Judge Medicare contractors can initiate (or resume) recoupment immediately upon receipt of the QIC’s decision or dismissal notice regardless of subsequent appeal to the ALJ (3 rd level of appeal) and all further appeals. Ø If the ALJ level process reverses the Medicare overpayment determination, Medicare will refund both principal and interest collected + pay interest on any recouped funds that may kept from ongoing Medicare payments. Ø If other outstanding debts, interest is applied against those first before payment to the provider is made. Ø Ø Can add up same issue items and fill jointly. RAC 2011 44
Contingency Fee Rules Ø RAC must payback the contingency fee if the claim was overturned at… l l Demonstration RAC Permanent RAC 2011 first level of appeal any level of appeal 45
Can the False Claims Act Apply? Ø If the RACs find ‘reckless disregard for the law’, referrals can be made to the appropriate agency –starting with the MAC/FI. Ø The MAC/FI can investigate further and refer for further investigation. Ø And the story continues. Ø NO HEAD IN THE SAND!! RAC 2011 46
RAC ATTACK Rollout Create tracking and trending tool. Ø Track all requests – look for patterns as to why the request was sent. Ø Track all recoupments with reasons. Implement physician & nursing documentation training; CDM changes; Dept head ed on charge capture/billable services; coding ed, continued inhouse defense auditing. Ø Determine best practices for TNT. . Ø Develop corrective action w/immediate implementation. This is not optional! Ø RAC 2011 47
Tools for Success Look at a tracking tool Ø Continue to learn from other states as the roll out to 2010 is completed. Ø Watch for ongoing education from CMS Ø Look for trends identified from auditing and data mining. Ø Internally audit, train – audit, train some more Ø Explore creation of a RAC Specialist-the most detailed person in the revenue cycle! Ø RAC 2011 48
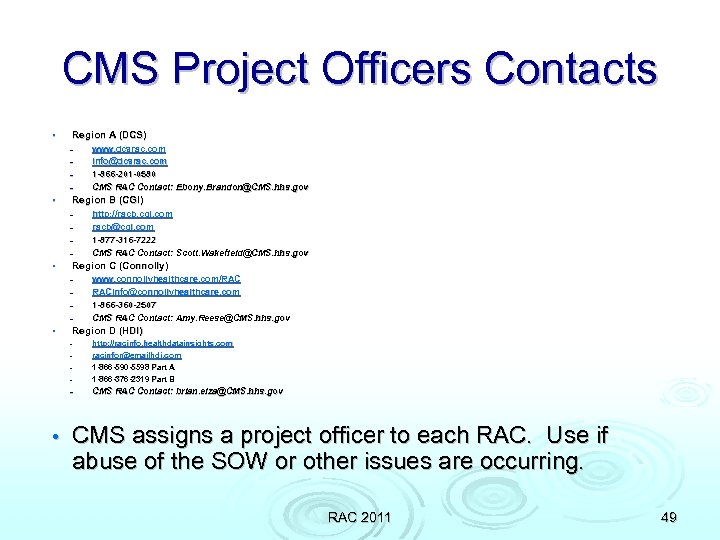
CMS Project Officers Contacts • Region A (DCS) – – • Region B (CGI) – – • http: //racb. cgi. com racb@cgi. com 1 -877 -316 -7222 CMS RAC Contact: Scott. Wakefield@CMS. hhs. gov Region C (Connolly) – – • www. dcsrac. com info@dcsrac. com 1 -866 -201 -0580 CMS RAC Contact: Ebony. Brandon@CMS. hhs. gov www. connollyhealthcare. com/RAC RACinfo@connollyhealthcare. com 1 -866 -360 -2507 CMS RAC Contact: Amy. Reese@CMS. hhs. gov Region D (HDI) – http: //racinfo. healthdatainsights. com racinfor@emailhdi. com 1 -866 -590 -5598 Part A 1 -866 -376 -2319 Part B – CMS RAC Contact: brian. elza@CMS. hhs. gov – – – • CMS assigns a project officer to each RAC. Use if abuse of the SOW or other issues are occurring. RAC 2011 49
ls of Leve 5 g the arizin umm S ppeal A RAC 2011 50
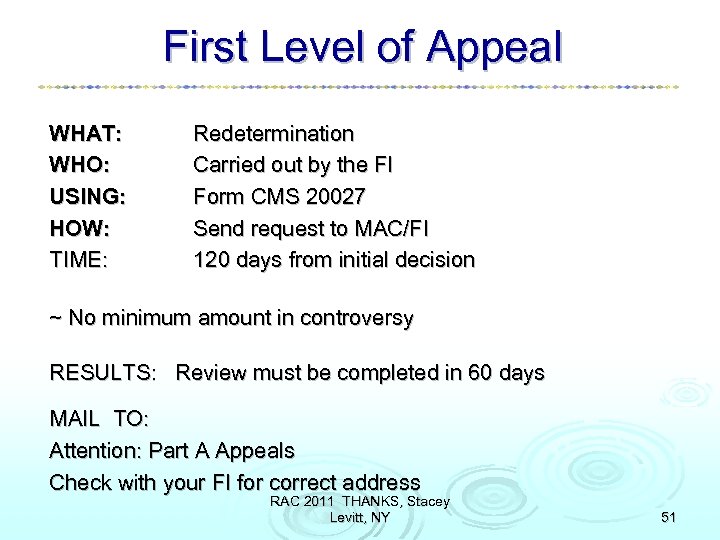
First Level of Appeal WHAT: WHO: USING: HOW: TIME: Redetermination Carried out by the FI Form CMS 20027 Send request to MAC/FI 120 days from initial decision ~ No minimum amount in controversy RESULTS: Review must be completed in 60 days MAIL TO: Attention: Part A Appeals Check with your FI for correct address RAC 2011 THANKS, Stacey Levitt, NY 51
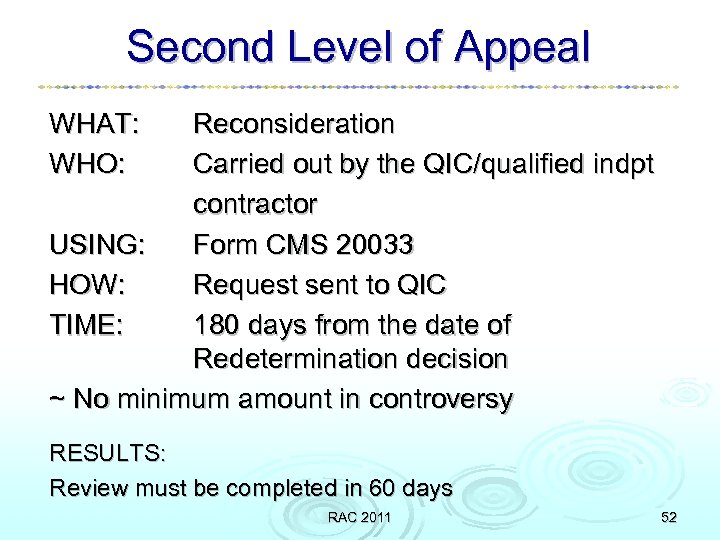
Second Level of Appeal WHAT: WHO: Reconsideration Carried out by the QIC/qualified indpt contractor USING: Form CMS 20033 HOW: Request sent to QIC TIME: 180 days from the date of Redetermination decision ~ No minimum amount in controversy RESULTS: Review must be completed in 60 days RAC 2011 52
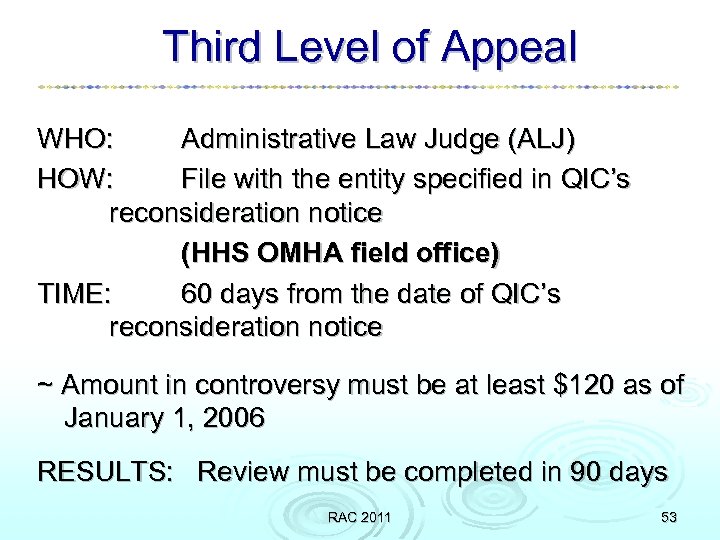
Third Level of Appeal WHO: Administrative Law Judge (ALJ) HOW: File with the entity specified in QIC’s reconsideration notice (HHS OMHA field office) TIME: 60 days from the date of QIC’s reconsideration notice ~ Amount in controversy must be at least $120 as of January 1, 2006 RESULTS: Review must be completed in 90 days RAC 2011 53
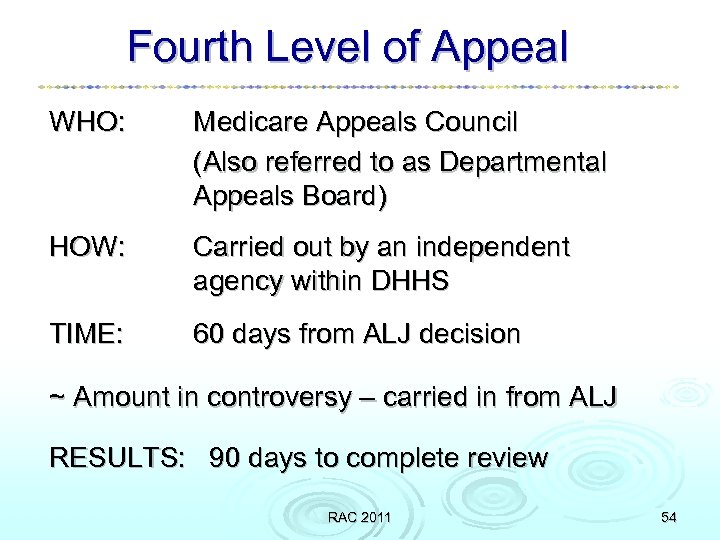
Fourth Level of Appeal WHO: Medicare Appeals Council (Also referred to as Departmental Appeals Board) HOW: Carried out by an independent agency within DHHS TIME: 60 days from ALJ decision ~ Amount in controversy – carried in from ALJ RESULTS: 90 days to complete review RAC 2011 54
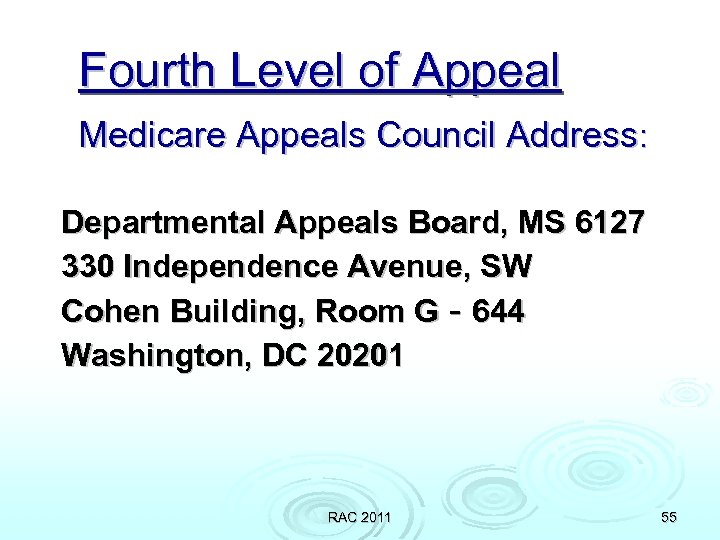
Fourth Level of Appeal Medicare Appeals Council Address: Departmental Appeals Board, MS 6127 330 Independence Avenue, SW Cohen Building, Room G‐ 644 Washington, DC 20201 RAC 2011 55
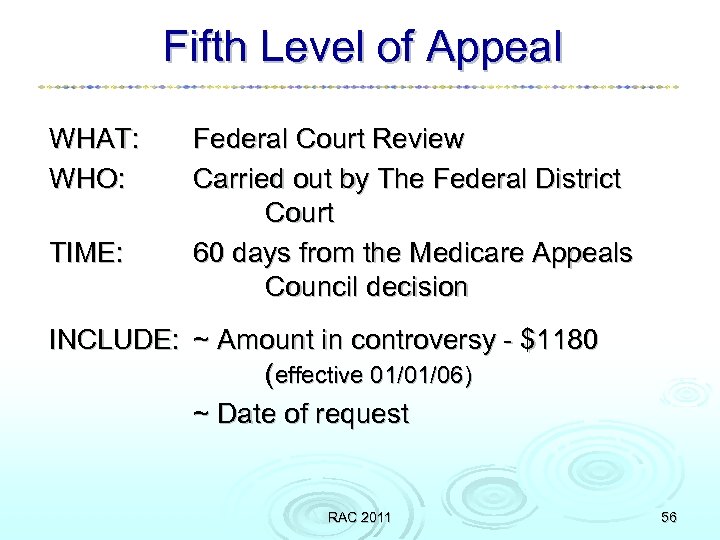
Fifth Level of Appeal WHAT: WHO: TIME: Federal Court Review Carried out by The Federal District Court 60 days from the Medicare Appeals Council decision INCLUDE: ~ Amount in controversy - $1180 (effective 01/01/06) ~ Date of request RAC 2011 56
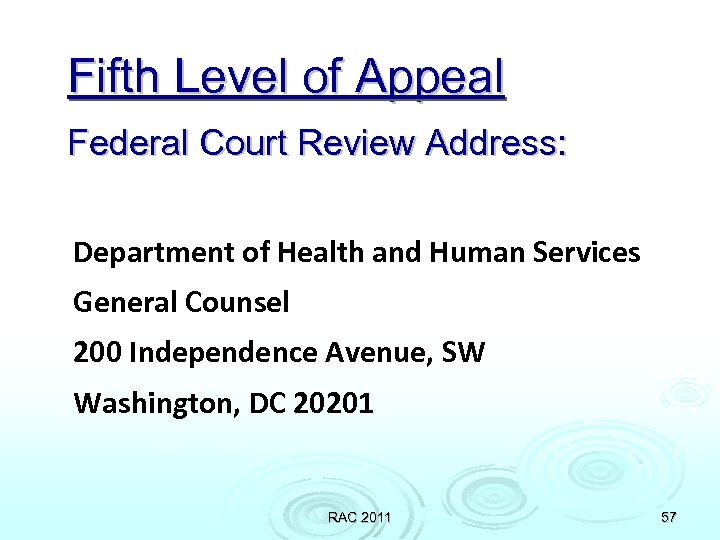
Fifth Level of Appeal Federal Court Review Address: Department of Health and Human Services General Counsel 200 Independence Avenue, SW Washington, DC 20201 RAC 2011 57
References: Appeals information Appeals: Administration Law Judge; Departmental Appeals Board; U. S. District Court Review Changes to chapter 29 – Appeals of claims decisions –revised Appeals of RAC decisions – MNU 2006‐ 02 Appeals of ALJ, Departmental Appeals Board, and U. S. District Court Review – CR 4152 Slide Material Culled from: 1) 06/2007 Medicare Appeals Process Provider Outreach & Education 2) CMS 03/07/2006_Appeals_Session_Materials RAC 2011 58
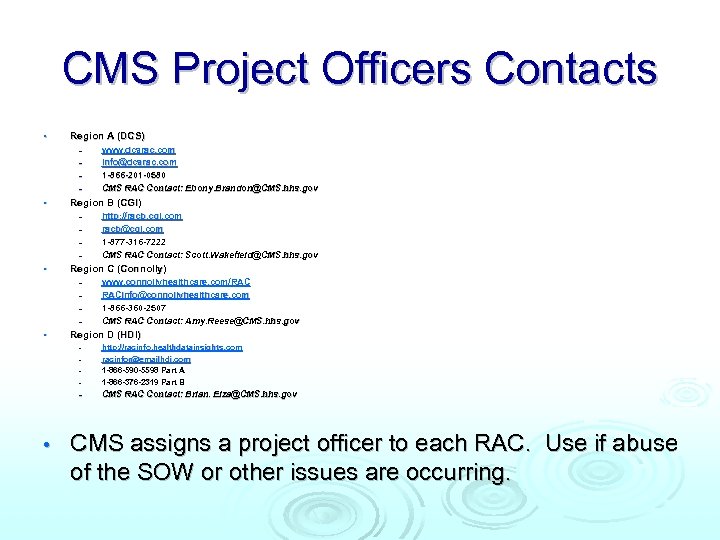
CMS Project Officers Contacts • Region A (DCS) – – • Region B (CGI) – – • http: //racb. cgi. com racb@cgi. com 1 -877 -316 -7222 CMS RAC Contact: Scott. Wakefield@CMS. hhs. gov Region C (Connolly) – – • www. dcsrac. com info@dcsrac. com 1 -866 -201 -0580 CMS RAC Contact: Ebony. Brandon@CMS. hhs. gov www. connollyhealthcare. com/RAC RACinfo@connollyhealthcare. com 1 -866 -360 -2507 CMS RAC Contact: Amy. Reese@CMS. hhs. gov Region D (HDI) – http: //racinfo. healthdatainsights. com racinfor@emailhdi. com 1 -866 -590 -5598 Part A 1 -866 -376 -2319 Part B – CMS RAC Contact: Brian. Elza@CMS. hhs. gov – – – • CMS assigns a project officer to each RAC. Use if abuse of the SOW or other issues are occurring.
AR Systems’ Contact Info Day Egusquiza, President AR Systems, Inc Box 2521 Twin Falls, Id 83303 208 423 9036 daylee 1@mindspring. com Thanks for joining us! See all our training opportunities + Boot Camps at www. healthcare-seminar. com RAC 2011 60
fa444e74b5b0ef6e1bc1b11895dada98.ppt