Diabetic Foot Syndrome 2.pptx
- Количество слайдов: 66
APPROACH to DIABETIC FOOT Dr. Faiez Alhmoud Surgery Dpt. Albashir Hospital (MOH)
Diabetic Foot (DF) It will be unwise if we restrict the term (DF) to foot infection, ulcer or gangrene in a diabetic patient n Why? n n n (advanced stage of the disease) n
Diabetic foot definition n Diabetic foot is a disease complex that can develop in the skin, muscles, or bones of the foot as a result of the nerve damage, poor circulation and/or infection that is associated with diabetes. n The Diabetic Foot may be defined as a syndrome in which neuropathy, angiopathy, and infection will lead to tissue breakdown resulting in morbidity and possible amputation ( WHO 1995 ) n Any foot pathology that result from diabetes or it’s long – term results (Boulton 2002)
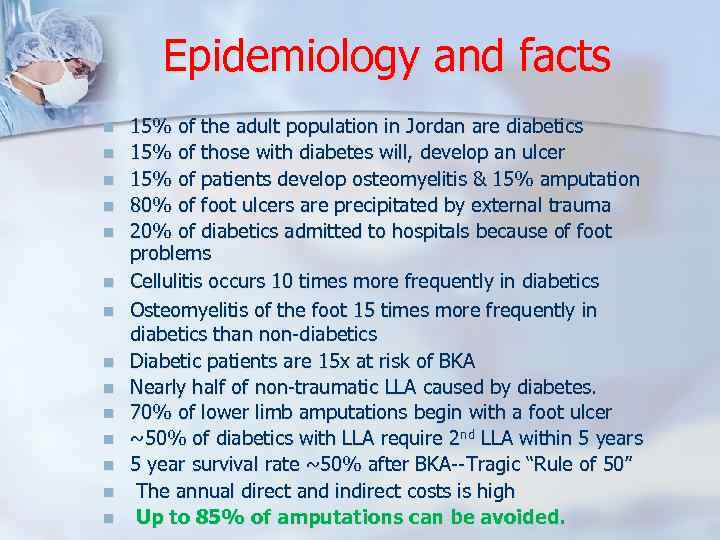
Epidemiology and facts n n n n 15% of the adult population in Jordan are diabetics 15% of those with diabetes will, develop an ulcer 15% of patients develop osteomyelitis & 15% amputation 80% of foot ulcers are precipitated by external trauma 20% of diabetics admitted to hospitals because of foot problems Cellulitis occurs 10 times more frequently in diabetics Osteomyelitis of the foot 15 times more frequently in diabetics than non-diabetics Diabetic patients are 15 x at risk of BKA Nearly half of non-traumatic LLA caused by diabetes. 70% of lower limb amputations begin with a foot ulcer ~50% of diabetics with LLA require 2 nd LLA within 5 years 5 year survival rate ~50% after BKA--Tragic “Rule of 50” The annual direct and indirect costs is high Up to 85% of amputations can be avoided.
Diabetic foot…. . facts n n Every 30 seconds a lower limb is lost somewhere in the world as a consequence of diabetes Diabetic foot infection require attention to local (foot) and systemic (metabolic) issues by multidisciplinary foot care team Only in the last 20 years progress in the understanding of pathogenesis and management of diabetic foot had been made However …. there is still gap between what’s known about diabetic foot and what’s really done to them
Natural history of diabetic foot It’s unwise to consider that major diabetic foot problem occur all of sudden n There is high risk foot which means n There are n 1 - Predisposing factors (Neuro- and angiopathy) ﺍﻟﻌﻮﺍﻣﻞ ﺍﻟﻤﻬﻴﺌﺔ 2 - Precipitating factors (Trauma and tinea) ﺍﻟﻌﻮﺍﻣﻞ ﺍﻟﻤﻌﺠﻠﺔ 3 - Perpetuating factors (Pt’s factors & delay healing) ﻋﻮﺍﻣﻞ ﺍﻟﺘﻜﺮﻳﺲ

What’s the high risk foot ? Long duration and uncontrolled D. M …Plus one or more: n Peripheral neuropathy n Peripheral vascular disease n Trauma n Previous ulcers n Diabetic nephropathy or retinopathy n Obesity n Lack of education n Male gender ? ? !!
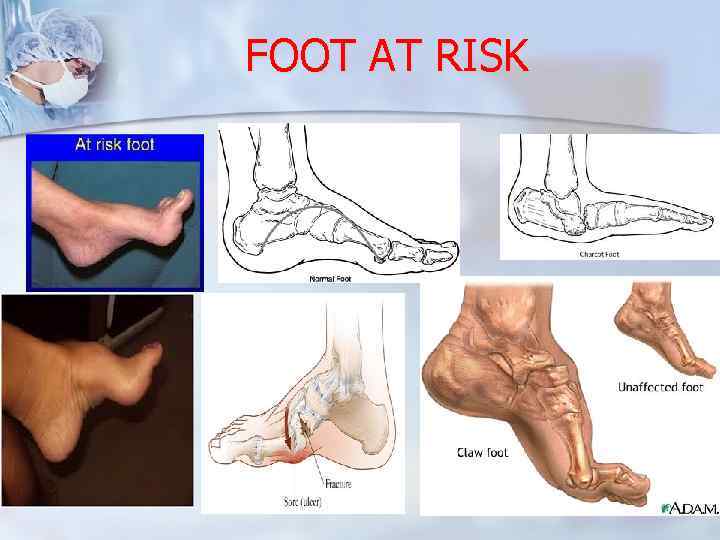
FOOT AT RISK
Pathophysiology The critical triad of : 1 - Neuropathy 2 - Foot deformity & 3 - Trauma …………… will lead to ulcer n The presentation in the majority of pts is an infected ulcer!!
Neuropathy n Sensory : lack of protective sensation (unrecognized trauma) Motor : Change in foot anatomy (Pressure points) & altered gait and deformity n n Autonomic : Lack of sweat ( dry & cracked skin )
Neuropathy The Gift of Pain “Pain: The gift nobody wants “. Paul Brand
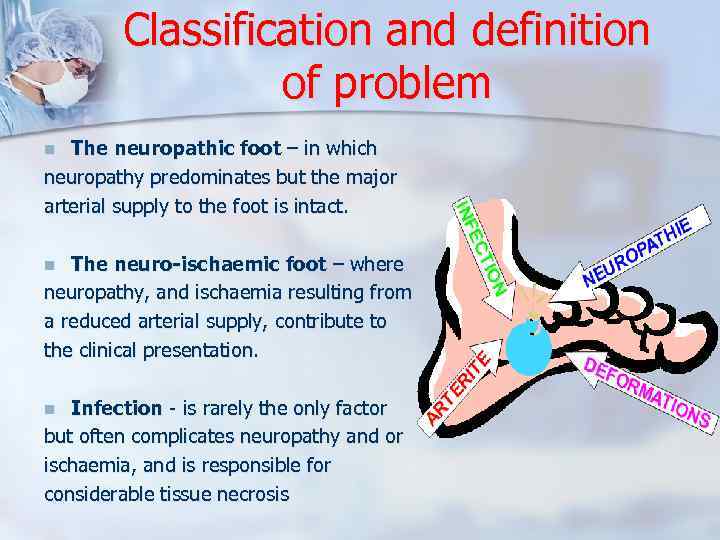
Classification and definition of problem The neuropathic foot – in which neuropathy predominates but the major arterial supply to the foot is intact. n The neuro-ischaemic foot – where neuropathy, and ischaemia resulting from a reduced arterial supply, contribute to the clinical presentation. n Infection - is rarely the only factor but often complicates neuropathy and or ischaemia, and is responsible for considerable tissue necrosis n
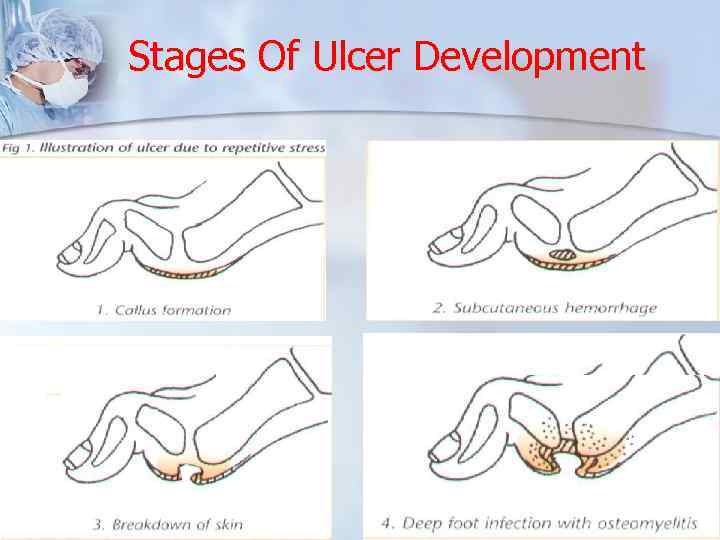
Stages Of Ulcer Development
Assessment History n Physical examinations n Investigations n n n Patient n Limb or foot n Wound n
Who will take care ? G. Physicians n General Surgeons n Diabetologists (Endocrinologist) n Orthopaedic surgeon n Vascular surgeon n Plastic surgeon n Podiatrists n Specialised nurse n
Assessment………. . History Generally: fever, chills, sweats, vom… n Condition : confused, depressed…. n Socially : neglected, lack of home sup n Neuropathy : Numbness, loss of sens. burning, tingling, numbness & nocturnal leg pains. n Others : duration, diabetic control, previous ulceration, smoking, HTN. . n
Assessment………Clinical Ex. What to look for ? n V. S : tachycardia, hypotension… n Signs of volume depletion n Cognitive state: delirium, stupor, coma n Limb-Foot: 1 - Biomechnics: deformities, change pressure points 2 - Vascular status ( arterial, venous, ABI, ischemia, gangrene… 3 - Neuropathy ( light touch, vibration, monofilament pressure 4 - Examining the feet for structural abnormalities such as nails, calluses, hammer toes, claw toes and flat foot
Diabetic Foot Examination n n n n D deformity I infection A atrophic nails B breakdown of skin E oedema T temperature I ischemia C callosities S skin colour
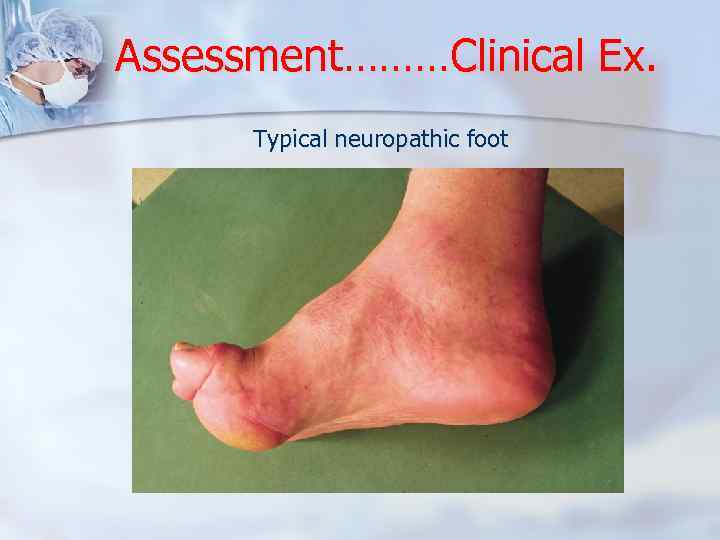
Assessment………Clinical Ex. Typical neuropathic foot
Neurologic assessment § § § § Temperature Vibration Sense Pressure Sense Light Touch Proprioception (Romberg’s Sign) Superficial Pain Reflexes
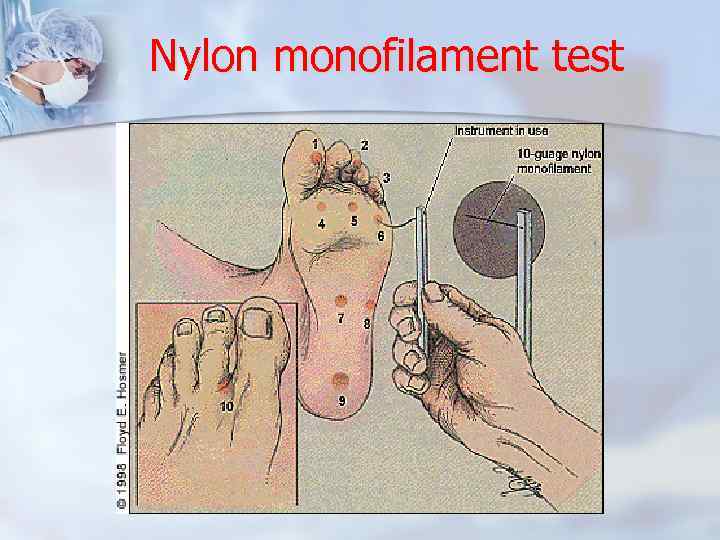
Nylon monofilament test
Neuropathy Charcot foot “Acute or subacute inflammation of all or part of the foot in people with diabetes complicated by distal symmetrical neuropathy, accompanying fracture or dislocation that cannot be explained by recent trauma, and with or without preceding ulceration of the surrounding skin” n (Jeffcoate 2004)
Diagnosis of Acute Charcot n Painless n Redness, swelling, and more than 2°C skin temperature difference when compared with the contralateral foot. n Dorsalis pedis pulses are often bounding. n The patient is afebrile unless a systemic infection is present.
Ulcer assessment 1. 2. 3. 4. 5. 6. 7. 8. 9. Site, size and shape Edges Establish its depth and involvement of deep structures Examine it for purulent exudates, necrosis, sinus tracts, and odor Assess the surrounding tissue for signs of edema, cellulitis, abscess, and fluctuation Perform a vascular evaluation. The ability to gently probe through the ulcer to bone has been shown to be highly predictive of osteomyelitis. Establish the ulcer's etiology Exclude systemic infection
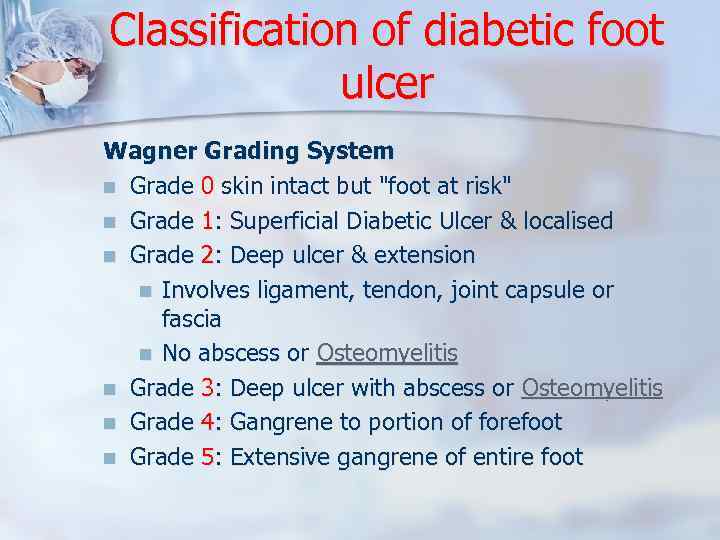
Classification of diabetic foot ulcer Wagner Grading System n Grade 0 skin intact but "foot at risk" n Grade 1: Superficial Diabetic Ulcer & localised n Grade 2: Deep ulcer & extension n Involves ligament, tendon, joint capsule or fascia n No abscess or Osteomyelitis n Grade 3: Deep ulcer with abscess or Osteomyelitis n Grade 4: Gangrene to portion of forefoot n Grade 5: Extensive gangrene of entire foot
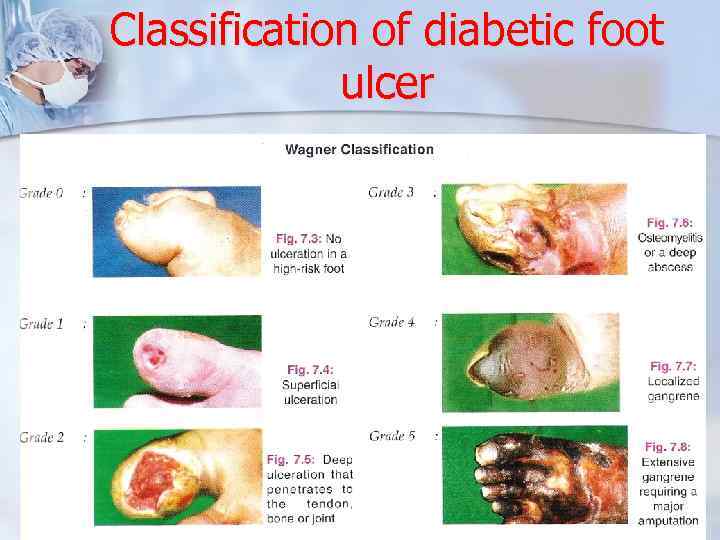
Classification of diabetic foot ulcer
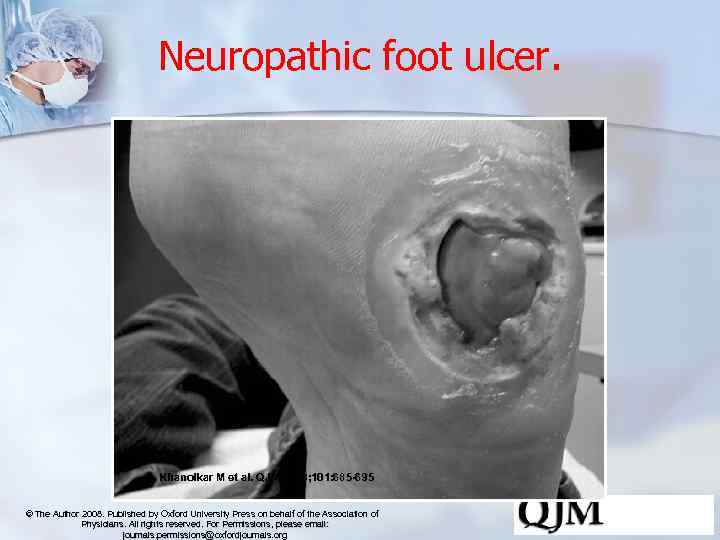
Neuropathic foot ulcer. Khanolkar M et al. QJM 2008; 101: 685 -695 © The Author 2008. Published by Oxford University Press on behalf of the Association of Physicians. All rights reserved. For Permissions, please email: journals. permissions@oxfordjournals. org
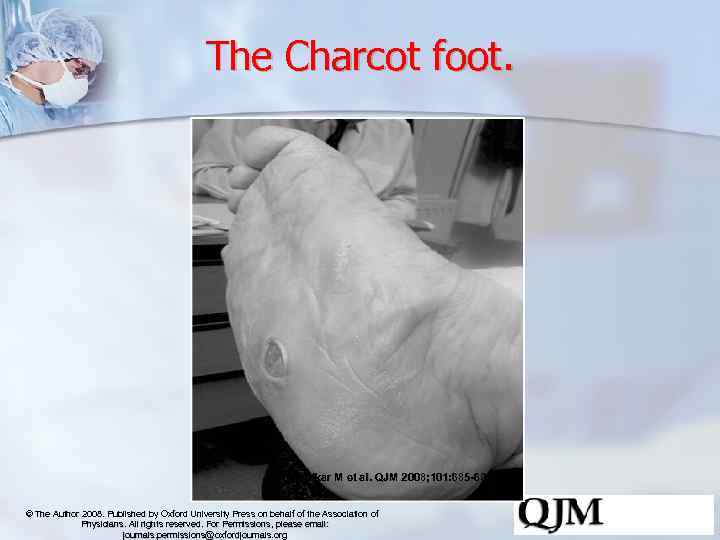
The Charcot foot. Khanolkar M et al. QJM 2008; 101: 685 -695 © The Author 2008. Published by Oxford University Press on behalf of the Association of Physicians. All rights reserved. For Permissions, please email: journals. permissions@oxfordjournals. org
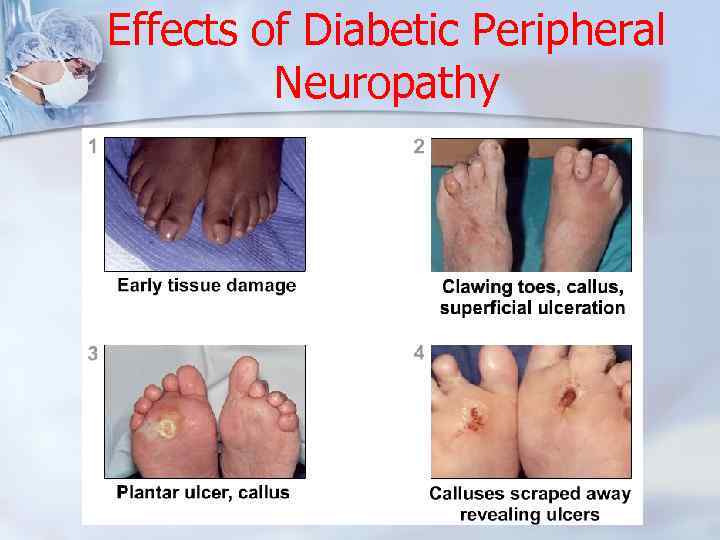
Effects of Diabetic Peripheral Neuropathy
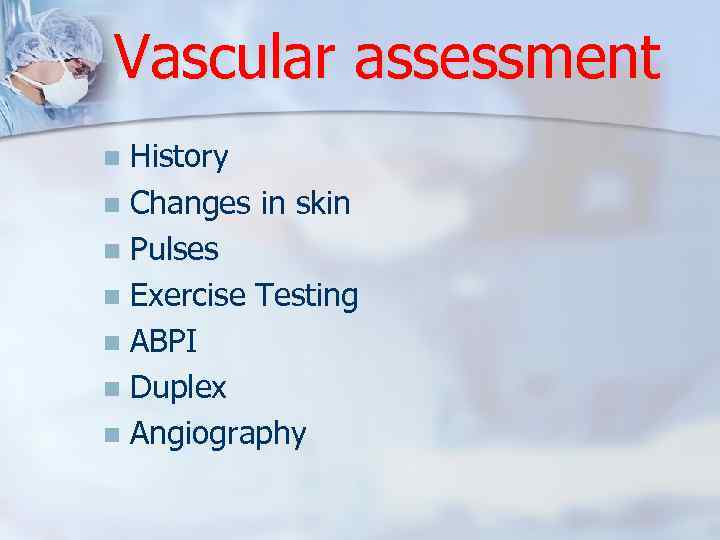
Vascular assessment History n Changes in skin n Pulses n Exercise Testing n ABPI n Duplex n Angiography n
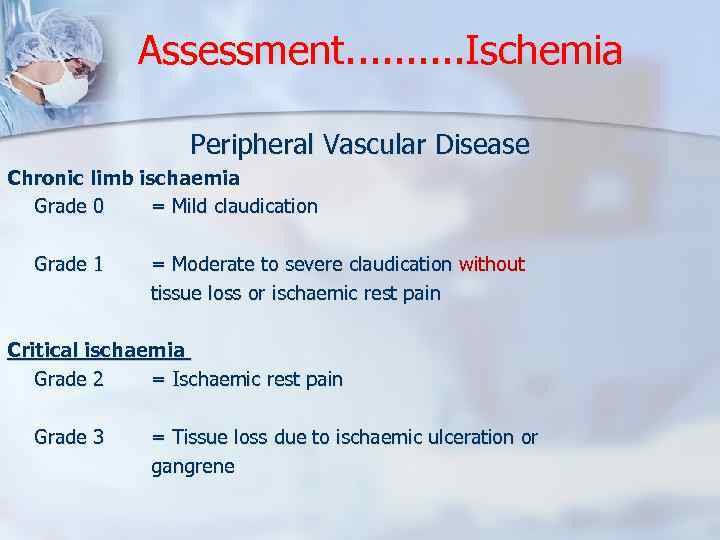
Assessment. . Ischemia Peripheral Vascular Disease Chronic limb ischaemia Grade 0 = Mild claudication Grade 1 = Moderate to severe claudication without tissue loss or ischaemic rest pain Critical ischaemia Grade 2 = Ischaemic rest pain Grade 3 = Tissue loss due to ischaemic ulceration or gangrene
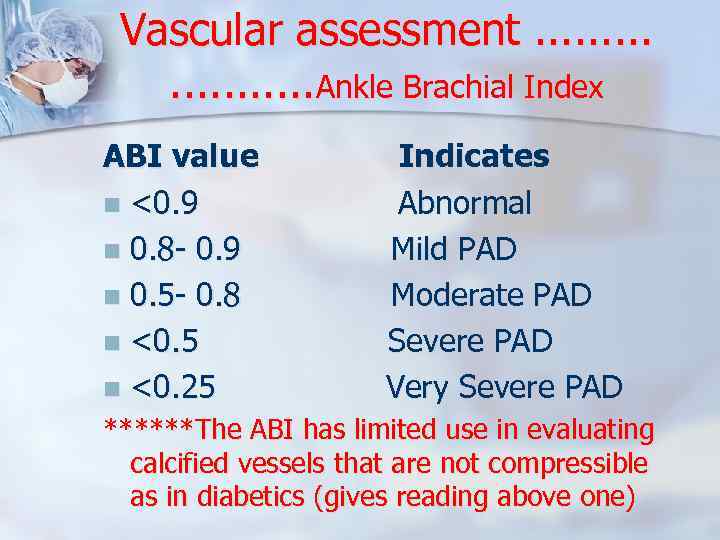
Vascular assessment. . . . . Ankle Brachial Index ABI value Indicates n <0. 9 Abnormal n 0. 8 - 0. 9 Mild PAD n 0. 5 - 0. 8 Moderate PAD n <0. 5 Severe PAD n <0. 25 Very Severe PAD ******The ABI has limited use in evaluating calcified vessels that are not compressible as in diabetics (gives reading above one)
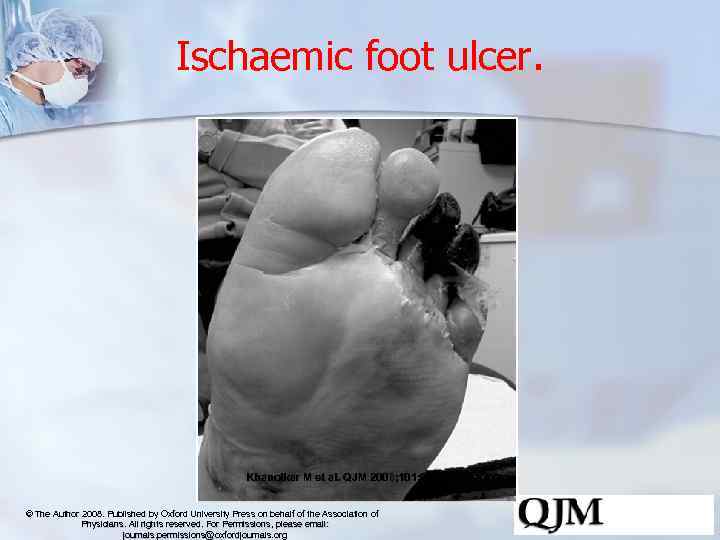
Ischaemic foot ulcer. Khanolkar M et al. QJM 2008; 101: 685 -695 © The Author 2008. Published by Oxford University Press on behalf of the Association of Physicians. All rights reserved. For Permissions, please email: journals. permissions@oxfordjournals. org
Assessment……. Infection is diagnosed clinically by n The presence of purulent secretion OR n At least 2 of the cardinal local manifestations of inflamation n n Hotness Redness Swelling Function loss or pain
Clinical assessment of infection Non-Limb-threatening Infections: n Superficial infection n Lack systemic toxicity n Minimal cellulitis (< 2 cm. Extension from portal of entry) n Ulcer-if present-doesnot penetrate fully thru skin n No bone or joint involvement n No underlying ischemia
Clinical assessment of infection Limb-threatening infections: n Extensive cellulitis (> 2 cm. ) n Lymphangitis n Full-thickness ulcers n Frequent bone & joint infections n Ischemia + gangrene n Fever + n Deep plantar abscesses n Bacteremia + hematogenous spreading infections
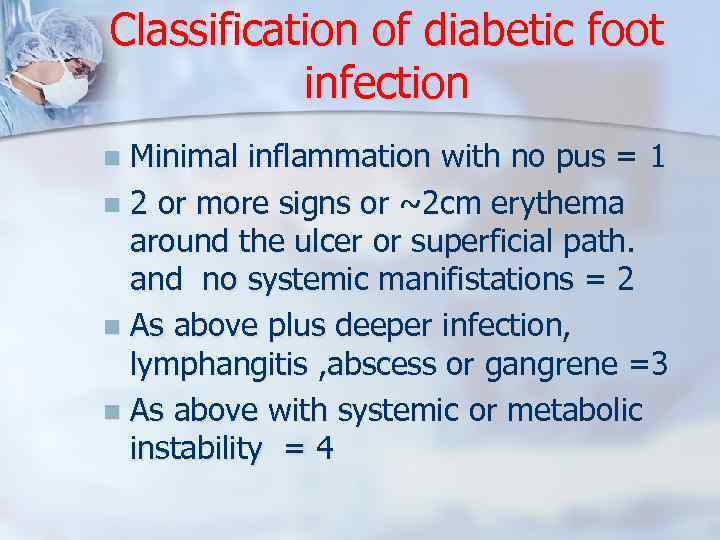
Classification of diabetic foot infection Minimal inflammation with no pus = 1 n 2 or more signs or ~2 cm erythema around the ulcer or superficial path. and no systemic manifistations = 2 n As above plus deeper infection, lymphangitis , abscess or gangrene =3 n As above with systemic or metabolic instability = 4 n

Classification of diabetic foot infection Non-Limb-threatening Infections:

Classification of diabetic foot infection Limb-threatening Infection:
Common Pathogens n n n n MILD infection = MONOMICROBIAL SEVERE infection = POLYMICROBIAL In acute wounds and cellulitis : S. aur. & B. Hem. Strept. are commonly found (+) In chronic infected wounds : add entrobacter (-) Macerated soaked wound : Pseudomonas Long duration & nonhealing : all the above plus fungi Deep infection & extensive necrosis with bad odor : all the above plus obligate anaerobes
Principles of diabetic foot ulcer management ﺑﺪﻫﺎ ﺻﺒﺮ
Five cornerstones of management of the diabetic foot The situation can be changed & possibly reduce amputation rates between 50% 85% by: 1 - Regular inspection and examination of the foot and patient education 2 - Identification of the foot at risk. 3 - Education of patient, family and healthcare providers. 4 - Appropriate footwear. 5 - Multidisciplinary approach & treatment of ulcerative 5 - M and non-ulcer pathology
Patient education Decreases the chance of occurrence n n Foot hygiene Daily inspection Proper footwear Prompt treatment of new lesions Must take an active role in their care n n n Disease management Routine nail care Ulcer management Elective surgery to correct structural deformities before ulcerations occur

A multidisciplinary approach n Providing : - Debridement, - Meticulous wound care, - Adequate vascular supply, - Metabolic control, - Antimicrobial treatment and -Relief of pressure (offloading) are essential in the treatment of foot ulcer.
Investigations n n n - Bloodwork for high BS, DKA, hyperosmolar state…. . Gram staining and culture Imaging Plain X-ray MRI ? Doppler – Angiogram US? For deep abscess Doppler and ABI
Approach to foot wound in diabetics General Principles 1 - Avoid antibiotics in uninfected foot 2 - Determine the need for hospitalization n Severe infection or critical ischemia 3 - Stabilize the patient and correct: - Fluids and electrolytes - Hyperglycemia, hyperosmolarity , acidosis - Treat other exacerbating factors 4 - Choose antibiotic regimen: Limited data support the use of topical antibiotics Mild-moderate infection, give narrow spectrum antibiotics –no anaerob Severe infection, give broad-spectrum with anaerobic coverage
Principles of Foot ulcer management 1. Infection Control 2. Offloading 3. Vascular assessment 4. Wound care

Infection Control n n n Foot infections are the most common cause of admission to hospital for patients with diabetes Infection is a precursor to amputation in many cases Need to be treated aggressively Sampling by sterile swabs misses important pathogens True bacteriological yield is obtained from deep tissue samples IF INFECTION IS PRESENT, DO NOT WAIT FOR SWAB RESULTS
Approach to foot wound in diabetics ……Principles of wound care 1 - Determine the need for surgery n Ranges from debridement to revascularization Determine life- or limb-threatening condition ( NF, GG, Ischemia…. ) 2 - Formulate wound care plan - Daily inspection Dressing and debridement as needed Removal of pressure…. . 3 - Twice- weekly follow up for outpatients 4 - WBC, ESR, C-RP, culture … are of limited value
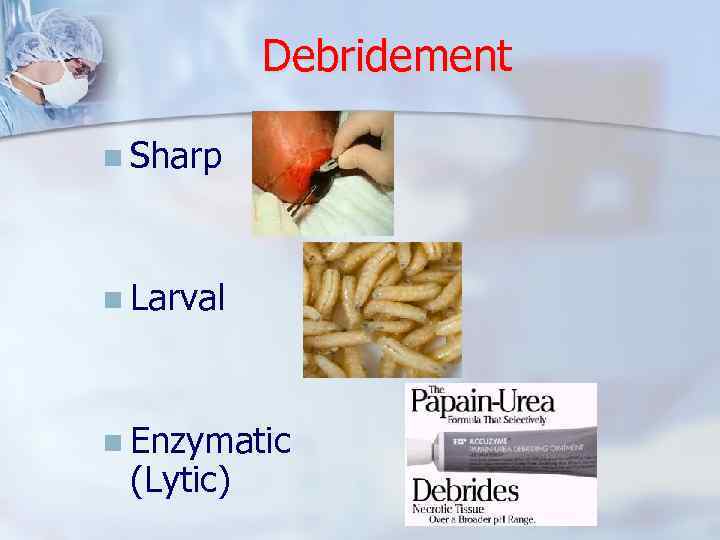
Debridement n Sharp n Larval n Enzymatic (Lytic)
Approach to diabetic foot ulcer According to ulcer stage 0 At-risk foot, no ulceration : Patient education, accommodative footwear, regular clinical examination 1 Superficial ulceration, not infected : Offloading with total contact cast (TCC), walking brace, or special footwear 2 Deep ulceration exposing tendons or joints : Surgical debridement, wound care, offloading, culture-specific antibiotics 3 Extensive ulceration or abscess : Debridement or partial amputation, offloading, culture-specific antibiotics
Approach to ischemic diabetic foot Ischemia Classification A Not ischemic : no treatment A B Ischemia without gangrene: Noninvasive vascular testing, vascular consultation if symptomatic C Partial (forefoot) gangrene : Vascular consultation and debridement D Complete foot gangrene : Major extremity amputation, vascular consultation
Approach to diabetic foot infection Antibiotics Empirical antibiotics Benzylpenicillin or ampicillin – Streptococcus sp. n Oxacillin, nafcillin or 1 st generation cephalosporin (eg. cefazolin) – Staphylococcus sp. n Quinolone + aminoglycoside (gentamycin) – Pseudomonas sp. n Methicillin-resistant Staphylococcus aureus – vancomycin or cotrimoxazole n Clostridial species are sensitive to a combination of penicillin G and clindamycin Duration of antibiotic treatment * 1 -2 weeks course for mild to moderate infections * more than 2 weeks for more serious infections * 6 - 8 weeks for osteomyelitis * If all infected bone is removed, a shorter course (1 -2 weeks) of antibiotics, as for soft tissue infection, may be adequate n

Offlaoding Remove pressure from the affected site is essential How ? - Footwear n - Specialised offloading devices

Offlaoding n Footwear Good shoes are integral to good foot health

Offloading
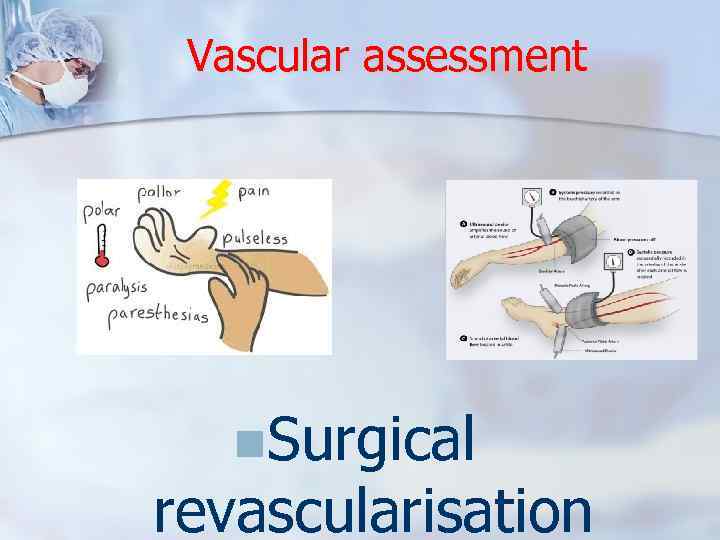
Vascular assessment n. Surgical revascularisation
Follow up n Osteomyelitis Consider potential osteomyelitis in any 1 - Deep or extensive chronic ulcer and over bony prominence 2 - Unhealed ulcer after 6 weeks of Abx. And offloading ttt. 3 - Ulcer in which bone is visible or easily felt 4 - Sausage toe
Osteomyelitis Initial screening tool is the plain X-ray : n Easily obtained, relatively inexpensive and provides anatomical information n Demineralization, periosteal reaction, bony destruction: (the classic triad) n Appear after 30 – 50% of bone is destroyed and can take as much as 2 weeks to appear n Found in other conditions such as fracture or deformity n Sensitivity and specificity approximately 54% and 80%

Osteomyelitis
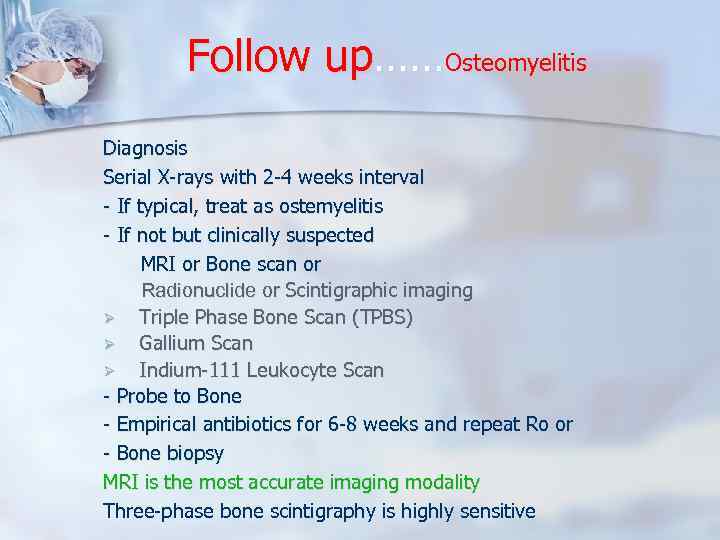
Follow up……Osteomyelitis Diagnosis Serial X-rays with 2 -4 weeks interval - If typical, treat as ostemyelitis - If not but clinically suspected MRI or Bone scan or Radionuclide or Scintigraphic imaging Ø Triple Phase Bone Scan (TPBS) Ø Gallium Scan Ø Indium-111 Leukocyte Scan - Probe to Bone - Empirical antibiotics for 6 -8 weeks and repeat Ro or - Bone biopsy MRI is the most accurate imaging modality Three-phase bone scintigraphy is highly sensitive
Outcome n Good outcome to appropriate therapy In 80– 90% of mild-moderate infection 50 -80% of severe or OM infection n Poor outcome associated with Signs of systemic infection Inadequate limb ischemia OM Necrosis or gangrene Proximal site of infection Inexperienced surgeon
Prevention Early detection of neuropathy n Educate patient about - Optimizing glycemic control n - Using appropriate footwear Avoid foot trauma Perform daily self examination Smoking cessation n Refer patient with critical ischemia -
Key Message Of all late complications of diabetes, foot problems are the most easily detectable and easily preventable. n Relatively simple interventions can reduce amputations by 50 - 80%. (Bakker et al 1994). n Strategies aimed at preventing foot ulcers are cost effective and cost saving. n “The pathway to amputation Is littered with bandages and dressings which have deceived both the doctor and patient into thinking that by dressing an ulcer they were curing it” n Diabetics should treat their Feet like their Face n

Key Message

Mission: … Happy Feet QUSTIONS ?
Diabetic Foot Syndrome 2.pptx