948621d4c9dfdd9cba545a4e25281c47.ppt
- Количество слайдов: 86
Approach to Altered LOC Gabriel Piper March 31 st, 2011
Objectives ► Background ► Assessment ► Approach to the diagnosis ► Managing the undifferentiated altered LOC patient ► Cases!
What is not included? ► An exhaustive review of the work-up or management of specific causes of altered LOC (these are covered elsewhere)
Definitions – Altered LOC ► Hypervigilence - abnormally increased arousal, responsiveness to stimuli, and scanning of the environment for threats. ► Obtundation - awake but not alert. Psychomotor retardation is present ► Drowsiness or lethargy - simulates light sleep. The patient is arousable by touch or noise and can maintain alertness for a period of time. ► Stupor - can be aroused only by vigorous stimuli. Efforts to avoid stimulation are displayed. Little or no spontaneous activity, and shows little motor or verbal activity once aroused. ► Coma - the patient is not arousable at all to verbal or physical stimuli, and no attempt is made to avoid painful or noxious stimuli.
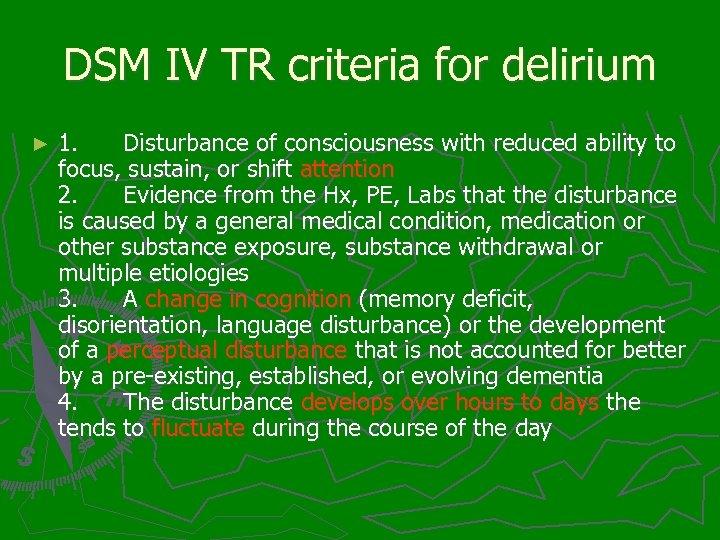
DSM IV TR criteria for delirium ► 1. Disturbance of consciousness with reduced ability to focus, sustain, or shift attention 2. Evidence from the Hx, PE, Labs that the disturbance is caused by a general medical condition, medication or other substance exposure, substance withdrawal or multiple etiologies 3. A change in cognition (memory deficit, disorientation, language disturbance) or the development of a perceptual disturbance that is not accounted for better by a pre-existing, established, or evolving dementia 4. The disturbance develops over hours to days the tends to fluctuate during the course of the day
Pathophysiology
Recognizing Altered LOC The evaluation of a patient’s mental status involves an assessment of two factors: 1) level of consciousness 2) content of consciousness or cognitive function
Assessing Level of consciousness ► Several scales have been created to assess LOC ► GCS, AVPU, ACDU, SMS ► GCS most common in Calgary
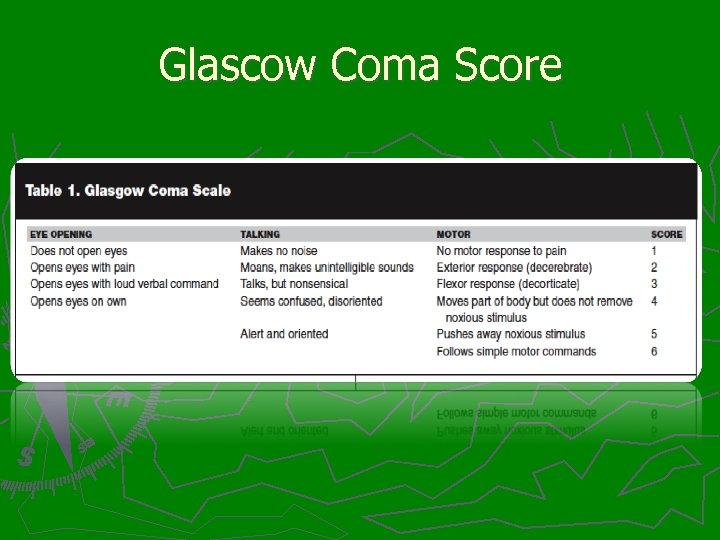
Glascow Coma Score
Simplified Motor Score ► SMS is as good as GCS for predicting important clinical outcomes (emergency intubation, clinically significant brain injury, neurosurgical intervention, and mortality) and has been found to have higher inter-rater reliability ► 3 point scale: obeys commands=2 localizes pain=1 withdrawals to pain or worse=0
Assessing Delirium ► ED docs aren’t very good at diagnosing delirium Study by Lewis of 385 emergency patients aged >65 physician had noted altered mental status in only 17% of patients with delirium
Confusion Assessment Method 1) acute onset and fluctuating course 2) inattention 3) disorganized thinking 4) altered level of consciousness. A diagnosis of delirium according to the CAM requires the presence of features 1, 2, and either 3 or 4
Beware the hypoalert patient Hypoactive delirium makes up 50% of delirious patients vs 25% for hyperactive (25% are mixed)
Now that you have made the diagnosis – what next?
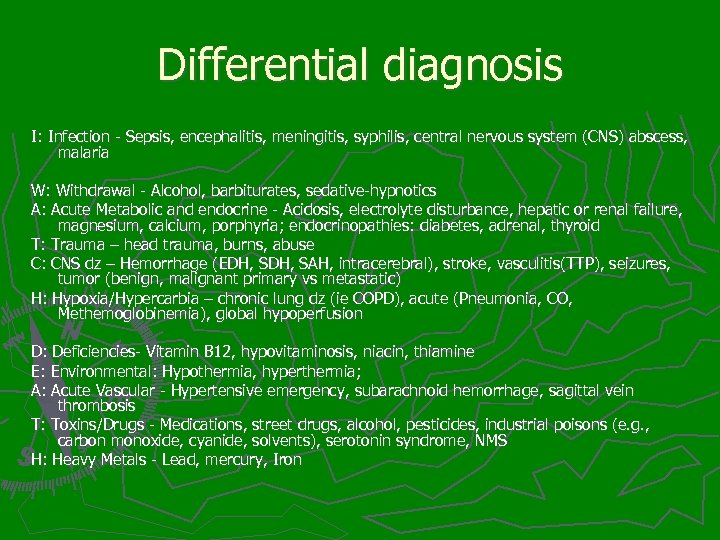
Differential diagnosis I: Infection - Sepsis, encephalitis, meningitis, syphilis, central nervous system (CNS) abscess, malaria W: Withdrawal - Alcohol, barbiturates, sedative-hypnotics A: Acute Metabolic and endocrine - Acidosis, electrolyte disturbance, hepatic or renal failure, magnesium, calcium, porphyria; endocrinopathies: diabetes, adrenal, thyroid T: Trauma – head trauma, burns, abuse C: CNS dz – Hemorrhage (EDH, SAH, intracerebral), stroke, vasculitis(TTP), seizures, tumor (benign, malignant primary vs metastatic) H: Hypoxia/Hypercarbia – chronic lung dz (ie COPD), acute (Pneumonia, CO, Methemoglobinemia), global hypoperfusion D: Deficiencies- Vitamin B 12, hypovitaminosis, niacin, thiamine E: Environmental: Hypothermia, hyperthermia; A: Acute Vascular - Hypertensive emergency, subarachnoid hemorrhage, sagittal vein thrombosis T: Toxins/Drugs - Medications, street drugs, alcohol, pesticides, industrial poisons (e. g. , carbon monoxide, cyanide, solvents), serotonin syndrome, NMS H: Heavy Metals - Lead, mercury, Iron
Other mnemonics ► DIM TOPS § Drugs/withdrawal § Infection § Metabolic § Trauma § Other (endocrine, environmental) § Psych § Structural, seizure ► AEIOU TIPS ► Find one that works for you!
However…. . Let’s create an approach we can use in the ED

Airway ► “GCS <8 then intubate” ► Important to take entire clinical picture into context ► In the abscence of other indications, defer intubation until hypoglycemia and opioid toxicity have been excluded ► maintain C-spine collar if history unknown
Breathing ► Hypoxia: pneumonia, CHF, PE, COPD ► Respiratory depression: opioids, brainstem injury ► Hyperpnia: § Profound Met Acidosis Methanol/EG DKA/AKA/SKA Sepsis - Pulmonary source § Respiratory Stimulation Salicylates
Circulation ► Tachy and Altered…too broad ► Brady and Altered § BB § Li § Organophosphates § Uremic encephalopathy § Hyperkalemia § Ischemia § shock
Circulation cont ► Hypotension: § volume/blood loss § Sepsis § cardiogenic shock § Addisonian crisis ► Hypertension: § hypertensive encephalopathy § hyperadrenergic crises
Hot and Altered ► Meningitis/Encephalitis/Abscess ► Thyroid storm ► Hyperthermia ► CVA/CNS bleeds ► Tox § Sympathomimetics/Anticholinergics § Withdrawal § NMS/SS/MH § Cholinergics § ASA
Cold and Altered ► Environmental ► Infection ► Thyroid ► Wernicke’s (hypothalamic dysfunction)
Glucose ► Consider it the 5 th vital sign ► If hypoglycemic, treat with 1 -2 amps of D 50
Coma cocktail - DONT ► Dextrose ► Oxygen ► Naloxone ► Thiamine ► Flumazanil?
Raised ICP? ► deep coma ► unilateral dilated pupil (unexplained by drug effect or eye disease) ► abnormal posturing ► abnormal breathing patterns +/- hypertension and bradycardia

Treat Fever ► Acetominophen ► Cooling ► Benzodiazepines
Consider early antibiotics for sepsis/menigitis ► Early Abx shown to be important in severe infections ► Draw blood cultures prior to starting Abx ► Give Abx before sending to CT if high suspicion of infection
Agitated delirium ► Clear association exists between illicit drug use and the syndrome but not universal. ► Non-drug related causes are almost always psychotic (schizophrenia, bipolar) ► Treat if: § Presence of excited delirium § Continued maximal struggle despite attempts at maximal restraint
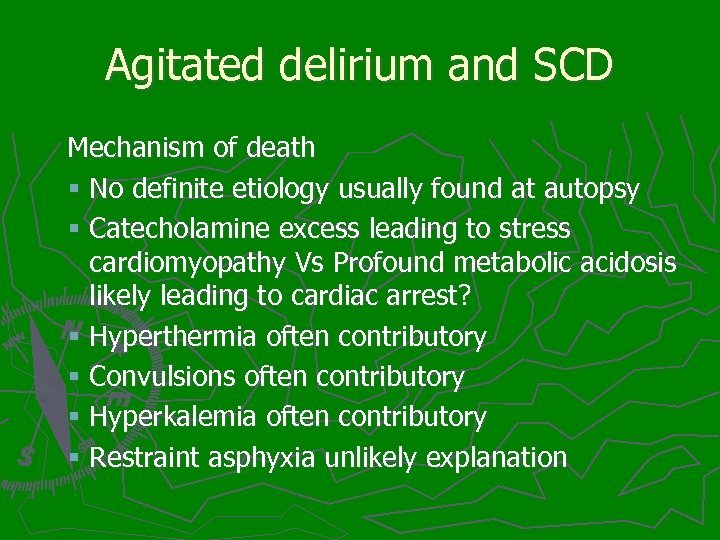
Agitated delirium and SCD Mechanism of death § No definite etiology usually found at autopsy § Catecholamine excess leading to stress cardiomyopathy Vs Profound metabolic acidosis likely leading to cardiac arrest? § Hyperthermia often contributory § Convulsions often contributory § Hyperkalemia often contributory § Restraint asphyxia unlikely explanation
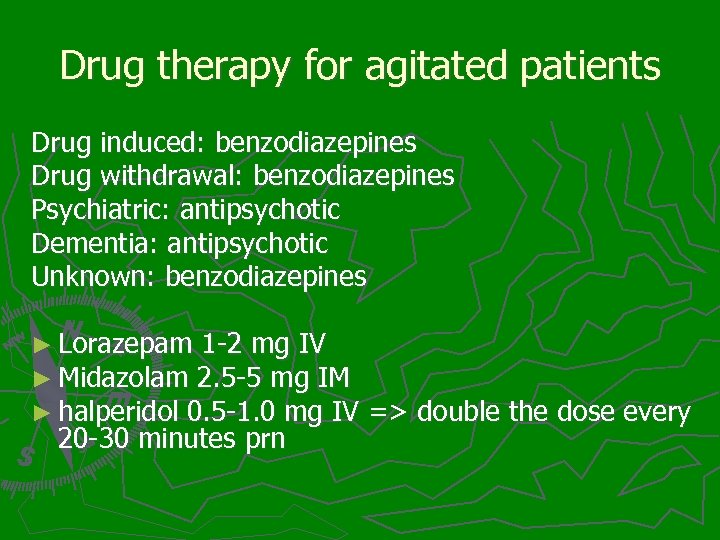
Drug therapy for agitated patients Drug induced: benzodiazepines Drug withdrawal: benzodiazepines Psychiatric: antipsychotic Dementia: antipsychotic Unknown: benzodiazepines ► Lorazepam 1 -2 mg IV ► Midazolam 2. 5 -5 mg IM ► halperidol 0. 5 -1. 0 mg IV => double the dose every 20 -30 minutes prn
Now that you have treated life threatening emergencies and have calmed the patient down…. . Time to figure out what is going on
History ► Collateral ► Baseline ► Change in mental status ► PMHx ► Medications/toxins ► Social history ► ROS
Collateral ► EMS: onset, location, evidence of trauma, information about home environment, medications in home ► Family/friends: focal signs prior to LOC, prodromal symptoms (fevers, HA, etc), ingestions, access to medications ► Other: Old charts, net care, medic alert bracelet
Baseline ► mental and behavioural status; normally fully oriented, cognitively intact, attentive and capable of normal social functioning. ► if the patient has an abnormal baseline mental status => try and semi-quantitate the degree and time course of any mental status changes (when he last drove a car, balanced a checkbook, fed himself, dressed himself, had a coherent conversation and so on) ► social functioning, occupational status, physical status
Change in Mental Status ► ► ► time of onset course and lability precipitating events (seizure, head injury) presence of lucid intervals changes in sleep-awake cycle; Disturbance in the sleep-wake cycle often occurs early in the course of delirium. "sundowning" phenomenon degree of attentiveness and distractability; the ability to sustain a conversation or a task short term memory changes perceptual disturbances -illusions, hallucinations, delusions emotional lability and poor capacity to modulate emotional behaviour psychomotor disturbances - asterixis, myoclonus, motor restlessness
PMHx Chronic illnesses (hepatic or renal failure, endocrinopathies, COPD, DM, CHF) ► immunosuppression ► Previous history of alcoholism or Wernicke's encephalopathy ► Physical, emotional, mental disabilities ► Recent hospitalisations ► Recent surgery ► Recent cancer treatment (paraneoplastic syndrome) ► Recent outpatient therapy or dialysis ► Recent depression or suicide ideation ►
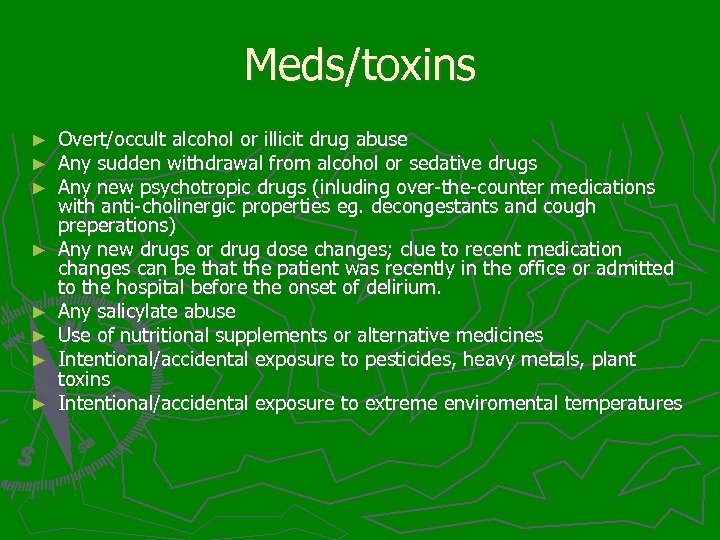
Meds/toxins ► ► ► ► Overt/occult alcohol or illicit drug abuse Any sudden withdrawal from alcohol or sedative drugs Any new psychotropic drugs (inluding over-the-counter medications with anti-cholinergic properties eg. decongestants and cough preperations) Any new drugs or drug dose changes; clue to recent medication changes can be that the patient was recently in the office or admitted to the hospital before the onset of delirium. Any salicylate abuse Use of nutritional supplements or alternative medicines Intentional/accidental exposure to pesticides, heavy metals, plant toxins Intentional/accidental exposure to extreme enviromental temperatures
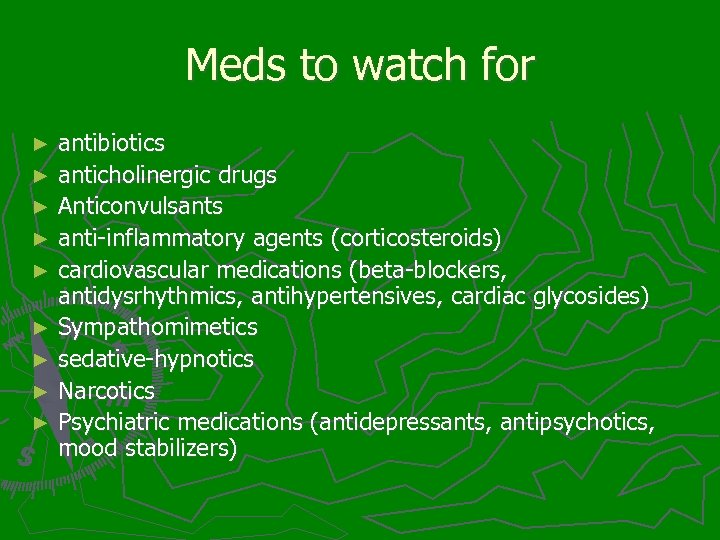
Meds to watch for antibiotics ► anticholinergic drugs ► Anticonvulsants ► anti-inflammatory agents (corticosteroids) ► cardiovascular medications (beta-blockers, antidysrhythmics, antihypertensives, cardiac glycosides) ► Sympathomimetics ► sedative-hypnotics ► Narcotics ► Psychiatric medications (antidepressants, antipsychotics, mood stabilizers) ►
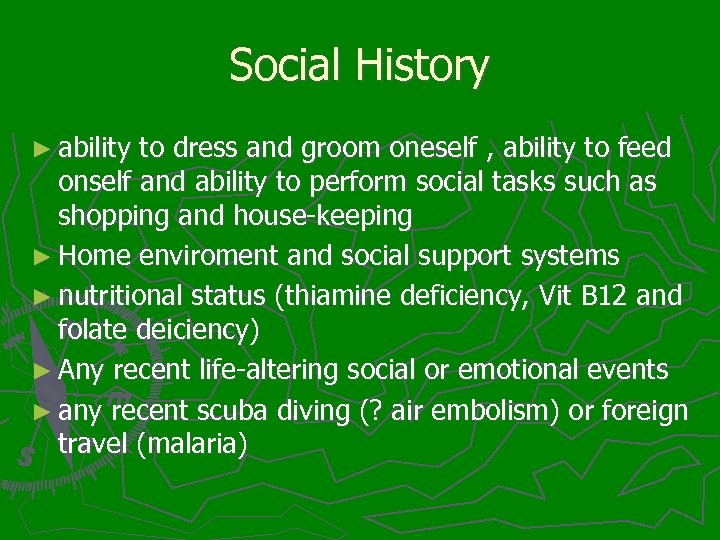
Social History ► ability to dress and groom oneself , ability to feed onself and ability to perform social tasks such as shopping and house-keeping ► Home enviroment and social support systems ► nutritional status (thiamine deficiency, Vit B 12 and folate deiciency) ► Any recent life-altering social or emotional events ► any recent scuba diving (? air embolism) or foreign travel (malaria)
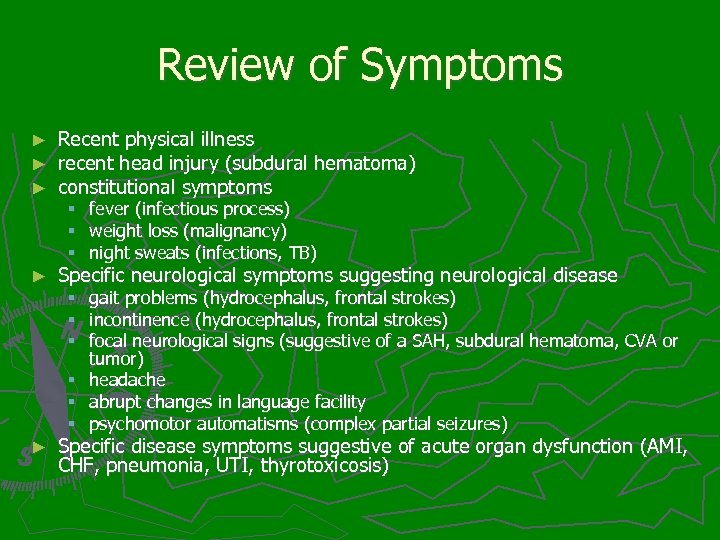
Review of Symptoms ► ► ► Recent physical illness recent head injury (subdural hematoma) constitutional symptoms § § § ► fever (infectious process) weight loss (malignancy) night sweats (infections, TB) gait problems (hydrocephalus, frontal strokes) incontinence (hydrocephalus, frontal strokes) focal neurological signs (suggestive of a SAH, subdural hematoma, CVA or tumor) headache abrupt changes in language facility psychomotor automatisms (complex partial seizures) Specific neurological symptoms suggesting neurological disease § § § ► Specific disease symptoms suggestive of acute organ dysfunction (AMI, CHF, pneumonia, UTI, thyrotoxicosis)
Physical Exam ► Complete physical exam ► Look for physical evidence of diseases that may have precipitated altered LOC ► Mental status exam to diagnose subtle delirium and to help differentiate delirium from dementia



Neuro ► ► ► ► ► Pupils (brainstem lesion, toxidromes) nystagmus (Wernicke's encephalopathy, PCP intoxication, alchohol (s) intoxication) cranial nerves (CVA, CNS tumor, Wernicke's opthalmoplegia) muscle strength, tone, clonus, abnormal movements (CVA, spaceoccupying lesions, NMS or serotonin syndrome) pathologic primitive reflexes (frontal lobe tumor, strokes or subdural) gait apraxia (hydrocephalus, chronic subdural) peripheral neuropathy (alcoholic, porphyria, paraneoplastic, vitamin B 12 deficiency) circumoral and distal limb paresthesias and tetany (hypocalcemia) Reflexes: generalized hyperreflexia can be found in serotonin syndrome, tetanus, rabies and strychnine poisoning; while delayed "hung up" reflexes are found in myxedema coma
Skin ► ► ► increased pigmentation Jaundice, spider nevi, caput medusa Needle tracks cyanosis unresponsive to oxygen (methemoglobinemia) feathering burns (lightning injury) Petechiae and Ecchymosis: § § Confined to head and neck – seizure or strangulation or emesis Bleeding diathesis – thrombocytopenia, DIC Vasculitis menigococcemia perspiration: Fevers, Hypoglycemia, pheochromocytoma - dry, warm, flushed - think tox ► Cellulitis/nec fasc ► uremic frost, anasarca (renal failure) ►
HEENT ► Stiff neck, positive Jolt test ► Cherry red lips: CO ► skull - scalp hematoma, Battle's sign, hemotympanum, CSF otorrhea, raccoon eyes, diffuse subconjunctival hemorrhage, epistaxis, CSF rhinorrhea (traumatic head injury); palpable shunt (shunt malfunction) ► Tongue bitten on lateral aspect (seizures) ► odor of breath – alcohol, almonds (cyanide), acetone (DKA), ammonia (fetor hepaticus)
Cardiac/Resp/Abdo ► cardiac ischemia/AMI (abnormal heart sounds, murmurs) ► CHF (tachypnea, abnormal heart sounds, murmurs, rales, hepatomegealy, pedal edema) ► pneumonia (tachypnea, rales, bronchial breathing) ► Intra-abdominal infections (peritonitis, ascites)
Syndromes ► liver failure - jaundice, spider nevi, caput medusae, ascites, hepatomegaly or shrunken hard liver, genital atrophy, gynecomastia, fetor hepaticus ► Thyrotoxicosis - enlarged thyroid, autonomic hyperactivity, exopthalmos, pretibial myxedema ► toxidromes eg. anticholinergic toxicity (red flushed skin, mydriasis, tachycardia, hypertension, urinary retention, decreased bowel sounds)
Mental Status exam? ► Do I have to do a MMSE? ► Exam should include assessment of: § the patient's ability to focus and sustain attention § the patient's capacity to think in an organized manner § the patient's short-term memory * A change in baseline in any of these should make you think of delirium
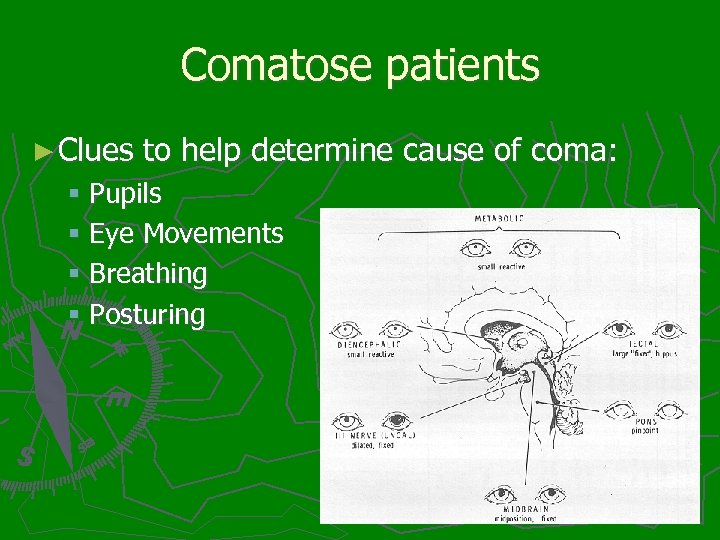
Comatose patients ► Clues to help determine cause of coma: § Pupils § Eye Movements § Breathing § Posturing
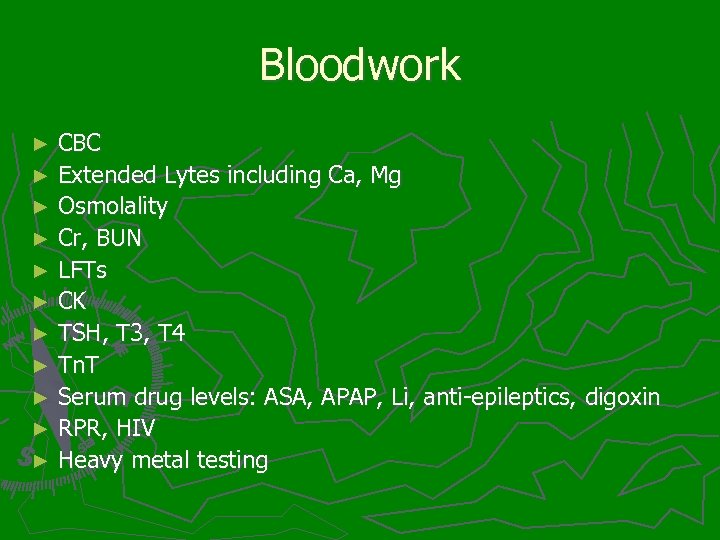
Bloodwork CBC ► Extended Lytes including Ca, Mg ► Osmolality ► Cr, BUN ► LFTs ► CK ► TSH, T 3, T 4 ► Tn. T ► Serum drug levels: ASA, APAP, Li, anti-epileptics, digoxin ► RPR, HIV ► Heavy metal testing ►
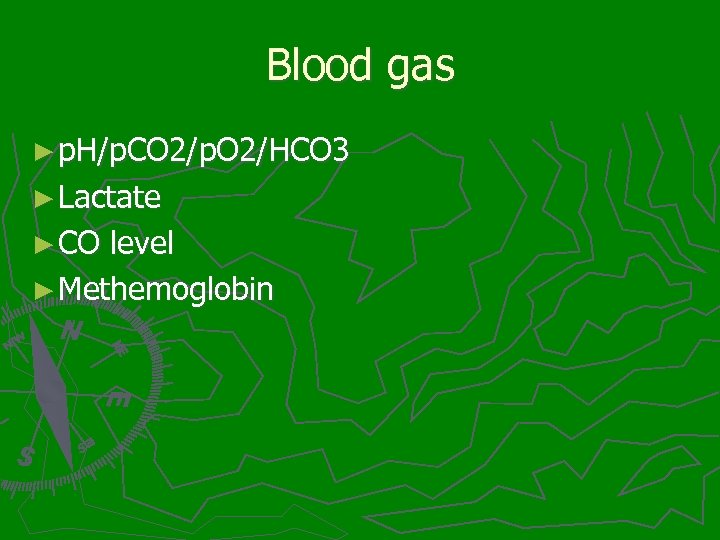
Blood gas ► p. H/p. CO 2/p. O 2/HCO 3 ► Lactate ► CO level ► Methemoglobin
Urine ► Urinalysis ► Urine pregnancy ► Urine drugs of Abuse?
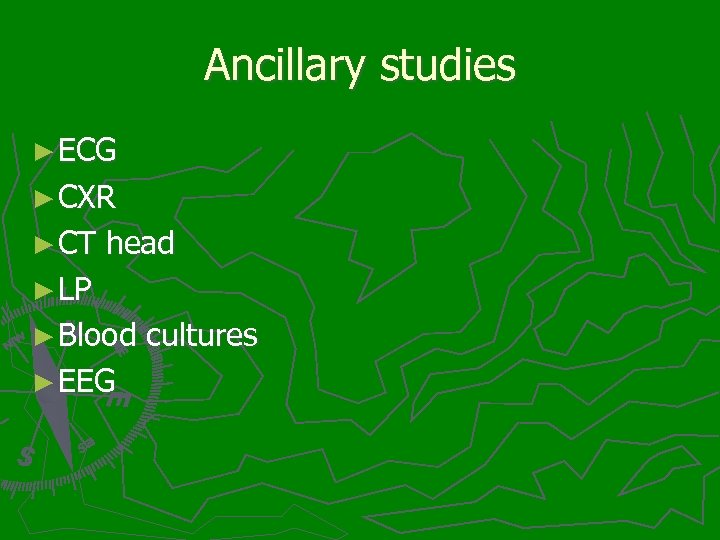
Ancillary studies ► ECG ► CXR ► CT head ► LP ► Blood cultures ► EEG
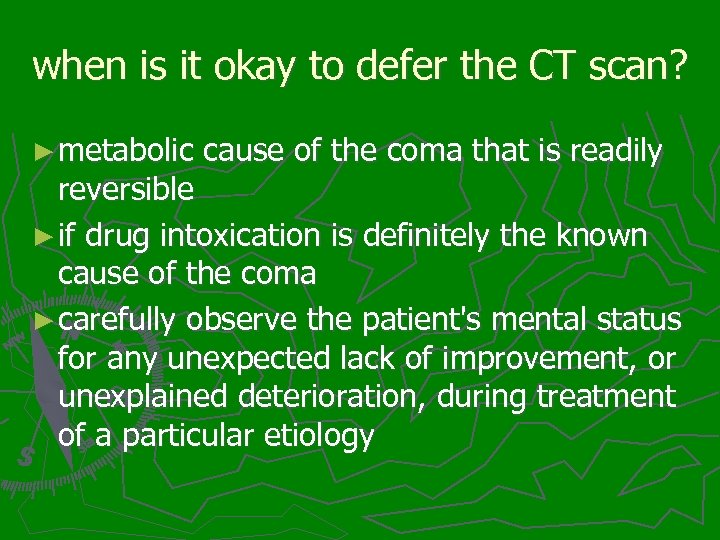
when is it okay to defer the CT scan? ► metabolic cause of the coma that is readily reversible ► if drug intoxication is definitely the known cause of the coma ► carefully observe the patient's mental status for any unexpected lack of improvement, or unexplained deterioration, during treatment of a particular etiology
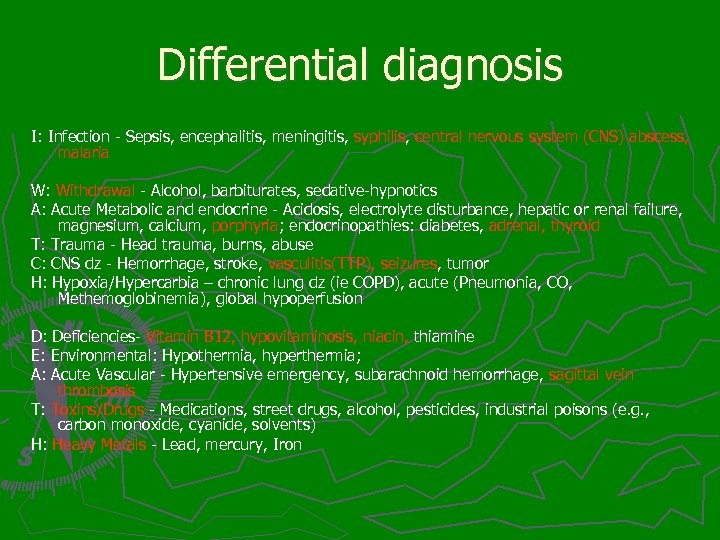
Differential diagnosis I: Infection - Sepsis, encephalitis, meningitis, syphilis, central nervous system (CNS) abscess, malaria W: Withdrawal - Alcohol, barbiturates, sedative-hypnotics A: Acute Metabolic and endocrine - Acidosis, electrolyte disturbance, hepatic or renal failure, magnesium, calcium, porphyria; endocrinopathies: diabetes, adrenal, thyroid T: Trauma - Head trauma, burns, abuse C: CNS dz - Hemorrhage, stroke, vasculitis(TTP), seizures, tumor H: Hypoxia/Hypercarbia – chronic lung dz (ie COPD), acute (Pneumonia, CO, Methemoglobinemia), global hypoperfusion D: Deficiencies- Vitamin B 12, hypovitaminosis, niacin, thiamine E: Environmental: Hypothermia, hyperthermia; A: Acute Vascular - Hypertensive emergency, subarachnoid hemorrhage, sagittal vein thrombosis T: Toxins/Drugs - Medications, street drugs, alcohol, pesticides, industrial poisons (e. g. , carbon monoxide, cyanide, solvents) H: Heavy Metals - Lead, mercury, Iron
Managing Delirium ► minimize sensory overload by limiting the number of care-givers and ensuring a quiet enviroment ► allow family members to remain in constant/frequent attendance ► do not leave patients unattended in the hallway and ensure that the bed side-rails are up
Cases
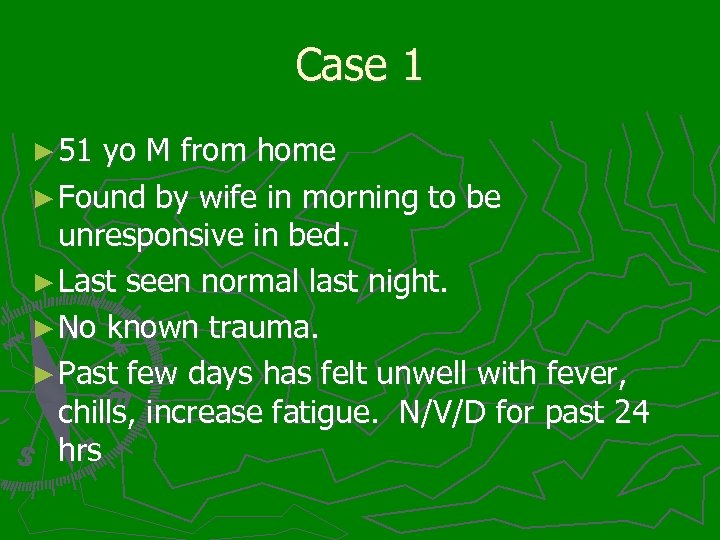
Case 1 ► 51 yo M from home ► Found by wife in morning to be unresponsive in bed. ► Last seen normal last night. ► No known trauma. ► Past few days has felt unwell with fever, chills, increase fatigue. N/V/D for past 24 hrs
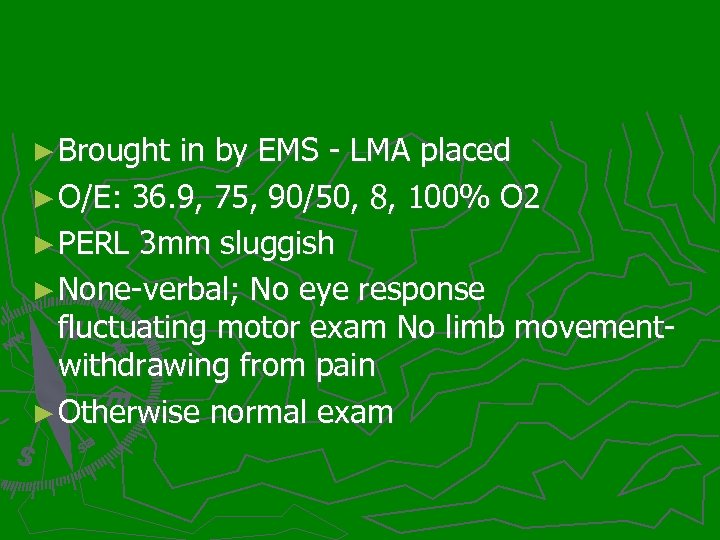
► Brought in by EMS - LMA placed ► O/E: 36. 9, 75, 90/50, 8, 100% O 2 ► PERL 3 mm sluggish ► None-verbal; No eye response fluctuating motor exam No limb movementwithdrawing from pain ► Otherwise normal exam
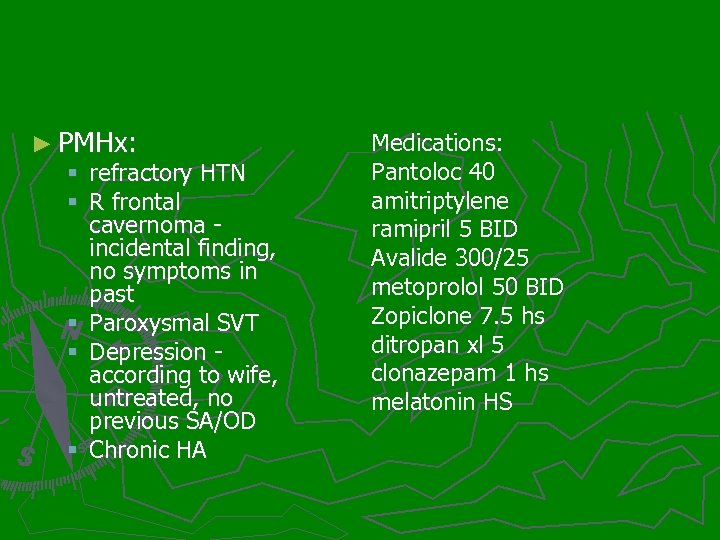
► PMHx: § refractory HTN § R frontal cavernoma - incidental finding, no symptoms in past § Paroxysmal SVT § Depression - according to wife, untreated, no previous SA/OD § Chronic HA Medications: Pantoloc 40 amitriptylene ramipril 5 BID Avalide 300/25 metoprolol 50 BID Zopiclone 7. 5 hs ditropan xl 5 clonazepam 1 hs melatonin HS
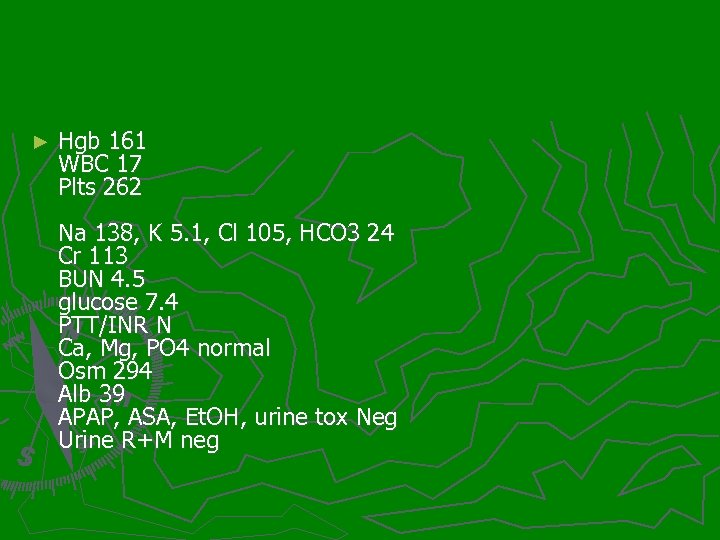
► Hgb 161 WBC 17 Plts 262 Na 138, K 5. 1, Cl 105, HCO 3 24 Cr 113 BUN 4. 5 glucose 7. 4 PTT/INR N Ca, Mg, PO 4 normal Osm 294 Alb 39 APAP, ASA, Et. OH, urine tox Neg Urine R+M neg
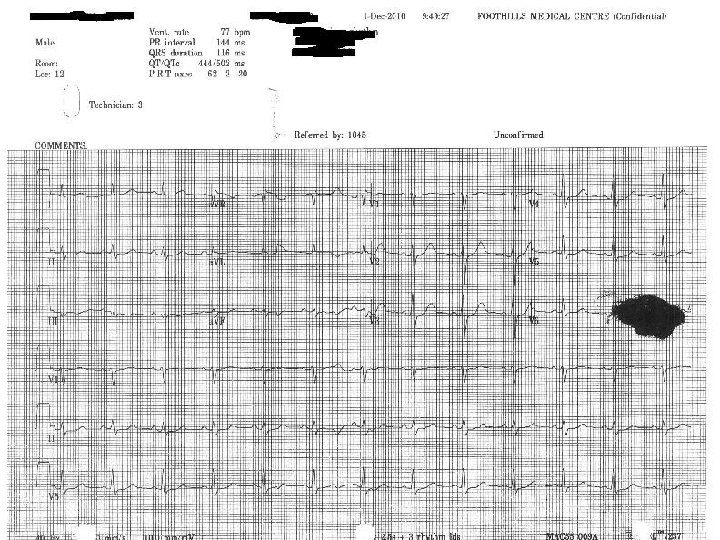
► CT head – no change from previous ► LP – normal ► EEG – Normal
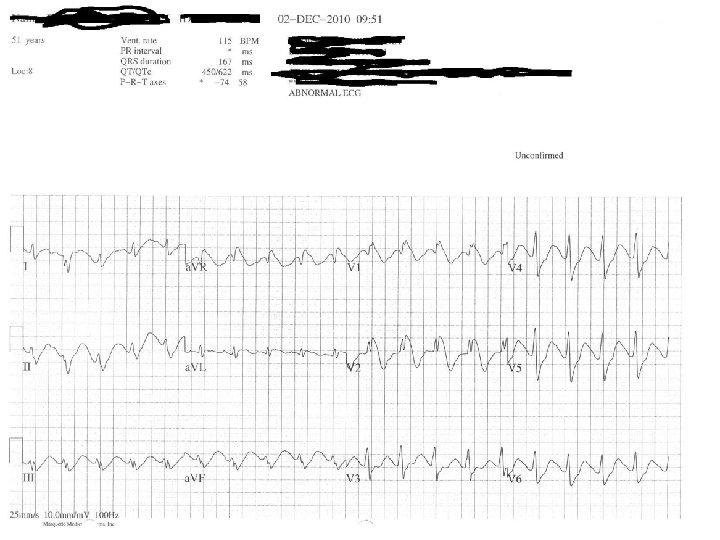
Case 2 ► It is 15 mins after handover and the nurse tells you she is concerned about a 22 year old Female patient ► handed over as a case of “found down at a party" with normal CXR, ECG and labs, urine is pending.
► HR = 100 BP = 120/70 RR = 12 T = 36. 0 ► no response to pain, eyes do not open, un- intelligible sounds ► you also note a rapid, mild, but prominent twitching of upper and lower extremities.
Non-convulsive Status epilepticus ► ongoing subtle status epilepticus should be suspected if there any ongoing subtle twitching, jerking movements, fluttering eyelids - especially if the patient has a history of seizures + evidence of tongue biting, urinary incontinence
Case 3 ► 32 yo M with presents with fever, altered mental status, and vomiting.
patient was too altered to provide a history from family members ► 3 days before admission, when he developed fevers and confusion, and began vomiting. He complained of a headache and neck stiffness. ► HIV positive. Has never been on antiretroviral therapy. ► He was not taking any medications before the onset of his illness and had no known drug allergies. His last CD 4 count of 146 cells/µL was measured a month and a half before admission. The patient smokes tobacco and reportedly has a history of significant alcohol intake. ►
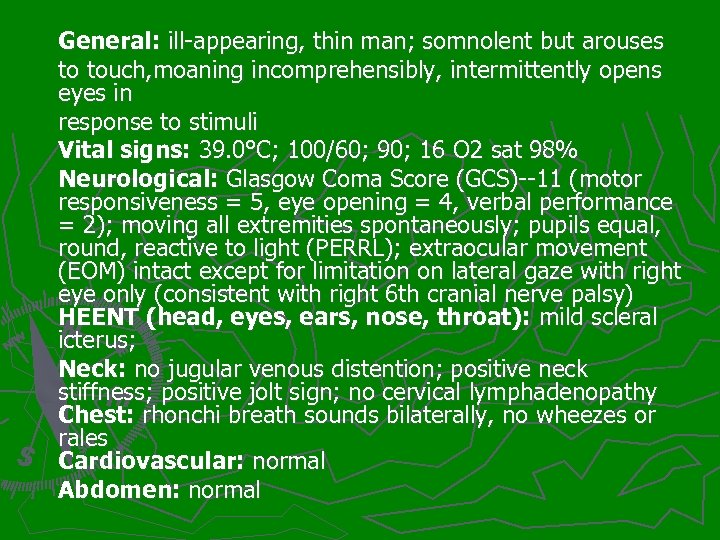
General: ill-appearing, thin man; somnolent but arouses to touch, moaning incomprehensibly, intermittently opens eyes in response to stimuli Vital signs: 39. 0°C; 100/60; 90; 16 O 2 sat 98% Neurological: Glasgow Coma Score (GCS)--11 (motor responsiveness = 5, eye opening = 4, verbal performance = 2); moving all extremities spontaneously; pupils equal, round, reactive to light (PERRL); extraocular movement (EOM) intact except for limitation on lateral gaze with right eye only (consistent with right 6 th cranial nerve palsy) HEENT (head, eyes, ears, nose, throat): mild scleral icterus; Neck: no jugular venous distention; positive neck stiffness; positive jolt sign; no cervical lymphadenopathy Chest: rhonchi breath sounds bilaterally, no wheezes or rales Cardiovascular: normal Abdomen: normal
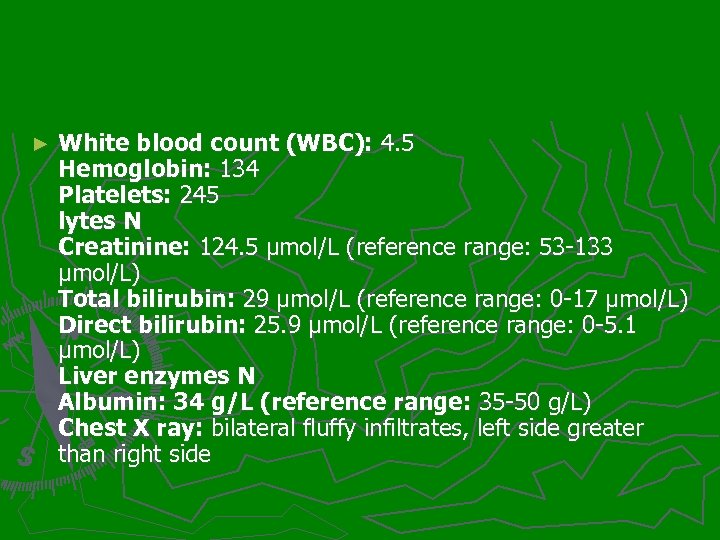
► White blood count (WBC): 4. 5 Hemoglobin: 134 Platelets: 245 lytes N Creatinine: 124. 5 µmol/L (reference range: 53 -133 µmol/L) Total bilirubin: 29 µmol/L (reference range: 0 -17 µmol/L) Direct bilirubin: 25. 9 µmol/L (reference range: 0 -5. 1 µmol/L) Liver enzymes N Albumin: 34 g/L (reference range: 35 -50 g/L) Chest X ray: bilateral fluffy infiltrates, left side greater than right side
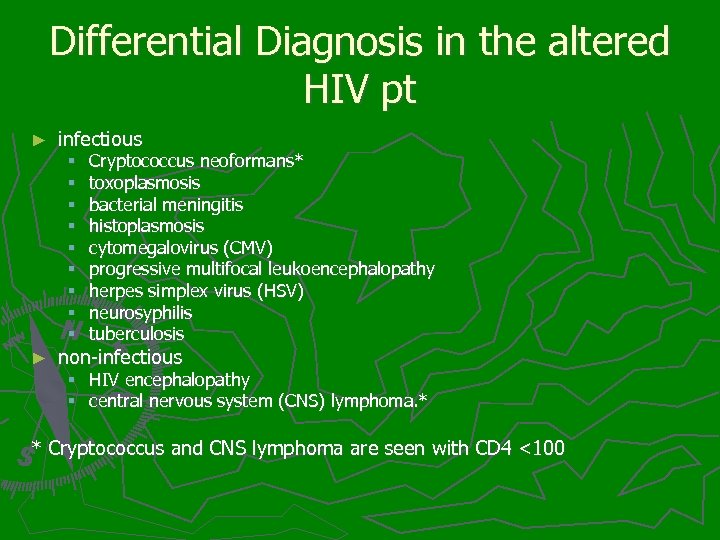
Differential Diagnosis in the altered HIV pt ► infectious § § § § § ► Cryptococcus neoformans* toxoplasmosis bacterial meningitis histoplasmosis cytomegalovirus (CMV) progressive multifocal leukoencephalopathy herpes simplex virus (HSV) neurosyphilis tuberculosis non-infectious § HIV encephalopathy § central nervous system (CNS) lymphoma. * * Cryptococcus and CNS lymphoma are seen with CD 4 <100
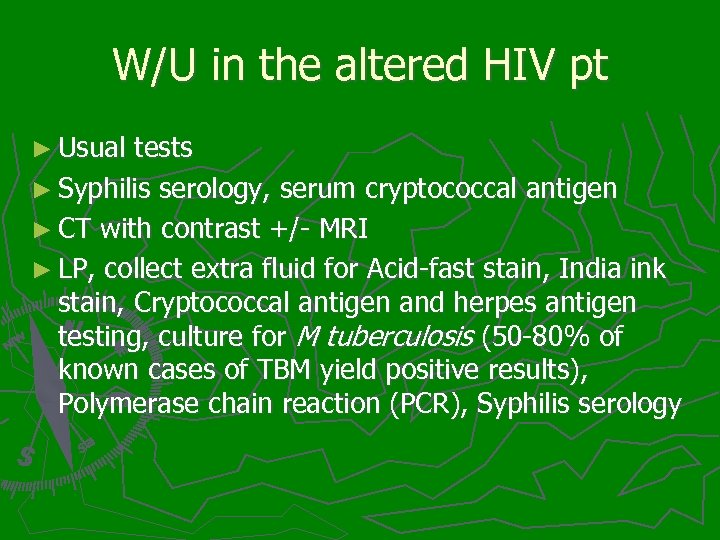
W/U in the altered HIV pt ► Usual tests ► Syphilis serology, serum cryptococcal antigen ► CT with contrast +/- MRI ► LP, collect extra fluid for Acid-fast stain, India ink stain, Cryptococcal antigen and herpes antigen testing, culture for M tuberculosis (50 -80% of known cases of TBM yield positive results), Polymerase chain reaction (PCR), Syphilis serology
Case 4 ► 88 yo M, brought into ED by family because he is less responsive than usual ► Fell out of bed last night
► 36. 5, 70, 130/80, 16, 94% ► Patient is somnolent and does not answer questions appropriately ► Exam is unremarkable except for patient is somnolent and does not answer questions appropriately ► According to family he is normally able to sustain a conversation
Delirium vs. Dementia ► both delirium and dementia are characterized by a global impairment in cognitive functioning ► meticulous history-taking is sometimes required to differentiate between these two entities ► Beware hypoactive delirium in the demented patient!
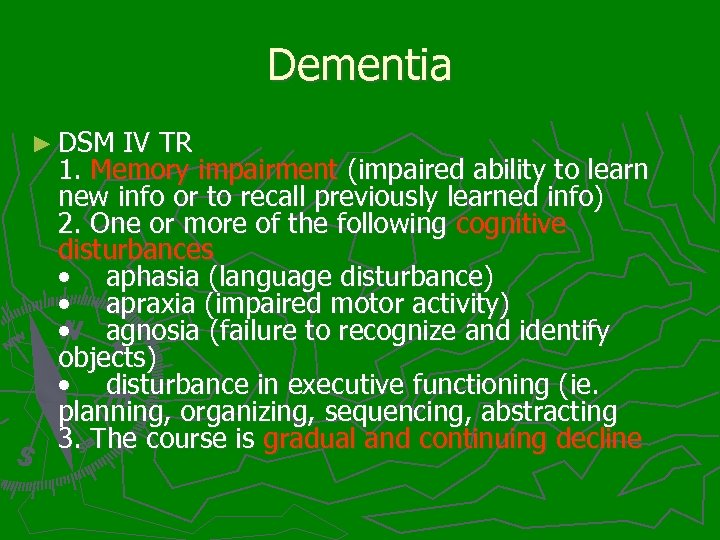
Dementia ► DSM IV TR 1. Memory impairment (impaired ability to learn new info or to recall previously learned info) 2. One or more of the following cognitive disturbances • aphasia (language disturbance) • apraxia (impaired motor activity) • agnosia (failure to recognize and identify objects) • disturbance in executive functioning (ie. planning, organizing, sequencing, abstracting 3. The course is gradual and continuing decline
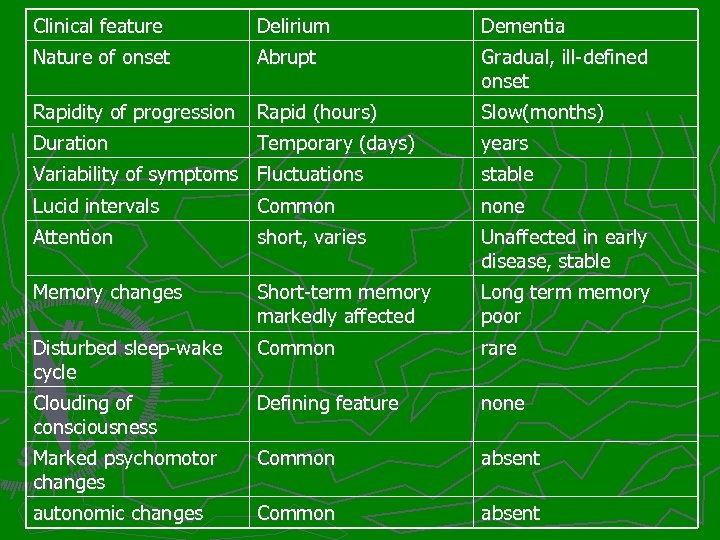
Clinical feature Delirium Dementia Nature of onset Abrupt Gradual, ill-defined onset Rapidity of progression Rapid (hours) Slow(months) Duration years Temporary (days) Variability of symptoms Fluctuations stable Lucid intervals Common none Attention short, varies Unaffected in early disease, stable Memory changes Short-term memory markedly affected Long term memory poor Disturbed sleep-wake cycle Common rare Clouding of consciousness Defining feature none Marked psychomotor changes Common absent autonomic changes Common absent
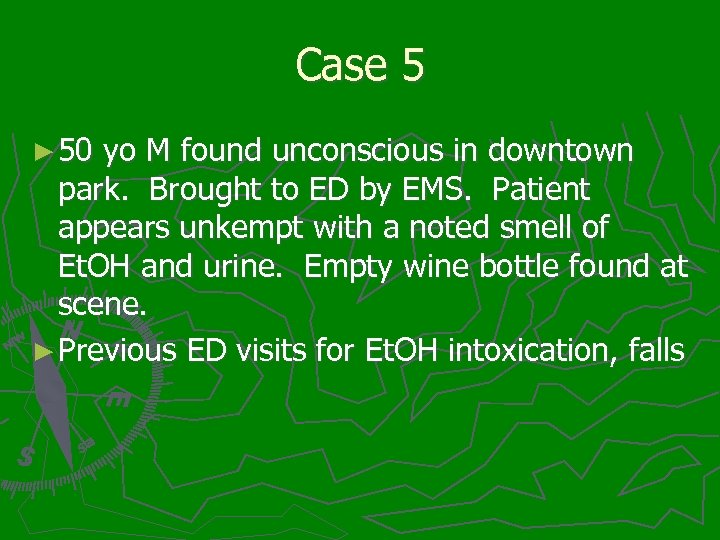
Case 5 ► 50 yo M found unconscious in downtown park. Brought to ED by EMS. Patient appears unkempt with a noted smell of Et. OH and urine. Empty wine bottle found at scene. ► Previous ED visits for Et. OH intoxication, falls
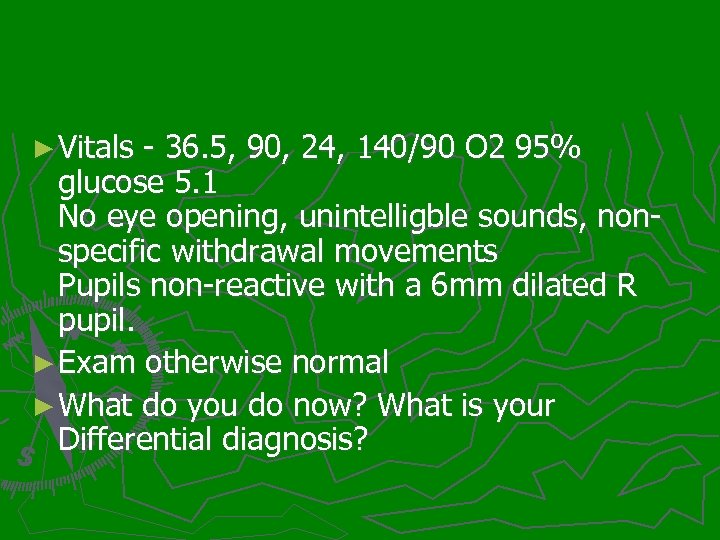
► Vitals - 36. 5, 90, 24, 140/90 O 2 95% glucose 5. 1 No eye opening, unintelligble sounds, nonspecific withdrawal movements Pupils non-reactive with a 6 mm dilated R pupil. ► Exam otherwise normal ► What do you do now? What is your Differential diagnosis?
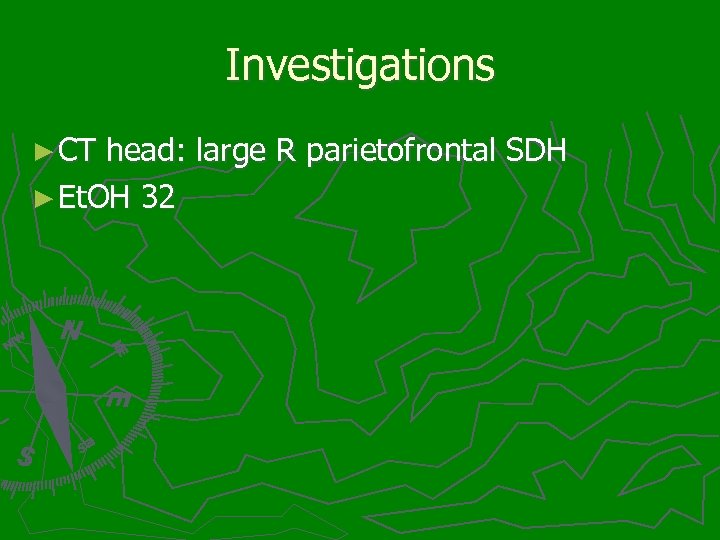
Investigations ► CT head: large R parietofrontal SDH ► Et. OH 32
References: ► Rosen’s ► EM clinics of NA: Volume 28, Issue 3, Pages 439 -718 (August 2010). Alterations of Consciousness in the Emergency Department ► Others as noted in presenter’s notes
948621d4c9dfdd9cba545a4e25281c47.ppt