DOC-20160607-WA0002.pptx
- Количество слайдов: 33
 Aplastic anaemias
Aplastic anaemias
 Anaemia is a disorder with haemoglobin level and/or RBC reduction. Women 120 g/l or 36%. Men 130 g/l or 40%.
Anaemia is a disorder with haemoglobin level and/or RBC reduction. Women 120 g/l or 36%. Men 130 g/l or 40%.
 Clinical manifestations of anaemias Compensatory mechanisms: pallor, tachycardia, shortness of breath, Dyspnea, other signs of cardiovascular insufficiency. Tissue hypoxia: weakness, high fatiguability, headache dizziness
Clinical manifestations of anaemias Compensatory mechanisms: pallor, tachycardia, shortness of breath, Dyspnea, other signs of cardiovascular insufficiency. Tissue hypoxia: weakness, high fatiguability, headache dizziness
 Erythropoiesis regulation O 2 concentration; erythropoietin; HIF; iron; hepcidin; Нb concentration in erythrocariocytes; Vitamin В 12, folic acid, etc
Erythropoiesis regulation O 2 concentration; erythropoietin; HIF; iron; hepcidin; Нb concentration in erythrocariocytes; Vitamin В 12, folic acid, etc
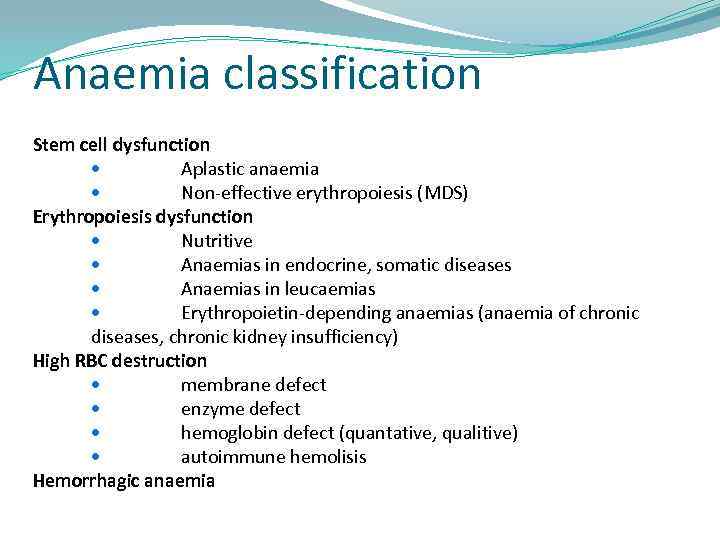 Anaemia classification Stem cell dysfunction Aplastic anaemia Non-effective erythropoiesis (МDS) Erythropoiesis dysfunction Nutritive Anaemias in endocrine, somatic diseases Anaemias in leucaemias Erythropoietin-depending anaemias (anaemia of chronic diseases, chronic kidney insufficiency) High RBC destruction membrane defect enzyme defect hemoglobin defect (quantative, qualitive) autoimmune hemolisis Hemorrhagic anaemia
Anaemia classification Stem cell dysfunction Aplastic anaemia Non-effective erythropoiesis (МDS) Erythropoiesis dysfunction Nutritive Anaemias in endocrine, somatic diseases Anaemias in leucaemias Erythropoietin-depending anaemias (anaemia of chronic diseases, chronic kidney insufficiency) High RBC destruction membrane defect enzyme defect hemoglobin defect (quantative, qualitive) autoimmune hemolisis Hemorrhagic anaemia
 Aplastic anaemia (АА) is a consequence of PPSC depression, when its' quantity lowens up to 1%, which leads to the bone marrow aplasia. Morphology: reduced marrow stem cells, increased fat spaces and pancytopenia in a blood film.
Aplastic anaemia (АА) is a consequence of PPSC depression, when its' quantity lowens up to 1%, which leads to the bone marrow aplasia. Morphology: reduced marrow stem cells, increased fat spaces and pancytopenia in a blood film.
 Epidemiology 2 -4 cases per 1 mln. population in USA and Europe In Thailand Japan – 11 -14 cases per 1 mln. population Age: 20 -25 years and upwards 60 years Statistically - no incidence difference between men and women
Epidemiology 2 -4 cases per 1 mln. population in USA and Europe In Thailand Japan – 11 -14 cases per 1 mln. population Age: 20 -25 years and upwards 60 years Statistically - no incidence difference between men and women
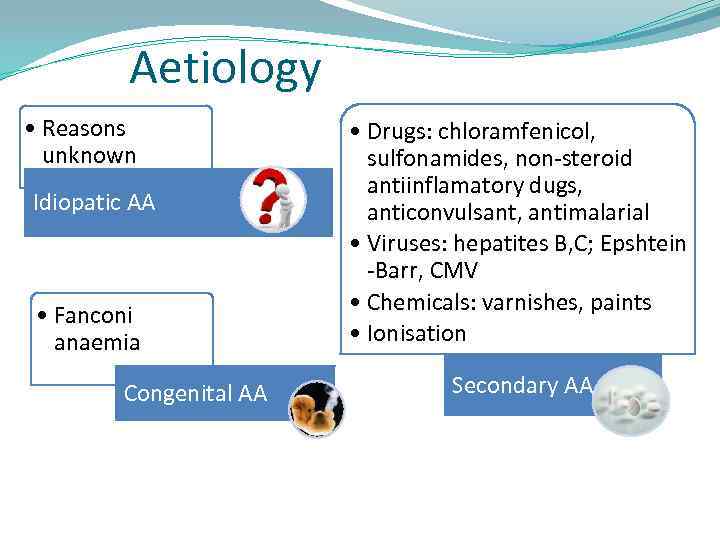 Aetiology • Reasons unknown Idiopatic АА • Fanconi anaemia Congenital АА • Drugs: chloramfenicol, sulfonamides, non-steroid antiinflamatory dugs, anticonvulsant, antimalarial • Viruses: hepatites В, С; Epshtein -Barr, CMV • Chemicals: varnishes, paints • Ionisation Secondary АА
Aetiology • Reasons unknown Idiopatic АА • Fanconi anaemia Congenital АА • Drugs: chloramfenicol, sulfonamides, non-steroid antiinflamatory dugs, anticonvulsant, antimalarial • Viruses: hepatites В, С; Epshtein -Barr, CMV • Chemicals: varnishes, paints • Ionisation Secondary АА
 Clinics Anaemia Hemorrhage Infections Lymphatic nodes, liver and spleen are not enlarged
Clinics Anaemia Hemorrhage Infections Lymphatic nodes, liver and spleen are not enlarged
 Course Acute - massive hemorrage severe infections lethal outcome in 3 -4 months Subacute weakness, fatigue later– hemorrage Chronic there is an identifiable cause recovery after aetiology factor is reduced
Course Acute - massive hemorrage severe infections lethal outcome in 3 -4 months Subacute weakness, fatigue later– hemorrage Chronic there is an identifiable cause recovery after aetiology factor is reduced
 Laboratory features Anaemia Leucopenia (absolute granulocyte number ) 500 -1000 WBC: average severity 200 -500: severe less than 200 cells: extremely severe Thrombocytopenia Histology: Fat spaces predominance in the bone marrow (trephine biopsy)
Laboratory features Anaemia Leucopenia (absolute granulocyte number ) 500 -1000 WBC: average severity 200 -500: severe less than 200 cells: extremely severe Thrombocytopenia Histology: Fat spaces predominance in the bone marrow (trephine biopsy)
 Differential diagnosis Acute leuacemia Megaloblastic anaemia Primary myelofibrosis Hypersplenism MDS
Differential diagnosis Acute leuacemia Megaloblastic anaemia Primary myelofibrosis Hypersplenism MDS
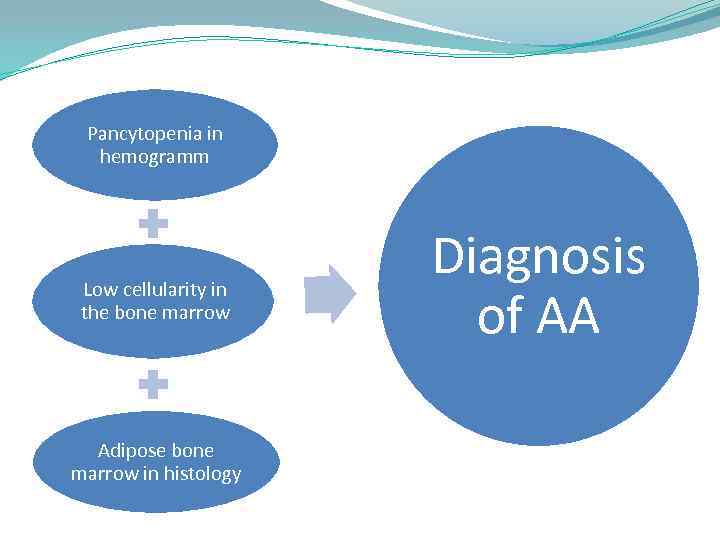 Pancytopenia in hemogramm Low cellularity in the bone marrow Adipose bone marrow in histology Diagnosis of АА
Pancytopenia in hemogramm Low cellularity in the bone marrow Adipose bone marrow in histology Diagnosis of АА
 Histology
Histology
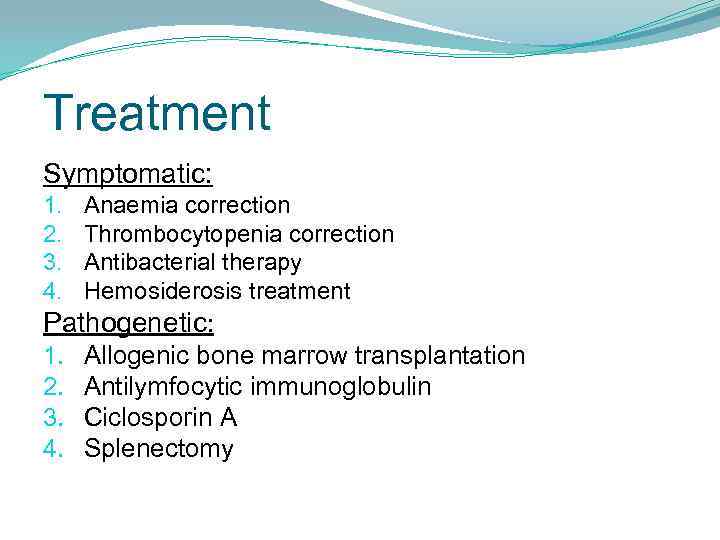 Treatment Symptomatic: 1. 2. 3. 4. Anaemia correction Thrombocytopenia correction Antibacterial therapy Hemosiderosis treatment Pathogenetic: 1. 2. 3. 4. Allogenic bone marrow transplantation Antilymfocytic immunoglobulin Ciclosporin А Splenectomy
Treatment Symptomatic: 1. 2. 3. 4. Anaemia correction Thrombocytopenia correction Antibacterial therapy Hemosiderosis treatment Pathogenetic: 1. 2. 3. 4. Allogenic bone marrow transplantation Antilymfocytic immunoglobulin Ciclosporin А Splenectomy
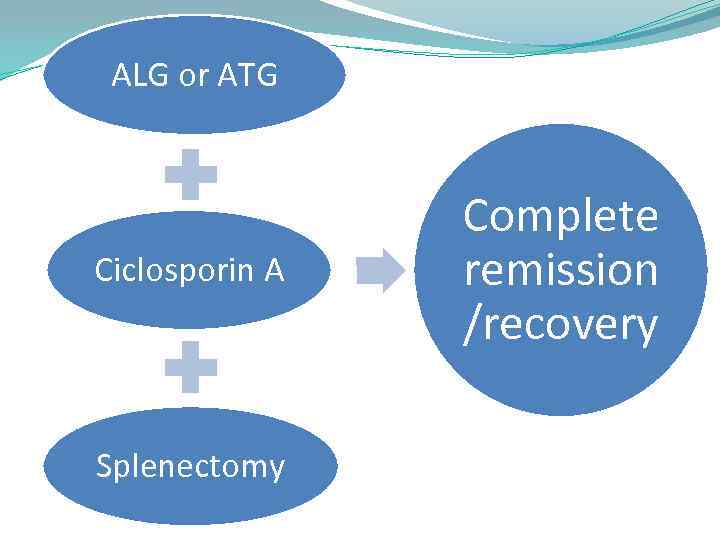 ALG or ATG Ciclosporin А Splenectomy Complete remission /recovery
ALG or ATG Ciclosporin А Splenectomy Complete remission /recovery
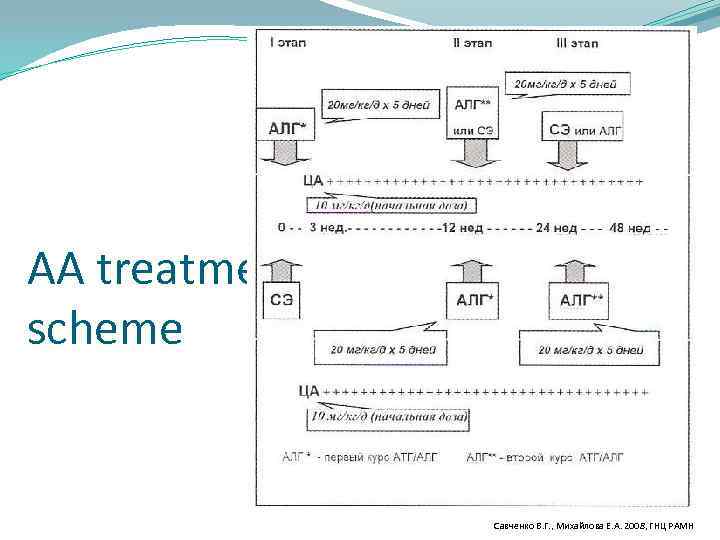 AA treatment scheme Савченко В. Г. , Михайлова Е. А. 2008, ГНЦ РАМН
AA treatment scheme Савченко В. Г. , Михайлова Е. А. 2008, ГНЦ РАМН
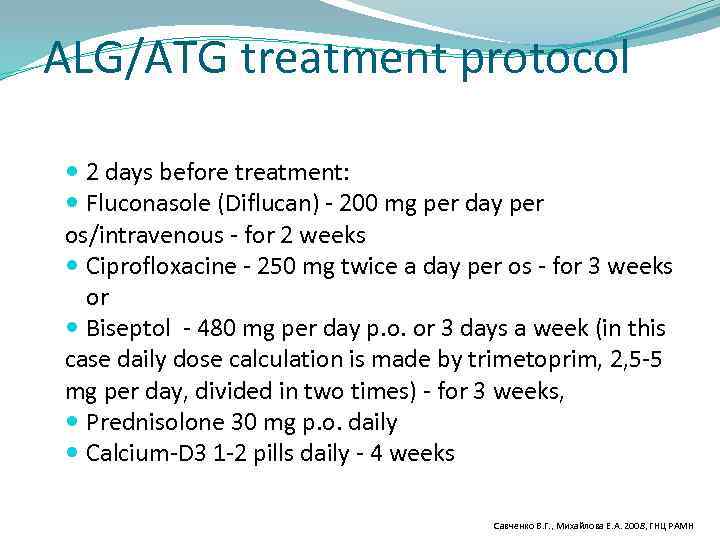 ALG/ATG treatment protocol 2 days before treatment: Fluconasole (Diflucan) - 200 mg per day per os/intravenous - for 2 weeks Ciprofloxacine - 250 mg twice a day per os - for 3 weeks or Biseptol - 480 mg per day p. o. or 3 days a week (in this case daily dose calculation is made by trimetoprim, 2, 5 -5 mg per day, divided in two times) - for 3 weeks, Prednisolone 30 mg p. o. daily Calcium-D 3 1 -2 pills daily - 4 weeks Савченко В. Г. , Михайлова Е. А. 2008, ГНЦ РАМН
ALG/ATG treatment protocol 2 days before treatment: Fluconasole (Diflucan) - 200 mg per day per os/intravenous - for 2 weeks Ciprofloxacine - 250 mg twice a day per os - for 3 weeks or Biseptol - 480 mg per day p. o. or 3 days a week (in this case daily dose calculation is made by trimetoprim, 2, 5 -5 mg per day, divided in two times) - for 3 weeks, Prednisolone 30 mg p. o. daily Calcium-D 3 1 -2 pills daily - 4 weeks Савченко В. Г. , Михайлова Е. А. 2008, ГНЦ РАМН
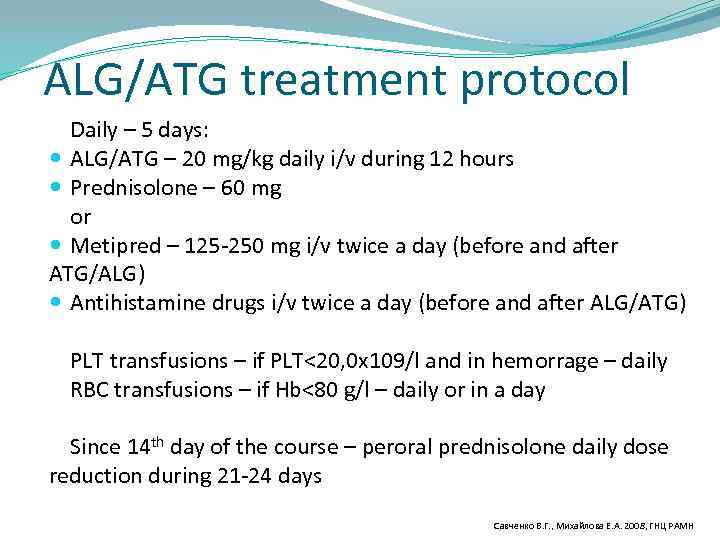 ALG/ATG treatment protocol Daily – 5 days: ALG/ATG – 20 mg/kg daily i/v during 12 hours Prednisolone – 60 mg or Metipred – 125 -250 mg i/v twice a day (before and after ATG/ALG) Antihistamine drugs i/v twice a day (before and after ALG/ATG) PLT transfusions – if PLT<20, 0 x 109/l and in hemorrage – daily RBC transfusions – if Hb<80 g/l – daily or in a day Since 14 th day of the course – peroral prednisolone daily dose reduction during 21 -24 days Савченко В. Г. , Михайлова Е. А. 2008, ГНЦ РАМН
ALG/ATG treatment protocol Daily – 5 days: ALG/ATG – 20 mg/kg daily i/v during 12 hours Prednisolone – 60 mg or Metipred – 125 -250 mg i/v twice a day (before and after ATG/ALG) Antihistamine drugs i/v twice a day (before and after ALG/ATG) PLT transfusions – if PLT<20, 0 x 109/l and in hemorrage – daily RBC transfusions – if Hb<80 g/l – daily or in a day Since 14 th day of the course – peroral prednisolone daily dose reduction during 21 -24 days Савченко В. Г. , Михайлова Е. А. 2008, ГНЦ РАМН
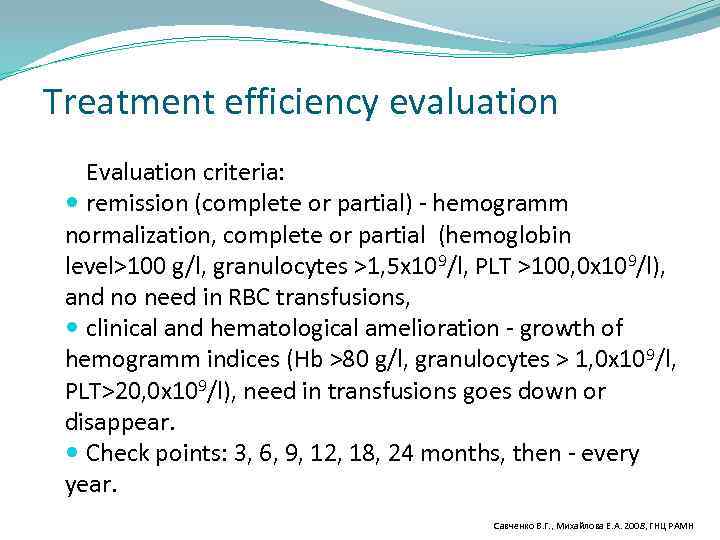 Treatment efficiency evaluation Evaluation criteria: remission (complete or partial) - hemogramm normalization, complete or partial (hemoglobin level>100 g/l, granulocytes >1, 5 x 109/l, PLT >100, 0 x 109/l), and no need in RBC transfusions, clinical and hematological amelioration - growth of hemogramm indices (Hb >80 g/l, granulocytes > 1, 0 x 109/l, PLT>20, 0 x 109/l), need in transfusions goes down or disappear. Check points: 3, 6, 9, 12, 18, 24 months, then - every year. Савченко В. Г. , Михайлова Е. А. 2008, ГНЦ РАМН
Treatment efficiency evaluation Evaluation criteria: remission (complete or partial) - hemogramm normalization, complete or partial (hemoglobin level>100 g/l, granulocytes >1, 5 x 109/l, PLT >100, 0 x 109/l), and no need in RBC transfusions, clinical and hematological amelioration - growth of hemogramm indices (Hb >80 g/l, granulocytes > 1, 0 x 109/l, PLT>20, 0 x 109/l), need in transfusions goes down or disappear. Check points: 3, 6, 9, 12, 18, 24 months, then - every year. Савченко В. Г. , Михайлова Е. А. 2008, ГНЦ РАМН
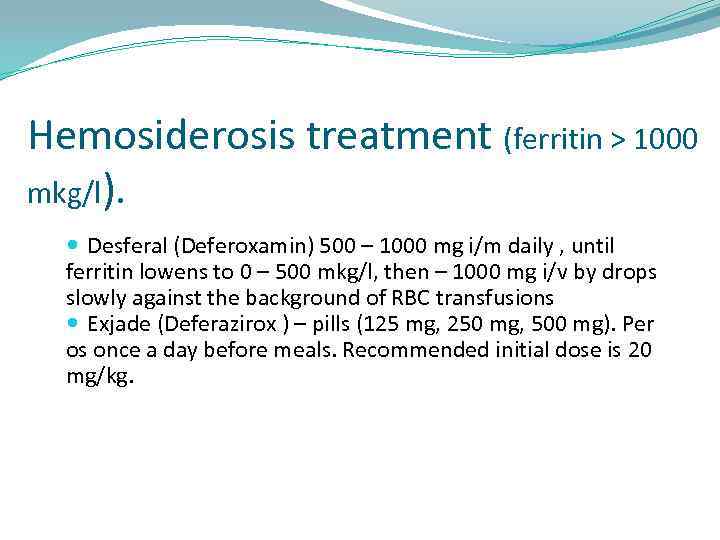 Hemosiderosis treatment (ferritin > 1000 mkg/l). Desferal (Deferoxamin) 500 – 1000 mg i/m daily , until ferritin lowens to 0 – 500 mkg/l, then – 1000 mg i/v by drops slowly against the background of RBC transfusions Exjade (Deferazirox ) – pills (125 mg, 250 mg, 500 mg). Per os once a day before meals. Recommended initial dose is 20 mg/kg.
Hemosiderosis treatment (ferritin > 1000 mkg/l). Desferal (Deferoxamin) 500 – 1000 mg i/m daily , until ferritin lowens to 0 – 500 mkg/l, then – 1000 mg i/v by drops slowly against the background of RBC transfusions Exjade (Deferazirox ) – pills (125 mg, 250 mg, 500 mg). Per os once a day before meals. Recommended initial dose is 20 mg/kg.
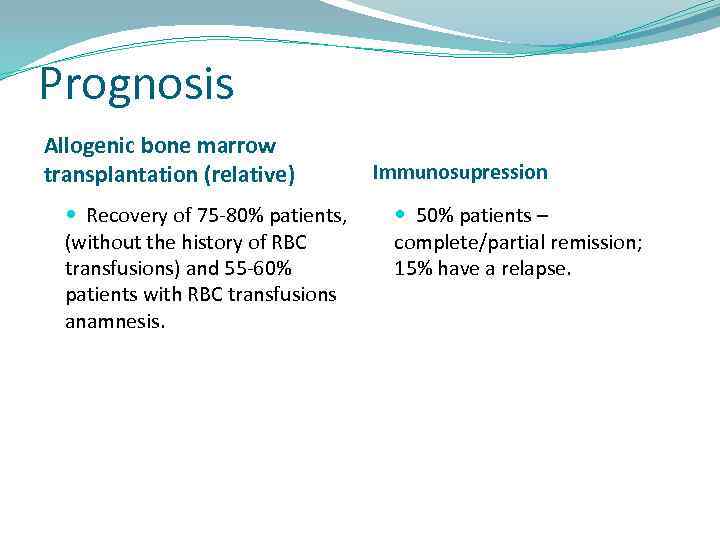 Prognosis Allogenic bone marrow transplantation (relative) Recovery of 75 -80% patients, (without the history of RBC transfusions) and 55 -60% patients with RBC transfusions anamnesis. Immunosupression 50% patients – complete/partial remission; 15% have a relapse.
Prognosis Allogenic bone marrow transplantation (relative) Recovery of 75 -80% patients, (without the history of RBC transfusions) and 55 -60% patients with RBC transfusions anamnesis. Immunosupression 50% patients – complete/partial remission; 15% have a relapse.
 Pure RBC aplasia (PRCA) Can be a nosology or a syndrome Severe normochromic anaemia with low reticulocytes level Pure RBC aplasia in a bone marrow: absence or severe reduction of eryhrocariocytes without its complete hypoplasia High serum iron concentration Hemosiderosis of organs and skin Need for RBC transfusions
Pure RBC aplasia (PRCA) Can be a nosology or a syndrome Severe normochromic anaemia with low reticulocytes level Pure RBC aplasia in a bone marrow: absence or severe reduction of eryhrocariocytes without its complete hypoplasia High serum iron concentration Hemosiderosis of organs and skin Need for RBC transfusions
 PRCA I. Congenital form – Diamond-Blackfan anaemia II. Acquired forms: A. Primary 1. autoimmune 2. preleuacemia 3. idiopathic В. Secondary form combined with thymoma, hemoblastoses, sold neoplasms, infections (human parvovirus В 19, HIV, infectious mononucleosis, viral hepatites, parotitis, cytomegalovirus, atypic pneumonia, meningococcemia, leishmaniosis) 5. Chronic hemolytic anaemias 6. Collagenoses – vasculites (lupus erythematosus, rheumatoid arthritis, mixed deseases of connective tissue) 7. Drugs, chemicals 8. Pregnancy 9. Severe chronic kidney insufficiency 10. Malnutrition 11. Different After АВО – incompatible bone marrow transplantation, autoimmune hypothyroidism, autoimmune chronic hepatitis, anti-erythropoietin antibodies while treatment with erythropoietin.
PRCA I. Congenital form – Diamond-Blackfan anaemia II. Acquired forms: A. Primary 1. autoimmune 2. preleuacemia 3. idiopathic В. Secondary form combined with thymoma, hemoblastoses, sold neoplasms, infections (human parvovirus В 19, HIV, infectious mononucleosis, viral hepatites, parotitis, cytomegalovirus, atypic pneumonia, meningococcemia, leishmaniosis) 5. Chronic hemolytic anaemias 6. Collagenoses – vasculites (lupus erythematosus, rheumatoid arthritis, mixed deseases of connective tissue) 7. Drugs, chemicals 8. Pregnancy 9. Severe chronic kidney insufficiency 10. Malnutrition 11. Different After АВО – incompatible bone marrow transplantation, autoimmune hypothyroidism, autoimmune chronic hepatitis, anti-erythropoietin antibodies while treatment with erythropoietin.
 PRCA - treatment 1 st variant (“benign”) – immunosuppression leads to erythropoiesis recovery (autoimmune hemolytic anaemia – PRCA). In another variant a neoplasm from blocked cells (erythricariocytes) always develops – erythroblastic leuacemia. PRCA can be cured with immunosupression, but a disease, combined with it (lymphoma, CLL, TСD 8 -CLL) stays the same.
PRCA - treatment 1 st variant (“benign”) – immunosuppression leads to erythropoiesis recovery (autoimmune hemolytic anaemia – PRCA). In another variant a neoplasm from blocked cells (erythricariocytes) always develops – erythroblastic leuacemia. PRCA can be cured with immunosupression, but a disease, combined with it (lymphoma, CLL, TСD 8 -CLL) stays the same.
 MDS - clonal hematological disease characterised with uneffectice hemopoiesis (apoptosed cells quantity rises). Common signs: Cytopenia Dysmyelopoiesis Often transformation to AL (up to 30%)
MDS - clonal hematological disease characterised with uneffectice hemopoiesis (apoptosed cells quantity rises). Common signs: Cytopenia Dysmyelopoiesis Often transformation to AL (up to 30%)
 MDS Cytopenia considered severe in Нb level < 100 g/l, PLT< 100 thous. , neutroph < 1, 5 thous. Cytogenetics: 5 q-, y-, 20 q- – good prognosis; 7 th chromosome breaks, complex anomalies (more than 3) – unfavorable. Risk groups: Low – median survival 5 – 7 years; Intermediate – 3 – 5 years; Intermediate – 1 – 2 years; High – 5 months.
MDS Cytopenia considered severe in Нb level < 100 g/l, PLT< 100 thous. , neutroph < 1, 5 thous. Cytogenetics: 5 q-, y-, 20 q- – good prognosis; 7 th chromosome breaks, complex anomalies (more than 3) – unfavorable. Risk groups: Low – median survival 5 – 7 years; Intermediate – 3 – 5 years; Intermediate – 1 – 2 years; High – 5 months.
 MDS - Diagnosis of exclusion - Differential diagnosis: megaloblastic anaemias, АА, PNH, autoimmune hemolytic anaemia, Fisher. Evance syndrome, AL, viral hepatites, HIV, SLE, lymphoproliferative diseases, tbs, Cr …. .
MDS - Diagnosis of exclusion - Differential diagnosis: megaloblastic anaemias, АА, PNH, autoimmune hemolytic anaemia, Fisher. Evance syndrome, AL, viral hepatites, HIV, SLE, lymphoproliferative diseases, tbs, Cr …. .
 MDS classification RA (refractory anaemia) - anaemia in the bone marrow: dyserythropoiesis , < 5% of blasts, < 15% of ring sideroblasts; RA with ring sideroblasts - anaemia, in the bone marrow: dyserythropoiesis , < 5% of blasts, > 15% of ring sideroblasts; Refractory cytopenia with multilinear dysplasia – cytopenia, in the bone marrow: dyserythropoiesis , < 5% of blasts, < 15% of ring sideroblasts; Refractory cytopenia with multilinear dysplasia with ring sideroblasts; RAEB-1 (refractory anaemia with an excess of blasts), blasts 5 -9%; RAEB-2 (blasts 10 -20%); MDS non-classified; 5 q – syndrome – anaemia, thrombocytosis, in the bone marrow: dyserythropoiesis , < 5% of blasts,
MDS classification RA (refractory anaemia) - anaemia in the bone marrow: dyserythropoiesis , < 5% of blasts, < 15% of ring sideroblasts; RA with ring sideroblasts - anaemia, in the bone marrow: dyserythropoiesis , < 5% of blasts, > 15% of ring sideroblasts; Refractory cytopenia with multilinear dysplasia – cytopenia, in the bone marrow: dyserythropoiesis , < 5% of blasts, < 15% of ring sideroblasts; Refractory cytopenia with multilinear dysplasia with ring sideroblasts; RAEB-1 (refractory anaemia with an excess of blasts), blasts 5 -9%; RAEB-2 (blasts 10 -20%); MDS non-classified; 5 q – syndrome – anaemia, thrombocytosis, in the bone marrow: dyserythropoiesis , < 5% of blasts,
 CMML According to FAB CMML is in an MDS group, according to WHO, russian claasification – is a separate form. Classification: CMML–MDS – MDS signs, leu < 12 thous. , monocytosis > 1 thous. ; CMML – MPD – leu > 12 thous. , monocytosis > 1 thous. ; CMML-1 – blasts in the BM< 5%; CMML-2 – blasts in the BM 5 -19%.
CMML According to FAB CMML is in an MDS group, according to WHO, russian claasification – is a separate form. Classification: CMML–MDS – MDS signs, leu < 12 thous. , monocytosis > 1 thous. ; CMML – MPD – leu > 12 thous. , monocytosis > 1 thous. ; CMML-1 – blasts in the BM< 5%; CMML-2 – blasts in the BM 5 -19%.
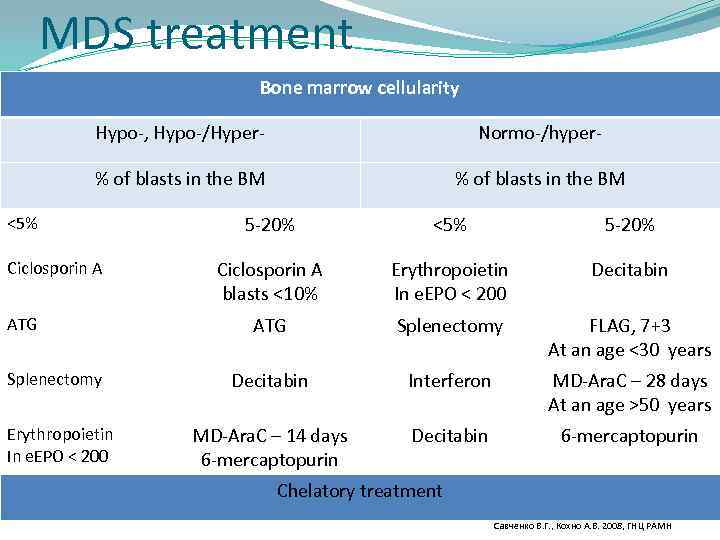 MDS treatment Bone marrow cellularity Hypo-, Hypo-/Hyper- Normo-/hyper- % of blasts in the BM <5% Ciclosporin A ATG Splenectomy Erythropoietin In e. EPO < 200 5 -20% <5% 5 -20% Ciclosporin A blasts <10% Erythropoietin In e. EPO < 200 Decitabin ATG Splenectomy FLAG, 7+3 At an age <30 years Decitabin Interferon MD-Ara. C – 28 days At an age >50 years MD-Ara. C – 14 days 6 -mercaptopurin Decitabin 6 -mercaptopurin Chelatory treatment Савченко В. Г. , Кохно А. В. 2008, ГНЦ РАМН
MDS treatment Bone marrow cellularity Hypo-, Hypo-/Hyper- Normo-/hyper- % of blasts in the BM <5% Ciclosporin A ATG Splenectomy Erythropoietin In e. EPO < 200 5 -20% <5% 5 -20% Ciclosporin A blasts <10% Erythropoietin In e. EPO < 200 Decitabin ATG Splenectomy FLAG, 7+3 At an age <30 years Decitabin Interferon MD-Ara. C – 28 days At an age >50 years MD-Ara. C – 14 days 6 -mercaptopurin Decitabin 6 -mercaptopurin Chelatory treatment Савченко В. Г. , Кохно А. В. 2008, ГНЦ РАМН
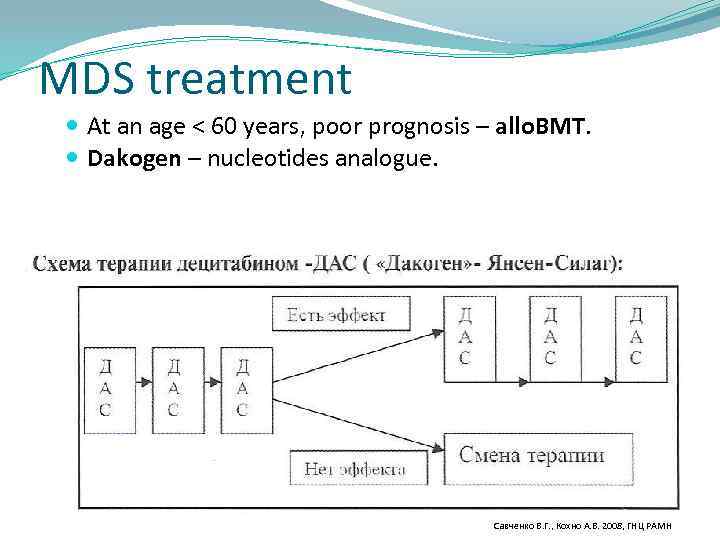 MDS treatment At an age < 60 years, poor prognosis – аllo. BMT. Dakogen – nucleotides analogue. Савченко В. Г. , Кохно А. В. 2008, ГНЦ РАМН
MDS treatment At an age < 60 years, poor prognosis – аllo. BMT. Dakogen – nucleotides analogue. Савченко В. Г. , Кохно А. В. 2008, ГНЦ РАМН
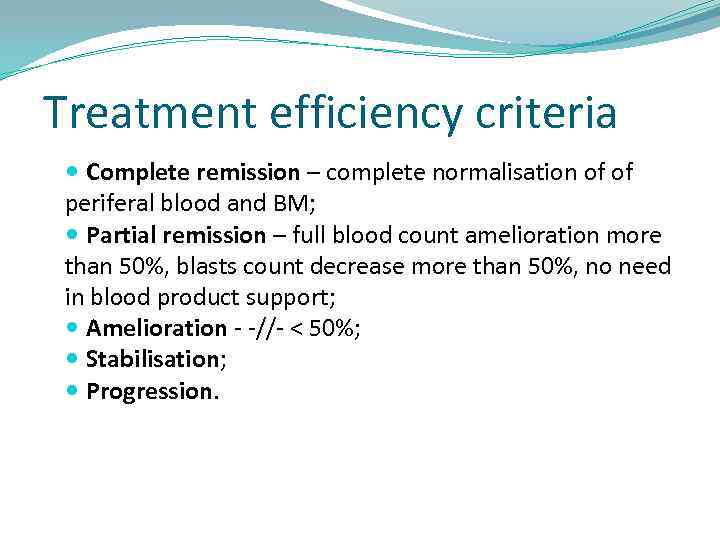 Treatment efficiency criteria Complete remission – complete normalisation of of periferal blood and BM; Partial remission – full blood count amelioration more than 50%, blasts count decrease more than 50%, no need in blood product support; Amelioration - -//- < 50%; Stabilisation; Progression.
Treatment efficiency criteria Complete remission – complete normalisation of of periferal blood and BM; Partial remission – full blood count amelioration more than 50%, blasts count decrease more than 50%, no need in blood product support; Amelioration - -//- < 50%; Stabilisation; Progression.


