9eb8fcd677ae4460765270b590f71da6.ppt
- Количество слайдов: 64
APC/OPPS Update for CY 2016 Sponsored By: APCNow www. APCNow. com Presented By: Duane C. Abbey, Ph. D. , CFP Abbey & Abbey, Consultants, Inc. Duane@aaciweb. com http: //www. APCNow. com http: //www. HIPAAMaster. com Version 17 - Generic Notes © 1994 -2016, Abbey & Abbey, Consultants, Inc. CPT® Codes – © 2014 -2016 AMA © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 1
Presentation Faculty Duane C. Abbey, Ph. D. , CFP – Dr. Abbey is a healthcare consultant and educator with over 20 years of experience. He has worked with hospitals, clinics, physicians in various specialties, home health agencies and other health care providers. His primary work is with optimizing reimbursement under various Prospective Payment Systems. He also works extensively with various compliance issues and performs chargemaster reviews along with coding and billing audits. Dr. Abbey is the President of Abbey & Abbey, Consultants, Inc. A wide range of consulting services is provided across the country including charge master reviews, APC compliance reviews, in-service training, physician training, and coding and billing reviews. Dr. Abbey is the author of fourteen books on health care, including: • “Non-Physician Providers: Guide to Coding, Billing, and Reimbursement” • “Emergency Department: Coding, Billing and Reimbursement”, and • “Chargemasters: Strategies to Ensure Accurate Reimbursement and Compliance”. Recent books include: “Compliance for Coding, Billing & Reimbursement A Systematic Approach to Developing a Comprehensive Program”, “Introduction to Healthcare Payment Systems”, “Fee Schedule Payment Systems” and “Prospective Payment Systems” from Taylor and Francis. He has just finished the fourth book in the Healthcare Payment System Series; “Cost-Based, Charge-Based and Contractual Payment Systems”. © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 2
Disclaimer This workshop and other material provided are designed to provide accurate and authoritative information. The authors, presenters and sponsors have made every reasonable effort to ensure the accuracy of the information provided in this workshop material. However, all appropriate sources should be verified for the correct ICD-9 -CM Codes, ICD-10 -CM Diagnosis Codes, ICD-10 -PCS Procedure Codes, CPT/HCPCS Codes and Revenue Center Codes. The user is ultimately responsible for correct coding and billing. The author and presenters are not liable and make no guarantee or warranty; either expressed or implied, that the information compiled or presented is errorfree. All users need to verify information with the Fiscal Intermediary, Carriers, other third party payers, and the various directives and memorandums issued by CMS, DOJ, OIG and associated state and federal governmental agencies. The user assumes all risk and liability with the use and/or misuse of this information. © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 3
OPPS Final Update for CY 2016 Objectives Ø To review the many proposed and finalized changes to APCs for 2016. Ø To recognize the general trends for APCs with particular attention to increased bundling. Ø To understand how recent changes in the cost reporting process affect APCs payments. Ø To understand the complex nature of APCs and associated compliance issues including RAC concerns. Ø To review changes in grouping with particular attention to new CPT and HCPCS codes. Ø To appreciate the potential financial and operational impact of the proposed changes. Ø To understand how important it is for hospitals to comment to the proposed changes. Ø To understand the difference between composite and comprehensive APCs. Ø To review the possible impact of the proposed change on high impact areas such as observation, the Emergency Department, interventional radiology and associated areas. Ø To review changes to and trends for the Provider-Based Rule (PBR). Ø To discuss anticipated future changes and directions for APCs. © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 4
OPPS Final Update for CY 2016 Acronyms/Terminology Ø Ø Ø Ø APCs – Ambulatory Payment Classifications APGs – Ambulatory Patient Groups ASC – Ambulatory Surgical Center CAH – Critical Access Hospital CCRs – Cost-to-Charge Ratios CPT – Current Procedural Terminology E/M – Evaluation and Management FFS – Fee-for-Service HCPCS – Healthcare Common Procedure Coding System ICD-9 -CM – International Classification of Diseases, Ninth Edition, Clinical MAC – Medicare Administrative Contractor Med. PAC – Medicare Advisory Commission MPFS – Medicare Physician Fee Schedule NCCI – National Correct Coding Initiative AWV – Annual Well Visit PPPS – Personalized Preventive Plan Services © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 5
OPPS Final Update for CY 2016 Acronyms/Terminology Ø Ø Ø Ø NCD/LCD – National/Local Coverage Decision NTIOL –New Technology Intraocular Lens OCE – Outpatient Code Editor OPD – [Hospital] Outpatient Department OPPS – [Hospital] Outpatient Prospective Payment System PHP – Partial Hospitalization Program PM – Program Memorandum PPS – Prospective Payment System QIO – Quality Improvement Organization SI – Status Indicator ASC – Ambulatory Surgical Center RBRVS – Resource Based Relative Value System MPFS – Medicare Physician Fee Schedule Developed through RBRVS VBP – Value Based Purchasing PCR – Payment to Cost Ratio § Note: The Federal Register entry has pages of acronyms! © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 6
OPPS Final Update for CY 2016 General Comments Ø APCs are becoming increasingly complex and more difficult to understand. § Enormous Federal Register entries are now the norm. Ø APCs represent a payment system that is experiencing significant changes each year. Ø Significantly increased bundling through packaging is still being added. § APCs appear to be moving back toward APGs. Ø There are wide variations in payments from year to year. Ø Significant compliance concerns exist within the overall APC payment system. § In some cases these compliance concerns result because of lack of explicit guidance from CMS. § At some point the RAC auditors will become more involved in APCs. Ø APCs and the underlying coding systems (i. e. , CPT and HCPCS) generate constant change and the need to be updated. Ø Tracking and verifying that correct payment is received is difficult. § It is critical to track adjudication and overall payment. Ø Major issues with hospital charges, CCRs and the cost report are present. § Federal Register Fanatics Look for how many times the word ‘believe’ is used by CMS. What are you allowed to ‘believe’? © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 7
OPPS Final Update for CY 2016 General Comments Ø Note: Citations to the Federal Register are to the November 13, 2016, 1633 F edition (yes, Friday the 13 th!) – 311 pages(!) Ø This Federal Register entry discusses a number of different topics. Not all the topics discussed necessarily relate to APCs (Ambulatory Payment Classifications). ASCs (Ambulatory Surgical Centers) are now paid under a hybrid payment system of APCs and MPFS (Medicare Physician Fee Schedule). Ø Here are some of the other issues discussed in this Federal Register. § Hospital Outpatient Prospective Payment and Ambulatory Surgical Center Payment Systems and Quality Reporting Programs; § Short Inpatient Hospital Stays; § Transition for Certain Medicare-Dependent, Small Rural Hospitals under the Hospital Inpatient Prospective Payment System; § Provider Administrative Appeals and Judicial Review Ø This is a final Federal Register entry, so there are very few topics for which comments can be made. Ø Also, be certain to download all the Addenda that are in compressed format. Particularly, Addendum A and Addendum B. Note also Addendum C for the Status Indicators that drive the APC grouping process. © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 8
OPPS Final Update for CY 2016 APC Background Information Ø APC Fundamentals § Encounter Driven System • Some Exceptions – Example: Two separate blood transfusions on the same day or two imaging services at different times on the same day. § CPT/HCPCS Code Driven • If the service is not coded with a CPT or HCPCS (and/or proper modifiers), then there will be absolutely no payment! § APC Grouper Multiple APCs from Given Claim § Inpatient-Only Procedures • Surgery, if performed outpatient, will not be paid at all! (Patient Liability? ) • How is this list determined? § Covered, Non-Covered and Payment System Interfaces • Example: Self-Administrable Drugs § Pass-Through Payments – Directly Based on Charges Made – Covert Charges to Costs How? (Hint: Cost-to-Charge Ratios) © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 9
OPPS Final Update for CY 2016 APC Background Information Ø APC Weight, and Thus Payment, Determination § Hospital Charges Converted to Costs • How is this done? • Do we charge for everything? • Do we charge correctly for everything? § Statistical Process Using the Costs • Geometric Mean • Mean Cost for Given APC/Mean Cost for All APCs = the APC Weight § Variation of Costs Within a Given APC Category • “ … we annually review the items and services within an APC group to determine, with respect to comparability of the use of resources, if the highest cost for an item or service in the APC group is more than 2 times greater than the lowest cost for an item or service within the same APC group (referred to as the “ 2 times rule”). ” (80 FR 70373) ü The list for this year is significantly shortened: o 5165 – Level 5 ENT Procedures o 5731 – Level 1 Minor Procedures o 5841 - Psychotherapy © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 10
OPPS Final Update for CY 2016 APC Background Information Ø Use of Claims to Statistically Develop the APC Weights § Because outpatient encounters often involve multiple services, the APC grouping process often (if not a majority of the time) generates multiple APCs. § CMS can use only pure claims, that is, claims that group to a single APC. These are called ‘singleton’ claims. § CMS is trying very hard to get around this situation because many of the claims filed by hospitals never get considered when the actual APC weights are determined. • Small Example: CPT=86891 – Intra- or Post-Operative Blood Salvage ü For CY 2016, APC=5674, SI=“Q 1” (STV-Packaged) o Payment is $440. 53 o CY 2015 $125. 07, CY 2012 $14. 95 o What is going on here? ü A device is used to save blood, reprocess the blood and generally re-infuse. ü Is it possible to have ONLY 86891 on a claim? ü What are the costs involved? © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 11
OPPS Final Update for CY 2016 APC Background Information Ø APC Cost Outliers § Complicated Two-Tiered Formula § Based on Excessive Costs - How are costs determined? § Nationally, does CMS make full outlier payments? Ø Provider-Based Rule (42 CFR § 413. 65) § Provider-Based Clinics § Provider-Based Clinical Services § Potentially, two claim forms filed – CMS-1450 (UB-04) for technical component and CMS-1500 (1500) for professional component. § Reduction in payment for professional component • Site-of-Service Differential in RBRVS (MPFS) • Place-of-Service (POS) driven on CMS-1500 § Series of Criteria to Meet If to be Provider-Based • On-Campus versus Off-Campus See New Reporting Requirements – “-PO” Modifier on UB-04 & POS=19/22 on the 1500 claim form. • See Physician Supervision Developments Important ü Changes in rules, regulations and interpretations. © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 12
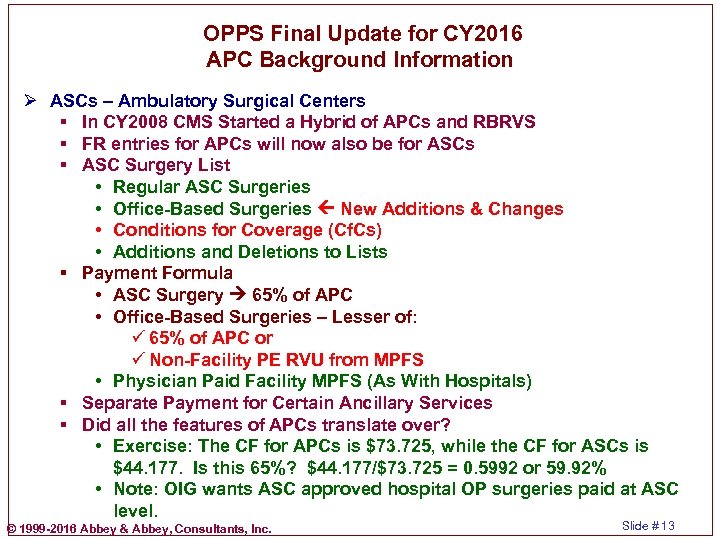
OPPS Final Update for CY 2016 APC Background Information Ø ASCs – Ambulatory Surgical Centers § In CY 2008 CMS Started a Hybrid of APCs and RBRVS § FR entries for APCs will now also be for ASCs § ASC Surgery List • Regular ASC Surgeries • Office-Based Surgeries New Additions & Changes • Conditions for Coverage (Cf. Cs) • Additions and Deletions to Lists § Payment Formula • ASC Surgery 65% of APC • Office-Based Surgeries – Lesser of: ü 65% of APC or ü Non-Facility PE RVU from MPFS • Physician Paid Facility MPFS (As With Hospitals) § Separate Payment for Certain Ancillary Services § Did all the features of APCs translate over? • Exercise: The CF for APCs is $73. 725, while the CF for ASCs is $44. 177. Is this 65%? $44. 177/$73. 725 = 0. 5992 or 59. 92% • Note: OIG wants ASC approved hospital OP surgeries paid at ASC level. © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 13
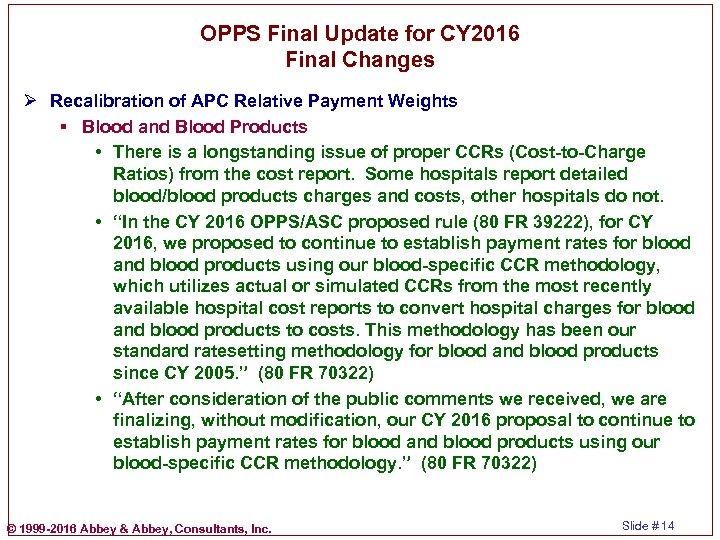
OPPS Final Update for CY 2016 Final Changes Ø Recalibration of APC Relative Payment Weights § Blood and Blood Products • There is a longstanding issue of proper CCRs (Cost-to-Charge Ratios) from the cost report. Some hospitals report detailed blood/blood products charges and costs, other hospitals do not. • “In the CY 2016 OPPS/ASC proposed rule (80 FR 39222), for CY 2016, we proposed to continue to establish payment rates for blood and blood products using our blood-specific CCR methodology, which utilizes actual or simulated CCRs from the most recently available hospital cost reports to convert hospital charges for blood and blood products to costs. This methodology has been our standard ratesetting methodology for blood and blood products since CY 2005. ” (80 FR 70322) • “After consideration of the public comments we received, we are finalizing, without modification, our CY 2016 proposal to continue to establish payment rates for blood and blood products using our blood-specific CCR methodology. ” (80 FR 70322) © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 14
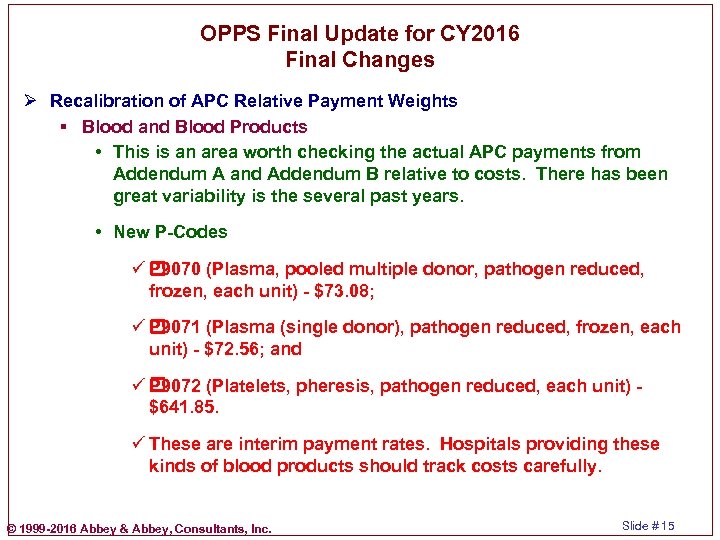
OPPS Final Update for CY 2016 Final Changes Ø Recalibration of APC Relative Payment Weights § Blood and Blood Products • This is an area worth checking the actual APC payments from Addendum A and Addendum B relative to costs. There has been great variability is the several past years. • New P-Codes ü P 9070 (Plasma, pooled multiple donor, pathogen reduced, frozen, each unit) - $73. 08; ü P 9071 (Plasma (single donor), pathogen reduced, frozen, each unit) - $72. 56; and ü P 9072 (Platelets, pheresis, pathogen reduced, each unit) - $641. 85. ü These are interim payment rates. Hospitals providing these kinds of blood products should track costs carefully. © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 15
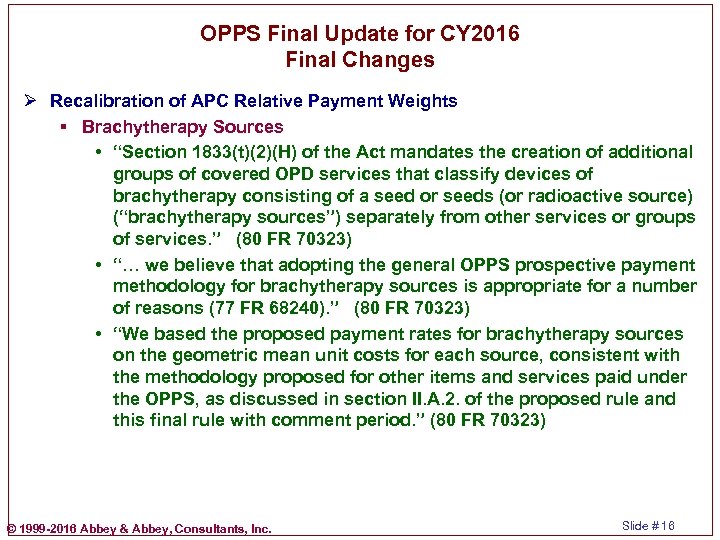
OPPS Final Update for CY 2016 Final Changes Ø Recalibration of APC Relative Payment Weights § Brachytherapy Sources • “Section 1833(t)(2)(H) of the Act mandates the creation of additional groups of covered OPD services that classify devices of brachytherapy consisting of a seed or seeds (or radioactive source) (“brachytherapy sources”) separately from other services or groups of services. ” (80 FR 70323) • “… we believe that adopting the general OPPS prospective payment methodology for brachytherapy sources is appropriate for a number of reasons (77 FR 68240). ” (80 FR 70323) • “We based the proposed payment rates for brachytherapy sources on the geometric mean unit costs for each source, consistent with the methodology proposed for other items and services paid under the OPPS, as discussed in section II. A. 2. of the proposed rule and this final rule with comment period. ” (80 FR 70323) © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 16
OPPS Final Update for CY 2016 Final Changes Ø Recalibration of APC Relative Payment Weights § Brachytherapy Sources • “As stated above, we believe that geometric mean costs based on hospital claims data for brachytherapy sources have produced reasonably consistent per-source cost estimates over the past several years, comparable to the patterns we have observed for many other OPPS services whose payments are set based upon relative payment weights from claims data. We believe that our persource payment methodology specific to each source’s radioisotope, radioactive intensity, and stranded or non-stranded configuration, supplemented by payment based on the number of sources used in a specific clinical case, adequately accounts for the major expected sources of variability across treatments. ” (80 FR 70324) • “Under the OPPS, it is the relativity of costs, not the absolute costs, that is important, and we believe that brachytherapy sources are appropriately paid according to the standard OPPS approach. (80 FR 70324) © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 17
OPPS Final Update for CY 2016 Final Changes Ø Recalibration of APC Relative Payment Weights § Brachytherapy Sources • “Therefore, when establishing charges for HDR iridium-192, we expect hospitals to project the number of treatments that would be provided over the life of the source and establish charges for the source accordingly. ” (80 FR 70324) • “We believe that some variation in relative cost from year to year is to be expected in a prospective payment system, particularly for low-volume items. ” (80 FR 70325) ü Why does CMS break out this discussion about payments for brachytherapy sources? ü How is CMS ‘supposed’ to be paying form brachytherapy sources. © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 18
OPPS Final Update for CY 2016 Final Changes Ø Recalibration of APC Relative Payment Weights § Establishment of Comprehensive APCs • “In the CY 2014 OPPS/ASC final rule with comment period (78 FR 74861 through 74910), we finalized a comprehensive payment policy that packages payment for adjunctive and secondary items, services, and procedures into the most costly primary procedure under the OPPS at the claim level. The policy was finalized in CY 2014, but the effective date was delayed until January 1, 2015, to allow additional time for further analysis, opportunity for public comment, and systems preparation. The comprehensive APC (CAPC) policy was implemented effective January 1, 2015, with modifications and clarifications in response to public comments received regarding specific provisions of the C-APC policy (79 FR 66798 through 66810). ” (80 FR 70325) • “Payments for adjunctive services are packaged into the payments for the primary services. This results in a single prospective payment for each of the primary, comprehensive services based on the costs of all reported services at the claim level. ” (80 FR 70326) © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 19
OPPS Final Update for CY 2016 Final Changes Ø Recalibration of APC Relative Payment Weights § Comprehensive APCs • “Under this policy, we designated a HCPCS code assigned to a CAPC as the primary service (identified by a new OPPS status indicator “J 1”). ” • See the related concept of “Significant Procedure Consolidation” from APGs (Ambulatory Patient Groups). • See also the NCCI Edit Coding Policy Manual for information concerning integral part and coding edits. • What is excluded from the C-APCs? ü Non-Covered Services ü Services that must be paid separately (e. g. , mammography, ambulance, brachytherapy, self-administered drugs, items paid on a cost pass-through basis. © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 20
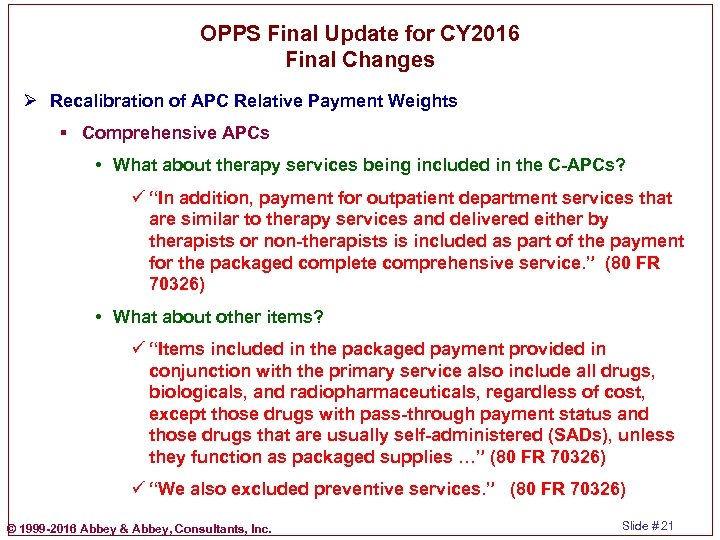
OPPS Final Update for CY 2016 Final Changes Ø Recalibration of APC Relative Payment Weights § Comprehensive APCs • What about therapy services being included in the C-APCs? ü “In addition, payment for outpatient department services that are similar to therapy services and delivered either by therapists or non-therapists is included as part of the payment for the packaged complete comprehensive service. ” (80 FR 70326) • What about other items? ü “Items included in the packaged payment provided in conjunction with the primary service also include all drugs, biologicals, and radiopharmaceuticals, regardless of cost, except those drugs with pass-through payment status and those drugs that are usually self-administered (SADs), unless they function as packaged supplies …” (80 FR 70326) ü “We also excluded preventive services. ” (80 FR 70326) © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 21
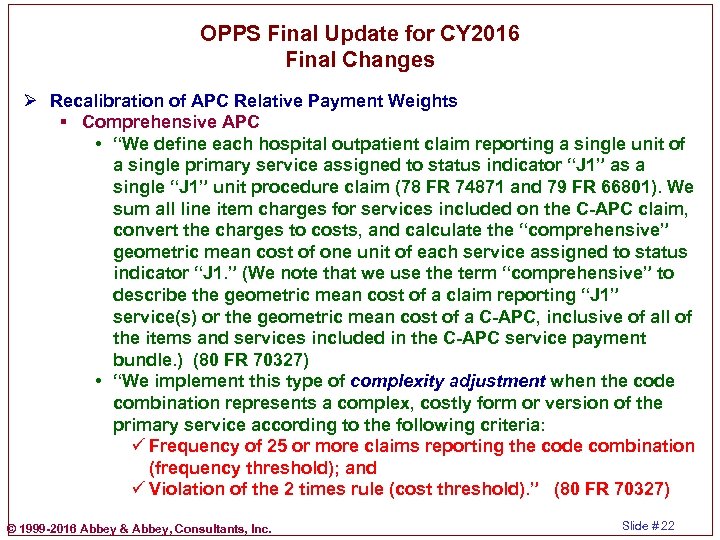
OPPS Final Update for CY 2016 Final Changes Ø Recalibration of APC Relative Payment Weights § Comprehensive APC • “We define each hospital outpatient claim reporting a single unit of a single primary service assigned to status indicator “J 1” as a single “J 1” unit procedure claim (78 FR 74871 and 79 FR 66801). We sum all line item charges for services included on the C-APC claim, convert the charges to costs, and calculate the “comprehensive” geometric mean cost of one unit of each service assigned to status indicator “J 1. ” (We note that we use the term “comprehensive” to describe the geometric mean cost of a claim reporting “J 1” service(s) or the geometric mean cost of a C-APC, inclusive of all of the items and services included in the C-APC service payment bundle. ) (80 FR 70327) • “We implement this type of complexity adjustment when the code combination represents a complex, costly form or version of the primary service according to the following criteria: ü Frequency of 25 or more claims reporting the code combination (frequency threshold); and ü Violation of the 2 times rule (cost threshold). ” (80 FR 70327) © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 22
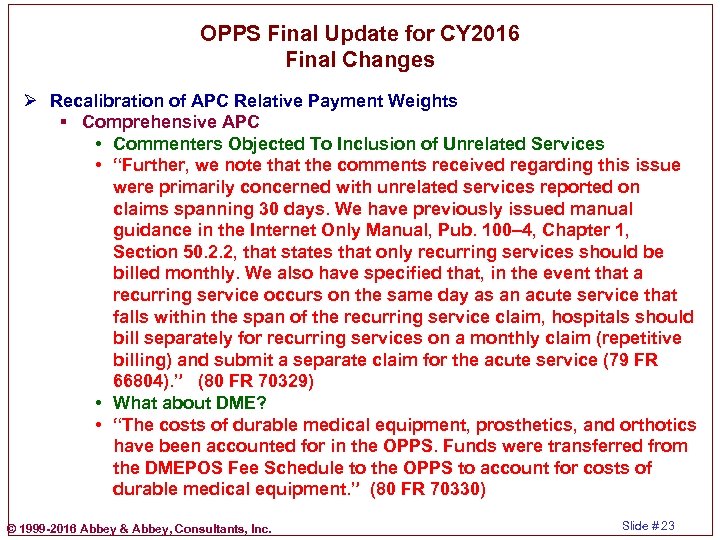
OPPS Final Update for CY 2016 Final Changes Ø Recalibration of APC Relative Payment Weights § Comprehensive APC • Commenters Objected To Inclusion of Unrelated Services • “Further, we note that the comments received regarding this issue were primarily concerned with unrelated services reported on claims spanning 30 days. We have previously issued manual guidance in the Internet Only Manual, Pub. 100– 4, Chapter 1, Section 50. 2. 2, that states that only recurring services should be billed monthly. We also have specified that, in the event that a recurring service occurs on the same day as an acute service that falls within the span of the recurring service claim, hospitals should bill separately for recurring services on a monthly claim (repetitive billing) and submit a separate claim for the acute service (79 FR 66804). ” (80 FR 70329) • What about DME? • “The costs of durable medical equipment, prosthetics, and orthotics have been accounted for in the OPPS. Funds were transferred from the DMEPOS Fee Schedule to the OPPS to account for costs of durable medical equipment. ” (80 FR 70330) © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 23
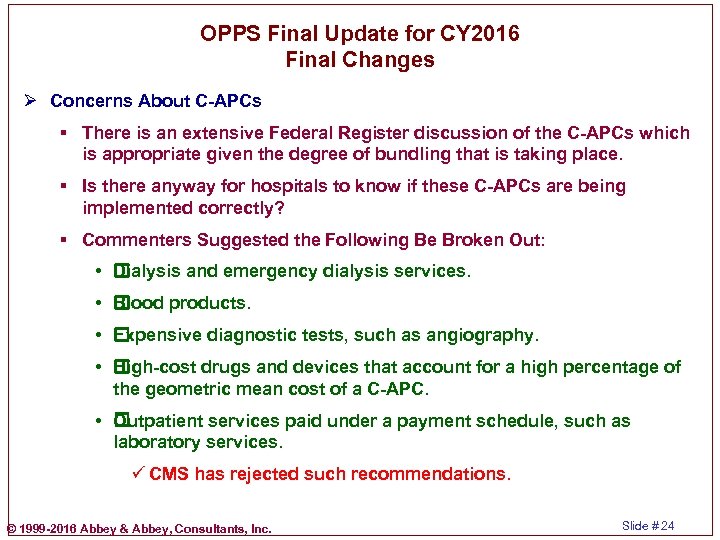
OPPS Final Update for CY 2016 Final Changes Ø Concerns About C-APCs § There is an extensive Federal Register discussion of the C-APCs which is appropriate given the degree of bundling that is taking place. § Is there anyway for hospitals to know if these C-APCs are being implemented correctly? § Commenters Suggested the Following Be Broken Out: • Dialysis and emergency dialysis services. • Blood products. • Expensive diagnostic tests, such as angiography. • High-cost drugs and devices that account for a high percentage of the geometric mean cost of a C-APC. • Outpatient services paid under a payment schedule, such as laboratory services. ü CMS has rejected such recommendations. © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 24
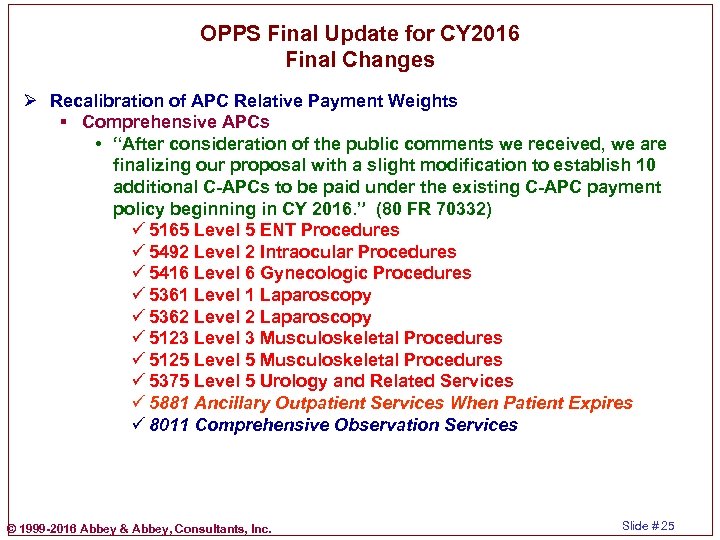
OPPS Final Update for CY 2016 Final Changes Ø Recalibration of APC Relative Payment Weights § Comprehensive APCs • “After consideration of the public comments we received, we are finalizing our proposal with a slight modification to establish 10 additional C-APCs to be paid under the existing C-APC payment policy beginning in CY 2016. ” (80 FR 70332) ü 5165 Level 5 ENT Procedures ü 5492 Level 2 Intraocular Procedures ü 5416 Level 6 Gynecologic Procedures ü 5361 Level 1 Laparoscopy ü 5362 Level 2 Laparoscopy ü 5123 Level 3 Musculoskeletal Procedures ü 5125 Level 5 Musculoskeletal Procedures ü 5375 Level 5 Urology and Related Services ü 5881 Ancillary Outpatient Services When Patient Expires ü 8011 Comprehensive Observation Services © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 25
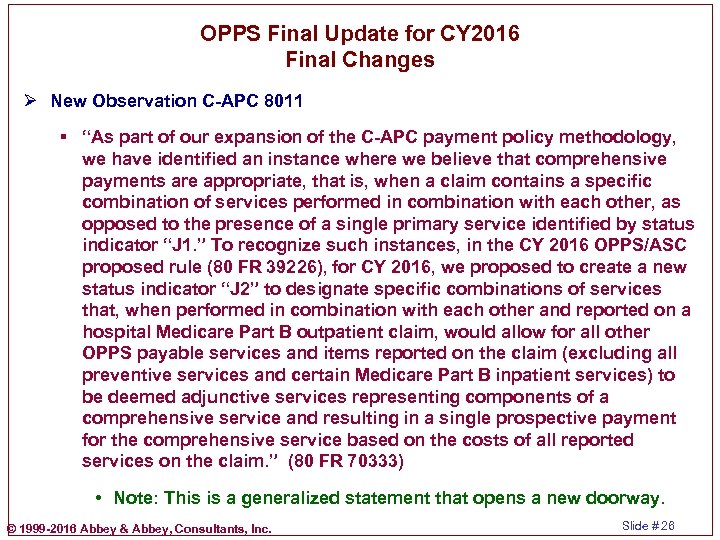
OPPS Final Update for CY 2016 Final Changes Ø New Observation C-APC 8011 § “As part of our expansion of the C-APC payment policy methodology, we have identified an instance where we believe that comprehensive payments are appropriate, that is, when a claim contains a specific combination of services performed in combination with each other, as opposed to the presence of a single primary service identified by status indicator “J 1. ” To recognize such instances, in the CY 2016 OPPS/ASC proposed rule (80 FR 39226), for CY 2016, we proposed to create a new status indicator “J 2” to designate specific combinations of services that, when performed in combination with each other and reported on a hospital Medicare Part B outpatient claim, would allow for all other OPPS payable services and items reported on the claim (excluding all preventive services and certain Medicare Part B inpatient services) to be deemed adjunctive services representing components of a comprehensive service and resulting in a single prospective payment for the comprehensive service based on the costs of all reported services on the claim. ” (80 FR 70333) • Note: This is a generalized statement that opens a new doorway. © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 26
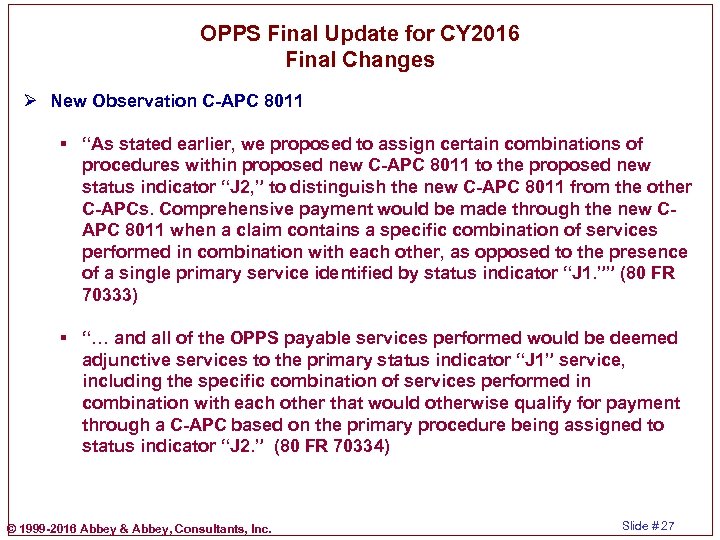
OPPS Final Update for CY 2016 Final Changes Ø New Observation C-APC 8011 § “As stated earlier, we proposed to assign certain combinations of procedures within proposed new C-APC 8011 to the proposed new status indicator “J 2, ” to distinguish the new C-APC 8011 from the other C-APCs. Comprehensive payment would be made through the new CAPC 8011 when a claim contains a specific combination of services performed in combination with each other, as opposed to the presence of a single primary service identified by status indicator “J 1. ”” (80 FR 70333) § “… and all of the OPPS payable services performed would be deemed adjunctive services to the primary status indicator “J 1” service, including the specific combination of services performed in combination with each other that would otherwise qualify for payment through a C-APC based on the primary procedure being assigned to status indicator “J 2. ” (80 FR 70334) © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 27
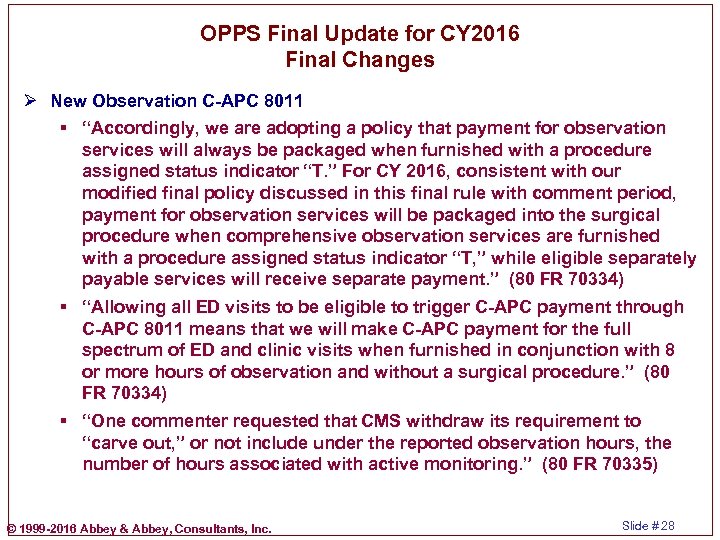
OPPS Final Update for CY 2016 Final Changes Ø New Observation C-APC 8011 § “Accordingly, we are adopting a policy that payment for observation services will always be packaged when furnished with a procedure assigned status indicator “T. ” For CY 2016, consistent with our modified final policy discussed in this final rule with comment period, payment for observation services will be packaged into the surgical procedure when comprehensive observation services are furnished with a procedure assigned status indicator “T, ” while eligible separately payable services will receive separate payment. ” (80 FR 70334) § “Allowing all ED visits to be eligible to trigger C-APC payment through C-APC 8011 means that we will make C-APC payment for the full spectrum of ED and clinic visits when furnished in conjunction with 8 or more hours of observation and without a surgical procedure. ” (80 FR 70334) § “One commenter requested that CMS withdraw its requirement to “carve out, ” or not include under the reported observation hours, the number of hours associated with active monitoring. ” (80 FR 70335) © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 28
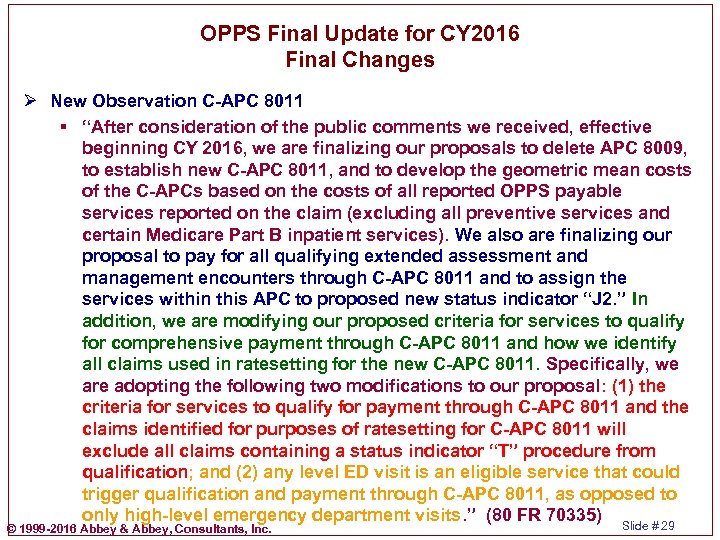
OPPS Final Update for CY 2016 Final Changes Ø New Observation C-APC 8011 § “After consideration of the public comments we received, effective beginning CY 2016, we are finalizing our proposals to delete APC 8009, to establish new C-APC 8011, and to develop the geometric mean costs of the C-APCs based on the costs of all reported OPPS payable services reported on the claim (excluding all preventive services and certain Medicare Part B inpatient services). We also are finalizing our proposal to pay for all qualifying extended assessment and management encounters through C-APC 8011 and to assign the services within this APC to proposed new status indicator “J 2. ” In addition, we are modifying our proposed criteria for services to qualify for comprehensive payment through C-APC 8011 and how we identify all claims used in ratesetting for the new C-APC 8011. Specifically, we are adopting the following two modifications to our proposal: (1) the criteria for services to qualify for payment through C-APC 8011 and the claims identified for purposes of ratesetting for C-APC 8011 will exclude all claims containing a status indicator “T” procedure from qualification; and (2) any level ED visit is an eligible service that could trigger qualification and payment through C-APC 8011, as opposed to only high-level emergency department visits. ” (80 FR 70335) Slide # 29 © 1999 -2016 Abbey & Abbey, Consultants, Inc.
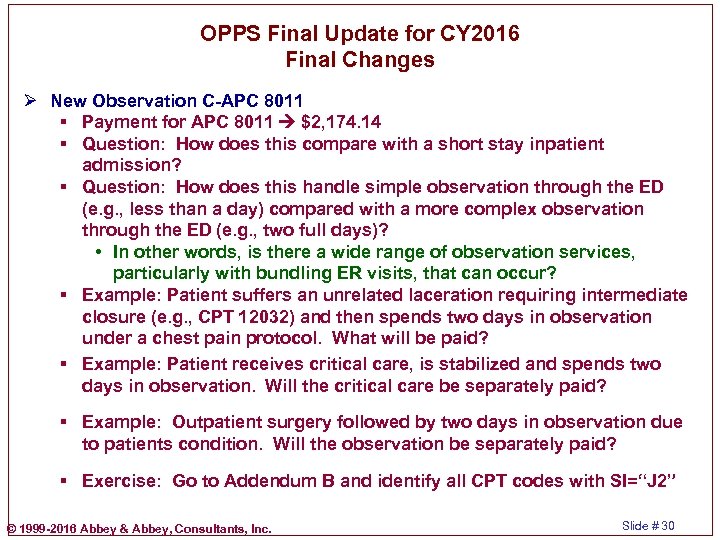
OPPS Final Update for CY 2016 Final Changes Ø New Observation C-APC 8011 § Payment for APC 8011 $2, 174. 14 § Question: How does this compare with a short stay inpatient admission? § Question: How does this handle simple observation through the ED (e. g. , less than a day) compared with a more complex observation through the ED (e. g. , two full days)? • In other words, is there a wide range of observation services, particularly with bundling ER visits, that can occur? § Example: Patient suffers an unrelated laceration requiring intermediate closure (e. g. , CPT 12032) and then spends two days in observation under a chest pain protocol. What will be paid? § Example: Patient receives critical care, is stabilized and spends two days in observation. Will the critical care be separately paid? § Example: Outpatient surgery followed by two days in observation due to patients condition. Will the observation be separately paid? § Exercise: Go to Addendum B and identify all CPT codes with SI=“J 2” © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 30
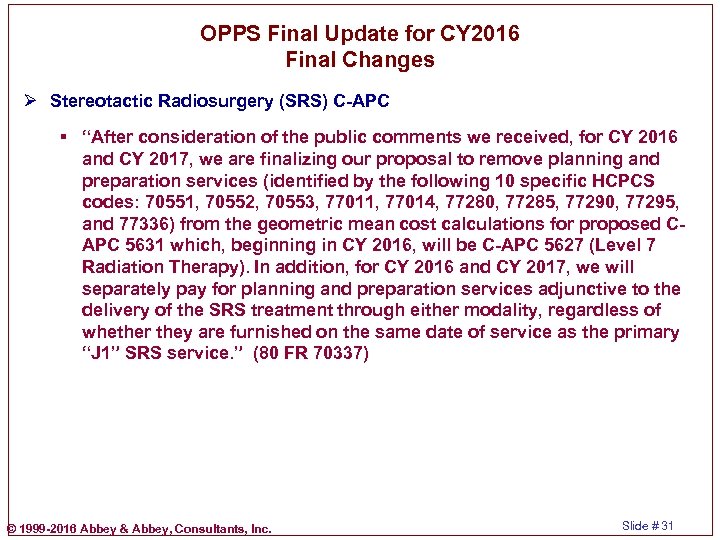
OPPS Final Update for CY 2016 Final Changes Ø Stereotactic Radiosurgery (SRS) C-APC § “After consideration of the public comments we received, for CY 2016 and CY 2017, we are finalizing our proposal to remove planning and preparation services (identified by the following 10 specific HCPCS codes: 70551, 70552, 70553, 77011, 77014, 77280, 77285, 77290, 77295, and 77336) from the geometric mean cost calculations for proposed CAPC 5631 which, beginning in CY 2016, will be C-APC 5627 (Level 7 Radiation Therapy). In addition, for CY 2016 and CY 2017, we will separately pay for planning and preparation services adjunctive to the delivery of the SRS treatment through either modality, regardless of whether they are furnished on the same date of service as the primary “J 1” SRS service. ” (80 FR 70337) © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 31
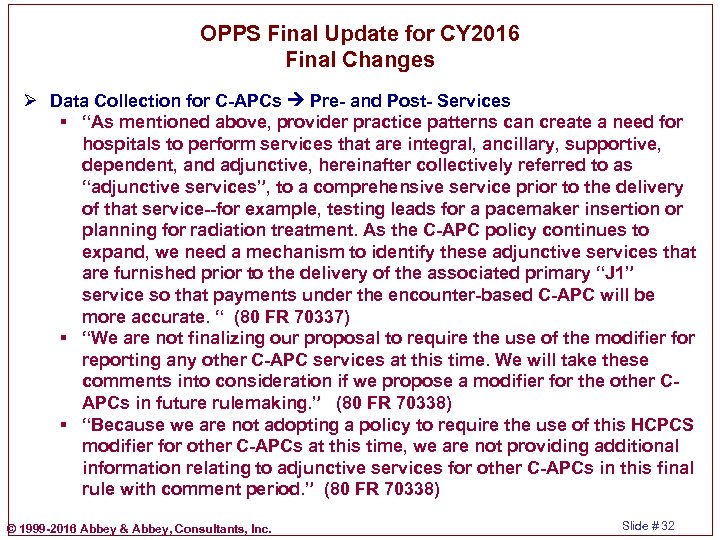
OPPS Final Update for CY 2016 Final Changes Ø Data Collection for C-APCs Pre- and Post- Services § “As mentioned above, provider practice patterns can create a need for hospitals to perform services that are integral, ancillary, supportive, dependent, and adjunctive, hereinafter collectively referred to as “adjunctive services”, to a comprehensive service prior to the delivery of that service--for example, testing leads for a pacemaker insertion or planning for radiation treatment. As the C-APC policy continues to expand, we need a mechanism to identify these adjunctive services that are furnished prior to the delivery of the associated primary “J 1” service so that payments under the encounter-based C-APC will be more accurate. “ (80 FR 70337) § “We are not finalizing our proposal to require the use of the modifier for reporting any other C-APC services at this time. We will take these comments into consideration if we propose a modifier for the other CAPCs in future rulemaking. ” (80 FR 70338) § “Because we are not adopting a policy to require the use of this HCPCS modifier for other C-APCs at this time, we are not providing additional information relating to adjunctive services for other C-APCs in this final rule with comment period. ” (80 FR 70338) © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 32
OPPS Final Update for CY 2016 Final Changes Ø Inpatient-Only Composite APC 5881 § “Currently, composite APC 0375 (Ancillary Outpatient Services When Patient Dies) packages payment for all services provided on the same date as an inpatient only procedure that is performed on an emergence basis on an outpatient who dies before admission when the modifier “– CA” appears on the claim. For CY 2016, we proposed to provide payment through proposed renumbered C-APC 5881 for all services reported on the same claim as an inpatient only procedure with the modifier “–CA. ”” (80 FR 70339) § “We did not receive any public comments on this proposal. Therefore, we are finalizing, without modification, our proposal to provide payment through renumbered C-APC 5881 for all services provided on the same date and reported on the same claim as an inpatient only procedure with the modifier “–CA. ”” (80 FR 70339) § Payment for C-APC 5881 $6, 143. 75 (For CY 2015 $3, 704. 16 – Why the big change? ) © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 33
OPPS Final Update for CY 2016 Final Changes Ø Other Composite APCs § Low Dose Rate (LDR) Prostate Brachytherapy • See CPT codes 55875 and 77778 • APC 5375 $3, 393. 73 § Mental Health Services – APC • “Therefore, we are finalizing our CY 2016 proposal, without modification, that when the aggregate payment for specified mental health services provided by one hospital to a single beneficiary on one date of service, based on the payment rates associated with the APCs for the individual services, exceeds the maximum per diem payment rate for partial hospitalization services provided by a hospital, those specified mental health services will be assigned to renumbered composite APC 8010 (Mental Health Services Composite) (existing APC 0034) for CY 2016. ” (80 FR 70334) • APC 8010 $212. 67 § Multiple Imaging Composite APCs (8004, 8005, 8006, 8007, 8008) • No logic changes. © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 34
OPPS Final Update for CY 2016 Final Changes Ø Conditionally Packaged Ancillary Services § “After consideration of the public comments we received, we are finalizing our proposal to conditionally packaged ancillary services assigned to APCs 5734, 5673, and 5674 for CY 2016. ” (80 FR 70345) • 5734 Level 4 Minor Procedures Q 1 $119. 58 • 5673 Level 3 Pathology Q 2 $229. 13 • 5674 Level 4 Pathology Q 2 $459. 96 § What does this mean? Can you think of any examples where this might be problematic? § “After consideration of the public comments we received, we are finalizing our policy to continue to exempt preventive services from the ancillary services packaging policy for CY 2016. ” (80 FR 703454) § Drugs and Biologicals That Function as Supplies When Used in a Surgical Procedure • “Supplies can be anything that is not equipment and include not only minor, inexpensive, or commodity-type items but also include a wide range of products used in the hospital outpatient setting, including certain implantable medical devices, drugs, biologicals, or radiopharmaceuticals … “ (80 FR 70346) © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 35
OPPS Final Update for CY 2016 Final Changes Ø Conditionally Packaged Ancillary Services § “In CY 2014, we finalized a policy to package payment for most clinical diagnostic laboratory tests in the OPPS (78 FR 74939 through 74942 and 42 CFR 419. 2(b)(17)). Under current policy, certain clinical diagnostic laboratory tests that are listed on the Clinical Laboratory Fee Schedule (CLFS) are packaged in the OPPS as integral, ancillary, supportive, dependent, or adjunctive to the primary service or services provided in the hospital outpatient setting on the same date of service as the laboratory test. Specifically, we conditionally package laboratory tests and only pay separately for a laboratory test when (1) it is the only service provided to a beneficiary on a given date of service; or (2) it is conducted on the same date of service as the primary service, but is ordered for a different diagnosis than the other hospital outpatient services and ordered by a practitioner different than the practitioner who ordered the other hospital outpatient services. (80 FR 70348) § See the “-L 1” modifier © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 36
OPPS Final Update for CY 2016 Final Changes Ø Conditionally Packaged Ancillary Services § “We concluded that hospitals generally do not view laboratory tests occurring on a different day than a primary service during an outpatient stay as a reason for separate payment. Therefore, we proposed to package laboratory tests that are reported on the same claim with a primary service, regardless of the date of service. ” (80 FR 70349) § See Molecular Biology Tests 81490, 81535, 81536, 81538 § SI=“Q 4 Conditionally packaged laboratory tests. Paid under OPPS or CLFS. • "(1) Packaged APC payment if billed on the same claim as a HCPCS code assigned published status indicator “J 1, ” “J 2, ” “S, ” “T, ” “V, ” “Q 1, ” “Q 2, ” or “Q 3. ”" • "(2) In other circumstances, laboratory tests should have an SI=A and payment is made under the CLFS. “ ü Note that this is at a claim level, not a date of service level. © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 37
OPPS Final Update for CY 2016 Final Changes Ø Conversion Factor § There is a long discussion in the FR entry. § There is a problem with packaging of laboratory tests. • “Therefore, we overestimated the adjustment necessary to account for the new policy to package laboratory tests and underestimated the amount of spending that would continue for laboratory tests paid at the CLFS rates outside the OPPS by approximately $1 billion. This $1 billion effectively resulted in inflation in the OPPS payment rates resulting from excess packaged payment under the OPPS for laboratory tests for all OPPS services and duplicate payments for certain laboratory tests because we are paying the laboratory tests through packaged payment incorporated into the OPPS payment rates as well as through separate payment at the CLFS payment rates outside the OPPS. ” (80 FR 70353) • What does this mean? Can you relate this to your hospital? © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 38
OPPS Final Update for CY 2016 Final Changes Ø Conversion Factor § “As a result of these finalized policies, the OPD fee schedule increase factor for the CY 2016 OPPS is 1. 7 percent (which is 2. 4 percent, the estimate of the hospital inpatient market basket percentage increase, less the 0. 5 percentage point MFP adjustment, and less the 0. 2 percentage point additional adjustment). For CY 2016, we are using a conversion factor of $73. 725 in the calculation of the national unadjusted payment rates for those items and services for which payment rates are calculated using geometric mean costs. That is, the OPD fee schedule increase factor of 1. 7 percent for CY 2016, the required wage index budget neutrality adjustment of 0. 9992, the cancer hospital payment adjustment of 0. 9994, the -2. 0 percent adjustment to the conversion factor to eliminate the effects of classification changes that would otherwise result in an increase in aggregate OPPS payments (due to excess packaged payment under the OPPS for laboratory tests), and the adjustment of -0. 13 percentage point of projected OPPS spending for the difference in the pass-through spending result in a conversion factor for CY 2016 of $73. 725. ” (80 FR 70357) © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 39
OPPS Final Update for CY 2016 Final Changes Ø Wage Index § Surprisingly Long Discussion § “After consideration of the public comment we received, we are finalizing our proposal, without modification, to continue to use an OPPS labor-related share of 60 percent of the national OPPS payment for the CY 2016 OPPS. We also are finalizing the use of the final FY 2016 IPPS post-reclassified wage index for urban and rural areas in its entirety, including the frontier State wage index floor, the rural floor, geographic reclassifications, and all other applicable wage index adjustments, as the final CY 2016 wage index for OPPS hospitals and CMHCs based on where the facility is located for both the OPPS payment rate and the copayment standardized amount, …” (80 FR 70359) Ø Statewide Average Default CCRs § See Table 14 § These statewide averages (rural and urban) can be informative to hospitals relative to the hospitals CCRs. © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 40
OPPS Final Update for CY 2016 Final Changes Ø SCHs and EACHs § “After consideration of the public comments we received, we are finalizing our proposal for CY 2016 to continue our policy of a 7. 1 percent payment adjustment that is done in a budget neutral manner for rural SCHs, including EACHs, for all services and procedures paid under the OPPS, excluding separately payable drugs and biologicals, devices paid under the pass-through payment policy, and items paid at charges reduced to costs. “ (80 FR 70362) Ø Outlier Payments § “We simulated aggregated CY 2016 hospital outlier payments using these costs for several different fixed-dollar thresholds, holding the 1. 75 multiple threshold constant and assuming that outlier payments will continue to be made at 50 percent of the amount by which the cost of furnishing the service would exceed 1. 75 times the APC payment amount, until the total outlier payments equaled 1. 0 percent of aggregated estimated total CY 2016 OPPS payments. We estimated that a fixed-dollar threshold of $3, 250, combined with the multiple threshold of 1. 75 times the APC payment rate, will allocate 1. 0 percent of aggregated total OPPS payments to outlier payments. (80 FR 70365) © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 41
OPPS Final Update for CY 2016 Final Changes Ø Beneficiary Copayment Amounts § The goal is to have the coinsurance be at 20%. • This is the same coinsurance as with the physician MPFS. • Note: CMS distinguishes coinsurance (a %) from copayment ($ amount). § With the number of changes that occur each year, that is, APC assignments, CPT/HCPCS changes and CPT/HCPCS mappings to APCs, the calculation of the copayment amount for each APC is sometimes problematic. § Particularly with new APCs the copayment amount may be above that which would be calculated at the 20% coinsurance amount. © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 42
OPPS Final Update for CY 2016 Final Changes Ø New Technology APCs § Additional 22 New Technology APC Groups for CY 2016 § Procedures Assigned to New Technology APC Groups • Transprostatic Urethral Implants Procedures • Retinal Prosthesis Implant Procedures Ø Payment for Devices § Expiration of Transitional Pass-Through Payments § Reducing Transitional Pass-Through Payment to Offset Packaging § Device-Intensive Procedures • “After consideration of the public comments we received, we are finalizing our proposal, without modification, that, beginning in CY 2016, only the procedures that require the implantation of a device that are assigned to a device-intensive APC will require a device code on the claim. ” (80 FR 70377) § No Cost/Full Credit and Partial Credit Devices • See “-FB” and “-FC” Modifiers § Adjustments to Payment for Discontinued Device-Intensive Procedures • See “-73”, “-74” and “-52” Modifiers © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 43
OPPS Final Update for CY 2016 Final Changes Ø Final OPPS APC-Specific Policies § Treatment of New CPT/HCPCS Codes § Each year CMS addresses specific areas. Depending upon your hospital’s services, some of these may be of interest. § Here are some examples: • Airway Endoscopy Procedures • Cardiac Rehabilitation • Cardiac Telemetry • Eye Surgery • Gastrointestinal (GI) Procedures • Gynecologic Procedures • Orthopedic Procedures • Skin Procedures • Pathology Services • Radiation Oncology • Urology • Vascular Procedures • ENT Procedures © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 44
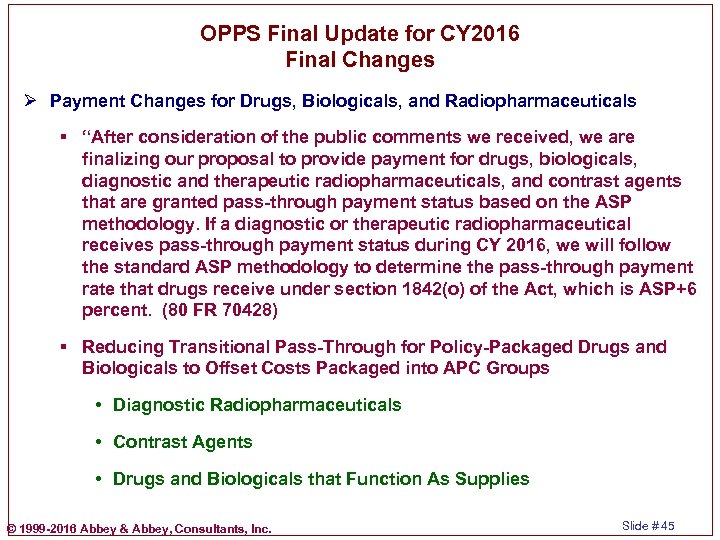
OPPS Final Update for CY 2016 Final Changes Ø Payment Changes for Drugs, Biologicals, and Radiopharmaceuticals § “After consideration of the public comments we received, we are finalizing our proposal to provide payment for drugs, biologicals, diagnostic and therapeutic radiopharmaceuticals, and contrast agents that are granted pass-through payment status based on the ASP methodology. If a diagnostic or therapeutic radiopharmaceutical receives pass-through payment status during CY 2016, we will follow the standard ASP methodology to determine the pass-through payment rate that drugs receive under section 1842(o) of the Act, which is ASP+6 percent. (80 FR 70428) § Reducing Transitional Pass-Through for Policy-Packaged Drugs and Biologicals to Offset Costs Packaged into APC Groups • Diagnostic Radiopharmaceuticals • Contrast Agents • Drugs and Biologicals that Function As Supplies © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 45
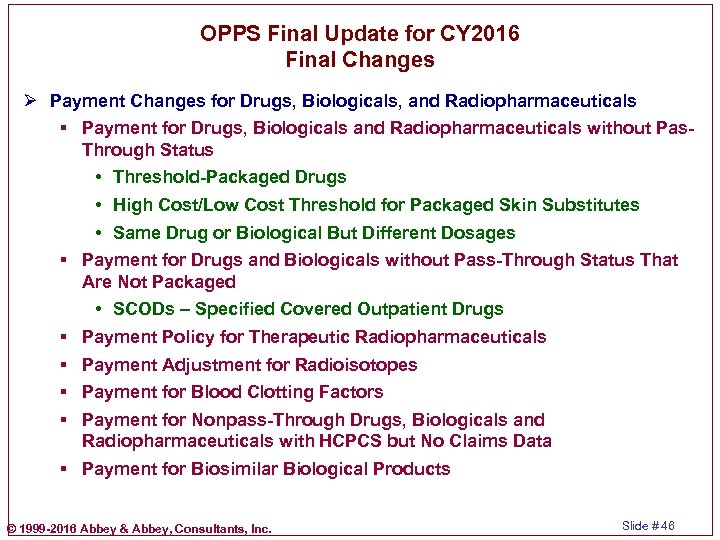
OPPS Final Update for CY 2016 Final Changes Ø Payment Changes for Drugs, Biologicals, and Radiopharmaceuticals § Payment for Drugs, Biologicals and Radiopharmaceuticals without Pas. Through Status • Threshold-Packaged Drugs • High Cost/Low Cost Threshold for Packaged Skin Substitutes • Same Drug or Biological But Different Dosages § Payment for Drugs and Biologicals without Pass-Through Status That Are Not Packaged • SCODs – Specified Covered Outpatient Drugs § Payment Policy for Therapeutic Radiopharmaceuticals § Payment Adjustment for Radioisotopes § Payment for Blood Clotting Factors § Payment for Nonpass-Through Drugs, Biologicals and Radiopharmaceuticals with HCPCS but No Claims Data § Payment for Biosimilar Biological Products © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 46
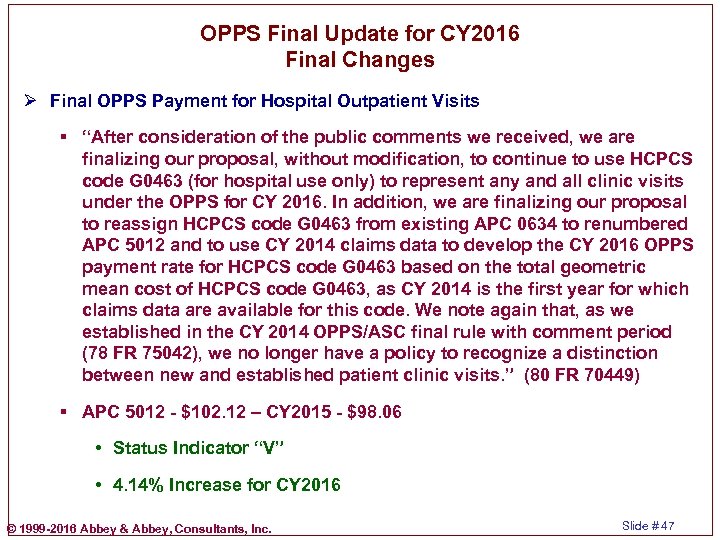
OPPS Final Update for CY 2016 Final Changes Ø Final OPPS Payment for Hospital Outpatient Visits § “After consideration of the public comments we received, we are finalizing our proposal, without modification, to continue to use HCPCS code G 0463 (for hospital use only) to represent any and all clinic visits under the OPPS for CY 2016. In addition, we are finalizing our proposal to reassign HCPCS code G 0463 from existing APC 0634 to renumbered APC 5012 and to use CY 2014 claims data to develop the CY 2016 OPPS payment rate for HCPCS code G 0463 based on the total geometric mean cost of HCPCS code G 0463, as CY 2014 is the first year for which claims data are available for this code. We note again that, as we established in the CY 2014 OPPS/ASC final rule with comment period (78 FR 75042), we no longer have a policy to recognize a distinction between new and established patient clinic visits. ” (80 FR 70449) § APC 5012 - $102. 12 – CY 2015 - $98. 06 • Status Indicator “V” • 4. 14% Increase for CY 2016 © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 47
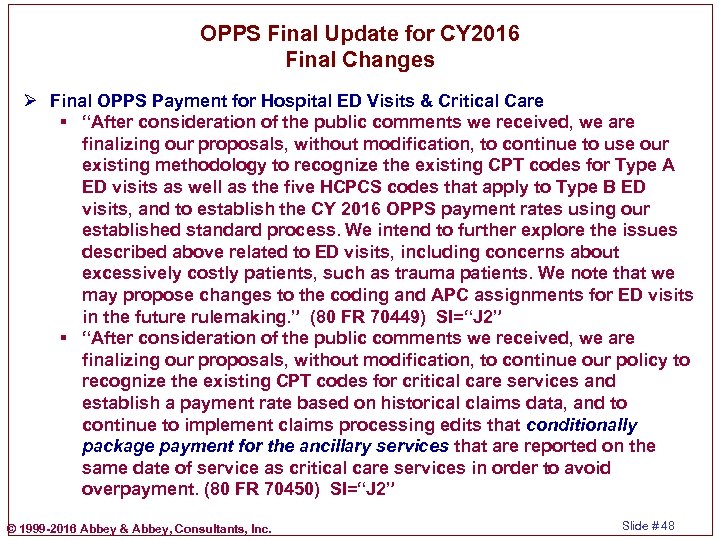
OPPS Final Update for CY 2016 Final Changes Ø Final OPPS Payment for Hospital ED Visits & Critical Care § “After consideration of the public comments we received, we are finalizing our proposals, without modification, to continue to use our existing methodology to recognize the existing CPT codes for Type A ED visits as well as the five HCPCS codes that apply to Type B ED visits, and to establish the CY 2016 OPPS payment rates using our established standard process. We intend to further explore the issues described above related to ED visits, including concerns about excessively costly patients, such as trauma patients. We note that we may propose changes to the coding and APC assignments for ED visits in the future rulemaking. ” (80 FR 70449) SI=“J 2” § “After consideration of the public comments we received, we are finalizing our proposals, without modification, to continue our policy to recognize the existing CPT codes for critical care services and establish a payment rate based on historical claims data, and to continue to implement claims processing edits that conditionally package payment for the ancillary services that are reported on the same date of service as critical care services in order to avoid overpayment. (80 FR 70450) SI=“J 2” © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 48
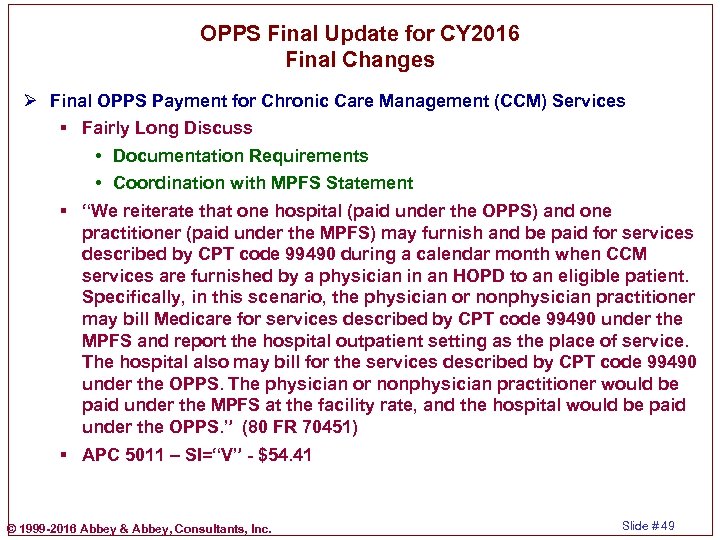
OPPS Final Update for CY 2016 Final Changes Ø Final OPPS Payment for Chronic Care Management (CCM) Services § Fairly Long Discuss • Documentation Requirements • Coordination with MPFS Statement § “We reiterate that one hospital (paid under the OPPS) and one practitioner (paid under the MPFS) may furnish and be paid for services described by CPT code 99490 during a calendar month when CCM services are furnished by a physician in an HOPD to an eligible patient. Specifically, in this scenario, the physician or nonphysician practitioner may bill Medicare for services described by CPT code 99490 under the MPFS and report the hospital outpatient setting as the place of service. The hospital also may bill for the services described by CPT code 99490 under the OPPS. The physician or nonphysician practitioner would be paid under the MPFS at the facility rate, and the hospital would be paid under the OPPS. ” (80 FR 70451) § APC 5011 – SI=“V” - $54. 41 © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 49
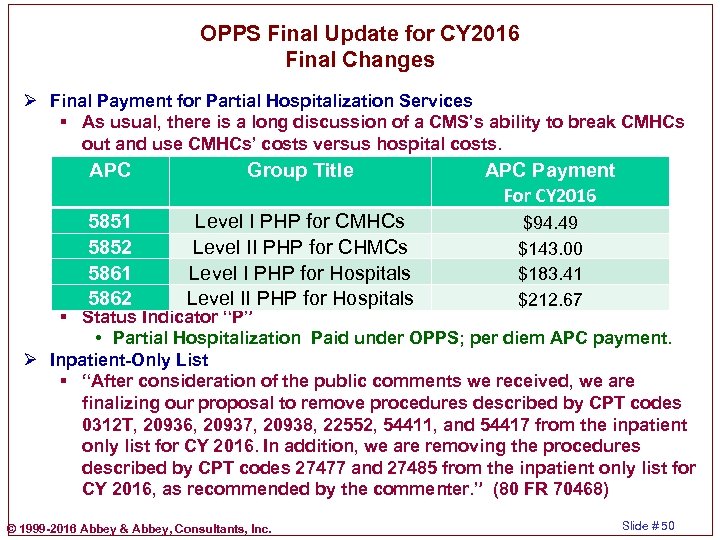
OPPS Final Update for CY 2016 Final Changes Ø Final Payment for Partial Hospitalization Services § As usual, there is a long discussion of a CMS’s ability to break CMHCs out and use CMHCs’ costs versus hospital costs. APC Group Title APC Payment For CY 2016 5851 5852 5861 5862 Level I PHP for CMHCs Level II PHP for CHMCs Level I PHP for Hospitals Level II PHP for Hospitals $94. 49 $143. 00 $183. 41 $212. 67 § Status Indicator “P” • Partial Hospitalization Paid under OPPS; per diem APC payment. Ø Inpatient-Only List § “After consideration of the public comments we received, we are finalizing our proposal to remove procedures described by CPT codes 0312 T, 20936, 20937, 20938, 22552, 54411, and 54417 from the inpatient only list for CY 2016. In addition, we are removing the procedures described by CPT codes 27477 and 27485 from the inpatient only list for CY 2016, as recommended by the commenter. ” (80 FR 70468) © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 50
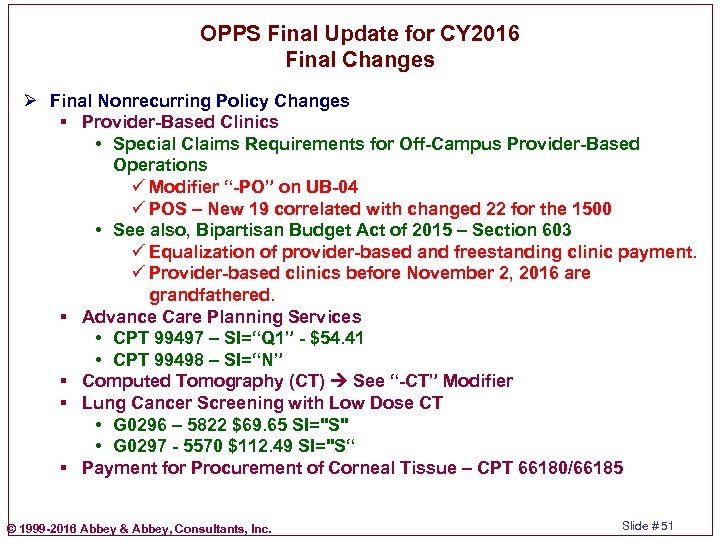
OPPS Final Update for CY 2016 Final Changes Ø Final Nonrecurring Policy Changes § Provider-Based Clinics • Special Claims Requirements for Off-Campus Provider-Based Operations ü Modifier “-PO” on UB-04 ü POS – New 19 correlated with changed 22 for the 1500 • See also, Bipartisan Budget Act of 2015 – Section 603 ü Equalization of provider-based and freestanding clinic payment. ü Provider-based clinics before November 2, 2016 are grandfathered. § Advance Care Planning Services • CPT 99497 – SI=“Q 1” - $54. 41 • CPT 99498 – SI=“N” § Computed Tomography (CT) See “-CT” Modifier § Lung Cancer Screening with Low Dose CT • G 0296 – 5822 $69. 65 SI="S" • G 0297 - 5570 $112. 49 SI="S“ § Payment for Procurement of Corneal Tissue – CPT 66180/66185 © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 51
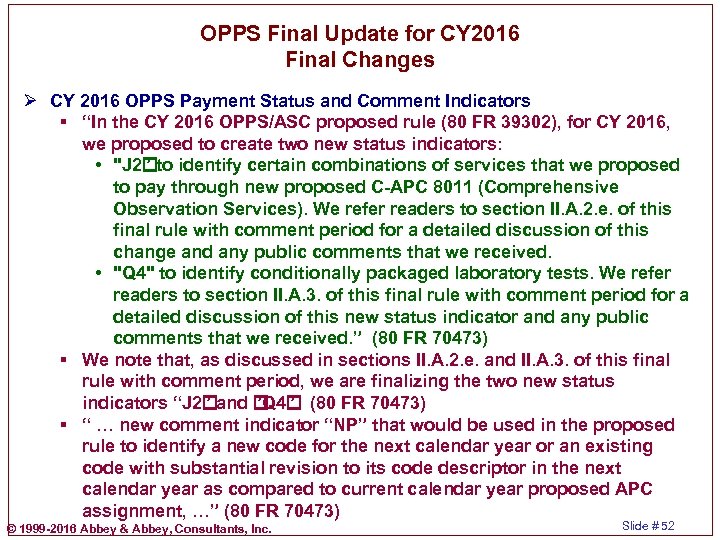
OPPS Final Update for CY 2016 Final Changes Ø CY 2016 OPPS Payment Status and Comment Indicators § “In the CY 2016 OPPS/ASC proposed rule (80 FR 39302), for CY 2016, we proposed to create two new status indicators: • "J 2 ” to identify certain combinations of services that we proposed to pay through new proposed C-APC 8011 (Comprehensive Observation Services). We refer readers to section II. A. 2. e. of this final rule with comment period for a detailed discussion of this change and any public comments that we received. • "Q 4" to identify conditionally packaged laboratory tests. We refer readers to section II. A. 3. of this final rule with comment period for a detailed discussion of this new status indicator and any public comments that we received. ” (80 FR 70473) § We note that, as discussed in sections II. A. 2. e. and II. A. 3. of this final rule with comment period, we are finalizing the two new status indicators “J 2 ” and ”. (80 FR 70473) ”Q 4 § “ … new comment indicator “NP” that would be used in the proposed rule to identify a new code for the next calendar year or an existing code with substantial revision to its code descriptor in the next calendar year as compared to current calendar year proposed APC assignment, …” (80 FR 70473) © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 52
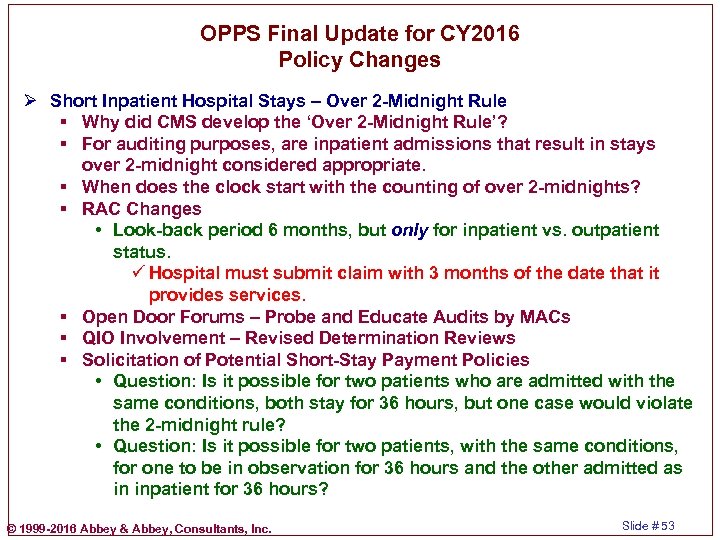
OPPS Final Update for CY 2016 Policy Changes Ø Short Inpatient Hospital Stays – Over 2 -Midnight Rule § Why did CMS develop the ‘Over 2 -Midnight Rule’? § For auditing purposes, are inpatient admissions that result in stays over 2 -midnight considered appropriate. § When does the clock start with the counting of over 2 -midnights? § RAC Changes • Look-back period 6 months, but only for inpatient vs. outpatient status. ü Hospital must submit claim with 3 months of the date that it provides services. § Open Door Forums – Probe and Educate Audits by MACs § QIO Involvement – Revised Determination Reviews § Solicitation of Potential Short-Stay Payment Policies • Question: Is it possible for two patients who are admitted with the same conditions, both stay for 36 hours, but one case would violate the 2 -midnight rule? • Question: Is it possible for two patients, with the same conditions, for one to be in observation for 36 hours and the other admitted as in inpatient for 36 hours? © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 53
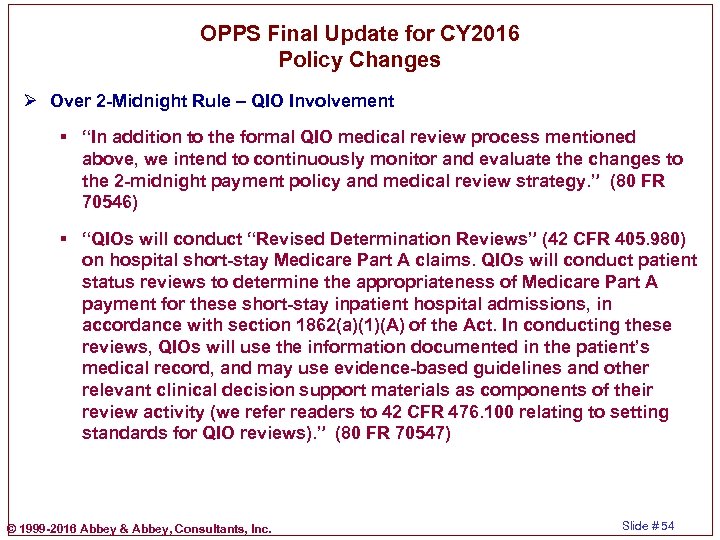
OPPS Final Update for CY 2016 Policy Changes Ø Over 2 -Midnight Rule – QIO Involvement § “In addition to the formal QIO medical review process mentioned above, we intend to continuously monitor and evaluate the changes to the 2 -midnight payment policy and medical review strategy. ” (80 FR 70546) § “QIOs will conduct “Revised Determination Reviews” (42 CFR 405. 980) on hospital short-stay Medicare Part A claims. QIOs will conduct patient status reviews to determine the appropriateness of Medicare Part A payment for these short-stay inpatient hospital admissions, in accordance with section 1862(a)(1)(A) of the Act. In conducting these reviews, QIOs will use the information documented in the patient’s medical record, and may use evidence-based guidelines and other relevant clinical decision support materials as components of their review activity (we refer readers to 42 CFR 476. 100 relating to setting standards for QIO reviews). ” (80 FR 70547) © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 54
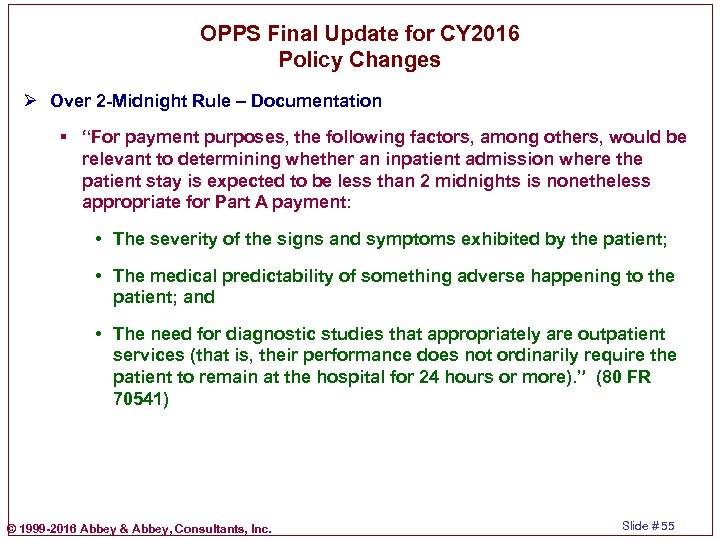
OPPS Final Update for CY 2016 Policy Changes Ø Over 2 -Midnight Rule – Documentation § “For payment purposes, the following factors, among others, would be relevant to determining whether an inpatient admission where the patient stay is expected to be less than 2 midnights is nonetheless appropriate for Part A payment: • The severity of the signs and symptoms exhibited by the patient; • The medical predictability of something adverse happening to the patient; and • The need for diagnostic studies that appropriately are outpatient services (that is, their performance does not ordinarily require the patient to remain at the hospital for 24 hours or more). ” (80 FR 70541) © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 55
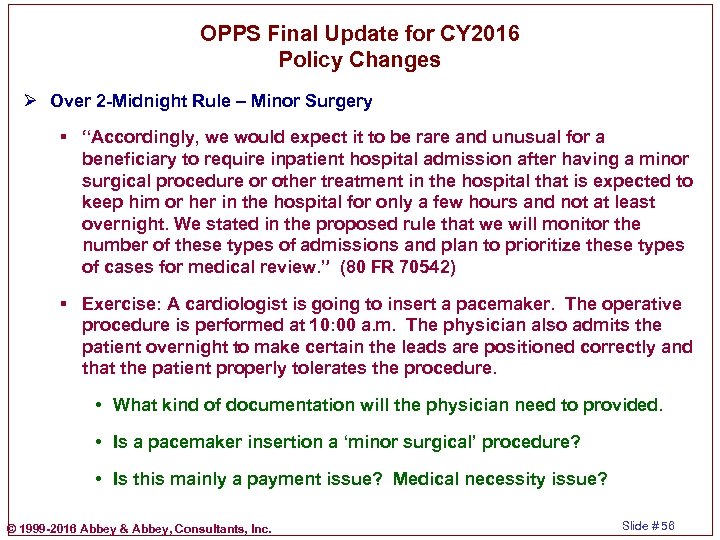
OPPS Final Update for CY 2016 Policy Changes Ø Over 2 -Midnight Rule – Minor Surgery § “Accordingly, we would expect it to be rare and unusual for a beneficiary to require inpatient hospital admission after having a minor surgical procedure or other treatment in the hospital that is expected to keep him or her in the hospital for only a few hours and not at least overnight. We stated in the proposed rule that we will monitor the number of these types of admissions and plan to prioritize these types of cases for medical review. ” (80 FR 70542) § Exercise: A cardiologist is going to insert a pacemaker. The operative procedure is performed at 10: 00 a. m. The physician also admits the patient overnight to make certain the leads are positioned correctly and that the patient properly tolerates the procedure. • What kind of documentation will the physician need to provided. • Is a pacemaker insertion a ‘minor surgical’ procedure? • Is this mainly a payment issue? Medical necessity issue? © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 56
OPPS Final Update for CY 2016 Policy Changes Ø Over 2 -Midnight Rule – Commenters’ Recommendation to Rescind § “Comment: Several commenters, including Med. PAC and the American Medical Association (AMA), recommended that CMS rescind the 2 midnight rule in its entirety. Some of the commenters stated that any time-based admission policy would interfere with physician judgment. In addition, Med. PAC expressed concern that the 2 -midnight rule may provide hospitals with an incentive to lengthen hospital stays in order to avoid scrutiny and that longer stays generally increase costs and expose Medicare beneficiaries to greater physical risk while also conflicting with the general incentives of the prospective payment system to reduce hospital lengths of stay. Med. PAC also stated that the Commission recommended that CMS withdraw the 2 -midnight rule because it becomes redundant in light of Med. PAC recommendations related to the Recovery Audit Program. The AMA expressed concern that the 2 -midnight rule places considerable burden on the admitting physician and erodes the ability of physicians and providers to improve health outcomes through personalized, evidence-based clinical care because it detracts from admission criteria that depend upon clinical judgment. ” (80 FR 70542 -70543) © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 57
OPPS Final Update for CY 2016 Policy Changes Ø Over 2 -Midnight Rule – Comment § “Comment: One commenter suggested that CMS (1) clarify that inpatient hospital admissions with expected lengths of stay less than 2 midnights are neither rare nor unusual; (2) reemphasize that inpatient care and observation services are not the same level of care and, therefore, inpatient hospital admissions are not appropriate as a substitute for lengthy (greater than 2 midnights) outpatient hospital stays; (3) allow the 2 -midnight benchmark to serve exclusively as a medical review threshold to determine the general appropriateness for claim payment; and (4) realign its policy with existing guidance by asserting that, regardless of the expected length of stay, documentation of the medical necessity as well as the need for inpatient hospital care is the requisite component of every inpatient admission appropriately paid under Medicare Part A. ” (80 FR 70544) © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 58
OPPS Final Update for CY 2016 Policy Changes Ø Over 2 -Midnight Rule – Observation Different From Inpatient § “With respect to the comment about hospital level of care, we note that while we do not refer to “level of care” in guidance regarding hospital inpatient admission decisions, but, rather, have consistently provided physicians with the aforementioned time-based guidelines regarding when an inpatient hospital admission is payable under Part A, we do note that, by definition, there are differences between observation services furnished in the outpatient setting and services furnished to hospital inpatients. Specifically, observation services, as defined in Section 290 of Chapter 4 of the Medicare Claims Processing Manual, are a well-defined set of specific, clinically appropriate services, which include ongoing short-term treatment, assessment, and reassessment, that are furnished while a decision is being made, regarding whether patients will require further treatment as hospital inpatients or if they are able to be discharged from the hospital. ” (80 FR 70545) © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 59
OPPS Final Update for CY 2016 Policy Changes Ø Over 2 -Midnight Rule § “After consideration of the public comments we received, we are finalizing, without modification, our proposal to revise our previous “rare and unusual” exceptions policy to allow for Medicare Part A payment on a case-by-case basis for inpatient admissions that do not satisfy the 2 -midnight benchmark, if the documentation in the medical record supports the admitting physician’s determination that the patient requires inpatient hospital care despite an expected length of stay that is less than 2 midnights. Accordingly, we also are finalizing our proposal to revise § 412. 3(d) to reflect the above policy modification and to increase clarity. ” (80 FR 70545) © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 60
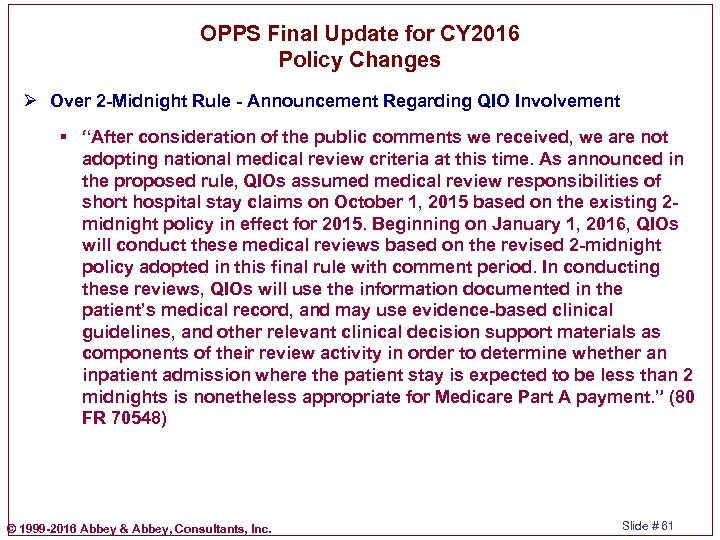
OPPS Final Update for CY 2016 Policy Changes Ø Over 2 -Midnight Rule - Announcement Regarding QIO Involvement § “After consideration of the public comments we received, we are not adopting national medical review criteria at this time. As announced in the proposed rule, QIOs assumed medical review responsibilities of short hospital stay claims on October 1, 2015 based on the existing 2 midnight policy in effect for 2015. Beginning on January 1, 2016, QIOs will conduct these medical reviews based on the revised 2 -midnight policy adopted in this final rule with comment period. In conducting these reviews, QIOs will use the information documented in the patient’s medical record, and may use evidence-based clinical guidelines, and other relevant clinical decision support materials as components of their review activity in order to determine whether an inpatient admission where the patient stay is expected to be less than 2 midnights is nonetheless appropriate for Medicare Part A payment. ” (80 FR 70548) © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 61
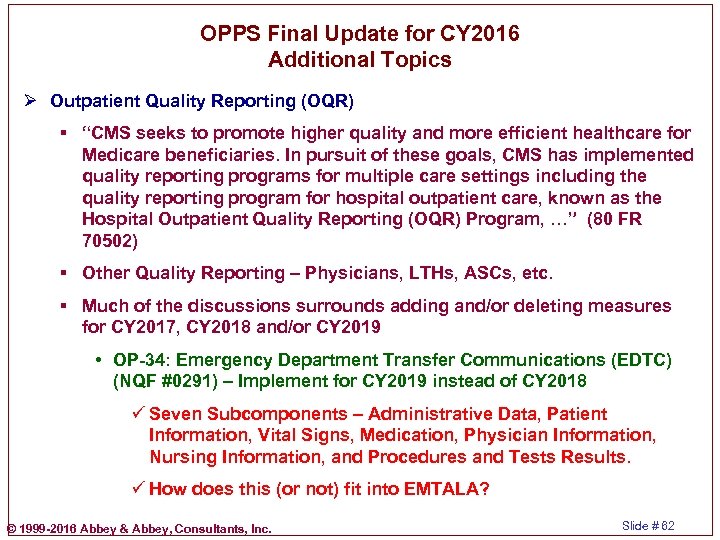
OPPS Final Update for CY 2016 Additional Topics Ø Outpatient Quality Reporting (OQR) § “CMS seeks to promote higher quality and more efficient healthcare for Medicare beneficiaries. In pursuit of these goals, CMS has implemented quality reporting programs for multiple care settings including the quality reporting program for hospital outpatient care, known as the Hospital Outpatient Quality Reporting (OQR) Program, …” (80 FR 70502) § Other Quality Reporting – Physicians, LTHs, ASCs, etc. § Much of the discussions surrounds adding and/or deleting measures for CY 2017, CY 2018 and/or CY 2019 • OP-34: Emergency Department Transfer Communications (EDTC) (NQF #0291) – Implement for CY 2019 instead of CY 2018 ü Seven Subcomponents – Administrative Data, Patient Information, Vital Signs, Medication, Physician Information, Nursing Information, and Procedures and Tests Results. ü How does this (or not) fit into EMTALA? © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 62
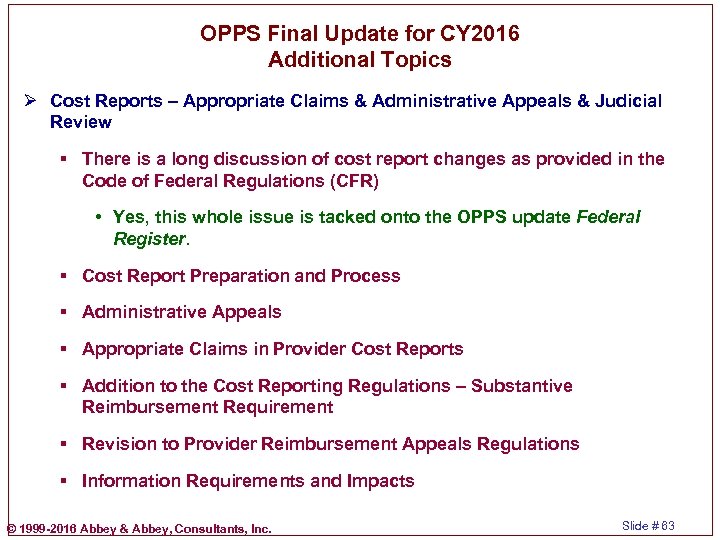
OPPS Final Update for CY 2016 Additional Topics Ø Cost Reports – Appropriate Claims & Administrative Appeals & Judicial Review § There is a long discussion of cost report changes as provided in the Code of Federal Regulations (CFR) • Yes, this whole issue is tacked onto the OPPS update Federal Register. § Cost Report Preparation and Process § Administrative Appeals § Appropriate Claims in Provider Cost Reports § Addition to the Cost Reporting Regulations – Substantive Reimbursement Requirement § Revision to Provider Reimbursement Appeals Regulations § Information Requirements and Impacts © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 63
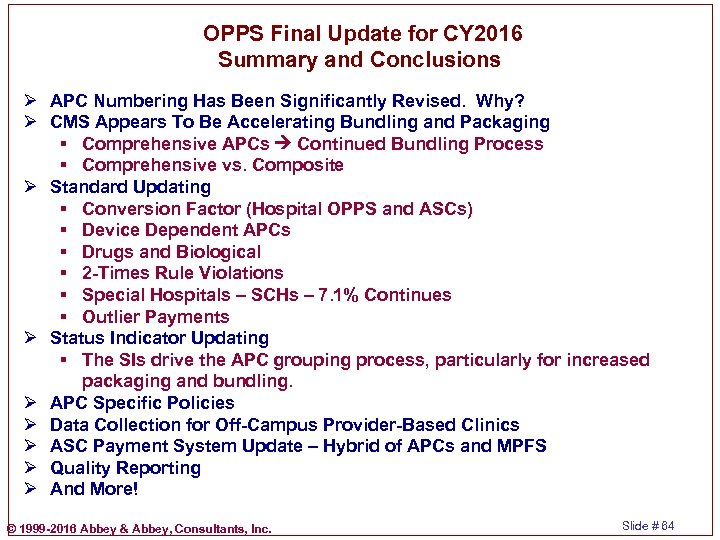
OPPS Final Update for CY 2016 Summary and Conclusions Ø APC Numbering Has Been Significantly Revised. Why? Ø CMS Appears To Be Accelerating Bundling and Packaging § Comprehensive APCs Continued Bundling Process § Comprehensive vs. Composite Ø Standard Updating § Conversion Factor (Hospital OPPS and ASCs) § Device Dependent APCs § Drugs and Biological § 2 -Times Rule Violations § Special Hospitals – SCHs – 7. 1% Continues § Outlier Payments Ø Status Indicator Updating § The SIs drive the APC grouping process, particularly for increased packaging and bundling. Ø APC Specific Policies Ø Data Collection for Off-Campus Provider-Based Clinics Ø ASC Payment System Update – Hybrid of APCs and MPFS Ø Quality Reporting Ø And More! © 1999 -2016 Abbey & Abbey, Consultants, Inc. Slide # 64
9eb8fcd677ae4460765270b590f71da6.ppt