5-2 Aortic valve disease.ppt
- Количество слайдов: 68
 Aortic Valve Disease
Aortic Valve Disease
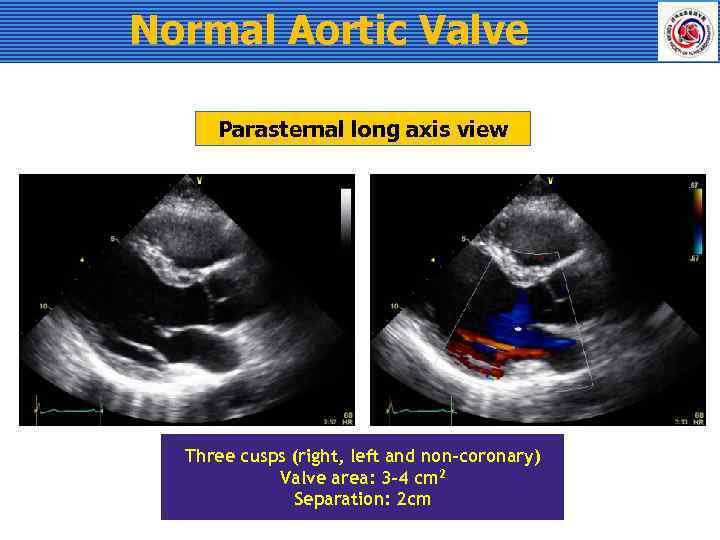 Normal Aortic Valve Parasternal long axis view Three cusps (right, left and non-coronary) Valve area: 3 -4 cm 2 Separation: 2 cm
Normal Aortic Valve Parasternal long axis view Three cusps (right, left and non-coronary) Valve area: 3 -4 cm 2 Separation: 2 cm
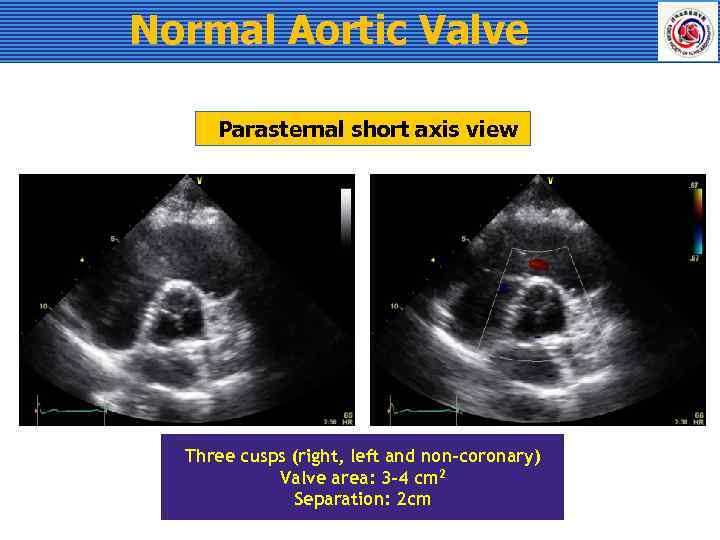 Normal Aortic Valve Parasternal short axis view Three cusps (right, left and non-coronary) Valve area: 3 -4 cm 2 Separation: 2 cm
Normal Aortic Valve Parasternal short axis view Three cusps (right, left and non-coronary) Valve area: 3 -4 cm 2 Separation: 2 cm
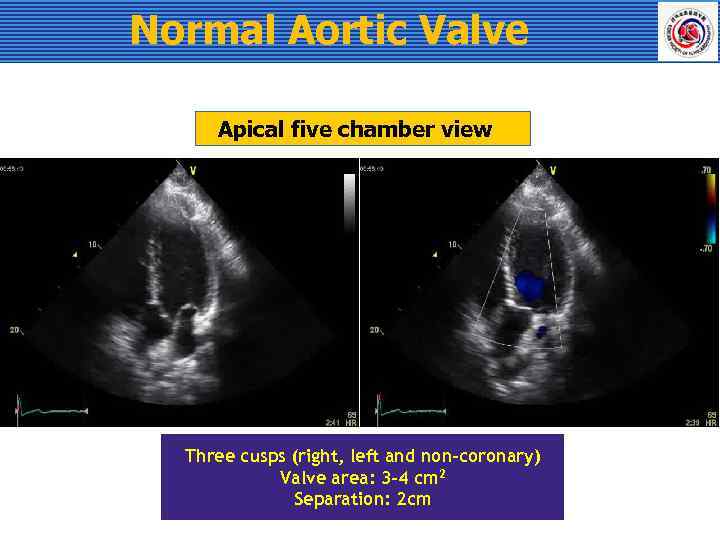 Normal Aortic Valve Apical five chamber view Three cusps (right, left and non-coronary) Valve area: 3 -4 cm 2 Separation: 2 cm
Normal Aortic Valve Apical five chamber view Three cusps (right, left and non-coronary) Valve area: 3 -4 cm 2 Separation: 2 cm
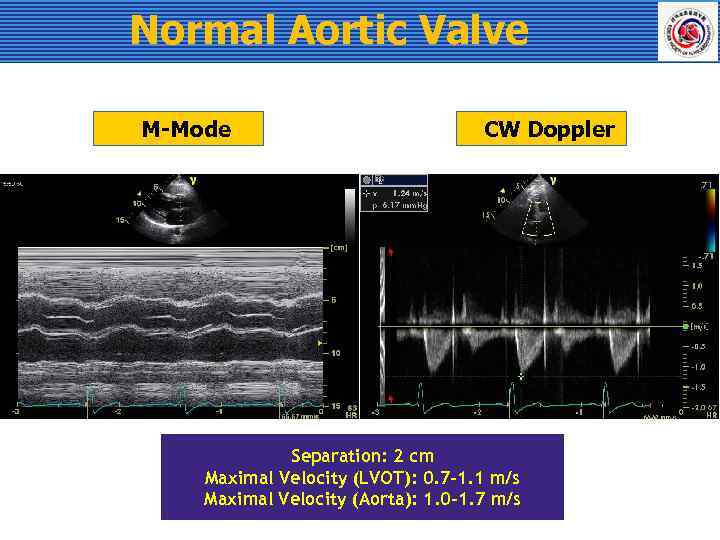 Normal Aortic Valve M-Mode CW Doppler Separation: 2 cm Maximal Velocity (LVOT): 0. 7 -1. 1 m/s Maximal Velocity (Aorta): 1. 0 -1. 7 m/s
Normal Aortic Valve M-Mode CW Doppler Separation: 2 cm Maximal Velocity (LVOT): 0. 7 -1. 1 m/s Maximal Velocity (Aorta): 1. 0 -1. 7 m/s
 Congenital Anomaly Unicuspid valve Bicuspid valve Quadricuspid valve
Congenital Anomaly Unicuspid valve Bicuspid valve Quadricuspid valve
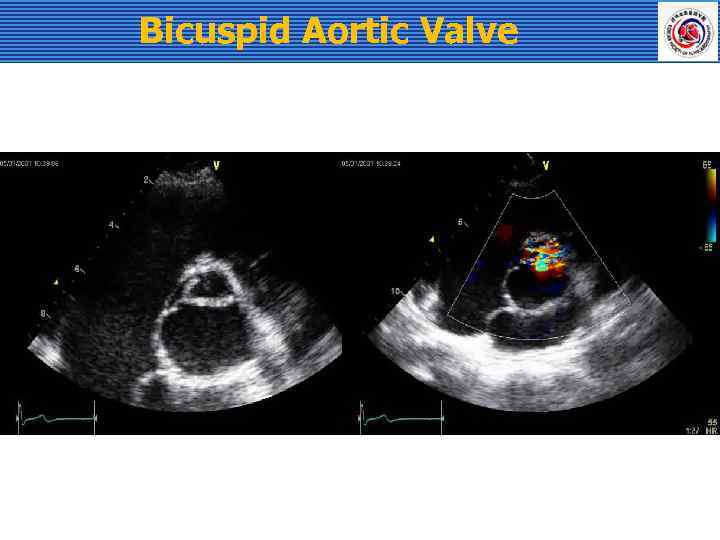
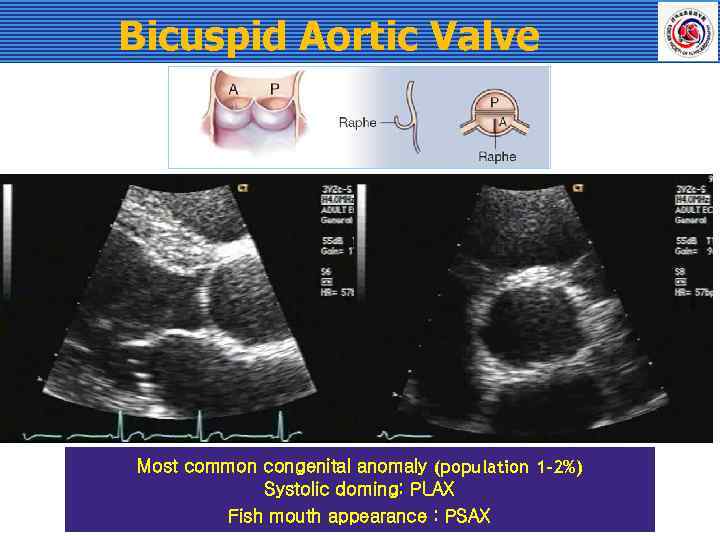 Bicuspid Aortic Valve Most common congenital anomaly (population 1 -2%) Systolic doming: PLAX Fish mouth appearance : PSAX
Bicuspid Aortic Valve Most common congenital anomaly (population 1 -2%) Systolic doming: PLAX Fish mouth appearance : PSAX
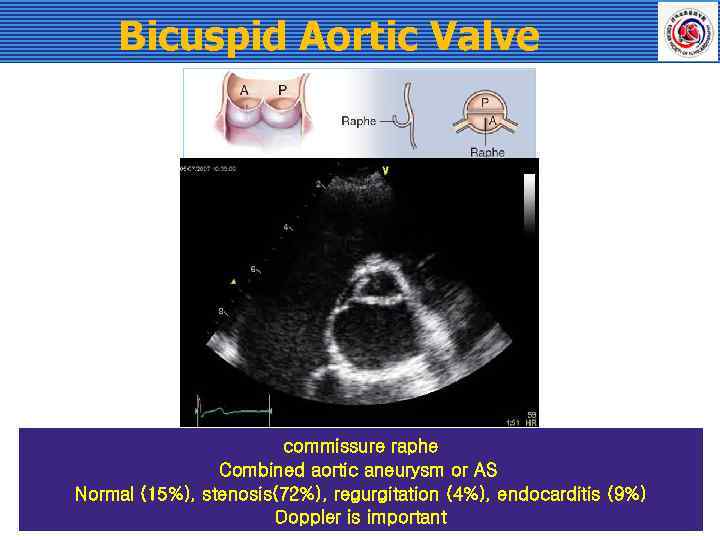 Bicuspid Aortic Valve commissure raphe Combined aortic aneurysm or AS Normal (15%), stenosis(72%), regurgitation (4%), endocarditis (9%) Doppler is important
Bicuspid Aortic Valve commissure raphe Combined aortic aneurysm or AS Normal (15%), stenosis(72%), regurgitation (4%), endocarditis (9%) Doppler is important
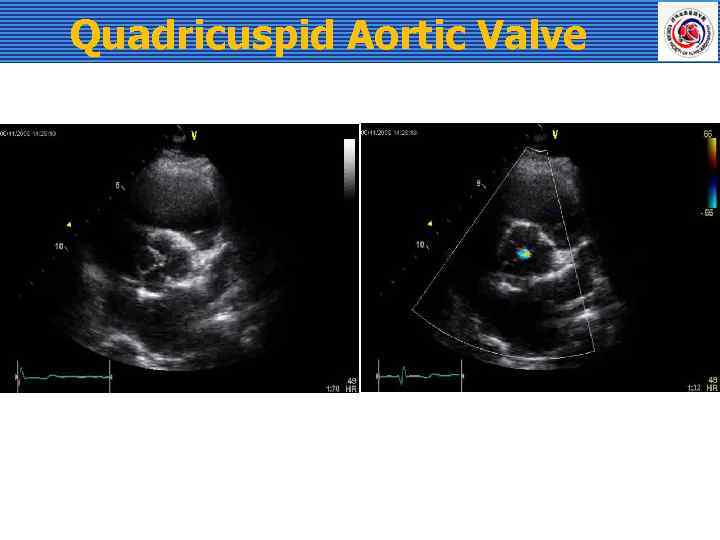 Quadricuspid Aortic Valve
Quadricuspid Aortic Valve
 Aortic Stenosis
Aortic Stenosis
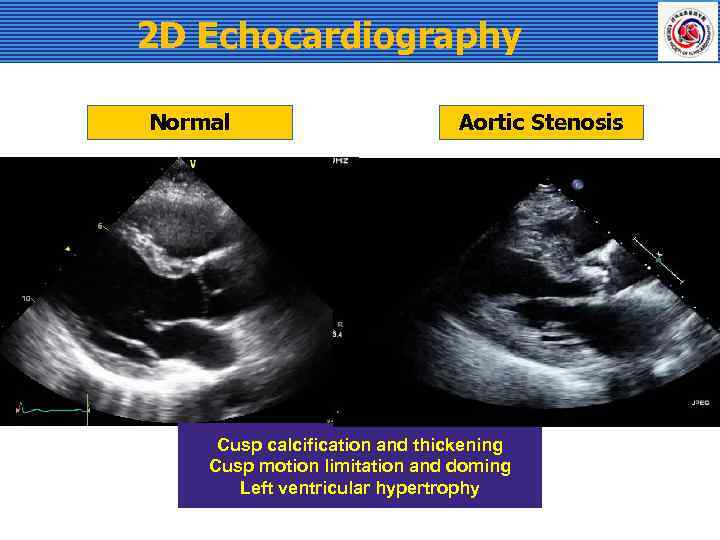 2 D Echocardiography Normal Aortic Stenosis Cusp calcification and thickening Cusp motion limitation and doming Left ventricular hypertrophy
2 D Echocardiography Normal Aortic Stenosis Cusp calcification and thickening Cusp motion limitation and doming Left ventricular hypertrophy
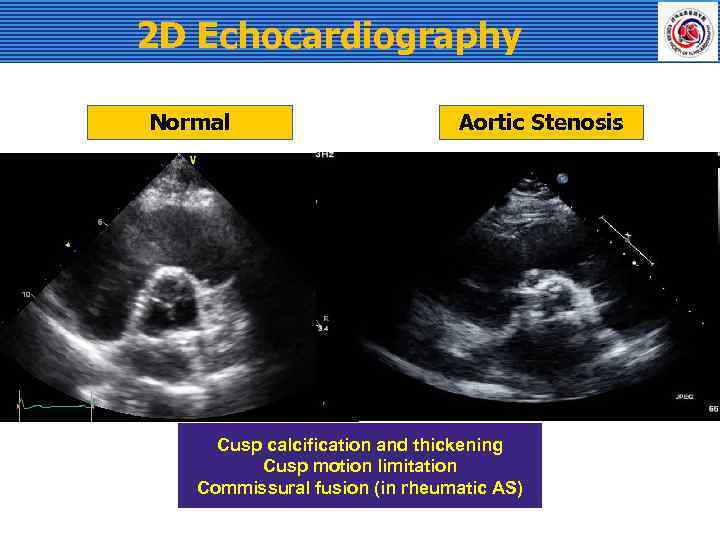 2 D Echocardiography Normal Aortic Stenosis Cusp calcification and thickening Cusp motion limitation Commissural fusion (in rheumatic AS)
2 D Echocardiography Normal Aortic Stenosis Cusp calcification and thickening Cusp motion limitation Commissural fusion (in rheumatic AS)
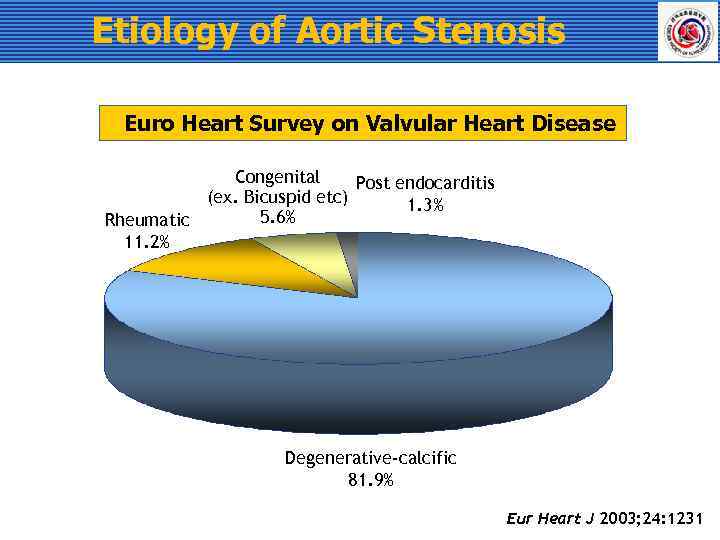 Etiology of Aortic Stenosis Euro Heart Survey on Valvular Heart Disease Congenital Post endocarditis (ex. Bicuspid etc) 1. 3% 5. 6% Rheumatic 11. 2% Degenerative-calcific 81. 9% Eur Heart J 2003; 24: 1231
Etiology of Aortic Stenosis Euro Heart Survey on Valvular Heart Disease Congenital Post endocarditis (ex. Bicuspid etc) 1. 3% 5. 6% Rheumatic 11. 2% Degenerative-calcific 81. 9% Eur Heart J 2003; 24: 1231
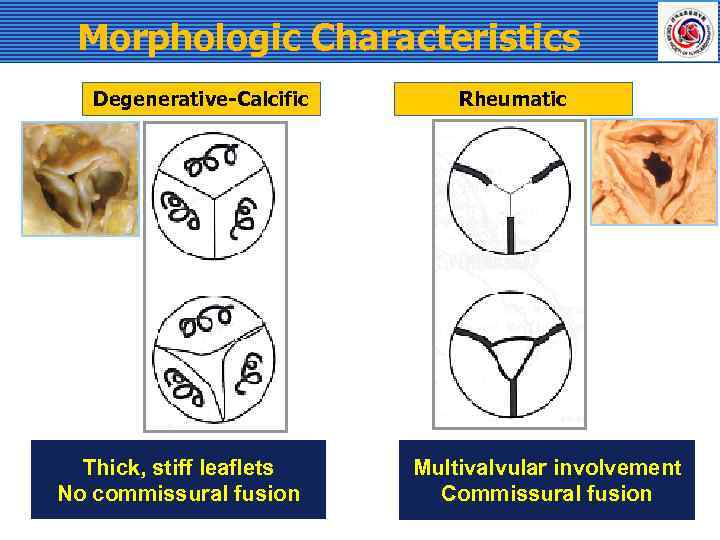 Morphologic Characteristics Degenerative-Calcific Thick, stiff leaflets No commissural fusion Rheumatic Multivalvular involvement Commissural fusion
Morphologic Characteristics Degenerative-Calcific Thick, stiff leaflets No commissural fusion Rheumatic Multivalvular involvement Commissural fusion
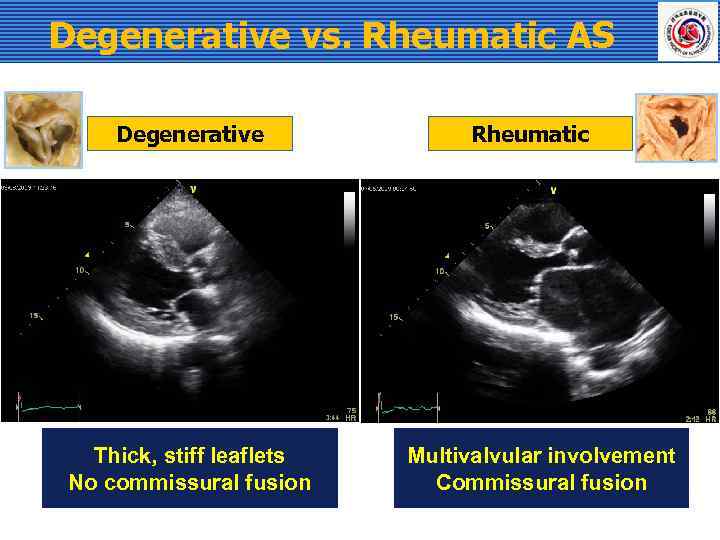 Degenerative vs. Rheumatic AS Degenerative Thick, stiff leaflets No commissural fusion Rheumatic Multivalvular involvement Commissural fusion
Degenerative vs. Rheumatic AS Degenerative Thick, stiff leaflets No commissural fusion Rheumatic Multivalvular involvement Commissural fusion
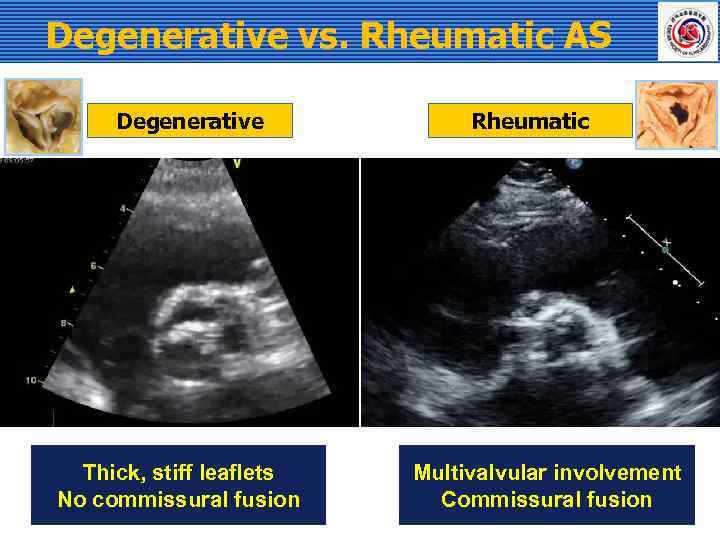 Degenerative vs. Rheumatic AS Degenerative Thick, stiff leaflets No commissural fusion Rheumatic Multivalvular involvement Commissural fusion
Degenerative vs. Rheumatic AS Degenerative Thick, stiff leaflets No commissural fusion Rheumatic Multivalvular involvement Commissural fusion
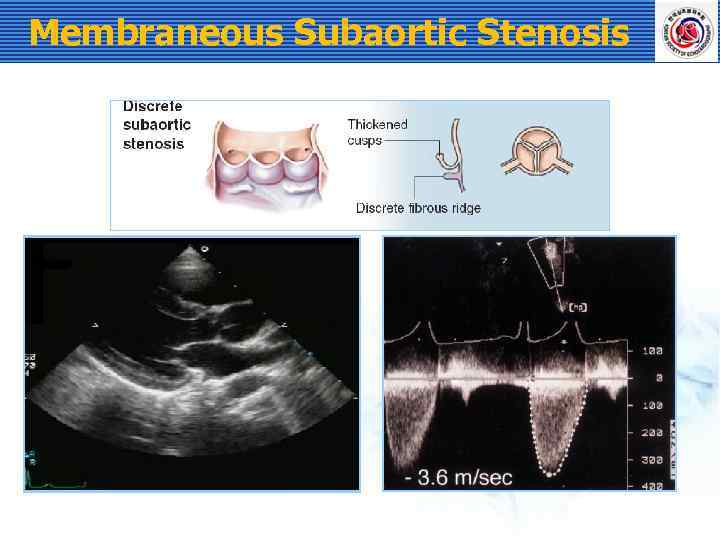 Membraneous Subaortic Stenosis
Membraneous Subaortic Stenosis
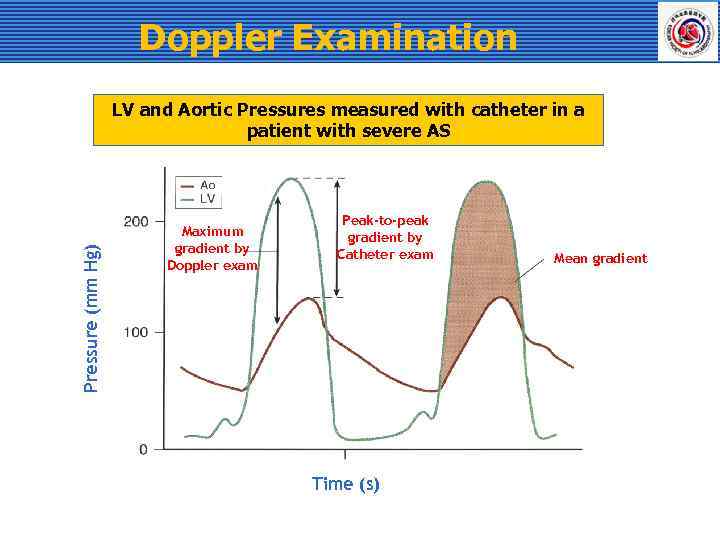 Doppler Examination Pressure (mm Hg) LV and Aortic Pressures measured with catheter in a patient with severe AS Maximum gradient by Doppler exam Peak-to-peak gradient by Catheter exam Time (s) Mean gradient
Doppler Examination Pressure (mm Hg) LV and Aortic Pressures measured with catheter in a patient with severe AS Maximum gradient by Doppler exam Peak-to-peak gradient by Catheter exam Time (s) Mean gradient
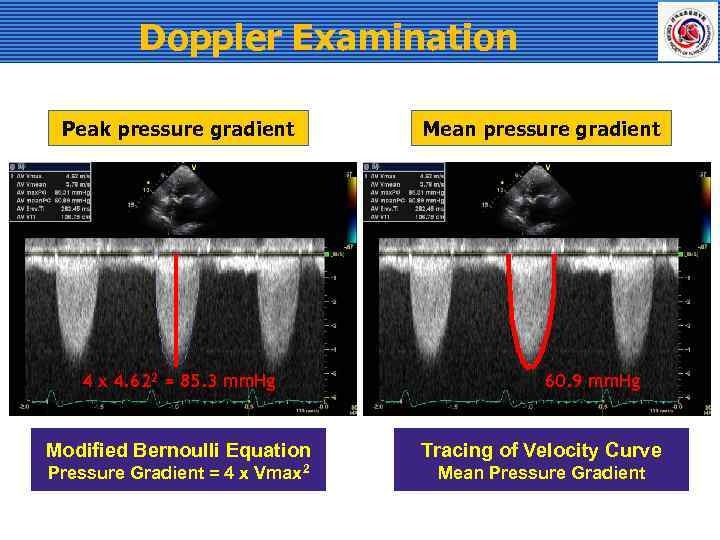 Doppler Examination Peak pressure gradient 4 x 4. 622 = 85. 3 mm. Hg Mean pressure gradient 60. 9 mm. Hg Modified Bernoulli Equation Tracing of Velocity Curve Pressure Gradient = 4 x Vmax 2 Mean Pressure Gradient
Doppler Examination Peak pressure gradient 4 x 4. 622 = 85. 3 mm. Hg Mean pressure gradient 60. 9 mm. Hg Modified Bernoulli Equation Tracing of Velocity Curve Pressure Gradient = 4 x Vmax 2 Mean Pressure Gradient
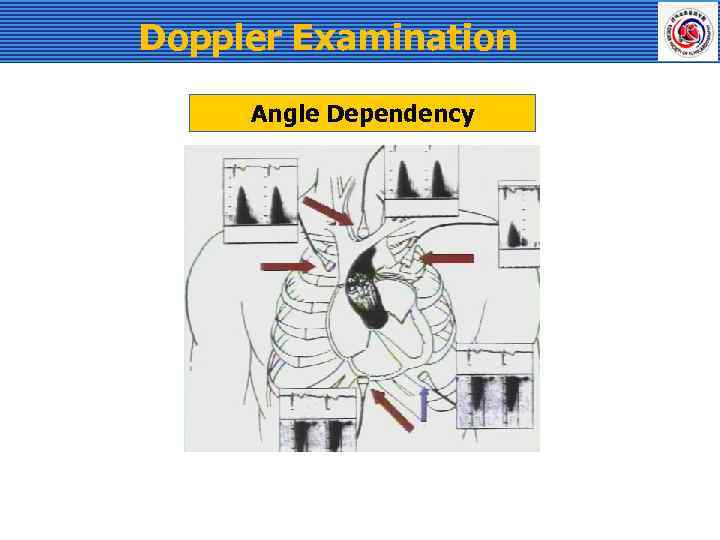 Doppler Examination Angle Dependency
Doppler Examination Angle Dependency
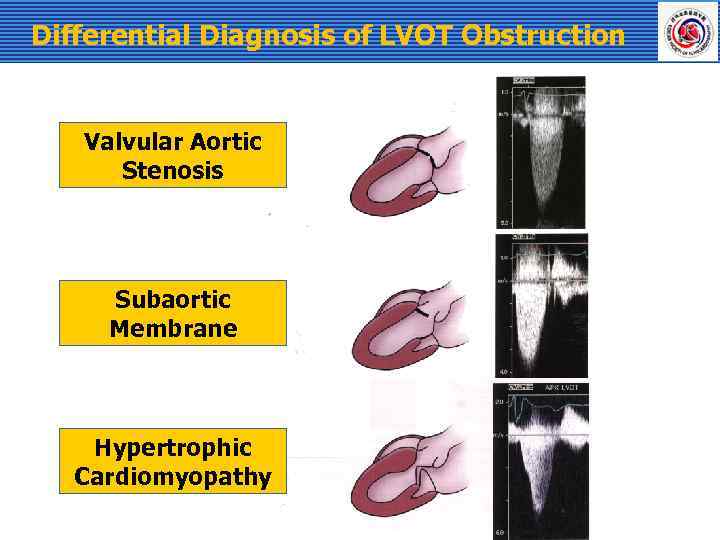 Differential Diagnosis of LVOT Obstruction Valvular Aortic Stenosis Subaortic Membrane Hypertrophic Cardiomyopathy
Differential Diagnosis of LVOT Obstruction Valvular Aortic Stenosis Subaortic Membrane Hypertrophic Cardiomyopathy
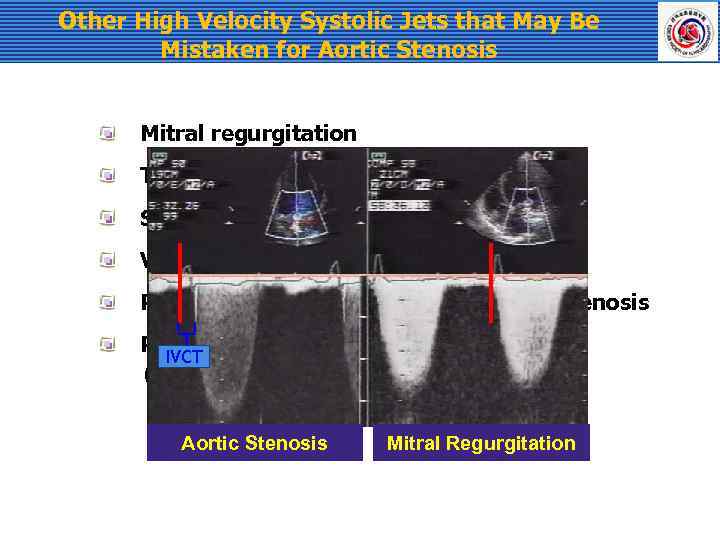 Other High Velocity Systolic Jets that May Be Mistaken for Aortic Stenosis Mitral regurgitation Tricuspid regurgitation Supravalvular stenosis Ventricular septal defect Pulmonic or branch pulmonary artery stenosis Peripheral vascular stenosis IVCT (e. q. , subclavian artery) Aortic Stenosis Mitral Regurgitation
Other High Velocity Systolic Jets that May Be Mistaken for Aortic Stenosis Mitral regurgitation Tricuspid regurgitation Supravalvular stenosis Ventricular septal defect Pulmonic or branch pulmonary artery stenosis Peripheral vascular stenosis IVCT (e. q. , subclavian artery) Aortic Stenosis Mitral Regurgitation
 Calculation of Valve Area 2 D Planimetry Continuity equation
Calculation of Valve Area 2 D Planimetry Continuity equation
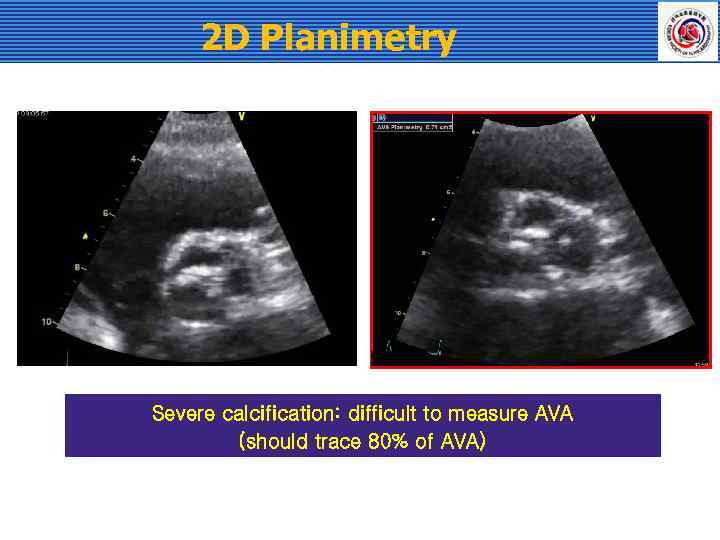 2 D Planimetry Severe calcification: difficult to measure AVA (should trace 80% of AVA)
2 D Planimetry Severe calcification: difficult to measure AVA (should trace 80% of AVA)
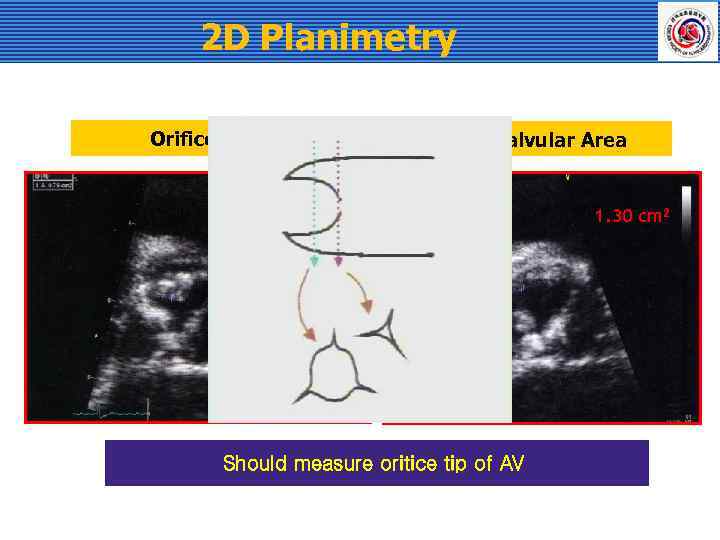 2 D Planimetry Orifice Tip Subvalvular Area 0. 76 cm 2 Should measure oritice tip of AV 1. 30 cm 2
2 D Planimetry Orifice Tip Subvalvular Area 0. 76 cm 2 Should measure oritice tip of AV 1. 30 cm 2
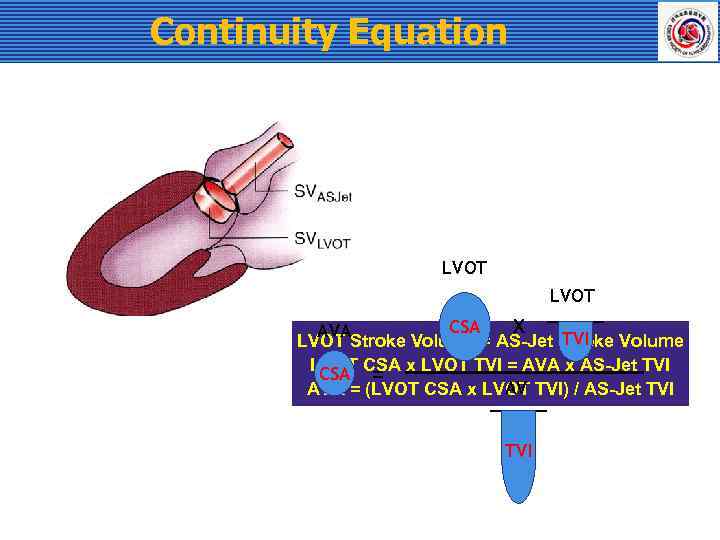 Continuity Equation LVOT X CSA AVA TVI LVOT Stroke Volume = AS-Jet Stroke Volume LVOT CSA x LVOT TVI = AVA x AS-Jet TVI CSA = AV AVA = (LVOT CSA x LVOT TVI) / AS-Jet TVI
Continuity Equation LVOT X CSA AVA TVI LVOT Stroke Volume = AS-Jet Stroke Volume LVOT CSA x LVOT TVI = AVA x AS-Jet TVI CSA = AV AVA = (LVOT CSA x LVOT TVI) / AS-Jet TVI
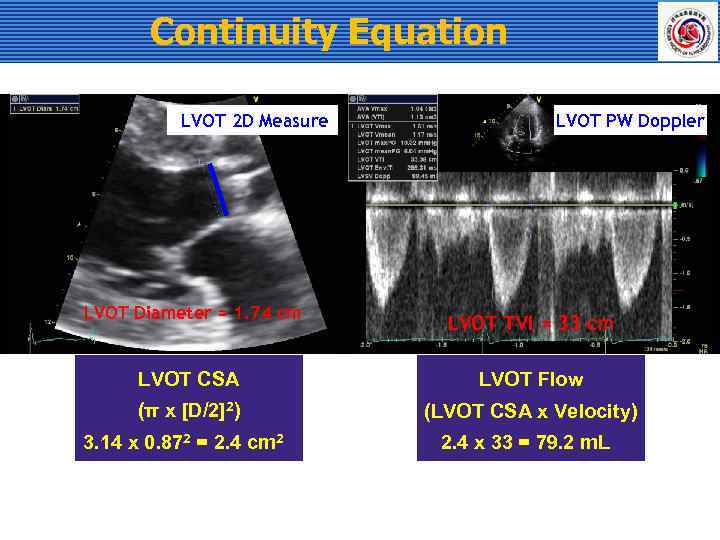 Continuity Equation LVOT 2 D Measure LVOT PW Doppler LVOT Diameter = 1. 74 cm LVOT TVI = 33 cm LVOT CSA LVOT Flow (π x [D/2]2) (LVOT CSA x Velocity) 3. 14 x 0. 872 = 2. 4 cm 2 2. 4 x 33 = 79. 2 m. L
Continuity Equation LVOT 2 D Measure LVOT PW Doppler LVOT Diameter = 1. 74 cm LVOT TVI = 33 cm LVOT CSA LVOT Flow (π x [D/2]2) (LVOT CSA x Velocity) 3. 14 x 0. 872 = 2. 4 cm 2 2. 4 x 33 = 79. 2 m. L
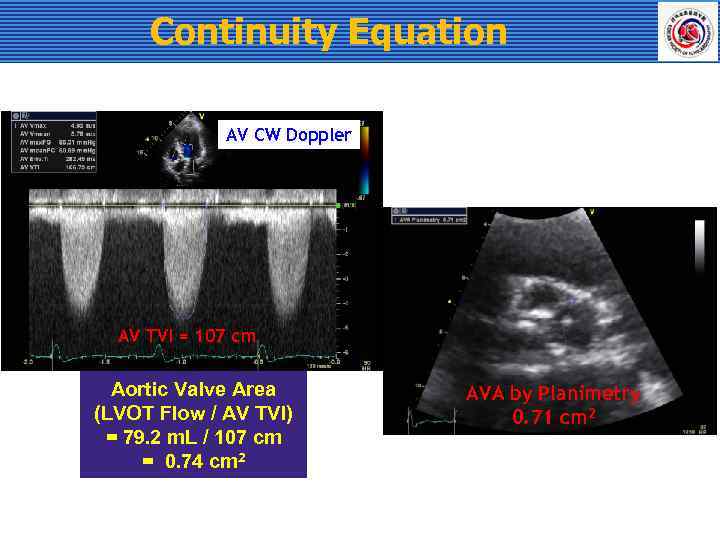 Continuity Equation AV CW Doppler AV TVI = 107 cm Aortic Valve Area (LVOT Flow / AV TVI) = 79. 2 m. L / 107 cm = 0. 74 cm 2 AVA by Planimetry 0. 71 cm 2
Continuity Equation AV CW Doppler AV TVI = 107 cm Aortic Valve Area (LVOT Flow / AV TVI) = 79. 2 m. L / 107 cm = 0. 74 cm 2 AVA by Planimetry 0. 71 cm 2
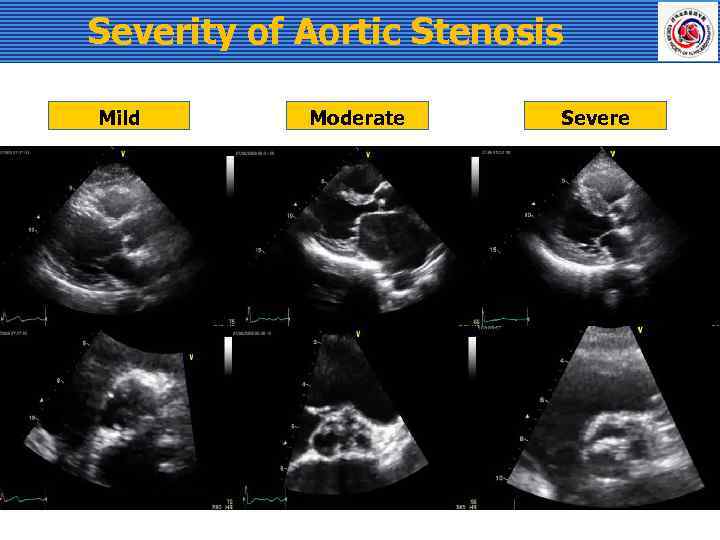 Severity of Aortic Stenosis Mild Moderate Severe
Severity of Aortic Stenosis Mild Moderate Severe
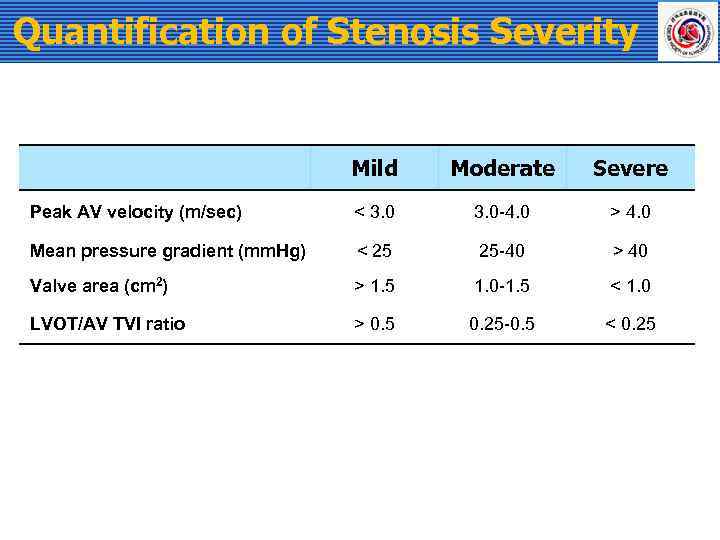 Quantification of Stenosis Severity Mild Moderate Severe Peak AV velocity (m/sec) < 3. 0 -4. 0 > 4. 0 Mean pressure gradient (mm. Hg) < 25 25 -40 > 40 Valve area (cm 2) > 1. 5 1. 0 -1. 5 < 1. 0 LVOT/AV TVI ratio > 0. 5 0. 25 -0. 5 < 0. 25
Quantification of Stenosis Severity Mild Moderate Severe Peak AV velocity (m/sec) < 3. 0 -4. 0 > 4. 0 Mean pressure gradient (mm. Hg) < 25 25 -40 > 40 Valve area (cm 2) > 1. 5 1. 0 -1. 5 < 1. 0 LVOT/AV TVI ratio > 0. 5 0. 25 -0. 5 < 0. 25
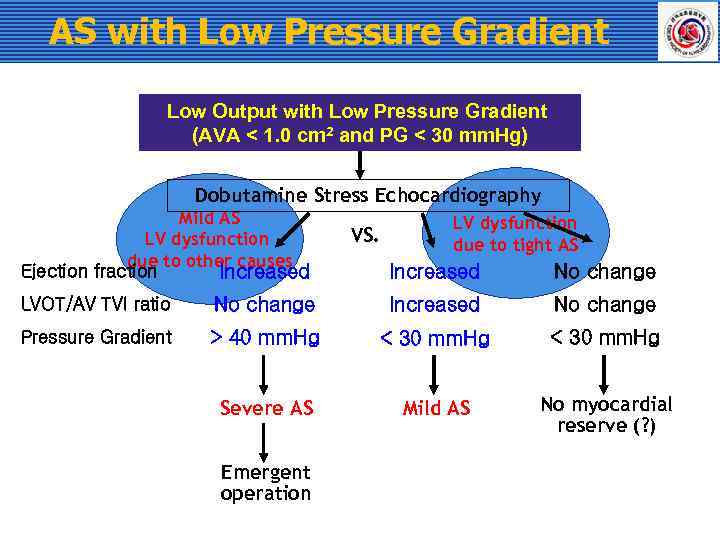 AS with Low Pressure Gradient Low Output with Low Pressure Gradient (AVA < 1. 0 cm 2 and PG < 30 mm. Hg) Dobutamine Stress Echocardiography Mild AS LV dysfunction due to other causes Ejection fraction Increased VS. LV dysfunction due to tight AS Increased No change LVOT/AV TVI ratio No change Increased No change Pressure Gradient > 40 mm. Hg < 30 mm. Hg Severe AS Mild AS No myocardial reserve (? ) Emergent operation
AS with Low Pressure Gradient Low Output with Low Pressure Gradient (AVA < 1. 0 cm 2 and PG < 30 mm. Hg) Dobutamine Stress Echocardiography Mild AS LV dysfunction due to other causes Ejection fraction Increased VS. LV dysfunction due to tight AS Increased No change LVOT/AV TVI ratio No change Increased No change Pressure Gradient > 40 mm. Hg < 30 mm. Hg Severe AS Mild AS No myocardial reserve (? ) Emergent operation
 Aortic Regurgitation
Aortic Regurgitation
 Etiology of Aortic Regurgitation Cusp pathology Aortic wall pathology including aortitis Congenital
Etiology of Aortic Regurgitation Cusp pathology Aortic wall pathology including aortitis Congenital
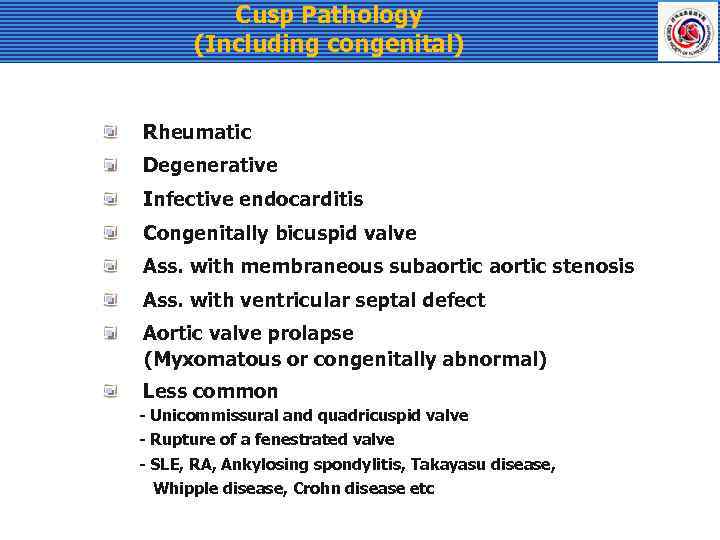 Cusp Pathology (Including congenital) Rheumatic Degenerative Infective endocarditis Congenitally bicuspid valve Ass. with membraneous subaortic stenosis Ass. with ventricular septal defect Aortic valve prolapse (Myxomatous or congenitally abnormal) Less common - Unicommissural and quadricuspid valve - Rupture of a fenestrated valve - SLE, RA, Ankylosing spondylitis, Takayasu disease, Whipple disease, Crohn disease etc
Cusp Pathology (Including congenital) Rheumatic Degenerative Infective endocarditis Congenitally bicuspid valve Ass. with membraneous subaortic stenosis Ass. with ventricular septal defect Aortic valve prolapse (Myxomatous or congenitally abnormal) Less common - Unicommissural and quadricuspid valve - Rupture of a fenestrated valve - SLE, RA, Ankylosing spondylitis, Takayasu disease, Whipple disease, Crohn disease etc
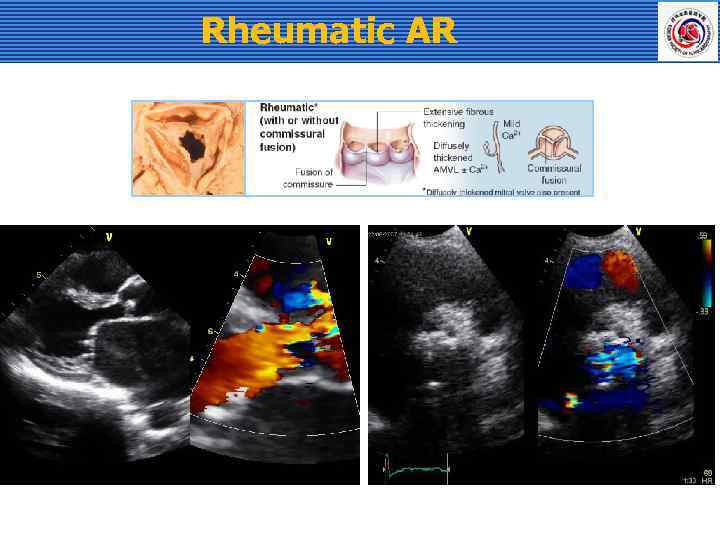 Rheumatic AR
Rheumatic AR
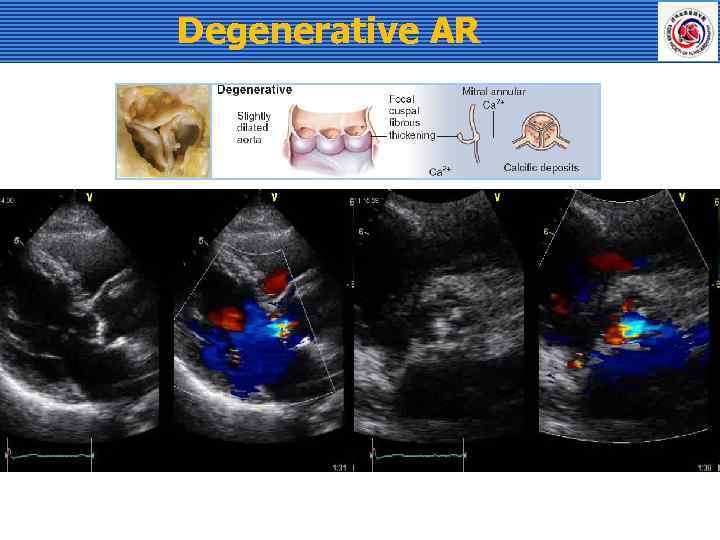 Degenerative AR
Degenerative AR
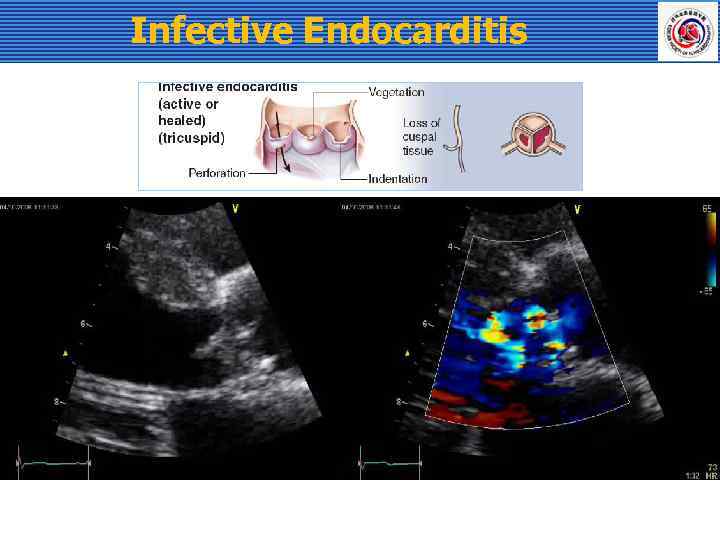 Infective Endocarditis
Infective Endocarditis
 Bicuspid Aortic Valve
Bicuspid Aortic Valve
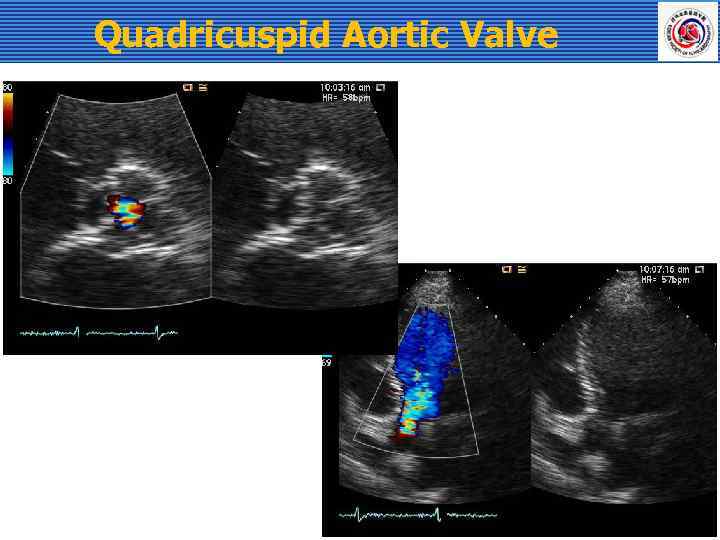 Quadricuspid Aortic Valve
Quadricuspid Aortic Valve
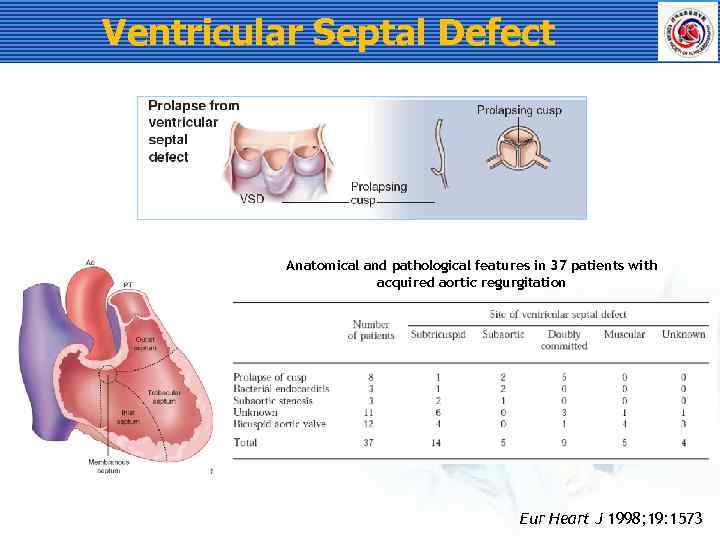 Ventricular Septal Defect Anatomical and pathological features in 37 patients with acquired aortic regurgitation Eur Heart J 1998; 19: 1573
Ventricular Septal Defect Anatomical and pathological features in 37 patients with acquired aortic regurgitation Eur Heart J 1998; 19: 1573
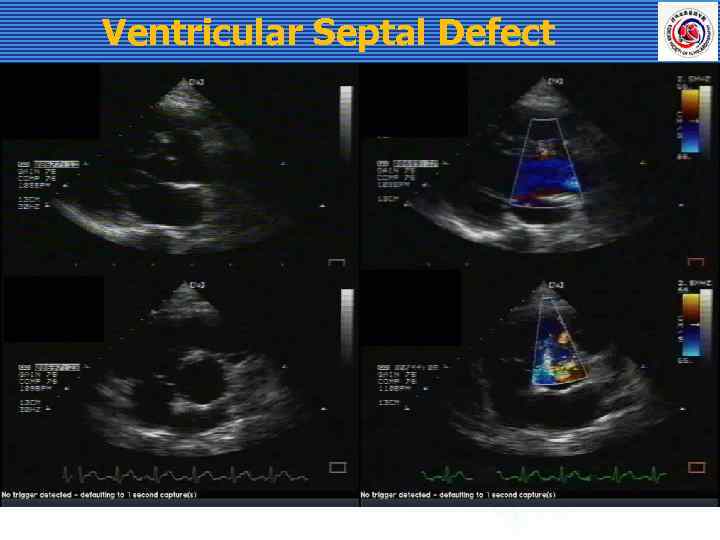 Ventricular Septal Defect
Ventricular Septal Defect
 Aortic Valve Prolapse Best seen in parasternal long axis view Disruption of commissural support - Dissection - Dilatation - Ass. with VSD - Myxomatous or congenitally abnormality
Aortic Valve Prolapse Best seen in parasternal long axis view Disruption of commissural support - Dissection - Dilatation - Ass. with VSD - Myxomatous or congenitally abnormality
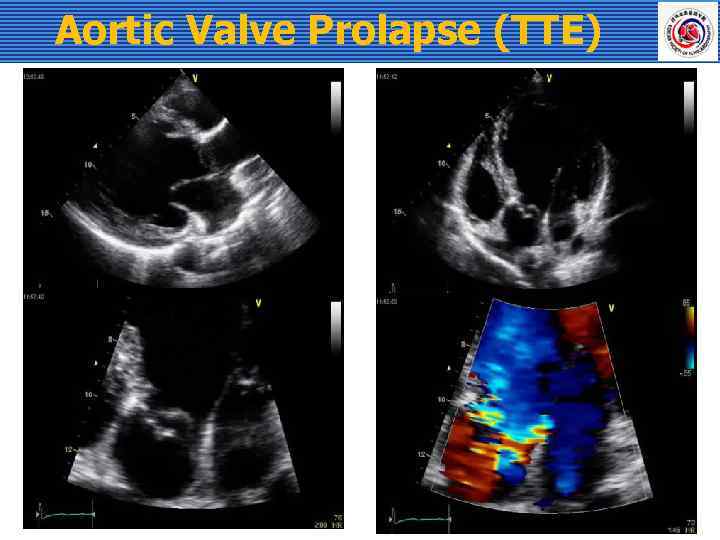 Aortic Valve Prolapse (TTE)
Aortic Valve Prolapse (TTE)
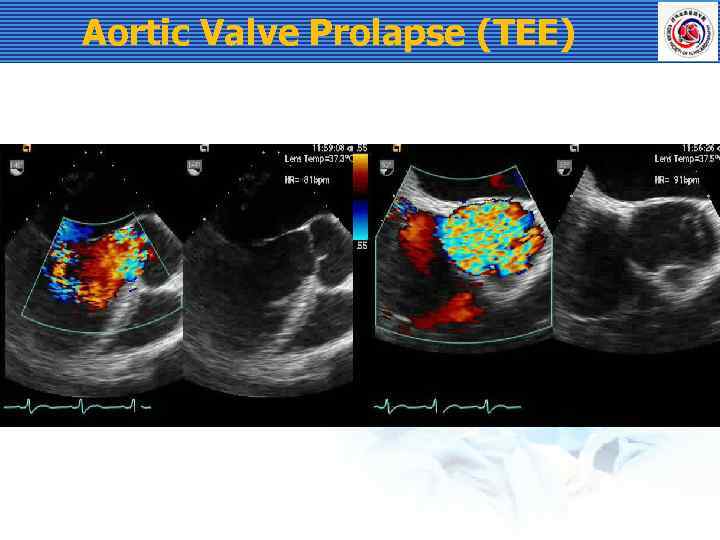 Aortic Valve Prolapse (TEE)
Aortic Valve Prolapse (TEE)
 Aortic Root Disease Aortic dilatation related with - Hypertension - Age-related (degenerative) - Bicuspid AV Aortic dissection Cystic medial necrosis (Marfan syndrome) Takayasu arteritis Behcet’s disease Ankylosing spondylitis Less common - Syphilitic aortitis, psoriatic arthritis, UC, giant cell arteritis - relapsing polychondritis, Reiter syndrome
Aortic Root Disease Aortic dilatation related with - Hypertension - Age-related (degenerative) - Bicuspid AV Aortic dissection Cystic medial necrosis (Marfan syndrome) Takayasu arteritis Behcet’s disease Ankylosing spondylitis Less common - Syphilitic aortitis, psoriatic arthritis, UC, giant cell arteritis - relapsing polychondritis, Reiter syndrome
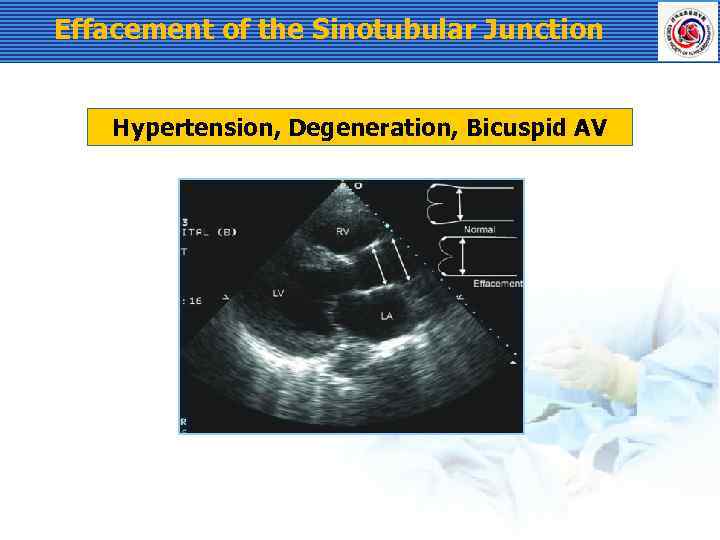 Effacement of the Sinotubular Junction Hypertension, Degeneration, Bicuspid AV
Effacement of the Sinotubular Junction Hypertension, Degeneration, Bicuspid AV
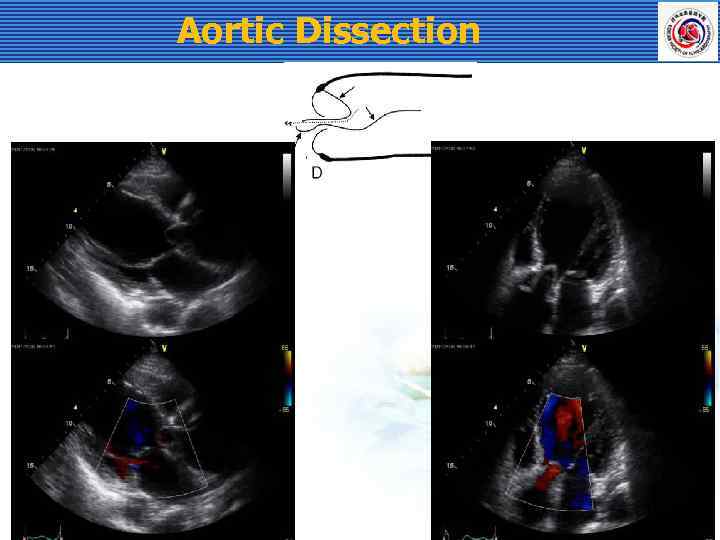 Aortic Dissection
Aortic Dissection
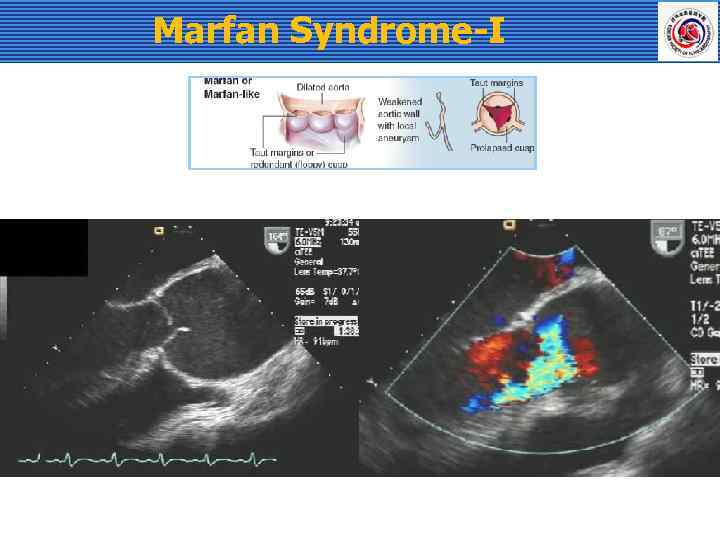 Marfan Syndrome-I
Marfan Syndrome-I
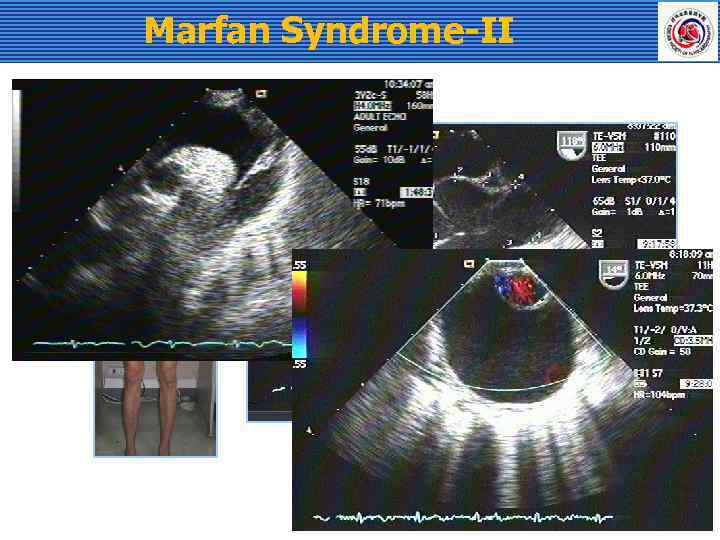 Marfan Syndrome-II
Marfan Syndrome-II
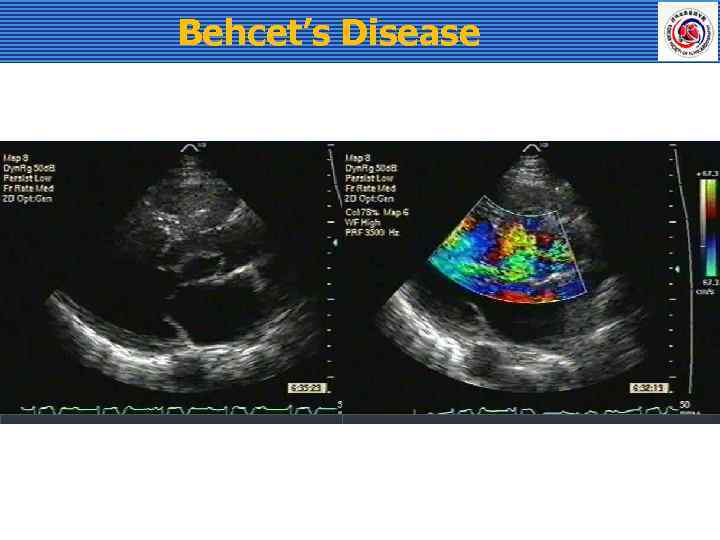 Behcet’s Disease
Behcet’s Disease
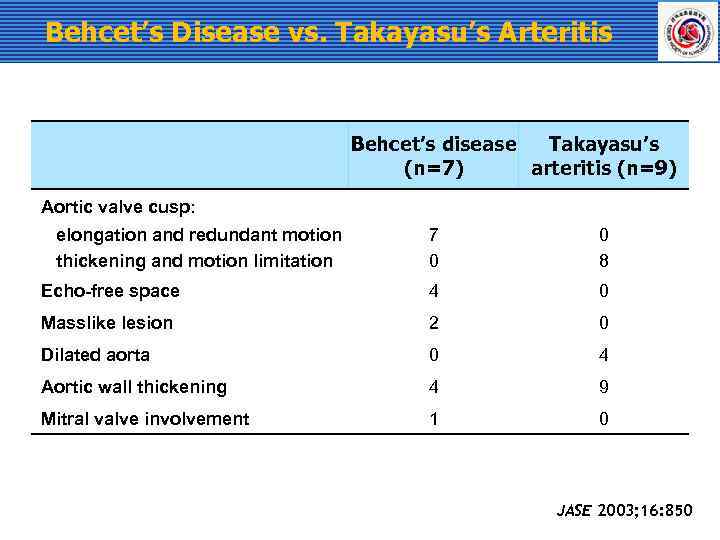 Behcet’s Disease vs. Takayasu’s Arteritis Behcet’s disease Takayasu’s (n=7) arteritis (n=9) Aortic valve cusp: elongation and redundant motion thickening and motion limitation 7 0 0 8 Echo-free space 4 0 Masslike lesion 2 0 Dilated aorta 0 4 Aortic wall thickening 4 9 Mitral valve involvement 1 0 JASE 2003; 16: 850
Behcet’s Disease vs. Takayasu’s Arteritis Behcet’s disease Takayasu’s (n=7) arteritis (n=9) Aortic valve cusp: elongation and redundant motion thickening and motion limitation 7 0 0 8 Echo-free space 4 0 Masslike lesion 2 0 Dilated aorta 0 4 Aortic wall thickening 4 9 Mitral valve involvement 1 0 JASE 2003; 16: 850
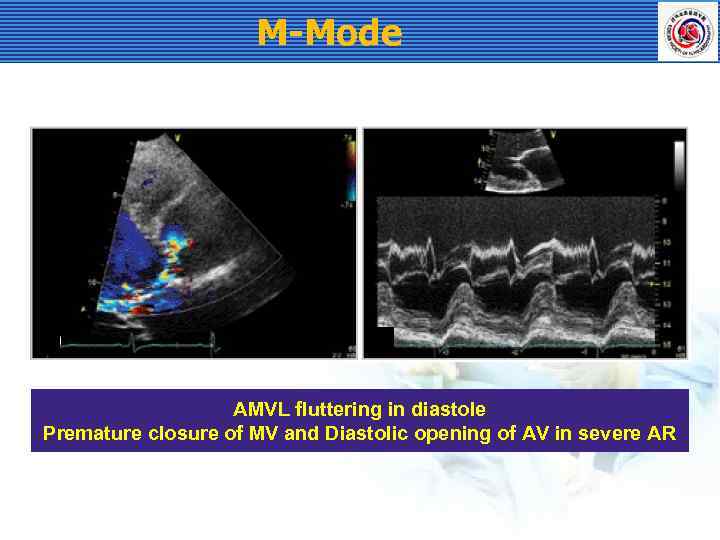 M-Mode AMVL fluttering in diastole Premature closure of MV and Diastolic opening of AV in severe AR
M-Mode AMVL fluttering in diastole Premature closure of MV and Diastolic opening of AV in severe AR
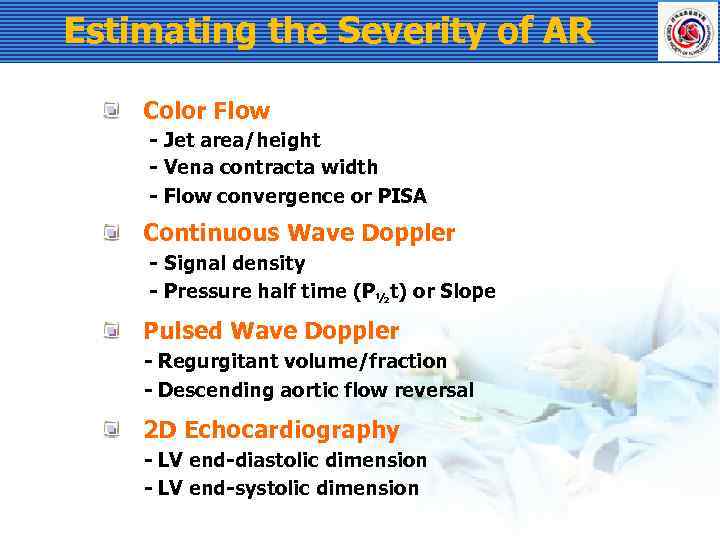 Estimating the Severity of AR Color Flow - Jet area/height - Vena contracta width - Flow convergence or PISA Continuous Wave Doppler - Signal density - Pressure half time (P½t) or Slope Pulsed Wave Doppler - Regurgitant volume/fraction - Descending aortic flow reversal 2 D Echocardiography - LV end-diastolic dimension - LV end-systolic dimension
Estimating the Severity of AR Color Flow - Jet area/height - Vena contracta width - Flow convergence or PISA Continuous Wave Doppler - Signal density - Pressure half time (P½t) or Slope Pulsed Wave Doppler - Regurgitant volume/fraction - Descending aortic flow reversal 2 D Echocardiography - LV end-diastolic dimension - LV end-systolic dimension
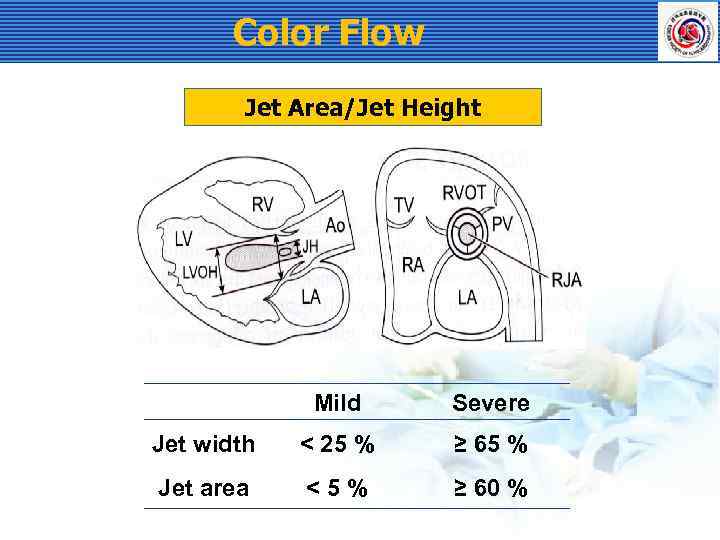 Color Flow Jet Area/Jet Height Mild Severe Jet width < 25 % ≥ 65 % Jet area <5% ≥ 60 %
Color Flow Jet Area/Jet Height Mild Severe Jet width < 25 % ≥ 65 % Jet area <5% ≥ 60 %
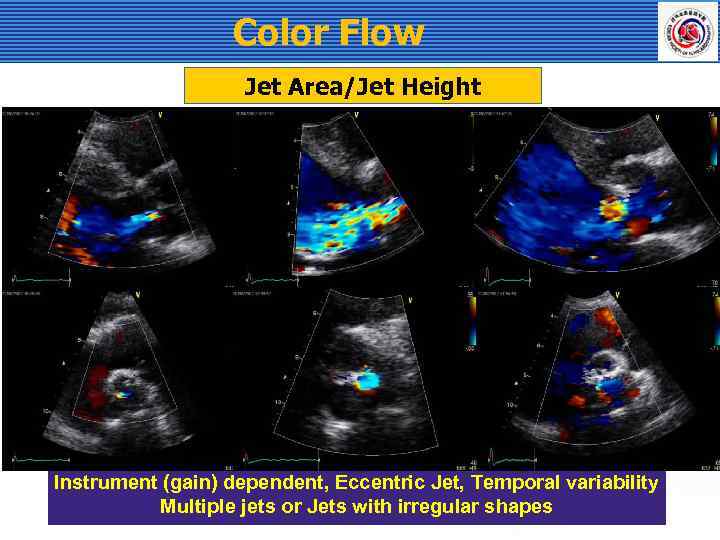 Color Flow Jet Area/Jet Height Instrument (gain) dependent, Eccentric Jet, Temporal variability Multiple jets or Jets with irregular shapes
Color Flow Jet Area/Jet Height Instrument (gain) dependent, Eccentric Jet, Temporal variability Multiple jets or Jets with irregular shapes
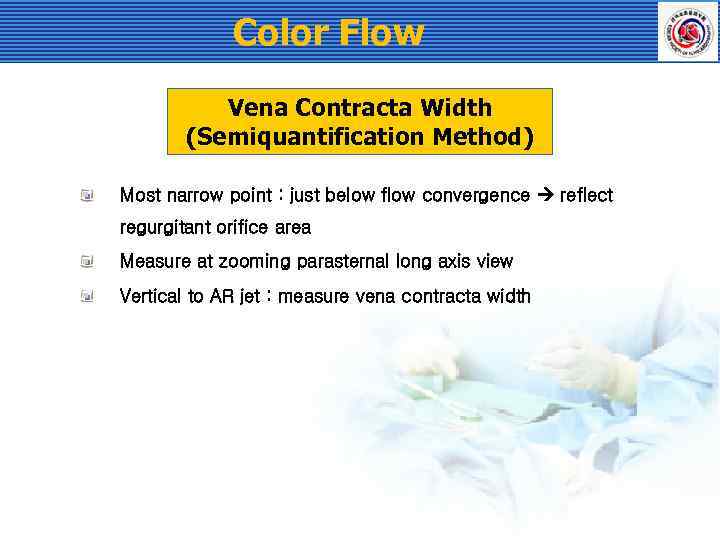 Color Flow Vena Contracta Width (Semiquantification Method) Most narrow point : just below flow convergence reflect regurgitant orifice area Measure at zooming parasternal long axis view Vertical to AR jet : measure vena contracta width
Color Flow Vena Contracta Width (Semiquantification Method) Most narrow point : just below flow convergence reflect regurgitant orifice area Measure at zooming parasternal long axis view Vertical to AR jet : measure vena contracta width
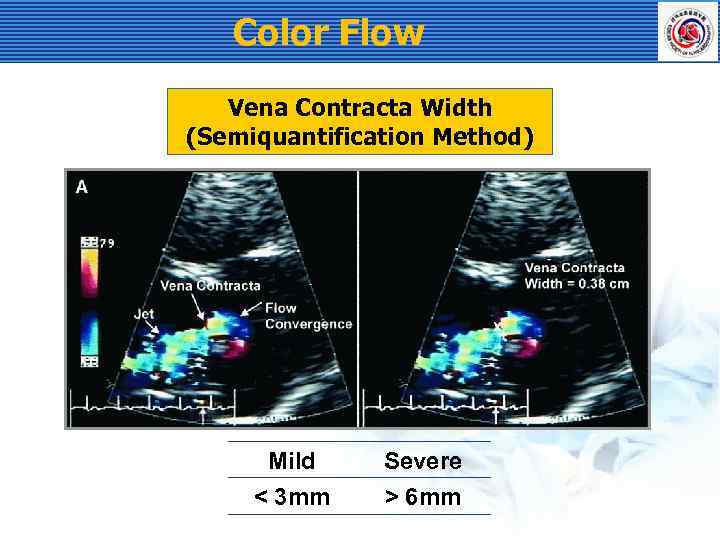 Color Flow Vena Contracta Width (Semiquantification Method) Mild Severe < 3 mm > 6 mm
Color Flow Vena Contracta Width (Semiquantification Method) Mild Severe < 3 mm > 6 mm
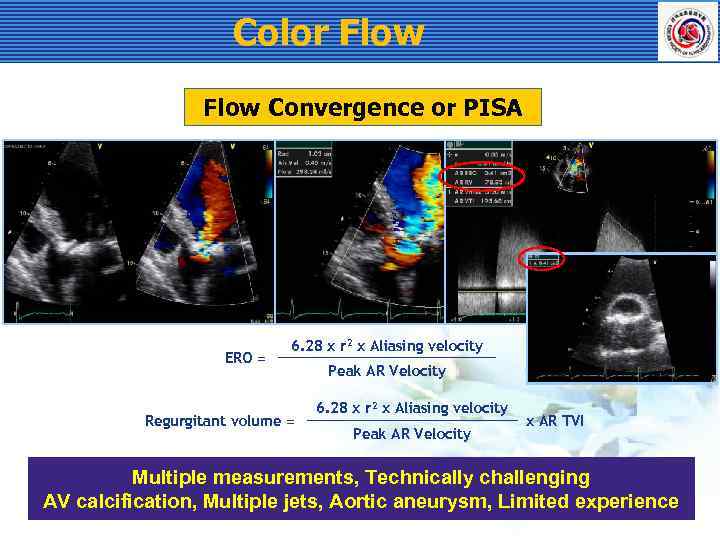 Color Flow Convergence or PISA ERO = 6. 28 x r 2 x Aliasing velocity Regurgitant volume = Peak AR Velocity 6. 28 x r 2 x Aliasing velocity Peak AR Velocity x AR TVI Multiple measurements, Technically challenging AV calcification, Multiple jets, Aortic aneurysm, Limited experience
Color Flow Convergence or PISA ERO = 6. 28 x r 2 x Aliasing velocity Regurgitant volume = Peak AR Velocity 6. 28 x r 2 x Aliasing velocity Peak AR Velocity x AR TVI Multiple measurements, Technically challenging AV calcification, Multiple jets, Aortic aneurysm, Limited experience
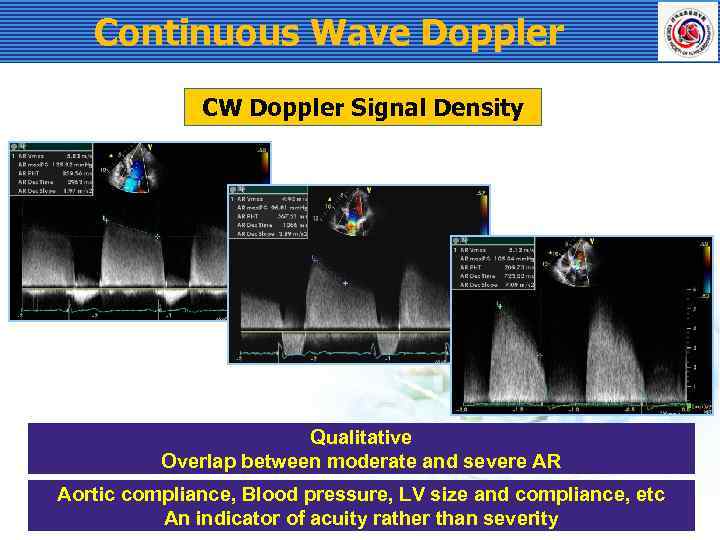 Continuous Wave Doppler CW Doppler Signal Density Qualitative Overlap between moderate and severe AR Aortic compliance, Blood pressure, LV size and compliance, etc An indicator of acuity rather than severity
Continuous Wave Doppler CW Doppler Signal Density Qualitative Overlap between moderate and severe AR Aortic compliance, Blood pressure, LV size and compliance, etc An indicator of acuity rather than severity
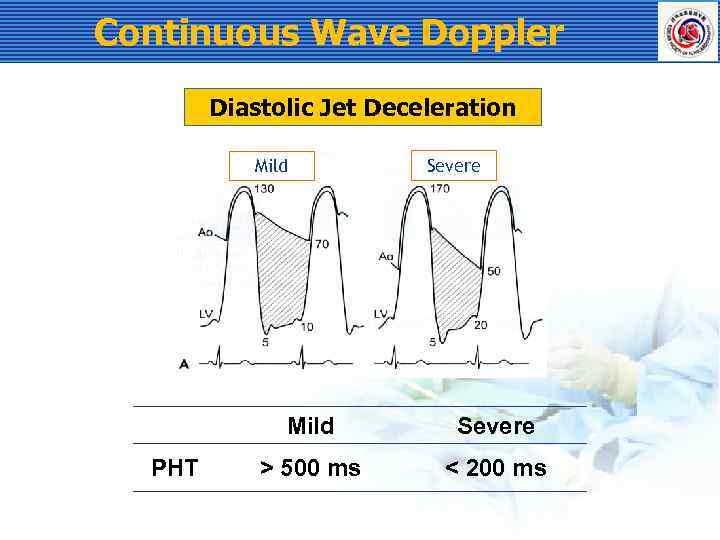 Continuous Wave Doppler Diastolic Jet Deceleration Mild Severe Mild PHT Severe > 500 ms < 200 ms
Continuous Wave Doppler Diastolic Jet Deceleration Mild Severe Mild PHT Severe > 500 ms < 200 ms
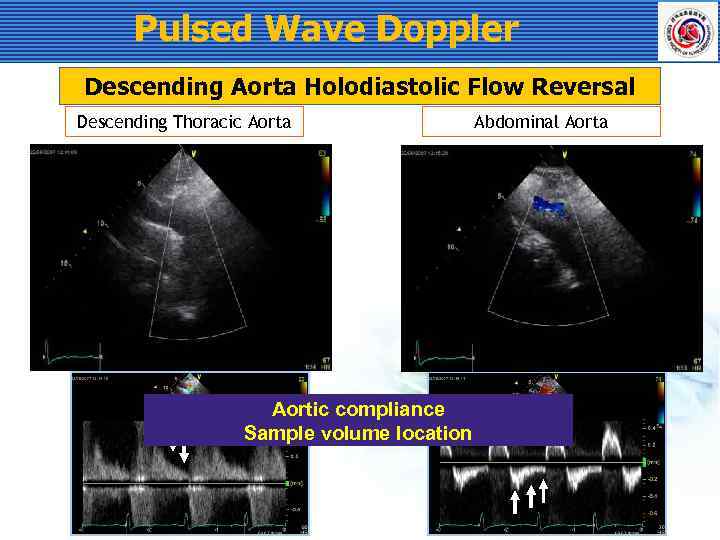 Pulsed Wave Doppler Descending Aorta Holodiastolic Flow Reversal Descending Thoracic Aorta Aortic compliance Sample volume location Abdominal Aorta
Pulsed Wave Doppler Descending Aorta Holodiastolic Flow Reversal Descending Thoracic Aorta Aortic compliance Sample volume location Abdominal Aorta
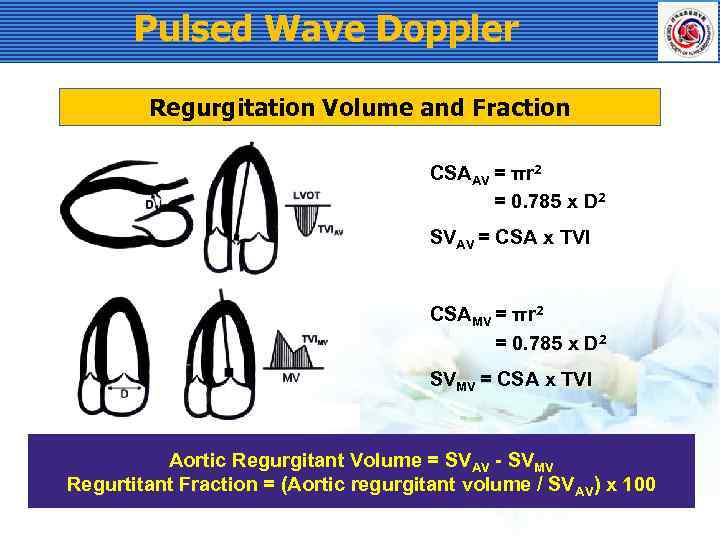 Pulsed Wave Doppler Regurgitation Volume and Fraction CSAAV = πr 2 = 0. 785 x D 2 SVAV = CSA x TVI CSAMV = πr 2 = 0. 785 x D 2 SVMV = CSA x TVI Aortic Regurgitant Volume = SVAV - SVMV Regurtitant Fraction = (Aortic regurgitant volume / SVAV) x 100
Pulsed Wave Doppler Regurgitation Volume and Fraction CSAAV = πr 2 = 0. 785 x D 2 SVAV = CSA x TVI CSAMV = πr 2 = 0. 785 x D 2 SVMV = CSA x TVI Aortic Regurgitant Volume = SVAV - SVMV Regurtitant Fraction = (Aortic regurgitant volume / SVAV) x 100
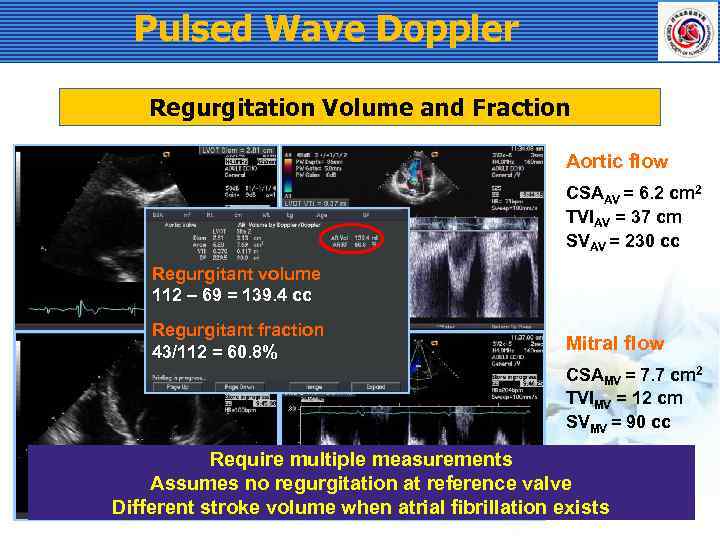 Pulsed Wave Doppler Regurgitation Volume and Fraction Aortic flow CSAAV = 6. 2 cm 2 TVIAV = 37 cm SVAV = 230 cc Regurgitant volume 112 – 69 = 139. 4 cc Regurgitant fraction 43/112 = 60. 8% Mitral flow CSAMV = 7. 7 cm 2 TVIMV = 12 cm SVMV = 90 cc Require multiple measurements Assumes no regurgitation at reference valve Different stroke volume when atrial fibrillation exists
Pulsed Wave Doppler Regurgitation Volume and Fraction Aortic flow CSAAV = 6. 2 cm 2 TVIAV = 37 cm SVAV = 230 cc Regurgitant volume 112 – 69 = 139. 4 cc Regurgitant fraction 43/112 = 60. 8% Mitral flow CSAMV = 7. 7 cm 2 TVIMV = 12 cm SVMV = 90 cc Require multiple measurements Assumes no regurgitation at reference valve Different stroke volume when atrial fibrillation exists
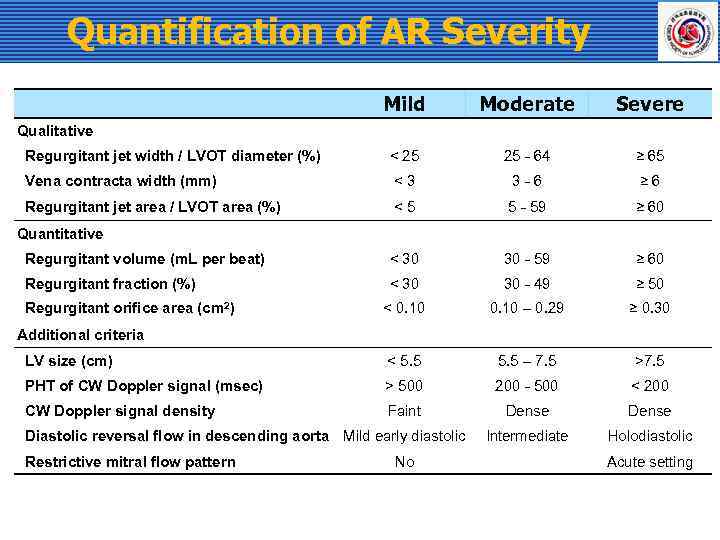 Quantification of AR Severity Mild Moderate Severe Regurgitant jet width / LVOT diameter (%) < 25 25 - 64 ≥ 65 Vena contracta width (mm) <3 3 -6 ≥ 6 Regurgitant jet area / LVOT area (%) <5 5 - 59 ≥ 60 Regurgitant volume (m. L per beat) < 30 30 - 59 ≥ 60 Regurgitant fraction (%) < 30 30 - 49 ≥ 50 < 0. 10 – 0. 29 ≥ 0. 30 LV size (cm) < 5. 5 – 7. 5 >7. 5 PHT of CW Doppler signal (msec) > 500 200 - 500 < 200 CW Doppler signal density Faint Dense Intermediate Holodiastolic Qualitative Quantitative Regurgitant orifice area (cm 2) Additional criteria Diastolic reversal flow in descending aorta Mild early diastolic Restrictive mitral flow pattern No Acute setting
Quantification of AR Severity Mild Moderate Severe Regurgitant jet width / LVOT diameter (%) < 25 25 - 64 ≥ 65 Vena contracta width (mm) <3 3 -6 ≥ 6 Regurgitant jet area / LVOT area (%) <5 5 - 59 ≥ 60 Regurgitant volume (m. L per beat) < 30 30 - 59 ≥ 60 Regurgitant fraction (%) < 30 30 - 49 ≥ 50 < 0. 10 – 0. 29 ≥ 0. 30 LV size (cm) < 5. 5 – 7. 5 >7. 5 PHT of CW Doppler signal (msec) > 500 200 - 500 < 200 CW Doppler signal density Faint Dense Intermediate Holodiastolic Qualitative Quantitative Regurgitant orifice area (cm 2) Additional criteria Diastolic reversal flow in descending aorta Mild early diastolic Restrictive mitral flow pattern No Acute setting
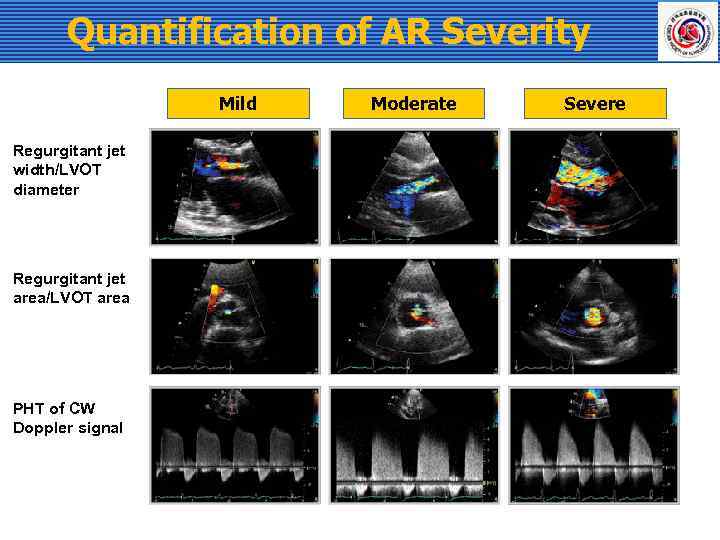 Quantification of AR Severity Mild Regurgitant jet width/LVOT diameter Regurgitant jet area/LVOT area PHT of CW Doppler signal Moderate Severe
Quantification of AR Severity Mild Regurgitant jet width/LVOT diameter Regurgitant jet area/LVOT area PHT of CW Doppler signal Moderate Severe
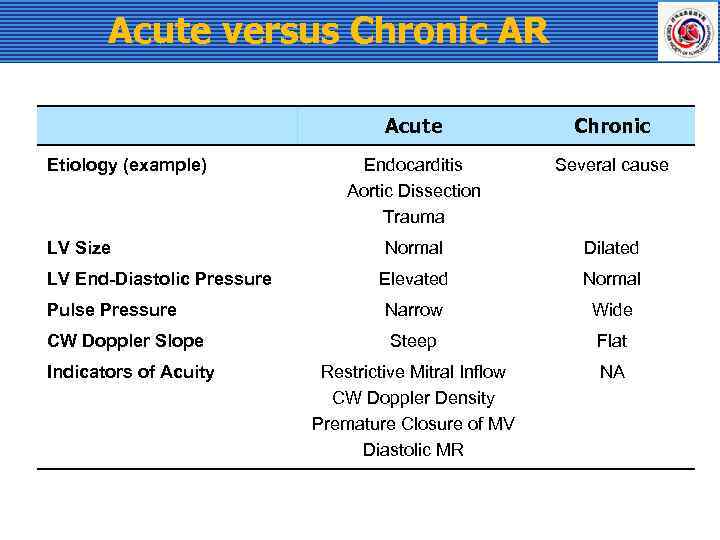 Acute versus Chronic AR Acute Etiology (example) LV Size LV End-Diastolic Pressure Pulse Pressure CW Doppler Slope Indicators of Acuity Chronic Endocarditis Aortic Dissection Trauma Several cause Normal Dilated Elevated Normal Narrow Wide Steep Flat Restrictive Mitral Inflow CW Doppler Density Premature Closure of MV Diastolic MR NA
Acute versus Chronic AR Acute Etiology (example) LV Size LV End-Diastolic Pressure Pulse Pressure CW Doppler Slope Indicators of Acuity Chronic Endocarditis Aortic Dissection Trauma Several cause Normal Dilated Elevated Normal Narrow Wide Steep Flat Restrictive Mitral Inflow CW Doppler Density Premature Closure of MV Diastolic MR NA
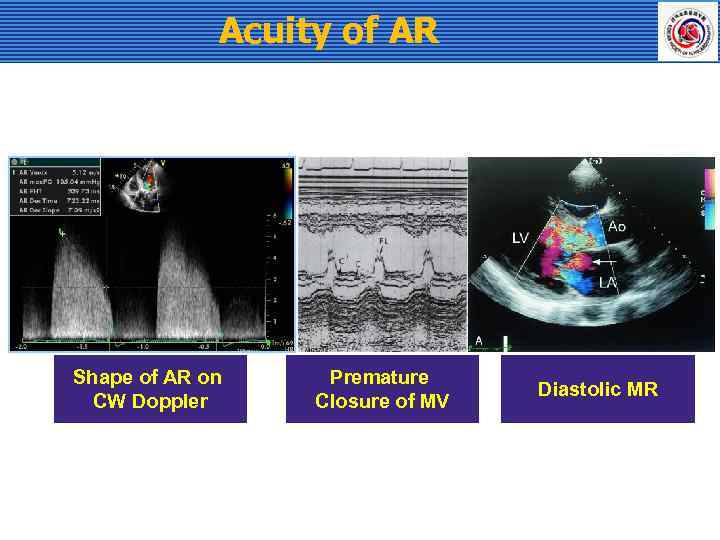 Acuity of AR Shape of AR on CW Doppler Premature Closure of MV Diastolic MR
Acuity of AR Shape of AR on CW Doppler Premature Closure of MV Diastolic MR



