Aortic & Systemic Disease Classification 65% 20%10%







































- Размер: 10.3 Mегабайта
- Количество слайдов: 55
Описание презентации Aortic & Systemic Disease Classification 65% 20%10% по слайдам
 Aortic & Systemic Disease
Aortic & Systemic Disease
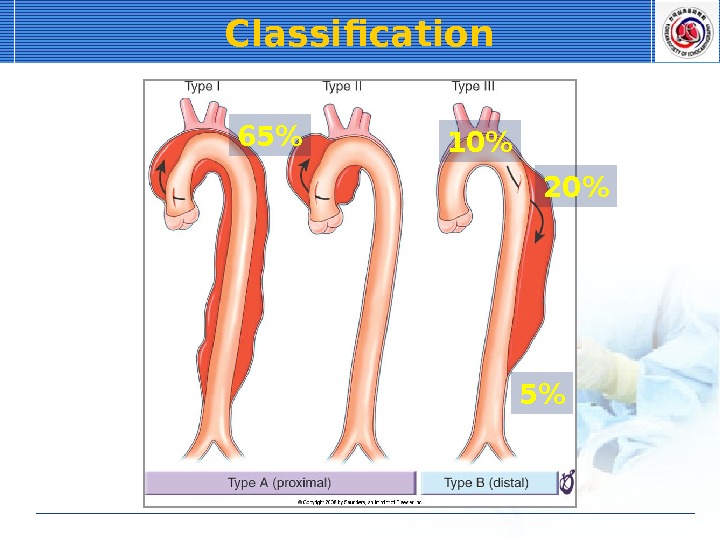
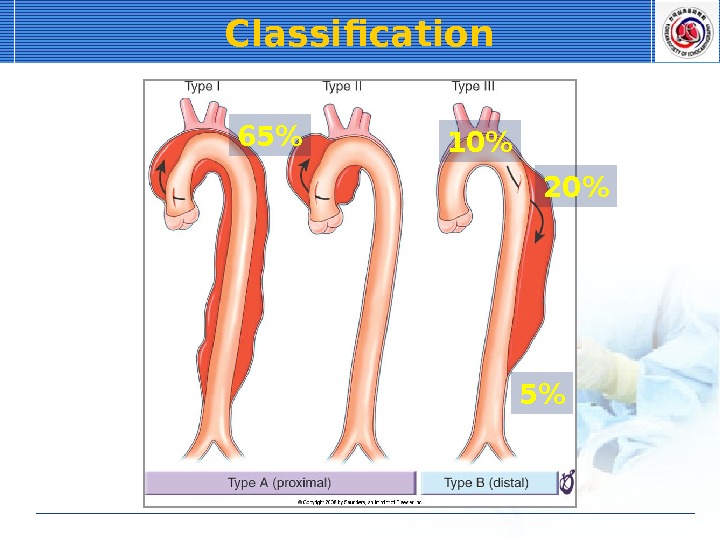 Classification 65% 20%10% 5%
Classification 65% 20%10% 5%
 Symptoms Pain 96% of patients Sudden severe onset Tearing, ripping, sharp, stabbing Migrating pain (17%) Location • Anterior only: ascending aorta in 90% • Interscapular only: descending thoracic aorta in 90% • Neck, throat, jaw, face: ascending aorta • Back, abdomen, lower extremities: descending aorta Pleuritic pain • Hemopericardium
Symptoms Pain 96% of patients Sudden severe onset Tearing, ripping, sharp, stabbing Migrating pain (17%) Location • Anterior only: ascending aorta in 90% • Interscapular only: descending thoracic aorta in 90% • Neck, throat, jaw, face: ascending aorta • Back, abdomen, lower extremities: descending aorta Pleuritic pain • Hemopericardium
 Laboratory Findings Chest X-ray Widening of the aortic silhouette • 81 – 90% Calcium sign • Intimal calcification from the outer aortic border > 1 cm • Suggestive Pleural effusion • Left side Normal chest X-ray • Up to 12%
Laboratory Findings Chest X-ray Widening of the aortic silhouette • 81 – 90% Calcium sign • Intimal calcification from the outer aortic border > 1 cm • Suggestive Pleural effusion • Left side Normal chest X-ray • Up to 12%
 Calcium Sign
Calcium Sign
 Diagnostic Techniques Contrast-enhanced CT Diagnostic clues • 2 distinct aortic lumen and intimal flap • 3 -dimensional display by spiral CT – Aorta and branches
Diagnostic Techniques Contrast-enhanced CT Diagnostic clues • 2 distinct aortic lumen and intimal flap • 3 -dimensional display by spiral CT – Aorta and branches
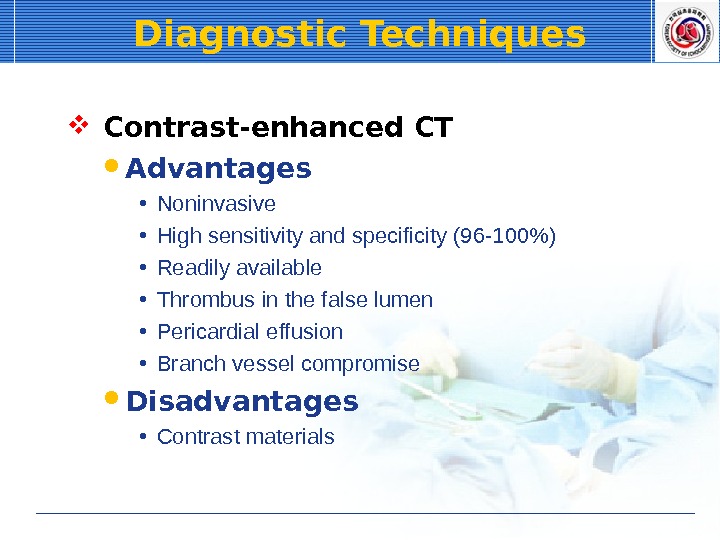
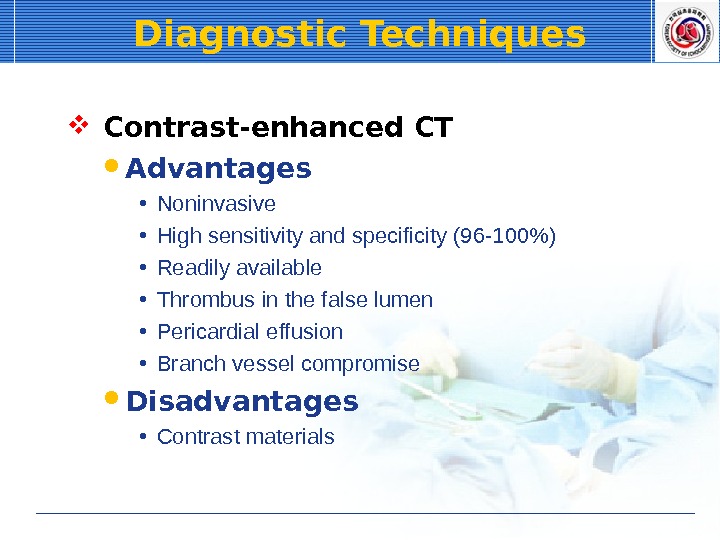 Diagnostic Techniques Contrast-enhanced CT Advantages • Noninvasive • High sensitivity and specificity (96 -100%) • Readily available • Thrombus in the false lumen • Pericardial effusion • Branch vessel compromise Disadvantages • Contrast materials
Diagnostic Techniques Contrast-enhanced CT Advantages • Noninvasive • High sensitivity and specificity (96 -100%) • Readily available • Thrombus in the false lumen • Pericardial effusion • Branch vessel compromise Disadvantages • Contrast materials
 Diagnostic Techniques Transthoracic echocardiography (TTE)
Diagnostic Techniques Transthoracic echocardiography (TTE)
 Diagnostic Techniques Transthoracic echocardiography (TTE)
Diagnostic Techniques Transthoracic echocardiography (TTE)
 Diagnostic Techniques Transthoracic echocardiography (TTE)
Diagnostic Techniques Transthoracic echocardiography (TTE)
 Diagnostic Techniques Transthoracic echocardiography (TTE)
Diagnostic Techniques Transthoracic echocardiography (TTE)
 Diagnostic Techniques Transthoracic echocardiography (TTE)
Diagnostic Techniques Transthoracic echocardiography (TTE)
 Diagnostic Techniques Transthoracic echocardiography (TTE)
Diagnostic Techniques Transthoracic echocardiography (TTE)
 Diagnostic Techniques Echocardiography Advantages • Readily available • Noninvasive • Quick to perform at the bedside Transthoracic echocardiography (TTE) • Sensitivity: 59 – 85% • Specificity: 63 – 96% • Limited by image quality
Diagnostic Techniques Echocardiography Advantages • Readily available • Noninvasive • Quick to perform at the bedside Transthoracic echocardiography (TTE) • Sensitivity: 59 – 85% • Specificity: 63 – 96% • Limited by image quality
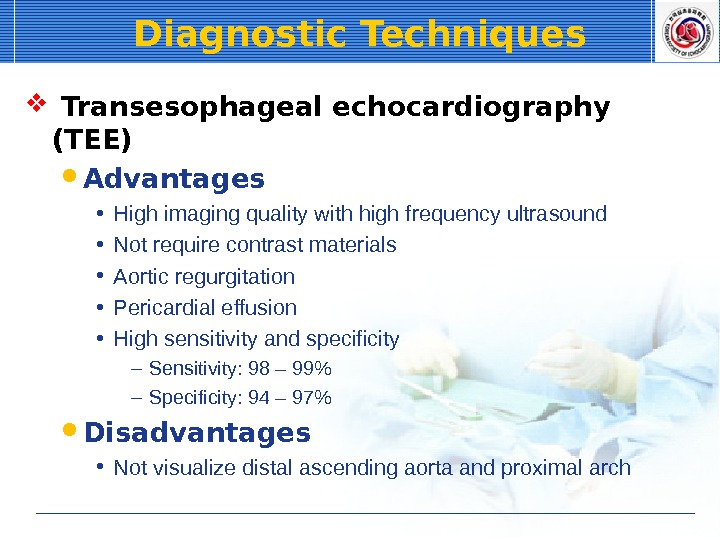
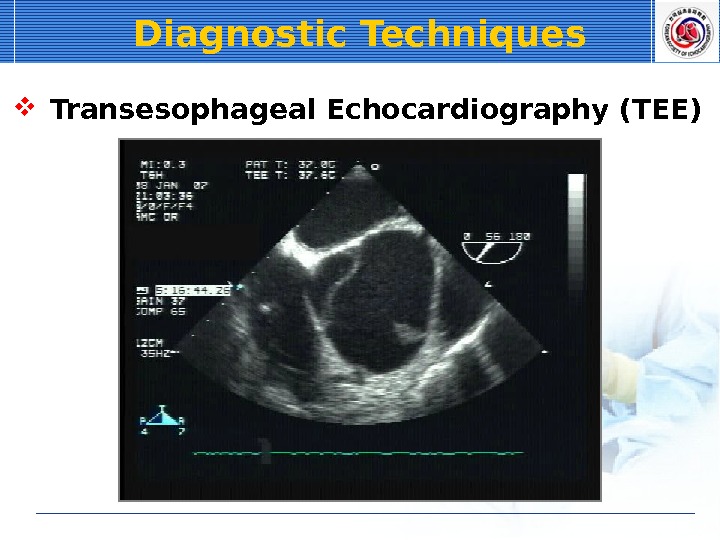
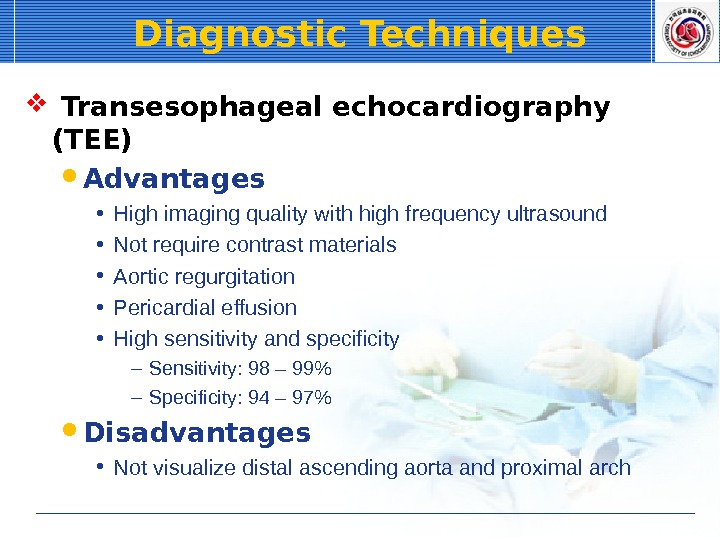 Diagnostic Techniques Transesophageal echocardiography (TEE) Advantages • High imaging quality with high frequency ultrasound • Not require contrast materials • Aortic regurgitation • Pericardial effusion • High sensitivity and specificity – Sensitivity: 98 – 99% – Specificity: 94 – 97% Disadvantages • Not visualize distal ascending aorta and proximal arch
Diagnostic Techniques Transesophageal echocardiography (TEE) Advantages • High imaging quality with high frequency ultrasound • Not require contrast materials • Aortic regurgitation • Pericardial effusion • High sensitivity and specificity – Sensitivity: 98 – 99% – Specificity: 94 – 97% Disadvantages • Not visualize distal ascending aorta and proximal arch
 Diagnostic Techniques Transesophageal Echocardiography (TEE)
Diagnostic Techniques Transesophageal Echocardiography (TEE)
 Diagnostic Techniques Transesophageal Echocardiography (TEE)
Diagnostic Techniques Transesophageal Echocardiography (TEE)
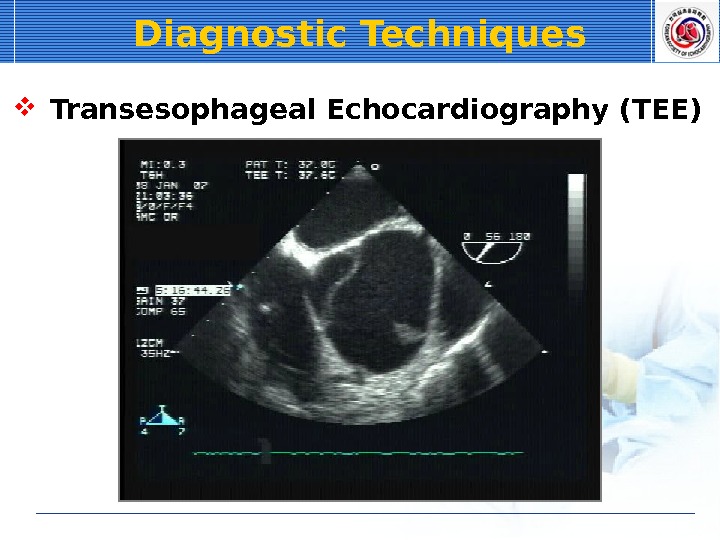 Diagnostic Techniques Transesophageal Echocardiography (TEE)
Diagnostic Techniques Transesophageal Echocardiography (TEE)
 Diagnostic Techniques Transesophageal Echocardiography (TEE)
Diagnostic Techniques Transesophageal Echocardiography (TEE)
 Diagnostic Techniques Transesophageal Echocardiography (TEE)
Diagnostic Techniques Transesophageal Echocardiography (TEE)
 Immediate Medical Management Blood pressure reduction Goal • Systolic BP: 100 – 120 mm. Hg • Heart rate: 60 – 80 / m • Reducing d. P/dt (beta blocker) Pain control • Morphine
Immediate Medical Management Blood pressure reduction Goal • Systolic BP: 100 – 120 mm. Hg • Heart rate: 60 – 80 / m • Reducing d. P/dt (beta blocker) Pain control • Morphine
 Immediate Medical Management Blood pressure reduction Anticipating aorta surgery • Sodium nitroprusside • Esmolol Labetalol • Alpha and beta blocking Contraindicated to beta blocker • Severe sinus bradycardia, AV block, bronchospasm, congestive heart failure • Diltiazem, verapamil • ACE inhibitors
Immediate Medical Management Blood pressure reduction Anticipating aorta surgery • Sodium nitroprusside • Esmolol Labetalol • Alpha and beta blocking Contraindicated to beta blocker • Severe sinus bradycardia, AV block, bronchospasm, congestive heart failure • Diltiazem, verapamil • ACE inhibitors
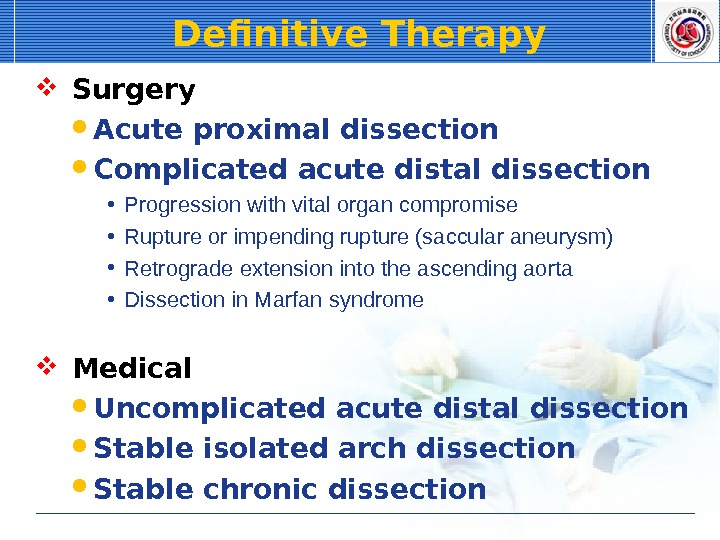
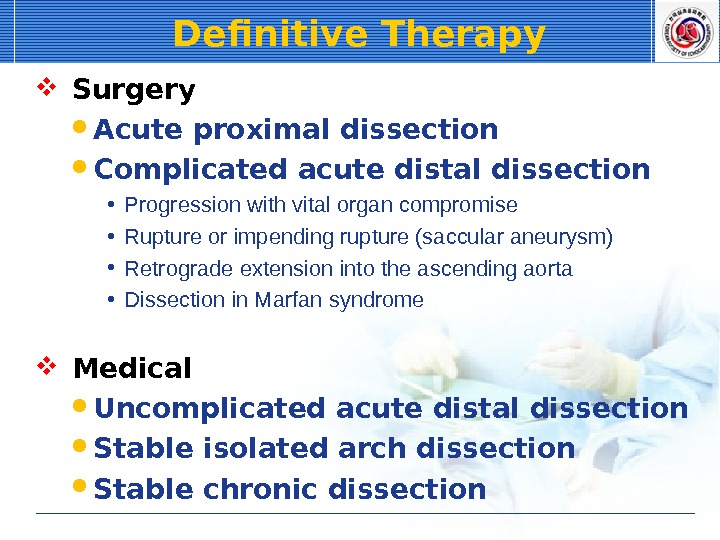 Definitive Therapy Surgery Acute proximal dissection Complicated acute distal dissection • Progression with vital organ compromise • Rupture or impending rupture (saccular aneurysm) • Retrograde extension into the ascending aorta • Dissection in Marfan syndrome Medical Uncomplicated acute distal dissection Stable isolated arch dissection Stable chronic dissection
Definitive Therapy Surgery Acute proximal dissection Complicated acute distal dissection • Progression with vital organ compromise • Rupture or impending rupture (saccular aneurysm) • Retrograde extension into the ascending aorta • Dissection in Marfan syndrome Medical Uncomplicated acute distal dissection Stable isolated arch dissection Stable chronic dissection
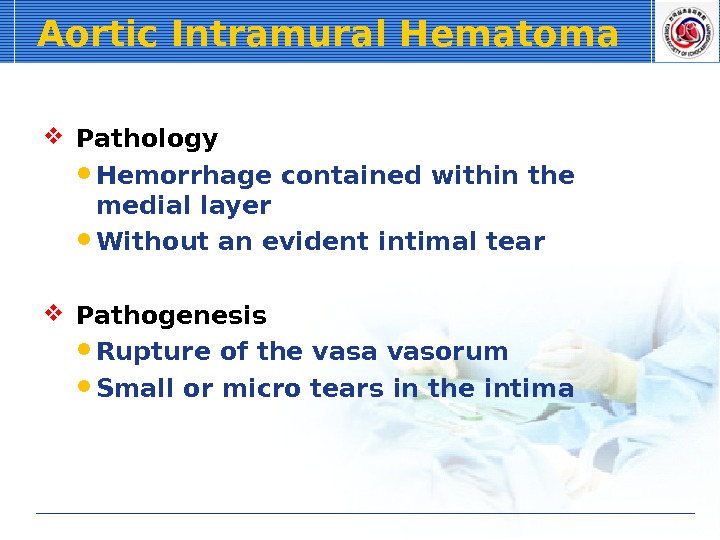
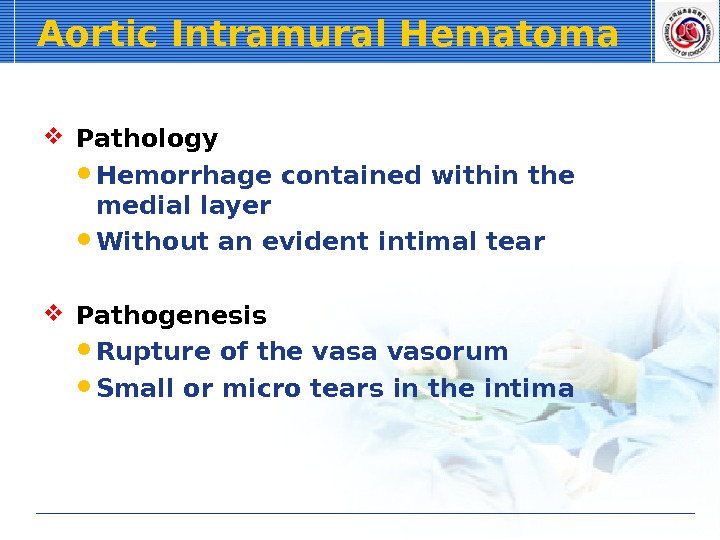 Aortic Intramural Hematoma Pathology Hemorrhage contained within the medial layer Without an evident intimal tear Pathogenesis Rupture of the vasa vasorum Small or micro tears in the intima
Aortic Intramural Hematoma Pathology Hemorrhage contained within the medial layer Without an evident intimal tear Pathogenesis Rupture of the vasa vasorum Small or micro tears in the intima
 Aortic Intramural Hematoma Computed tomography
Aortic Intramural Hematoma Computed tomography
 Aortic Intramural Hematoma T
Aortic Intramural Hematoma T
 Aortic Intramural Hematoma T
Aortic Intramural Hematoma T
 Aortic Intramural Hematoma T
Aortic Intramural Hematoma T
 Abdominal Aortic Aneurysm
Abdominal Aortic Aneurysm
 Abdominal Aortic Aneurysm
Abdominal Aortic Aneurysm
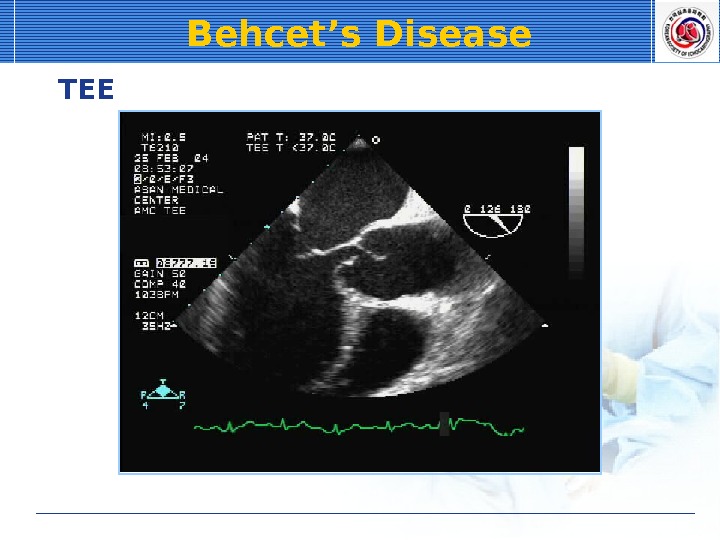
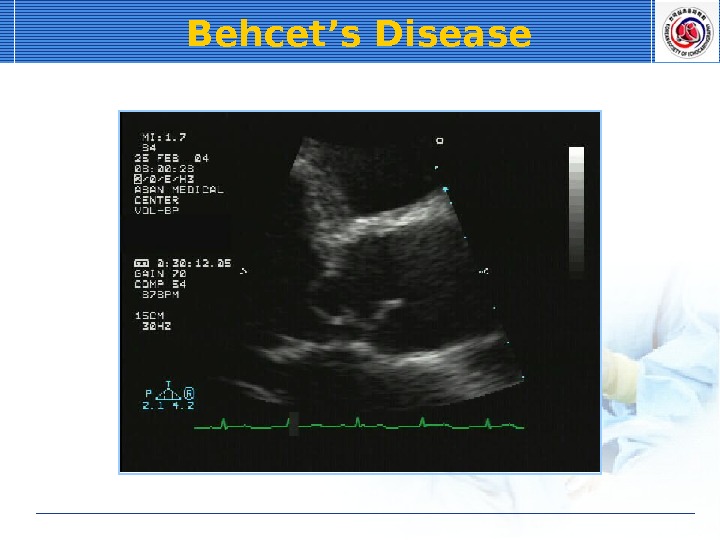 Behcet’s Disease
Behcet’s Disease
 Behcet’s Disease
Behcet’s Disease
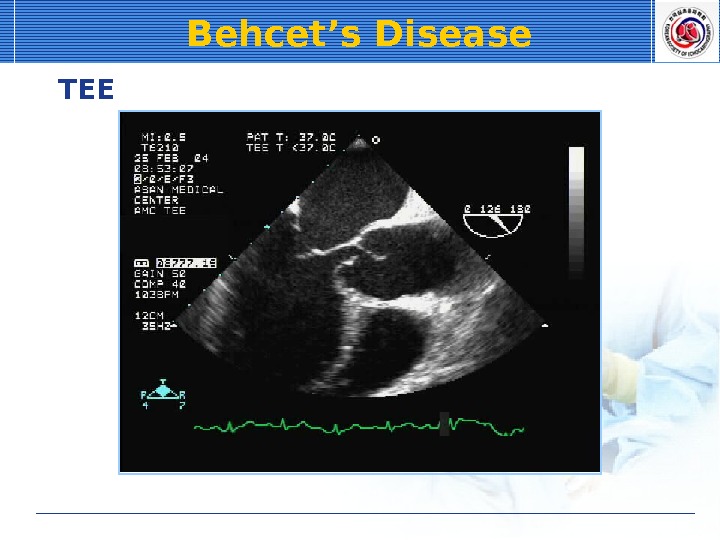 Behcet’s Disease T
Behcet’s Disease T
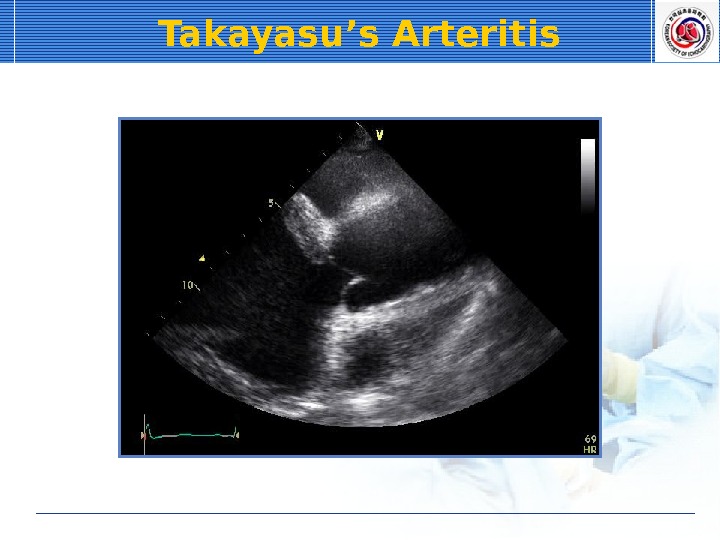
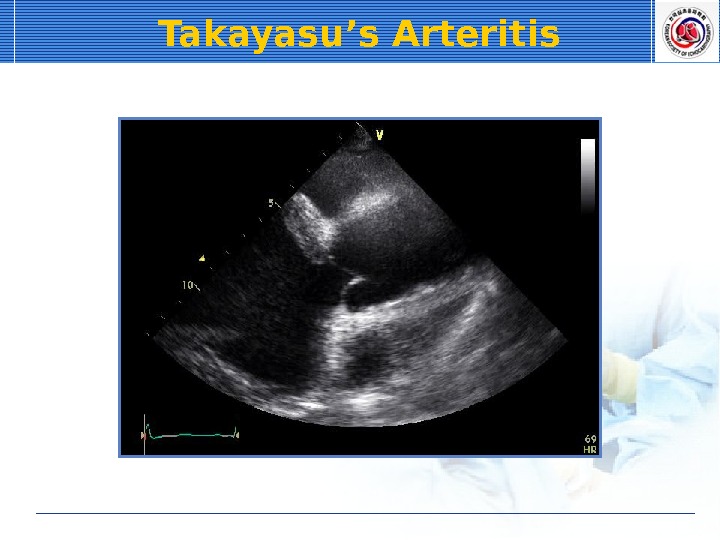 Takayasu’s Arteritis
Takayasu’s Arteritis
 Takayasu’s Arteritis
Takayasu’s Arteritis
 Takayasu’s Arteritis T
Takayasu’s Arteritis T
 Severe Aortic Atherosclerosis
Severe Aortic Atherosclerosis
 Severe Aortic Atherosclerosis
Severe Aortic Atherosclerosis
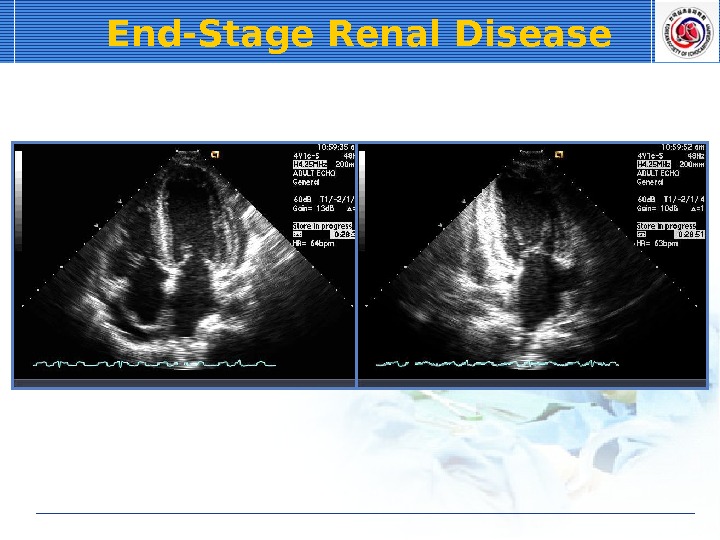
 End-Stage Renal Disease LV hypertrophy Pericardial effusion Early stage: diastolic dysfunction Late stage: systolic dysfunction
End-Stage Renal Disease LV hypertrophy Pericardial effusion Early stage: diastolic dysfunction Late stage: systolic dysfunction
 End-Stage Renal Disease
End-Stage Renal Disease
 End-Stage Renal Disease
End-Stage Renal Disease
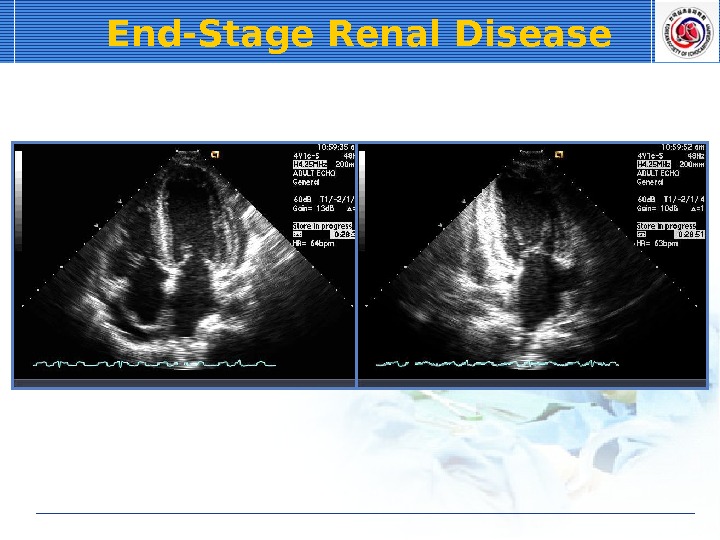 End-Stage Renal Disease
End-Stage Renal Disease
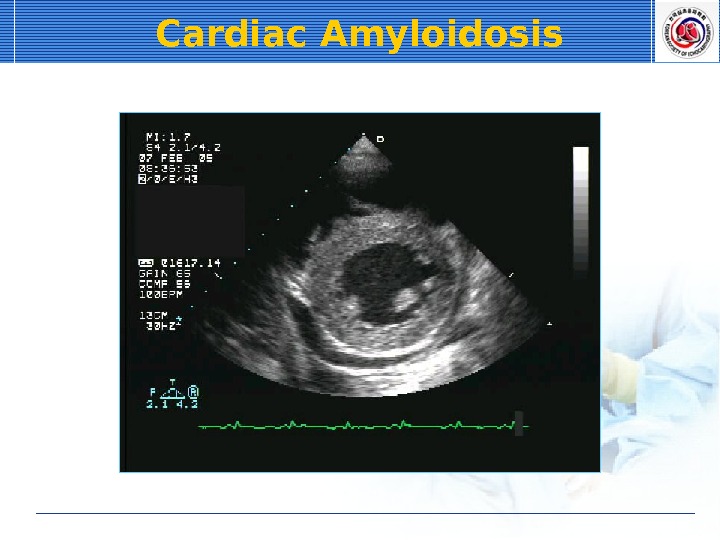
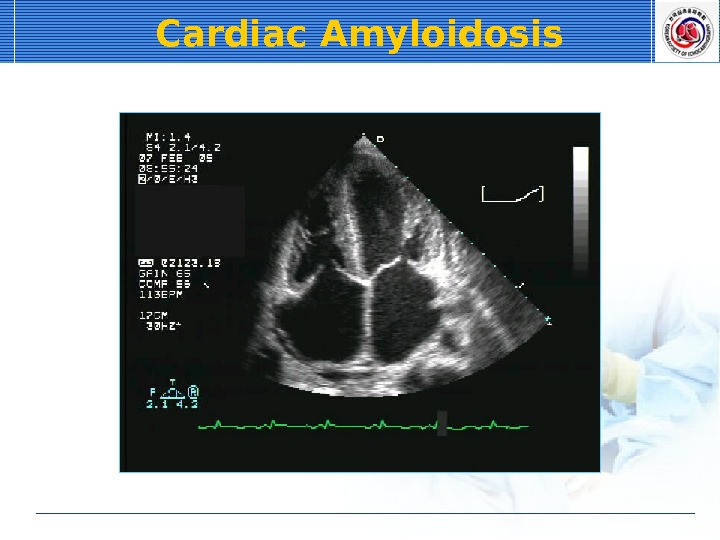
 Cardiac Amyloidosis LV hypertrophy Atrial enlargement Sparkling texture of myocardium Restrictive physiology Pericardial effusion Valvular thickening & regurgitation Low QRS voltage
Cardiac Amyloidosis LV hypertrophy Atrial enlargement Sparkling texture of myocardium Restrictive physiology Pericardial effusion Valvular thickening & regurgitation Low QRS voltage
 Cardiac Amyloidosis
Cardiac Amyloidosis
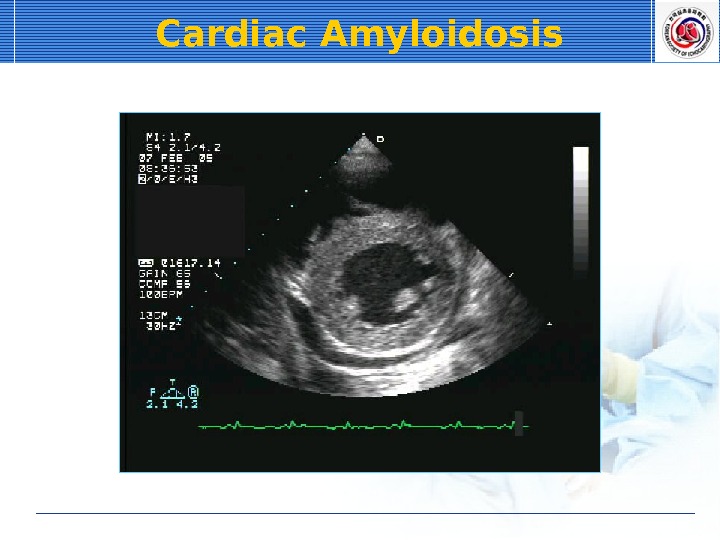 Cardiac Amyloidosis
Cardiac Amyloidosis
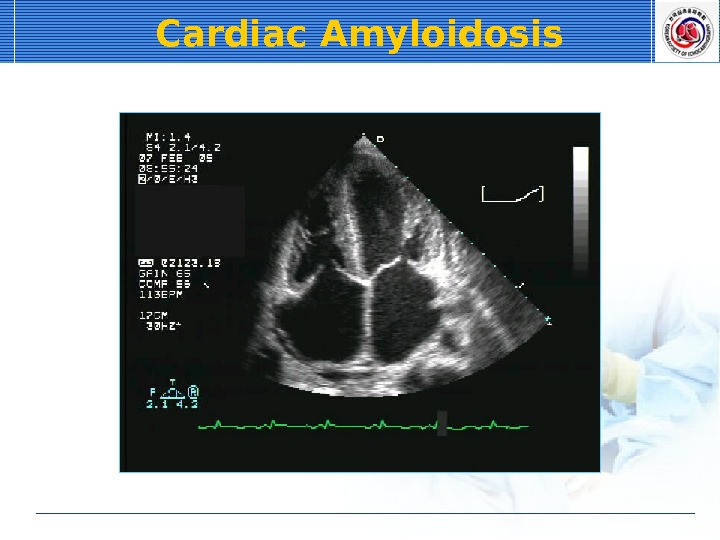 Cardiac Amyloidosis
Cardiac Amyloidosis
 Cardiac Amyloidosis
Cardiac Amyloidosis
 Cardiac Amyloidosis
Cardiac Amyloidosis
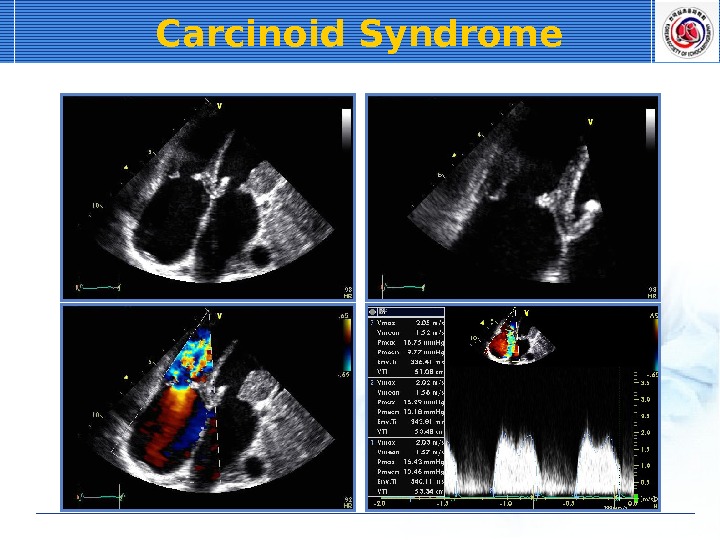
 Carcinoid Syndrome Common in hepatic involvement Caused by secretion of serotonin, bradykinin Fibrosis & thickening of TV & PV stenosis or regurgitation Lt side valve: 10%
Carcinoid Syndrome Common in hepatic involvement Caused by secretion of serotonin, bradykinin Fibrosis & thickening of TV & PV stenosis or regurgitation Lt side valve: 10%
 Carcinoid Syndrome
Carcinoid Syndrome
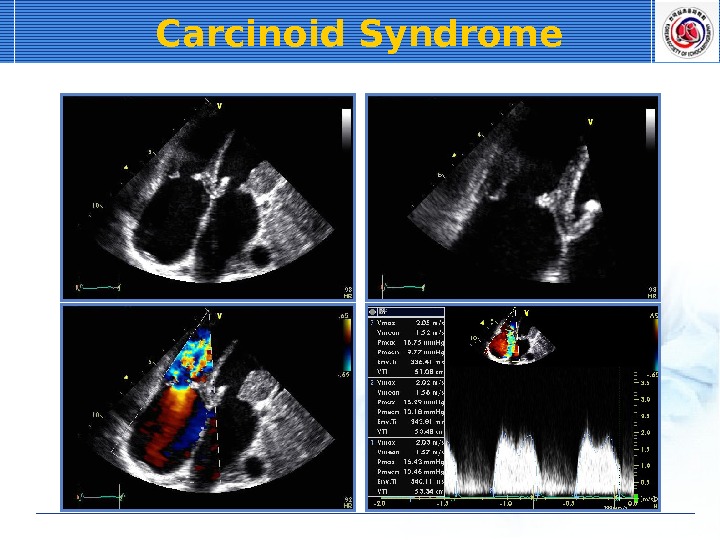 Carcinoid Syndrome
Carcinoid Syndrome
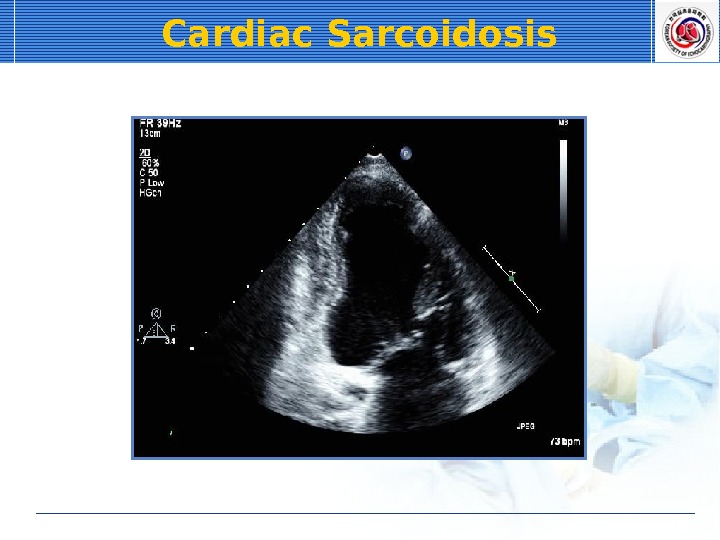
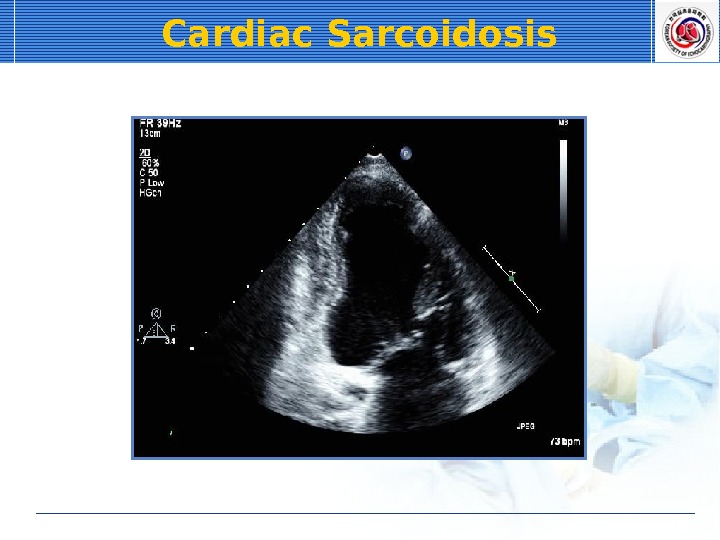
 Cardiac Sarcoidosis Cardiac involvement: 20% Cardiac fibrosis & RWMA • Basal & lateral LV • Wall thinning & aneurysm formation • restrictive morphology
Cardiac Sarcoidosis Cardiac involvement: 20% Cardiac fibrosis & RWMA • Basal & lateral LV • Wall thinning & aneurysm formation • restrictive morphology
 Cardiac Sarcoidosis
Cardiac Sarcoidosis
 Cardiac Sarcoidosis
Cardiac Sarcoidosis
 Cardiac Sarcoidosis
Cardiac Sarcoidosis

