9-3 aorta disease.ppt
- Количество слайдов: 55
 Aortic & Systemic Disease
Aortic & Systemic Disease
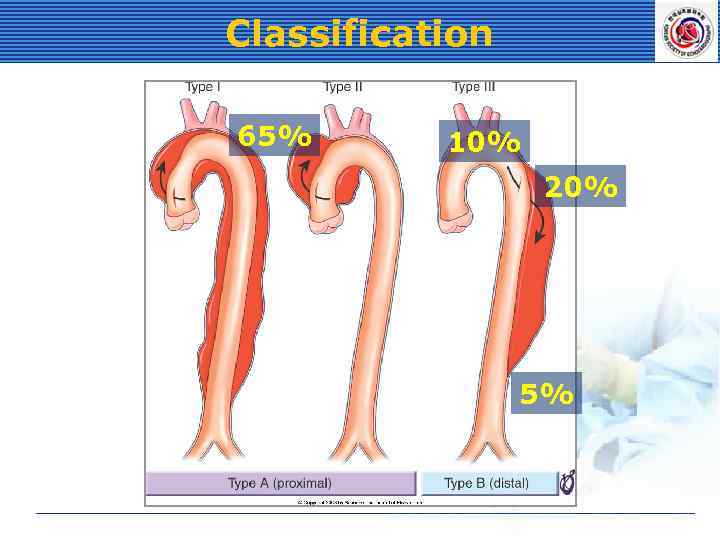 Classification 65% 10% 20% 5%
Classification 65% 10% 20% 5%
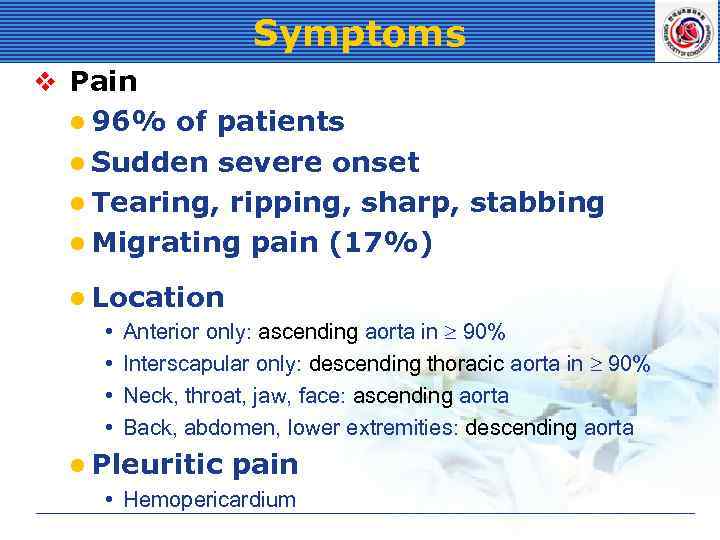 Symptoms v Pain l 96% of patients l Sudden severe onset l Tearing, ripping, sharp, stabbing l Migrating pain (17%) l Location • Anterior only: ascending aorta in 90% • Interscapular only: descending thoracic aorta in 90% • Neck, throat, jaw, face: ascending aorta • Back, abdomen, lower extremities: descending aorta l Pleuritic pain • Hemopericardium
Symptoms v Pain l 96% of patients l Sudden severe onset l Tearing, ripping, sharp, stabbing l Migrating pain (17%) l Location • Anterior only: ascending aorta in 90% • Interscapular only: descending thoracic aorta in 90% • Neck, throat, jaw, face: ascending aorta • Back, abdomen, lower extremities: descending aorta l Pleuritic pain • Hemopericardium
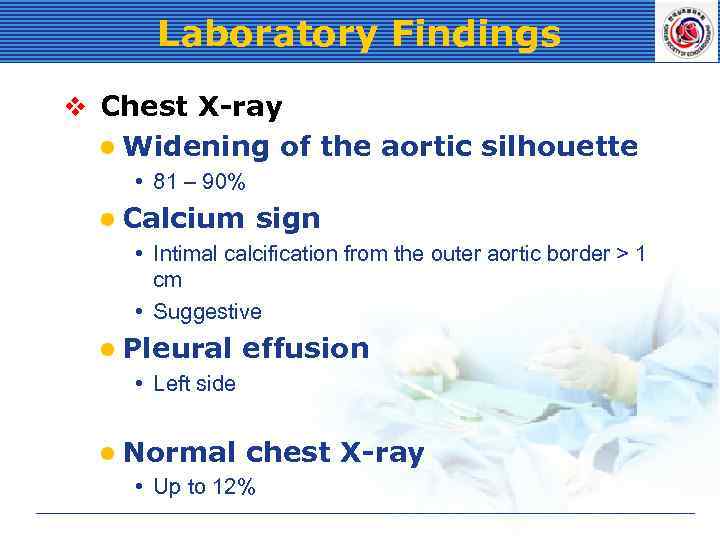 Laboratory Findings v Chest X-ray l Widening of the aortic silhouette • 81 – 90% l Calcium sign • Intimal calcification from the outer aortic border > 1 cm • Suggestive l Pleural effusion • Left side l Normal chest • Up to 12% X-ray
Laboratory Findings v Chest X-ray l Widening of the aortic silhouette • 81 – 90% l Calcium sign • Intimal calcification from the outer aortic border > 1 cm • Suggestive l Pleural effusion • Left side l Normal chest • Up to 12% X-ray
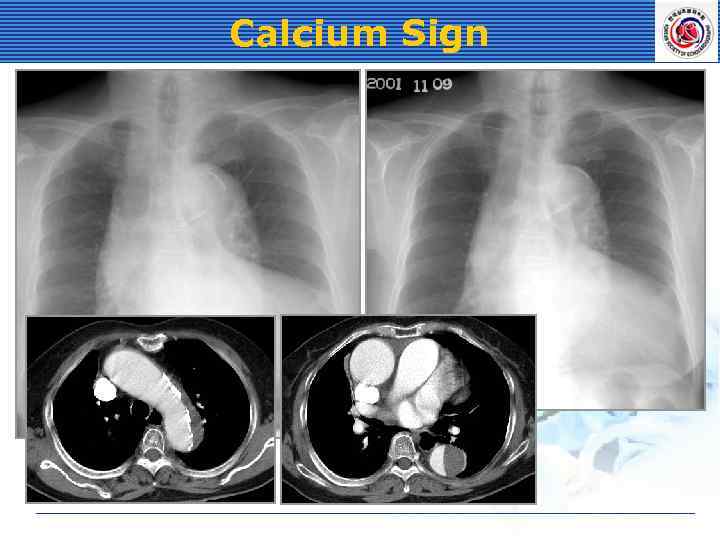 Calcium Sign
Calcium Sign
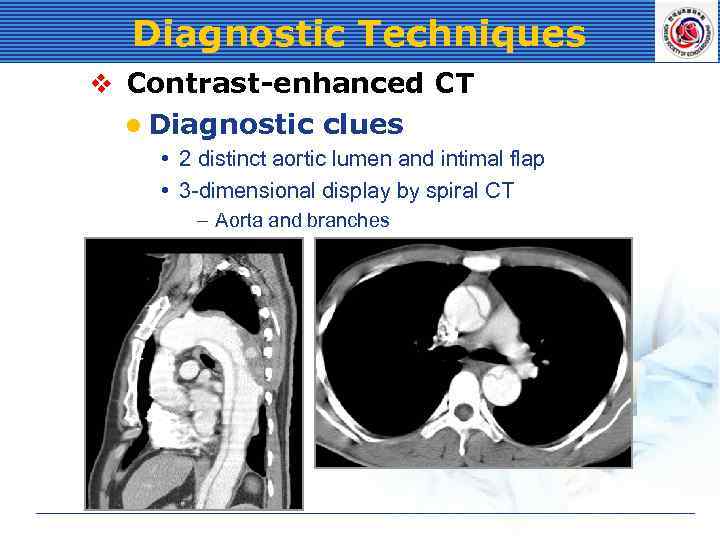 Diagnostic Techniques v Contrast-enhanced CT l Diagnostic clues • 2 distinct aortic lumen and intimal flap • 3 -dimensional display by spiral CT – Aorta and branches
Diagnostic Techniques v Contrast-enhanced CT l Diagnostic clues • 2 distinct aortic lumen and intimal flap • 3 -dimensional display by spiral CT – Aorta and branches
 Diagnostic Techniques v Contrast-enhanced CT l Advantages • • • Noninvasive High sensitivity and specificity (96 -100%) Readily available Thrombus in the false lumen Pericardial effusion Branch vessel compromise l Disadvantages • Contrast materials
Diagnostic Techniques v Contrast-enhanced CT l Advantages • • • Noninvasive High sensitivity and specificity (96 -100%) Readily available Thrombus in the false lumen Pericardial effusion Branch vessel compromise l Disadvantages • Contrast materials
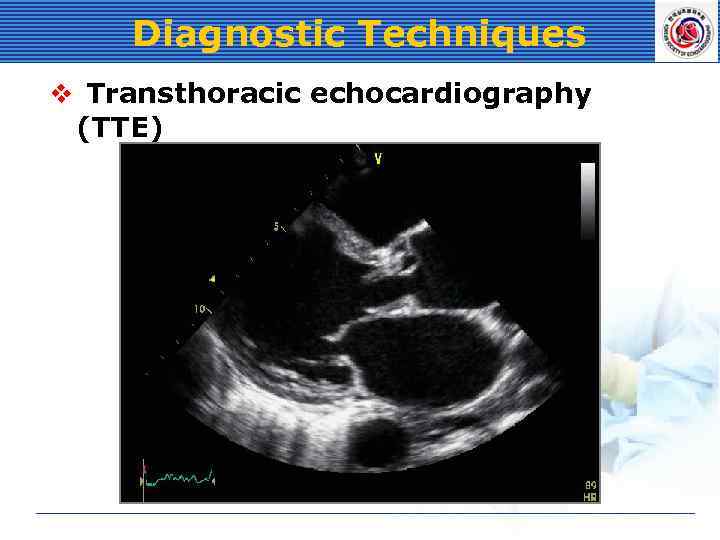 Diagnostic Techniques v Transthoracic echocardiography (TTE)
Diagnostic Techniques v Transthoracic echocardiography (TTE)
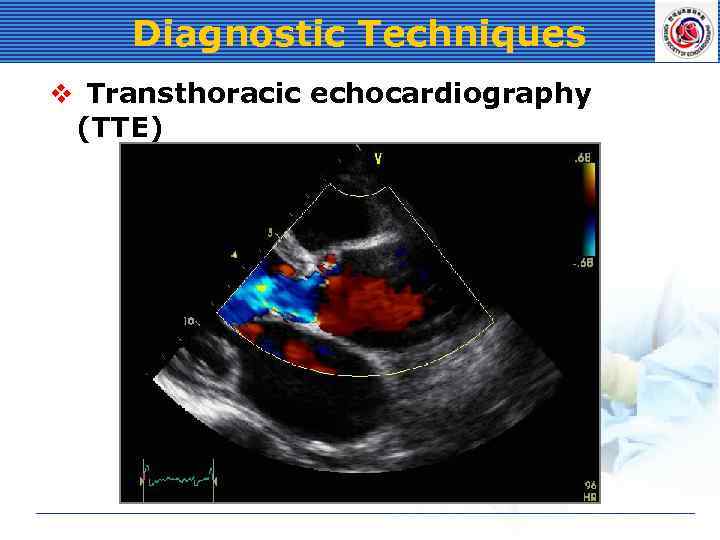 Diagnostic Techniques v Transthoracic echocardiography (TTE)
Diagnostic Techniques v Transthoracic echocardiography (TTE)
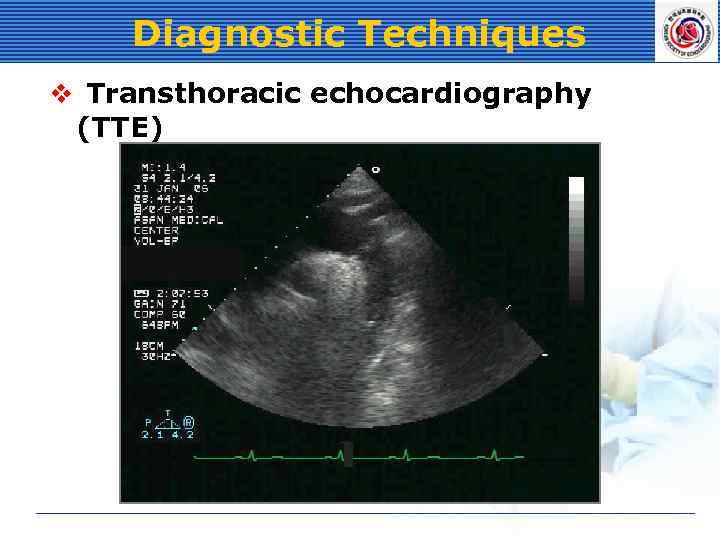 Diagnostic Techniques v Transthoracic echocardiography (TTE)
Diagnostic Techniques v Transthoracic echocardiography (TTE)
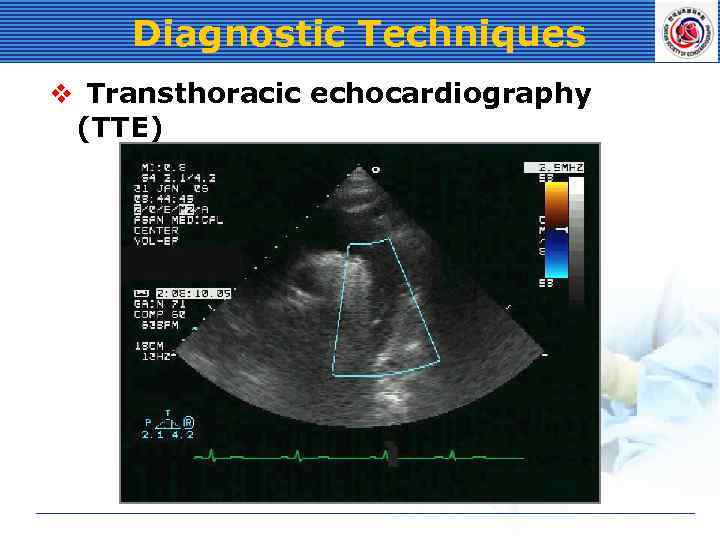 Diagnostic Techniques v Transthoracic echocardiography (TTE)
Diagnostic Techniques v Transthoracic echocardiography (TTE)
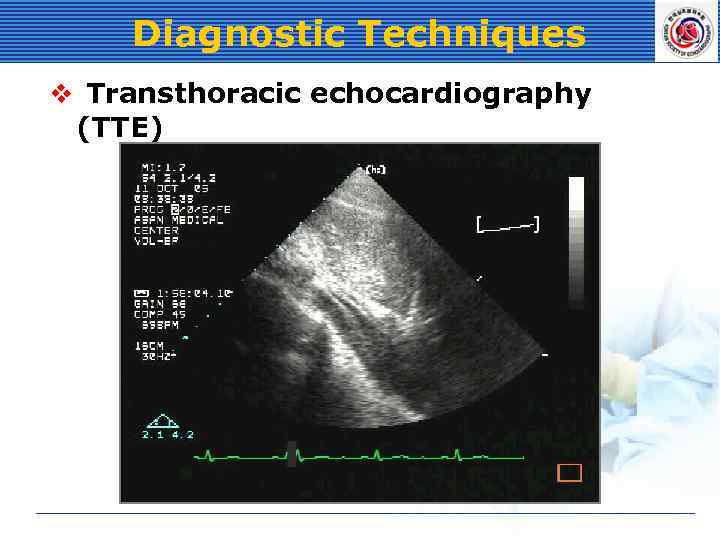 Diagnostic Techniques v Transthoracic echocardiography (TTE)
Diagnostic Techniques v Transthoracic echocardiography (TTE)
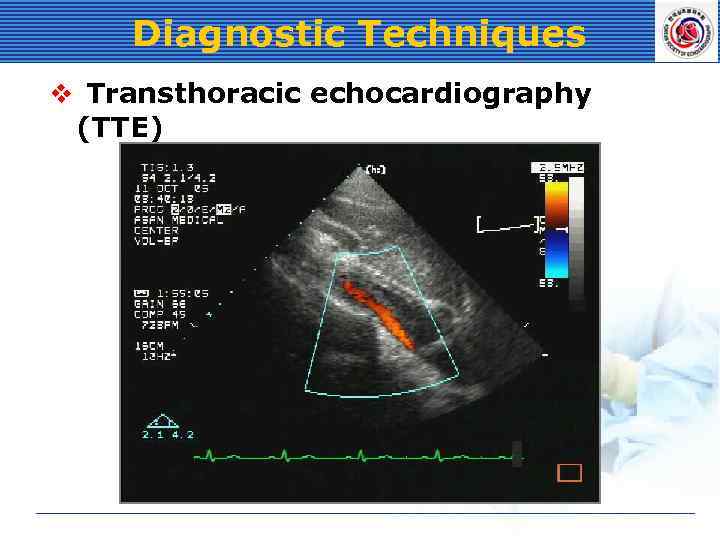 Diagnostic Techniques v Transthoracic echocardiography (TTE)
Diagnostic Techniques v Transthoracic echocardiography (TTE)
 Diagnostic Techniques v Echocardiography l Advantages • Readily available • Noninvasive • Quick to perform at the bedside l Transthoracic (TTE) echocardiography • Sensitivity: 59 – 85% • Specificity: 63 – 96% • Limited by image quality
Diagnostic Techniques v Echocardiography l Advantages • Readily available • Noninvasive • Quick to perform at the bedside l Transthoracic (TTE) echocardiography • Sensitivity: 59 – 85% • Specificity: 63 – 96% • Limited by image quality
 Diagnostic Techniques v Transesophageal echocardiography (TEE) l Advantages • • • High imaging quality with high frequency ultrasound Not require contrast materials Aortic regurgitation Pericardial effusion High sensitivity and specificity – Sensitivity: 98 – 99% – Specificity: 94 – 97% l Disadvantages • Not visualize distal ascending aorta and proximal arch
Diagnostic Techniques v Transesophageal echocardiography (TEE) l Advantages • • • High imaging quality with high frequency ultrasound Not require contrast materials Aortic regurgitation Pericardial effusion High sensitivity and specificity – Sensitivity: 98 – 99% – Specificity: 94 – 97% l Disadvantages • Not visualize distal ascending aorta and proximal arch
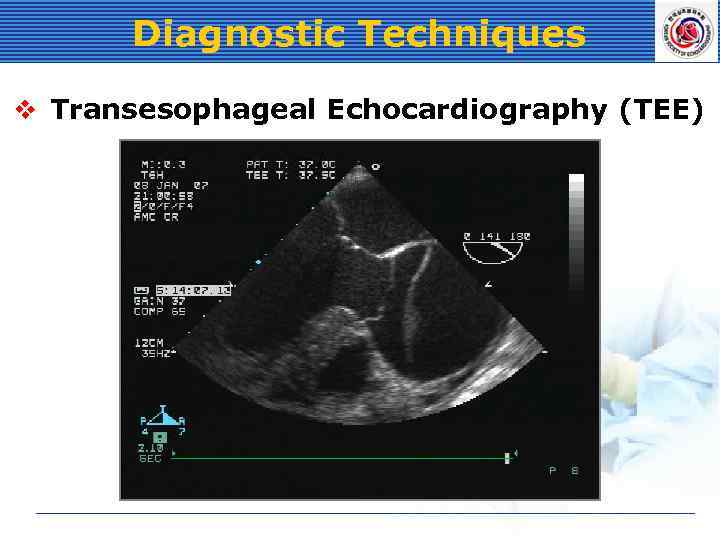 Diagnostic Techniques v Transesophageal Echocardiography (TEE)
Diagnostic Techniques v Transesophageal Echocardiography (TEE)
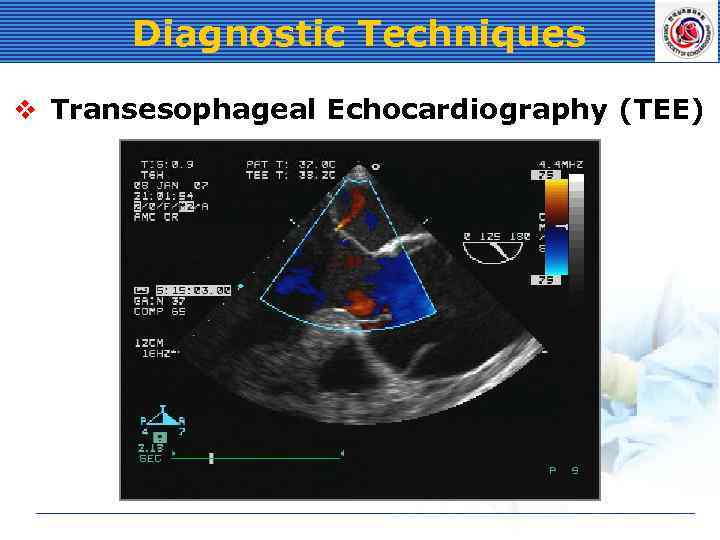 Diagnostic Techniques v Transesophageal Echocardiography (TEE)
Diagnostic Techniques v Transesophageal Echocardiography (TEE)
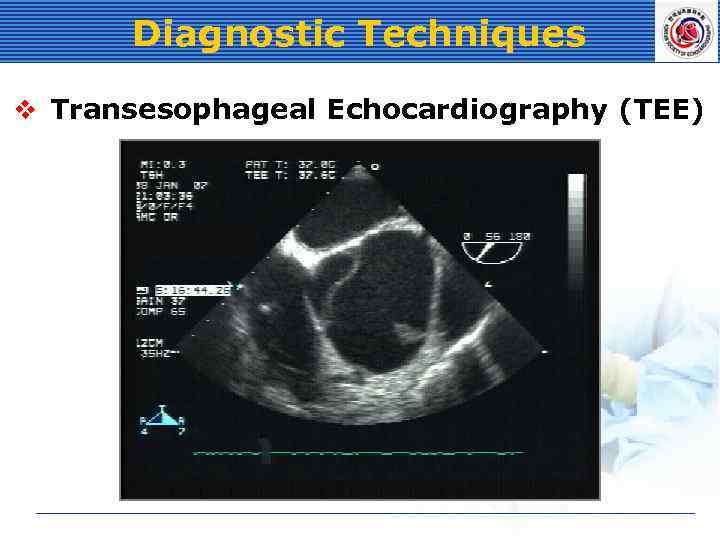 Diagnostic Techniques v Transesophageal Echocardiography (TEE)
Diagnostic Techniques v Transesophageal Echocardiography (TEE)
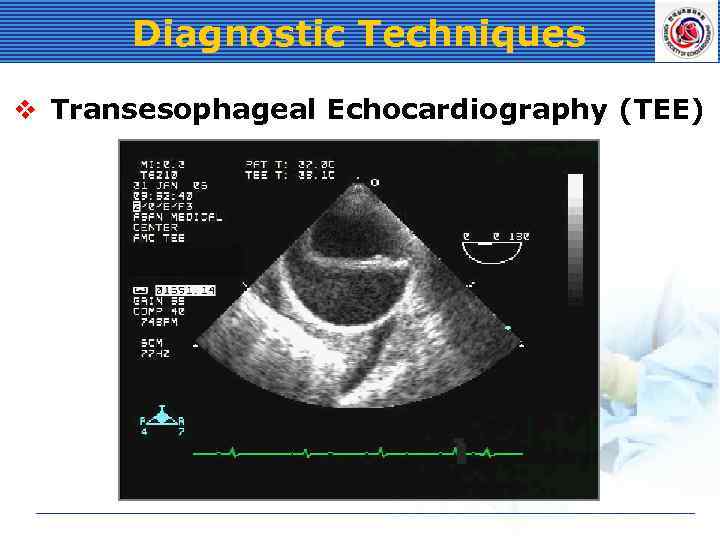 Diagnostic Techniques v Transesophageal Echocardiography (TEE)
Diagnostic Techniques v Transesophageal Echocardiography (TEE)
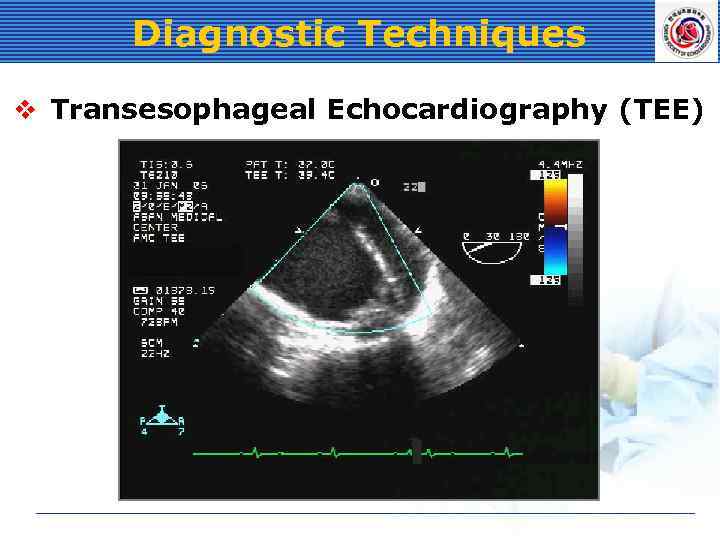 Diagnostic Techniques v Transesophageal Echocardiography (TEE)
Diagnostic Techniques v Transesophageal Echocardiography (TEE)
 Immediate Medical Management v Blood pressure reduction l Goal • Systolic BP: 100 – 120 mm. Hg • Heart rate: 60 – 80 / m • Reducing d. P/dt (beta blocker) l Pain control • Morphine
Immediate Medical Management v Blood pressure reduction l Goal • Systolic BP: 100 – 120 mm. Hg • Heart rate: 60 – 80 / m • Reducing d. P/dt (beta blocker) l Pain control • Morphine
 Immediate Medical Management v Blood pressure reduction l Anticipating aorta surgery • Sodium nitroprusside • Esmolol l Labetalol • Alpha and beta blocking l Contraindicated to beta blocker • Severe sinus bradycardia, AV block, bronchospasm, congestive heart failure • Diltiazem, verapamil • ACE inhibitors
Immediate Medical Management v Blood pressure reduction l Anticipating aorta surgery • Sodium nitroprusside • Esmolol l Labetalol • Alpha and beta blocking l Contraindicated to beta blocker • Severe sinus bradycardia, AV block, bronchospasm, congestive heart failure • Diltiazem, verapamil • ACE inhibitors
 Definitive Therapy v Surgery l Acute proximal dissection l Complicated acute distal dissection • • Progression with vital organ compromise Rupture or impending rupture (saccular aneurysm) Retrograde extension into the ascending aorta Dissection in Marfan syndrome v Medical l Uncomplicated acute distal dissection l Stable isolated arch dissection l Stable chronic dissection
Definitive Therapy v Surgery l Acute proximal dissection l Complicated acute distal dissection • • Progression with vital organ compromise Rupture or impending rupture (saccular aneurysm) Retrograde extension into the ascending aorta Dissection in Marfan syndrome v Medical l Uncomplicated acute distal dissection l Stable isolated arch dissection l Stable chronic dissection
 Aortic Intramural Hematoma v Pathology l Hemorrhage contained within the medial layer l Without an evident intimal tear v Pathogenesis l Rupture of the vasa vasorum l Small or micro tears in the intima
Aortic Intramural Hematoma v Pathology l Hemorrhage contained within the medial layer l Without an evident intimal tear v Pathogenesis l Rupture of the vasa vasorum l Small or micro tears in the intima
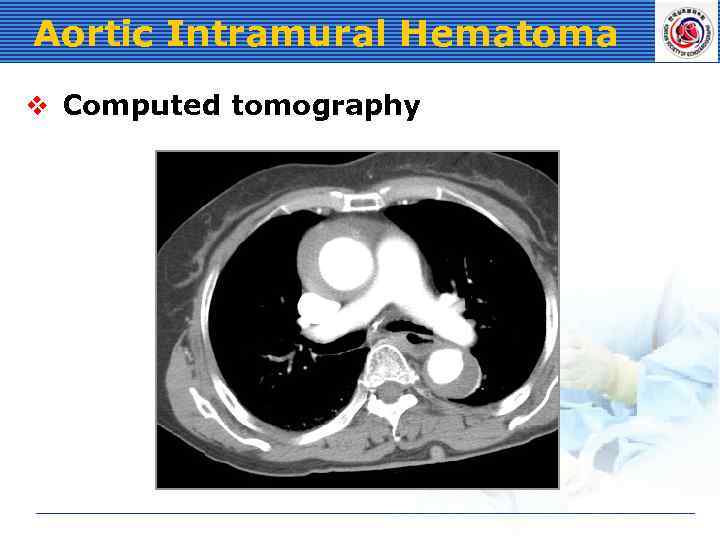 Aortic Intramural Hematoma v Computed tomography
Aortic Intramural Hematoma v Computed tomography
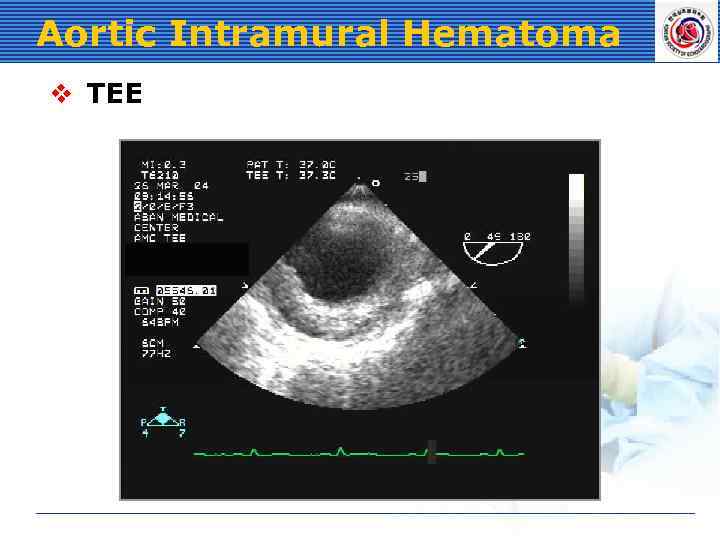 Aortic Intramural Hematoma v TEE
Aortic Intramural Hematoma v TEE
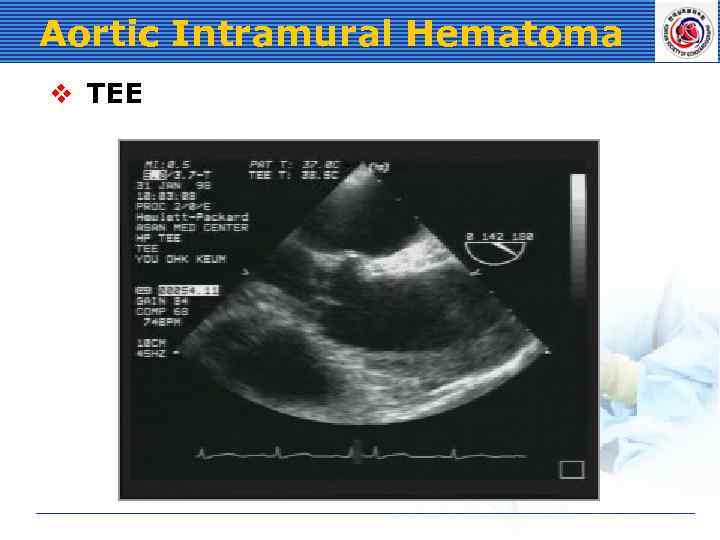 Aortic Intramural Hematoma v TEE
Aortic Intramural Hematoma v TEE
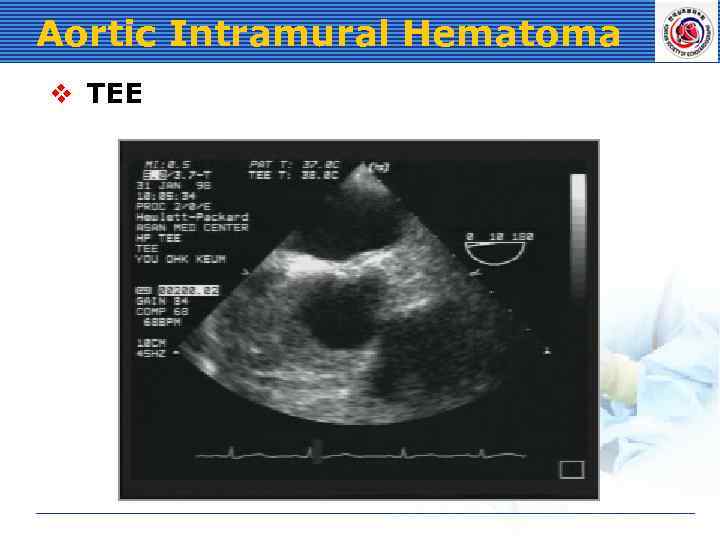 Aortic Intramural Hematoma v TEE
Aortic Intramural Hematoma v TEE
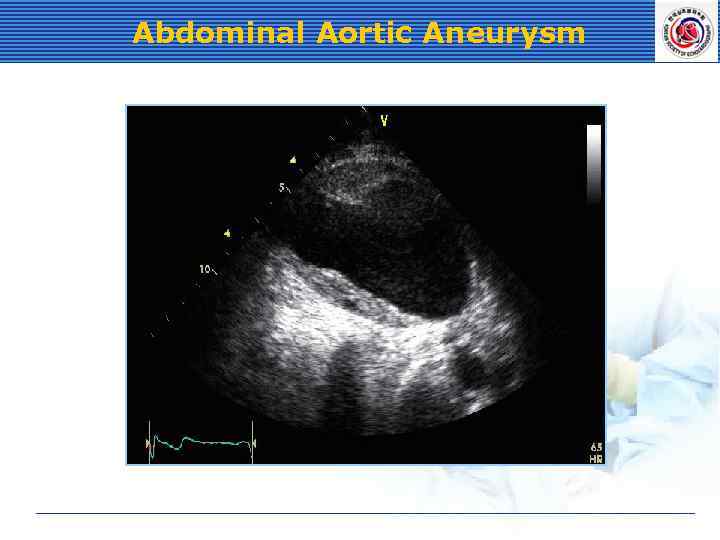 Abdominal Aortic Aneurysm
Abdominal Aortic Aneurysm
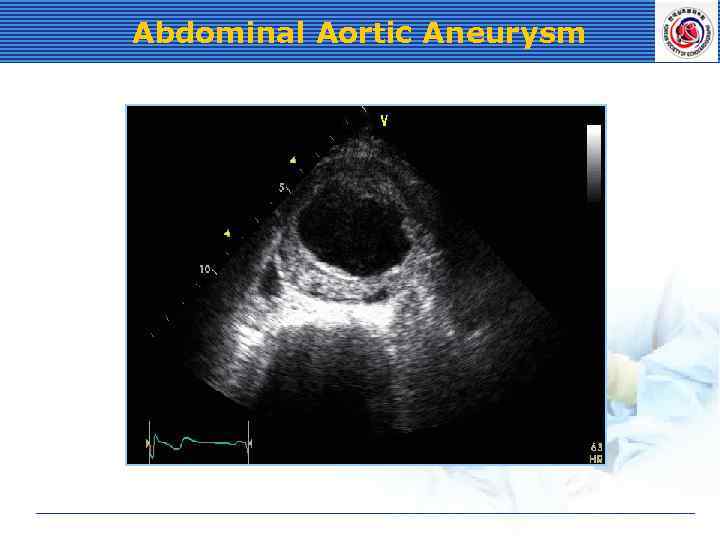 Abdominal Aortic Aneurysm
Abdominal Aortic Aneurysm
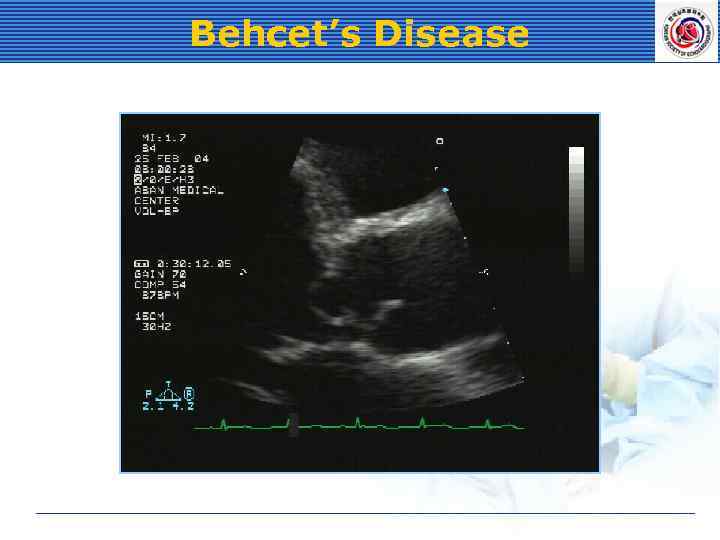 Behcet’s Disease
Behcet’s Disease
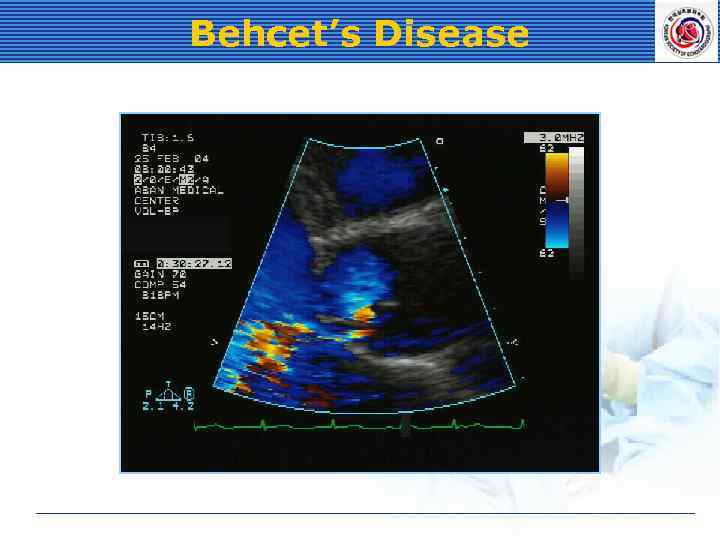 Behcet’s Disease
Behcet’s Disease
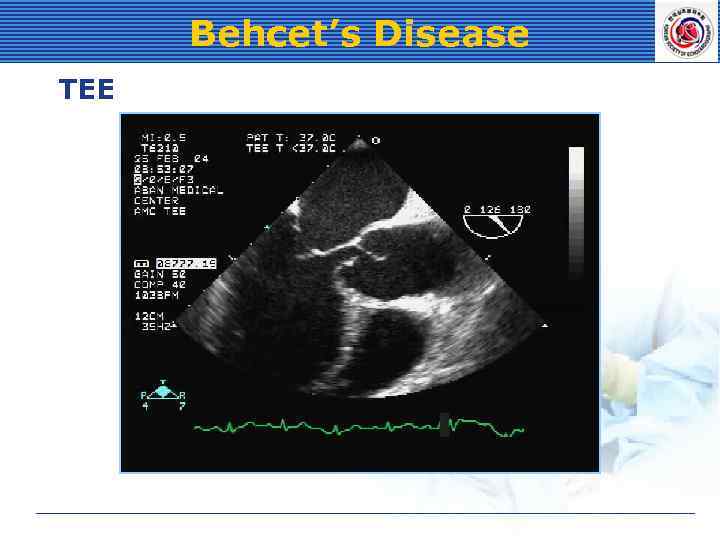 Behcet’s Disease TEE
Behcet’s Disease TEE
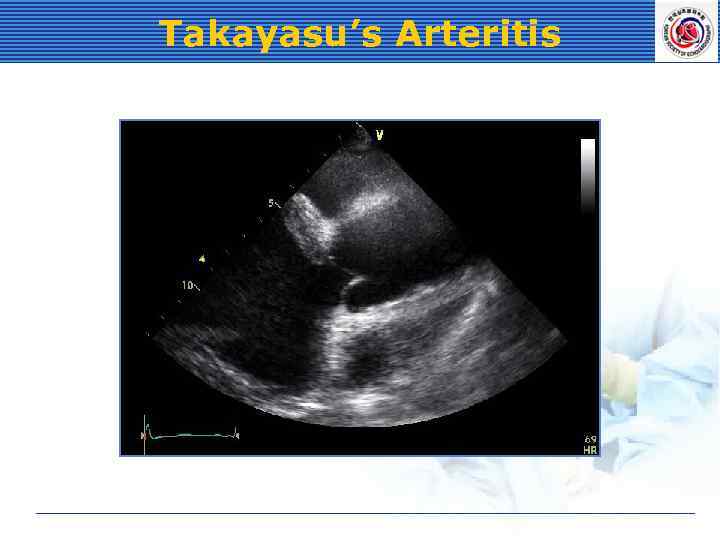 Takayasu’s Arteritis
Takayasu’s Arteritis
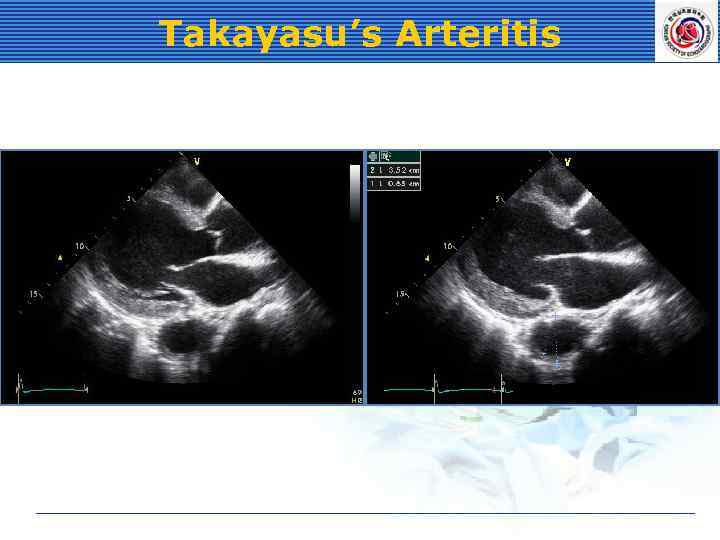 Takayasu’s Arteritis
Takayasu’s Arteritis
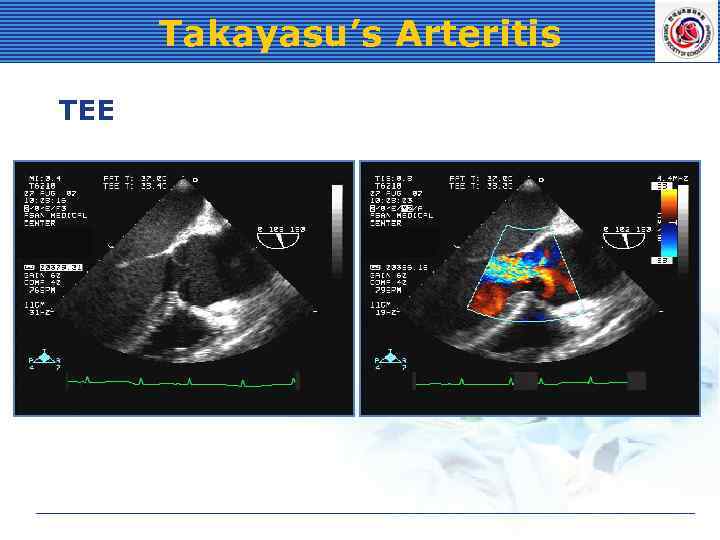 Takayasu’s Arteritis TEE
Takayasu’s Arteritis TEE
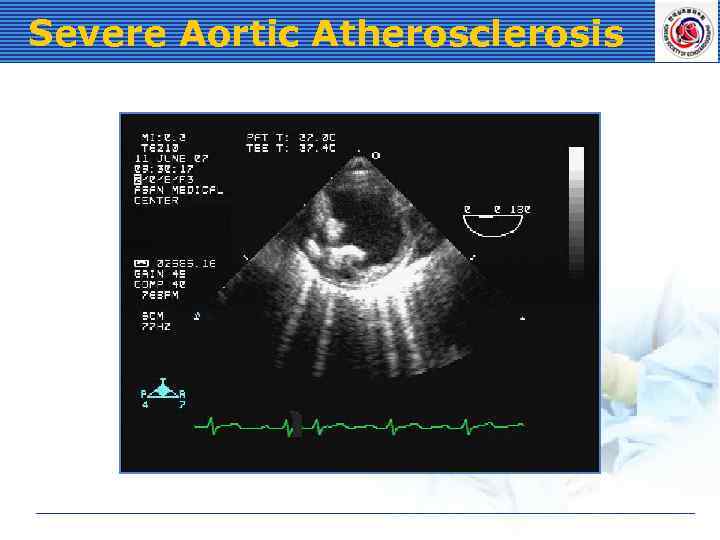 Severe Aortic Atherosclerosis
Severe Aortic Atherosclerosis
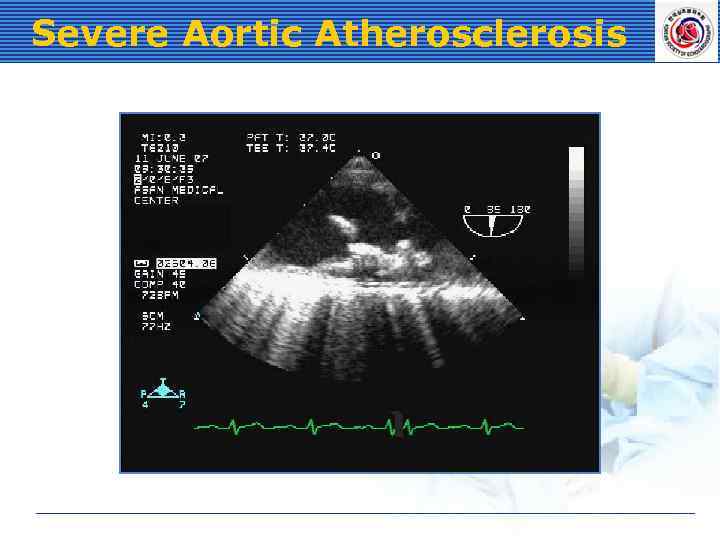 Severe Aortic Atherosclerosis
Severe Aortic Atherosclerosis
 End-Stage Renal Disease l LV hypertrophy l Pericardial l Early effusion stage: diastolic dysfunction Late stage: systolic dysfunction
End-Stage Renal Disease l LV hypertrophy l Pericardial l Early effusion stage: diastolic dysfunction Late stage: systolic dysfunction
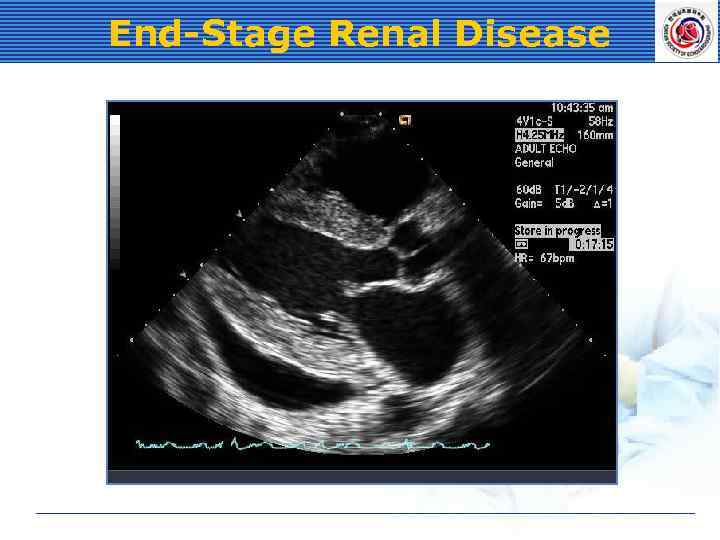 End-Stage Renal Disease
End-Stage Renal Disease
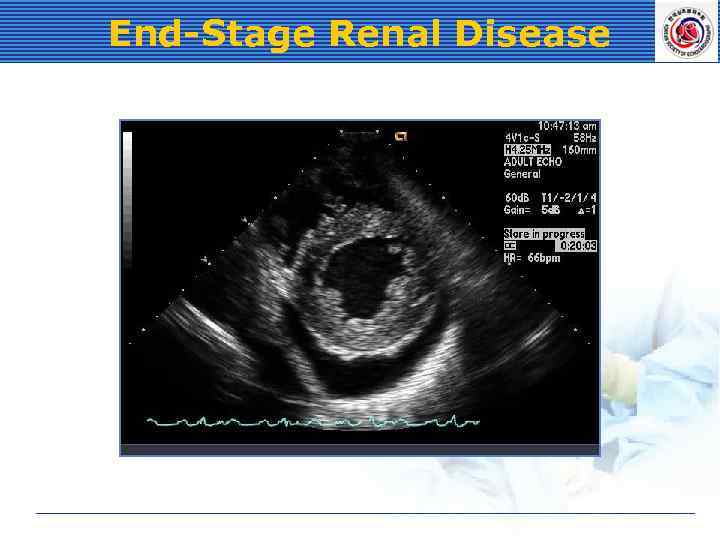 End-Stage Renal Disease
End-Stage Renal Disease
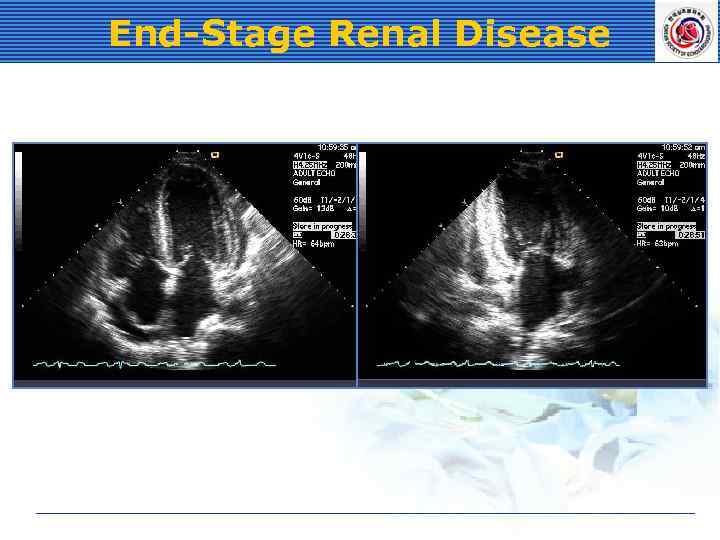 End-Stage Renal Disease
End-Stage Renal Disease
 Cardiac Amyloidosis l LV hypertrophy l Atrial enlargement l Sparkling texture of myocardium l Restrictive physiology l Pericardial effusion l Valvular thickening & regurgitation l Low QRS voltage
Cardiac Amyloidosis l LV hypertrophy l Atrial enlargement l Sparkling texture of myocardium l Restrictive physiology l Pericardial effusion l Valvular thickening & regurgitation l Low QRS voltage
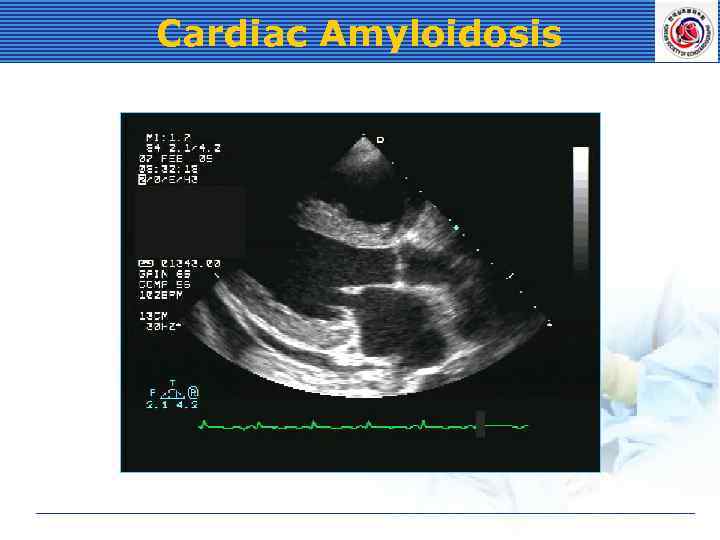 Cardiac Amyloidosis
Cardiac Amyloidosis
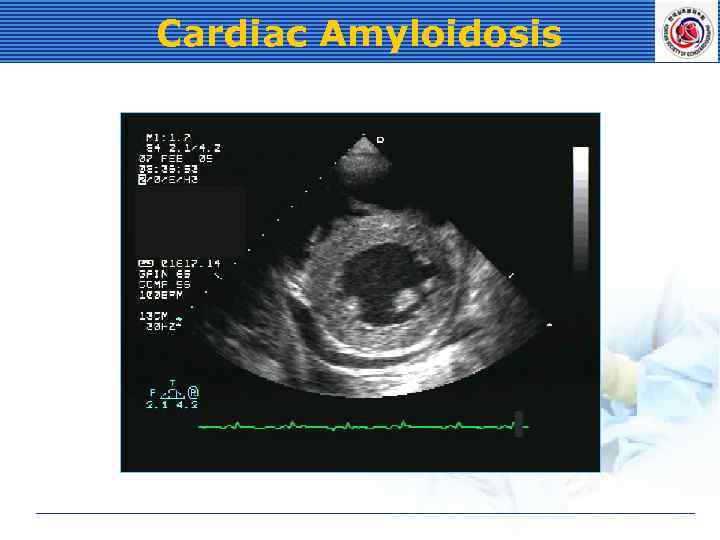 Cardiac Amyloidosis
Cardiac Amyloidosis
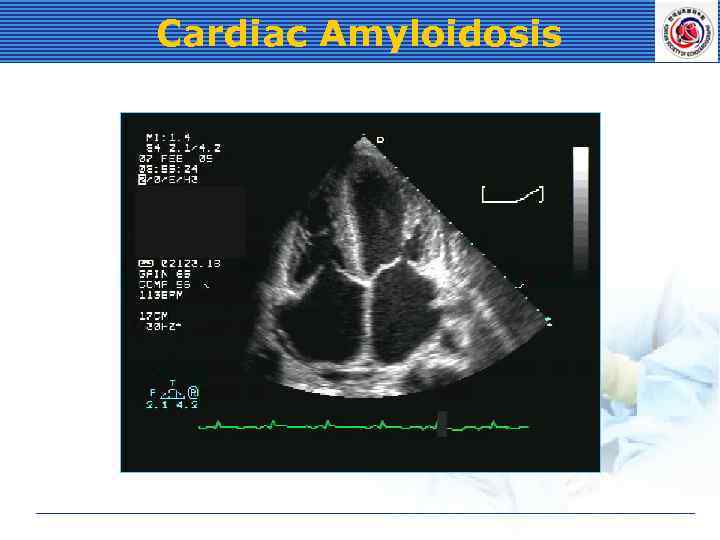 Cardiac Amyloidosis
Cardiac Amyloidosis
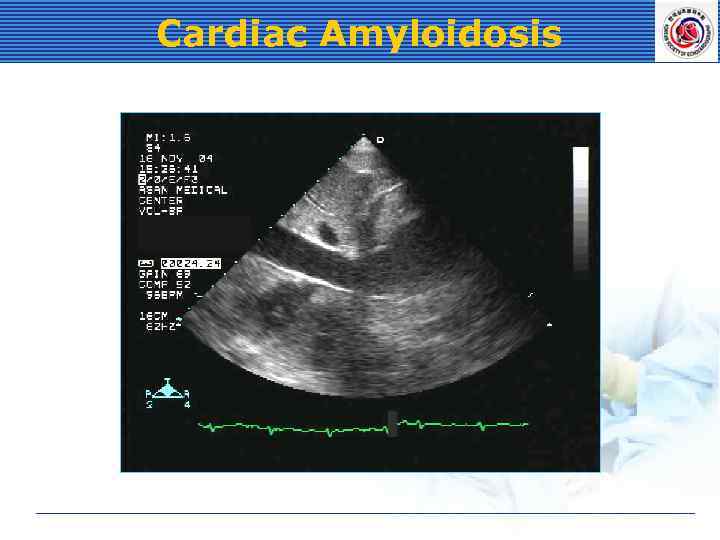 Cardiac Amyloidosis
Cardiac Amyloidosis
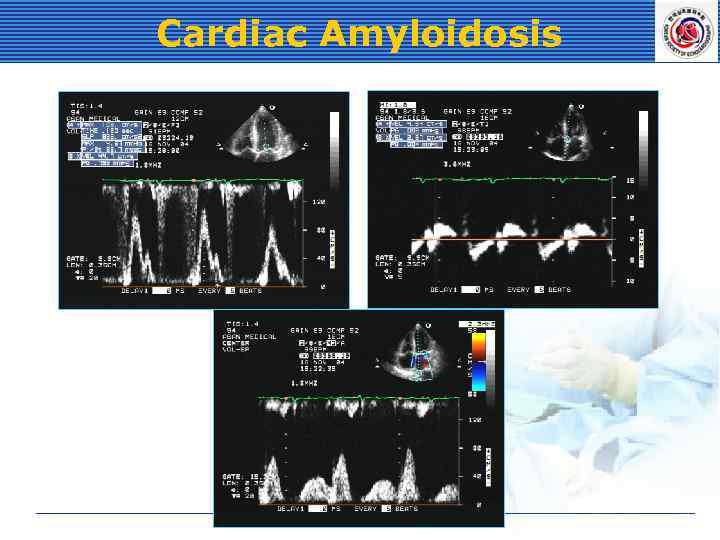 Cardiac Amyloidosis
Cardiac Amyloidosis
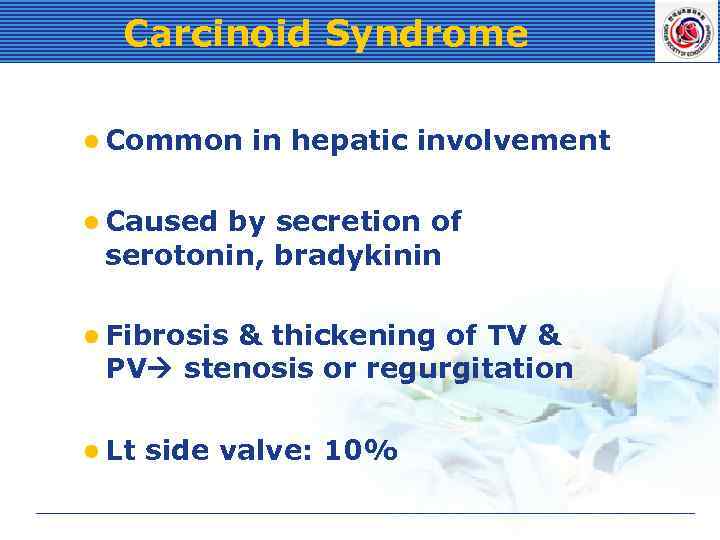 Carcinoid Syndrome l Common in hepatic involvement l Caused by secretion of serotonin, bradykinin l Fibrosis & thickening of TV & PV stenosis or regurgitation l Lt side valve: 10%
Carcinoid Syndrome l Common in hepatic involvement l Caused by secretion of serotonin, bradykinin l Fibrosis & thickening of TV & PV stenosis or regurgitation l Lt side valve: 10%
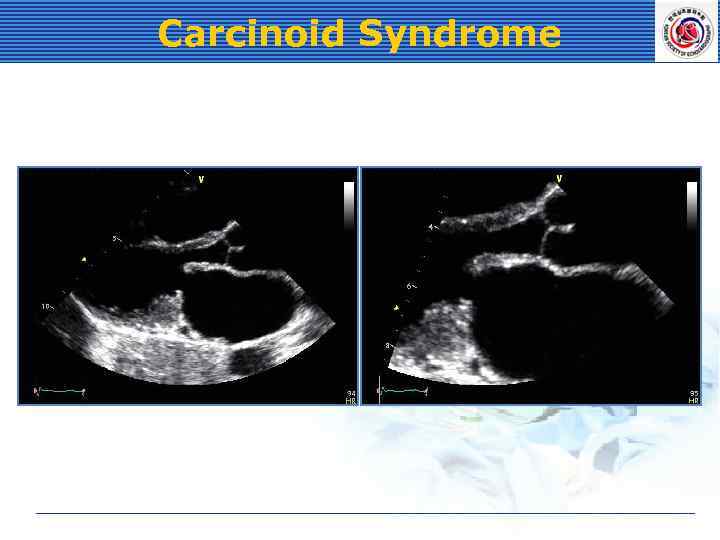 Carcinoid Syndrome
Carcinoid Syndrome
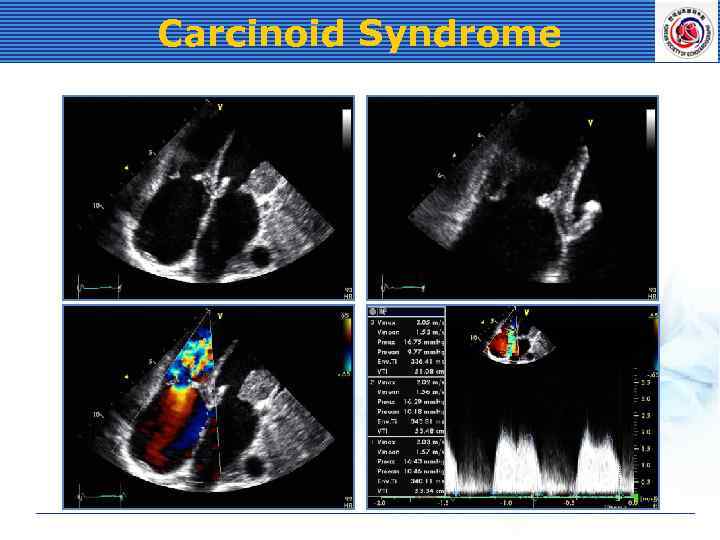 Carcinoid Syndrome
Carcinoid Syndrome
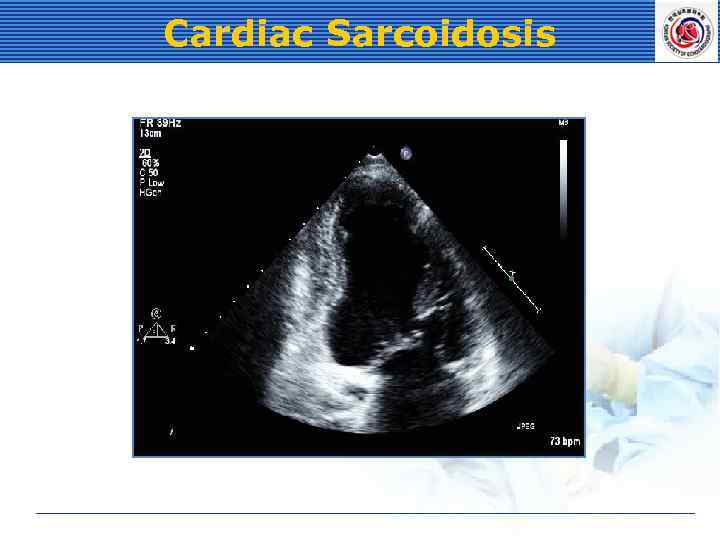
 Cardiac Sarcoidosis l Cardiac involvement: 20% l Cardiac fibrosis & RWMA • Basal & lateral LV • Wall thinning & aneurysm formation • restrictive morphology
Cardiac Sarcoidosis l Cardiac involvement: 20% l Cardiac fibrosis & RWMA • Basal & lateral LV • Wall thinning & aneurysm formation • restrictive morphology
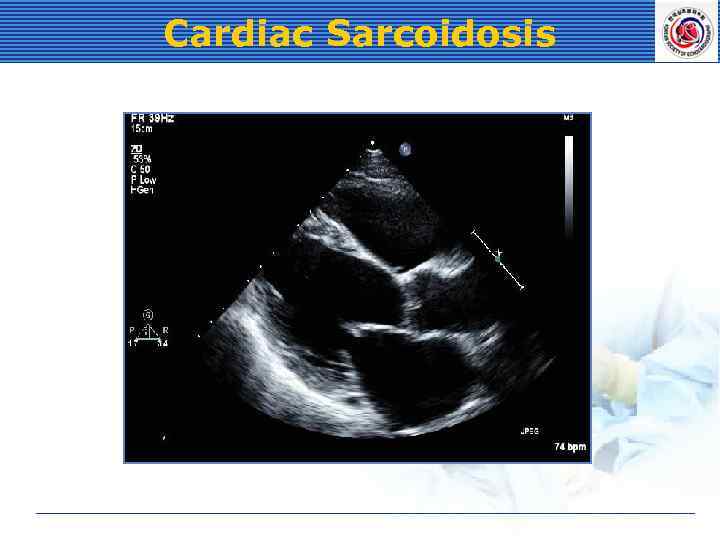 Cardiac Sarcoidosis
Cardiac Sarcoidosis
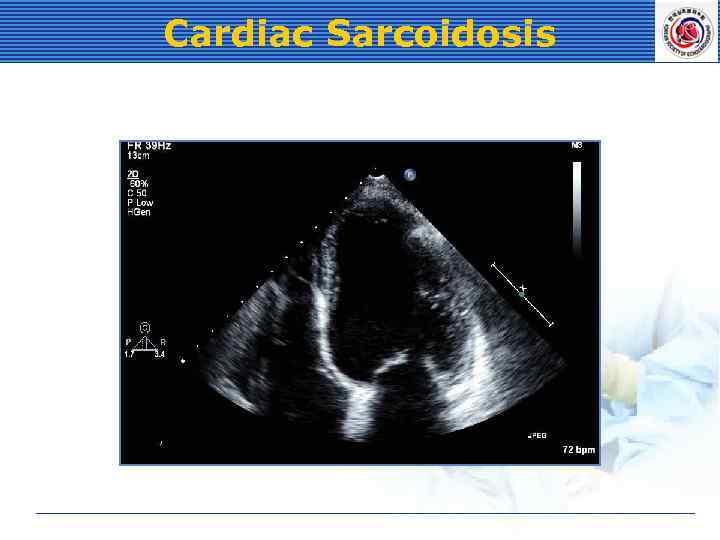 Cardiac Sarcoidosis
Cardiac Sarcoidosis
 Cardiac Sarcoidosis
Cardiac Sarcoidosis


