f5e1238cc0113505a113296e8d5f3625.ppt
- Количество слайдов: 58
 Aortic Stenosis Randall Harada Echo conference: 12 Sep 2007
Aortic Stenosis Randall Harada Echo conference: 12 Sep 2007
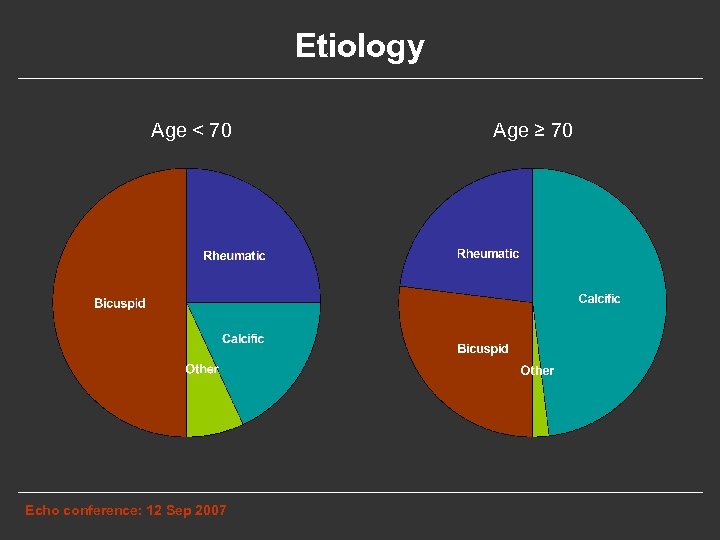 Etiology Age < 70 Echo conference: 12 Sep 2007 Age ≥ 70
Etiology Age < 70 Echo conference: 12 Sep 2007 Age ≥ 70
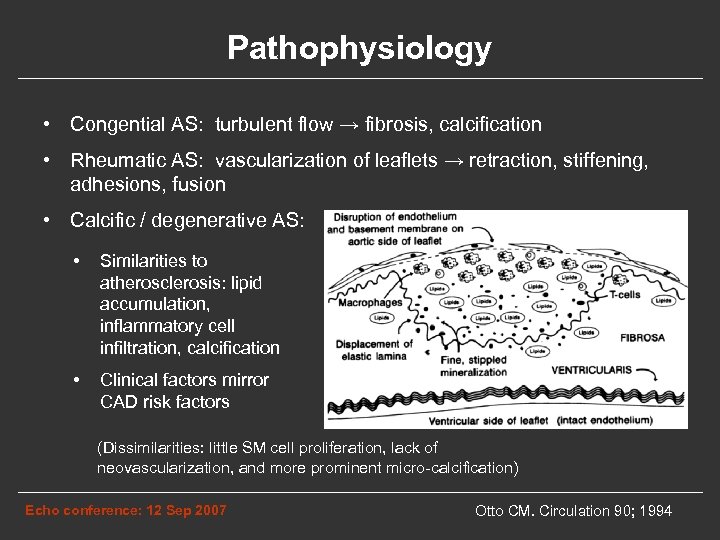 Pathophysiology • Congential AS: turbulent flow → fibrosis, calcification • Rheumatic AS: vascularization of leaflets → retraction, stiffening, adhesions, fusion • Calcific / degenerative AS: • Similarities to atherosclerosis: lipid accumulation, inflammatory cell infiltration, calcification • Clinical factors mirror CAD risk factors (Dissimilarities: little SM cell proliferation, lack of neovascularization, and more prominent micro-calcification) Echo conference: 12 Sep 2007 Otto CM. Circulation 90; 1994
Pathophysiology • Congential AS: turbulent flow → fibrosis, calcification • Rheumatic AS: vascularization of leaflets → retraction, stiffening, adhesions, fusion • Calcific / degenerative AS: • Similarities to atherosclerosis: lipid accumulation, inflammatory cell infiltration, calcification • Clinical factors mirror CAD risk factors (Dissimilarities: little SM cell proliferation, lack of neovascularization, and more prominent micro-calcification) Echo conference: 12 Sep 2007 Otto CM. Circulation 90; 1994
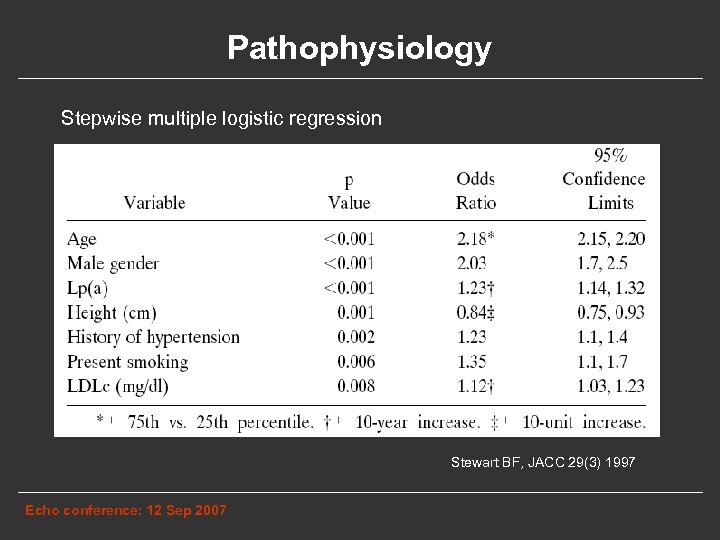 Pathophysiology Stepwise multiple logistic regression Stewart BF, JACC 29(3) 1997 Echo conference: 12 Sep 2007
Pathophysiology Stepwise multiple logistic regression Stewart BF, JACC 29(3) 1997 Echo conference: 12 Sep 2007
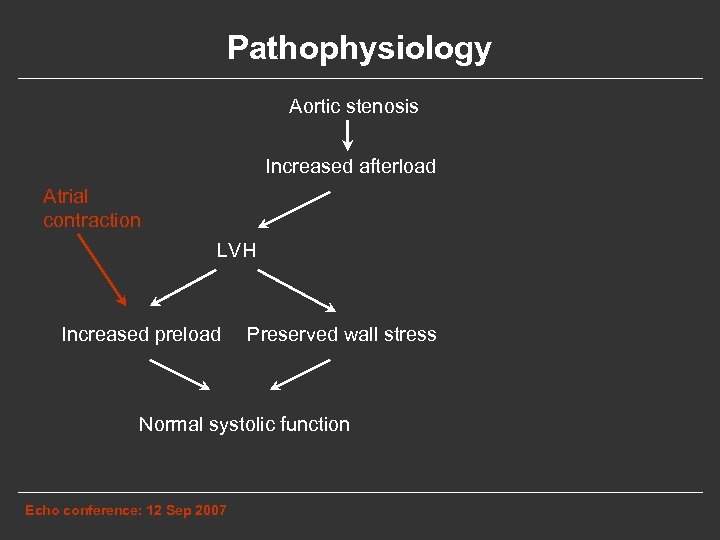 Pathophysiology Aortic stenosis Increased afterload Atrial contraction LVH Increased preload Preserved wall stress Normal systolic function Echo conference: 12 Sep 2007
Pathophysiology Aortic stenosis Increased afterload Atrial contraction LVH Increased preload Preserved wall stress Normal systolic function Echo conference: 12 Sep 2007
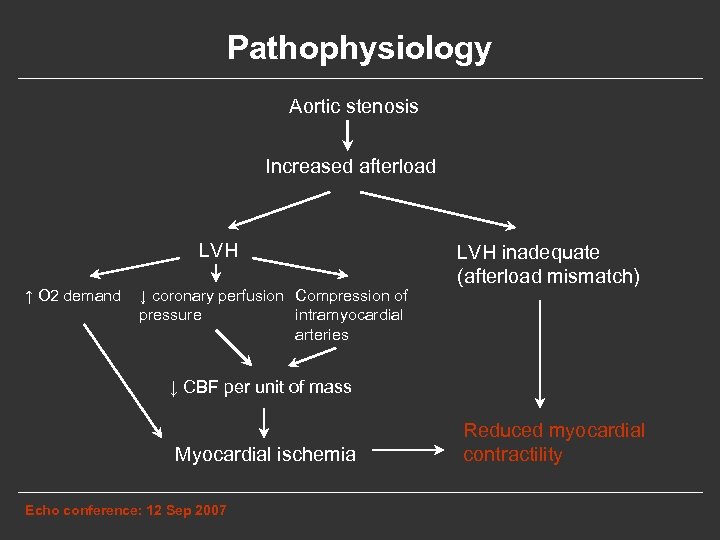 Pathophysiology Aortic stenosis Increased afterload LVH ↑ O 2 demand ↓ coronary perfusion Compression of pressure intramyocardial arteries LVH inadequate (afterload mismatch) ↓ CBF per unit of mass Myocardial ischemia Echo conference: 12 Sep 2007 Reduced myocardial contractility
Pathophysiology Aortic stenosis Increased afterload LVH ↑ O 2 demand ↓ coronary perfusion Compression of pressure intramyocardial arteries LVH inadequate (afterload mismatch) ↓ CBF per unit of mass Myocardial ischemia Echo conference: 12 Sep 2007 Reduced myocardial contractility
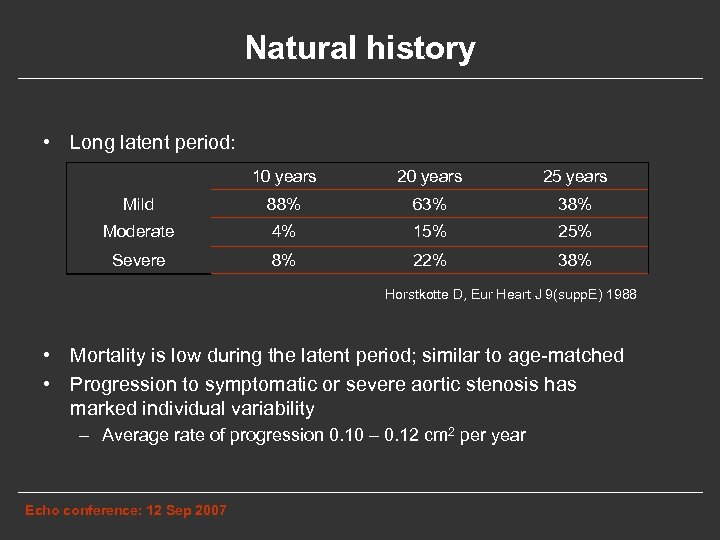 Natural history • Long latent period: 10 years 25 years Mild 88% 63% 38% Moderate 4% 15% 25% Severe 8% 22% 38% Horstkotte D, Eur Heart J 9(supp. E) 1988 • Mortality is low during the latent period; similar to age-matched • Progression to symptomatic or severe aortic stenosis has marked individual variability – Average rate of progression 0. 10 – 0. 12 cm 2 per year Echo conference: 12 Sep 2007
Natural history • Long latent period: 10 years 25 years Mild 88% 63% 38% Moderate 4% 15% 25% Severe 8% 22% 38% Horstkotte D, Eur Heart J 9(supp. E) 1988 • Mortality is low during the latent period; similar to age-matched • Progression to symptomatic or severe aortic stenosis has marked individual variability – Average rate of progression 0. 10 – 0. 12 cm 2 per year Echo conference: 12 Sep 2007
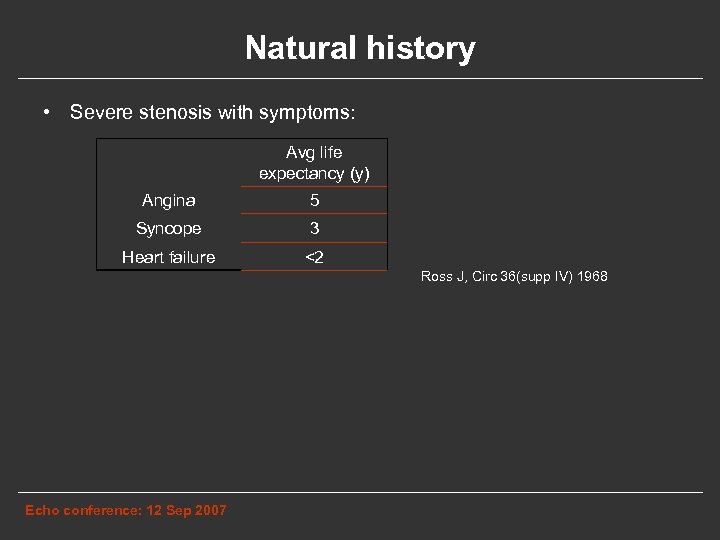 Natural history • Severe stenosis with symptoms: Avg life expectancy (y) Angina 5 Syncope 3 Heart failure <2 Ross J, Circ 36(supp IV) 1968 Echo conference: 12 Sep 2007
Natural history • Severe stenosis with symptoms: Avg life expectancy (y) Angina 5 Syncope 3 Heart failure <2 Ross J, Circ 36(supp IV) 1968 Echo conference: 12 Sep 2007
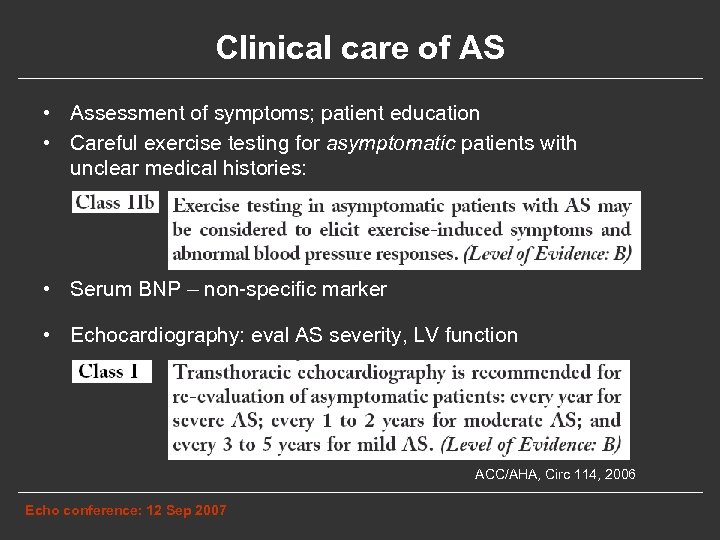 Clinical care of AS • Assessment of symptoms; patient education • Careful exercise testing for asymptomatic patients with unclear medical histories: • Serum BNP – non-specific marker • Echocardiography: eval AS severity, LV function ACC/AHA, Circ 114, 2006 Echo conference: 12 Sep 2007
Clinical care of AS • Assessment of symptoms; patient education • Careful exercise testing for asymptomatic patients with unclear medical histories: • Serum BNP – non-specific marker • Echocardiography: eval AS severity, LV function ACC/AHA, Circ 114, 2006 Echo conference: 12 Sep 2007
 Medical therapy • Antibiotic prophylaxis no longer recommended • No medical therapies proven to prevent or delay AS • In severe AS, atrial fibrillation is often poorly tolerated Echo conference: 12 Sep 2007
Medical therapy • Antibiotic prophylaxis no longer recommended • No medical therapies proven to prevent or delay AS • In severe AS, atrial fibrillation is often poorly tolerated Echo conference: 12 Sep 2007
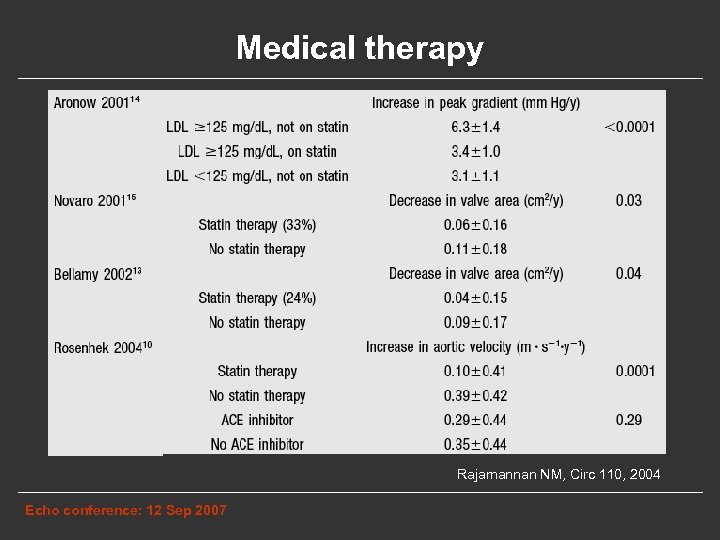 Medical therapy Rajamannan NM, Circ 110, 2004 Echo conference: 12 Sep 2007
Medical therapy Rajamannan NM, Circ 110, 2004 Echo conference: 12 Sep 2007
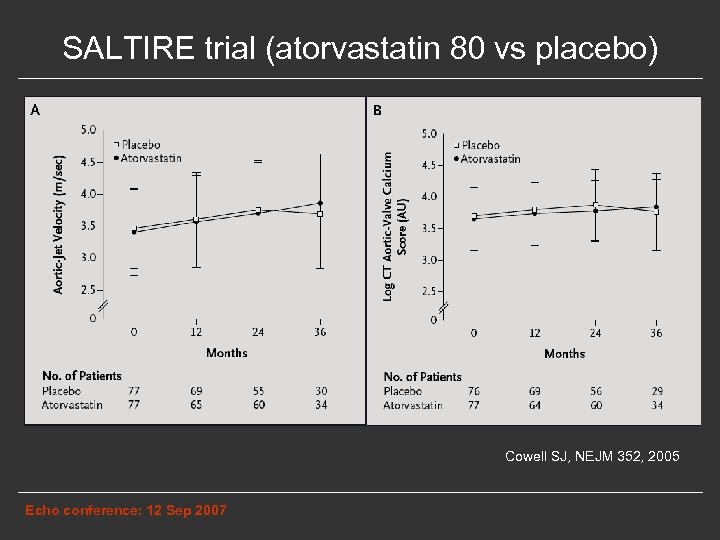 SALTIRE trial (atorvastatin 80 vs placebo) Cowell SJ, NEJM 352, 2005 Echo conference: 12 Sep 2007
SALTIRE trial (atorvastatin 80 vs placebo) Cowell SJ, NEJM 352, 2005 Echo conference: 12 Sep 2007
 RAAVE study • 121 patients • Not randomized – Active arm: patients who need statin due to hyperlipidemia • Mean LDL 160 mg/d. L → at end of study: 93 mg/d. L • Higher prevalence of HTN and diabetes – Control arm: patients who do not meet guidelines for a statin • Mean LDL 119 mg/d. L → at end of study: 118 mg/d. L Moura LM, JACC 49, 2007 Echo conference: 12 Sep 2007
RAAVE study • 121 patients • Not randomized – Active arm: patients who need statin due to hyperlipidemia • Mean LDL 160 mg/d. L → at end of study: 93 mg/d. L • Higher prevalence of HTN and diabetes – Control arm: patients who do not meet guidelines for a statin • Mean LDL 119 mg/d. L → at end of study: 118 mg/d. L Moura LM, JACC 49, 2007 Echo conference: 12 Sep 2007
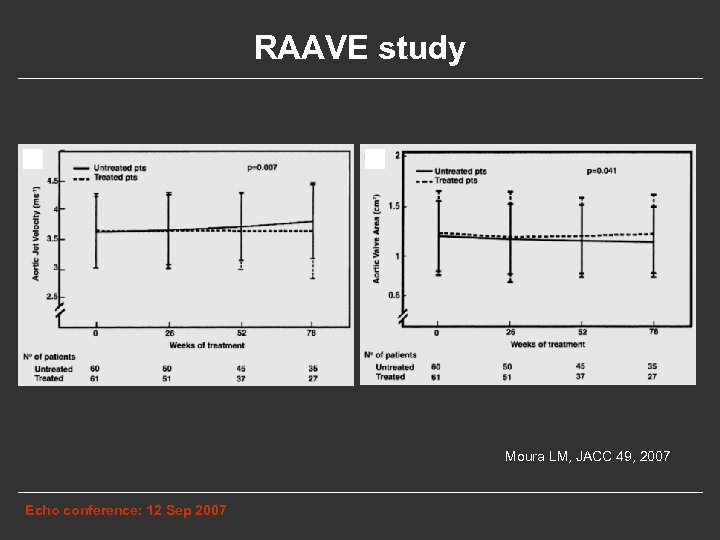 RAAVE study Moura LM, JACC 49, 2007 Echo conference: 12 Sep 2007
RAAVE study Moura LM, JACC 49, 2007 Echo conference: 12 Sep 2007
 Ongoing Statin RCTs • Stop Aortic Stenosis (STOP-AS) - U. S. • Simvastatin and Ezetimibe in Aortic Stenosis (SEAS) Europe • Aortic Stenosis Progression Observation Measuring Effects of Rosuvastatin (? ? ? ) - Canada ASTRONOMER Echo conference: 12 Sep 2007
Ongoing Statin RCTs • Stop Aortic Stenosis (STOP-AS) - U. S. • Simvastatin and Ezetimibe in Aortic Stenosis (SEAS) Europe • Aortic Stenosis Progression Observation Measuring Effects of Rosuvastatin (? ? ? ) - Canada ASTRONOMER Echo conference: 12 Sep 2007
 Evaluation of AS severity • Maximum aortic velocity • Mean transvalvular gradient • Aortic valve area by continuity equation Echo conference: 12 Sep 2007
Evaluation of AS severity • Maximum aortic velocity • Mean transvalvular gradient • Aortic valve area by continuity equation Echo conference: 12 Sep 2007
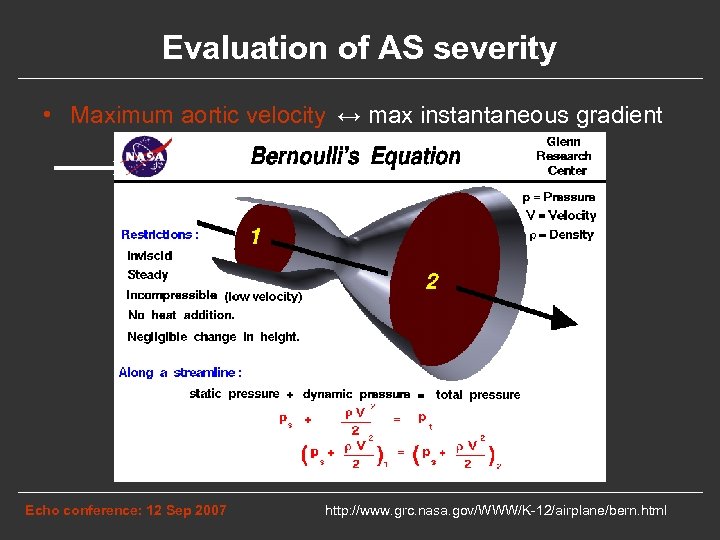 Evaluation of AS severity • Maximum aortic velocity ↔ max instantaneous gradient ← 71 mm. Hg 4. 2 m/s Echo conference: 12 Sep 2007 http: //www. grc. nasa. gov/WWW/K-12/airplane/bern. html
Evaluation of AS severity • Maximum aortic velocity ↔ max instantaneous gradient ← 71 mm. Hg 4. 2 m/s Echo conference: 12 Sep 2007 http: //www. grc. nasa. gov/WWW/K-12/airplane/bern. html
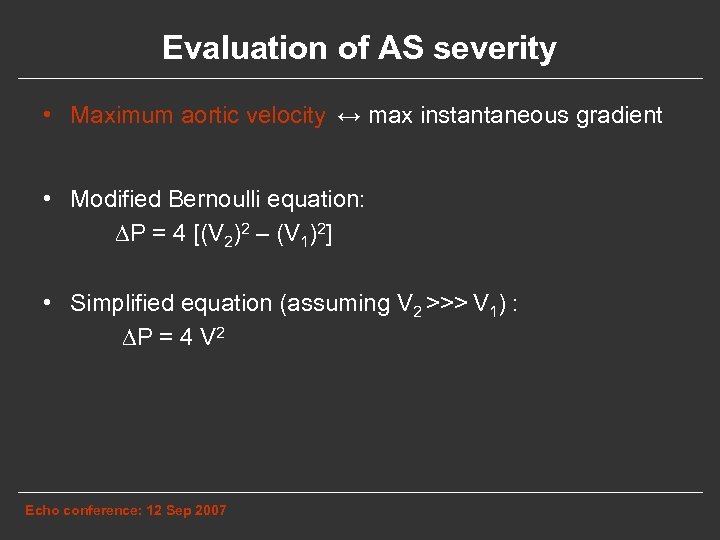 Evaluation of AS severity • Maximum aortic velocity ↔ max instantaneous gradient • Modified Bernoulli equation: ∆P = 4 [(V 2)2 – (V 1)2] • Simplified equation (assuming V 2 >>> V 1) : ∆P = 4 V 2 Echo conference: 12 Sep 2007
Evaluation of AS severity • Maximum aortic velocity ↔ max instantaneous gradient • Modified Bernoulli equation: ∆P = 4 [(V 2)2 – (V 1)2] • Simplified equation (assuming V 2 >>> V 1) : ∆P = 4 V 2 Echo conference: 12 Sep 2007
 Evaluation of AS severity • Maximum aortic velocity • Most reproducible • Strongest predictor of clinical outcomes • Mild: • Moderate: • Severe: Echo conference: 12 Sep 2007 2. 6 – 3. 0 m/s 3 – 4 m/s >4 m/s
Evaluation of AS severity • Maximum aortic velocity • Most reproducible • Strongest predictor of clinical outcomes • Mild: • Moderate: • Severe: Echo conference: 12 Sep 2007 2. 6 – 3. 0 m/s 3 – 4 m/s >4 m/s
 Evaluation of AS severity • Maximum aortic velocity • Mean transvalvular gradient • Aortic valve area by continuity equation Echo conference: 12 Sep 2007
Evaluation of AS severity • Maximum aortic velocity • Mean transvalvular gradient • Aortic valve area by continuity equation Echo conference: 12 Sep 2007
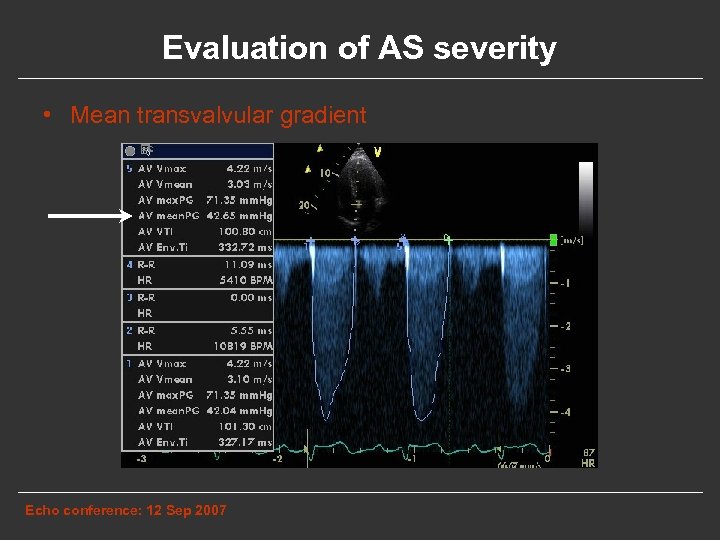 Evaluation of AS severity • Mean transvalvular gradient Echo conference: 12 Sep 2007
Evaluation of AS severity • Mean transvalvular gradient Echo conference: 12 Sep 2007
 Evaluation of AS severity • Mean transvalvular gradient • Mild: • Moderate: • Severe: Echo conference: 12 Sep 2007 < 25 mm Hg 25 – 40 mm Hg > 40 mm Hg
Evaluation of AS severity • Mean transvalvular gradient • Mild: • Moderate: • Severe: Echo conference: 12 Sep 2007 < 25 mm Hg 25 – 40 mm Hg > 40 mm Hg
 Evaluation of AS severity • Maximum aortic velocity • Mean transvalvular gradient • Aortic valve area by continuity equation Echo conference: 12 Sep 2007
Evaluation of AS severity • Maximum aortic velocity • Mean transvalvular gradient • Aortic valve area by continuity equation Echo conference: 12 Sep 2007
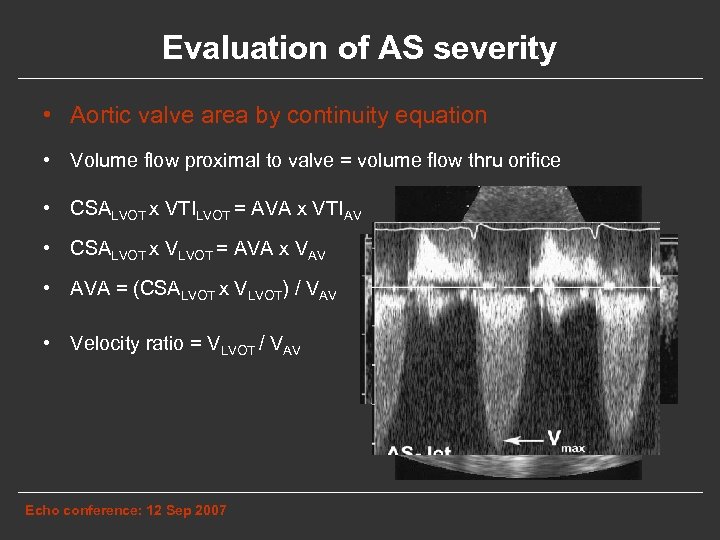 Evaluation of AS severity • Aortic valve area by continuity equation • Volume flow proximal to valve = volume flow thru orifice • CSALVOT x VTILVOT = AVA x VTIAV • CSALVOT x VLVOT = AVA x VAV • AVA = (CSALVOT x VLVOT) / VAV • Velocity ratio = VLVOT / VAV Echo conference: 12 Sep 2007
Evaluation of AS severity • Aortic valve area by continuity equation • Volume flow proximal to valve = volume flow thru orifice • CSALVOT x VTILVOT = AVA x VTIAV • CSALVOT x VLVOT = AVA x VAV • AVA = (CSALVOT x VLVOT) / VAV • Velocity ratio = VLVOT / VAV Echo conference: 12 Sep 2007
 Evaluation of AS severity • Aortic valve area by continuity equation • Severity by AHA criteria: – Mild: – Moderate: – Severe: > 1. 5 cm 2 1. 0 – 1. 5 cm 2 < 1. 0 cm 2 • Severity by BIDMC criteria: – Mild: – Moderate: – Severe: > 1. 2 cm 2 0. 8 – 1. 2 cm 2 < 0. 8 cm 2 • Dimensionless ratio < 0. 25 corresponds to severe AS Echo conference: 12 Sep 2007
Evaluation of AS severity • Aortic valve area by continuity equation • Severity by AHA criteria: – Mild: – Moderate: – Severe: > 1. 5 cm 2 1. 0 – 1. 5 cm 2 < 1. 0 cm 2 • Severity by BIDMC criteria: – Mild: – Moderate: – Severe: > 1. 2 cm 2 0. 8 – 1. 2 cm 2 < 0. 8 cm 2 • Dimensionless ratio < 0. 25 corresponds to severe AS Echo conference: 12 Sep 2007
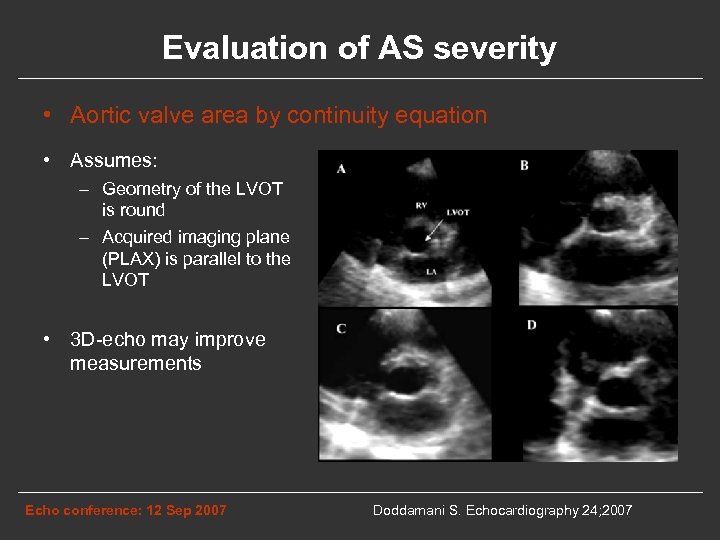 Evaluation of AS severity • Aortic valve area by continuity equation • Assumes: – Geometry of the LVOT is round – Acquired imaging plane (PLAX) is parallel to the LVOT • 3 D-echo may improve measurements Echo conference: 12 Sep 2007 Doddamani S. Echocardiography 24; 2007
Evaluation of AS severity • Aortic valve area by continuity equation • Assumes: – Geometry of the LVOT is round – Acquired imaging plane (PLAX) is parallel to the LVOT • 3 D-echo may improve measurements Echo conference: 12 Sep 2007 Doddamani S. Echocardiography 24; 2007
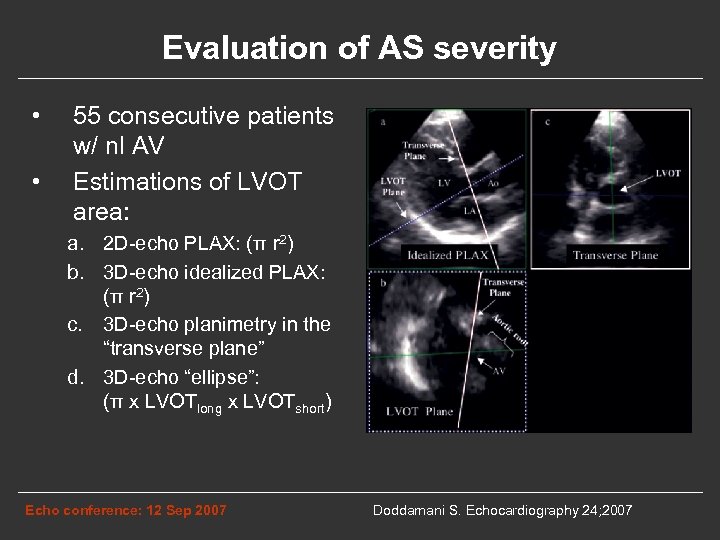 Evaluation of AS severity • • 55 consecutive patients w/ nl AV Estimations of LVOT area: a. 2 D-echo PLAX: (π r 2) b. 3 D-echo idealized PLAX: (π r 2) c. 3 D-echo planimetry in the “transverse plane” d. 3 D-echo “ellipse”: (π x LVOTlong x LVOTshort) Echo conference: 12 Sep 2007 Doddamani S. Echocardiography 24; 2007
Evaluation of AS severity • • 55 consecutive patients w/ nl AV Estimations of LVOT area: a. 2 D-echo PLAX: (π r 2) b. 3 D-echo idealized PLAX: (π r 2) c. 3 D-echo planimetry in the “transverse plane” d. 3 D-echo “ellipse”: (π x LVOTlong x LVOTshort) Echo conference: 12 Sep 2007 Doddamani S. Echocardiography 24; 2007
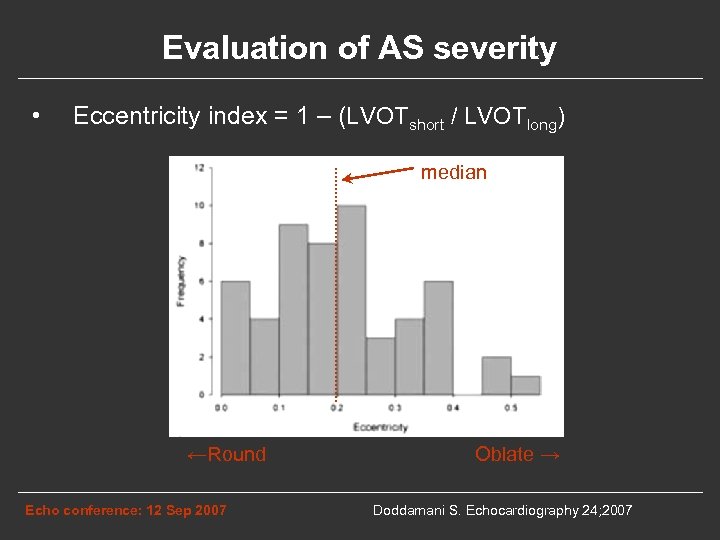 Evaluation of AS severity • Eccentricity index = 1 – (LVOTshort / LVOTlong) median ←Round Echo conference: 12 Sep 2007 Oblate → Doddamani S. Echocardiography 24; 2007
Evaluation of AS severity • Eccentricity index = 1 – (LVOTshort / LVOTlong) median ←Round Echo conference: 12 Sep 2007 Oblate → Doddamani S. Echocardiography 24; 2007
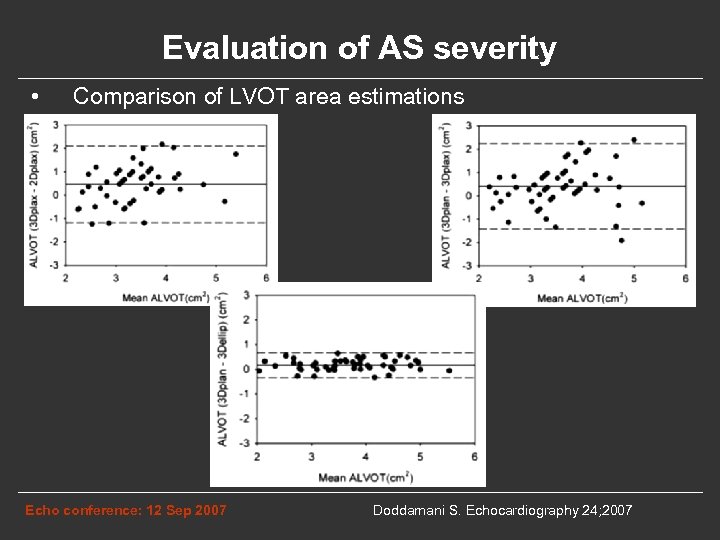 Evaluation of AS severity • Comparison of LVOT area estimations Echo conference: 12 Sep 2007 Doddamani S. Echocardiography 24; 2007
Evaluation of AS severity • Comparison of LVOT area estimations Echo conference: 12 Sep 2007 Doddamani S. Echocardiography 24; 2007
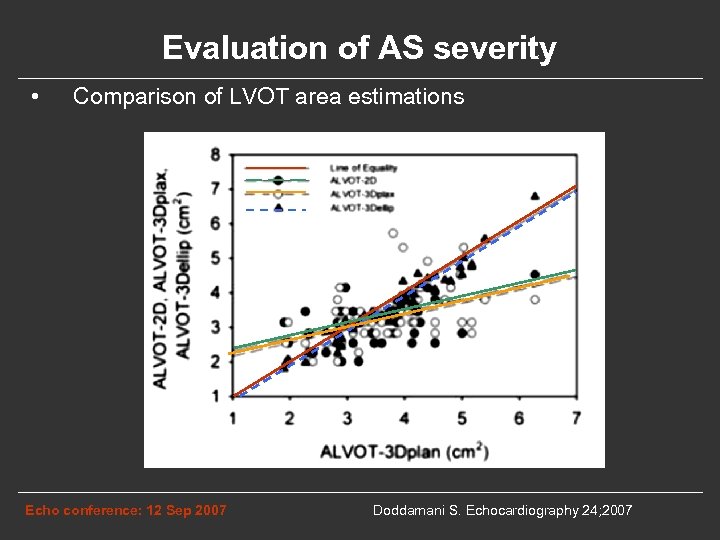 Evaluation of AS severity • Comparison of LVOT area estimations Echo conference: 12 Sep 2007 Doddamani S. Echocardiography 24; 2007
Evaluation of AS severity • Comparison of LVOT area estimations Echo conference: 12 Sep 2007 Doddamani S. Echocardiography 24; 2007
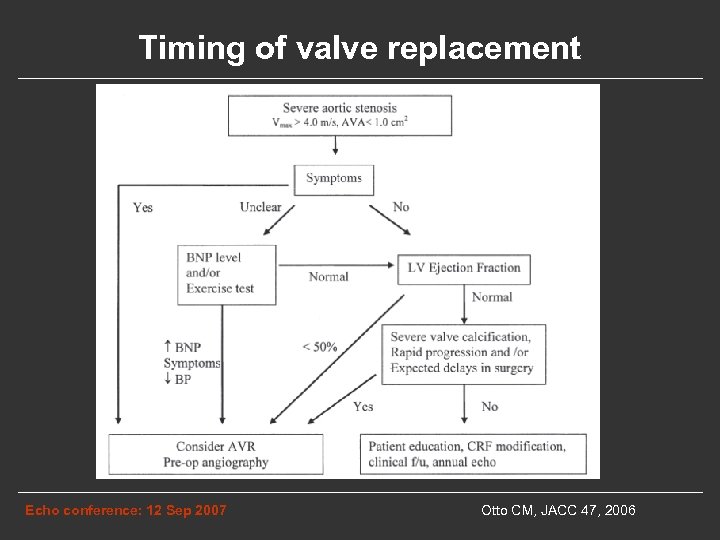 Timing of valve replacement Echo conference: 12 Sep 2007 Otto CM, JACC 47, 2006
Timing of valve replacement Echo conference: 12 Sep 2007 Otto CM, JACC 47, 2006
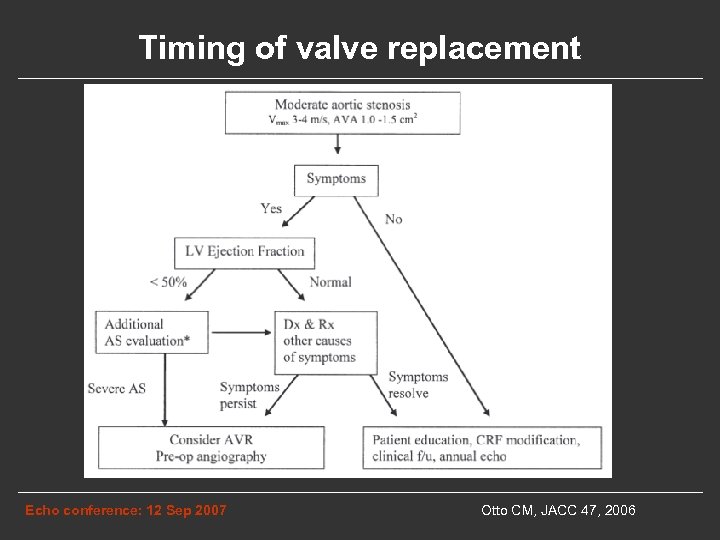 Timing of valve replacement Echo conference: 12 Sep 2007 Otto CM, JACC 47, 2006
Timing of valve replacement Echo conference: 12 Sep 2007 Otto CM, JACC 47, 2006
 Asymptomatic patients • Risk of sudden death with AS < 1% • What is the risk of surgery? Echo conference: 12 Sep 2007
Asymptomatic patients • Risk of sudden death with AS < 1% • What is the risk of surgery? Echo conference: 12 Sep 2007
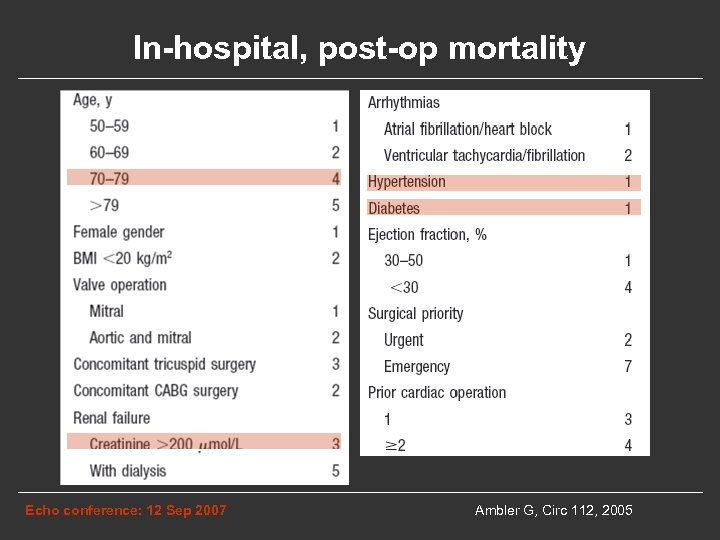 In-hospital, post-op mortality Echo conference: 12 Sep 2007 Ambler G, Circ 112, 2005
In-hospital, post-op mortality Echo conference: 12 Sep 2007 Ambler G, Circ 112, 2005
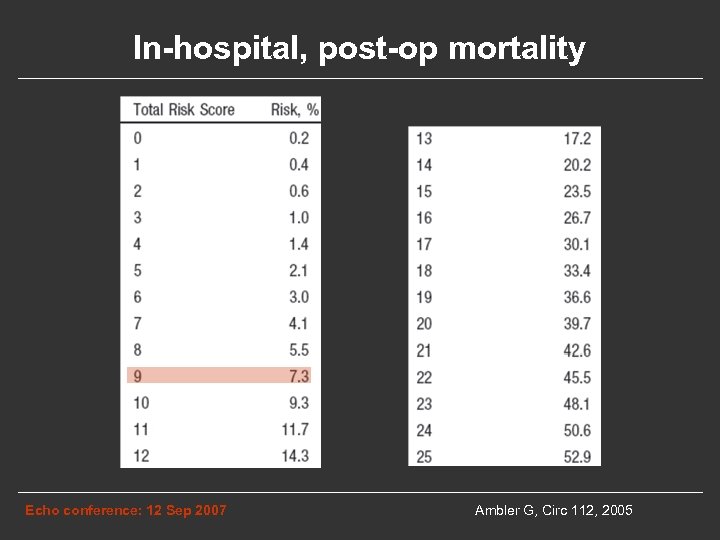 In-hospital, post-op mortality Echo conference: 12 Sep 2007 Ambler G, Circ 112, 2005
In-hospital, post-op mortality Echo conference: 12 Sep 2007 Ambler G, Circ 112, 2005
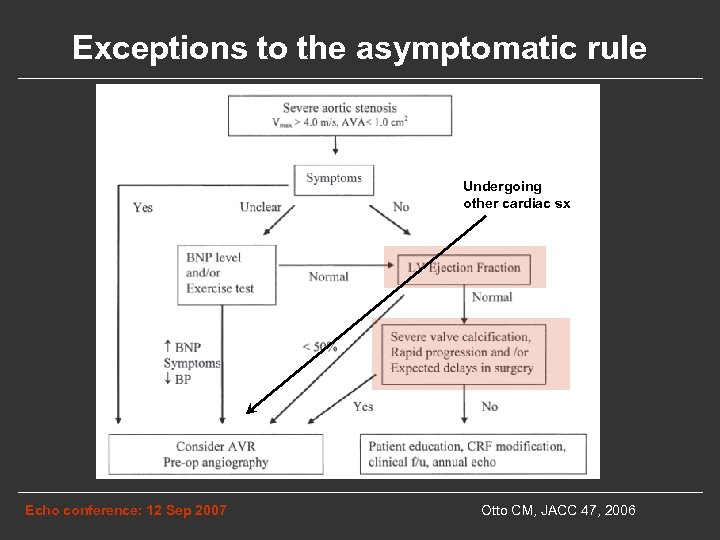 Exceptions to the asymptomatic rule Undergoing other cardiac sx Echo conference: 12 Sep 2007 Otto CM, JACC 47, 2006
Exceptions to the asymptomatic rule Undergoing other cardiac sx Echo conference: 12 Sep 2007 Otto CM, JACC 47, 2006
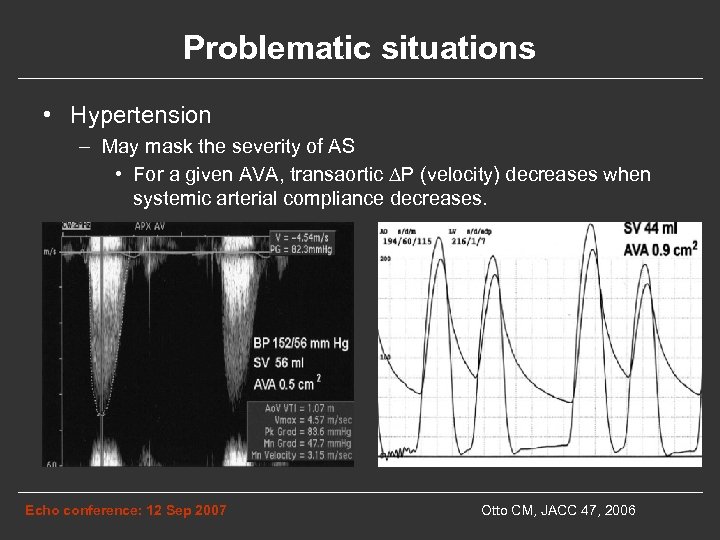 Problematic situations • Hypertension – May mask the severity of AS • For a given AVA, transaortic ∆P (velocity) decreases when systemic arterial compliance decreases. Echo conference: 12 Sep 2007 Otto CM, JACC 47, 2006
Problematic situations • Hypertension – May mask the severity of AS • For a given AVA, transaortic ∆P (velocity) decreases when systemic arterial compliance decreases. Echo conference: 12 Sep 2007 Otto CM, JACC 47, 2006
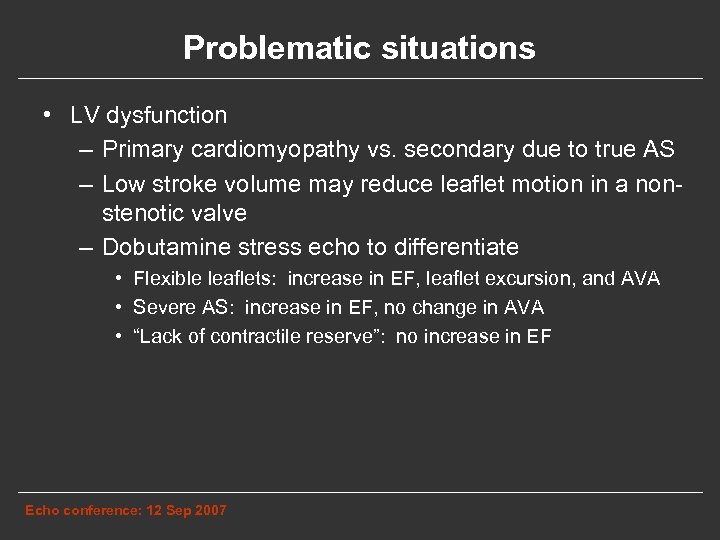 Problematic situations • LV dysfunction – Primary cardiomyopathy vs. secondary due to true AS – Low stroke volume may reduce leaflet motion in a nonstenotic valve – Dobutamine stress echo to differentiate • Flexible leaflets: increase in EF, leaflet excursion, and AVA • Severe AS: increase in EF, no change in AVA • “Lack of contractile reserve”: no increase in EF Echo conference: 12 Sep 2007
Problematic situations • LV dysfunction – Primary cardiomyopathy vs. secondary due to true AS – Low stroke volume may reduce leaflet motion in a nonstenotic valve – Dobutamine stress echo to differentiate • Flexible leaflets: increase in EF, leaflet excursion, and AVA • Severe AS: increase in EF, no change in AVA • “Lack of contractile reserve”: no increase in EF Echo conference: 12 Sep 2007
 Congenital AS • Subvalvar • Supravalvar • Valvar Echo conference: 12 Sep 2007
Congenital AS • Subvalvar • Supravalvar • Valvar Echo conference: 12 Sep 2007
 Subvalvar / Subaortic stenosis • Dynamic stenosis: – HOCM • Fixed stenosis: – Thin membrane – Thick fibromuscular ridge Echo conference: 12 Sep 2007
Subvalvar / Subaortic stenosis • Dynamic stenosis: – HOCM • Fixed stenosis: – Thin membrane – Thick fibromuscular ridge Echo conference: 12 Sep 2007
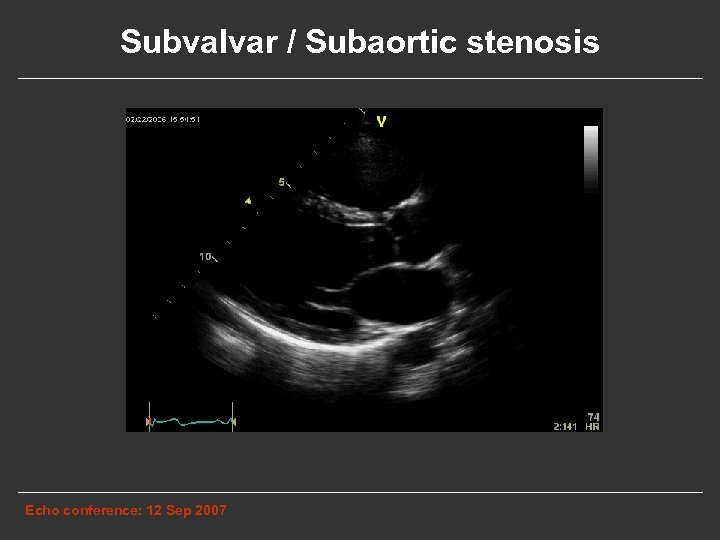 Subvalvar / Subaortic stenosis Echo conference: 12 Sep 2007
Subvalvar / Subaortic stenosis Echo conference: 12 Sep 2007
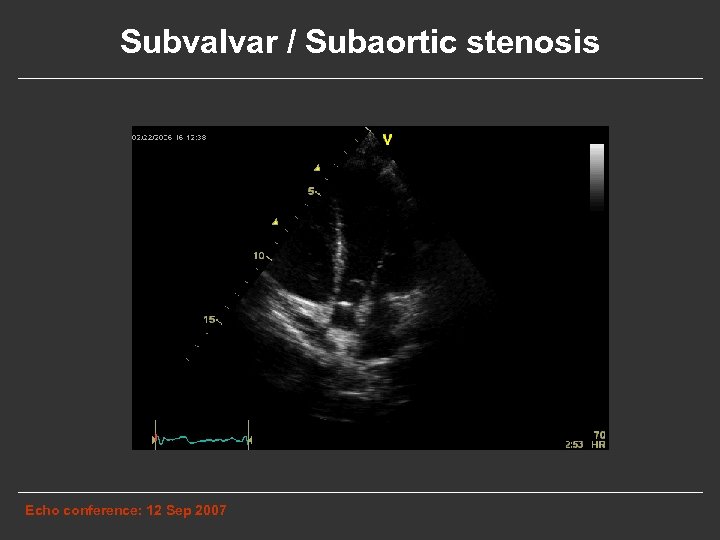 Subvalvar / Subaortic stenosis Echo conference: 12 Sep 2007
Subvalvar / Subaortic stenosis Echo conference: 12 Sep 2007
 Subaortic stenosis • Pathophysiology – Underlying abnormality of LVOT structure – Turbulent flow → progressive LVOT fibrosis → AV leaflet thickening → AR 55% – Infectious endocarditis 12% • Timing of surgery – Children: gradient ≥ 30 mm Hg – Adults: gradient ≥ 50 mm Hg – AR • Recurrence rate: 15 - 27% reoperation Echo conference: 12 Sep 2007
Subaortic stenosis • Pathophysiology – Underlying abnormality of LVOT structure – Turbulent flow → progressive LVOT fibrosis → AV leaflet thickening → AR 55% – Infectious endocarditis 12% • Timing of surgery – Children: gradient ≥ 30 mm Hg – Adults: gradient ≥ 50 mm Hg – AR • Recurrence rate: 15 - 27% reoperation Echo conference: 12 Sep 2007
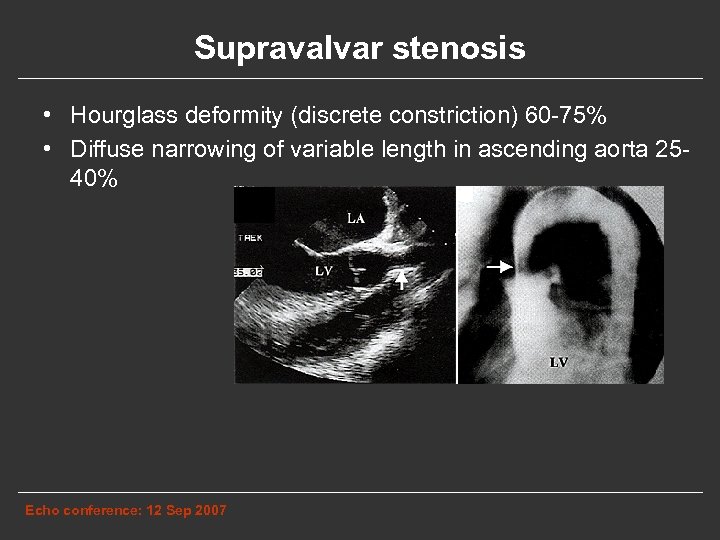 Supravalvar stenosis • Hourglass deformity (discrete constriction) 60 -75% • Diffuse narrowing of variable length in ascending aorta 2540% Echo conference: 12 Sep 2007
Supravalvar stenosis • Hourglass deformity (discrete constriction) 60 -75% • Diffuse narrowing of variable length in ascending aorta 2540% Echo conference: 12 Sep 2007
 Supravalvar stenosis • Etiologies – – Homozygous familial hypercholesterolemia Familial autosomal dominant form – mutation of elastin gene Sporadic mutation form As a feature of Williams syndrome • Gene deletions (including elastin) • Short stature, facial abnormalities, visuospatial cognition defects, renovascular HTN, mental retardation • Endocarditis prophylaxis • Indications for surgery uncertain Echo conference: 12 Sep 2007
Supravalvar stenosis • Etiologies – – Homozygous familial hypercholesterolemia Familial autosomal dominant form – mutation of elastin gene Sporadic mutation form As a feature of Williams syndrome • Gene deletions (including elastin) • Short stature, facial abnormalities, visuospatial cognition defects, renovascular HTN, mental retardation • Endocarditis prophylaxis • Indications for surgery uncertain Echo conference: 12 Sep 2007
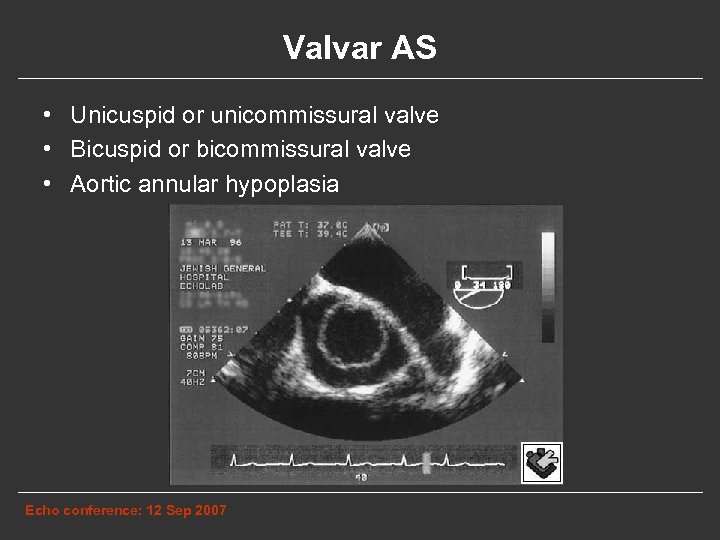 Valvar AS • Unicuspid or unicommissural valve • Bicuspid or bicommissural valve • Aortic annular hypoplasia Echo conference: 12 Sep 2007
Valvar AS • Unicuspid or unicommissural valve • Bicuspid or bicommissural valve • Aortic annular hypoplasia Echo conference: 12 Sep 2007
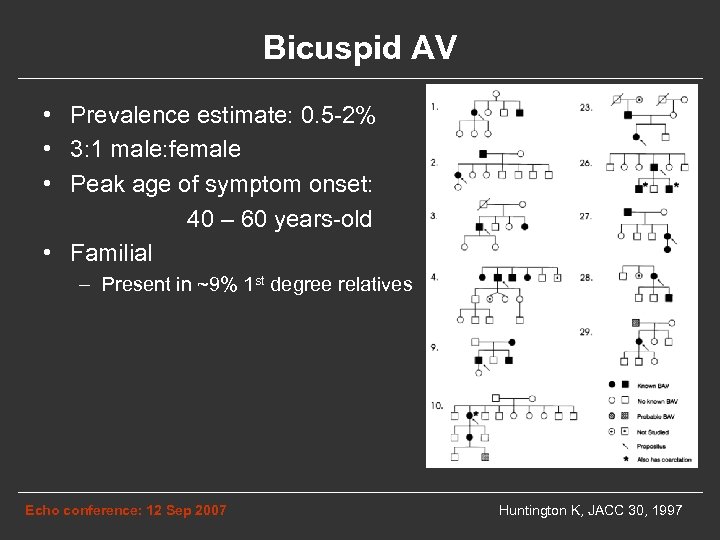 Bicuspid AV • Prevalence estimate: 0. 5 -2% • 3: 1 male: female • Peak age of symptom onset: 40 – 60 years-old • Familial – Present in ~9% 1 st degree relatives Echo conference: 12 Sep 2007 Huntington K, JACC 30, 1997
Bicuspid AV • Prevalence estimate: 0. 5 -2% • 3: 1 male: female • Peak age of symptom onset: 40 – 60 years-old • Familial – Present in ~9% 1 st degree relatives Echo conference: 12 Sep 2007 Huntington K, JACC 30, 1997
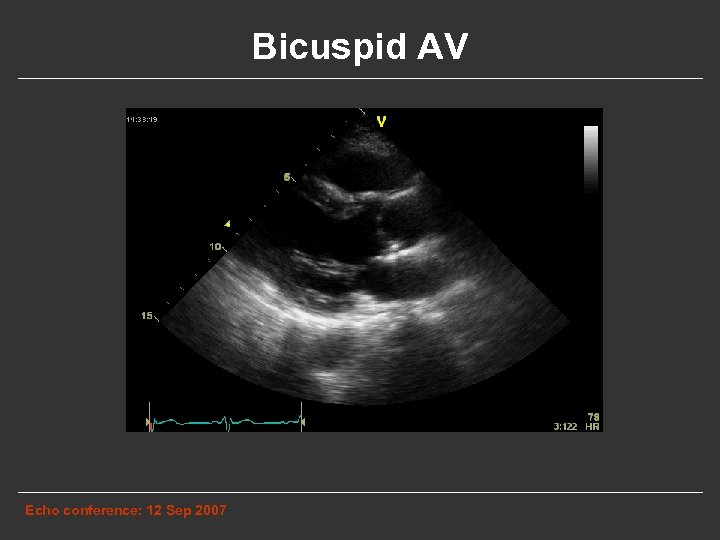 Bicuspid AV Echo conference: 12 Sep 2007
Bicuspid AV Echo conference: 12 Sep 2007
 Bicuspid AV Echo conference: 12 Sep 2007
Bicuspid AV Echo conference: 12 Sep 2007
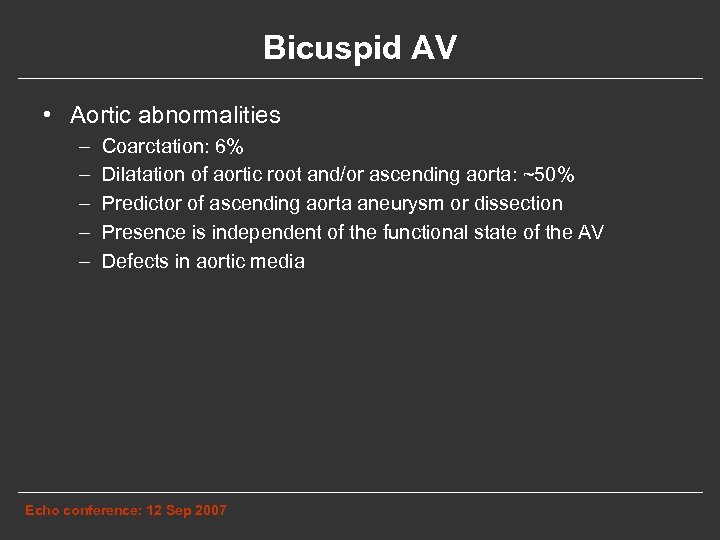 Bicuspid AV • Aortic abnormalities – – – Coarctation: 6% Dilatation of aortic root and/or ascending aorta: ~50% Predictor of ascending aorta aneurysm or dissection Presence is independent of the functional state of the AV Defects in aortic media Echo conference: 12 Sep 2007
Bicuspid AV • Aortic abnormalities – – – Coarctation: 6% Dilatation of aortic root and/or ascending aorta: ~50% Predictor of ascending aorta aneurysm or dissection Presence is independent of the functional state of the AV Defects in aortic media Echo conference: 12 Sep 2007
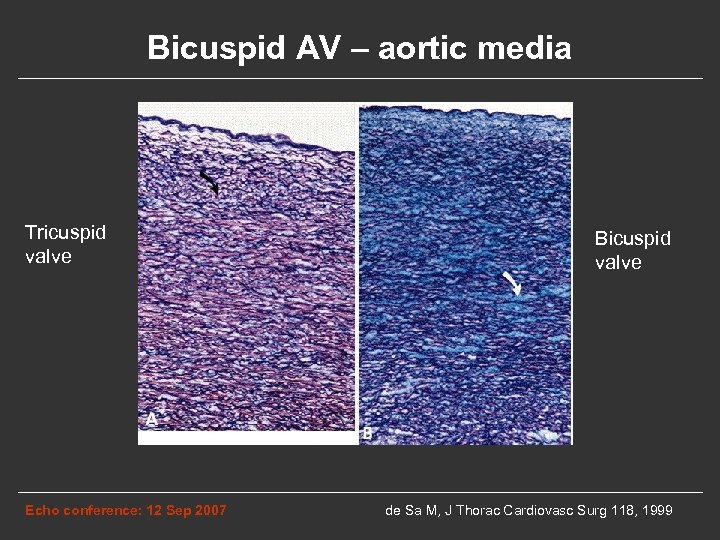 Bicuspid AV – aortic media Tricuspid valve Echo conference: 12 Sep 2007 Bicuspid valve de Sa M, J Thorac Cardiovasc Surg 118, 1999
Bicuspid AV – aortic media Tricuspid valve Echo conference: 12 Sep 2007 Bicuspid valve de Sa M, J Thorac Cardiovasc Surg 118, 1999
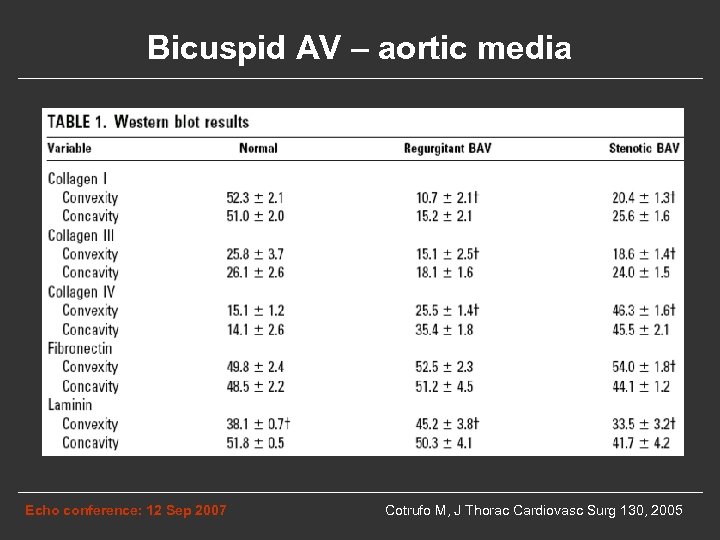 Bicuspid AV – aortic media Echo conference: 12 Sep 2007 Cotrufo M, J Thorac Cardiovasc Surg 130, 2005
Bicuspid AV – aortic media Echo conference: 12 Sep 2007 Cotrufo M, J Thorac Cardiovasc Surg 130, 2005
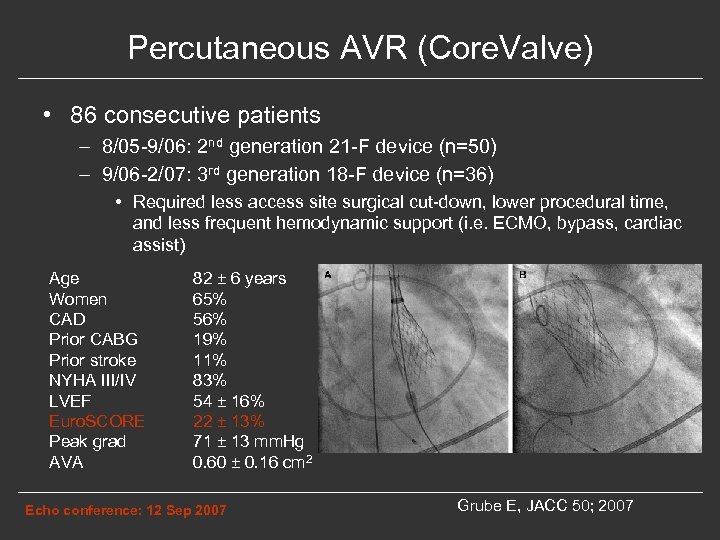 Percutaneous AVR (Core. Valve) • 86 consecutive patients – 8/05 -9/06: 2 nd generation 21 -F device (n=50) – 9/06 -2/07: 3 rd generation 18 -F device (n=36) • Required less access site surgical cut-down, lower procedural time, and less frequent hemodynamic support (i. e. ECMO, bypass, cardiac assist) Age Women CAD Prior CABG Prior stroke NYHA III/IV LVEF Euro. SCORE Peak grad AVA 82 ± 6 years 65% 56% 19% 11% 83% 54 ± 16% 22 ± 13% 71 ± 13 mm. Hg 0. 60 ± 0. 16 cm 2 Echo conference: 12 Sep 2007 Grube E, JACC 50; 2007
Percutaneous AVR (Core. Valve) • 86 consecutive patients – 8/05 -9/06: 2 nd generation 21 -F device (n=50) – 9/06 -2/07: 3 rd generation 18 -F device (n=36) • Required less access site surgical cut-down, lower procedural time, and less frequent hemodynamic support (i. e. ECMO, bypass, cardiac assist) Age Women CAD Prior CABG Prior stroke NYHA III/IV LVEF Euro. SCORE Peak grad AVA 82 ± 6 years 65% 56% 19% 11% 83% 54 ± 16% 22 ± 13% 71 ± 13 mm. Hg 0. 60 ± 0. 16 cm 2 Echo conference: 12 Sep 2007 Grube E, JACC 50; 2007
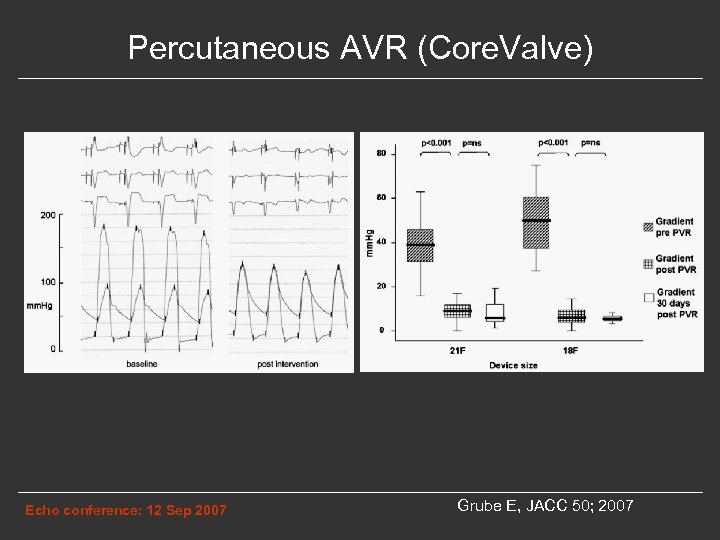 Percutaneous AVR (Core. Valve) Echo conference: 12 Sep 2007 Grube E, JACC 50; 2007
Percutaneous AVR (Core. Valve) Echo conference: 12 Sep 2007 Grube E, JACC 50; 2007
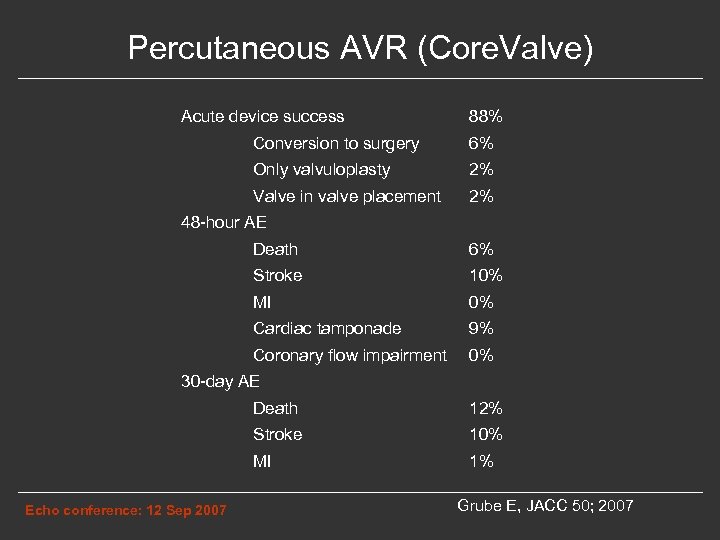 Percutaneous AVR (Core. Valve) Acute device success 88% Conversion to surgery 6% Only valvuloplasty 2% Valve in valve placement 2% 48 -hour AE Death 6% Stroke 10% MI 0% Cardiac tamponade 9% Coronary flow impairment 0% 30 -day AE Death Stroke 10% MI Echo conference: 12 Sep 2007 12% 1% Grube E, JACC 50; 2007
Percutaneous AVR (Core. Valve) Acute device success 88% Conversion to surgery 6% Only valvuloplasty 2% Valve in valve placement 2% 48 -hour AE Death 6% Stroke 10% MI 0% Cardiac tamponade 9% Coronary flow impairment 0% 30 -day AE Death Stroke 10% MI Echo conference: 12 Sep 2007 12% 1% Grube E, JACC 50; 2007
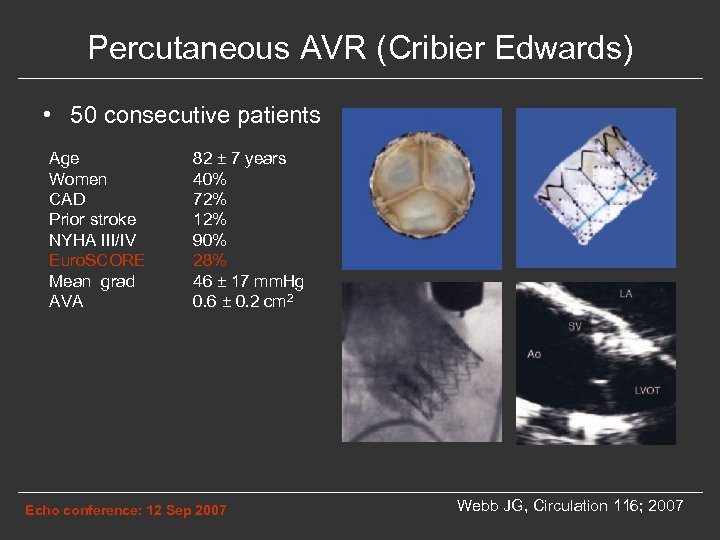 Percutaneous AVR (Cribier Edwards) • 50 consecutive patients Age Women CAD Prior stroke NYHA III/IV Euro. SCORE Mean grad AVA 82 ± 7 years 40% 72% 12% 90% 28% 46 ± 17 mm. Hg 0. 6 ± 0. 2 cm 2 Echo conference: 12 Sep 2007 Webb JG, Circulation 116; 2007
Percutaneous AVR (Cribier Edwards) • 50 consecutive patients Age Women CAD Prior stroke NYHA III/IV Euro. SCORE Mean grad AVA 82 ± 7 years 40% 72% 12% 90% 28% 46 ± 17 mm. Hg 0. 6 ± 0. 2 cm 2 Echo conference: 12 Sep 2007 Webb JG, Circulation 116; 2007
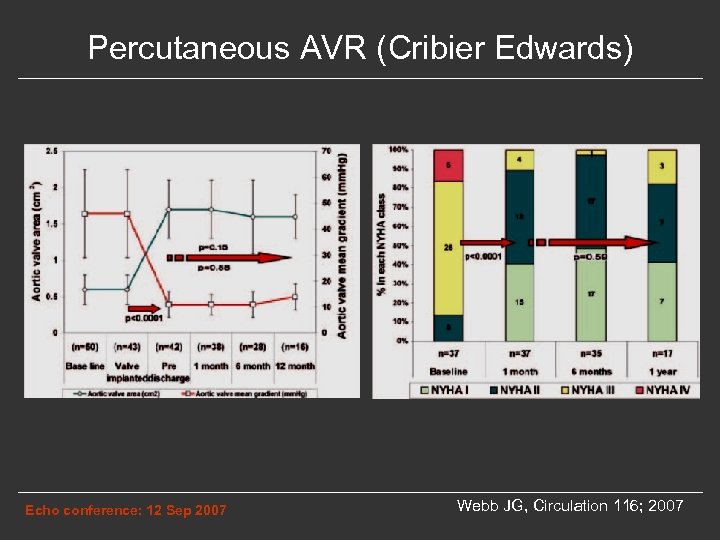 Percutaneous AVR (Cribier Edwards) Echo conference: 12 Sep 2007 Webb JG, Circulation 116; 2007
Percutaneous AVR (Cribier Edwards) Echo conference: 12 Sep 2007 Webb JG, Circulation 116; 2007
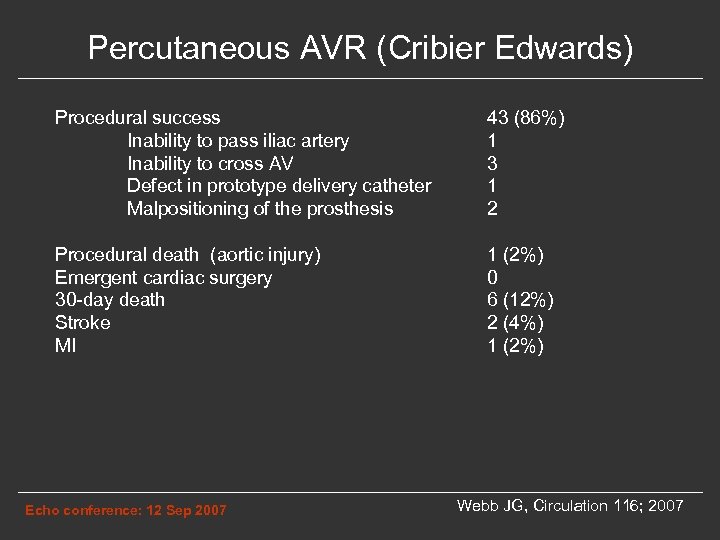 Percutaneous AVR (Cribier Edwards) Procedural success Inability to pass iliac artery Inability to cross AV Defect in prototype delivery catheter Malpositioning of the prosthesis 43 (86%) 1 3 1 2 Procedural death (aortic injury) Emergent cardiac surgery 30 -day death Stroke MI 1 (2%) 0 6 (12%) 2 (4%) 1 (2%) Echo conference: 12 Sep 2007 Webb JG, Circulation 116; 2007
Percutaneous AVR (Cribier Edwards) Procedural success Inability to pass iliac artery Inability to cross AV Defect in prototype delivery catheter Malpositioning of the prosthesis 43 (86%) 1 3 1 2 Procedural death (aortic injury) Emergent cardiac surgery 30 -day death Stroke MI 1 (2%) 0 6 (12%) 2 (4%) 1 (2%) Echo conference: 12 Sep 2007 Webb JG, Circulation 116; 2007


