ANTIBIOTICSLearning Points Basics Choosing antibiotics Overview. Basics Make

ANTIBIOTICS
Learning Points Basics Choosing antibiotics Overview
Basics Make sure you try to collect cultures before starting antibiotics Many antibiotics require renal dosing, such as vancomycin. If you’re unsure the dose call the pharmacist. ID approval is required for many antibiotics such as vancomycin, levofloxacin, ciprofloxacin. Call the ID fellow for approval when required. Use your Sanford Guide and hospital antibiograms to help guide you Sanford Guide now has an app for iphones – very useful on the wards! Epocrates app also has useful guides
Case A 62-year-old man with history of poorly controlled Diabetes, HTN, and Hyperlipidemia presents with worsening left lower extremity pain. Physical exam reveals cellulitis and possible wound infection, with concern for osteomyelitis.
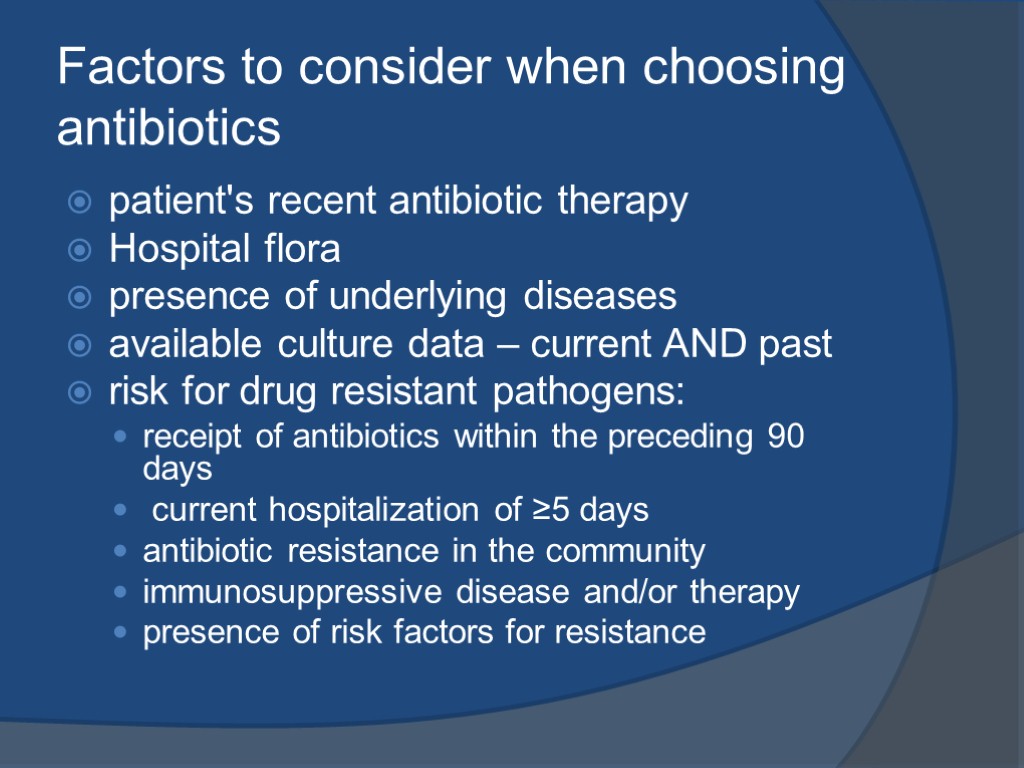
Factors to consider when choosing antibiotics patient's recent antibiotic therapy Hospital flora presence of underlying diseases available culture data – current AND past risk for drug resistant pathogens: receipt of antibiotics within the preceding 90 days current hospitalization of ≥5 days antibiotic resistance in the community immunosuppressive disease and/or therapy presence of risk factors for resistance
Choosing an antibiotic: Think about Location: Where did the patient become ill? Travel? Exposure? Where did the infection anatomically originate? Where in the body, has or will the infection spread to? Think about the bug you are treating:
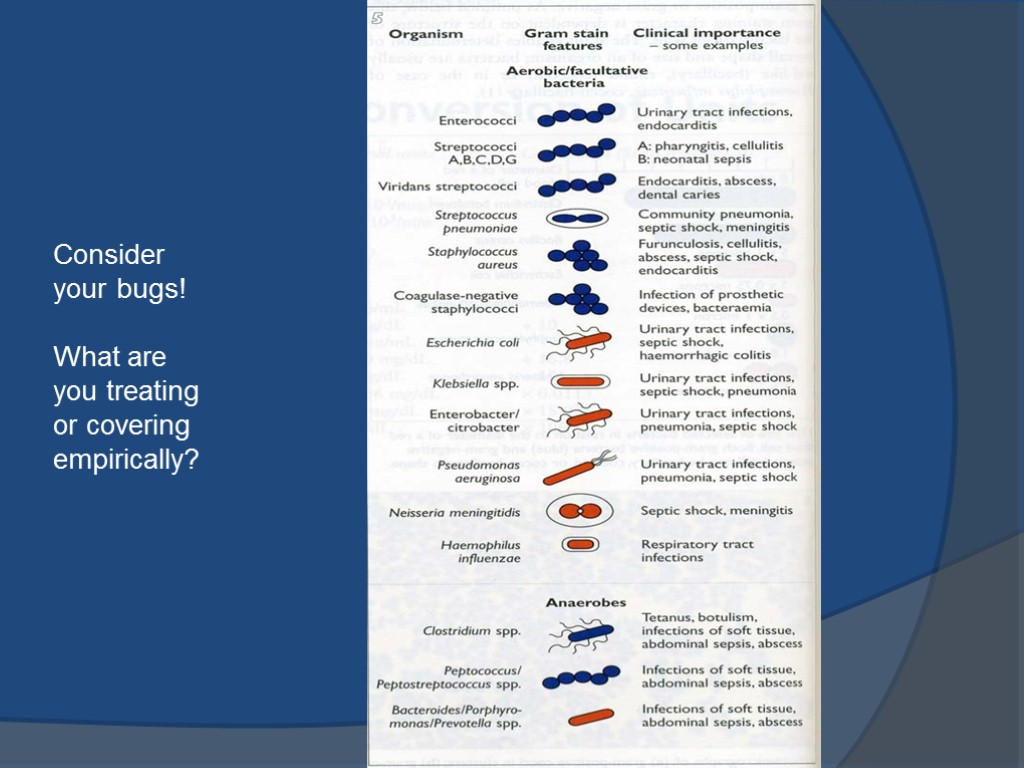
Consider your bugs! What are you treating or covering empirically?
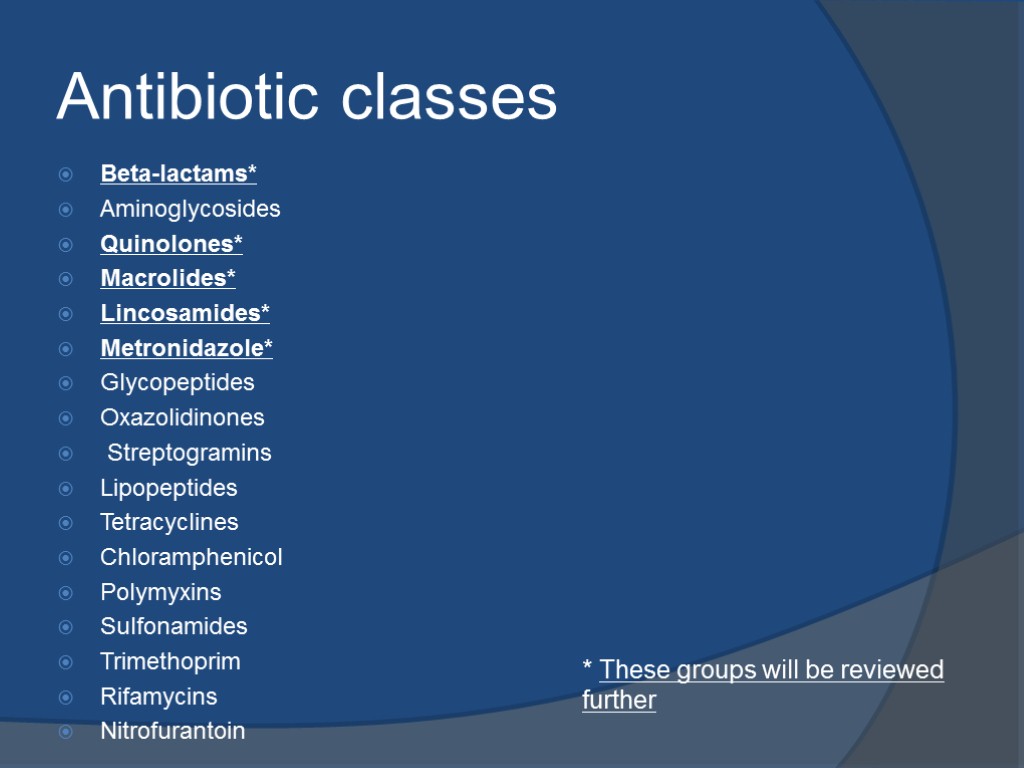
Antibiotic classes Beta-lactams* Aminoglycosides Quinolones* Macrolides* Lincosamides* Metronidazole* Glycopeptides Oxazolidinones Streptogramins Lipopeptides Tetracyclines Chloramphenicol Polymyxins Sulfonamides Trimethoprim Rifamycins Nitrofurantoin * These groups will be reviewed further
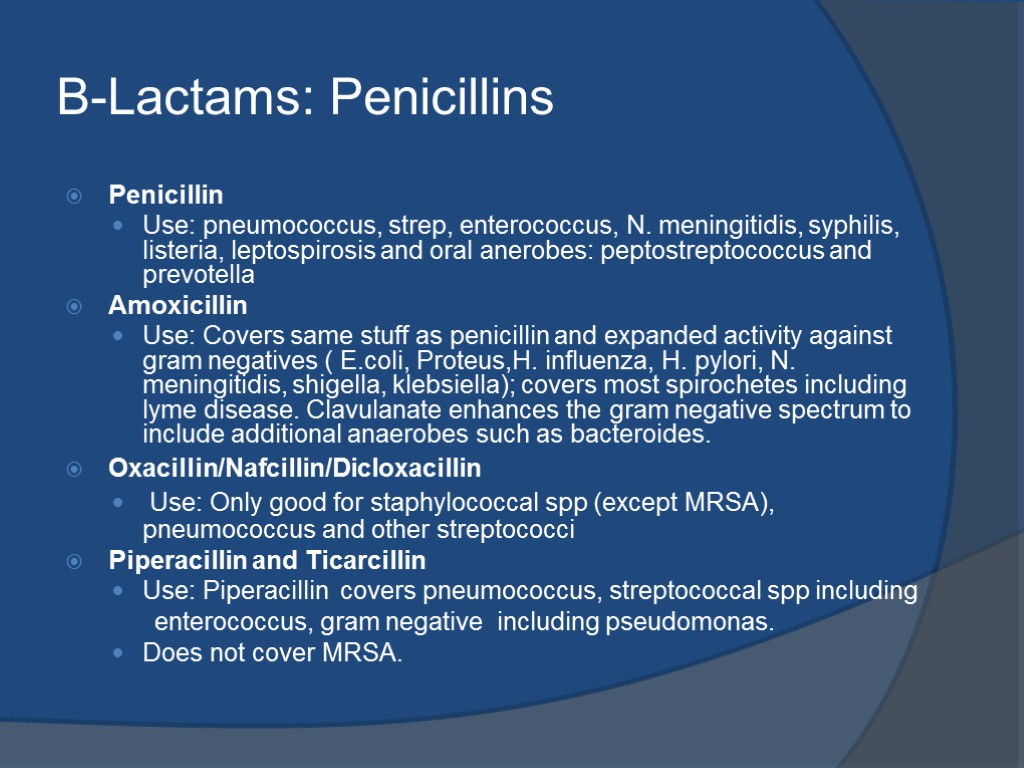
B-Lactams: Penicillins Penicillin Use: pneumococcus, strep, enterococcus, N. meningitidis, syphilis, listeria, leptospirosis and oral anerobes: peptostreptococcus and prevotella Amoxicillin Use: Covers same stuff as penicillin and expanded activity against gram negatives ( E.coli, Proteus,H. influenza, H. pylori, N. meningitidis, shigella, klebsiella); covers most spirochetes including lyme disease. Clavulanate enhances the gram negative spectrum to include additional anaerobes such as bacteroides. Oxacillin/Nafcillin/Dicloxacillin Use: Only good for staphylococcal spp (except MRSA), pneumococcus and other streptococci Piperacillin and Ticarcillin Use: Piperacillin covers pneumococcus, streptococcal spp including enterococcus, gram negative including pseudomonas. Does not cover MRSA.
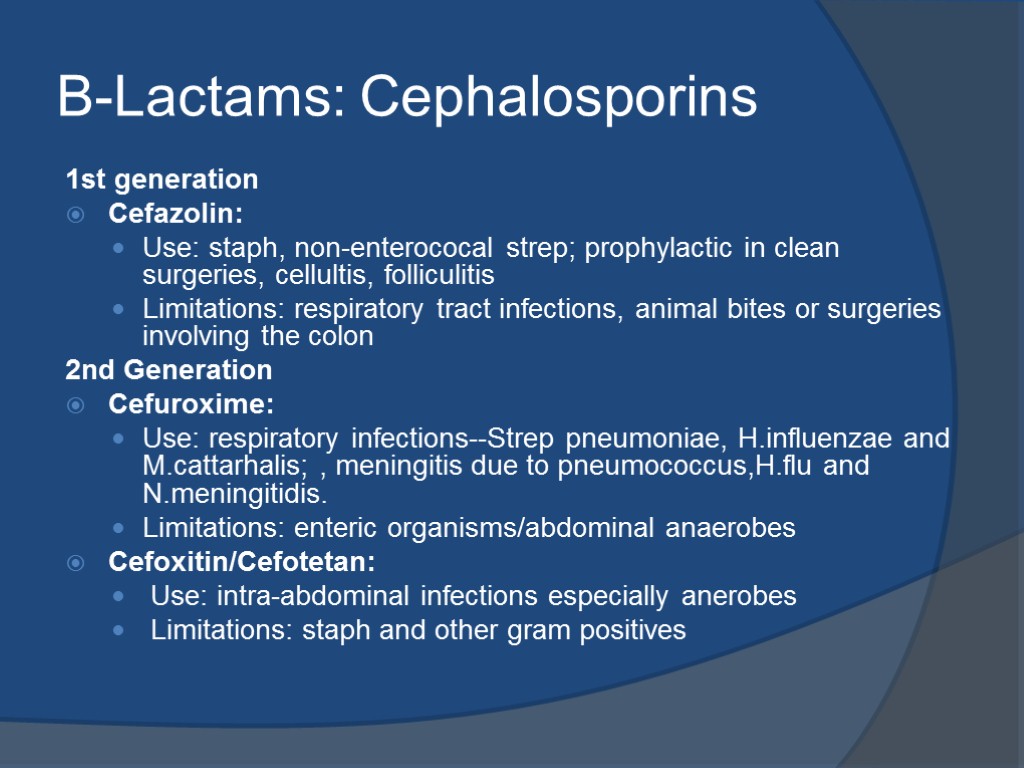
B-Lactams: Cephalosporins 1st generation Cefazolin: Use: staph, non-enterococal strep; prophylactic in clean surgeries, cellultis, folliculitis Limitations: respiratory tract infections, animal bites or surgeries involving the colon 2nd Generation Cefuroxime: Use: respiratory infections--Strep pneumoniae, H.influenzae and M.cattarhalis; , meningitis due to pneumococcus,H.flu and N.meningitidis. Limitations: enteric organisms/abdominal anaerobes Cefoxitin/Cefotetan: Use: intra-abdominal infections especially anerobes Limitations: staph and other gram positives
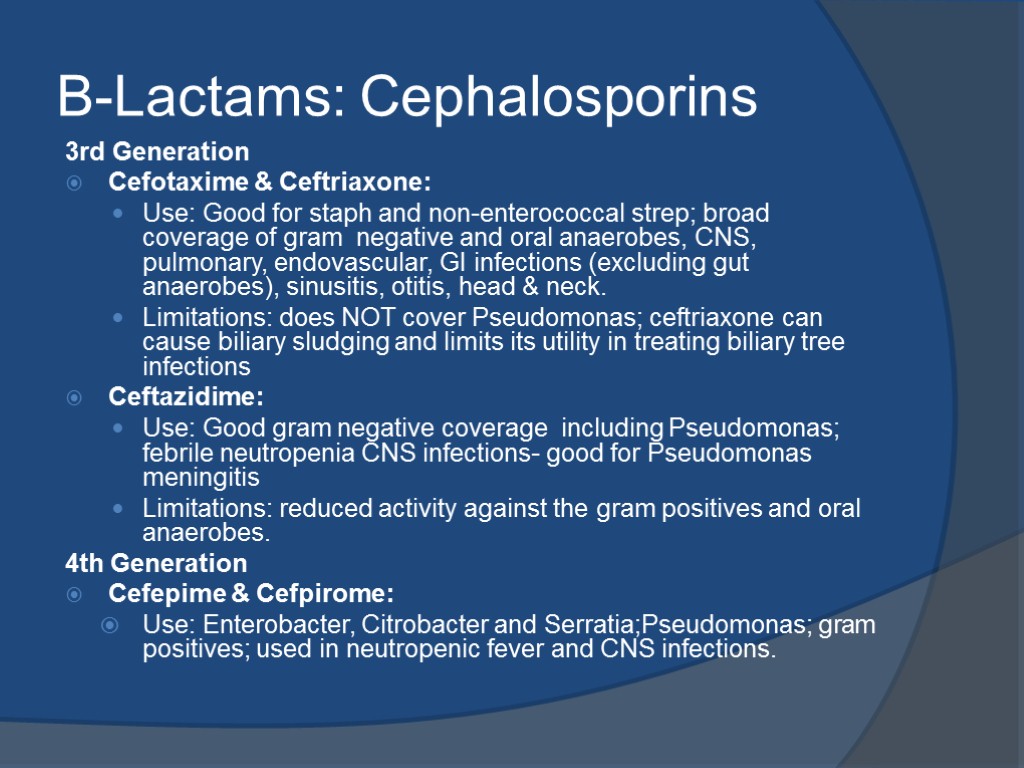
B-Lactams: Cephalosporins 3rd Generation Cefotaxime & Ceftriaxone: Use: Good for staph and non-enterococcal strep; broad coverage of gram negative and oral anaerobes, CNS, pulmonary, endovascular, GI infections (excluding gut anaerobes), sinusitis, otitis, head & neck. Limitations: does NOT cover Pseudomonas; ceftriaxone can cause biliary sludging and limits its utility in treating biliary tree infections Ceftazidime: Use: Good gram negative coverage including Pseudomonas; febrile neutropenia CNS infections- good for Pseudomonas meningitis Limitations: reduced activity against the gram positives and oral anaerobes. 4th Generation Cefepime & Cefpirome: Use: Enterobacter, Citrobacter and Serratia;Pseudomonas; gram positives; used in neutropenic fever and CNS infections.
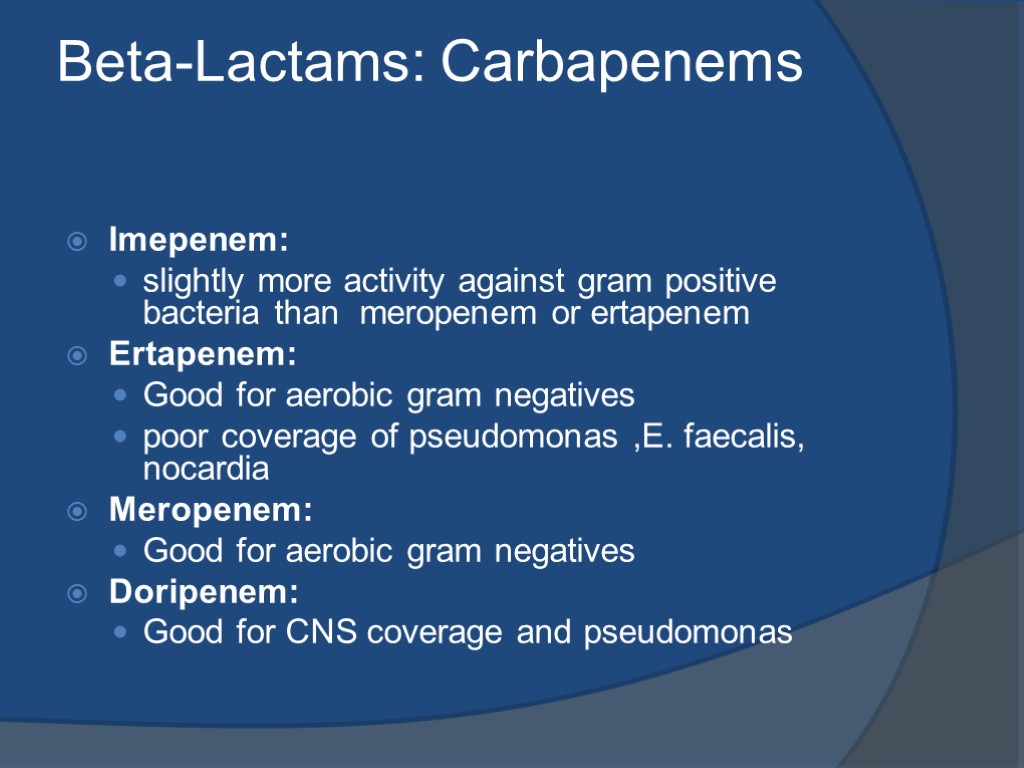
Beta-Lactams: Carbapenems Imepenem: slightly more activity against gram positive bacteria than meropenem or ertapenem Ertapenem: Good for aerobic gram negatives poor coverage of pseudomonas ,E. faecalis, nocardia Meropenem: Good for aerobic gram negatives Doripenem: Good for CNS coverage and pseudomonas
Beta-Lactams Cautions: Beta-lactam allergy can occur in up to 10% 5%-10% cross-sensitivity in penicillin, cephalosporins, and carbapenems Side effects: diarrhea, nausea, rash
Quinolones: Ciprofloxacin: Use: Covers most aerobic gram negatives including Pseudomonas. penetrates CNS, prostate, lungs Limited against staph Non-ciprofloxacin quinolones: Ofloxacin, Levofloxacin, Moxifloxacin: Gemifloxacin: Use: Great for respiratory pathogens, most enteric gram negatives Only levofloxacin covers pseudomonas Covers some atypicals: Mycoplasma, Chlamydia, Legionella Cautions: Can cause Qt prolongation, tendon rupture, CNS toxicity Do not use in patients with epilepsy or existing CNS lesions or inflammation Side effects: Commonly causes C diff
Macrolides: Erythromycin, Clarithromycin, Azithromycin Use: Broad spectrum against gram positives including strep, staph aureus (MSSA) Good for atypical oganism such as Mycoplasma, Chlamydia, Legionella Covers N.gonorrhea, H flu, Legionella Caution: can interact with statin to cause myopathy Can cause Qt prolongation Side effects: GI upset
Lincosamides: Clindamycin Use: Reasonable gram positive aerobic coverage against strep and many staph including MRSA Special role in treating strep in necrotizing fascitits Anaerobic coverage better then penicillin but not as good as metronidazole Caution: can interact with neuromuscular blocking agents and cyclosporine Side effects: Diarrhea, commonly causes C difficile—avoid clindamycin if other good options exist.
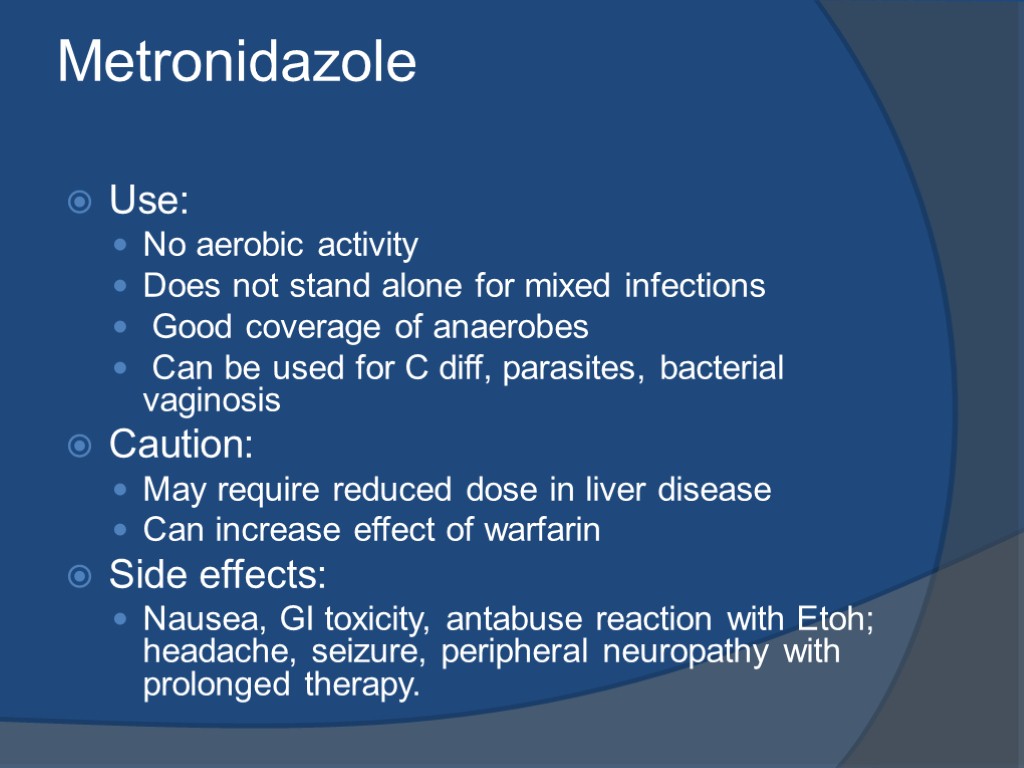
Metronidazole Use: No aerobic activity Does not stand alone for mixed infections Good coverage of anaerobes Can be used for C diff, parasites, bacterial vaginosis Caution: May require reduced dose in liver disease Can increase effect of warfarin Side effects: Nausea, GI toxicity, antabuse reaction with Etoh; headache, seizure, peripheral neuropathy with prolonged therapy.
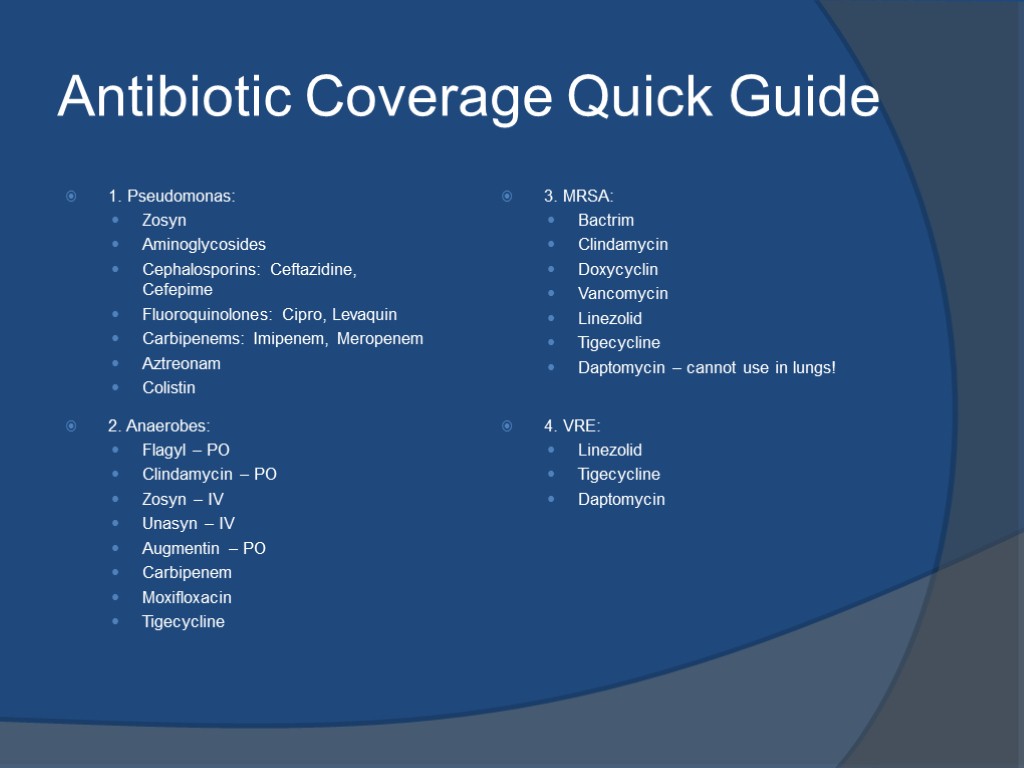
Antibiotic Coverage Quick Guide 1. Pseudomonas: Zosyn Aminoglycosides Cephalosporins: Ceftazidine, Cefepime Fluoroquinolones: Cipro, Levaquin Carbipenems: Imipenem, Meropenem Aztreonam Colistin 2. Anaerobes: Flagyl – PO Clindamycin – PO Zosyn – IV Unasyn – IV Augmentin – PO Carbipenem Moxifloxacin Tigecycline 3. MRSA: Bactrim Clindamycin Doxycyclin Vancomycin Linezolid Tigecycline Daptomycin – cannot use in lungs! 4. VRE: Linezolid Tigecycline Daptomycin
antibiotics_supporting_ppt.ppt
- Количество слайдов: 18

