bdf77630f2447cf9af2ad1db1de581ce.ppt
- Количество слайдов: 33
ANTEPARTUM HAEMORRHAGE
Obstetric Haemorrhage o Ranks as the First cause of maternal mortality accounting for 25 – 50 % of maternal deaths
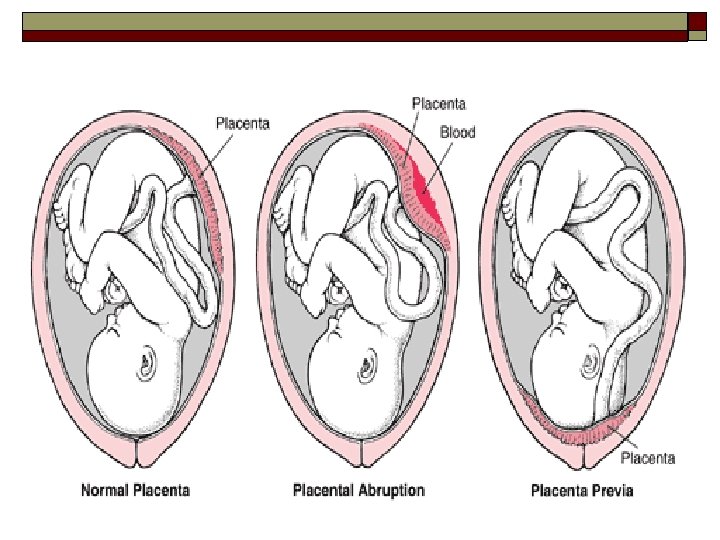
APH: Epediology & Causes o Magnitude: 4% of women may develop APH. o Causes: n placenta previa (1/200) n placental abruption (1/100) n uterine rupture (<1% in scarred uterus) n vasa previa (1/2000 -3000) n Local causes n Unknown origin
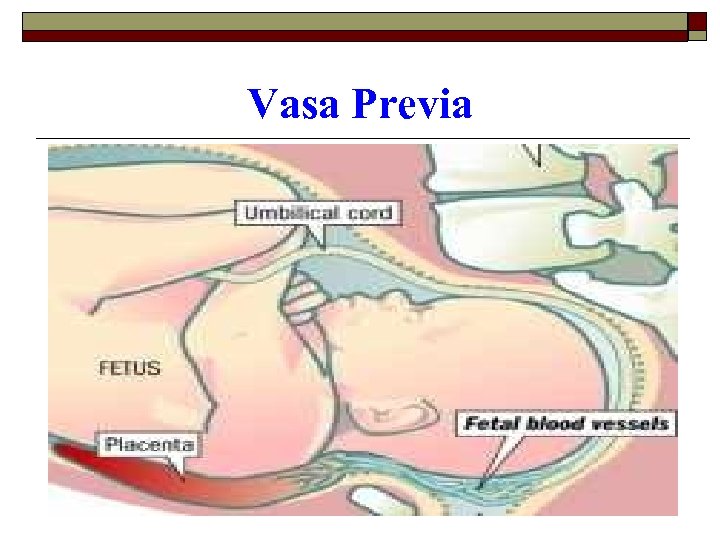
Vasa Previa
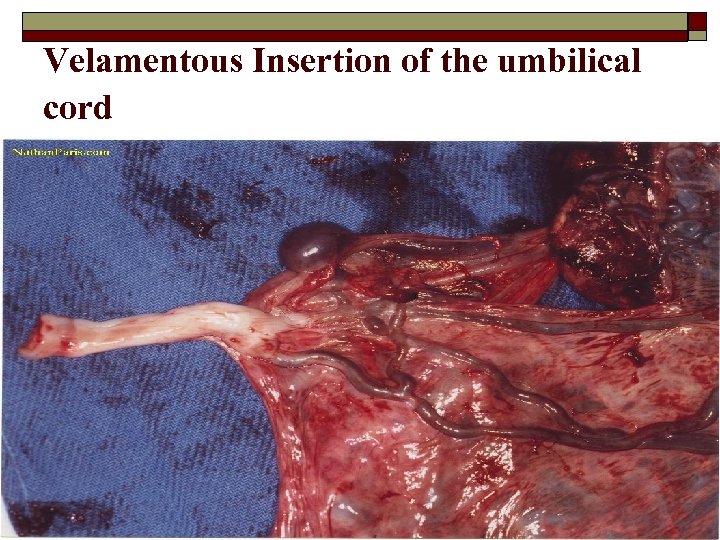
Velamentous Insertion of the umbilical cord
I. ABRUPTIO PLACENTA o Definition: n o Early separation of the normally implanted placenta after 28/40 and before the end of second stage of labour Recurrence: n The risk of recurrent abruption in a subsequent pregnancy is high.
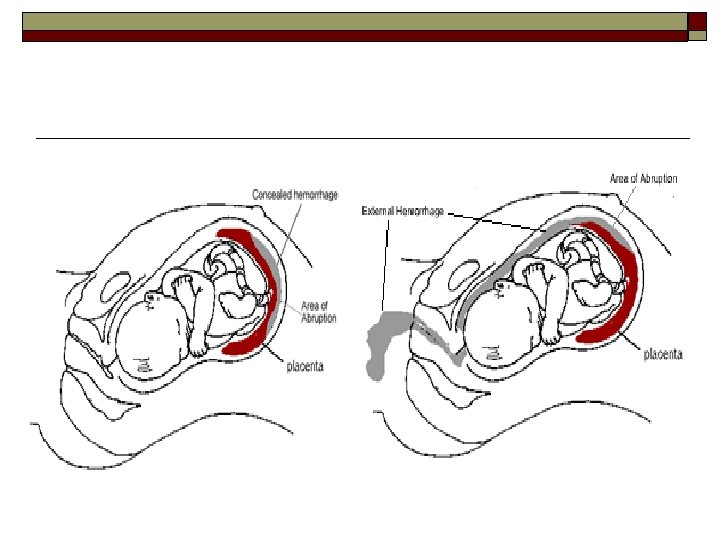
Abruptio placenta: Classifications Are based on 1. Extent of separation: Partial vs complete 2. Location of separation: Marginal Vs central 3. Clinical presentation: Revealed, concealed and mixed 4. Clinical Severity: Mild, Moderate and Severe
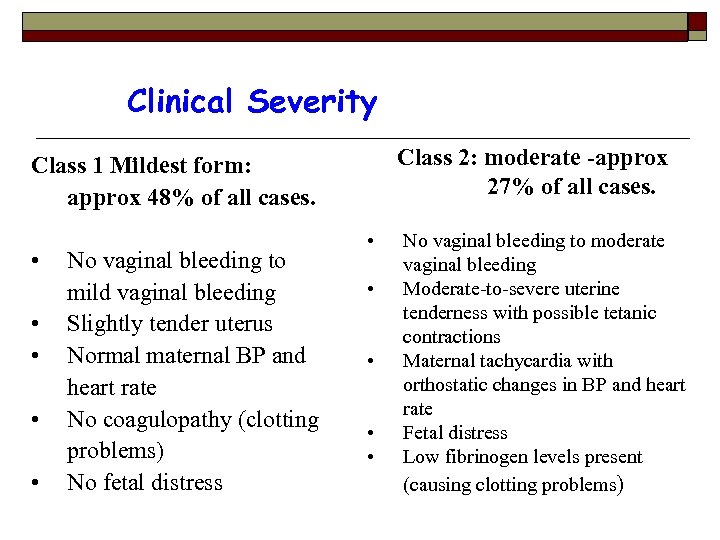
Clinical Severity Class 2: moderate -approx 27% of all cases. Class 1 Mildest form: approx 48% of all cases. • • • No vaginal bleeding to mild vaginal bleeding Slightly tender uterus Normal maternal BP and heart rate No coagulopathy (clotting problems) No fetal distress • • • No vaginal bleeding to moderate vaginal bleeding Moderate-to-severe uterine tenderness with possible tetanic contractions Maternal tachycardia with orthostatic changes in BP and heart rate Fetal distress Low fibrinogen levels present (causing clotting problems)
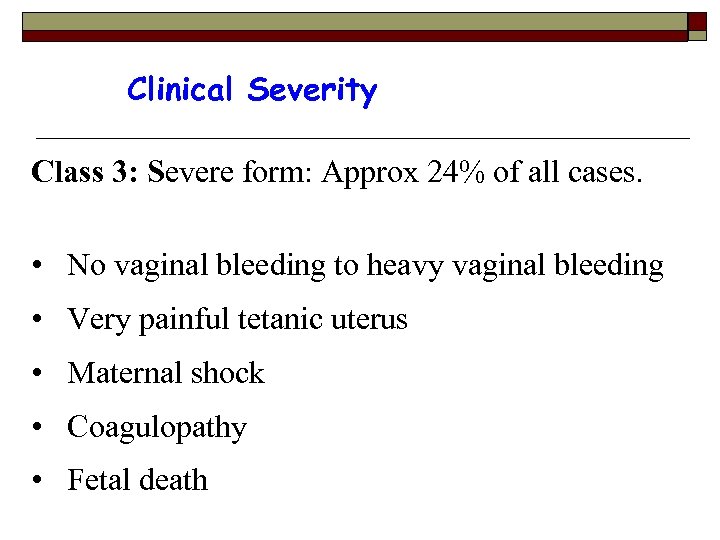
Clinical Severity Class 3: Severe form: Approx 24% of all cases. • No vaginal bleeding to heavy vaginal bleeding • Very painful tetanic uterus • Maternal shock • Coagulopathy • Fetal death
I. Abruptio placenta: Risk factors o Hypertensive Disease o Multiple pregnancy o Trauma o PPROM
I. Abruptio placenta: Risk factors o Anaemia o Polyhydramnios – sudden ↓intrauterine pressure o Short cord o Uterine leiomyoma: esp if located behind the placental implantation site, predispose to abruption
Abruptio Placenta: Features o Pain and tenderness n Initially localized then becomes generalized due to endometrial injury – extravasations of blood o Vaginal bleeding o Maternal distress o Often I. U. F. D
Placental Abruption: Complications o Shock o Acute renal failure n o Cause: ? seriously impaired renal perfusion 2° to ↓CO and intrarenal vasospasm as in preeclampsia DIC n Consumptive coagulopathy 2° to hypofibrinogenemia along with elevated levels of fibrinogen–fibrin degradation products
Placental Abruption: Complications o Fetal distress/demise o PPH o Couvelaire Uterus: n Widespread extravasation of blood into the uterine musculature and beneath the uterine serosa. o Sheehan syndrome o Puerperal sepsis
Placental Abruption: Management o Management depends on: n n n o fetal maturity, degree of severity, viability of the fetus/fetal distress Treatment modalities n n n Expectant management of pregnancy Induction/augmentation of labor Caesarean section
Placental Abruption: General Management 1. Delivery o Resuscitation n FFP, whole blood, IV fluids o Monitor BP o Catherization - monitor urine output
Placental Abruption: General Management o ARM o Induce/Augment labour n Oxytocin infusion or prostaglandin if necessary to induce contractions o Bed site clotting time n Done regularly
Placental Abruption: General Management 2. Caesarean Section o Indications for Caesarean Section n n o salvageable baby, Severe vaginal bleeding, Poor progress, Transverse lie, inadequate pelvis Post delivery -watch out for PPH n Why? o Myometrial myofibrin loose contractility o Failure to clot
PLACENTA PRAEVIA - DEGREES 1. Total placenta praevia The internal cervical os is covered completely by placenta. 2. Partial placenta praevia The internal os is partially covered by placenta.
PLACENTA PRAEVIA - DEGREES 3. Marginal placenta praevia The edge of the placenta is at the margin of the internal os. 4. Low-lying placenta The placenta is implanted in the lower uterine segment such that the placental edge actually does not reach the internal os but is in close proximity to it.
PLACENTA PRAEVIA: Predisposing factors o Multiparity o Advanced maternal age o Prior C/S or other uterine surgery o Prior placenta previa
Placenta Previa: Diagnosis o Painless vaginal bleeding in 2 nd/3 rd trimester o Confirmed by ultrasound o Up to 10% may have simultaneous abruption o Maternal shock is uncommon with 1 st presentation of bleeding
Placenta Previa: Obstetric Management o Vaginal exams are avoided o If possible, delay delivery until fetus is mature. o 34 weeks - buy time for steroids o Prevent contractions with tocolytics -indocid o Mobilize blood donors
Placenta Previa: Obstetric Management o o o i. Resuscitate - IV fluid and blood, Monitor BP and amount of bleeding Delivery Mild non persistent bleeding n GA 34 weeks o o n ii. Buy time for steroids and hospitalization. Prevent contractions with tocolytics Mobilize blood donors Oral haematenics GA 37 weeks = consider Elective CS Persistent bleeding requires immediate delivery whatever the gestation
Placenta Previa: Management o Indications for delivery: n n n Persistent bleeding requires delivery whatever the gestation Active labor Documented fetal lung maturity 37 weeks gestational age. Excessive bleeding Development of another obstetric complication mandating delivery
Placenta Praevia o Elective caesarean if 37 weeks o ? Never cut through the placenta
PLACENTA PRAEVIA o Lower segment may need to be packed o Placenta previa may be assoc. with placenta accreta, increta or percreta → PPH o PPH - 2° to poorly contractile nature of the LS of uterus.
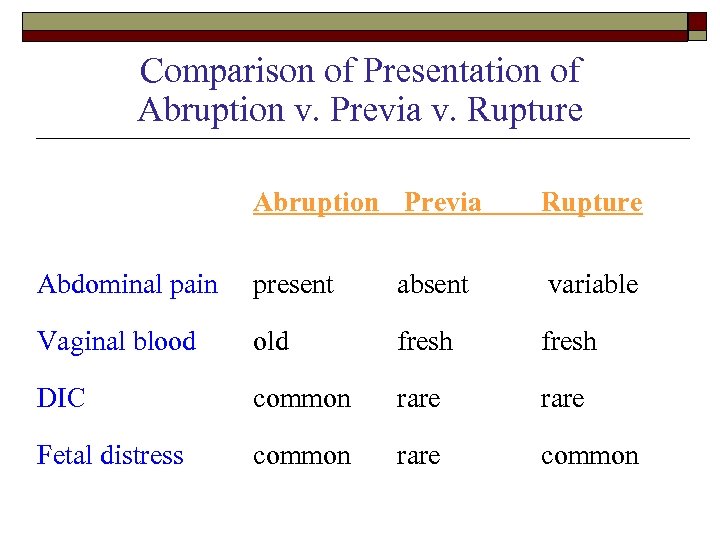
Comparison of Presentation of Abruption v. Previa v. Rupture Abruption Previa Rupture Abdominal pain present absent variable Vaginal blood old fresh DIC common rare Fetal distress common rare common
Vasa Previa o “Umbilical vessels separate in the membranes at a distance from the placental margin and some of the vessels (fetal) cross the internal os and occupy a position ahead of the presenting part of the fetus. ” o ROM may cause fetal exsanguination. o High fetal mortality (50 -75%) o Risk factor: multiple gestation (esp. , triplets).
Vasa Praevia o Diagnosis n n n o o Moderate vag bleeding + fetal distress Vessels may be palpable thru dilated cervix Vessels may be visible on ultrasound Difficult to distinguish clinically from abruption. Treatment n C/S, n Resuscitation of infant (volume)
Local & Unknown Causes of APH o Rupture of uterus o Carcinoma of cervix o Trauma o Cervical polyp o Bilharzia of cervix o Cervicitis
bdf77630f2447cf9af2ad1db1de581ce.ppt