6f3914e2197ae647c12071836aa74269.ppt
- Количество слайдов: 42
 Antenatal Hospital Encounters and Preterm Delivery, MA 2002 -2008 Lizzie Harvey, MPH CDC/CSTE Applied Epidemiology Fellow Massachusetts Department of Public Health June 5, 2012 1
Antenatal Hospital Encounters and Preterm Delivery, MA 2002 -2008 Lizzie Harvey, MPH CDC/CSTE Applied Epidemiology Fellow Massachusetts Department of Public Health June 5, 2012 1
 Background • MA Infants born <32 weeks gestation made up 1. 5% of the birth population but accounted for 63. 8% of infant deaths in 2008 • <32 weeks infants have an infant mortality rate (IMR) of 195 deaths/1, 000 live births – MA IMR is 5. 0 deaths/1, 000 live births
Background • MA Infants born <32 weeks gestation made up 1. 5% of the birth population but accounted for 63. 8% of infant deaths in 2008 • <32 weeks infants have an infant mortality rate (IMR) of 195 deaths/1, 000 live births – MA IMR is 5. 0 deaths/1, 000 live births
 Research Priorities • Prematurity is a research priority – IOM Report: “Preterm Birth: Causes, Consequences, and Prevention” – March of Dimes: • Prematurity Research Initiative • “Healthy Babies are worth the wait” campaign – ASTHO Presidential Challenge
Research Priorities • Prematurity is a research priority – IOM Report: “Preterm Birth: Causes, Consequences, and Prevention” – March of Dimes: • Prematurity Research Initiative • “Healthy Babies are worth the wait” campaign – ASTHO Presidential Challenge
 Conceptual Model for Premature Delivery Neighborhood Factors Family History Family hx of Preterm birth Maternal lbw Physical Abuse during pregnancy Maternal Behaviors Cervical Drug dependency incompetence High unemployment Lower SES Maternal smoking Stress Chronic Disease Black race Anemia Stress Low maternal Weight gain Chronic Hypertension Maternal Obstetric History Placental Low BMI Obesity Abruption Short cervix Prior preterm birth ↑ Maternal age Multiple pregnancies Pre eclampsia Asthma poorly controlled Diabetes INCREASED RISK OF PREMATURE DELIVERY Infections Chorioamnionitis Protective Trichomonasis Progesterone for prior PTD Bacterial vaginosis
Conceptual Model for Premature Delivery Neighborhood Factors Family History Family hx of Preterm birth Maternal lbw Physical Abuse during pregnancy Maternal Behaviors Cervical Drug dependency incompetence High unemployment Lower SES Maternal smoking Stress Chronic Disease Black race Anemia Stress Low maternal Weight gain Chronic Hypertension Maternal Obstetric History Placental Low BMI Obesity Abruption Short cervix Prior preterm birth ↑ Maternal age Multiple pregnancies Pre eclampsia Asthma poorly controlled Diabetes INCREASED RISK OF PREMATURE DELIVERY Infections Chorioamnionitis Protective Trichomonasis Progesterone for prior PTD Bacterial vaginosis
 Research Gaps • <32 week population – Low percentage of births – High IMR • Potential for intervention – Course of pregnancy – Hospital encounters
Research Gaps • <32 week population – Low percentage of births – High IMR • Potential for intervention – Course of pregnancy – Hospital encounters
 Research Question • In deliveries <32 weeks, are there patterns among antenatal hospital encounters and adverse pregnancy outcomes? – Demographic characteristics – Timing of hospital encounters – Number of hospital encounters – Diagnosis codes of hospital encounters
Research Question • In deliveries <32 weeks, are there patterns among antenatal hospital encounters and adverse pregnancy outcomes? – Demographic characteristics – Timing of hospital encounters – Number of hospital encounters – Diagnosis codes of hospital encounters
 Methods • Definitions: – Adverse outcome: Any delivery with a fetal death or infant death occurring before 1 year post-delivery – Hospital Encounters: • Emergency Department (ED) • Observational Stay (OS) • Hospital Discharge (HD)
Methods • Definitions: – Adverse outcome: Any delivery with a fetal death or infant death occurring before 1 year post-delivery – Hospital Encounters: • Emergency Department (ED) • Observational Stay (OS) • Hospital Discharge (HD)
 Methods: PELL Data System Vital and Health Status Data Newborn Hearing Screening Program Participation Data WIC Early Intervention ART Clinic Data Birth Defects Registry CORE Birth Certificate Child and Mother deaths (HD) Birth Mothers Fetal Death (HD) Birth Child 875, 708 births Geocoded birth data Census 2000 Data (and 2010 data) Linked birth-infant deaths Cancer Registry 1998 -2008 Contextual Data Pregnancy-associated deaths PRAMS Health Services Utilization Data w/ diagnosis codes & charges Non-birth Hospital Discharge Other Future Datasets: All Payers Data, School, NICU, Medicaid Databases to be added to system Observational Stays Emergency Department
Methods: PELL Data System Vital and Health Status Data Newborn Hearing Screening Program Participation Data WIC Early Intervention ART Clinic Data Birth Defects Registry CORE Birth Certificate Child and Mother deaths (HD) Birth Mothers Fetal Death (HD) Birth Child 875, 708 births Geocoded birth data Census 2000 Data (and 2010 data) Linked birth-infant deaths Cancer Registry 1998 -2008 Contextual Data Pregnancy-associated deaths PRAMS Health Services Utilization Data w/ diagnosis codes & charges Non-birth Hospital Discharge Other Future Datasets: All Payers Data, School, NICU, Medicaid Databases to be added to system Observational Stays Emergency Department
 Methods: PELL Data System Vital and Health Status Data CORE Birth Certificate Linked birth-infant deaths Fetal Death 2002 -2008 Health Services Utilization Data w/ diagnosis codes & charges Non-birth Hospital Discharge Observational Stays Emergency Department
Methods: PELL Data System Vital and Health Status Data CORE Birth Certificate Linked birth-infant deaths Fetal Death 2002 -2008 Health Services Utilization Data w/ diagnosis codes & charges Non-birth Hospital Discharge Observational Stays Emergency Department
 Methods • Exclusion criteria: – ≥ 32 weeks gestation delivery – Missing gestational age – HD, OS, or ED admission date outside conception and delivery date – Delivery hospitalization records • Analysis on SAS 9. 2: – Frequency distributions – Logistic regressions
Methods • Exclusion criteria: – ≥ 32 weeks gestation delivery – Missing gestational age – HD, OS, or ED admission date outside conception and delivery date – Delivery hospitalization records • Analysis on SAS 9. 2: – Frequency distributions – Logistic regressions
 Results—Data Merging 567, 323 Births, FD, ID Sorted and merged by child unique identifier 554, 603 ≥ 32 weeks 1, 494 missing GA 11, 226 <32 wks Code by adverse delivery Outcome and delete multiples 9, 330 DELIVERIES Sorted and merged by mother unique delivery identifier
Results—Data Merging 567, 323 Births, FD, ID Sorted and merged by child unique identifier 554, 603 ≥ 32 weeks 1, 494 missing GA 11, 226 <32 wks Code by adverse delivery Outcome and delete multiples 9, 330 DELIVERIES Sorted and merged by mother unique delivery identifier
 Results—Data Merging 9, 330 DELIVERIES 252, 853 ED 9, 330 DELIVERIES 118, 482 OS 9, 330 DELIVERIES 32, 360 HD Deleted non-prenatal hospitalization encounters by GA, delivery date and hospitalization admission date 10, 423 DEL+ED 9, 788 OS 9, 661 HD Merged back to delivery records by unique identifier to capture non-encounters 7, 013 NON-ENC. 2, 317 DEL. w/ ED 4, 013 ED ENC. 7, 788 NON-ENC. 1, 542 DEL. w/ OS 2, 048 OS ENC. 7, 695 NON ENC. 1, 635 DEL. w/ HD 2, 064 HD ENC. Final datasets: 1) 9, 330 unique deliveries 2) 11, 744 duplicate deliveries with every prenatal hospitalization
Results—Data Merging 9, 330 DELIVERIES 252, 853 ED 9, 330 DELIVERIES 118, 482 OS 9, 330 DELIVERIES 32, 360 HD Deleted non-prenatal hospitalization encounters by GA, delivery date and hospitalization admission date 10, 423 DEL+ED 9, 788 OS 9, 661 HD Merged back to delivery records by unique identifier to capture non-encounters 7, 013 NON-ENC. 2, 317 DEL. w/ ED 4, 013 ED ENC. 7, 788 NON-ENC. 1, 542 DEL. w/ OS 2, 048 OS ENC. 7, 695 NON ENC. 1, 635 DEL. w/ HD 2, 064 HD ENC. Final datasets: 1) 9, 330 unique deliveries 2) 11, 744 duplicate deliveries with every prenatal hospitalization
 Demographics by Delivery Characteristic Race Hispanic Non-Hispanic White Non-Hispanic Black API AI/Other Maternal Age <20 years 20 -34 years 35+ years Nativity US born PR Foreign born % 15. 1 60. 0 17. 7 5. 7 3. 4 9. 0 65. 7 25. 3 68. 9 3. 5 27. 6 N (9, 330) Characteristic % N Gestational Age ≤ 20 weeks 21 -24 weeks 25 -28 weeks 29 -31 weeks 6. 1 21. 6 28. 7 43. 6 568 2015 2677 4070 835 6124 2358 Delivery Method Vaginal VBAC Primary C-section Repeat C-section 50. 9 2. 6 37. 0 9. 1 4746 240 3456 848 6230 6550 2492 Plurality Singletons Twins Triplets+ 80. 9 17. 1 2. 0 7552 1596 182 1393 5351 1636 527 299 Maternal Education
Demographics by Delivery Characteristic Race Hispanic Non-Hispanic White Non-Hispanic Black API AI/Other Maternal Age <20 years 20 -34 years 35+ years Nativity US born PR Foreign born % 15. 1 60. 0 17. 7 5. 7 3. 4 9. 0 65. 7 25. 3 68. 9 3. 5 27. 6 N (9, 330) Characteristic % N Gestational Age ≤ 20 weeks 21 -24 weeks 25 -28 weeks 29 -31 weeks 6. 1 21. 6 28. 7 43. 6 568 2015 2677 4070 835 6124 2358 Delivery Method Vaginal VBAC Primary C-section Repeat C-section 50. 9 2. 6 37. 0 9. 1 4746 240 3456 848 6230 6550 2492 Plurality Singletons Twins Triplets+ 80. 9 17. 1 2. 0 7552 1596 182 1393 5351 1636 527 299 Maternal Education
 Initial Results • Exposure: Antenatal hospitalization – 44. 0% of deliveries <32 weeks had at least one non-delivery antenatal hospital encounter • Outcome: Adverse pregnancy outcome – 31. 2% of deliveries <32 weeks with at least one non-delivery antenatal hospitalizations had an adverse outcome – 34. 4% of all deliveries <32 weeks had an adverse outcome
Initial Results • Exposure: Antenatal hospitalization – 44. 0% of deliveries <32 weeks had at least one non-delivery antenatal hospital encounter • Outcome: Adverse pregnancy outcome – 31. 2% of deliveries <32 weeks with at least one non-delivery antenatal hospitalizations had an adverse outcome – 34. 4% of all deliveries <32 weeks had an adverse outcome
 Results: Demographic Characteristics, Hospital Encounters and Adverse Outcomes
Results: Demographic Characteristics, Hospital Encounters and Adverse Outcomes
 Univariate Analysis
Univariate Analysis
 Demographics by Any Hospitalization Characteristic Race Hispanic Non-Hispanic White Non-Hispanic Black API AI/Other Maternal Age <20 years 20 -34 years 35+ years Nativity US born PR Foreign born % Hosp 50. 3 42. 6 48. 2 35. 5 37. 8 49. 8 44. 6 40. 5 45. 9 56. 9 38. 6 % Non-Hosp Characteristic % Hosp % Non-Hosp Gestational Age ≤ 20 weeks 21 -24 weeks 25 -28 weeks 29 -31 weeks 36. 3 42. 0 44. 1 45. 9 63. 7 58. 0 55. 9 54. 1 50. 2 55. 4 59. 5 Delivery Method Vaginal VBAC Primary C-section Repeat C-section 41. 0 45. 0 46. 9 49. 3 59. 0 55. 0 53. 1 50. 7 54. 1 43. 1 61. 4 Plurality Singletons Twins Triplets+ 42. 9 47. 9 52. 7 57. 1 52. 1 47. 3 Payer Private Public Self-care Free care 41. 7 52. 0 31. 3 42. 6 58. 3 48. 0 68. 8 57. 4 49. 8 57. 4 51. 8 64. 5 62. 2 Maternal Education
Demographics by Any Hospitalization Characteristic Race Hispanic Non-Hispanic White Non-Hispanic Black API AI/Other Maternal Age <20 years 20 -34 years 35+ years Nativity US born PR Foreign born % Hosp 50. 3 42. 6 48. 2 35. 5 37. 8 49. 8 44. 6 40. 5 45. 9 56. 9 38. 6 % Non-Hosp Characteristic % Hosp % Non-Hosp Gestational Age ≤ 20 weeks 21 -24 weeks 25 -28 weeks 29 -31 weeks 36. 3 42. 0 44. 1 45. 9 63. 7 58. 0 55. 9 54. 1 50. 2 55. 4 59. 5 Delivery Method Vaginal VBAC Primary C-section Repeat C-section 41. 0 45. 0 46. 9 49. 3 59. 0 55. 0 53. 1 50. 7 54. 1 43. 1 61. 4 Plurality Singletons Twins Triplets+ 42. 9 47. 9 52. 7 57. 1 52. 1 47. 3 Payer Private Public Self-care Free care 41. 7 52. 0 31. 3 42. 6 58. 3 48. 0 68. 8 57. 4 49. 8 57. 4 51. 8 64. 5 62. 2 Maternal Education
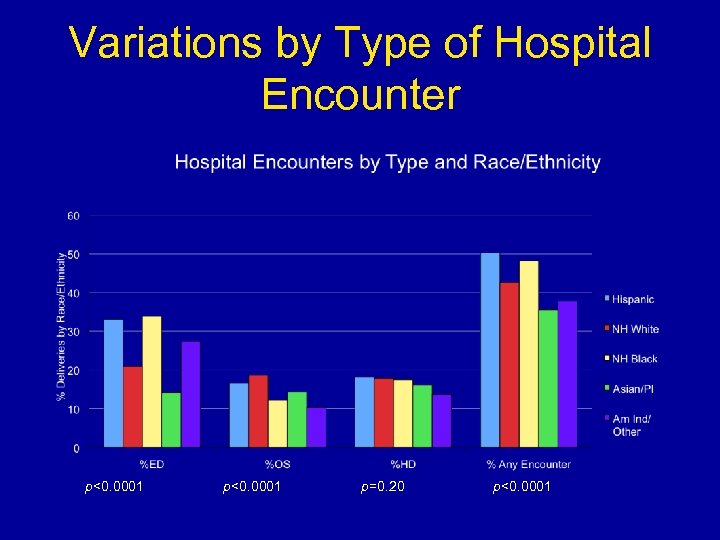 Variations by Type of Hospital Encounter p<0. 0001 p=0. 20 p<0. 0001
Variations by Type of Hospital Encounter p<0. 0001 p=0. 20 p<0. 0001
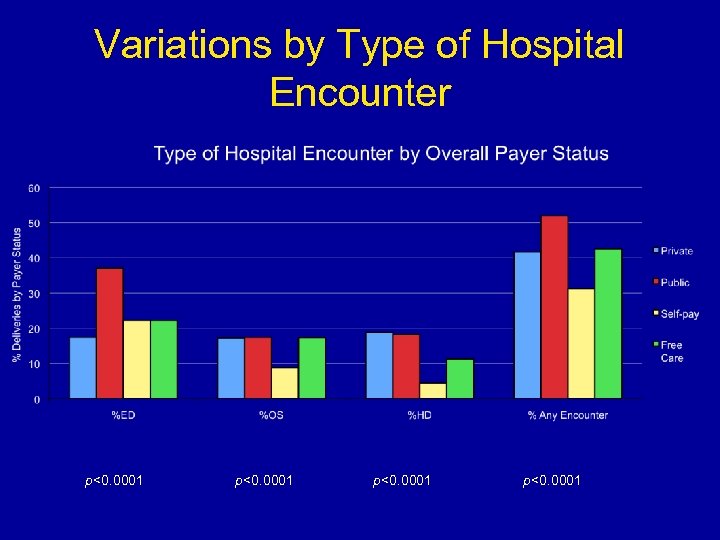 Variations by Type of Hospital Encounter p<0. 0001
Variations by Type of Hospital Encounter p<0. 0001
 Univariate Analysis
Univariate Analysis
 Demographics by Adverse Outcome Characteristic Race Hispanic Non-Hispanic White Non-Hispanic Black API AI/Other Maternal Age <20 years 20 -34 years 35+ years Nativity US born PR Foreign born % Adverse 35. 8 31. 4 38. 3 32. 4 41. 5 39. 2 34. 4 32. 5 30. 7 22. 5 38. 5 % Non-Adverse Characteristic % Adverse % Non-Adverse Gestational Age ≤ 20 weeks 21 -24 weeks 25 -28 weeks 29 -31 weeks 92. 1 79. 8 25. 7 9. 7 7. 9 20. 2 74. 3 90. 3 60. 8 65. 6 67. 5 Delivery Method Vaginal VBAC Primary C-section Repeat C-section 51. 9 53. 8 13. 7 48. 1 46. 3 86. 2 86. 3 69. 3 77. 5 61. 5 Plurality Singletons Twins Triplets+ 35. 1 32. 4 24. 6 64. 9 67. 6 75. 4 Payer Private Public Self-care Free care 34. 7 34. 9 61. 6 40. 0 65. 3 65. 1 38. 4 60. 0 64. 2 68. 6 64. 7 67. 9 58. 5 Maternal Education
Demographics by Adverse Outcome Characteristic Race Hispanic Non-Hispanic White Non-Hispanic Black API AI/Other Maternal Age <20 years 20 -34 years 35+ years Nativity US born PR Foreign born % Adverse 35. 8 31. 4 38. 3 32. 4 41. 5 39. 2 34. 4 32. 5 30. 7 22. 5 38. 5 % Non-Adverse Characteristic % Adverse % Non-Adverse Gestational Age ≤ 20 weeks 21 -24 weeks 25 -28 weeks 29 -31 weeks 92. 1 79. 8 25. 7 9. 7 7. 9 20. 2 74. 3 90. 3 60. 8 65. 6 67. 5 Delivery Method Vaginal VBAC Primary C-section Repeat C-section 51. 9 53. 8 13. 7 48. 1 46. 3 86. 2 86. 3 69. 3 77. 5 61. 5 Plurality Singletons Twins Triplets+ 35. 1 32. 4 24. 6 64. 9 67. 6 75. 4 Payer Private Public Self-care Free care 34. 7 34. 9 61. 6 40. 0 65. 3 65. 1 38. 4 60. 0 64. 2 68. 6 64. 7 67. 9 58. 5 Maternal Education
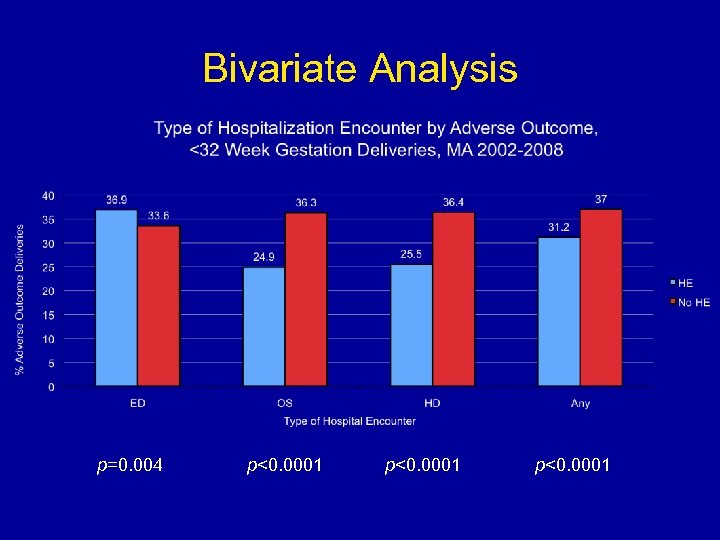 Bivariate Analysis p=0. 004 p<0. 0001
Bivariate Analysis p=0. 004 p<0. 0001
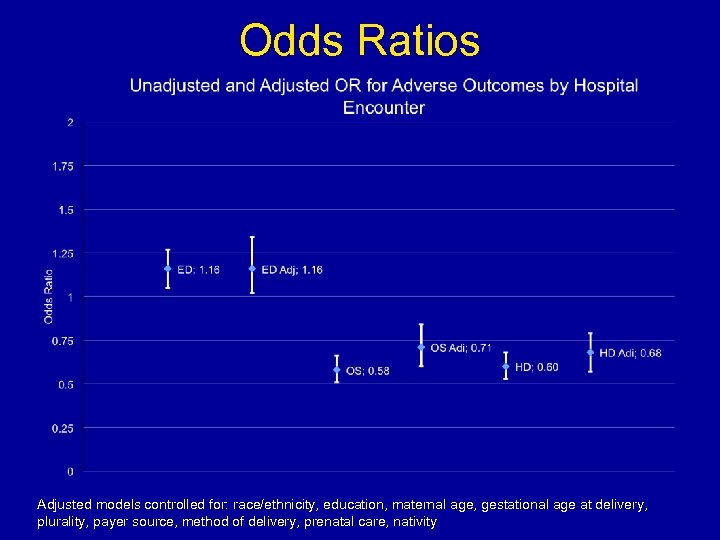 Odds Ratios Adjusted models controlled for: race/ethnicity, education, maternal age, gestational age at delivery, plurality, payer source, method of delivery, prenatal care, nativity
Odds Ratios Adjusted models controlled for: race/ethnicity, education, maternal age, gestational age at delivery, plurality, payer source, method of delivery, prenatal care, nativity
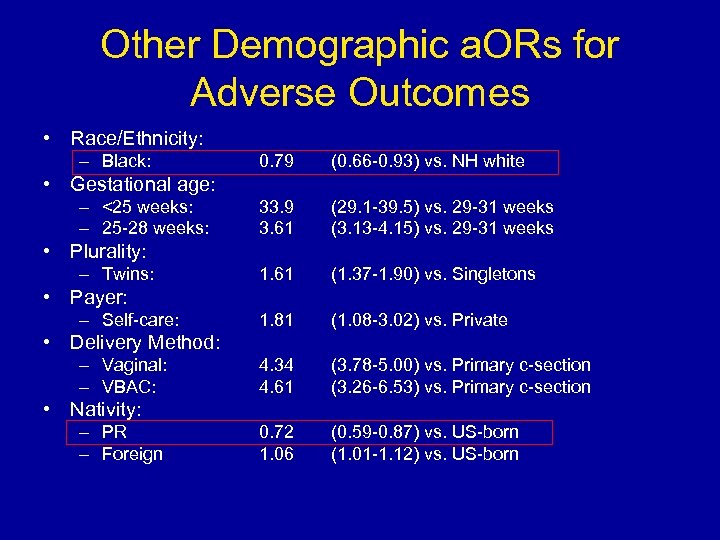 Other Demographic a. ORs for Adverse Outcomes • Race/Ethnicity: – Black: 0. 79 (0. 66 -0. 93) vs. NH white 33. 9 3. 61 (29. 1 -39. 5) vs. 29 -31 weeks (3. 13 -4. 15) vs. 29 -31 weeks 1. 61 (1. 37 -1. 90) vs. Singletons 1. 81 (1. 08 -3. 02) vs. Private 4. 34 4. 61 (3. 78 -5. 00) vs. Primary c-section (3. 26 -6. 53) vs. Primary c-section 0. 72 1. 06 (0. 59 -0. 87) vs. US-born (1. 01 -1. 12) vs. US-born • Gestational age: – <25 weeks: – 25 -28 weeks: • Plurality: – Twins: • Payer: – Self-care: • Delivery Method: – Vaginal: – VBAC: • Nativity: – PR – Foreign
Other Demographic a. ORs for Adverse Outcomes • Race/Ethnicity: – Black: 0. 79 (0. 66 -0. 93) vs. NH white 33. 9 3. 61 (29. 1 -39. 5) vs. 29 -31 weeks (3. 13 -4. 15) vs. 29 -31 weeks 1. 61 (1. 37 -1. 90) vs. Singletons 1. 81 (1. 08 -3. 02) vs. Private 4. 34 4. 61 (3. 78 -5. 00) vs. Primary c-section (3. 26 -6. 53) vs. Primary c-section 0. 72 1. 06 (0. 59 -0. 87) vs. US-born (1. 01 -1. 12) vs. US-born • Gestational age: – <25 weeks: – 25 -28 weeks: • Plurality: – Twins: • Payer: – Self-care: • Delivery Method: – Vaginal: – VBAC: • Nativity: – PR – Foreign
 Results: Timing of Hospital Encounters and Adverse Outcomes
Results: Timing of Hospital Encounters and Adverse Outcomes
 Variation in Timing of Encounters
Variation in Timing of Encounters
 Timing Indicators of Adverse Outcomes
Timing Indicators of Adverse Outcomes
 Results: Number of Hospital Encounters and Adverse Outcomes
Results: Number of Hospital Encounters and Adverse Outcomes
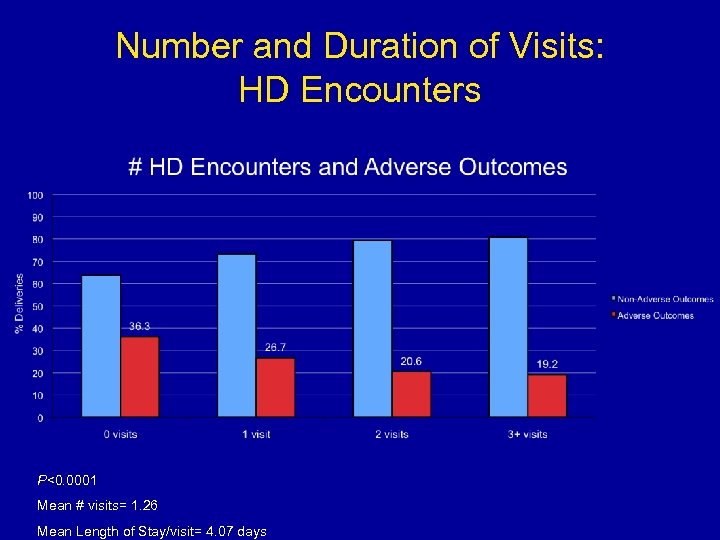 Number and Duration of Visits: HD Encounters P<0. 0001 Mean # visits= 1. 26 Mean Length of Stay/visit= 4. 07 days
Number and Duration of Visits: HD Encounters P<0. 0001 Mean # visits= 1. 26 Mean Length of Stay/visit= 4. 07 days
 Number and Duration of Visits: OS Encounters P<0. 0001 Mean # visits= 1. 33 Mean Length of Stay/visit= 0. 39 days
Number and Duration of Visits: OS Encounters P<0. 0001 Mean # visits= 1. 33 Mean Length of Stay/visit= 0. 39 days
 Number and Duration of Visits: ED Encounters P=0. 0095 Mean # visits= 1. 73 Mean Length of Stay/visit= 3. 40 hours
Number and Duration of Visits: ED Encounters P=0. 0095 Mean # visits= 1. 73 Mean Length of Stay/visit= 3. 40 hours
 No Increased Odds of Adverse Outcomes with Increased ED Encounters
No Increased Odds of Adverse Outcomes with Increased ED Encounters
 Results: Diagnosis Codes and Adverse Outcomes
Results: Diagnosis Codes and Adverse Outcomes
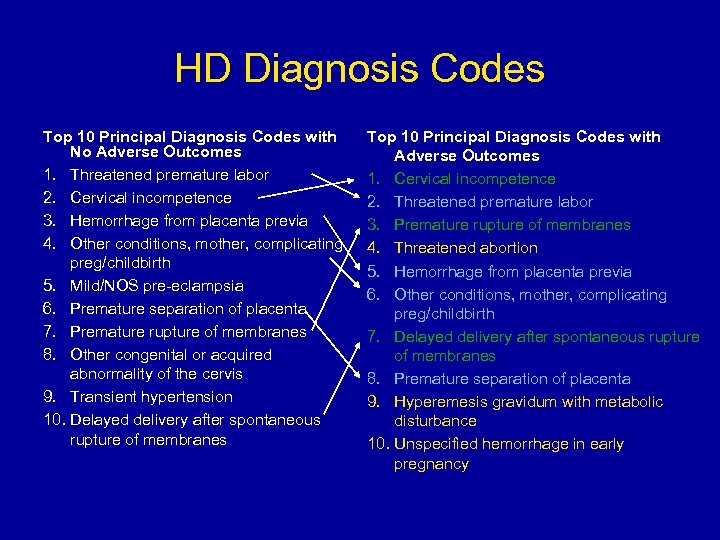 HD Diagnosis Codes Top 10 Principal Diagnosis Codes with No Adverse Outcomes 1. Threatened premature labor 2. Cervical incompetence 3. Hemorrhage from placenta previa 4. Other conditions, mother, complicating preg/childbirth 5. Mild/NOS pre-eclampsia 6. Premature separation of placenta 7. Premature rupture of membranes 8. Other congenital or acquired abnormality of the cervis 9. Transient hypertension 10. Delayed delivery after spontaneous rupture of membranes Top 10 Principal Diagnosis Codes with Adverse Outcomes 1. Cervical incompetence 2. Threatened premature labor 3. Premature rupture of membranes 4. Threatened abortion 5. Hemorrhage from placenta previa 6. Other conditions, mother, complicating preg/childbirth 7. Delayed delivery after spontaneous rupture of membranes 8. Premature separation of placenta 9. Hyperemesis gravidum with metabolic disturbance 10. Unspecified hemorrhage in early pregnancy
HD Diagnosis Codes Top 10 Principal Diagnosis Codes with No Adverse Outcomes 1. Threatened premature labor 2. Cervical incompetence 3. Hemorrhage from placenta previa 4. Other conditions, mother, complicating preg/childbirth 5. Mild/NOS pre-eclampsia 6. Premature separation of placenta 7. Premature rupture of membranes 8. Other congenital or acquired abnormality of the cervis 9. Transient hypertension 10. Delayed delivery after spontaneous rupture of membranes Top 10 Principal Diagnosis Codes with Adverse Outcomes 1. Cervical incompetence 2. Threatened premature labor 3. Premature rupture of membranes 4. Threatened abortion 5. Hemorrhage from placenta previa 6. Other conditions, mother, complicating preg/childbirth 7. Delayed delivery after spontaneous rupture of membranes 8. Premature separation of placenta 9. Hyperemesis gravidum with metabolic disturbance 10. Unspecified hemorrhage in early pregnancy
 OS Diagnosis Codes Top 10 Principal Diagnosis Codes with No Adverse Outcomes 1. Threatened premature labor 2. Other conditions, mother, complicating preg/childbirth 3. Premature rupture of membranes 4. Unspecified antepartum hemorrhage 5. Cervical incompetence 6. Mild/NOS pre-eclampsia 7. Hemorrhage from placenta previa 8. Transient hypertension 9. Other threatened labor 10. Severe pre-eclampsia Top 10 Principal Diagnosis Codes with Adverse Outcomes 1. Threatened premature labor 2. Cervical incompetence 3. Other conditions, mother, complicating preg/childbirth 4. Premature rupture of membranes 5. Unspecified hemorrhage in early pregnancy 6. Threatened abortion 7. Unspecified antepartum hemorrhage 8. Twin pregnancy 9. Intrauterine death 10. Mild/NOS pre-eclampsia
OS Diagnosis Codes Top 10 Principal Diagnosis Codes with No Adverse Outcomes 1. Threatened premature labor 2. Other conditions, mother, complicating preg/childbirth 3. Premature rupture of membranes 4. Unspecified antepartum hemorrhage 5. Cervical incompetence 6. Mild/NOS pre-eclampsia 7. Hemorrhage from placenta previa 8. Transient hypertension 9. Other threatened labor 10. Severe pre-eclampsia Top 10 Principal Diagnosis Codes with Adverse Outcomes 1. Threatened premature labor 2. Cervical incompetence 3. Other conditions, mother, complicating preg/childbirth 4. Premature rupture of membranes 5. Unspecified hemorrhage in early pregnancy 6. Threatened abortion 7. Unspecified antepartum hemorrhage 8. Twin pregnancy 9. Intrauterine death 10. Mild/NOS pre-eclampsia
 ED Diagnosis Codes Top 10 Principal Diagnosis Codes with No Adverse Outcomes 1. Other conditions, mother, complicating preg/childbirth 2. Threatened abortion 3. Unspecified hemorrhage in early pregnancy 4. Mild hyperemesis gravidarum 5. Other specified complications of pregnancy 6. Abdominal pain; unspecified site 7. Infections of genitourinary tract in pregnancy 8. Headache, Facial pain, Pain in head NOS 9. Unspecified antepartum hemorrhage 10. Asthma (bronchial) (allergic NOS) Top 10 Principal Diagnosis Codes with Adverse Outcomes 1. Other conditions, mother, complicating preg/childbirth 2. Threatened abortion 3. Unspecified hemorrhage in early pregnancy 4. Mild hyperemesis gravidarum 5. Other specified complications of pregnancy 6. Infections of genitourinary tract in pregnancy 7. Unspecified antepartum hemorrhage 8. Abdominal pain 9. Headache, Facial pain, Pain in head NOS, 10. Sprains/strains; neck, Anterior longitudinal (ligament), cervical, Atlanto-axial (joints), Atlanto-occipital (joints), Whiplash injury
ED Diagnosis Codes Top 10 Principal Diagnosis Codes with No Adverse Outcomes 1. Other conditions, mother, complicating preg/childbirth 2. Threatened abortion 3. Unspecified hemorrhage in early pregnancy 4. Mild hyperemesis gravidarum 5. Other specified complications of pregnancy 6. Abdominal pain; unspecified site 7. Infections of genitourinary tract in pregnancy 8. Headache, Facial pain, Pain in head NOS 9. Unspecified antepartum hemorrhage 10. Asthma (bronchial) (allergic NOS) Top 10 Principal Diagnosis Codes with Adverse Outcomes 1. Other conditions, mother, complicating preg/childbirth 2. Threatened abortion 3. Unspecified hemorrhage in early pregnancy 4. Mild hyperemesis gravidarum 5. Other specified complications of pregnancy 6. Infections of genitourinary tract in pregnancy 7. Unspecified antepartum hemorrhage 8. Abdominal pain 9. Headache, Facial pain, Pain in head NOS, 10. Sprains/strains; neck, Anterior longitudinal (ligament), cervical, Atlanto-axial (joints), Atlanto-occipital (joints), Whiplash injury
 Conclusions • 44% of all <32 wk deliveries had ≥ 1 hospital encounter – Of these deliveries, almost 1/3 will have an adverse outcome • Type of hospital encounter matters: – Deliveries with ≥ 1 ED encounter have a 16% greater risk of adverse outcomes than those with no encounter – OS and HD encounters are protective against adverse outcomes, with 29% and 32% decreased risk, respectively
Conclusions • 44% of all <32 wk deliveries had ≥ 1 hospital encounter – Of these deliveries, almost 1/3 will have an adverse outcome • Type of hospital encounter matters: – Deliveries with ≥ 1 ED encounter have a 16% greater risk of adverse outcomes than those with no encounter – OS and HD encounters are protective against adverse outcomes, with 29% and 32% decreased risk, respectively
 Conclusions • Demographic: – Gestational age is the driver of poor outcomes – Black mothers and PR born mothers have decreased odds of adverse outcomes – Twins, Self-care payment, and vaginal delivery have increased odds of adverse outcomes • Timing: – Deliveries with adverse outcomes will present sooner in pregnancy with each type of hospital encounter than those without – Women present sooner in the ED than OS or HD • Number: – HD and OS both have decreased odds of adverse outcomes with each additional visit – No increased risk of adverse outcomes with each additional ED visit • Diagnosis: – HD: Cervical incompetence, threatened premature labor, PROM – OS: Cervical incompetence, hemorrhage, threatened abortion – ED: Infections, hemorrhage, sprains/strains
Conclusions • Demographic: – Gestational age is the driver of poor outcomes – Black mothers and PR born mothers have decreased odds of adverse outcomes – Twins, Self-care payment, and vaginal delivery have increased odds of adverse outcomes • Timing: – Deliveries with adverse outcomes will present sooner in pregnancy with each type of hospital encounter than those without – Women present sooner in the ED than OS or HD • Number: – HD and OS both have decreased odds of adverse outcomes with each additional visit – No increased risk of adverse outcomes with each additional ED visit • Diagnosis: – HD: Cervical incompetence, threatened premature labor, PROM – OS: Cervical incompetence, hemorrhage, threatened abortion – ED: Infections, hemorrhage, sprains/strains
 Next Steps • Expand study population • Further refinement of diagnosis coding • Consult with clinicians – Share data by type of hospitalization – Feedback on potential interventions • Exploration of costs associated with hospital utilization
Next Steps • Expand study population • Further refinement of diagnosis coding • Consult with clinicians – Share data by type of hospitalization – Feedback on potential interventions • Exploration of costs associated with hospital utilization
 Acknowledgements • • • Hafsatou Diop, MD, MPH Xiaohui Cui, Ph. D Milton Kotelchuck, Ph. D, MPH Maria Vu, MPH Emily Lu, MPH Karin Downs, RN, MPH • CDC/CSTE Fellowship
Acknowledgements • • • Hafsatou Diop, MD, MPH Xiaohui Cui, Ph. D Milton Kotelchuck, Ph. D, MPH Maria Vu, MPH Emily Lu, MPH Karin Downs, RN, MPH • CDC/CSTE Fellowship
 References • CDC Premature Birth: – http: //www. cdc. gov/Features/Premature. Birth/ • IOM Report: – National Research Council. Preterm Birth: Causes, Consequences, and Prevention. Washington, DC: The National Academies Press, 2007. • PELL Data System: – https: //sph. bu. edu/index. php/Maternal-a-Child-Health/Pregnancy-to-Early-Life. Longitudinal-Linkage-b. PELLb/menu-id-452. html • MA Death Statistics: – http: //www. mass. gov/eohhs/docs/dph/research-epi/death-report-08. pdf • March of Dimes: – http: //www. marchofdimes. com • ASTHO Presidential Challenge: – http: //www. astho. org/t/pres_chal. aspx? id=6484
References • CDC Premature Birth: – http: //www. cdc. gov/Features/Premature. Birth/ • IOM Report: – National Research Council. Preterm Birth: Causes, Consequences, and Prevention. Washington, DC: The National Academies Press, 2007. • PELL Data System: – https: //sph. bu. edu/index. php/Maternal-a-Child-Health/Pregnancy-to-Early-Life. Longitudinal-Linkage-b. PELLb/menu-id-452. html • MA Death Statistics: – http: //www. mass. gov/eohhs/docs/dph/research-epi/death-report-08. pdf • March of Dimes: – http: //www. marchofdimes. com • ASTHO Presidential Challenge: – http: //www. astho. org/t/pres_chal. aspx? id=6484
 Thank you Contact Information: Lizzie. Harvey@gmail. com
Thank you Contact Information: Lizzie. Harvey@gmail. com


