cbb5b64328df4cdff0e3020149df9ef2.ppt
- Количество слайдов: 51
 Aneuploidy screening in pregnancy - modern approaches Prof. Lina Basel Director, The Raphael Recanati Genetics Institute, Beilinson hospital, Rabin Medical Center Schneider Children’s Medical Center of Israel Tel Aviv University
Aneuploidy screening in pregnancy - modern approaches Prof. Lina Basel Director, The Raphael Recanati Genetics Institute, Beilinson hospital, Rabin Medical Center Schneider Children’s Medical Center of Israel Tel Aviv University
 Rabin Medical Center/Schneider Children’s Medical Center of Israel Pediatric genetics Adult genetics Prenatal counseling Oncogenetics Genetic screening Molecular lab Cytogenetic lab including chromosomal microarray § PGD § § § §
Rabin Medical Center/Schneider Children’s Medical Center of Israel Pediatric genetics Adult genetics Prenatal counseling Oncogenetics Genetic screening Molecular lab Cytogenetic lab including chromosomal microarray § PGD § § § §
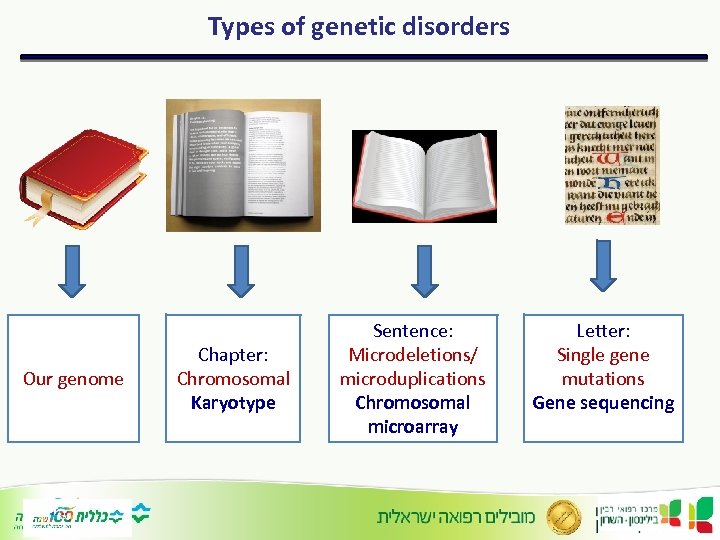 Types of genetic disorders Our genome Chapter: Chromosomal Karyotype Sentence: Microdeletions/ microduplications Chromosomal microarray Letter: Single gene mutations Gene sequencing
Types of genetic disorders Our genome Chapter: Chromosomal Karyotype Sentence: Microdeletions/ microduplications Chromosomal microarray Letter: Single gene mutations Gene sequencing
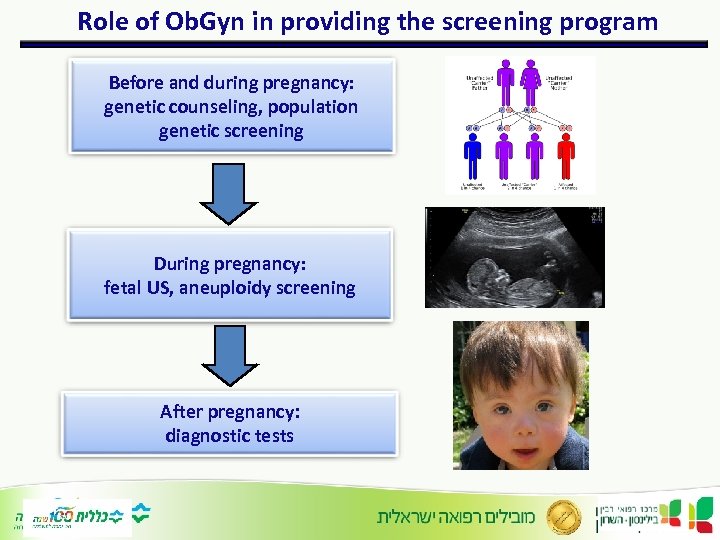 Role of Ob. Gyn in providing the screening program Before and during pregnancy: genetic counseling, population genetic screening During pregnancy: fetal US, aneuploidy screening After pregnancy: diagnostic tests
Role of Ob. Gyn in providing the screening program Before and during pregnancy: genetic counseling, population genetic screening During pregnancy: fetal US, aneuploidy screening After pregnancy: diagnostic tests
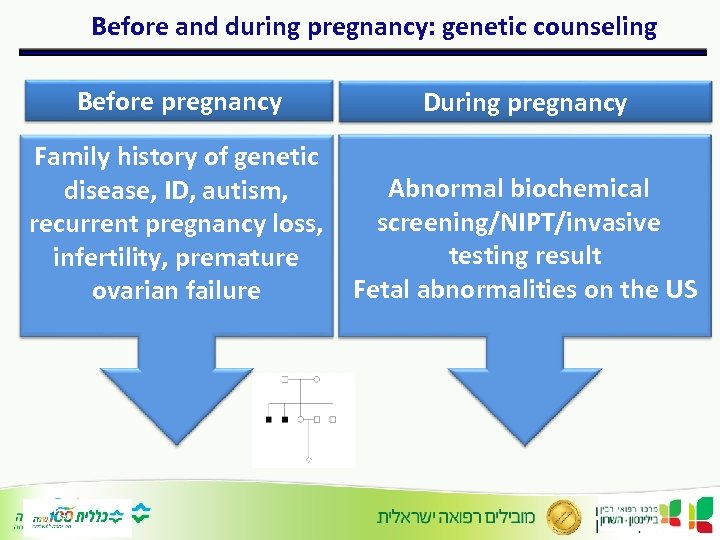 Before and during pregnancy: genetic counseling Before pregnancy During pregnancy Family history of genetic disease, ID, autism, recurrent pregnancy loss, infertility, premature ovarian failure Abnormal biochemical screening/NIPT/invasive testing result Fetal abnormalities on the US
Before and during pregnancy: genetic counseling Before pregnancy During pregnancy Family history of genetic disease, ID, autism, recurrent pregnancy loss, infertility, premature ovarian failure Abnormal biochemical screening/NIPT/invasive testing result Fetal abnormalities on the US
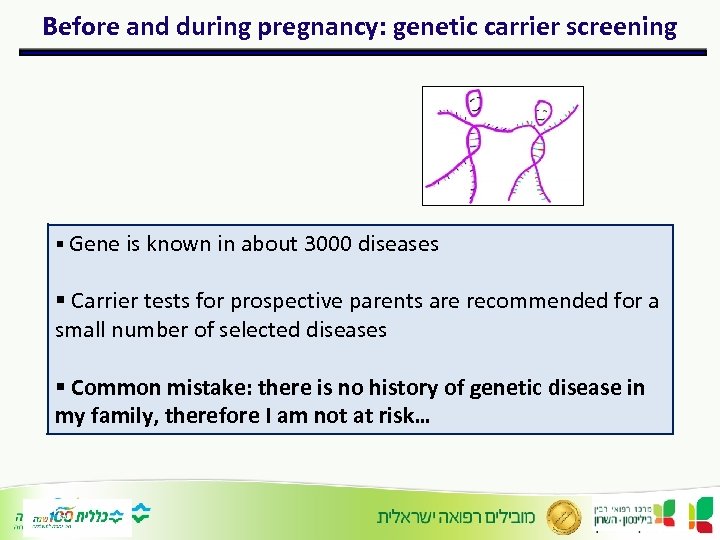 Before and during pregnancy: genetic carrier screening § Gene is known in about 3000 diseases § Carrier tests for prospective parents are recommended for a small number of selected diseases § Common mistake: there is no history of genetic disease in my family, therefore I am not at risk…
Before and during pregnancy: genetic carrier screening § Gene is known in about 3000 diseases § Carrier tests for prospective parents are recommended for a small number of selected diseases § Common mistake: there is no history of genetic disease in my family, therefore I am not at risk…
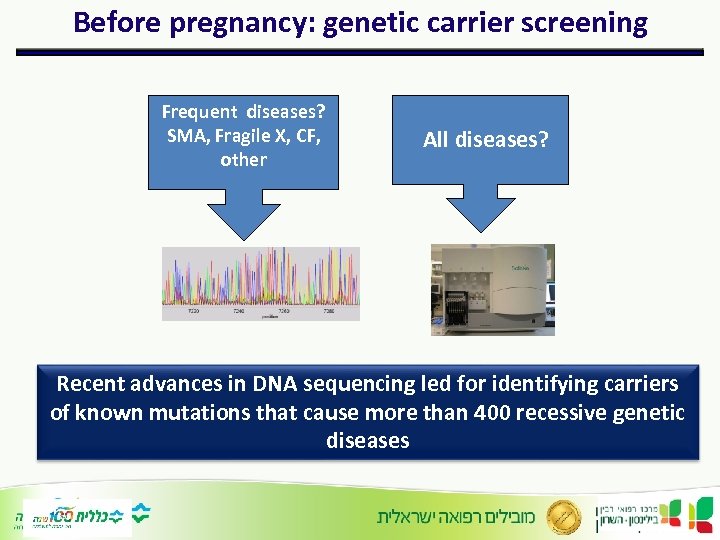 Before pregnancy: genetic carrier screening Frequent diseases? SMA, Fragile X, CF, other All diseases? Recent advances in DNA sequencing led for identifying carriers of known mutations that cause more than 400 recessive genetic diseases
Before pregnancy: genetic carrier screening Frequent diseases? SMA, Fragile X, CF, other All diseases? Recent advances in DNA sequencing led for identifying carriers of known mutations that cause more than 400 recessive genetic diseases
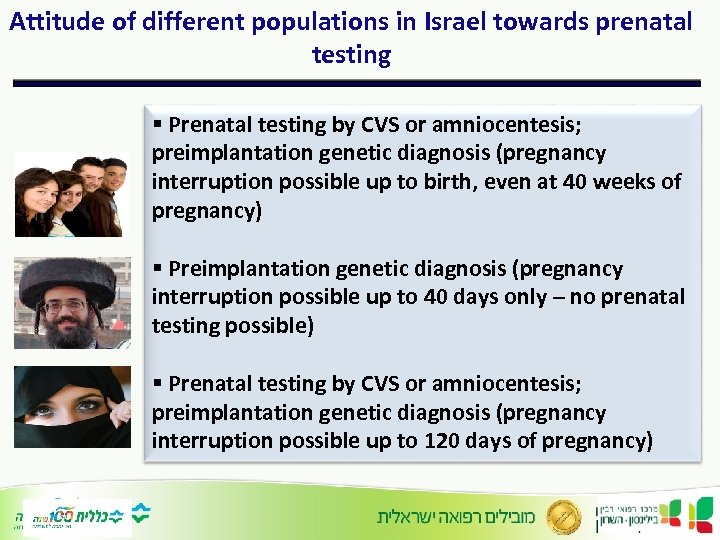 Attitude of different populations in Israel towards prenatal testing § Prenatal testing by CVS or amniocentesis; preimplantation genetic diagnosis (pregnancy interruption possible up to birth, even at 40 weeks of pregnancy) § Preimplantation genetic diagnosis (pregnancy interruption possible up to 40 days only – no prenatal testing possible) § Prenatal testing by CVS or amniocentesis; preimplantation genetic diagnosis (pregnancy interruption possible up to 120 days of pregnancy)
Attitude of different populations in Israel towards prenatal testing § Prenatal testing by CVS or amniocentesis; preimplantation genetic diagnosis (pregnancy interruption possible up to birth, even at 40 weeks of pregnancy) § Preimplantation genetic diagnosis (pregnancy interruption possible up to 40 days only – no prenatal testing possible) § Prenatal testing by CVS or amniocentesis; preimplantation genetic diagnosis (pregnancy interruption possible up to 120 days of pregnancy)
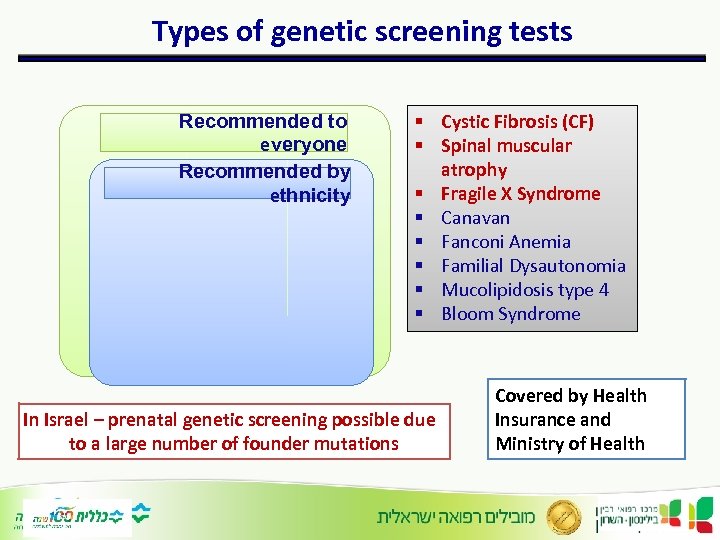 Types of genetic screening tests Recommended to everyone Recommended by ethnicity § Cystic Fibrosis (CF) § Spinal muscular atrophy § Fragile X Syndrome § Canavan § Fanconi Anemia § Familial Dysautonomia § Mucolipidosis type 4 § Bloom Syndrome In Israel – prenatal genetic screening possible due to a large number of founder mutations Covered by Health Insurance and Ministry of Health
Types of genetic screening tests Recommended to everyone Recommended by ethnicity § Cystic Fibrosis (CF) § Spinal muscular atrophy § Fragile X Syndrome § Canavan § Fanconi Anemia § Familial Dysautonomia § Mucolipidosis type 4 § Bloom Syndrome In Israel – prenatal genetic screening possible due to a large number of founder mutations Covered by Health Insurance and Ministry of Health
 http: //server. goldenhelix. org/israeli/
http: //server. goldenhelix. org/israeli/
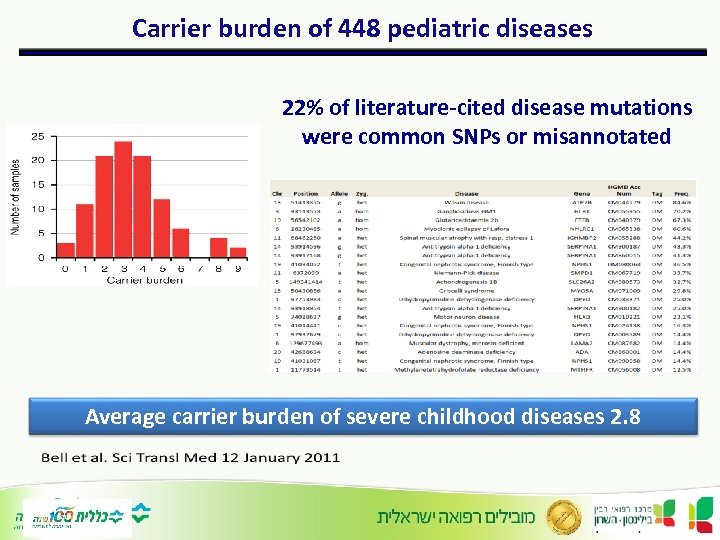 Carrier burden of 448 pediatric diseases 22% of literature-cited disease mutations were common SNPs or misannotated Average carrier burden of severe childhood diseases 2. 8
Carrier burden of 448 pediatric diseases 22% of literature-cited disease mutations were common SNPs or misannotated Average carrier burden of severe childhood diseases 2. 8
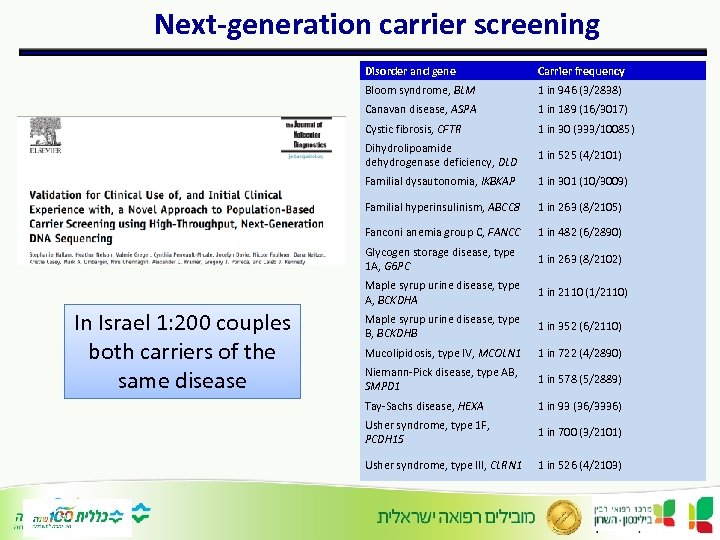 Next-generation carrier screening Disorder and gene Bloom syndrome, BLM 1 in 946 (3/2838) Canavan disease, ASPA 1 in 189 (16/3017) Cystic fibrosis, CFTR 1 in 30 (333/10085) Dihydrolipoamide dehydrogenase deficiency, DLD 1 in 525 (4/2101) Familial dysautonomia, IKBKAP 1 in 301 (10/3009) Familial hyperinsulinism, ABCC 8 1 in 263 (8/2105) Fanconi anemia group C, FANCC 1 in 482 (6/2890) Glycogen storage disease, type 1 A, G 6 PC 1 in 263 (8/2102) Maple syrup urine disease, type A, BCKDHA In Israel 1: 200 couples both carriers of the same disease Carrier frequency 1 in 2110 (1/2110) Maple syrup urine disease, type B, BCKDHB 1 in 352 (6/2110) Mucolipidosis, type IV, MCOLN 1 1 in 722 (4/2890) Niemann-Pick disease, type AB, SMPD 1 1 in 578 (5/2889) Tay-Sachs disease, HEXA 1 in 93 (36/3336) Usher syndrome, type 1 F, PCDH 15 1 in 700 (3/2101) Usher syndrome, type III, CLRN 1 1 in 526 (4/2103)
Next-generation carrier screening Disorder and gene Bloom syndrome, BLM 1 in 946 (3/2838) Canavan disease, ASPA 1 in 189 (16/3017) Cystic fibrosis, CFTR 1 in 30 (333/10085) Dihydrolipoamide dehydrogenase deficiency, DLD 1 in 525 (4/2101) Familial dysautonomia, IKBKAP 1 in 301 (10/3009) Familial hyperinsulinism, ABCC 8 1 in 263 (8/2105) Fanconi anemia group C, FANCC 1 in 482 (6/2890) Glycogen storage disease, type 1 A, G 6 PC 1 in 263 (8/2102) Maple syrup urine disease, type A, BCKDHA In Israel 1: 200 couples both carriers of the same disease Carrier frequency 1 in 2110 (1/2110) Maple syrup urine disease, type B, BCKDHB 1 in 352 (6/2110) Mucolipidosis, type IV, MCOLN 1 1 in 722 (4/2890) Niemann-Pick disease, type AB, SMPD 1 1 in 578 (5/2889) Tay-Sachs disease, HEXA 1 in 93 (36/3336) Usher syndrome, type 1 F, PCDH 15 1 in 700 (3/2101) Usher syndrome, type III, CLRN 1 1 in 526 (4/2103)
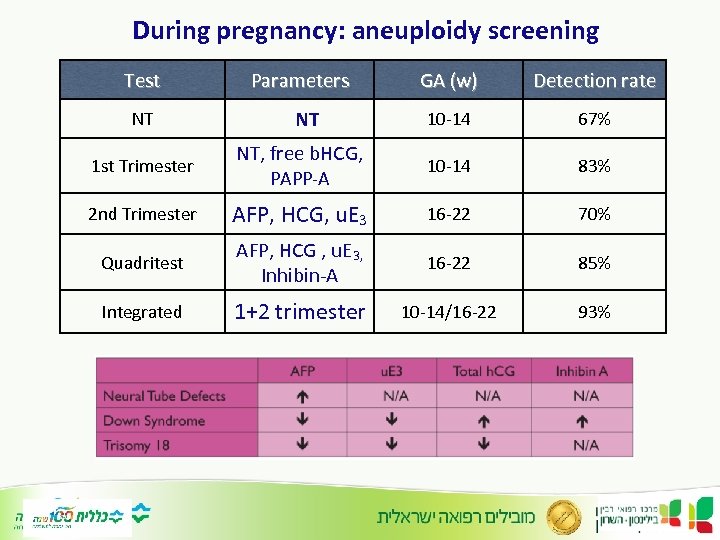 During pregnancy: aneuploidy screening Test NT Parameters NT GA (w) Detection rate 10 -14 67% 1 st Trimester NT, free b. HCG, PAPP-A 10 -14 83% 2 nd Trimester AFP, HCG, u. E 3 16 -22 70% Quadritest AFP, HCG , u. E 3, Inhibin-A 16 -22 85% Integrated 1+2 trimester 10 -14/16 -22 93%
During pregnancy: aneuploidy screening Test NT Parameters NT GA (w) Detection rate 10 -14 67% 1 st Trimester NT, free b. HCG, PAPP-A 10 -14 83% 2 nd Trimester AFP, HCG, u. E 3 16 -22 70% Quadritest AFP, HCG , u. E 3, Inhibin-A 16 -22 85% Integrated 1+2 trimester 10 -14/16 -22 93%
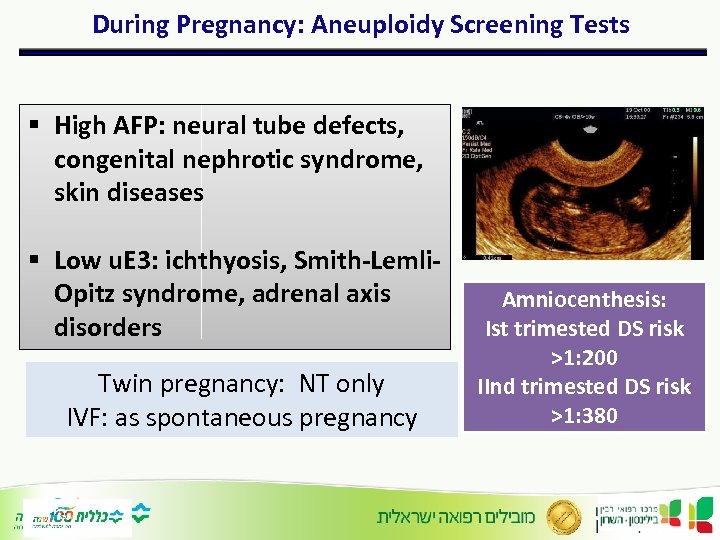 During Pregnancy: Aneuploidy Screening Tests § High AFP: neural tube defects, congenital nephrotic syndrome, skin diseases § Low u. E 3: ichthyosis, Smith-Lemli. Opitz syndrome, adrenal axis disorders Twin pregnancy: NT only IVF: as spontaneous pregnancy Amniocenthesis: Ist trimested DS risk >1: 200 IInd trimested DS risk >1: 380
During Pregnancy: Aneuploidy Screening Tests § High AFP: neural tube defects, congenital nephrotic syndrome, skin diseases § Low u. E 3: ichthyosis, Smith-Lemli. Opitz syndrome, adrenal axis disorders Twin pregnancy: NT only IVF: as spontaneous pregnancy Amniocenthesis: Ist trimested DS risk >1: 200 IInd trimested DS risk >1: 380
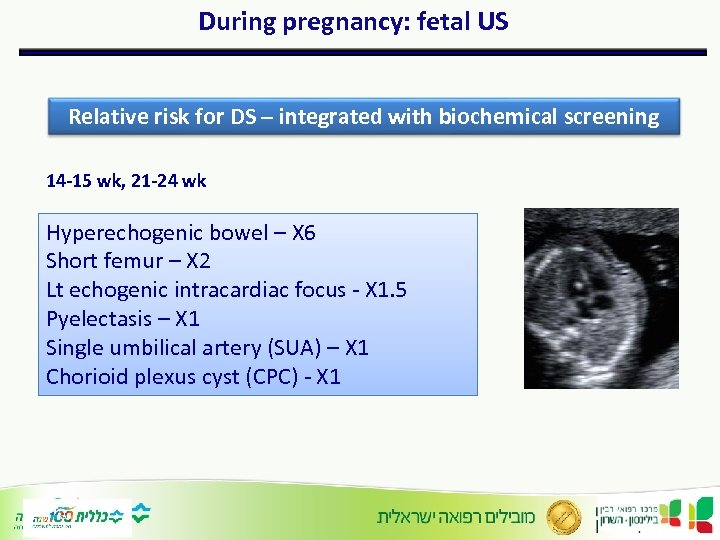 During pregnancy: fetal US Relative risk for DS – integrated with biochemical screening 14 -15 wk, 21 -24 wk Hyperechogenic bowel – X 6 Short femur – X 2 Lt echogenic intracardiac focus - X 1. 5 Pyelectasis – X 1 Single umbilical artery (SUA) – X 1 Chorioid plexus cyst (CPC) - X 1
During pregnancy: fetal US Relative risk for DS – integrated with biochemical screening 14 -15 wk, 21 -24 wk Hyperechogenic bowel – X 6 Short femur – X 2 Lt echogenic intracardiac focus - X 1. 5 Pyelectasis – X 1 Single umbilical artery (SUA) – X 1 Chorioid plexus cyst (CPC) - X 1
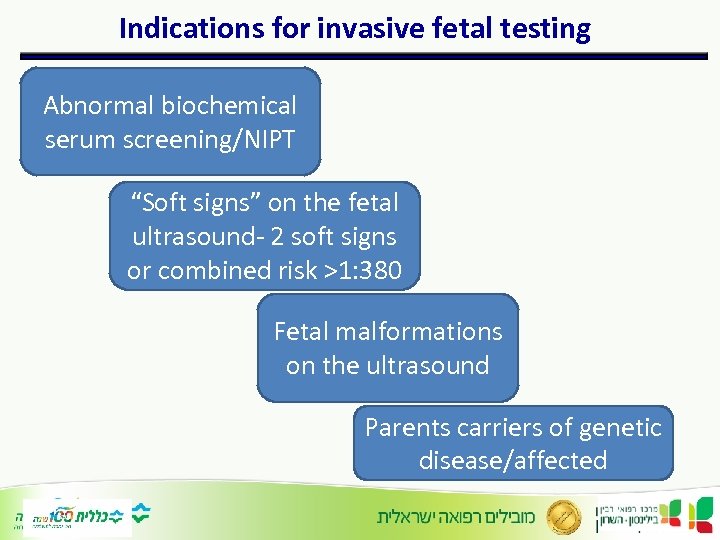 Indications for invasive fetal testing Abnormal biochemical serum screening/NIPT “Soft signs” on the fetal ultrasound- 2 soft signs or combined risk >1: 380 Fetal malformations on the ultrasound Parents carriers of genetic disease/affected
Indications for invasive fetal testing Abnormal biochemical serum screening/NIPT “Soft signs” on the fetal ultrasound- 2 soft signs or combined risk >1: 380 Fetal malformations on the ultrasound Parents carriers of genetic disease/affected
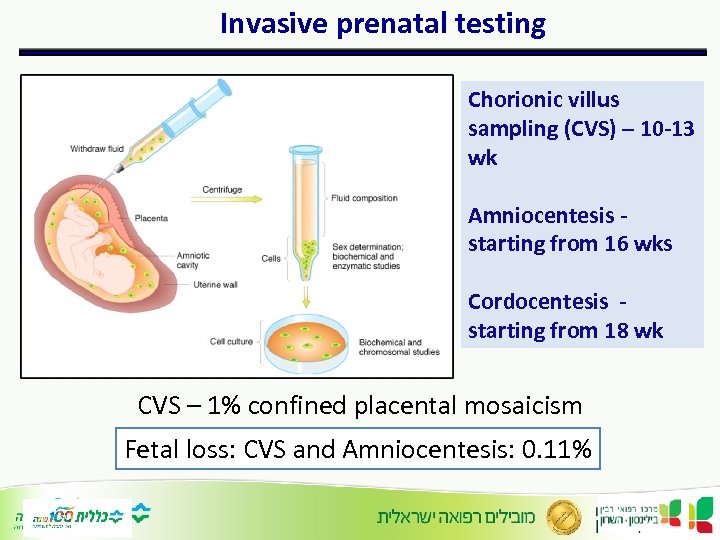 Invasive prenatal testing Chorionic villus sampling (CVS) – 10 -13 wk Amniocentesis starting from 16 wks Cordocentesis starting from 18 wk CVS – 1% confined placental mosaicism Fetal loss: CVS and Amniocentesis: 0. 11%
Invasive prenatal testing Chorionic villus sampling (CVS) – 10 -13 wk Amniocentesis starting from 16 wks Cordocentesis starting from 18 wk CVS – 1% confined placental mosaicism Fetal loss: CVS and Amniocentesis: 0. 11%
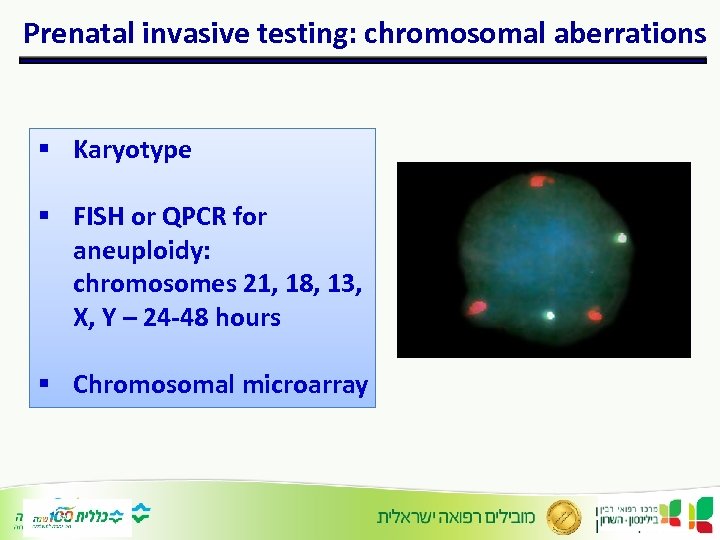 Prenatal invasive testing: chromosomal aberrations § Karyotype § FISH or QPCR for aneuploidy: chromosomes 21, 18, 13, X, Y – 24 -48 hours § Chromosomal microarray
Prenatal invasive testing: chromosomal aberrations § Karyotype § FISH or QPCR for aneuploidy: chromosomes 21, 18, 13, X, Y – 24 -48 hours § Chromosomal microarray
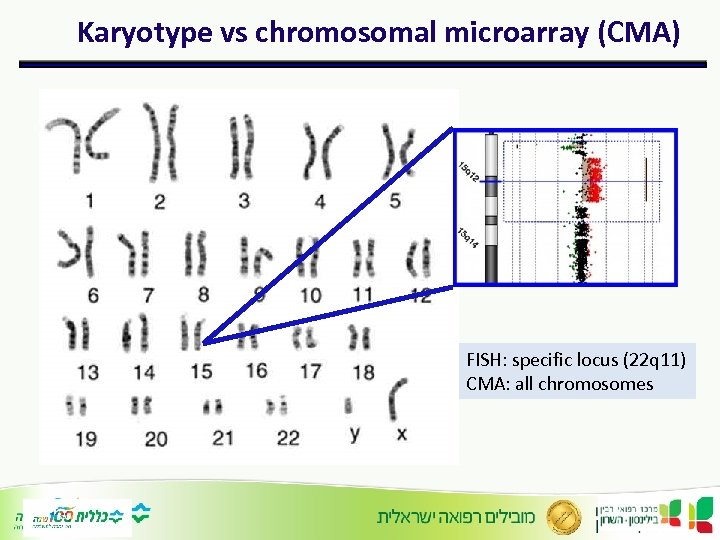 Karyotype vs chromosomal microarray (CMA) FISH: specific locus (22 q 11) CMA: all chromosomes
Karyotype vs chromosomal microarray (CMA) FISH: specific locus (22 q 11) CMA: all chromosomes
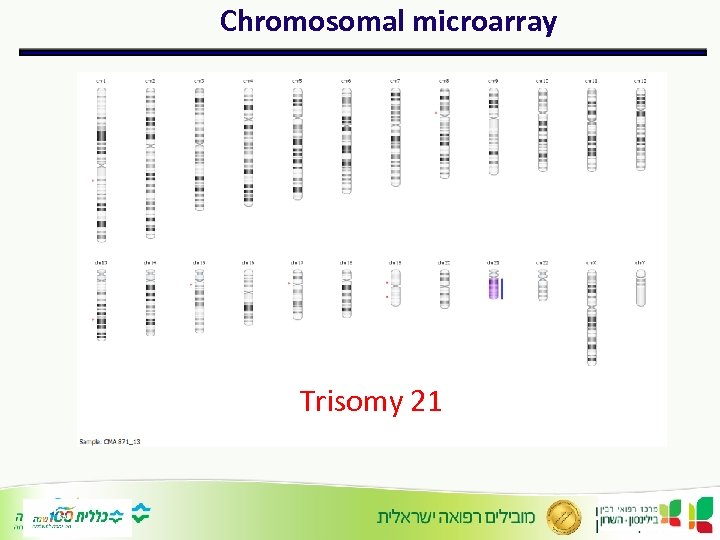 Chromosomal microarray Trisomy 21
Chromosomal microarray Trisomy 21
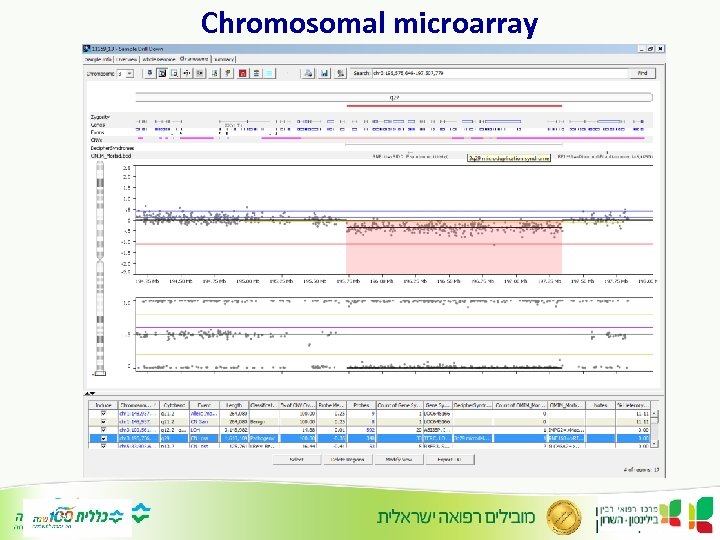 Chromosomal microarray
Chromosomal microarray
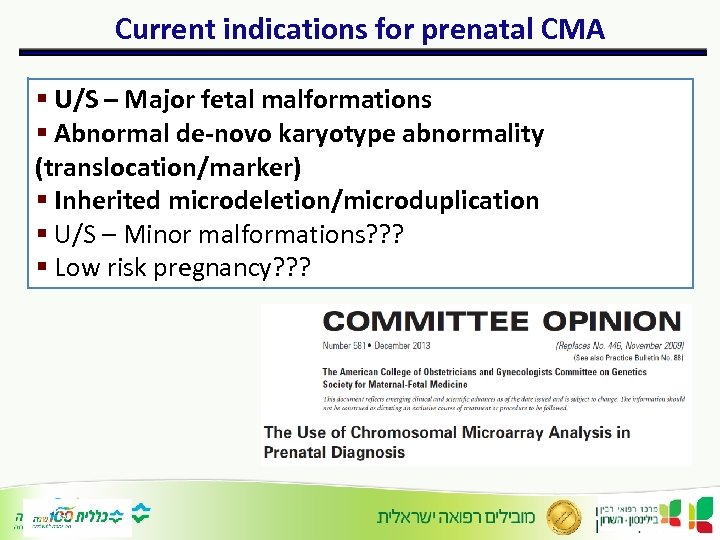 Current indications for prenatal CMA § U/S – Major fetal malformations § Abnormal de-novo karyotype abnormality (translocation/marker) § Inherited microdeletion/microduplication § U/S – Minor malformations? ? ? § Low risk pregnancy? ? ?
Current indications for prenatal CMA § U/S – Major fetal malformations § Abnormal de-novo karyotype abnormality (translocation/marker) § Inherited microdeletion/microduplication § U/S – Minor malformations? ? ? § Low risk pregnancy? ? ?
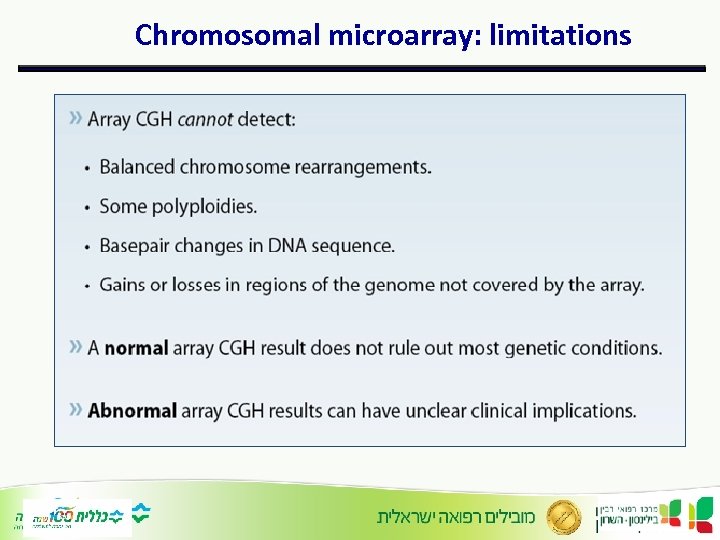 Chromosomal microarray: limitations
Chromosomal microarray: limitations
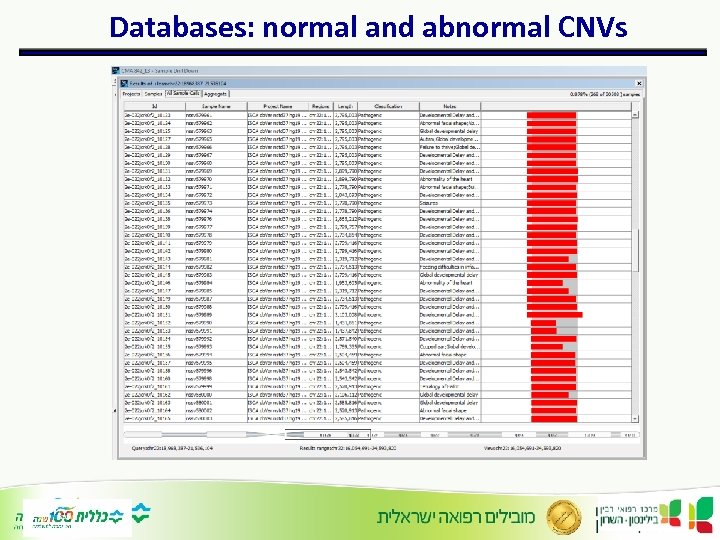 Databases: normal and abnormal CNVs
Databases: normal and abnormal CNVs
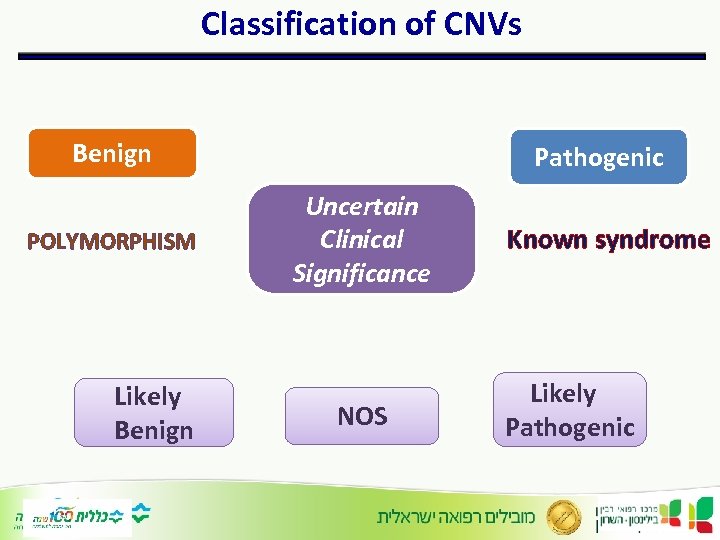 Classification of CNVs Benign POLYMORPHISM Likely Benign Pathogenic Uncertain Clinical Significance NOS Known syndrome Likely Pathogenic
Classification of CNVs Benign POLYMORPHISM Likely Benign Pathogenic Uncertain Clinical Significance NOS Known syndrome Likely Pathogenic
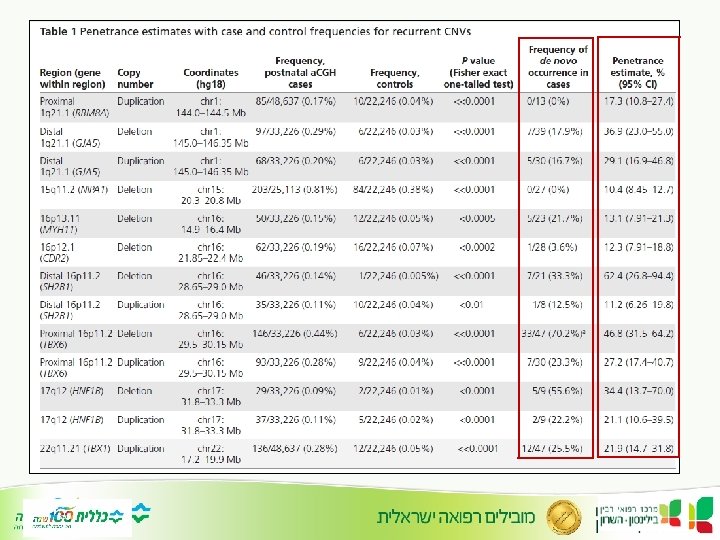
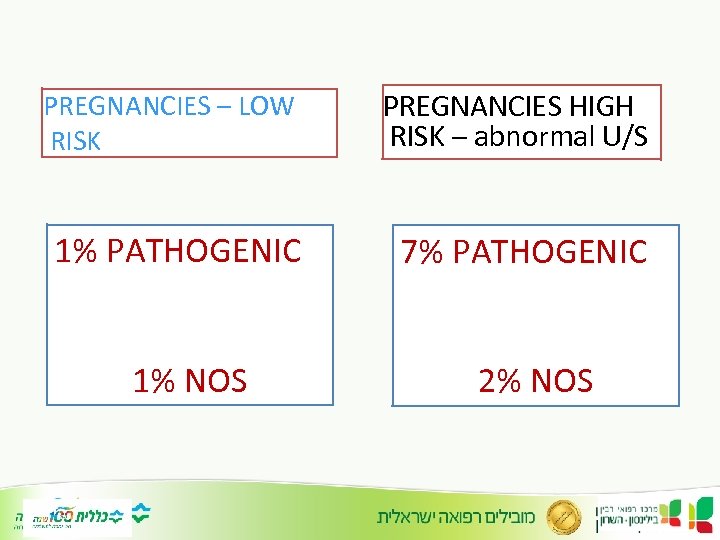 PREGNANCIES – LOW RISK PREGNANCIES HIGH RISK – abnormal U/S 1% PATHOGENIC 7% PATHOGENIC 1% NOS 2% NOS
PREGNANCIES – LOW RISK PREGNANCIES HIGH RISK – abnormal U/S 1% PATHOGENIC 7% PATHOGENIC 1% NOS 2% NOS
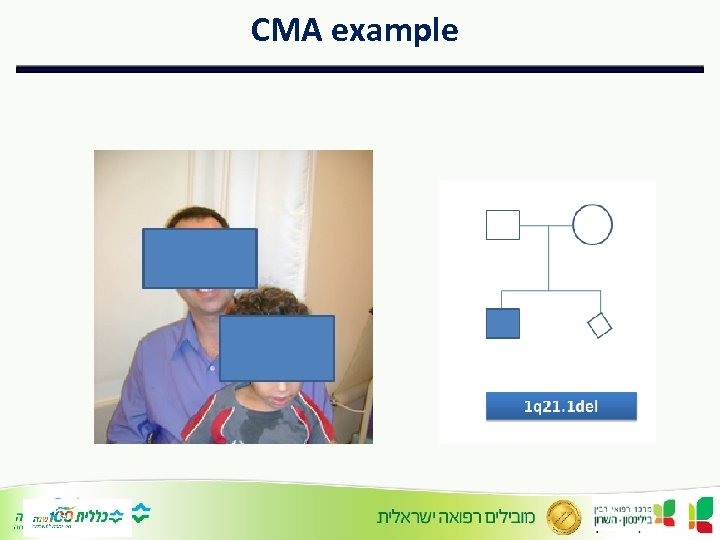 CMA example
CMA example
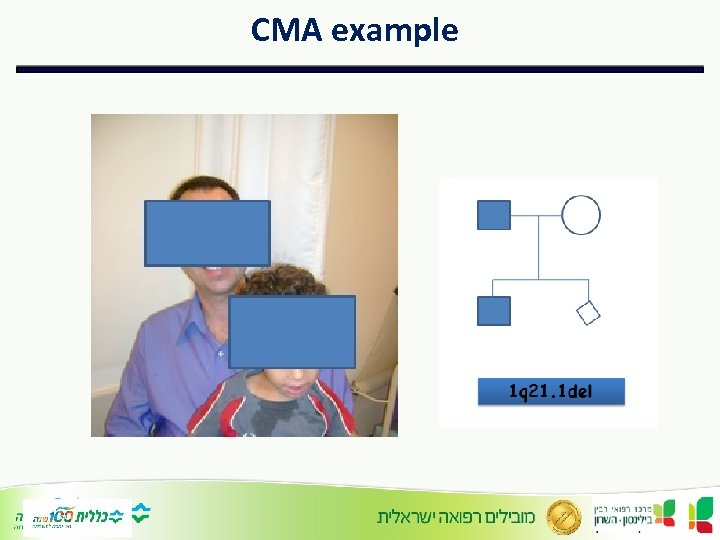 CMA example
CMA example
 To test or not to test?
To test or not to test?
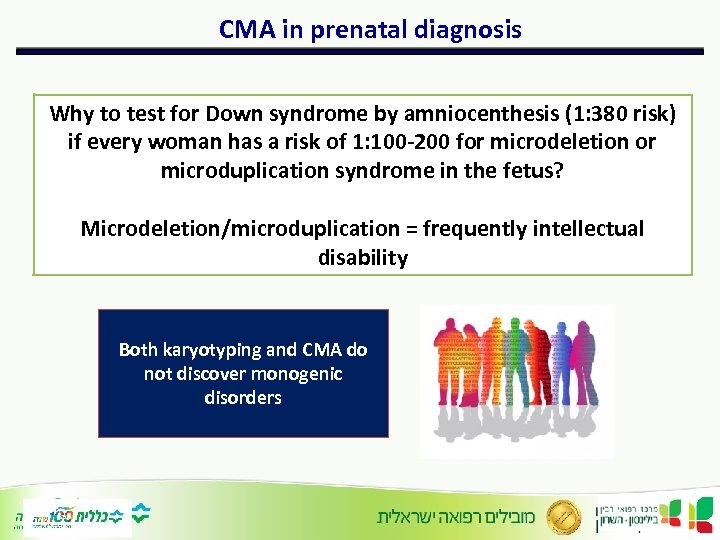 CMA in prenatal diagnosis Why to test for Down syndrome by amniocenthesis (1: 380 risk) if every woman has a risk of 1: 100 -200 for microdeletion or microduplication syndrome in the fetus? Microdeletion/microduplication = frequently intellectual disability Both karyotyping and CMA do not discover monogenic disorders
CMA in prenatal diagnosis Why to test for Down syndrome by amniocenthesis (1: 380 risk) if every woman has a risk of 1: 100 -200 for microdeletion or microduplication syndrome in the fetus? Microdeletion/microduplication = frequently intellectual disability Both karyotyping and CMA do not discover monogenic disorders
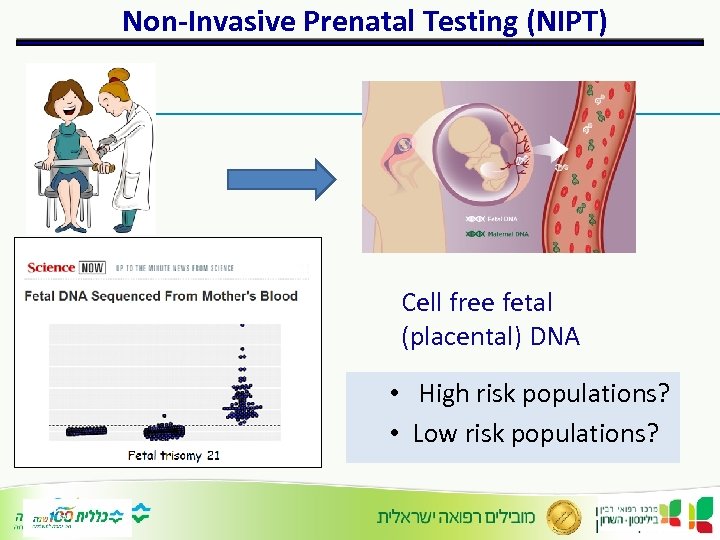 Non-Invasive Prenatal Testing (NIPT) Cell free fetal (placental) DNA • High risk populations? • Low risk populations?
Non-Invasive Prenatal Testing (NIPT) Cell free fetal (placental) DNA • High risk populations? • Low risk populations?
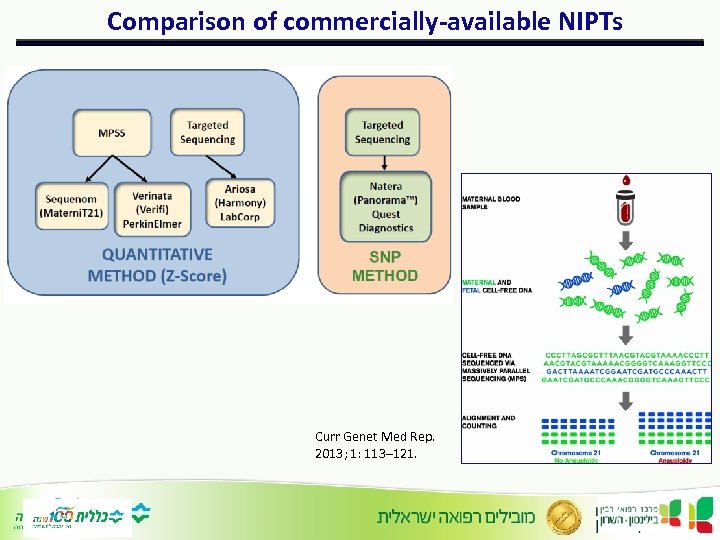 Comparison of commercially-available NIPTs Curr Genet Med Rep. 2013; 1: 113– 121.
Comparison of commercially-available NIPTs Curr Genet Med Rep. 2013; 1: 113– 121.
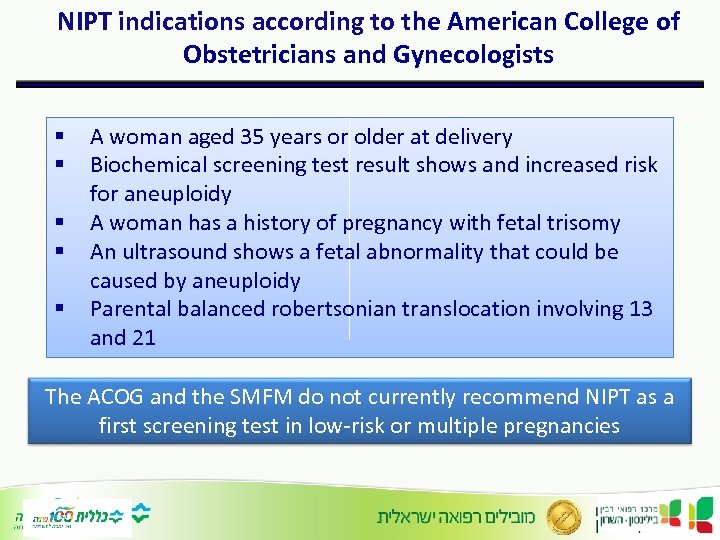 NIPT indications according to the American College of Obstetricians and Gynecologists § § § A woman aged 35 years or older at delivery Biochemical screening test result shows and increased risk for aneuploidy A woman has a history of pregnancy with fetal trisomy An ultrasound shows a fetal abnormality that could be caused by aneuploidy Parental balanced robertsonian translocation involving 13 and 21 The ACOG and the SMFM do not currently recommend NIPT as a first screening test in low-risk or multiple pregnancies
NIPT indications according to the American College of Obstetricians and Gynecologists § § § A woman aged 35 years or older at delivery Biochemical screening test result shows and increased risk for aneuploidy A woman has a history of pregnancy with fetal trisomy An ultrasound shows a fetal abnormality that could be caused by aneuploidy Parental balanced robertsonian translocation involving 13 and 21 The ACOG and the SMFM do not currently recommend NIPT as a first screening test in low-risk or multiple pregnancies
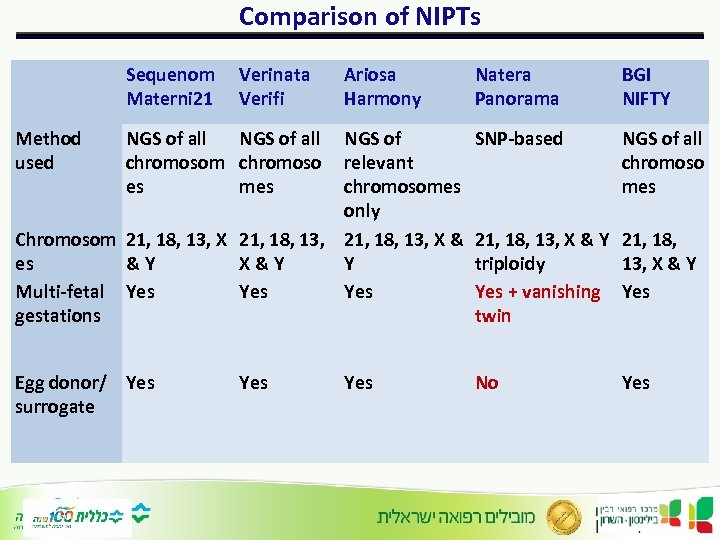 Comparison of NIPTs Sequenom Materni 21 Natera Panorama BGI NIFTY NGS of relevant chromosomes only Chromosom 21, 18, 13, X & es &Y X&Y Y Multi-fetal Yes Yes gestations SNP-based NGS of all chromoso mes Egg donor/ Yes surrogate No Method used Verinata Verifi Ariosa Harmony NGS of all chromosom chromoso es mes Yes 21, 18, 13, X & Y 21, 18, triploidy 13, X & Y Yes + vanishing Yes twin Yes
Comparison of NIPTs Sequenom Materni 21 Natera Panorama BGI NIFTY NGS of relevant chromosomes only Chromosom 21, 18, 13, X & es &Y X&Y Y Multi-fetal Yes Yes gestations SNP-based NGS of all chromoso mes Egg donor/ Yes surrogate No Method used Verinata Verifi Ariosa Harmony NGS of all chromosom chromoso es mes Yes 21, 18, 13, X & Y 21, 18, triploidy 13, X & Y Yes + vanishing Yes twin Yes
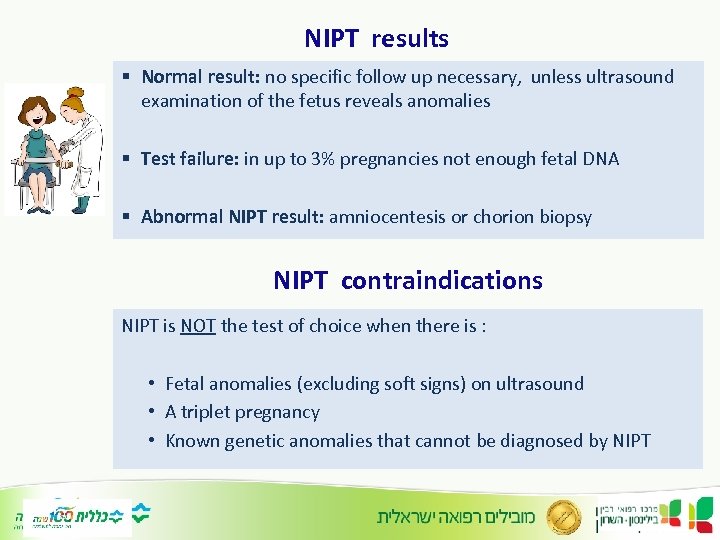 NIPT results § Normal result: no specific follow up necessary, unless ultrasound examination of the fetus reveals anomalies § Test failure: in up to 3% pregnancies not enough fetal DNA § Abnormal NIPT result: amniocentesis or chorion biopsy NIPT contraindications NIPT is NOT the test of choice when there is : • Fetal anomalies (excluding soft signs) on ultrasound • A triplet pregnancy • Known genetic anomalies that cannot be diagnosed by NIPT
NIPT results § Normal result: no specific follow up necessary, unless ultrasound examination of the fetus reveals anomalies § Test failure: in up to 3% pregnancies not enough fetal DNA § Abnormal NIPT result: amniocentesis or chorion biopsy NIPT contraindications NIPT is NOT the test of choice when there is : • Fetal anomalies (excluding soft signs) on ultrasound • A triplet pregnancy • Known genetic anomalies that cannot be diagnosed by NIPT
 NIPT reliability § Phenotype for sex aneuploidies is highly variable § Mosaicism in the fetus is a problem § Mosaicism in the mother is a problem § NIPT for sex aneuploidies is less accurate
NIPT reliability § Phenotype for sex aneuploidies is highly variable § Mosaicism in the fetus is a problem § Mosaicism in the mother is a problem § NIPT for sex aneuploidies is less accurate
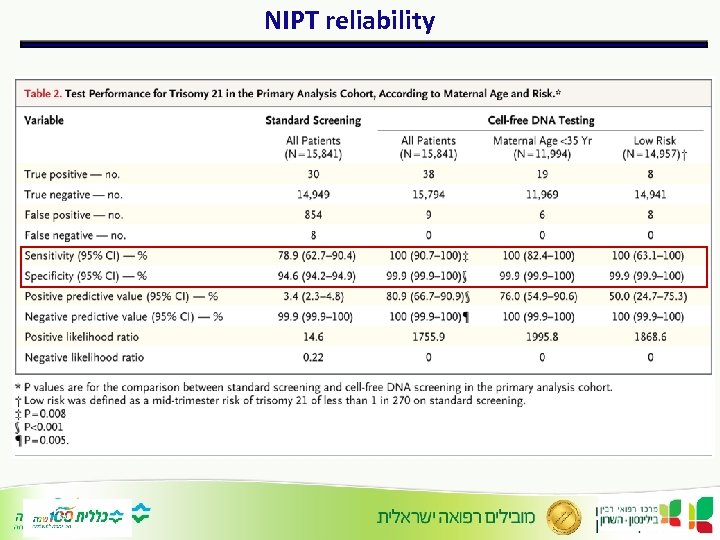 NIPT reliability
NIPT reliability
 NIPT reliability
NIPT reliability
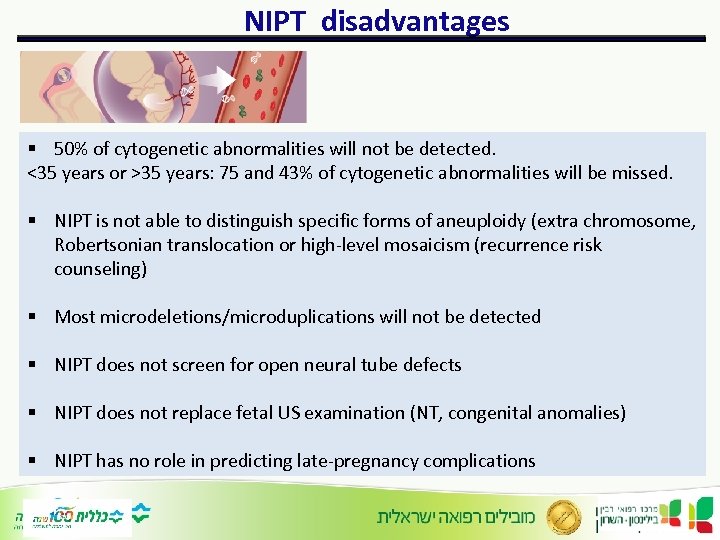 NIPT disadvantages § 50% of cytogenetic abnormalities will not be detected. <35 years or >35 years: 75 and 43% of cytogenetic abnormalities will be missed. § NIPT is not able to distinguish specific forms of aneuploidy (extra chromosome, Robertsonian translocation or high-level mosaicism (recurrence risk counseling) § Most microdeletions/microduplications will not be detected § NIPT does not screen for open neural tube defects § NIPT does not replace fetal US examination (NT, congenital anomalies) § NIPT has no role in predicting late-pregnancy complications
NIPT disadvantages § 50% of cytogenetic abnormalities will not be detected. <35 years or >35 years: 75 and 43% of cytogenetic abnormalities will be missed. § NIPT is not able to distinguish specific forms of aneuploidy (extra chromosome, Robertsonian translocation or high-level mosaicism (recurrence risk counseling) § Most microdeletions/microduplications will not be detected § NIPT does not screen for open neural tube defects § NIPT does not replace fetal US examination (NT, congenital anomalies) § NIPT has no role in predicting late-pregnancy complications
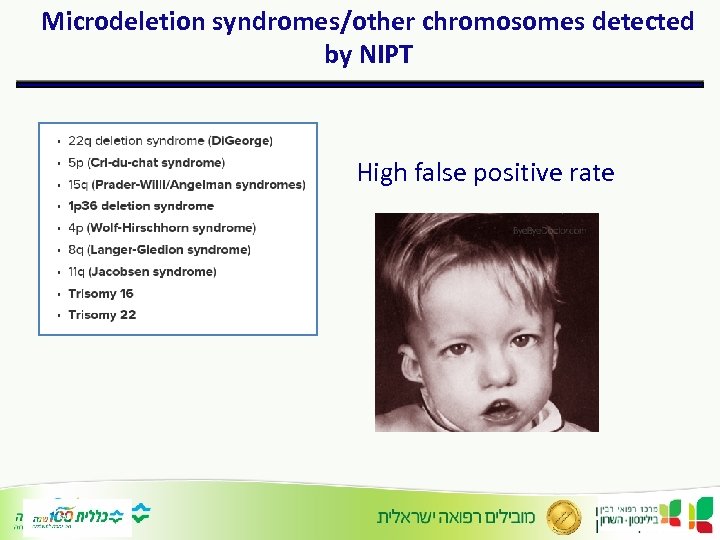 Microdeletion syndromes/other chromosomes detected by NIPT High false positive rate
Microdeletion syndromes/other chromosomes detected by NIPT High false positive rate
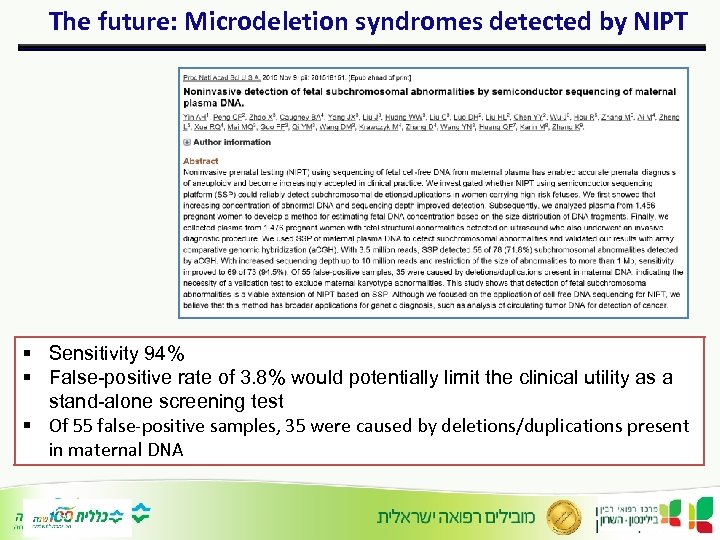 The future: Microdeletion syndromes detected by NIPT § Sensitivity 94% § False-positive rate of 3. 8% would potentially limit the clinical utility as a stand-alone screening test § Of 55 false-positive samples, 35 were caused by deletions/duplications present in maternal DNA
The future: Microdeletion syndromes detected by NIPT § Sensitivity 94% § False-positive rate of 3. 8% would potentially limit the clinical utility as a stand-alone screening test § Of 55 false-positive samples, 35 were caused by deletions/duplications present in maternal DNA
 The future: monogenic disorders detection by NIPT
The future: monogenic disorders detection by NIPT
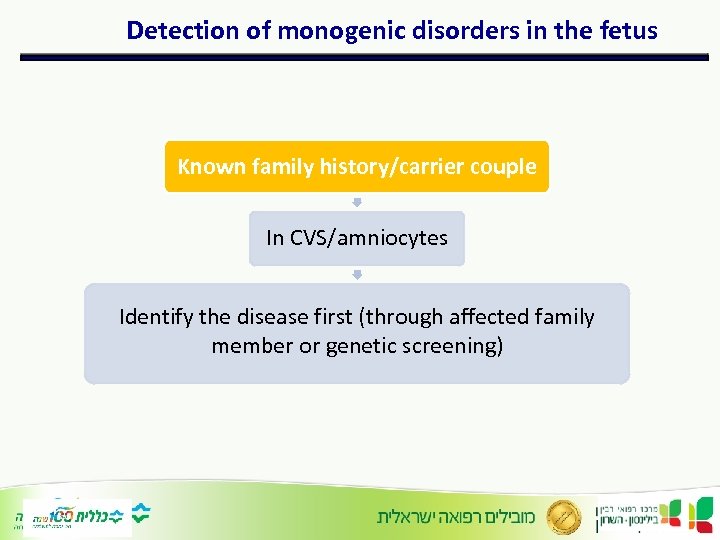 Detection of monogenic disorders in the fetus Known family history/carrier couple In CVS/amniocytes Identify the disease first (through affected family member or genetic screening)
Detection of monogenic disorders in the fetus Known family history/carrier couple In CVS/amniocytes Identify the disease first (through affected family member or genetic screening)
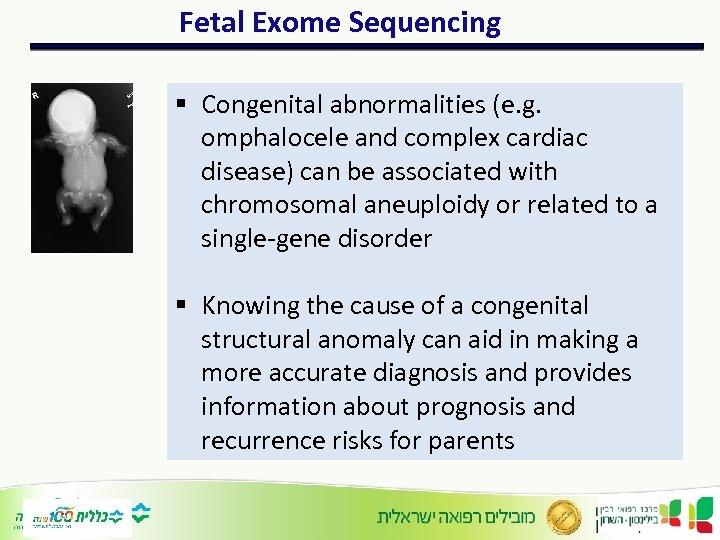 Fetal Exome Sequencing § Congenital abnormalities (e. g. omphalocele and complex cardiac disease) can be associated with chromosomal aneuploidy or related to a single-gene disorder § Knowing the cause of a congenital structural anomaly can aid in making a more accurate diagnosis and provides information about prognosis and recurrence risks for parents
Fetal Exome Sequencing § Congenital abnormalities (e. g. omphalocele and complex cardiac disease) can be associated with chromosomal aneuploidy or related to a single-gene disorder § Knowing the cause of a congenital structural anomaly can aid in making a more accurate diagnosis and provides information about prognosis and recurrence risks for parents
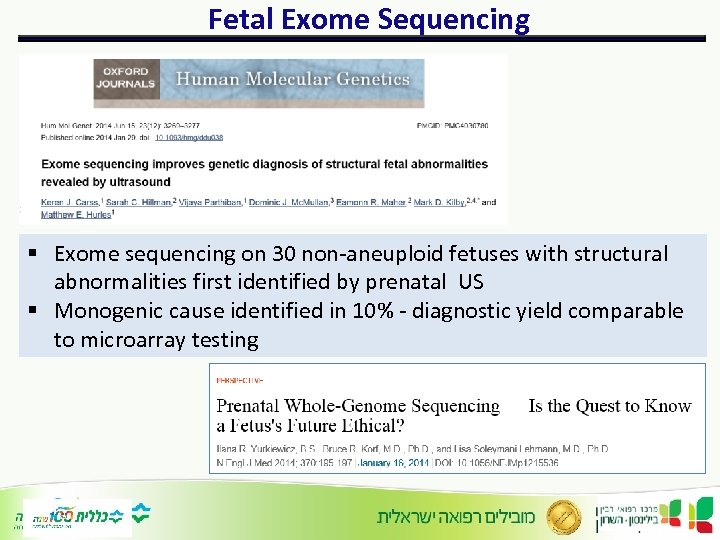 Fetal Exome Sequencing § Exome sequencing on 30 non-aneuploid fetuses with structural abnormalities first identified by prenatal US § Monogenic cause identified in 10% - diagnostic yield comparable to microarray testing
Fetal Exome Sequencing § Exome sequencing on 30 non-aneuploid fetuses with structural abnormalities first identified by prenatal US § Monogenic cause identified in 10% - diagnostic yield comparable to microarray testing
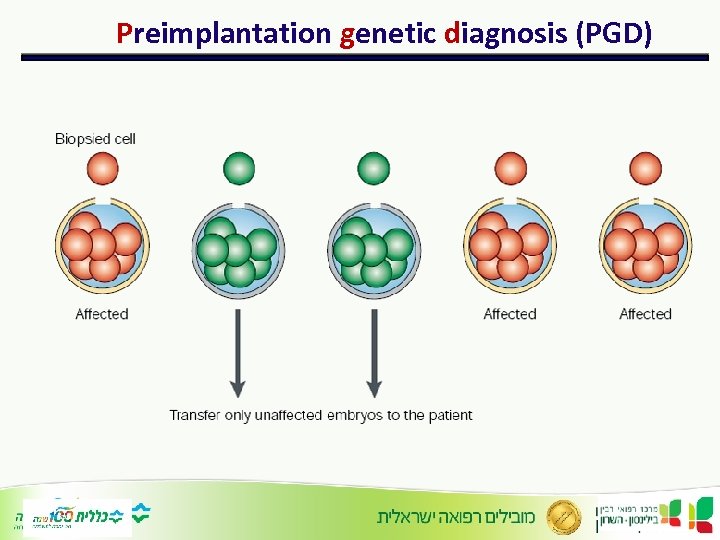 Preimplantation genetic diagnosis (PGD)
Preimplantation genetic diagnosis (PGD)
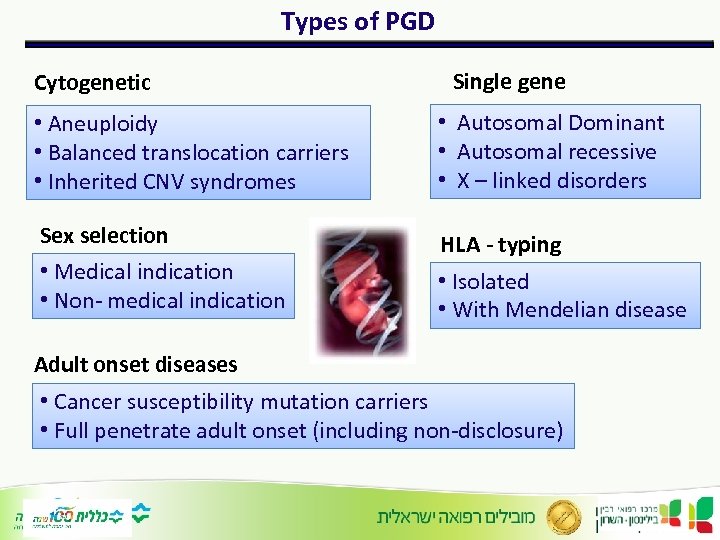 Types of PGD Cytogenetic Single gene • Aneuploidy • Balanced translocation carriers • Inherited CNV syndromes • Autosomal Dominant • Autosomal recessive • X – linked disorders Sex selection HLA - typing • Medical indication • Non- medical indication • Isolated • With Mendelian disease Adult onset diseases • Cancer susceptibility mutation carriers • Full penetrate adult onset (including non-disclosure)
Types of PGD Cytogenetic Single gene • Aneuploidy • Balanced translocation carriers • Inherited CNV syndromes • Autosomal Dominant • Autosomal recessive • X – linked disorders Sex selection HLA - typing • Medical indication • Non- medical indication • Isolated • With Mendelian disease Adult onset diseases • Cancer susceptibility mutation carriers • Full penetrate adult onset (including non-disclosure)
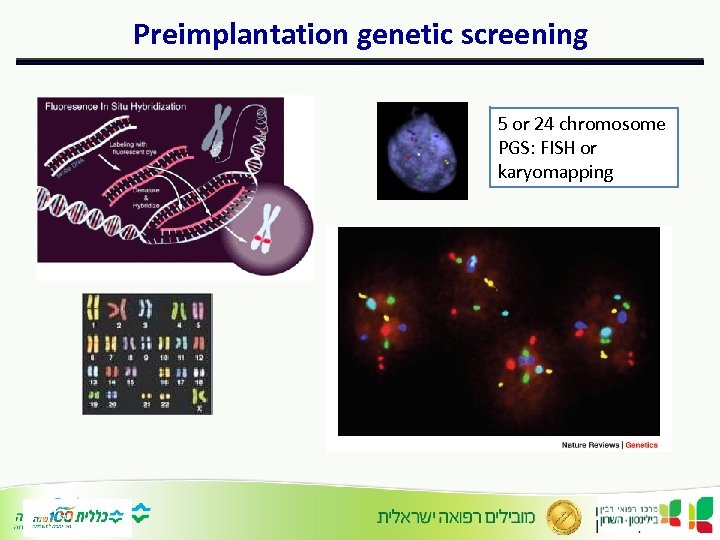 Preimplantation genetic screening 5 or 24 chromosome PGS: FISH or karyomapping
Preimplantation genetic screening 5 or 24 chromosome PGS: FISH or karyomapping
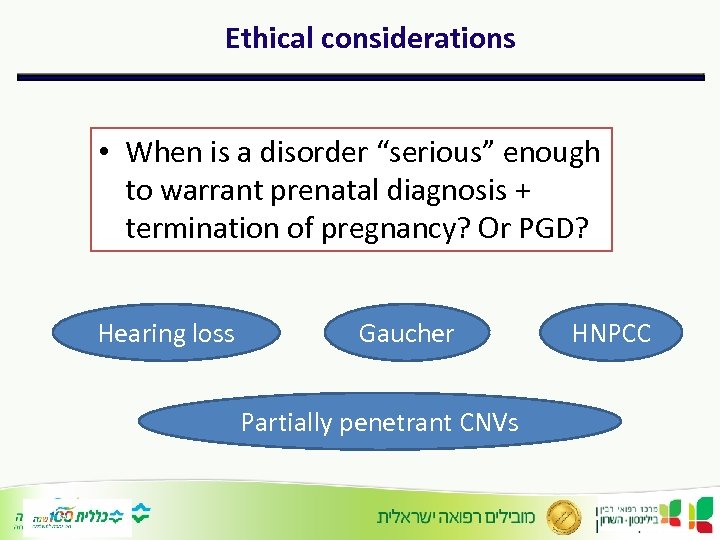 Ethical considerations • When is a disorder “serious” enough to warrant prenatal diagnosis + termination of pregnancy? Or PGD? Hearing loss Gaucher Partially penetrant CNVs HNPCC
Ethical considerations • When is a disorder “serious” enough to warrant prenatal diagnosis + termination of pregnancy? Or PGD? Hearing loss Gaucher Partially penetrant CNVs HNPCC
 Thank you!
Thank you!


