401a8e0f6ea72f79bee92036574d1860.ppt
- Количество слайдов: 72

ANESTHESIA
“Nothing in life is to be feared. It is only to be understood. ” Marie Curie (`868 -1934)
ANESTHESIA General anesthesia Regional anesthesia Monitored anesthesia care

General anesthesia
“Before him surgery was agony. ” Epitaph on a monument honoring W. Morton

General anesthesia The goals of general anesthesia: - Mandatory: -amnesia/sedation/hypnosis -analgesia -maintenance of homeostasis - Optionally: -muscle relaxation
General anesthesia indications Indications based on the surgical procedure: -surgical procedures requiring analgesia and muscle relaxation, that cannot be performed using regional anesthesia techniques: upper abdominal surgery, thoracic surgery, head and neck surgery, shoulder surgery etc. -surgical procedures that significally interfere with vital functions: neurosurgery, thoracic surgery, cardiac surgery, surgery of the aorta etc.

General anesthesia indications Indications based on the patient condition: -different pathologies or ongoing treatments that make the regional anesthesia tachniques contraindicated: the patients with coagulation disorders, anticoagulant treatments, infections or other lesions in the area where a regional anesthesia procedure would be performed; -systemic diseases with definite functional limitations: the patient with respiratory insufficency, shock, coma, major hydroelectrolytic or acido-basic imbalance.

Drugs used for general anesthesia Hypnosis Analgesia Muscle relaxation Maintenance of homeostasis can all be achieved by administering one or more drugs
Drugs used for general anesthesia • Inhalatory anesthetics: -gaseous form nitrous oxide -volatile liquids halothane, isoflurane, sevoflurane si desflurane The advantage of entering and leaving the body by ventilation with minimal metabolization. They result in sedation, analgesia and light muscle relaxation.
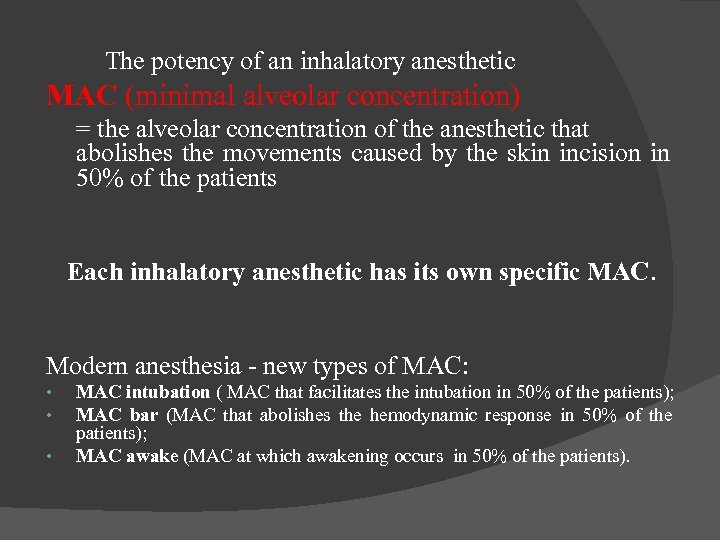
The potency of an inhalatory anesthetic MAC (minimal alveolar concentration) = the alveolar concentration of the anesthetic that abolishes the movements caused by the skin incision in 50% of the patients Each inhalatory anesthetic has its own specific MAC. Modern anesthesia - new types of MAC: • • • MAC intubation ( MAC that facilitates the intubation in 50% of the patients); MAC bar (MAC that abolishes the hemodynamic response in 50% of the patients); MAC awake (MAC at which awakening occurs in 50% of the patients).
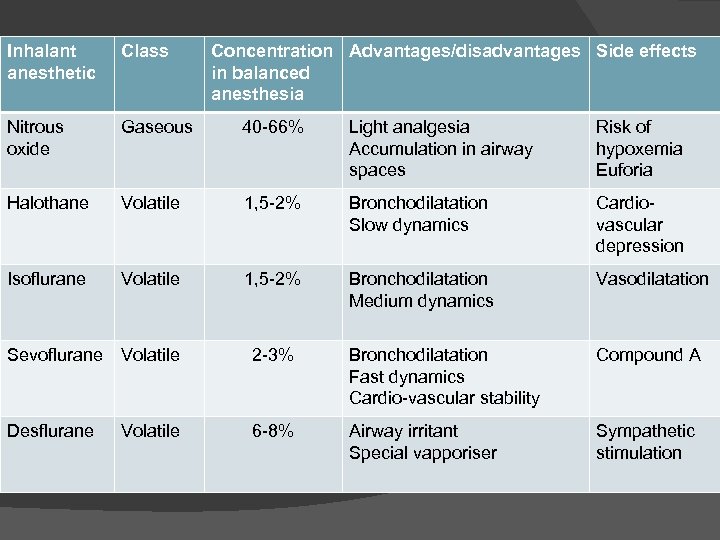
Inhalant anesthetic Class Concentration Advantages/disadvantages Side effects in balanced anesthesia Nitrous oxide Gaseous 40 -66% Light analgesia Accumulation in airway spaces Risk of hypoxemia Euforia Halothane Volatile 1, 5 -2% Bronchodilatation Slow dynamics Cardiovascular depression Isoflurane Volatile 1, 5 -2% Bronchodilatation Medium dynamics Vasodilatation Sevoflurane Volatile 2 -3% Bronchodilatation Fast dynamics Cardio-vascular stability Compound A Desflurane 6 -8% Airway irritant Special vapporiser Sympathetic stimulation Volatile
Intravenous anesthetics: Short acting: Barbiturates → metohexital thiopental, tiamital Imidazolic compounds → etomidate Alkylphenols → propofol Steroids → eltanolone Long acting: Ketamine Benzodiazepines → diazepam, midazolam
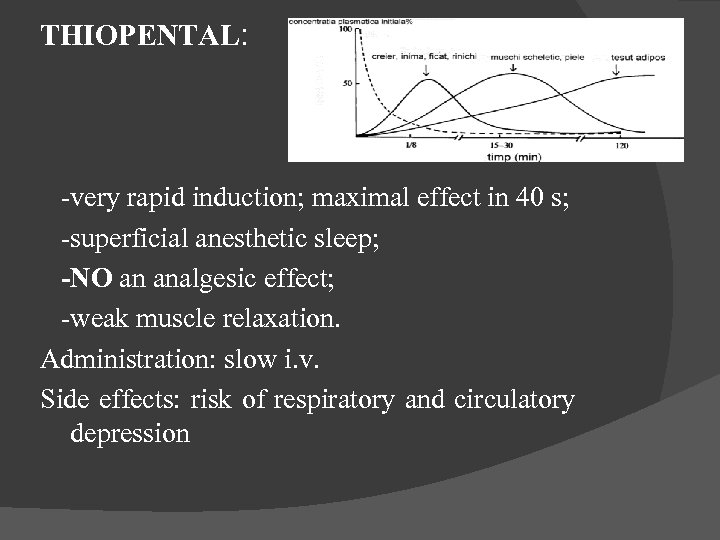
THIOPENTAL: -very rapid induction; maximal effect in 40 s; -superficial anesthetic sleep; -NO an analgesic effect; -weak muscle relaxation. Administration: slow i. v. Side effects: risk of respiratory and circulatory depression
PROPOFOL -very liposoluble fatty acid; -hepatic metabolisation in great extent → short effect; Pharmacodynamic action: -pharmacologic effects similar with those of Thiopental; -less residual effects.
KETAMINE Pharmacodynamic action: Dissociative anesthetic: - dissociation from the environment - superficial sleep - strong analgesia Advantages: -No respiratory depressant effect; -hemodynamic stability by the release of catecholamines -bronchodilatatory effect
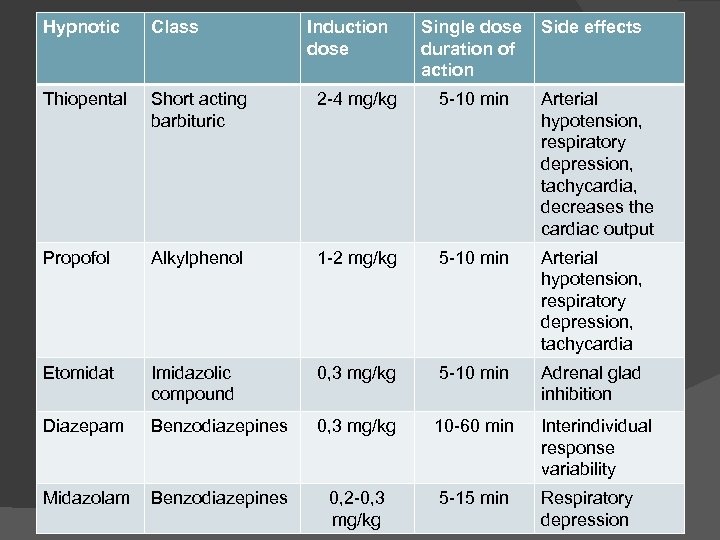
Hypnotic Class Induction dose Single dose duration of action Side effects Thiopental Short acting barbituric 2 -4 mg/kg 5 -10 min Arterial hypotension, respiratory depression, tachycardia, decreases the cardiac output Propofol Alkylphenol 1 -2 mg/kg 5 -10 min Arterial hypotension, respiratory depression, tachycardia Etomidat Imidazolic compound 0, 3 mg/kg 5 -10 min Adrenal glad inhibition Diazepam Benzodiazepines 0, 3 mg/kg 10 -60 min Interindividual response variability Midazolam Benzodiazepines 0, 2 -0, 3 mg/kg 5 -15 min Respiratory depression
Analgetics: Opioids: -the class of analgesics with the broadest intraanesthetic utilisation; -profound dose-dependant analgesia; -in spite of their quasi-constant use during general anesthesia, the opioids are not anesthetics because the loss of consciousness is not a regular effect -they regularly result in respiratory dosedependent depression. Cardiovascular depression is a variable effect.
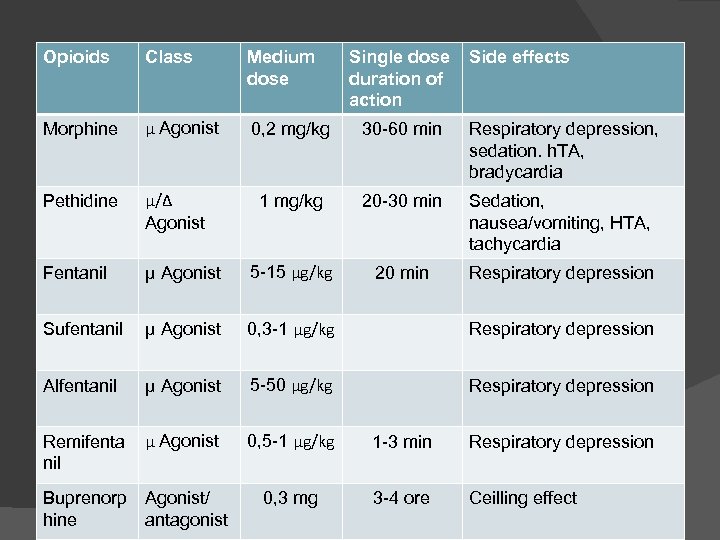
Opioids Class Medium dose Morphine μ Agonist 0, 2 mg/kg 30 -60 min Respiratory depression, sedation. h. TA, bradycardia Pethidine μ/Δ Agonist 1 mg/kg 20 -30 min Sedation, nausea/vomiting, HTA, tachycardia Fentanil μ Agonist 5 -15 μg/kg 20 min Respiratory depression Sufentanil μ Agonist 0, 3 -1 μg/kg Respiratory depression Alfentanil μ Agonist 5 -50 μg/kg Respiratory depression Remifenta nil μ Agonist 0, 5 -1 μg/kg 1 -3 min Respiratory depression 0, 3 mg 3 -4 ore Ceilling effect Buprenorp Agonist/ hine antagonist Single dose duration of action Side effects
Muscle relaxants: -substances that act at the neuromuscular junction level and prevent the transmission of the physiologic stimulus for the muscular contraction; -NO action on the CNS, NO loss of consciousness, NO analgesia; -utilized for the facilitation of the airway instrumentation, of mechanical ventilation and of the surgical intervention; -results in alveolar hypoventilation or apnea by the action on the respiratory muscles; -minimal cardio-vascular effects.
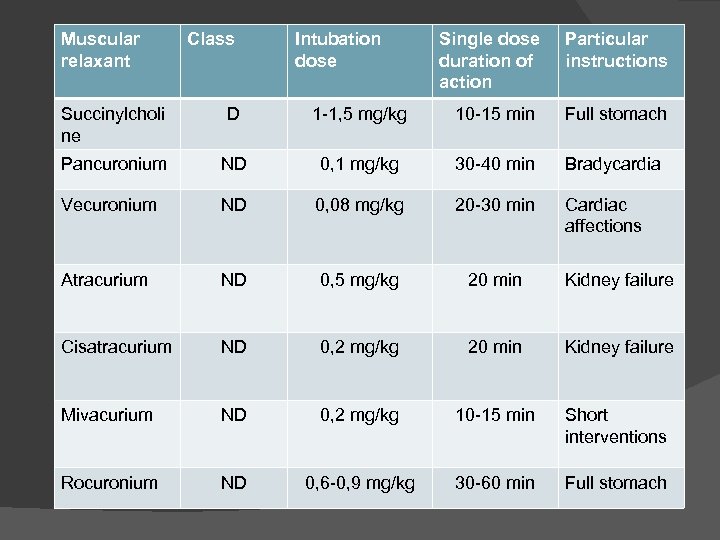
Muscular relaxant Class Intubation dose Single dose duration of action Particular instructions Succinylcholi ne D 1 -1, 5 mg/kg 10 -15 min Full stomach Pancuronium ND 0, 1 mg/kg 30 -40 min Bradycardia Vecuronium ND 0, 08 mg/kg 20 -30 min Cardiac affections Atracurium ND 0, 5 mg/kg 20 min Kidney failure Cisatracurium ND 0, 2 mg/kg 20 min Kidney failure Mivacurium ND 0, 2 mg/kg 10 -15 min Short interventions Rocuronium ND 0, 6 -0, 9 mg/kg 30 -60 min Full stomach
Anesthesia apparatus
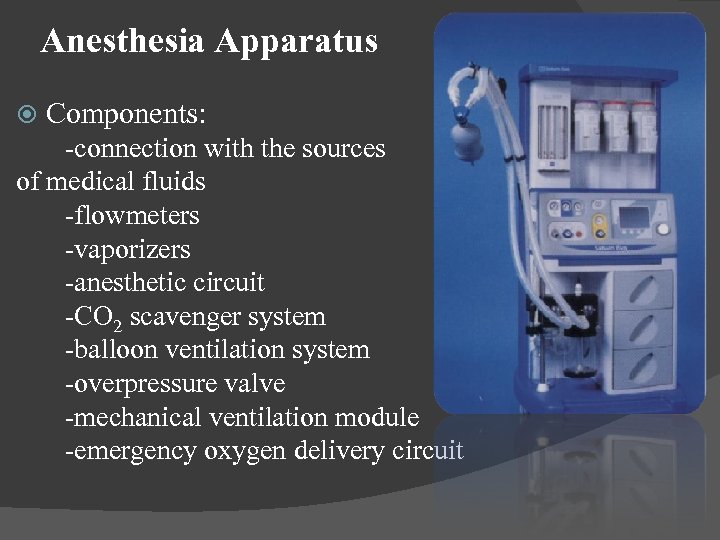
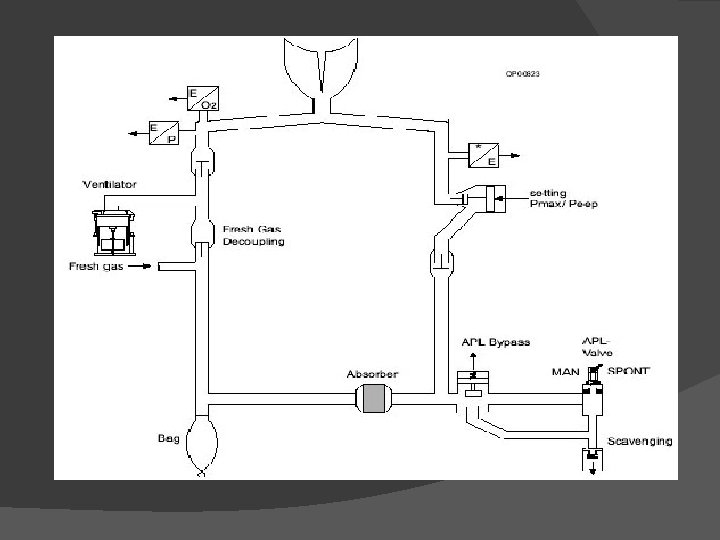
Anesthesia Apparatus Components: -connection with the sources of medical fluids -flowmeters -vaporizers -anesthetic circuit -CO 2 scavenger system -balloon ventilation system -overpressure valve -mechanical ventilation module -emergency oxygen delivery circuit
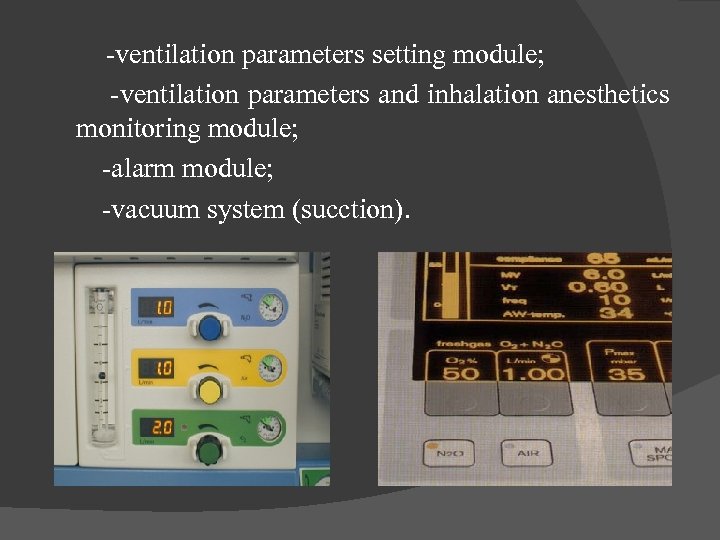
-ventilation parameters setting module; -ventilation parameters and inhalation anesthetics monitoring module; -alarm module; -vacuum system (sucction).
Intraanesthesic monitoring
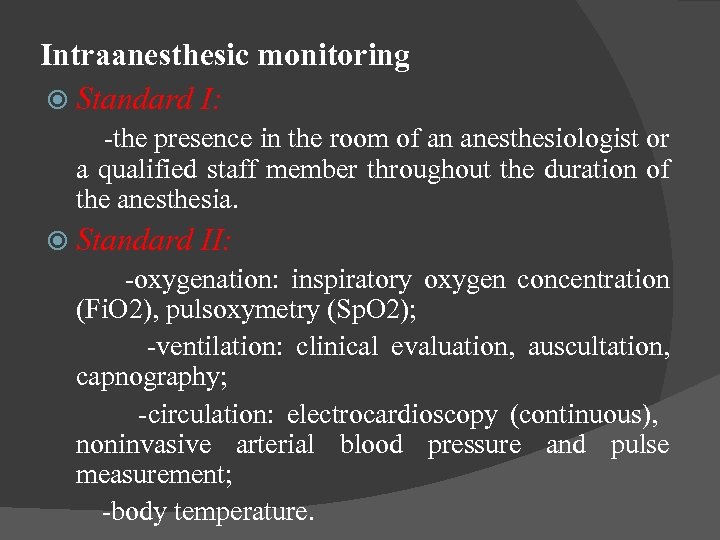
Intraanesthesic monitoring Standard I: -the presence in the room of an anesthesiologist or a qualified staff member throughout the duration of the anesthesia. Standard II: -oxygenation: inspiratory oxygen concentration (Fi. O 2), pulsoxymetry (Sp. O 2); -ventilation: clinical evaluation, auscultation, capnography; -circulation: electrocardioscopy (continuous), noninvasive arterial blood pressure and pulse measurement; -body temperature.
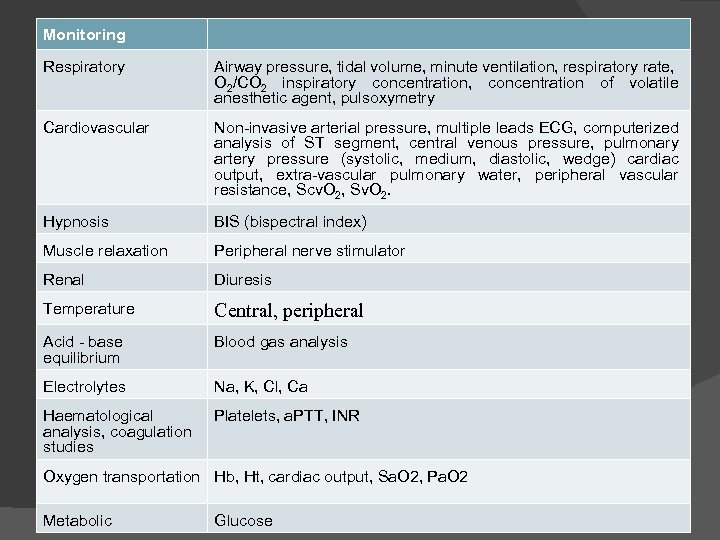
Monitoring Respiratory Airway pressure, tidal volume, minute ventilation, respiratory rate, O 2/CO 2 inspiratory concentration, concentration of volatile anesthetic agent, pulsoxymetry Cardiovascular Non-invasive arterial pressure, multiple leads ECG, computerized analysis of ST segment, central venous pressure, pulmonary artery pressure (systolic, medium, diastolic, wedge) cardiac output, extra-vascular pulmonary water, peripheral vascular resistance, Scv. O 2, Sv. O 2. Hypnosis BIS (bispectral index) Muscle relaxation Peripheral nerve stimulator Renal Diuresis Temperature Central, peripheral Acid - base equilibrium Blood gas analysis Electrolytes Na, K, Cl, Ca Haematological analysis, coagulation studies Platelets, a. PTT, INR Oxygen transportation Hb, Ht, cardiac output, Sa. O 2, Pa. O 2 Metabolic Glucose
Preanesthetic visit
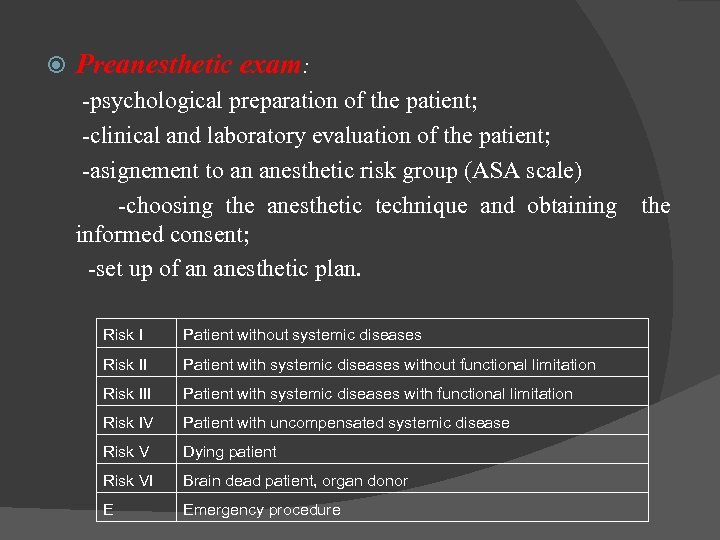
Preanesthetic exam: -psychological preparation of the patient; -clinical and laboratory evaluation of the patient; -asignement to an anesthetic risk group (ASA scale) -choosing the anesthetic technique and obtaining informed consent; -set up of an anesthetic plan. Risk I Patient without systemic diseases Risk II Patient with systemic diseases without functional limitation Risk III Patient with systemic diseases with functional limitation Risk IV Patient with uncompensated systemic disease Risk V Dying patient Risk VI Brain dead patient, organ donor E Emergency procedure the
Optimizing the patient status: -the correction of dysfunctions and diseases in the preoperative period. Premedication : -reduced anxiety and reduced need for intraoperative anesthetics; -decreasing certain risks (parasympathetic reflexes, the risk of aspiration); -the facilitation of postoperative analgesia.
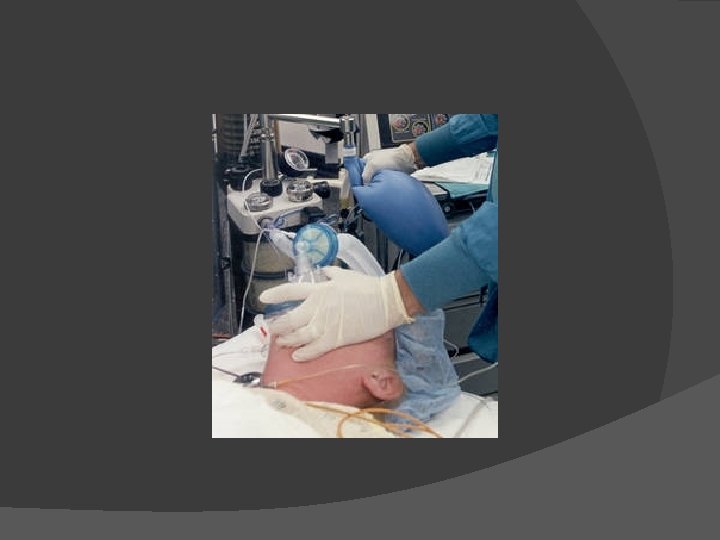
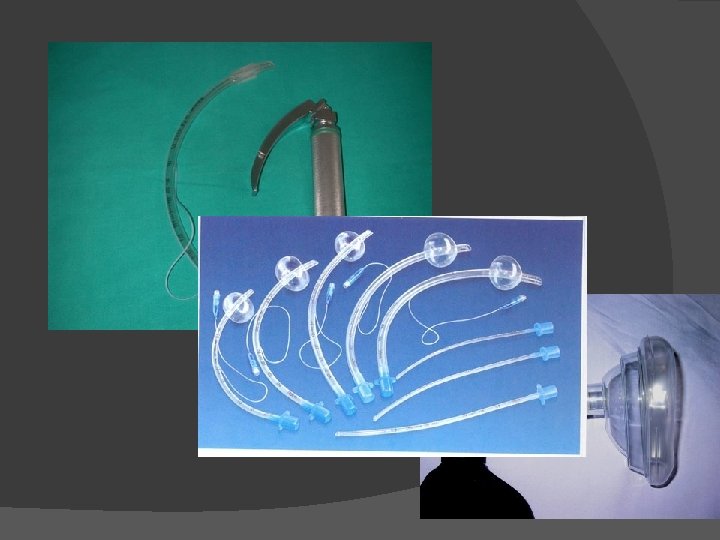
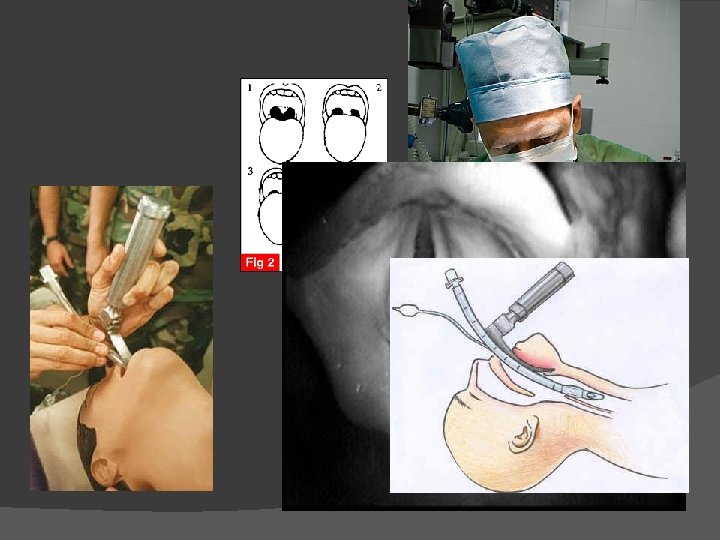
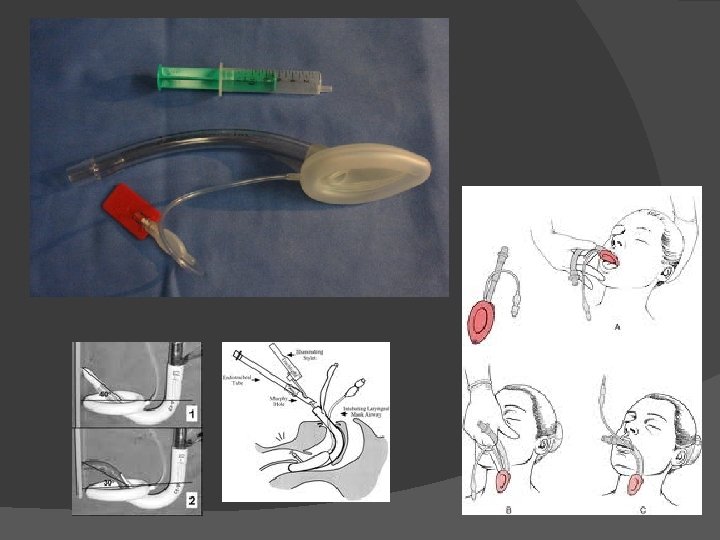
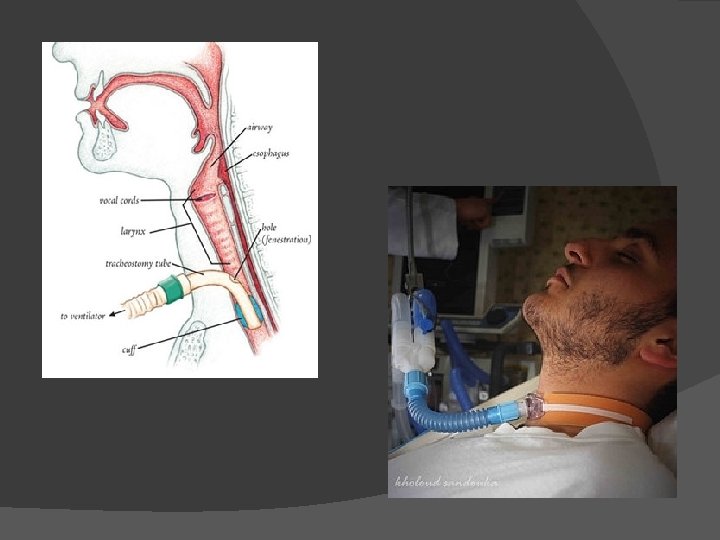
Phases of general anesthesia Induction phase: -the period of transition from the state of conscious to the state of general anesthesia; -CNS depression, ventilatory, cardiovascular depression, muscle relaxation; -securing the airway. Maintenace phase: -providing the adequate depth of anesthesia by administering anesthetics, analgesics and muscle relaxant agents. Emergency phase: -the interruption of the administration of all volatile or intravenous anesthetic agents; -the antagonisation of the muscle relaxant drug.


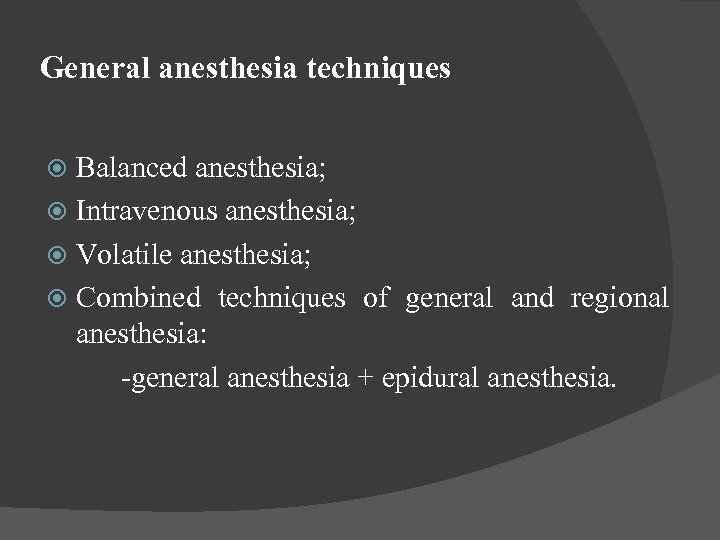
General anesthesia techniques Balanced anesthesia; Intravenous anesthesia; Volatile anesthesia; Combined techniques of general and regional anesthesia: -general anesthesia + epidural anesthesia.
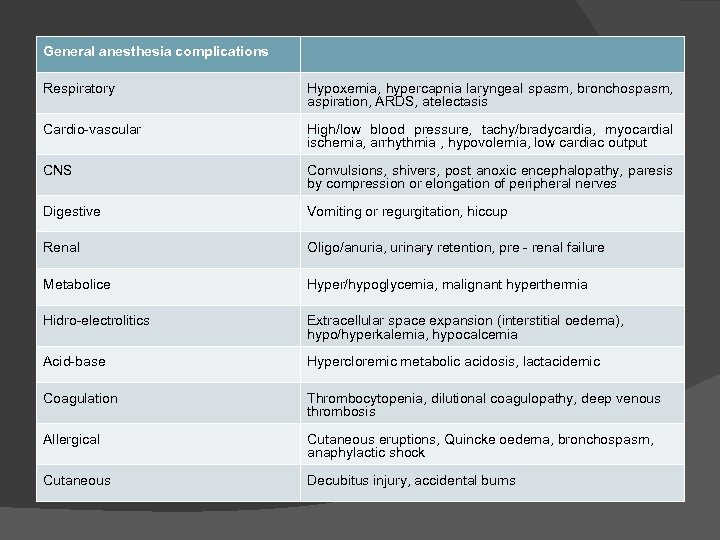
General anesthesia complications Respiratory Hypoxemia, hypercapnia laryngeal spasm, bronchospasm, aspiration, ARDS, atelectasis Cardio-vascular High/low blood pressure, tachy/bradycardia, myocardial ischemia, arrhythmia , hypovolemia, low cardiac output CNS Convulsions, shivers, post anoxic encephalopathy, paresis by compression or elongation of peripheral nerves Digestive Vomiting or regurgitation, hiccup Renal Oligo/anuria, urinary retention, pre - renal failure Metabolice Hyper/hypoglycemia, malignant hyperthermia Hidro-electrolitics Extracellular space expansion (interstitial oedema), hypo/hyperkalemia, hypocalcemia Acid-base Hypercloremic metabolic acidosis, lactacidemic Coagulation Thrombocytopenia, dilutional coagulopathy, deep venous thrombosis Allergical Cutaneous eruptions, Quincke oedema, bronchospasm, anaphylactic shock Cutaneous Decubitus injury, accidental burns
Regional anesthesia Subarachnoid (spinal) Epidural Sequential Caudal
Regional anesthesia Indications: -the area can be anesthetised using regional blocks; -the surgical procedure does not affect the vital functions; -patient's informed consent; Contraindications: -patient's refusal; -active coagulation disorders or anticoagulant treatment; -infections or haematoma at injection site; -neurological deficit and lack of cooperation.
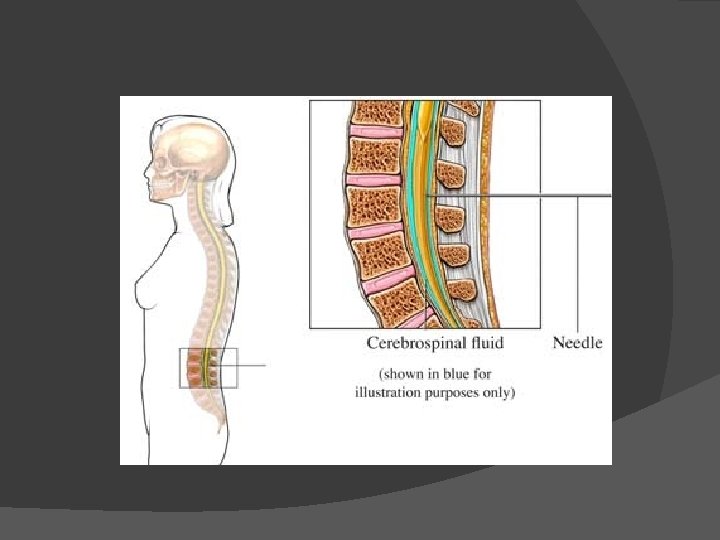
Spinal Anethesia: analgesia muscle relaxation sympathetic blockade -sympathetic blockade: hypotension, bradycardia, urinary retention; -hypovolemia is an absolute contraindication of spinal anesthesia; -epidural analgesia is the standard procedure for peripartum analgesia; -complications: systemic (high spred of anesthetictotal spinal anesthesia or systemic toxicity), headache.
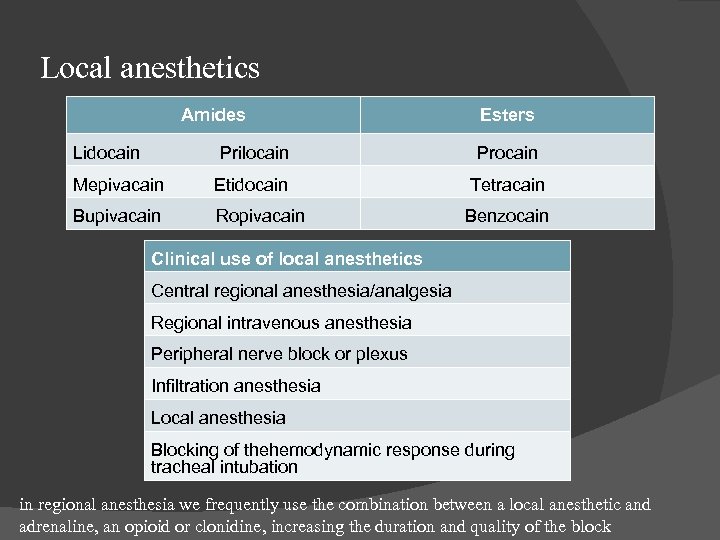
Local anesthetics Amides Lidocain Esters Prilocain Procain Mepivacain Etidocain Tetracain Bupivacain Ropivacain Benzocain Clinical use of local anesthetics Central regional anesthesia/analgesia Regional intravenous anesthesia Peripheral nerve block or plexus Infiltration anesthesia Local anesthesia Blocking of thehemodynamic response during tracheal intubation in regional anesthesia we frequently use the combination between a local anesthetic and adrenaline, an opioid or clonidine, increasing the duration and quality of the block
During regional anesthesia – mandatory equipments: Anesthesia delivery system Equipments and materials for airway management Oxygen source Monitoring: ventilation, oxygenation, circulation, blood pressure, EKG.
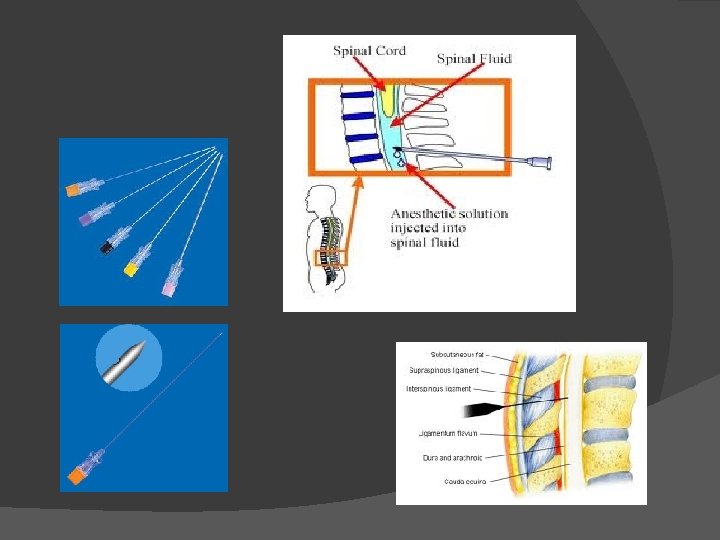
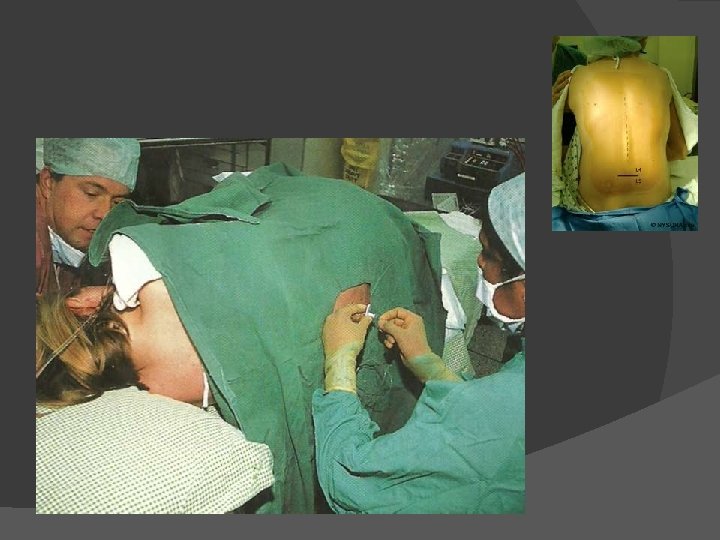
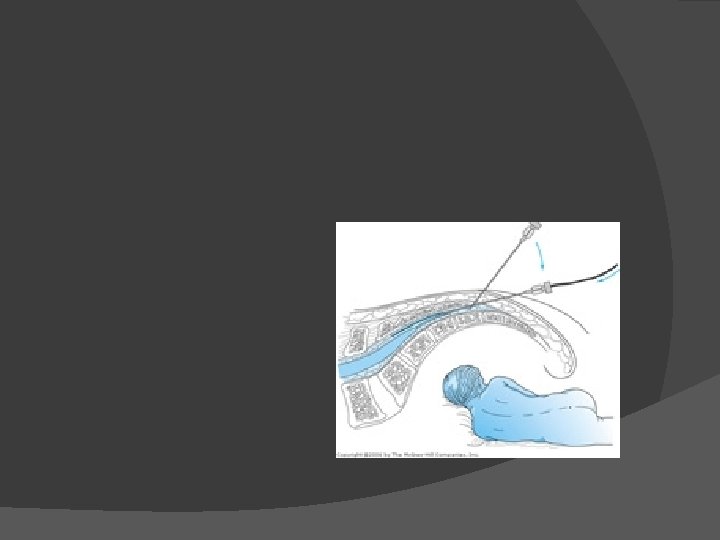
Spinal anesthesia (sub-arachnoid block)

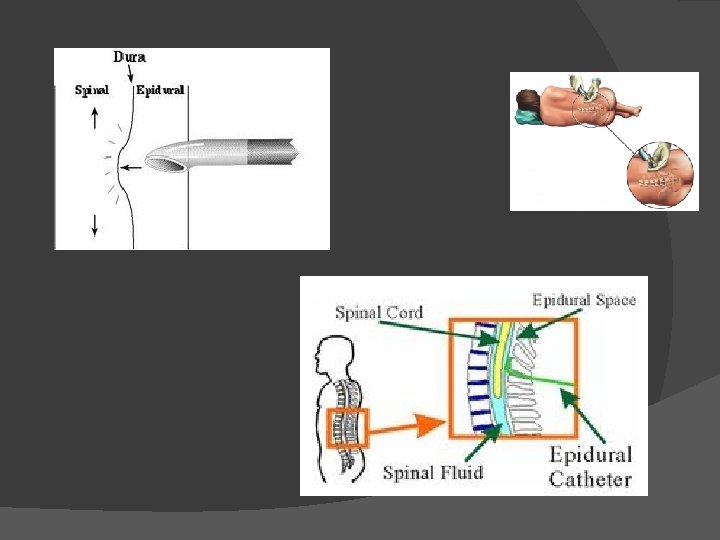
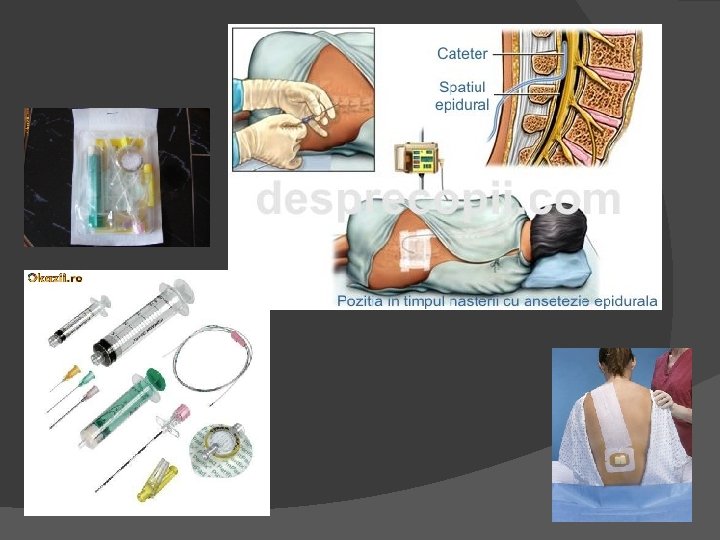
Epidural anesthesia
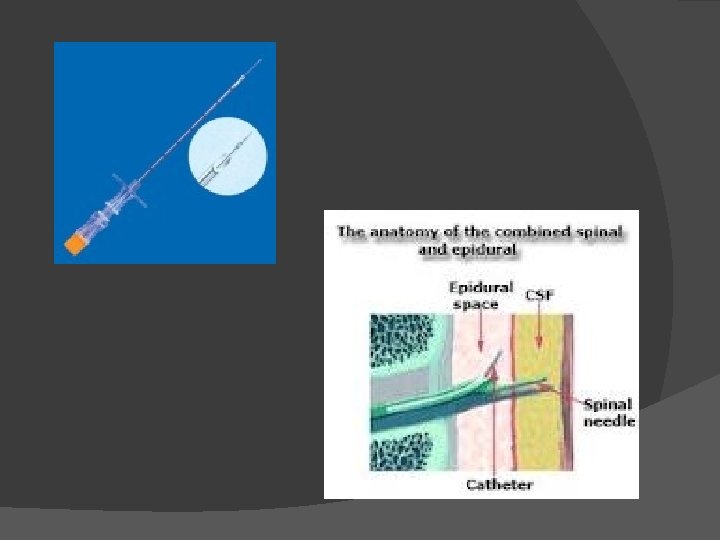
Sequential (combined) anesthesia spinal / epidural
Caudal anesthesia
Plexus anesthesia or peripheral nerves blockade Single-shot Catheter
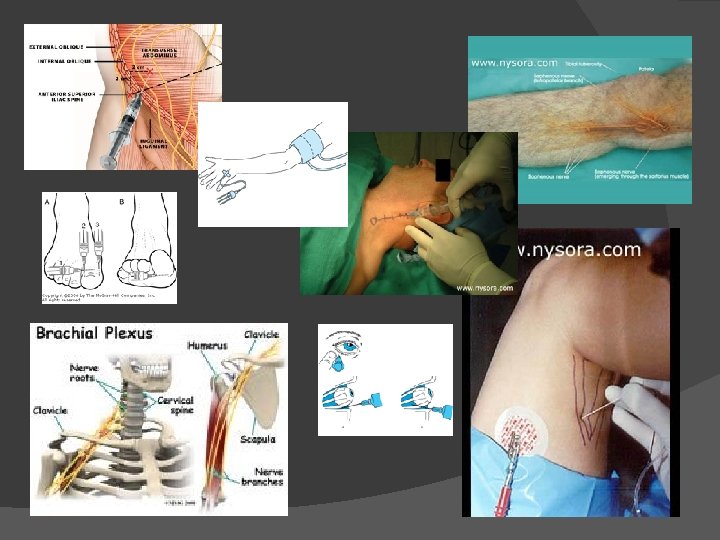
Local anesthesia contact topical - skin, mucous membrane application tissue infiltration
Monitored anesthesia care
Monitored anesthesia care - intravenous administration of anxiolytic, sedative, analgesic and amnesic drugs either isolated or supplementing a regional anesthesia procedure; - indicated in: painful diagnostic or therapeutic procedures or supplementing a inappropiate regional block; - the CPR equipments must be close-by at all times; - complications: respiratory depression with hypoventilation and loss of airway protection.

401a8e0f6ea72f79bee92036574d1860.ppt