0ef90cdd69d3c946e009359862343caf.ppt
- Количество слайдов: 47
 Anesthesia Monitoring in the Operating Room and ICU Dr. Mahmoud Al-mustafa
Anesthesia Monitoring in the Operating Room and ICU Dr. Mahmoud Al-mustafa
 Monitoring in the Past
Monitoring in the Past
 Monitoring in the Past n n n Visual monitoring of respiration and overall clinical appearance Finger on pulse Blood pressure (sometimes
Monitoring in the Past n n n Visual monitoring of respiration and overall clinical appearance Finger on pulse Blood pressure (sometimes
 ASA Monitoring Guidelines n STANDARD I Qualified anesthesia personnel shall be present in the room throughout the conduct of all general anesthetics, regional anesthetics and monitored anesthesia care.
ASA Monitoring Guidelines n STANDARD I Qualified anesthesia personnel shall be present in the room throughout the conduct of all general anesthetics, regional anesthetics and monitored anesthesia care.
 ASA Monitoring Guidelines n STANDARD II During all anesthetics, the patient’s oxygenation, ventilation, circulation and temperature shall be continually evaluated.
ASA Monitoring Guidelines n STANDARD II During all anesthetics, the patient’s oxygenation, ventilation, circulation and temperature shall be continually evaluated.
 Oxygenation Ensure adequate oxygen concentration in inspired gas and blood Methods § § § inspired gas oxygen analyzer with alarms (GA) pulse oximetry exposure to assess color
Oxygenation Ensure adequate oxygen concentration in inspired gas and blood Methods § § § inspired gas oxygen analyzer with alarms (GA) pulse oximetry exposure to assess color
 Pulse Oximetry q Theory § two wavelengths (660 and 960 nm) § calculates functional saturation (physiologic saturation) q Limitations § dyes or other hemoglobin species (carboxy, met, fetal, etc) § motion § low perfusion states § electrocautery § ambient light
Pulse Oximetry q Theory § two wavelengths (660 and 960 nm) § calculates functional saturation (physiologic saturation) q Limitations § dyes or other hemoglobin species (carboxy, met, fetal, etc) § motion § low perfusion states § electrocautery § ambient light
 Pulse Oximetry q Optical plethysmography § detects pulsatile changes in blood volume q Spectrophotometry § measures pulsatile hemoglobin saturation q Assumptions § all pulsation is arterial § light passes through pulsatile beds
Pulse Oximetry q Optical plethysmography § detects pulsatile changes in blood volume q Spectrophotometry § measures pulsatile hemoglobin saturation q Assumptions § all pulsation is arterial § light passes through pulsatile beds
 Ventilation n Objective n n ensure adequate ventilation of patient Methods qualitative clinical signs Ø Ø Ø chest excursion observation of reservoir bag auscultation of breath sounds quantitative measurement Ø Ø Ø end tidal carbon dioxide volume of expired gas continuous circuit disconnect monitor for mechanical ventilation
Ventilation n Objective n n ensure adequate ventilation of patient Methods qualitative clinical signs Ø Ø Ø chest excursion observation of reservoir bag auscultation of breath sounds quantitative measurement Ø Ø Ø end tidal carbon dioxide volume of expired gas continuous circuit disconnect monitor for mechanical ventilation
 Ventilation q General Anesthesia § qualitative clinical signs adequate § quantitative methods encouraged § endotracheal tube or laryngeal mask placement Ø § continual end tidal carbon dioxide identification continuous disconnect alarm mandatory during controlled ventilation q Regional Anesthesia and Monitored Anesthesia Care § continual qualitative clinical signs (minimum)
Ventilation q General Anesthesia § qualitative clinical signs adequate § quantitative methods encouraged § endotracheal tube or laryngeal mask placement Ø § continual end tidal carbon dioxide identification continuous disconnect alarm mandatory during controlled ventilation q Regional Anesthesia and Monitored Anesthesia Care § continual qualitative clinical signs (minimum)
 Capnography q Theory § main or sidestream sampling § several technical methods available q Applications § confirmation of intubation § monitoring for circuit disconnection § identification of airway obstruction § rebreathing/metabolic monitoring
Capnography q Theory § main or sidestream sampling § several technical methods available q Applications § confirmation of intubation § monitoring for circuit disconnection § identification of airway obstruction § rebreathing/metabolic monitoring
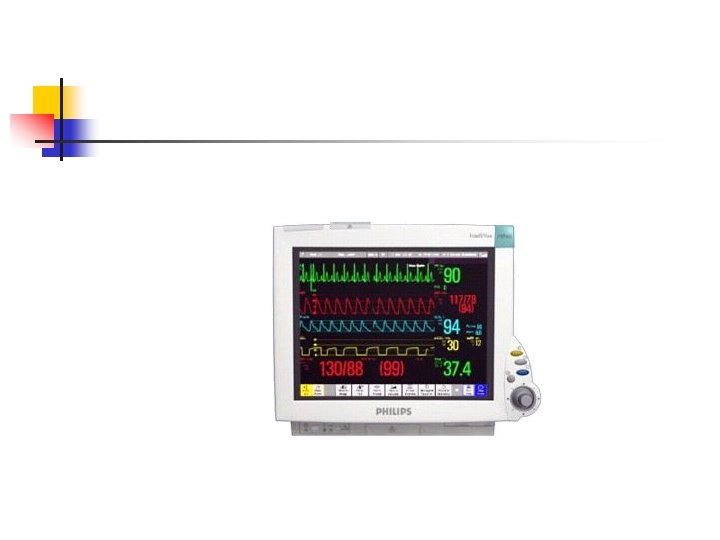
 Circulation q Objective § ensure adequacy of circulatory function q Methods § continuous electrocardiogram monitoring § arterial blood pressure and heart rate q 5 min § during GA one additional continual parameter
Circulation q Objective § ensure adequacy of circulatory function q Methods § continuous electrocardiogram monitoring § arterial blood pressure and heart rate q 5 min § during GA one additional continual parameter
 Temperature q Objective § aid in maintaining appropriate body temperature q Application § readily available method to continuously monitor temperature if changes are intended, anticipated or suspected q Methods § thermistor § temperature sensitive chemical reactions § location
Temperature q Objective § aid in maintaining appropriate body temperature q Application § readily available method to continuously monitor temperature if changes are intended, anticipated or suspected q Methods § thermistor § temperature sensitive chemical reactions § location
 Monitoring Temperature n n n Potential heat loss or risk of hyperthermia necessitates continuous temperature monitoring Normal heat loss during anesthesia averages 0. 5 - 1 C per hour, but usually not more that 2 - 3 C Temperature below 34 C may lead to significant morbidity
Monitoring Temperature n n n Potential heat loss or risk of hyperthermia necessitates continuous temperature monitoring Normal heat loss during anesthesia averages 0. 5 - 1 C per hour, but usually not more that 2 - 3 C Temperature below 34 C may lead to significant morbidity
 Monitoring Temperature n n n Hypothermia develops when thermoregulation fails to control balance of metabolic heat production and environment heat loss Normal response to heat loss is impaired during anesthesia Those at high risk are elderly, burn patients neonates, spinal cord injuries
Monitoring Temperature n n n Hypothermia develops when thermoregulation fails to control balance of metabolic heat production and environment heat loss Normal response to heat loss is impaired during anesthesia Those at high risk are elderly, burn patients neonates, spinal cord injuries
 Monitoring Temperature n n Hyperthermia Causes Malignant hyerthermia Endogenous pyrogens Excessive environmental warming Increases in metabolic rate secondary to: Thyrotoxicosis n Pheochromocytoma n
Monitoring Temperature n n Hyperthermia Causes Malignant hyerthermia Endogenous pyrogens Excessive environmental warming Increases in metabolic rate secondary to: Thyrotoxicosis n Pheochromocytoma n
 Monitoring Temperature Monitoring Sites n n n Tympanic Esophagus Bladder Rectum Blood (PA catheter) Skin
Monitoring Temperature Monitoring Sites n n n Tympanic Esophagus Bladder Rectum Blood (PA catheter) Skin
 Noninvasive Blood Pressure q Methodology § § § oscillometric algorithms automated reproducible q Limitations § cuff size Ø oversize erroneously low measurements Ø to small erroneously high
Noninvasive Blood Pressure q Methodology § § § oscillometric algorithms automated reproducible q Limitations § cuff size Ø oversize erroneously low measurements Ø to small erroneously high
 Electrocardiogram q 3 vs. 5 electrode system § three versus seven leads for diagnostic purposes q Heart rate measurement § R wave counting (any lead) q Ischemia Monitoring § lead II and V 5 are 90% sensitive § lead II, V 5 and V 4 up to 98% sensitive q Arrhythmia monitoring § lead II or esophageal for supraventricular arrhythmias § all leads for ventricular arrhythmias
Electrocardiogram q 3 vs. 5 electrode system § three versus seven leads for diagnostic purposes q Heart rate measurement § R wave counting (any lead) q Ischemia Monitoring § lead II and V 5 are 90% sensitive § lead II, V 5 and V 4 up to 98% sensitive q Arrhythmia monitoring § lead II or esophageal for supraventricular arrhythmias § all leads for ventricular arrhythmias
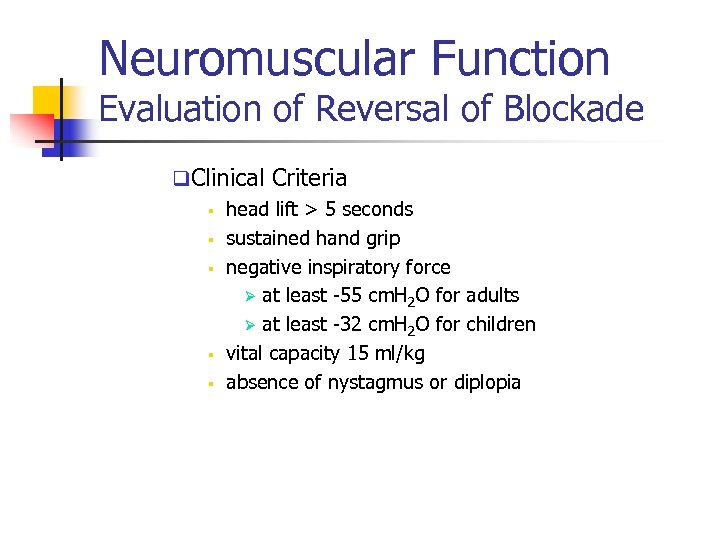 Neuromuscular Function Evaluation of Reversal of Blockade q. Clinical Criteria § head lift > 5 seconds § sustained hand grip § negative inspiratory force Ø at least -55 cm. H 2 O for adults Ø at least -32 cm. H 2 O for children § vital capacity 15 ml/kg § absence of nystagmus or diplopia
Neuromuscular Function Evaluation of Reversal of Blockade q. Clinical Criteria § head lift > 5 seconds § sustained hand grip § negative inspiratory force Ø at least -55 cm. H 2 O for adults Ø at least -32 cm. H 2 O for children § vital capacity 15 ml/kg § absence of nystagmus or diplopia
 Invasive monitoring n n n Arterial line Central venous pressure Pulmonary artery catheterization
Invasive monitoring n n n Arterial line Central venous pressure Pulmonary artery catheterization
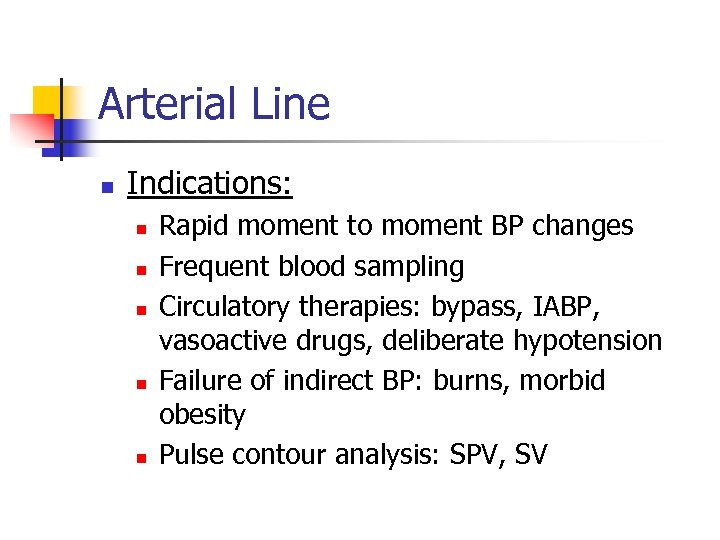 Arterial Line n Indications: n n n Rapid moment to moment BP changes Frequent blood sampling Circulatory therapies: bypass, IABP, vasoactive drugs, deliberate hypotension Failure of indirect BP: burns, morbid obesity Pulse contour analysis: SPV, SV
Arterial Line n Indications: n n n Rapid moment to moment BP changes Frequent blood sampling Circulatory therapies: bypass, IABP, vasoactive drugs, deliberate hypotension Failure of indirect BP: burns, morbid obesity Pulse contour analysis: SPV, SV
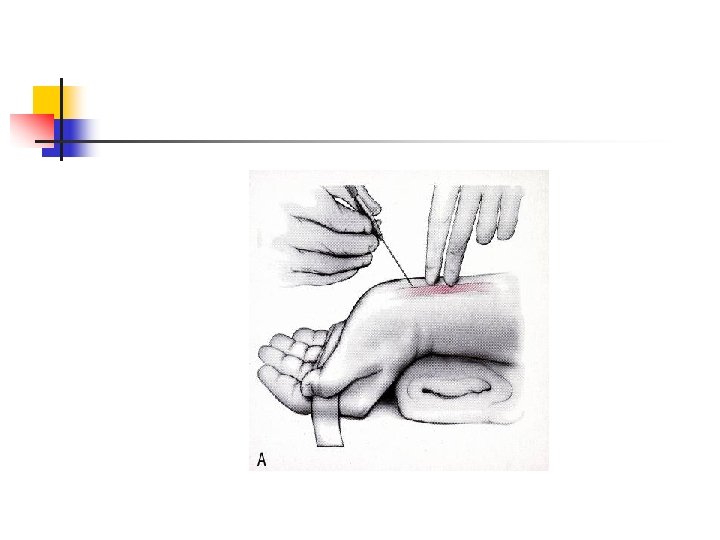
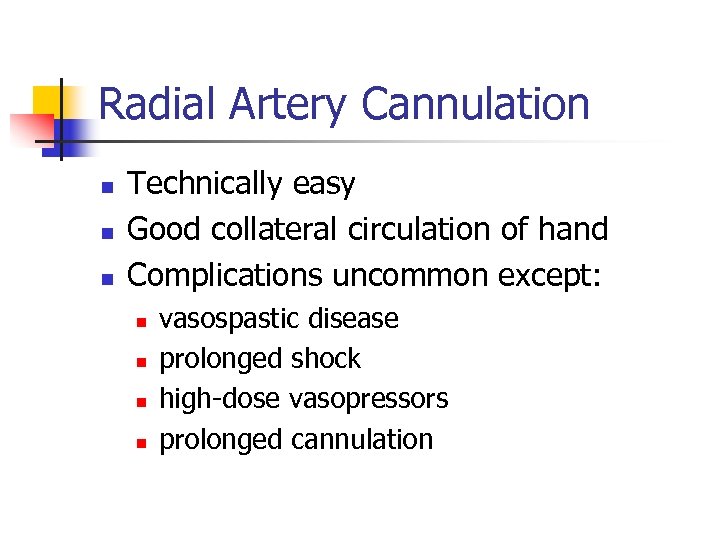 Radial Artery Cannulation n Technically easy Good collateral circulation of hand Complications uncommon except: n n vasospastic disease prolonged shock high-dose vasopressors prolonged cannulation
Radial Artery Cannulation n Technically easy Good collateral circulation of hand Complications uncommon except: n n vasospastic disease prolonged shock high-dose vasopressors prolonged cannulation
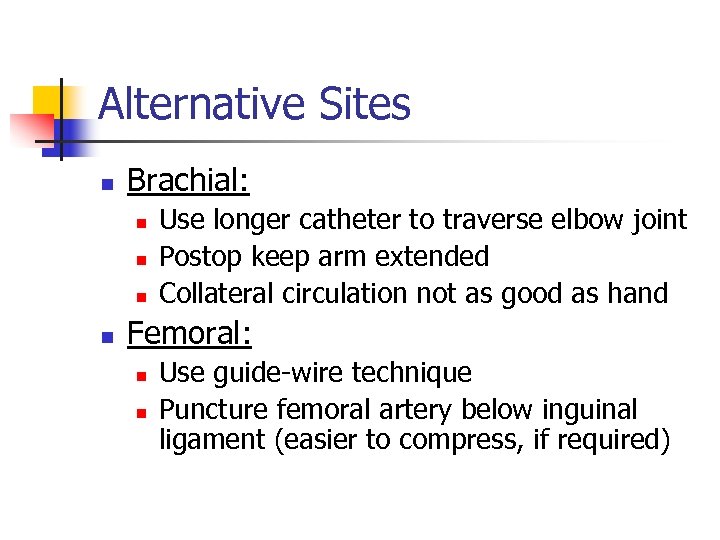 Alternative Sites n Brachial: n n Use longer catheter to traverse elbow joint Postop keep arm extended Collateral circulation not as good as hand Femoral: n n Use guide-wire technique Puncture femoral artery below inguinal ligament (easier to compress, if required)
Alternative Sites n Brachial: n n Use longer catheter to traverse elbow joint Postop keep arm extended Collateral circulation not as good as hand Femoral: n n Use guide-wire technique Puncture femoral artery below inguinal ligament (easier to compress, if required)
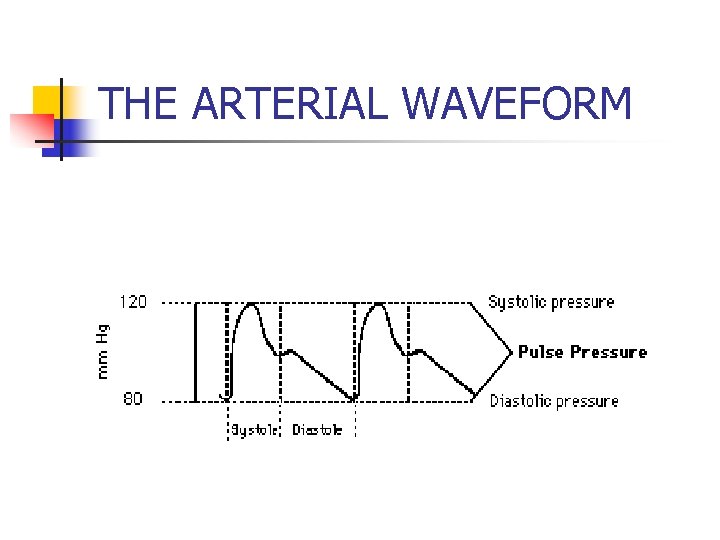 THE ARTERIAL WAVEFORM
THE ARTERIAL WAVEFORM
 Central Venous Line n Indications: n n n n CVP monitoring Advanced CV disease + major operation Secure vascular access for drugs: TLC Secure access for fluids: introducer sheath Aspiration of entrained air: sitting craniotomies Inadequate peripheral IV access Pacer, Swan Ganz
Central Venous Line n Indications: n n n n CVP monitoring Advanced CV disease + major operation Secure vascular access for drugs: TLC Secure access for fluids: introducer sheath Aspiration of entrained air: sitting craniotomies Inadequate peripheral IV access Pacer, Swan Ganz
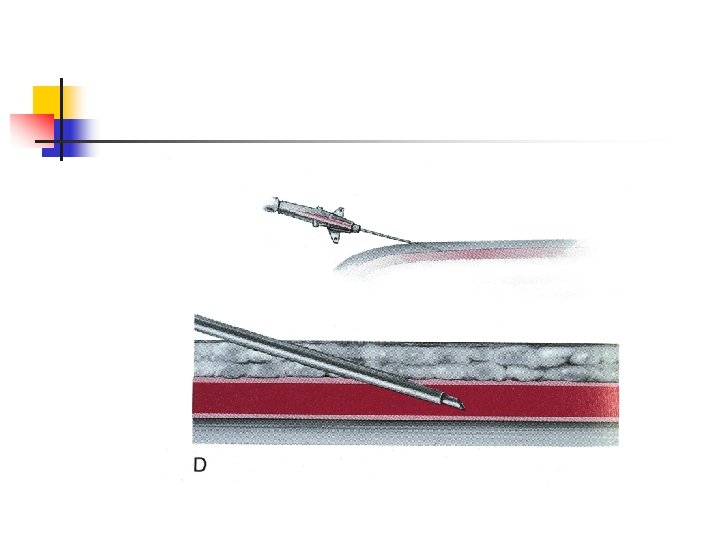
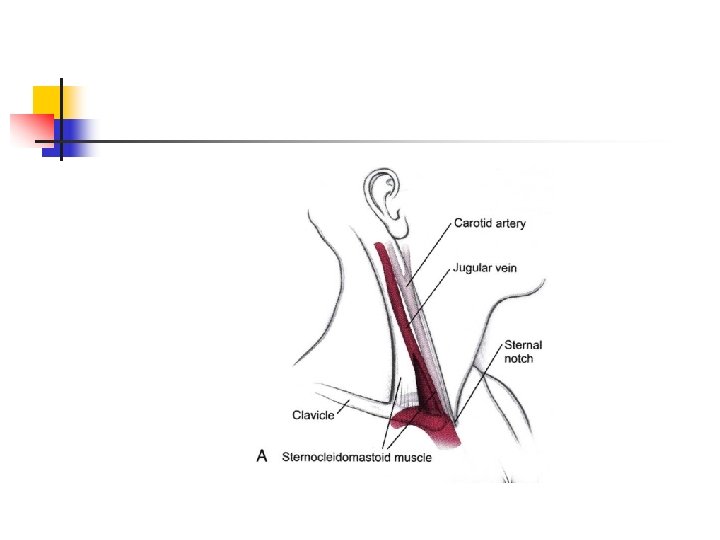
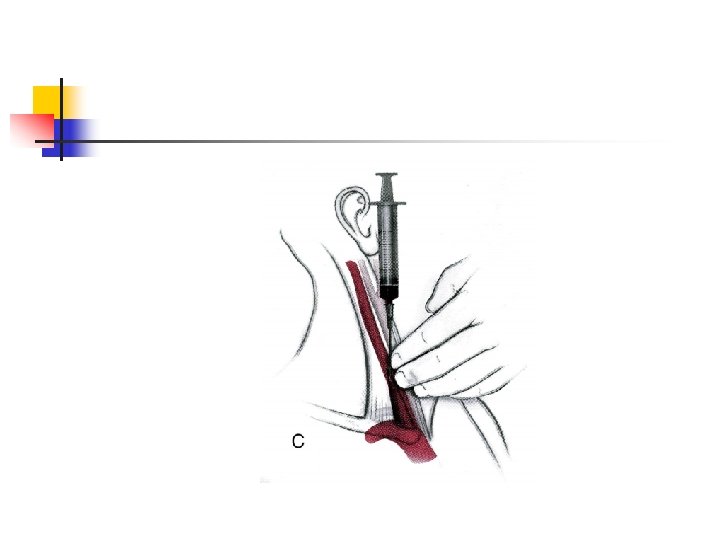
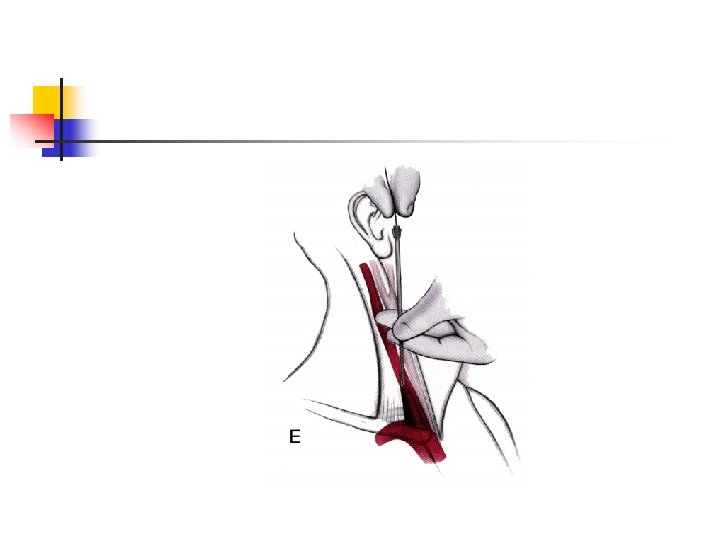
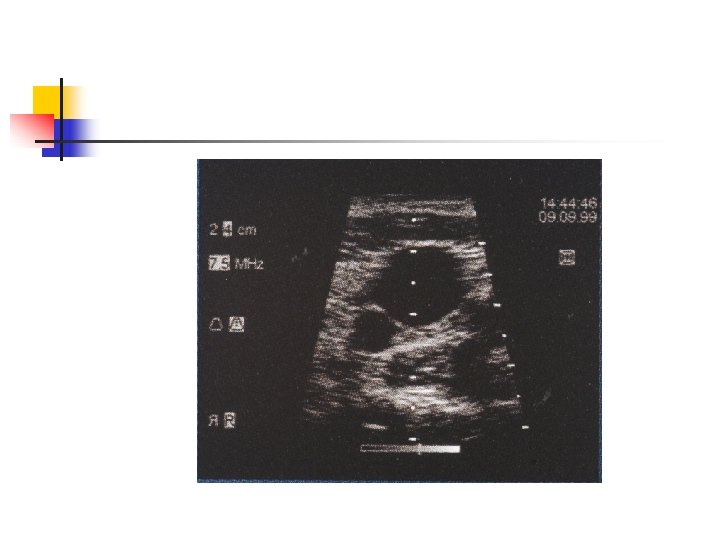
 Central Venous Line: RIJ n n n n IJ vein lies in groove between sternal + clavicular heads of sternocleidomastoid muscle IJ vein is lateral + slightly anterior to carotid Aseptic technique, head down Insert needle towards ipsilateral nipple Seldinger method: 22 G finder; 18 G needle, guidewire, scalpel blade, dilator + catheter Observe ECG + maintain control of guide-wire Ultrasound guidance; CXR post insertion
Central Venous Line: RIJ n n n n IJ vein lies in groove between sternal + clavicular heads of sternocleidomastoid muscle IJ vein is lateral + slightly anterior to carotid Aseptic technique, head down Insert needle towards ipsilateral nipple Seldinger method: 22 G finder; 18 G needle, guidewire, scalpel blade, dilator + catheter Observe ECG + maintain control of guide-wire Ultrasound guidance; CXR post insertion
 Advantages of RIJ n n n Consistent, predictable anatomic location Readily identifiable landmarks Short straight course to SVC Easy intraop access for anesthesiologist at patient’s head High success rate, 90 -99%
Advantages of RIJ n n n Consistent, predictable anatomic location Readily identifiable landmarks Short straight course to SVC Easy intraop access for anesthesiologist at patient’s head High success rate, 90 -99%
 Types of Central Catheters n n Variety of lengths, gauges, composition + lumens depending on purpose Introducer sheath (8 -8. 5 Fr): n Permits rapid fluid/blood infusion or Swan Trauma triple-lumen (12 Fr): n Rapid infusion via 12 g x 2; 16 g for CVP monitoring MAC 2: (9 Fr): n Rapid infusion via distal port; 12 g for CVP n Also allows for Swan insertion n More septations + stiffer plastic
Types of Central Catheters n n Variety of lengths, gauges, composition + lumens depending on purpose Introducer sheath (8 -8. 5 Fr): n Permits rapid fluid/blood infusion or Swan Trauma triple-lumen (12 Fr): n Rapid infusion via 12 g x 2; 16 g for CVP monitoring MAC 2: (9 Fr): n Rapid infusion via distal port; 12 g for CVP n Also allows for Swan insertion n More septations + stiffer plastic
 Alternative Sites n Subclavian: n n External jugular: n n n Easier to insert v. IJ if c-spine precautions Better patient comfort v. IJ Risk of pneumo- 2% Easy to cannulate if visible, no risk of pneumo 20%: cannot access central circulation Double cannulation of same vein (RIJ) n Serious complications: vein avulsion, catheter entanglement, catheter fracture
Alternative Sites n Subclavian: n n External jugular: n n n Easier to insert v. IJ if c-spine precautions Better patient comfort v. IJ Risk of pneumo- 2% Easy to cannulate if visible, no risk of pneumo 20%: cannot access central circulation Double cannulation of same vein (RIJ) n Serious complications: vein avulsion, catheter entanglement, catheter fracture
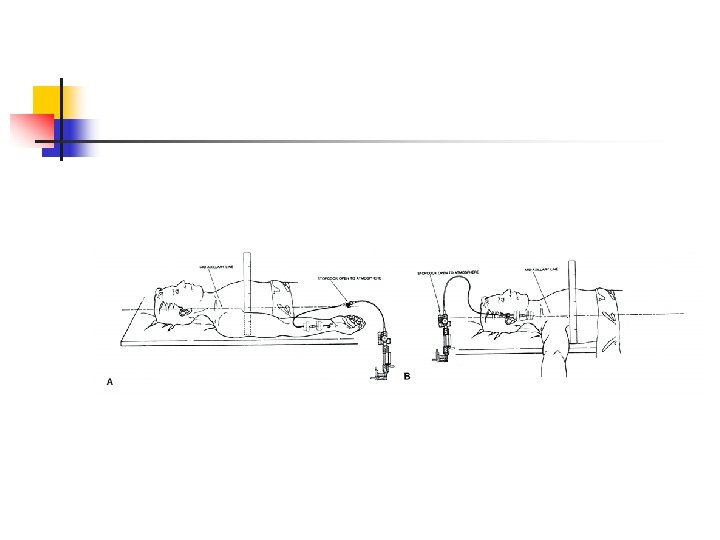
 CVP Monitoring n n n Reflects pressure at junction of vena cava + RA CVP is driving force for filling RA + RV CVP provides estimate of: n Intravascular blood volume n RV preload Trends in CVP are very useful Measure at end-expiration Zero at mid-axillary line
CVP Monitoring n n n Reflects pressure at junction of vena cava + RA CVP is driving force for filling RA + RV CVP provides estimate of: n Intravascular blood volume n RV preload Trends in CVP are very useful Measure at end-expiration Zero at mid-axillary line
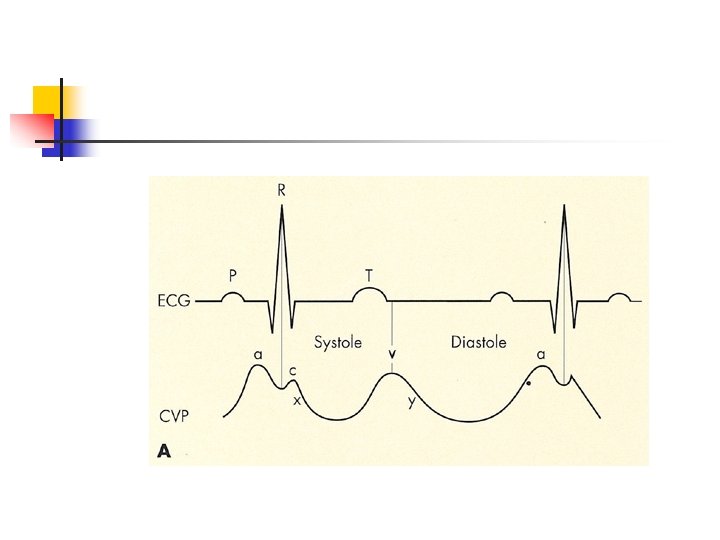
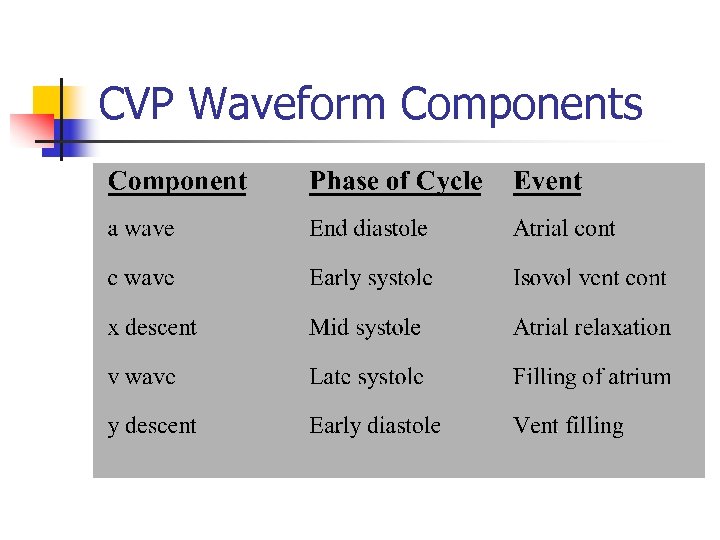 CVP Waveform Components
CVP Waveform Components
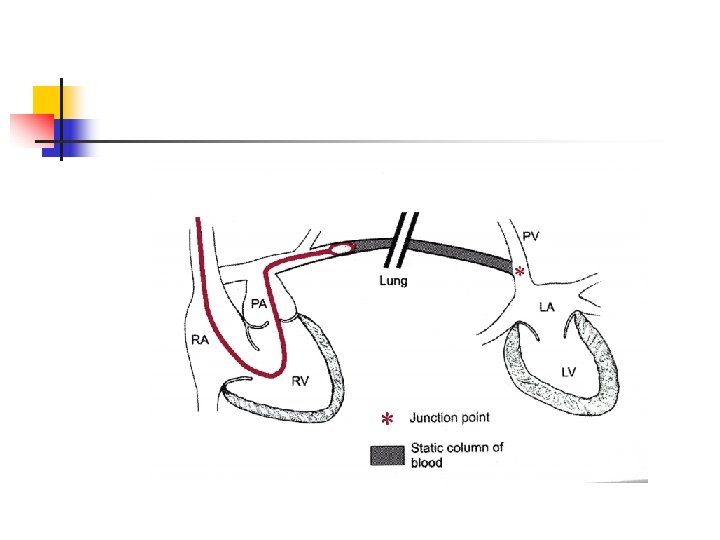
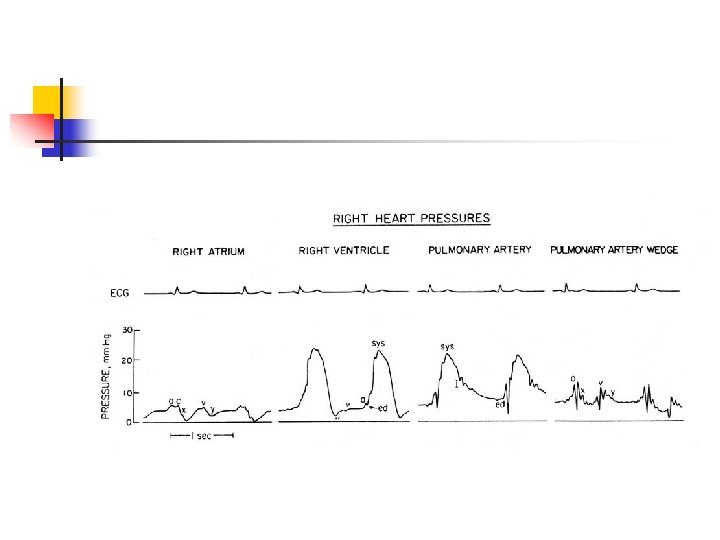
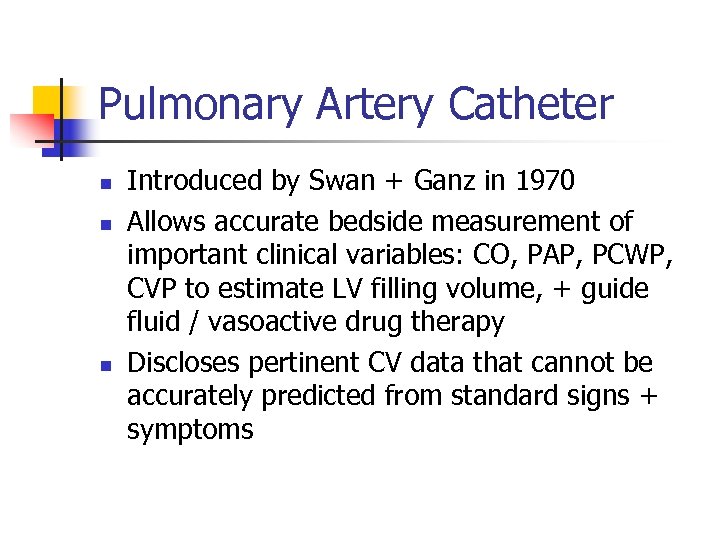 Pulmonary Artery Catheter n n n Introduced by Swan + Ganz in 1970 Allows accurate bedside measurement of important clinical variables: CO, PAP, PCWP, CVP to estimate LV filling volume, + guide fluid / vasoactive drug therapy Discloses pertinent CV data that cannot be accurately predicted from standard signs + symptoms
Pulmonary Artery Catheter n n n Introduced by Swan + Ganz in 1970 Allows accurate bedside measurement of important clinical variables: CO, PAP, PCWP, CVP to estimate LV filling volume, + guide fluid / vasoactive drug therapy Discloses pertinent CV data that cannot be accurately predicted from standard signs + symptoms
 Complications n n n Minor in 50%, e. g. , arrhythmias Transient RBBB- 0. 9 -5% n External pacer if pre-existing LBBB Misinformation Serious: 0. 1 -0. 5%: knotting, pulmonary infarction, PA rupture (e. g. , overwedge), endocarditis, structural heart damage Death: 0. 016%
Complications n n n Minor in 50%, e. g. , arrhythmias Transient RBBB- 0. 9 -5% n External pacer if pre-existing LBBB Misinformation Serious: 0. 1 -0. 5%: knotting, pulmonary infarction, PA rupture (e. g. , overwedge), endocarditis, structural heart damage Death: 0. 016%
 Summary n Invasive monitoring routinely performed n n n Permits improved understanding of BP, blood flow, + CV function Allows timely detection of hemodynamic events + initiation of treatment Requires correct technique + interpretation Complications occur from variety of reasons Risk: benefit ratio usually favorable in critically ill patients
Summary n Invasive monitoring routinely performed n n n Permits improved understanding of BP, blood flow, + CV function Allows timely detection of hemodynamic events + initiation of treatment Requires correct technique + interpretation Complications occur from variety of reasons Risk: benefit ratio usually favorable in critically ill patients
 Thank you
Thank you


