b4f8a8af7b2a99837a99ad5441ba0ad4.ppt
- Количество слайдов: 44
Anemia, Thrombocytopenia, & Blood Transfusions Joel Saltzman MD Hematology/Oncology Fellow Metro Health Medical Center
Objectives • An overview and approach to the anemic patient. • An overview and approach to the thrombocytopenic patient • An overview of blood transfusions with an evidence based approach
Anemia • A reduction below normal in the concentration of hemoglobin or red blood cells in the blood. • Hematocrit (<40% in men, <36% in women) • Hemoglobin (13. 2 g/dl in men, 11. 7 g/dl in women)
Symptoms of Anemia • Nonspecific and reflect tissue hypoxia: – Fatigue – Dyspnea on exertion – Palpatations – Headache – Confusion, decreased mental acuity – Skin pallor
History and Physical in Anemia • Duration and onset of symptoms • Change in stool habits: Stool Guaiacs in all • Splenomegaly? • Jaundiced?
Components of Oxygen Delivery • Hemoglobin in red cells • Respiration (Hemoglobin levels increase in hypoxic conditions) • Circulation (rate increases with anemia)
Classification of Anemia Kinetic classification • • Hypoproliferative Ineffective Erythropoiesis Hemolysis Bleeding Morphologic classification • • • Microcytic Macrocytic Normocytic
Anemia: A Kinetic Perspective • Erythrocytes in circulation represent a dynamic equilibrium between production and destruction of red cells • In response to acute anemia (ie blood loss) the healthy marrow is capable of producing erythrocytes 6 -8 times the normal rate (mediated through erythropoietin)
Reticulocyte Count • Is required in the evaluation of all patients with anemia as it is a simple measure of production • Young RBC that still contains a small amount of RNA • Normally take 1 day for reticulocyte to mature. Under influence of epo takes 2 -3 days • 1/120 th of RBC normally
Absolute Retic count • Retic counts are reported as a percentage: RBC count x Retic % = Absoulte retic count(normal: 4060, 000/μl 3) • Absolute Retic counts need to be corrected for early release ( If polychromasia is present) • Absolute retic/2 (for hct in mid 20’s) • Absolute retic/3 (hct <20)
Indirect Bilirubin: a marker of RBC destruction • 80% of normal Bilirubin production is a result of the degradation of hemoglobin • In the absence of liver disease Indirect Bilirubin is an excellent indicator of RBC destruction • LDH and Haptoglobin are other markers
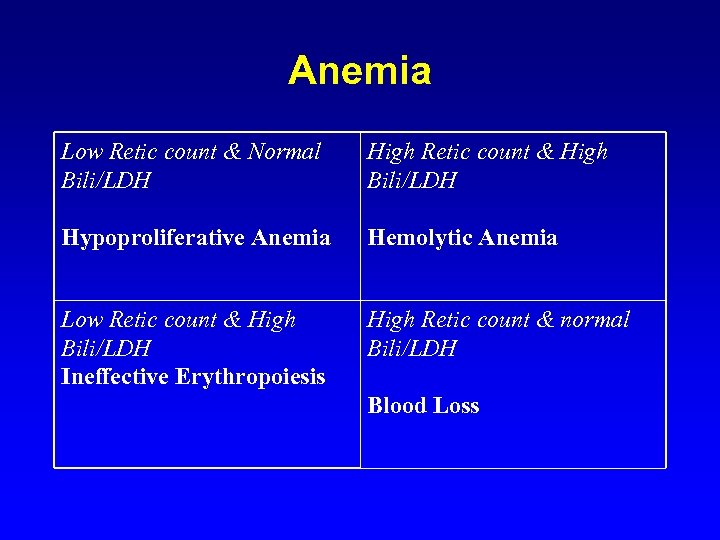
Anemia Low Retic count & Normal Bili/LDH High Retic count & High Bili/LDH Hypoproliferative Anemia Hemolytic Anemia Low Retic count & High Bili/LDH Ineffective Erythropoiesis High Retic count & normal Bili/LDH Blood Loss
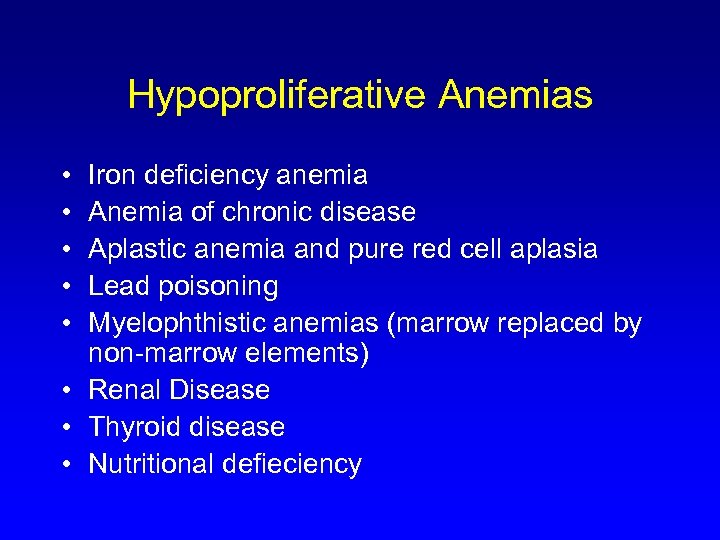
Hypoproliferative Anemias • • • Iron deficiency anemia Anemia of chronic disease Aplastic anemia and pure red cell aplasia Lead poisoning Myelophthistic anemias (marrow replaced by non-marrow elements) • Renal Disease • Thyroid disease • Nutritional defieciency
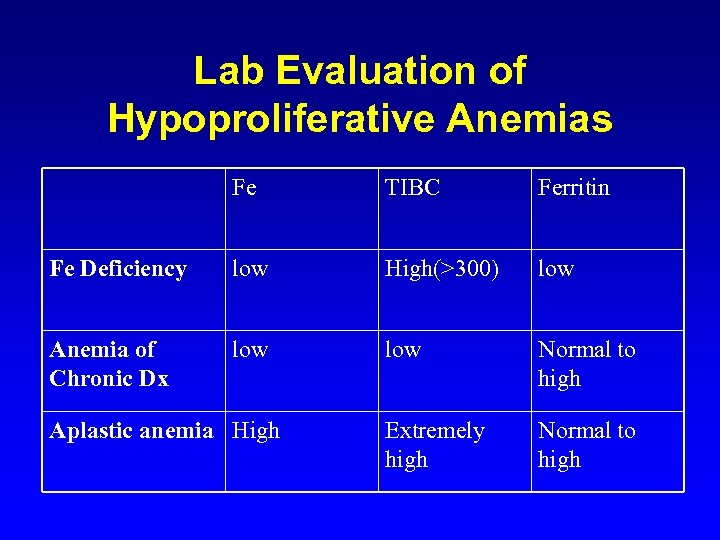
Lab Evaluation of Hypoproliferative Anemias Fe TIBC Ferritin Fe Deficiency low High(>300) low Anemia of Chronic Dx low Normal to high Extremely high Normal to high Aplastic anemia High
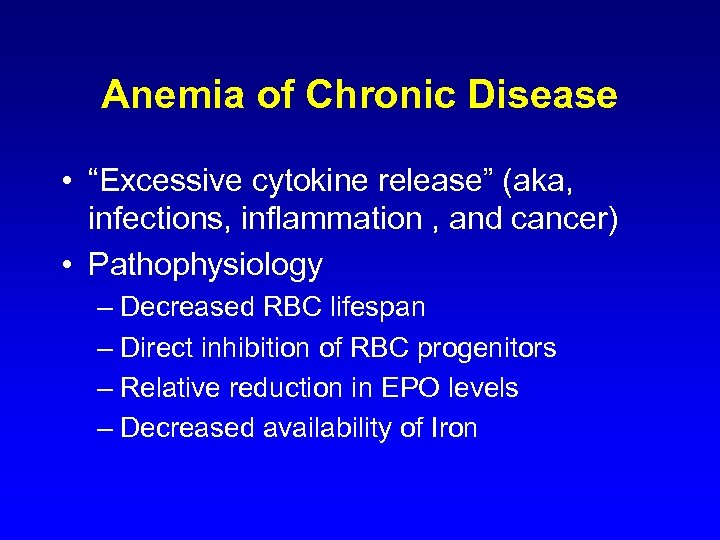
Anemia of Chronic Disease • “Excessive cytokine release” (aka, infections, inflammation , and cancer) • Pathophysiology – Decreased RBC lifespan – Direct inhibition of RBC progenitors – Relative reduction in EPO levels – Decreased availability of Iron
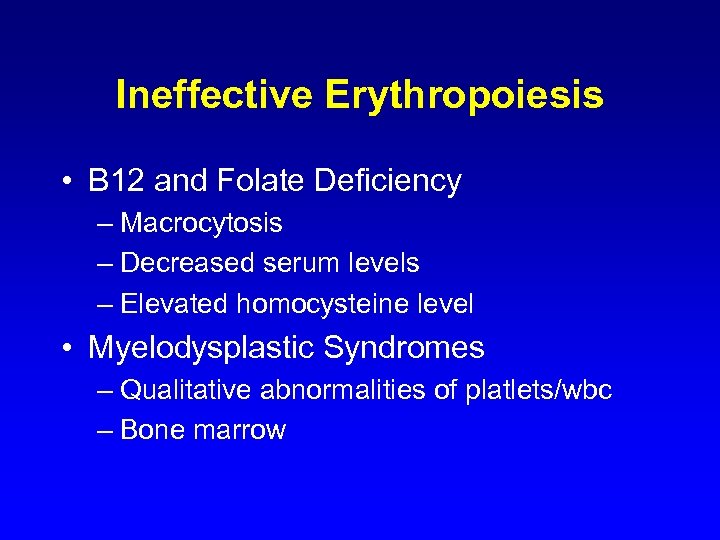
Ineffective Erythropoiesis • B 12 and Folate Deficiency – Macrocytosis – Decreased serum levels – Elevated homocysteine level • Myelodysplastic Syndromes – Qualitative abnormalities of platlets/wbc – Bone marrow
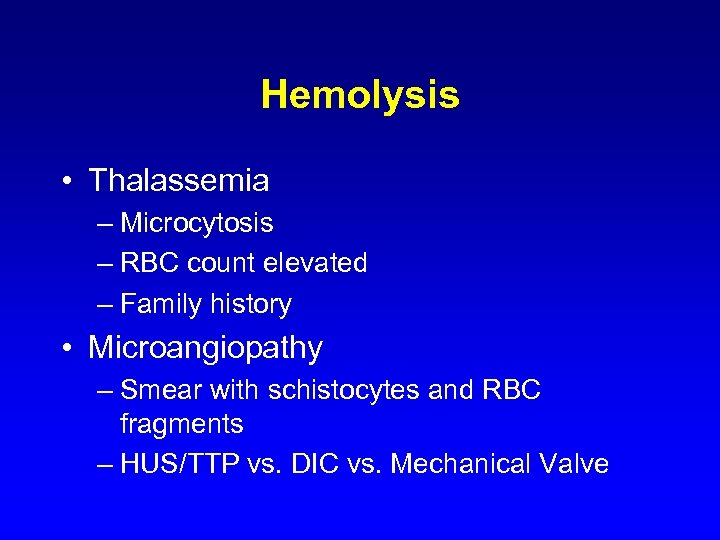
Hemolysis • Thalassemia – Microcytosis – RBC count elevated – Family history • Microangiopathy – Smear with schistocytes and RBC fragments – HUS/TTP vs. DIC vs. Mechanical Valve
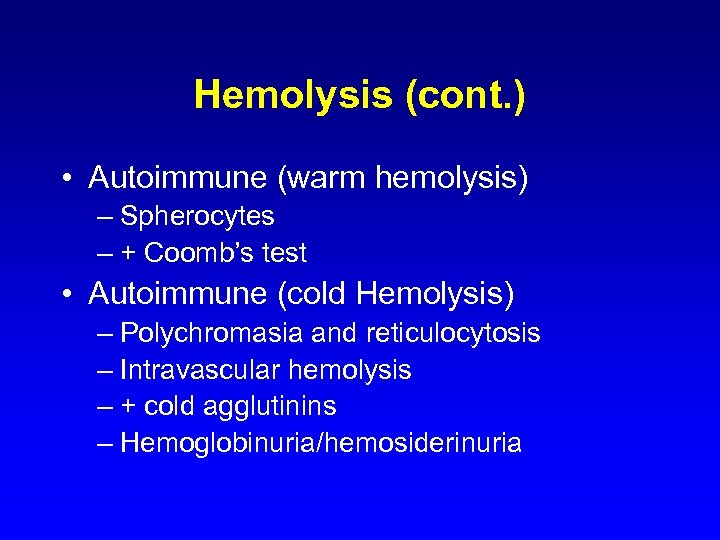
Hemolysis (cont. ) • Autoimmune (warm hemolysis) – Spherocytes – + Coomb’s test • Autoimmune (cold Hemolysis) – Polychromasia and reticulocytosis – Intravascular hemolysis – + cold agglutinins – Hemoglobinuria/hemosiderinuria
Bleeding • Labs directed at site of bleeding and clinical situation
RBC Transfusion • What is the best strategy for transfusion in a hospitalized patient population? • Is a liberal strategy better than a restrictive strategy in the critically ill patients? • What are the risks of transfusion?
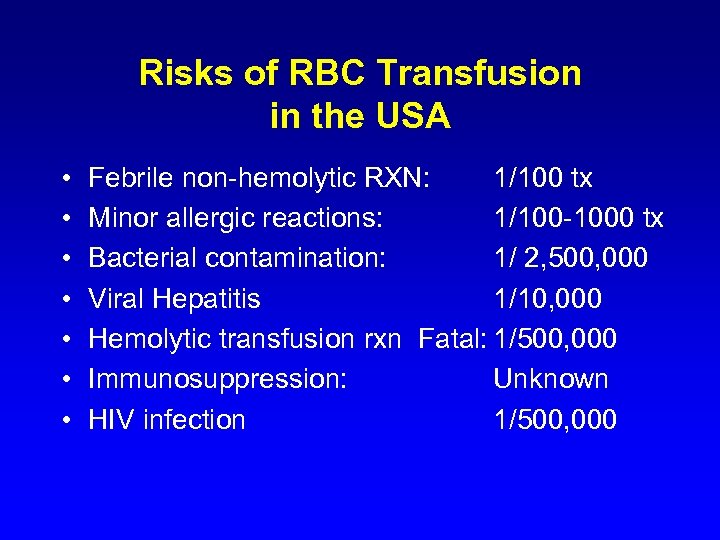
Risks of RBC Transfusion in the USA • • Febrile non-hemolytic RXN: 1/100 tx Minor allergic reactions: 1/100 -1000 tx Bacterial contamination: 1/ 2, 500, 000 Viral Hepatitis 1/10, 000 Hemolytic transfusion rxn Fatal: 1/500, 000 Immunosuppression: Unknown HIV infection 1/500, 000
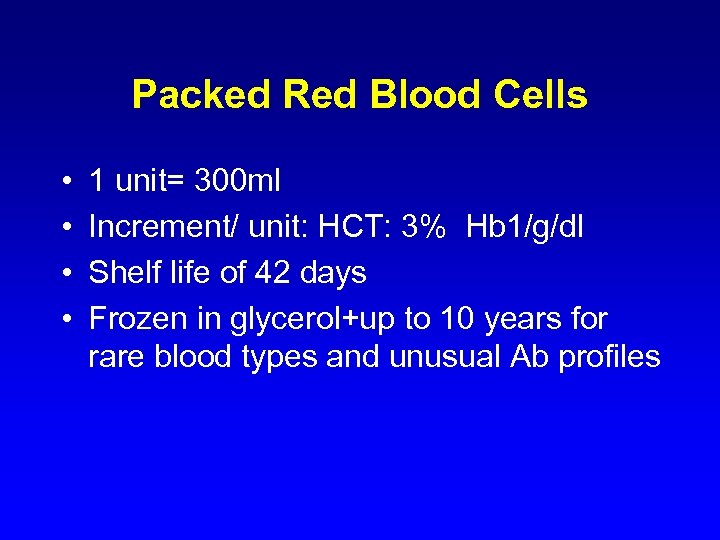
Packed Red Blood Cells • • 1 unit= 300 ml Increment/ unit: HCT: 3% Hb 1/g/dl Shelf life of 42 days Frozen in glycerol+up to 10 years for rare blood types and unusual Ab profiles
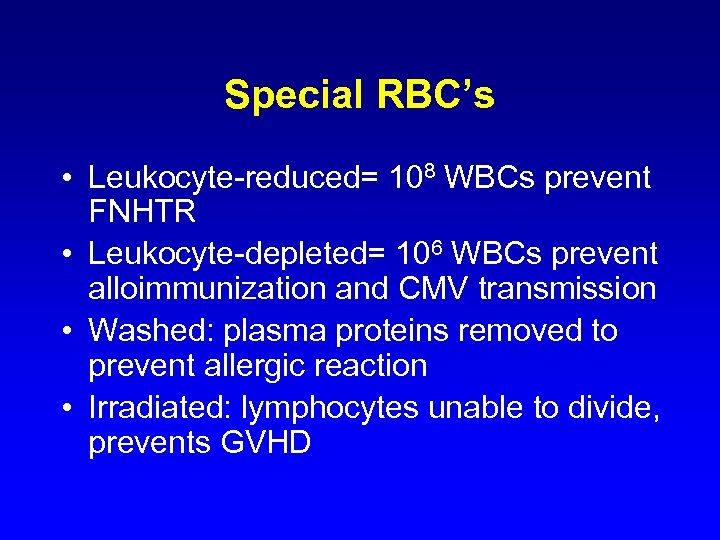
Special RBC’s • Leukocyte-reduced= 108 WBCs prevent FNHTR • Leukocyte-depleted= 106 WBCs prevent alloimmunization and CMV transmission • Washed: plasma proteins removed to prevent allergic reaction • Irradiated: lymphocytes unable to divide, prevents GVHD
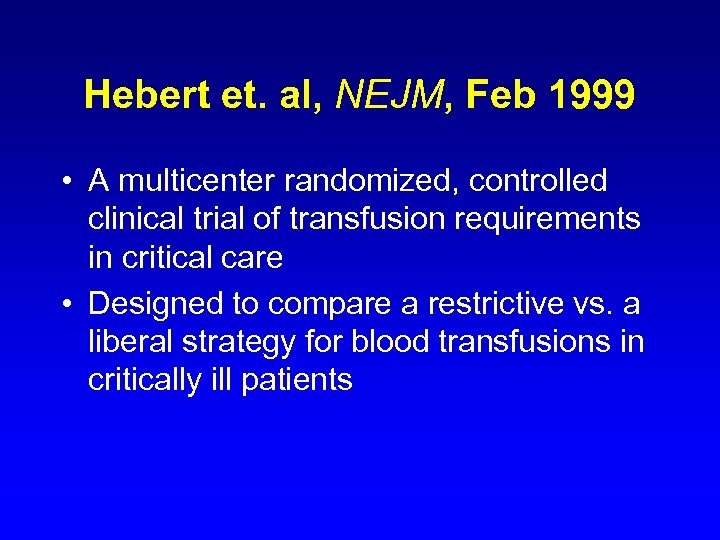
Hebert et. al, NEJM, Feb 1999 • A multicenter randomized, controlled clinical trial of transfusion requirements in critical care • Designed to compare a restrictive vs. a liberal strategy for blood transfusions in critically ill patients
Methods: Hebert et. al • 838 patients with euvolemia after initial treatment who had hemoglobin concentrations < 9. 0 g/dl within 72 hours of admission were enrolled • 418 pts: Restrictive arm: transfused for hb<7. 0 • 420 pts: Liberal arm: transfused for Hb< 10. 0
Exclusion Criteria • • Age <16 Inability to receive blood products Active blood loss at time of enrollment Chronic anemia: hb< 9. 0 in preceding month • Routine cardiac surgery patients
Study population • 6451 were assessed for eligibility • Consent rate was 41% • No significant differences were noted between the two groups • Average apache score was 21(hospital mortality of 40% for nonoperative patients or 29% for post-op pts)
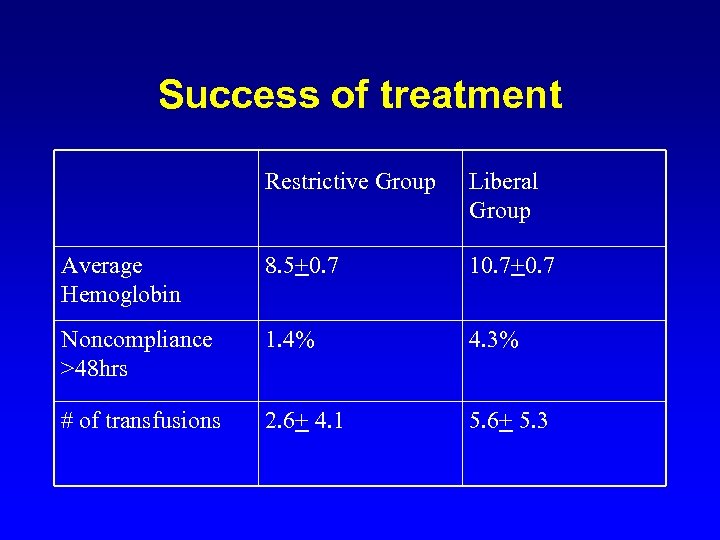
Success of treatment Restrictive Group Liberal Group Average Hemoglobin 8. 5+0. 7 10. 7+0. 7 Noncompliance >48 hrs 1. 4% 4. 3% # of transfusions 2. 6+ 4. 1 5. 6+ 5. 3
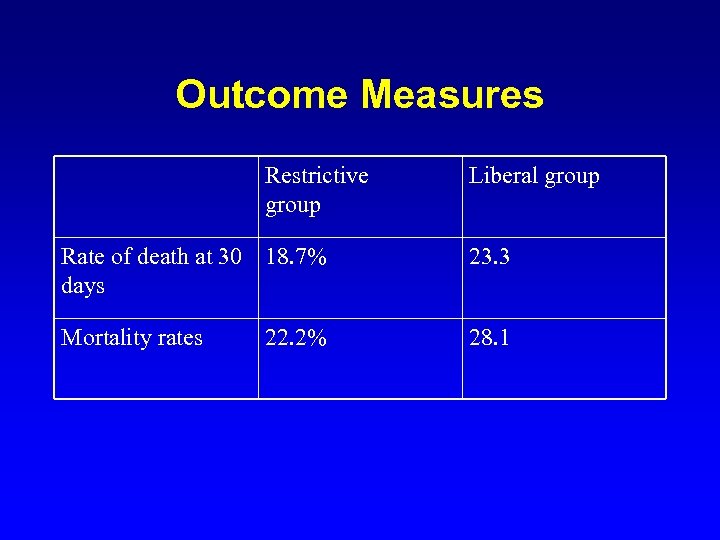
Outcome Measures Restrictive group Liberal group Rate of death at 30 18. 7% days 23. 3 Mortality rates 28. 1 22. 2%
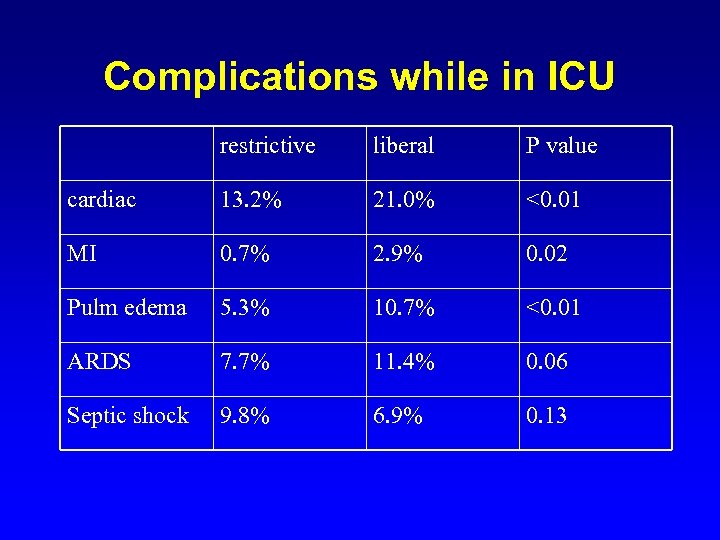
Complications while in ICU restrictive liberal P value cardiac 13. 2% 21. 0% <0. 01 MI 0. 7% 2. 9% 0. 02 Pulm edema 5. 3% 10. 7% <0. 01 ARDS 7. 7% 11. 4% 0. 06 Septic shock 9. 8% 6. 9% 0. 13
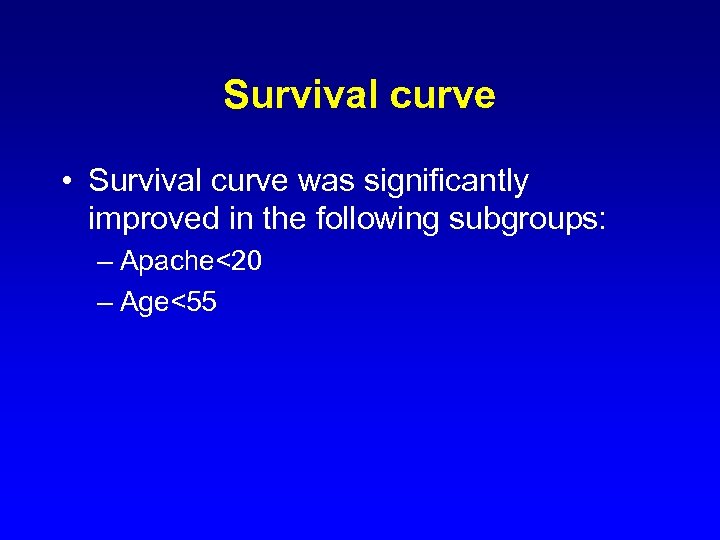
Survival curve • Survival curve was significantly improved in the following subgroups: – Apache<20 – Age<55
Conclusions • A restrictive approach to blood transfusions is as least as effective if not more effective than a more liberal approach • This is especially true in a healthier, younger population
Thrombocytopenia • Defined as a subnormal amount of platelets in the circulating blood • Pathophysiology is less well defined
Thrombocytopenia: Differential Diagnosis • • • Pseudothrombocytopenia Dilutional Thrombocytopenia Decreased Platelet production Increased Platelet Destruction Altered Distribution of Platelets
Pseudothrombocytopenia • Considered in patients without evidence of petechiae or ecchymoses • Most commonly caused by platelet clumping – Happens most frequently with EDTA – Associated with autoantibodies
Dilutional Thrombocytopenia • Large quantities of PRBC’s to treat massive hemmorhage
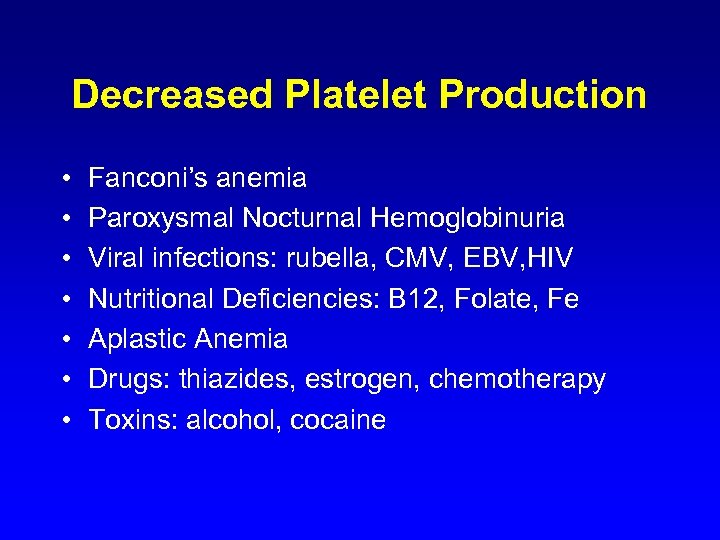
Decreased Platelet Production • • Fanconi’s anemia Paroxysmal Nocturnal Hemoglobinuria Viral infections: rubella, CMV, EBV, HIV Nutritional Deficiencies: B 12, Folate, Fe Aplastic Anemia Drugs: thiazides, estrogen, chemotherapy Toxins: alcohol, cocaine
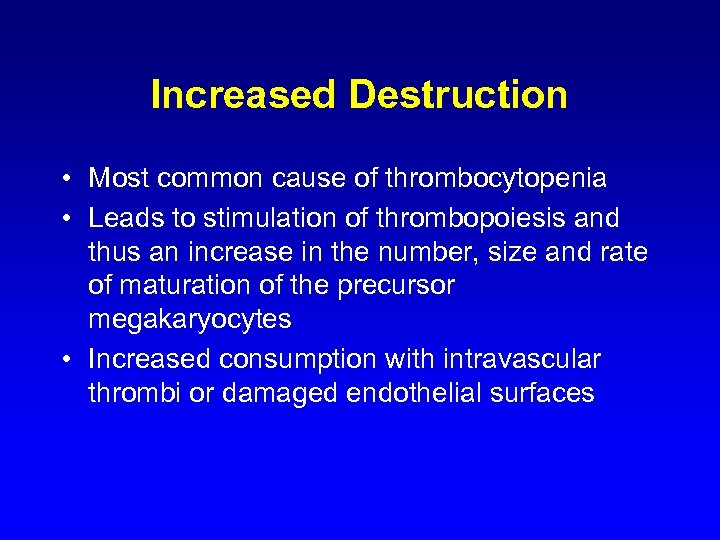
Increased Destruction • Most common cause of thrombocytopenia • Leads to stimulation of thrombopoiesis and thus an increase in the number, size and rate of maturation of the precursor megakaryocytes • Increased consumption with intravascular thrombi or damaged endothelial surfaces
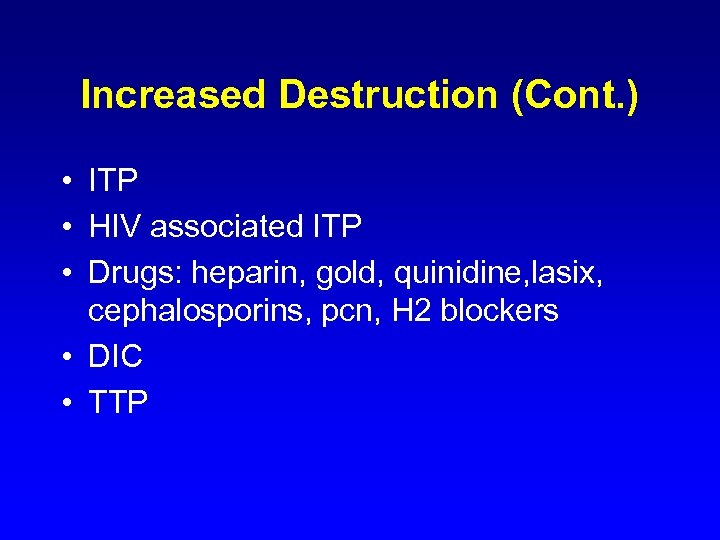
Increased Destruction (Cont. ) • ITP • HIV associated ITP • Drugs: heparin, gold, quinidine, lasix, cephalosporins, pcn, H 2 blockers • DIC • TTP
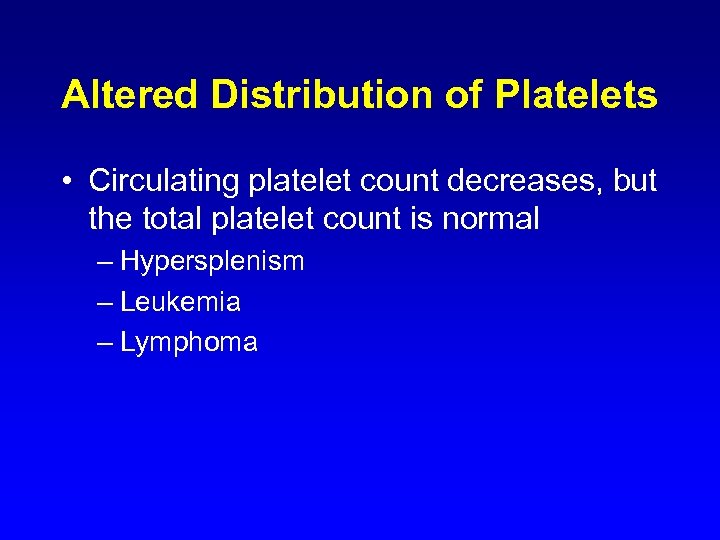
Altered Distribution of Platelets • Circulating platelet count decreases, but the total platelet count is normal – Hypersplenism – Leukemia – Lymphoma
Prophylactic Versus Therapeutic Platelet Transfusions • Platelet transfusions for active bleeding much more common on surgical and cardiology services • Prophylactic transfusions most common on hem/onc services • 10 x 109/L has become the standard clinical practice on hem/onc services
Factors affecting a patients response to platelet transfusion • Clinical situation: Fever, sepsis, splenomegaly, Bleeding, DIC • Patient: alloimunization, underlying disease, drugs (IVIG, Ampho B) • Length of time platelets stored • 15% of patients who require multiple transfusions become refractory
Strategies to improve response to platelet transfusions • • • Treat underlying condition Transfuse ABO identical platelets Transfuse platelets <48 hrs in storage Increase platelet dose Select compatible donor – Cross match – HLA match
Platelet Transfusions Reactions • Febrile nonhemolytic transfusion: caused by patients leucocytes reacting against donor leukocytes • Allergic reactions • Bacterial contamination: most common blood product with bacterial contamination
b4f8a8af7b2a99837a99ad5441ba0ad4.ppt