2bbed62c2de625f025e74ba5cf01fa34.ppt
- Количество слайдов: 94
 Anatomy and Physiology
Anatomy and Physiology
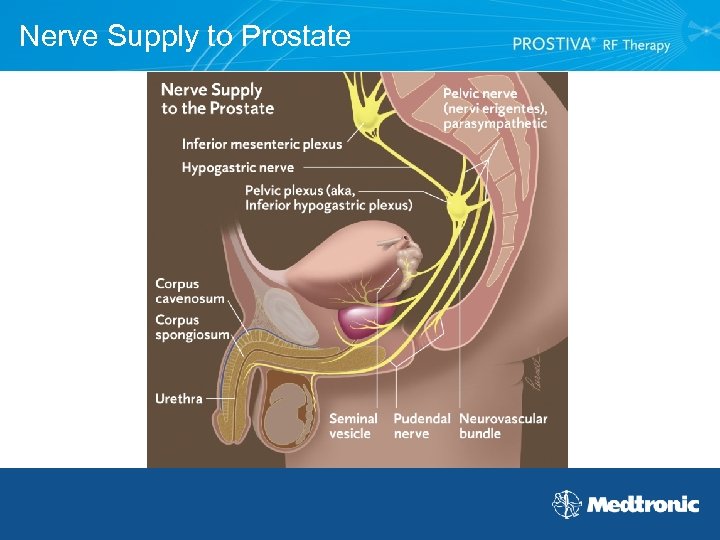 Nerve Supply to Prostate
Nerve Supply to Prostate
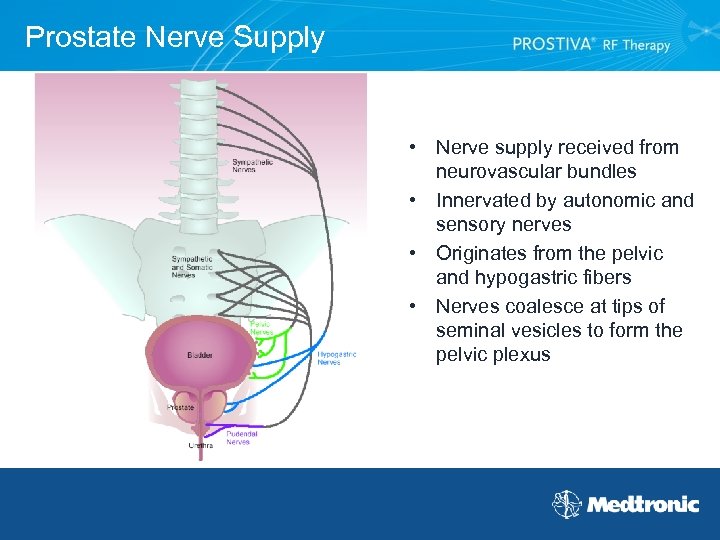 Prostate Nerve Supply • Nerve supply received from neurovascular bundles • Innervated by autonomic and sensory nerves • Originates from the pelvic and hypogastric fibers • Nerves coalesce at tips of seminal vesicles to form the pelvic plexus
Prostate Nerve Supply • Nerve supply received from neurovascular bundles • Innervated by autonomic and sensory nerves • Originates from the pelvic and hypogastric fibers • Nerves coalesce at tips of seminal vesicles to form the pelvic plexus
 Importance of Nerve Supply • Neurovascular bundles responsible for erectile function • Consideration for comfort control during PROSTIVA® RF Therapy procedure
Importance of Nerve Supply • Neurovascular bundles responsible for erectile function • Consideration for comfort control during PROSTIVA® RF Therapy procedure
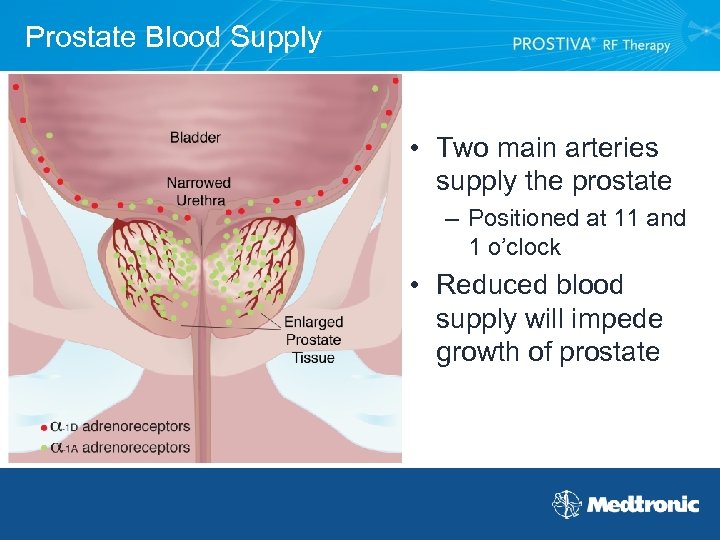 Prostate Blood Supply • Two main arteries supply the prostate – Positioned at 11 and 1 o’clock • Reduced blood supply will impede growth of prostate
Prostate Blood Supply • Two main arteries supply the prostate – Positioned at 11 and 1 o’clock • Reduced blood supply will impede growth of prostate
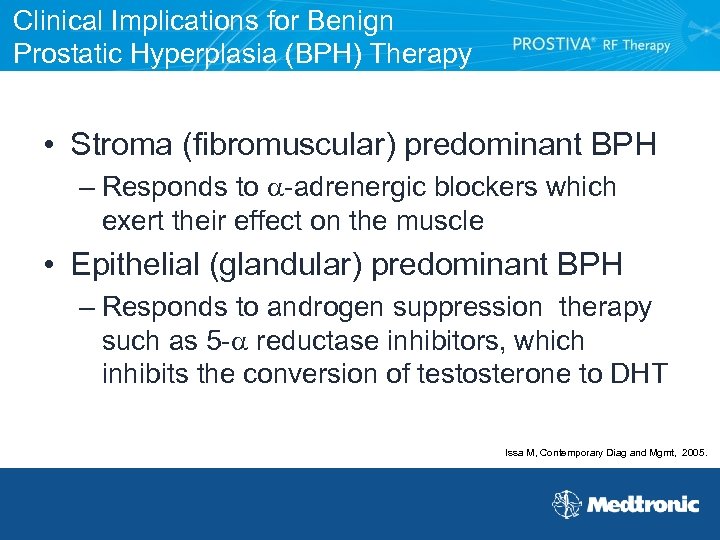 Clinical Implications for Benign Prostatic Hyperplasia (BPH) Therapy • Stroma (fibromuscular) predominant BPH – Responds to -adrenergic blockers which exert their effect on the muscle • Epithelial (glandular) predominant BPH – Responds to androgen suppression therapy such as 5 - reductase inhibitors, which inhibits the conversion of testosterone to DHT Issa M, Contemporary Diag and Mgmt, 2005.
Clinical Implications for Benign Prostatic Hyperplasia (BPH) Therapy • Stroma (fibromuscular) predominant BPH – Responds to -adrenergic blockers which exert their effect on the muscle • Epithelial (glandular) predominant BPH – Responds to androgen suppression therapy such as 5 - reductase inhibitors, which inhibits the conversion of testosterone to DHT Issa M, Contemporary Diag and Mgmt, 2005.
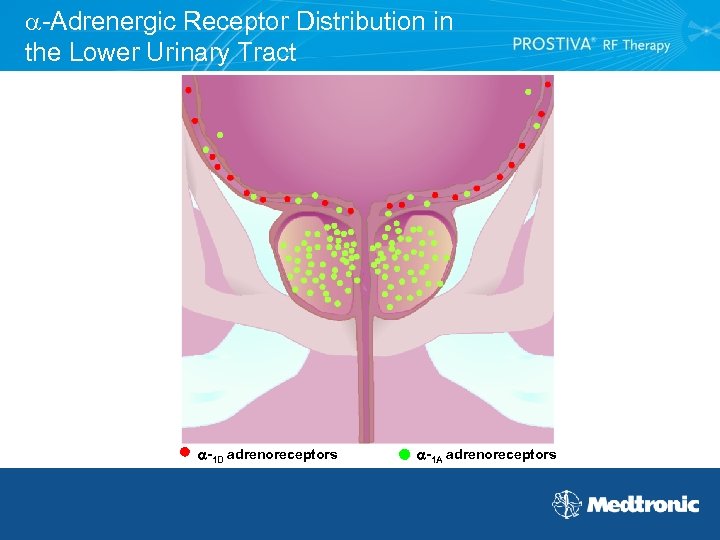 -Adrenergic Receptor Distribution in the Lower Urinary Tract -1 D adrenoreceptors -1 A adrenoreceptors
-Adrenergic Receptor Distribution in the Lower Urinary Tract -1 D adrenoreceptors -1 A adrenoreceptors
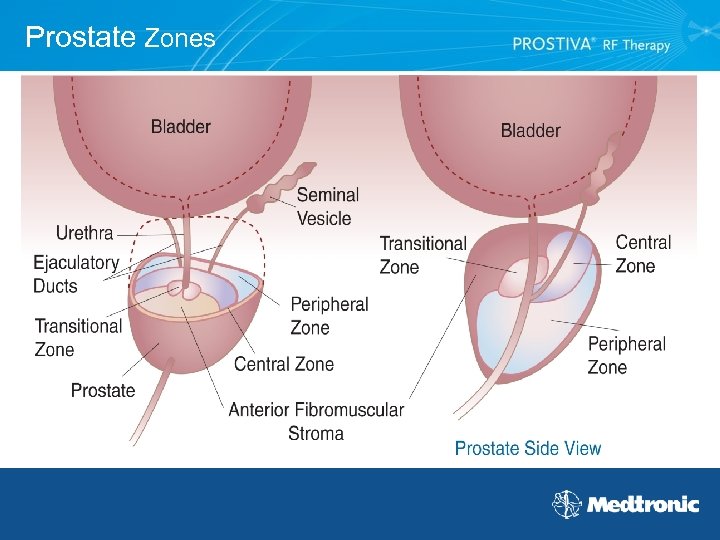 Prostate Zones
Prostate Zones
 Transitional Zone • Located anteriorly but surrounds the urethra • BPH primarily affects the transitional zone Percentage of the prostate – Peripheral zone - 70% – Central zone - 25% – Transitional zone - 5%
Transitional Zone • Located anteriorly but surrounds the urethra • BPH primarily affects the transitional zone Percentage of the prostate – Peripheral zone - 70% – Central zone - 25% – Transitional zone - 5%
 Benign Prostatic Hyperplasia (BPH) Overview
Benign Prostatic Hyperplasia (BPH) Overview
 Symptomatic BPH Population US Prevalence: 14. 9 Million US Incidence: 500, 000 Translates to: 50% of men over 50 60% of men over 60 70% of men over 70 80% of men over 80 US Census; Millennium Research, 2006; A. G. Edwards & Son, 2006.
Symptomatic BPH Population US Prevalence: 14. 9 Million US Incidence: 500, 000 Translates to: 50% of men over 50 60% of men over 60 70% of men over 70 80% of men over 80 US Census; Millennium Research, 2006; A. G. Edwards & Son, 2006.
 Why Treat BPH? • BPH is not cancer but it can lead to unwanted complications if not corrected • Urine retention and strain on the bladder can lead to – – Urinary tract infections Bladder or kidney damage Bladder stones Incontinence • When BPH is diagnosed and treated early, there is a lower risk of developing such complications
Why Treat BPH? • BPH is not cancer but it can lead to unwanted complications if not corrected • Urine retention and strain on the bladder can lead to – – Urinary tract infections Bladder or kidney damage Bladder stones Incontinence • When BPH is diagnosed and treated early, there is a lower risk of developing such complications
 Quality of Life of Untreated BPH Before PROSTIVA® RF Therapy • I couldn’t play golf because if I’d get out there I had to stop and find a bathroom to go. --Harold • I just had to go an awful lot – five or six times a night. --Paul • I didn’t really mind so much the fact that it was difficult to start urination, but what I really did mind was having the leakage. --Bill • It has an impact because first of all when you go into a strange store or a strange building, the first thing you have to zero in on is where are the restrooms. --Richard • I carried a cup in the car so I could urinate. I’ve urinated to relieve myself going 60 miles an hour! --Moses After PROSTIVA RF Therapy • The RF Therapy has changed my life. It has allowed me to do things that I couldn’t do without conditions before. --Richard • Prior to the RF Therapy, I was on two expensive medications for prostate problems and one of them I had to take twice a day. And after the Therapy, I’ve been able to drop them and don’t have to take them anymore which is great. --Bobby • PROSTIVA RF Therapy is the best thing I ever did in my life. --Harold
Quality of Life of Untreated BPH Before PROSTIVA® RF Therapy • I couldn’t play golf because if I’d get out there I had to stop and find a bathroom to go. --Harold • I just had to go an awful lot – five or six times a night. --Paul • I didn’t really mind so much the fact that it was difficult to start urination, but what I really did mind was having the leakage. --Bill • It has an impact because first of all when you go into a strange store or a strange building, the first thing you have to zero in on is where are the restrooms. --Richard • I carried a cup in the car so I could urinate. I’ve urinated to relieve myself going 60 miles an hour! --Moses After PROSTIVA RF Therapy • The RF Therapy has changed my life. It has allowed me to do things that I couldn’t do without conditions before. --Richard • Prior to the RF Therapy, I was on two expensive medications for prostate problems and one of them I had to take twice a day. And after the Therapy, I’ve been able to drop them and don’t have to take them anymore which is great. --Bobby • PROSTIVA RF Therapy is the best thing I ever did in my life. --Harold
 Click box to activate video This video clip is one patient’s experience only and may not reflect other patients' experiences
Click box to activate video This video clip is one patient’s experience only and may not reflect other patients' experiences
 Benign Prostatic Hyperplasia (BPH) Patient Evaluation and Diagnosis
Benign Prostatic Hyperplasia (BPH) Patient Evaluation and Diagnosis
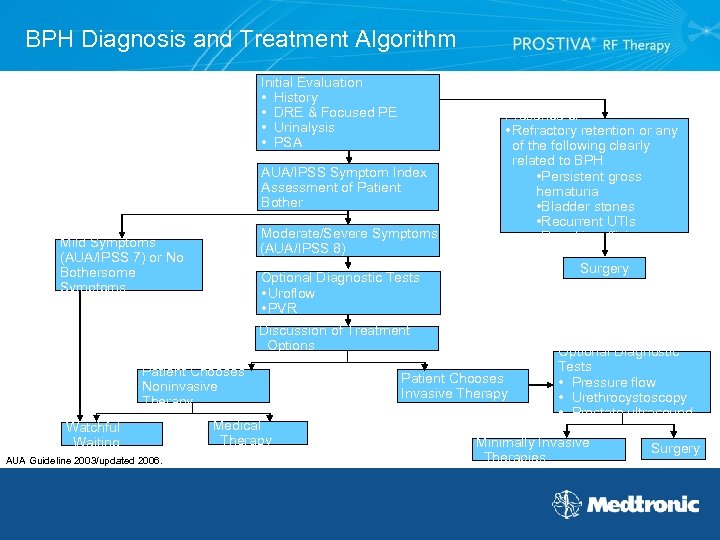 BPH Diagnosis and Treatment Algorithm Initial Evaluation • History • DRE & Focused PE • Urinalysis • PSA AUA/IPSS Symptom Index Assessment of Patient Bother Moderate/Severe Symptoms (AUA/IPSS 8) Mild Symptoms (AUA/IPSS 7) or No Bothersome Symptoms Presence of • Refractory retention or any of the following clearly related to BPH • Persistent gross hematuria • Bladder stones • Recurrent UTIs • Renal insufficiency Surgery Optional Diagnostic Tests • Uroflow • PVR Discussion of Treatment Options Patient Chooses Noninvasive Therapy Watchful Waiting AUA Guideline 2003/updated 2006. Medical Therapy Patient Chooses Invasive Therapy Optional Diagnostic Tests • Pressure flow • Urethrocystoscopy • Prostate ultrasound Minimally Invasive Therapies Surgery
BPH Diagnosis and Treatment Algorithm Initial Evaluation • History • DRE & Focused PE • Urinalysis • PSA AUA/IPSS Symptom Index Assessment of Patient Bother Moderate/Severe Symptoms (AUA/IPSS 8) Mild Symptoms (AUA/IPSS 7) or No Bothersome Symptoms Presence of • Refractory retention or any of the following clearly related to BPH • Persistent gross hematuria • Bladder stones • Recurrent UTIs • Renal insufficiency Surgery Optional Diagnostic Tests • Uroflow • PVR Discussion of Treatment Options Patient Chooses Noninvasive Therapy Watchful Waiting AUA Guideline 2003/updated 2006. Medical Therapy Patient Chooses Invasive Therapy Optional Diagnostic Tests • Pressure flow • Urethrocystoscopy • Prostate ultrasound Minimally Invasive Therapies Surgery
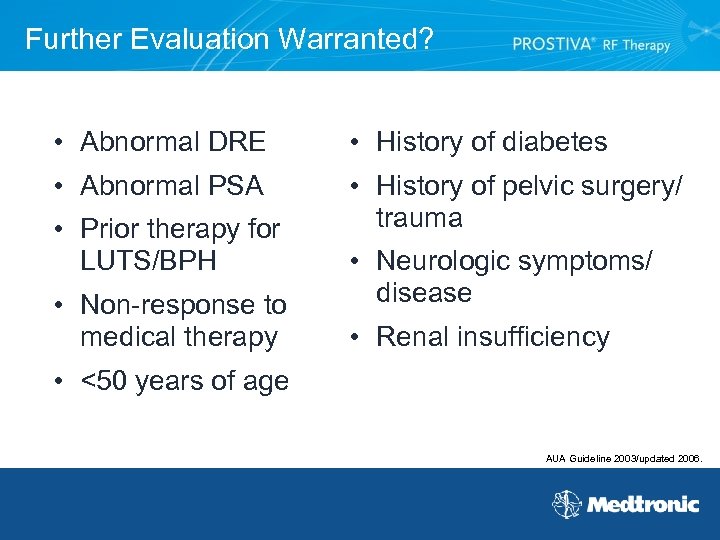 Further Evaluation Warranted? • Abnormal DRE • History of diabetes • Abnormal PSA • History of pelvic surgery/ trauma • Prior therapy for LUTS/BPH • Non-response to medical therapy • Neurologic symptoms/ disease • Renal insufficiency • <50 years of age AUA Guideline 2003/updated 2006.
Further Evaluation Warranted? • Abnormal DRE • History of diabetes • Abnormal PSA • History of pelvic surgery/ trauma • Prior therapy for LUTS/BPH • Non-response to medical therapy • Neurologic symptoms/ disease • Renal insufficiency • <50 years of age AUA Guideline 2003/updated 2006.
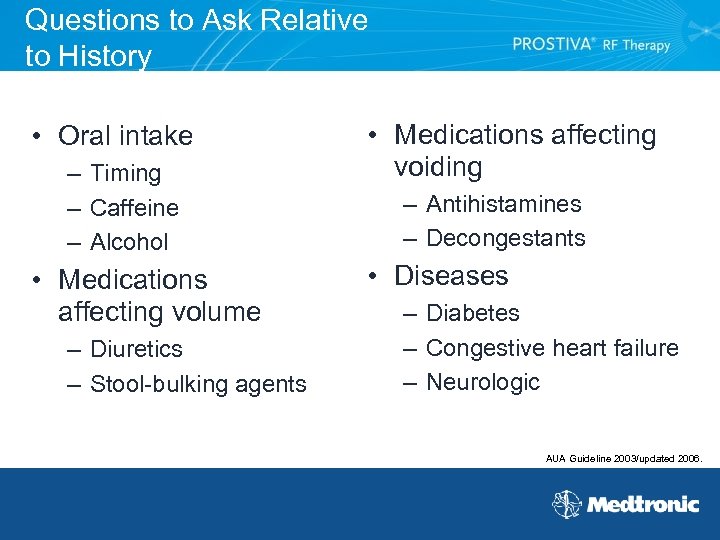 Questions to Ask Relative to History • Oral intake – Timing – Caffeine – Alcohol • Medications affecting volume – Diuretics – Stool-bulking agents • Medications affecting voiding – Antihistamines – Decongestants • Diseases – Diabetes – Congestive heart failure – Neurologic AUA Guideline 2003/updated 2006.
Questions to Ask Relative to History • Oral intake – Timing – Caffeine – Alcohol • Medications affecting volume – Diuretics – Stool-bulking agents • Medications affecting voiding – Antihistamines – Decongestants • Diseases – Diabetes – Congestive heart failure – Neurologic AUA Guideline 2003/updated 2006.
 Optional Diagnostic Tests Following initial evaluation • Uroflow – Urinary flow-rate recording (Qmax) • PVR If patient chooses invasive therapy • Pressure flow • Urethrocystoscopy • Prostate ultrasound AUA Guideline 2003/updated 2006.
Optional Diagnostic Tests Following initial evaluation • Uroflow – Urinary flow-rate recording (Qmax) • PVR If patient chooses invasive therapy • Pressure flow • Urethrocystoscopy • Prostate ultrasound AUA Guideline 2003/updated 2006.
 Standard Questionnaires for Patient’s Perception of BPH Symptoms • AUA Symptom Score • International Prostate Symptom Score (IPSS) • BPH Impact Index (Bother Score)
Standard Questionnaires for Patient’s Perception of BPH Symptoms • AUA Symptom Score • International Prostate Symptom Score (IPSS) • BPH Impact Index (Bother Score)
 AUA Symptom Score Index • Seven-item questionnaire related to BPH symptoms • Validated and reproducible • Determines disease severity • Documents response to therapy • Allows standardized comparisons of symptom relief when evaluating treatments AUA Guideline 2003/updated 2006.
AUA Symptom Score Index • Seven-item questionnaire related to BPH symptoms • Validated and reproducible • Determines disease severity • Documents response to therapy • Allows standardized comparisons of symptom relief when evaluating treatments AUA Guideline 2003/updated 2006.
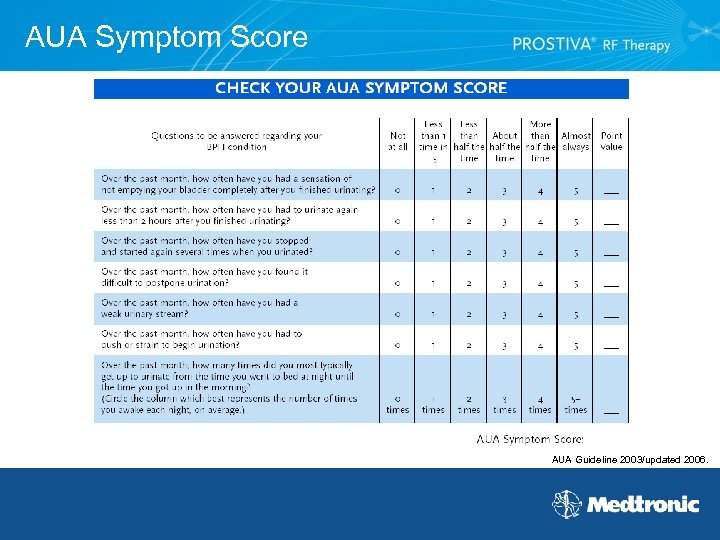 AUA Symptom Score AUA Guideline 2003/updated 2006.
AUA Symptom Score AUA Guideline 2003/updated 2006.
 Classification of AUA Symptom Scores The possible total runs from 0 -35 points with higher scores indicating more severe symptoms. Scores lower than 7 are considered mild and generally do not warrant treatment. Classification ranges • Mild (0 -7) • Moderate (8 -19) • Severe (20 -35) • Without bother or bothersome AUA Guideline 2003/updated 2006.
Classification of AUA Symptom Scores The possible total runs from 0 -35 points with higher scores indicating more severe symptoms. Scores lower than 7 are considered mild and generally do not warrant treatment. Classification ranges • Mild (0 -7) • Moderate (8 -19) • Severe (20 -35) • Without bother or bothersome AUA Guideline 2003/updated 2006.
 Initial Management and Discussion Using AUA Symptom Score Patients with mild symptoms (AUA symptom score ≤ 7) and Patients with moderate or severe symptoms (AUA symptom score ≥ 8) who are not bothered by their symptoms – Offer watchful waiting – Reassure patient – Reassess periodically
Initial Management and Discussion Using AUA Symptom Score Patients with mild symptoms (AUA symptom score ≤ 7) and Patients with moderate or severe symptoms (AUA symptom score ≥ 8) who are not bothered by their symptoms – Offer watchful waiting – Reassure patient – Reassess periodically
 Initial Management and Discussion Using AUA Symptom Score Patients with bothersome, moderate to severe symptoms (AUA Symptom Score ≥ 8) – Watchful waiting – Discuss BPH treatment options, including benefits and risks – Provide patient education materials
Initial Management and Discussion Using AUA Symptom Score Patients with bothersome, moderate to severe symptoms (AUA Symptom Score ≥ 8) – Watchful waiting – Discuss BPH treatment options, including benefits and risks – Provide patient education materials
 International Prostate Symptom Score (IPSS) AUA Symptom Score Index plus additional question on QOL as a function of urinary symptoms: “If you were to spend the rest of your life with your urinary condition just the way it is now, how would you feel about that? ” – Scale of 0 to 6 (delighted to terrible) – Note: While symptoms may be prevalent, they may not be troublesome O’Leary MP. Urology. 2000.
International Prostate Symptom Score (IPSS) AUA Symptom Score Index plus additional question on QOL as a function of urinary symptoms: “If you were to spend the rest of your life with your urinary condition just the way it is now, how would you feel about that? ” – Scale of 0 to 6 (delighted to terrible) – Note: While symptoms may be prevalent, they may not be troublesome O’Leary MP. Urology. 2000.
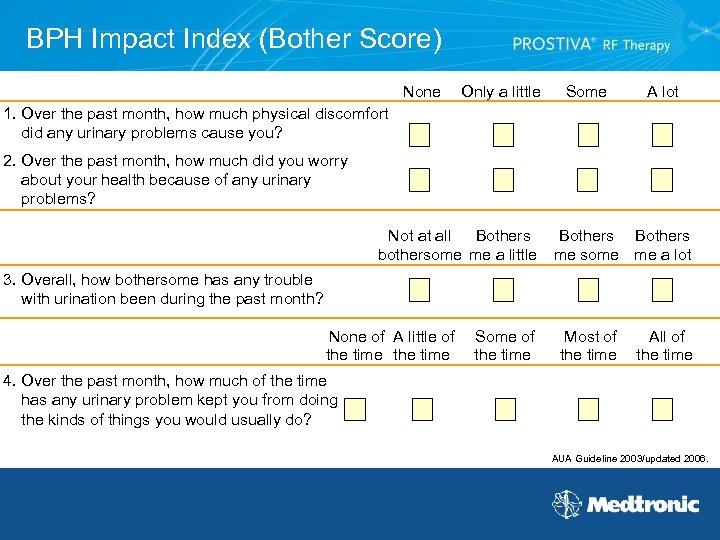 BPH Impact Index (Bother Score) None Only a little Some A lot 1. Over the past month, how much physical discomfort did any urinary problems cause you? 2. Over the past month, how much did you worry about your health because of any urinary problems? Not at all Bothers bothersome me a little Bothers me some me a lot 3. Overall, how bothersome has any trouble with urination been during the past month? None of A little of the time Some of the time Most of the time All of the time 4. Over the past month, how much of the time has any urinary problem kept you from doing the kinds of things you would usually do? AUA Guideline 2003/updated 2006.
BPH Impact Index (Bother Score) None Only a little Some A lot 1. Over the past month, how much physical discomfort did any urinary problems cause you? 2. Over the past month, how much did you worry about your health because of any urinary problems? Not at all Bothers bothersome me a little Bothers me some me a lot 3. Overall, how bothersome has any trouble with urination been during the past month? None of A little of the time Some of the time Most of the time All of the time 4. Over the past month, how much of the time has any urinary problem kept you from doing the kinds of things you would usually do? AUA Guideline 2003/updated 2006.
 Mechanism of Action
Mechanism of Action
 Definitions • Current - the number or amount of electrons flowing past a fixed point for a fixed amount of time • Current density - the amount of current flowing per unit area of a conductor surface • Electricity - the flow of atoms through various mediums such as fluids or metals that are called conductors. There are negatively charged particles inside the atoms called electrons. The electrons will move through a conductor if force or pressure is applied.
Definitions • Current - the number or amount of electrons flowing past a fixed point for a fixed amount of time • Current density - the amount of current flowing per unit area of a conductor surface • Electricity - the flow of atoms through various mediums such as fluids or metals that are called conductors. There are negatively charged particles inside the atoms called electrons. The electrons will move through a conductor if force or pressure is applied.
 Definitions - continued • Hyperthermia therapy - prostate tissue is heated to the range of 42 to 44 C. Tissue effect is temporary. • Resistance/impedance - resistance encountered by the electrons as they move through a conductor. Resistance/ impedance is measured in ohms. • Voltage - the force or pressure that moves electrons through a conductor.
Definitions - continued • Hyperthermia therapy - prostate tissue is heated to the range of 42 to 44 C. Tissue effect is temporary. • Resistance/impedance - resistance encountered by the electrons as they move through a conductor. Resistance/ impedance is measured in ohms. • Voltage - the force or pressure that moves electrons through a conductor.
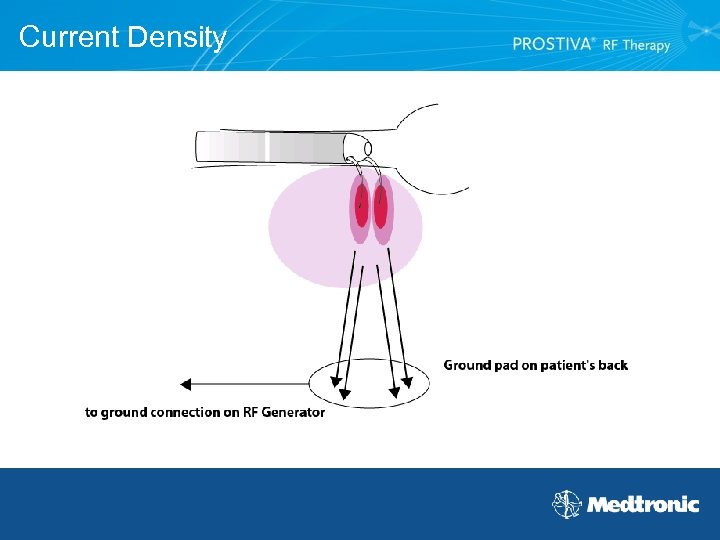 Current Density
Current Density
 Basic Function • The PROSTIVA® RF Therapy system generator produces the voltage (force) necessary to move the electrons through the prostate tissue to the grounding pad. • Electrons moving through the tissue vibrate the tissue causing heat from friction. – Temperature/time • 45 C – 60 Minutes • 55 C – 20 Minutes • 60 C – 5 Minutes • 70 C – 2 Minutes Boschef, et al. ASME, 2001.
Basic Function • The PROSTIVA® RF Therapy system generator produces the voltage (force) necessary to move the electrons through the prostate tissue to the grounding pad. • Electrons moving through the tissue vibrate the tissue causing heat from friction. – Temperature/time • 45 C – 60 Minutes • 55 C – 20 Minutes • 60 C – 5 Minutes • 70 C – 2 Minutes Boschef, et al. ASME, 2001.
 Impact of Heat on Tissue The heat generated in the tissue by the needles can be described as forming two zones. Pathological lesion • Produced when temperatures reach > 55° C • Described as coagulative necrosis (dead tissue surrounded by healthy tissue) Physiological lesion • Occurs at temperatures > 47° C • Surrounds the pathological lesion and is described as the gelatinized zone • Tissue is not killed, but damaged • Result is injury to the tissue that is accompanied with inflammation and edema, resembling a gel Boschef, et al. ASME, 2001.
Impact of Heat on Tissue The heat generated in the tissue by the needles can be described as forming two zones. Pathological lesion • Produced when temperatures reach > 55° C • Described as coagulative necrosis (dead tissue surrounded by healthy tissue) Physiological lesion • Occurs at temperatures > 47° C • Surrounds the pathological lesion and is described as the gelatinized zone • Tissue is not killed, but damaged • Result is injury to the tissue that is accompanied with inflammation and edema, resembling a gel Boschef, et al. ASME, 2001.
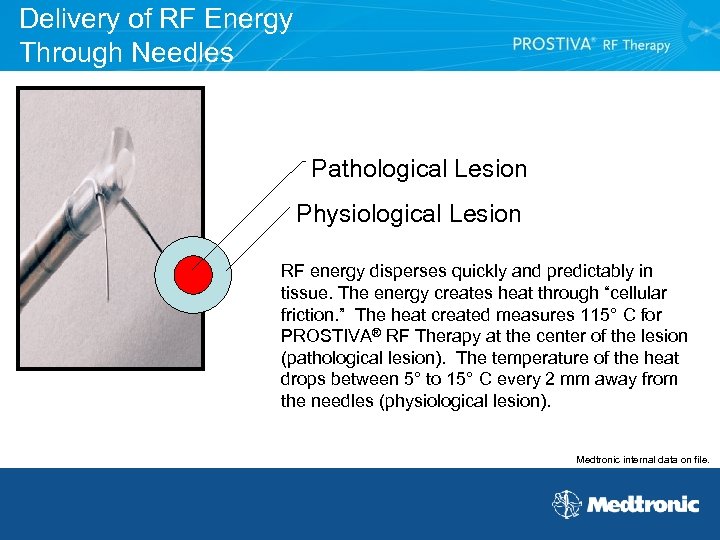 Delivery of RF Energy Through Needles Pathological Lesion Physiological Lesion RF energy disperses quickly and predictably in tissue. The energy creates heat through “cellular friction. ” The heat created measures 115° C for PROSTIVA® RF Therapy at the center of the lesion (pathological lesion). The temperature of the heat drops between 5° to 15° C every 2 mm away from the needles (physiological lesion). Medtronic internal data on file.
Delivery of RF Energy Through Needles Pathological Lesion Physiological Lesion RF energy disperses quickly and predictably in tissue. The energy creates heat through “cellular friction. ” The heat created measures 115° C for PROSTIVA® RF Therapy at the center of the lesion (pathological lesion). The temperature of the heat drops between 5° to 15° C every 2 mm away from the needles (physiological lesion). Medtronic internal data on file.
 Science Behind the Technology • Based on reasonable scientific analysis, PROSTIVA® RF Therapy works in the following ways: – Denervation – Devascularization
Science Behind the Technology • Based on reasonable scientific analysis, PROSTIVA® RF Therapy works in the following ways: – Denervation – Devascularization
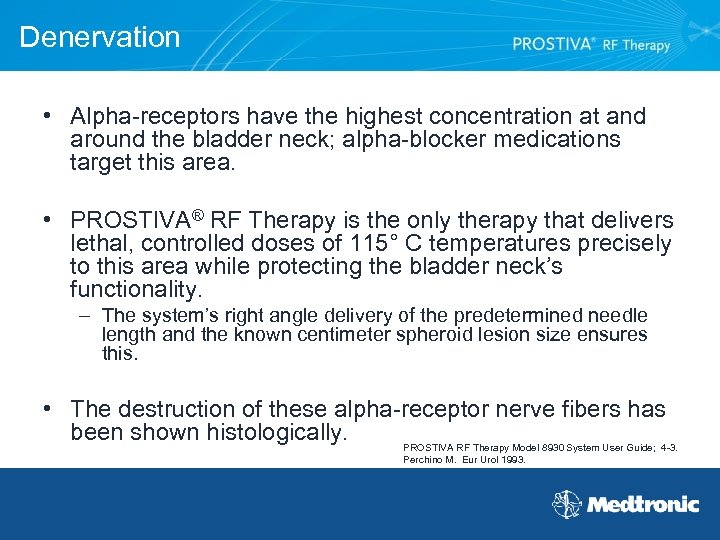 Denervation • Alpha-receptors have the highest concentration at and around the bladder neck; alpha-blocker medications target this area. • PROSTIVA® RF Therapy is the only therapy that delivers lethal, controlled doses of 115° C temperatures precisely to this area while protecting the bladder neck’s functionality. – The system’s right angle delivery of the predetermined needle length and the known centimeter spheroid lesion size ensures this. • The destruction of these alpha-receptor nerve fibers has been shown histologically. PROSTIVA RF Therapy Model 8930 System User Guide; 4 -3. Perchino M. Eur Urol 1993.
Denervation • Alpha-receptors have the highest concentration at and around the bladder neck; alpha-blocker medications target this area. • PROSTIVA® RF Therapy is the only therapy that delivers lethal, controlled doses of 115° C temperatures precisely to this area while protecting the bladder neck’s functionality. – The system’s right angle delivery of the predetermined needle length and the known centimeter spheroid lesion size ensures this. • The destruction of these alpha-receptor nerve fibers has been shown histologically. PROSTIVA RF Therapy Model 8930 System User Guide; 4 -3. Perchino M. Eur Urol 1993.
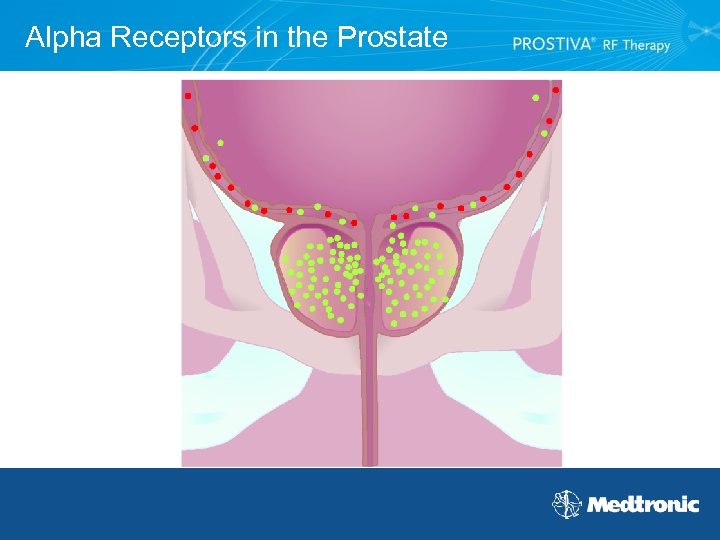 Alpha Receptors in the Prostate
Alpha Receptors in the Prostate
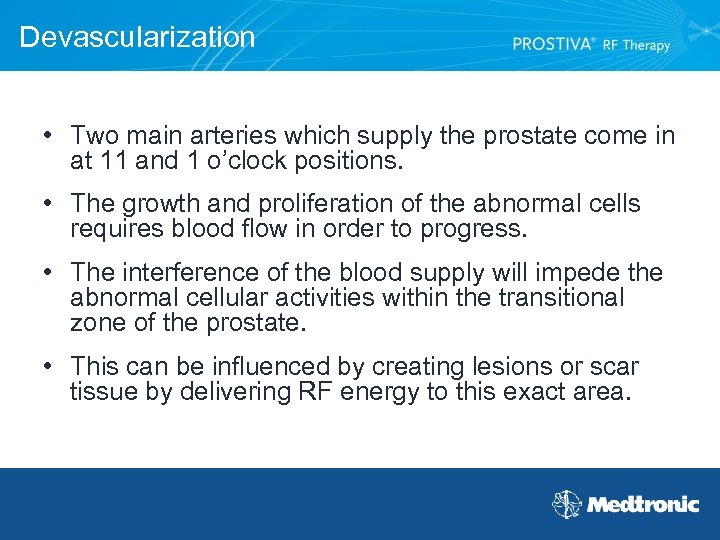 Devascularization • Two main arteries which supply the prostate come in at 11 and 1 o’clock positions. • The growth and proliferation of the abnormal cells requires blood flow in order to progress. • The interference of the blood supply will impede the abnormal cellular activities within the transitional zone of the prostate. • This can be influenced by creating lesions or scar tissue by delivering RF energy to this exact area.
Devascularization • Two main arteries which supply the prostate come in at 11 and 1 o’clock positions. • The growth and proliferation of the abnormal cells requires blood flow in order to progress. • The interference of the blood supply will impede the abnormal cellular activities within the transitional zone of the prostate. • This can be influenced by creating lesions or scar tissue by delivering RF energy to this exact area.
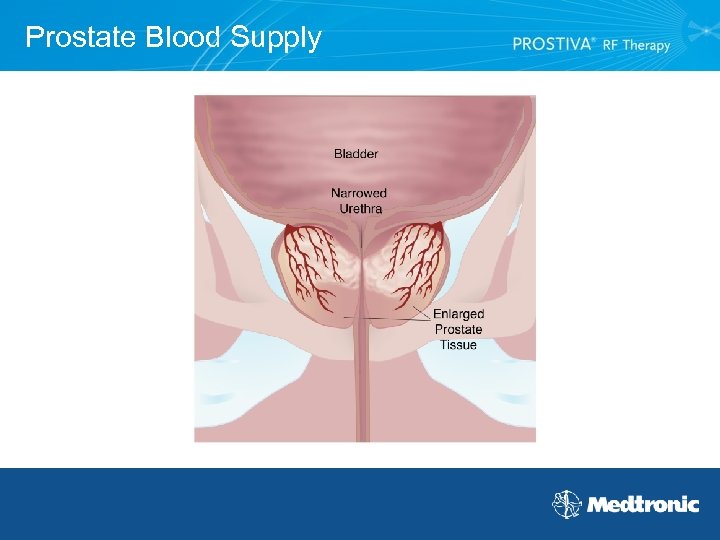 Prostate Blood Supply
Prostate Blood Supply
 PROSTIVA® RF Therapy Procedure and Its Impact on Size • Recall that 5 - reductase inhibitors block free testosterone from binding to 5 - reductase • PROSTIVA RF Therapy may kill: – 5 - reductase that is in the lesion – The blood vessels that carry the free testosterone to the transitional zone • PROSTIVA RF Therapy could decrease the size of the prostate
PROSTIVA® RF Therapy Procedure and Its Impact on Size • Recall that 5 - reductase inhibitors block free testosterone from binding to 5 - reductase • PROSTIVA RF Therapy may kill: – 5 - reductase that is in the lesion – The blood vessels that carry the free testosterone to the transitional zone • PROSTIVA RF Therapy could decrease the size of the prostate
 Mechanism of Action Animation Click to play movie
Mechanism of Action Animation Click to play movie
 MRI Movie Sequence Click to play movie Used by permission - Thayne Larson, M. D.
MRI Movie Sequence Click to play movie Used by permission - Thayne Larson, M. D.
 MRI Movie Sequence Click to play movie Used by permission - Thayne Larson, M. D.
MRI Movie Sequence Click to play movie Used by permission - Thayne Larson, M. D.
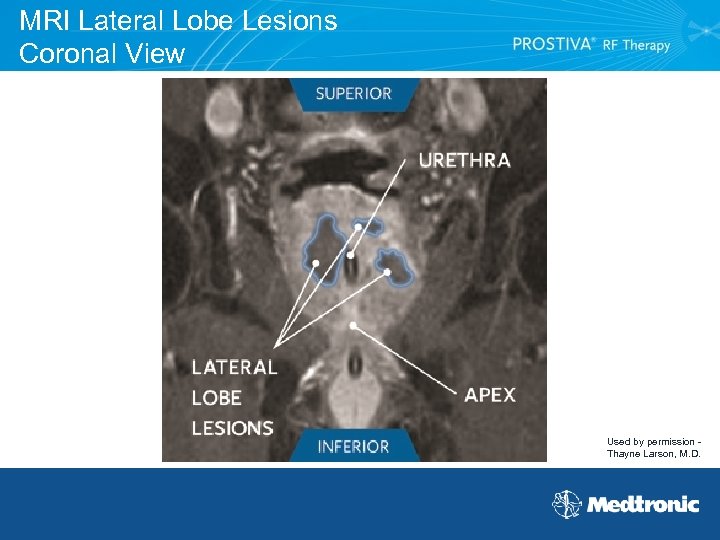 MRI Lateral Lobe Lesions Coronal View Used by permission Thayne Larson, M. D.
MRI Lateral Lobe Lesions Coronal View Used by permission Thayne Larson, M. D.
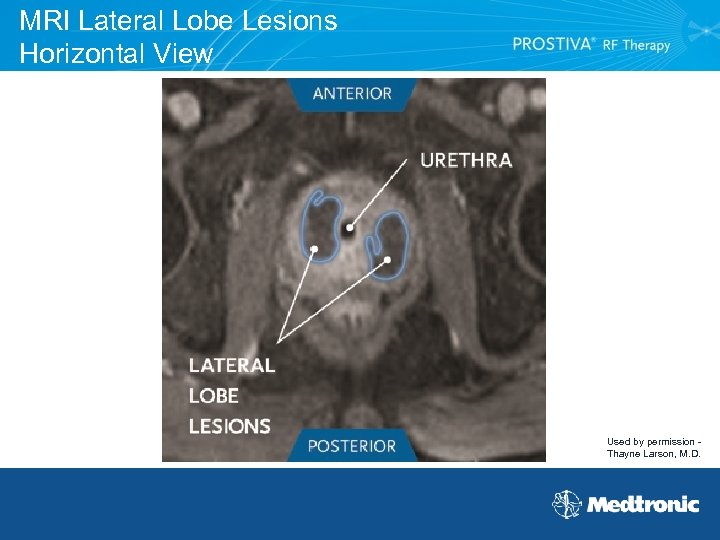 MRI Lateral Lobe Lesions Horizontal View Used by permission Thayne Larson, M. D.
MRI Lateral Lobe Lesions Horizontal View Used by permission Thayne Larson, M. D.
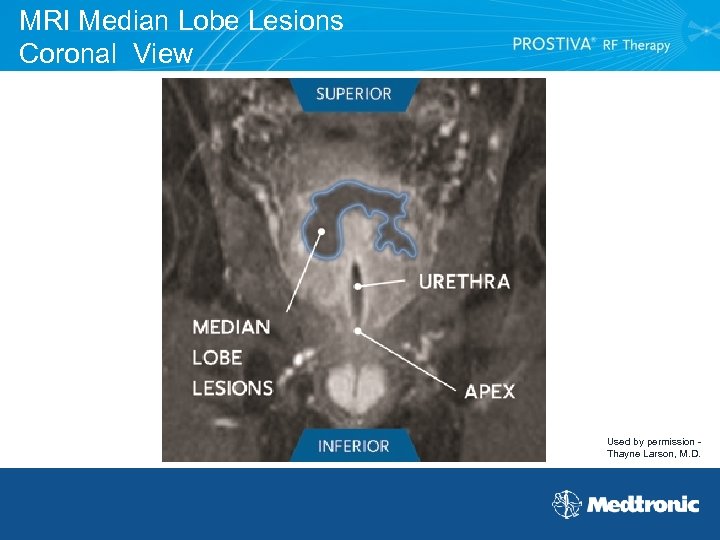 MRI Median Lobe Lesions Coronal View Used by permission Thayne Larson, M. D.
MRI Median Lobe Lesions Coronal View Used by permission Thayne Larson, M. D.
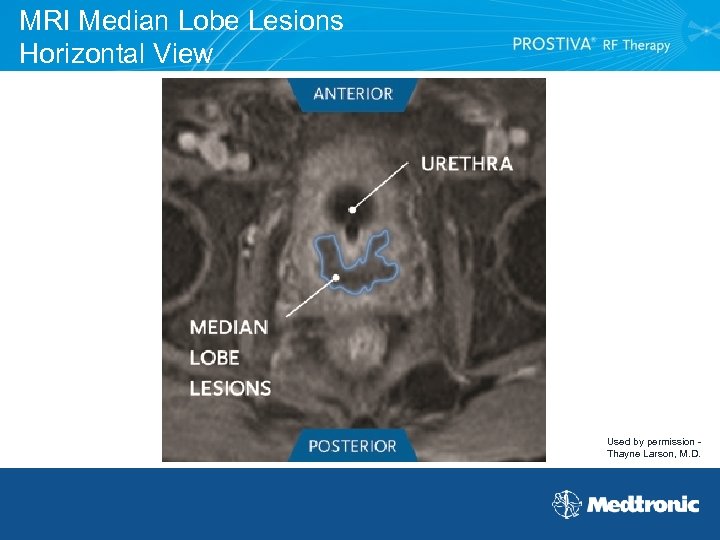 MRI Median Lobe Lesions Horizontal View Used by permission Thayne Larson, M. D.
MRI Median Lobe Lesions Horizontal View Used by permission Thayne Larson, M. D.
 Treatment Options for Benign Prostatic Hyperplasia (BPH)
Treatment Options for Benign Prostatic Hyperplasia (BPH)
 How do you balance the challenges of providing a good in-office experience versus long-term symptom relief for your patients?
How do you balance the challenges of providing a good in-office experience versus long-term symptom relief for your patients?
 What’s Your BPH Treatment Algorithm?
What’s Your BPH Treatment Algorithm?
 Treating BPH • Minor symptoms usually do not require treatment. • Moderate to severe symptoms tend to interfere with sleep and daily activities and usually require treatment.
Treating BPH • Minor symptoms usually do not require treatment. • Moderate to severe symptoms tend to interfere with sleep and daily activities and usually require treatment.
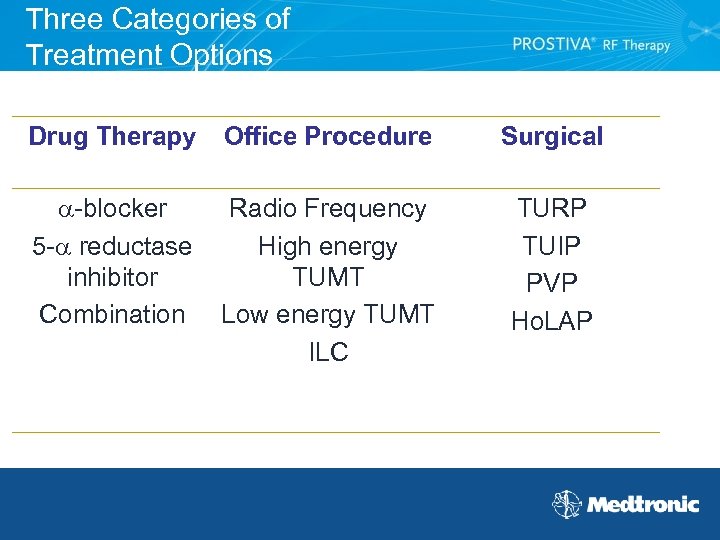 Three Categories of Treatment Options Drug Therapy Office Procedure Surgical -blocker 5 - reductase inhibitor Combination Radio Frequency High energy TUMT Low energy TUMT ILC TURP TUIP PVP Ho. LAP
Three Categories of Treatment Options Drug Therapy Office Procedure Surgical -blocker 5 - reductase inhibitor Combination Radio Frequency High energy TUMT Low energy TUMT ILC TURP TUIP PVP Ho. LAP
 Drug Therapy Advantages • No surgery • Effective for mild to moderate symptoms Disadvantages • Lifelong commitment to therapy • Effectiveness may decrease over time • Drug therapy can cause multiple side effects – Impotence, dizziness, headaches, fatigue, and decreased libido • Must take a daily pill for the rest of your life to maintain symptom relief and costs approximately $1, 000 per year http: //www. drugstore. com, 2006.
Drug Therapy Advantages • No surgery • Effective for mild to moderate symptoms Disadvantages • Lifelong commitment to therapy • Effectiveness may decrease over time • Drug therapy can cause multiple side effects – Impotence, dizziness, headaches, fatigue, and decreased libido • Must take a daily pill for the rest of your life to maintain symptom relief and costs approximately $1, 000 per year http: //www. drugstore. com, 2006.
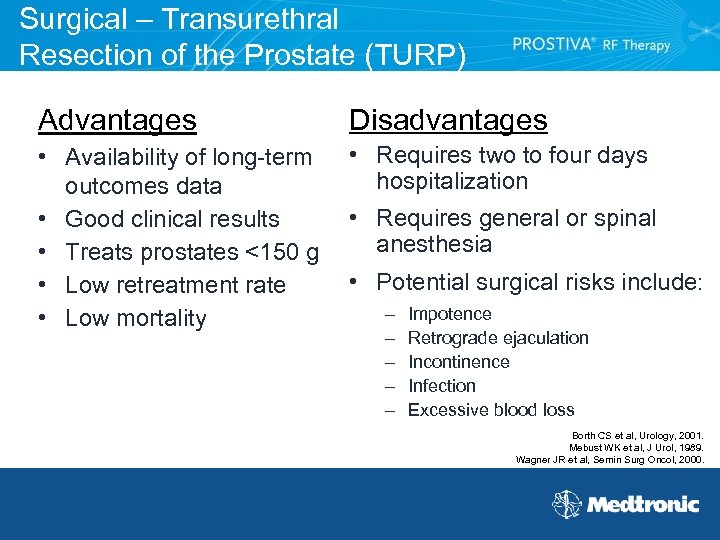 Surgical – Transurethral Resection of the Prostate (TURP) Advantages Disadvantages • Availability of long-term outcomes data • Good clinical results • Treats prostates <150 g • Low retreatment rate • Low mortality • Requires two to four days hospitalization • Requires general or spinal anesthesia • Potential surgical risks include: – – – Impotence Retrograde ejaculation Incontinence Infection Excessive blood loss Borth CS et al, Urology, 2001. Mebust WK et al, J Urol, 1989. Wagner JR et al, Semin Surg Oncol, 2000.
Surgical – Transurethral Resection of the Prostate (TURP) Advantages Disadvantages • Availability of long-term outcomes data • Good clinical results • Treats prostates <150 g • Low retreatment rate • Low mortality • Requires two to four days hospitalization • Requires general or spinal anesthesia • Potential surgical risks include: – – – Impotence Retrograde ejaculation Incontinence Infection Excessive blood loss Borth CS et al, Urology, 2001. Mebust WK et al, J Urol, 1989. Wagner JR et al, Semin Surg Oncol, 2000.
 Surgical - Green. Light PVP™ • • Hospital-based procedure Requires general anesthesia Better for smaller prostates TURP-like results
Surgical - Green. Light PVP™ • • Hospital-based procedure Requires general anesthesia Better for smaller prostates TURP-like results
 Surgical - Ho. LAP • Holmium laser ablation of the prostate (Ho. LAP) • Performed as an outpatient procedure • Tissue ablation is roughly equivalent to Green. Light PVP™ • Versatility of performing across multiple specialties and treating other urology conditions including strictures, tumors and stones
Surgical - Ho. LAP • Holmium laser ablation of the prostate (Ho. LAP) • Performed as an outpatient procedure • Tissue ablation is roughly equivalent to Green. Light PVP™ • Versatility of performing across multiple specialties and treating other urology conditions including strictures, tumors and stones
 Office Procedures • Avoid the need to take daily medication • Avoid some of the risks and complications associated with surgery
Office Procedures • Avoid the need to take daily medication • Avoid some of the risks and complications associated with surgery
 Office Procedures • Radio Frequency Therapy (PROSTIVA®) • Microwave Thermotherapy (TUMT) • Interstitial Laser Coagulation (ILC)
Office Procedures • Radio Frequency Therapy (PROSTIVA®) • Microwave Thermotherapy (TUMT) • Interstitial Laser Coagulation (ILC)
 Office Procedure - TUMT • Microwaves used to heat and destroy excess prostate tissue • Procedure takes about one hour • Some require 2 to 14 days of catheterization which can result in urinary tract infection
Office Procedure - TUMT • Microwaves used to heat and destroy excess prostate tissue • Procedure takes about one hour • Some require 2 to 14 days of catheterization which can result in urinary tract infection
 Office Procedure - ILC • Laser energy coagulates obstructing tissue of the enlarged prostate gland • The tissue that is destroyed is absorbed by the body and BPH symptoms decrease over time • May require extended post-procedural catheterization which can result in higher rates of urinary tract infection • Procedure takes less than one hour • Requires 5 to 14 days of catheterization
Office Procedure - ILC • Laser energy coagulates obstructing tissue of the enlarged prostate gland • The tissue that is destroyed is absorbed by the body and BPH symptoms decrease over time • May require extended post-procedural catheterization which can result in higher rates of urinary tract infection • Procedure takes less than one hour • Requires 5 to 14 days of catheterization
 PROSTIVA® RF Therapy Indication for Use PROSTIVA® Radio Frequency Therapy is indicated for the treatment of symptoms due to urinary outflow obstruction secondary to benign prostatic hyperplasia (BPH) in men over the age of 50 with prostate sizes between 20 and 50 cm 3. PROSTIVA® RF Therapy System User Guide.
PROSTIVA® RF Therapy Indication for Use PROSTIVA® Radio Frequency Therapy is indicated for the treatment of symptoms due to urinary outflow obstruction secondary to benign prostatic hyperplasia (BPH) in men over the age of 50 with prostate sizes between 20 and 50 cm 3. PROSTIVA® RF Therapy System User Guide.
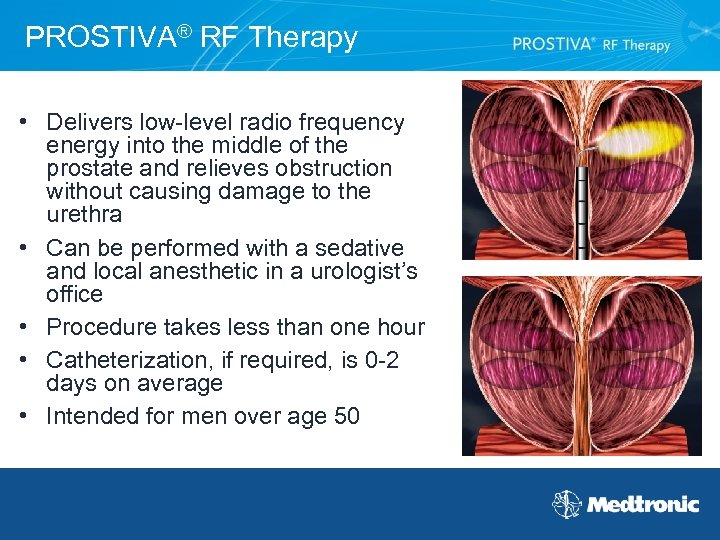 PROSTIVA® RF Therapy • Delivers low-level radio frequency energy into the middle of the prostate and relieves obstruction without causing damage to the urethra • Can be performed with a sedative and local anesthetic in a urologist’s office • Procedure takes less than one hour • Catheterization, if required, is 0 -2 days on average • Intended for men over age 50
PROSTIVA® RF Therapy • Delivers low-level radio frequency energy into the middle of the prostate and relieves obstruction without causing damage to the urethra • Can be performed with a sedative and local anesthetic in a urologist’s office • Procedure takes less than one hour • Catheterization, if required, is 0 -2 days on average • Intended for men over age 50
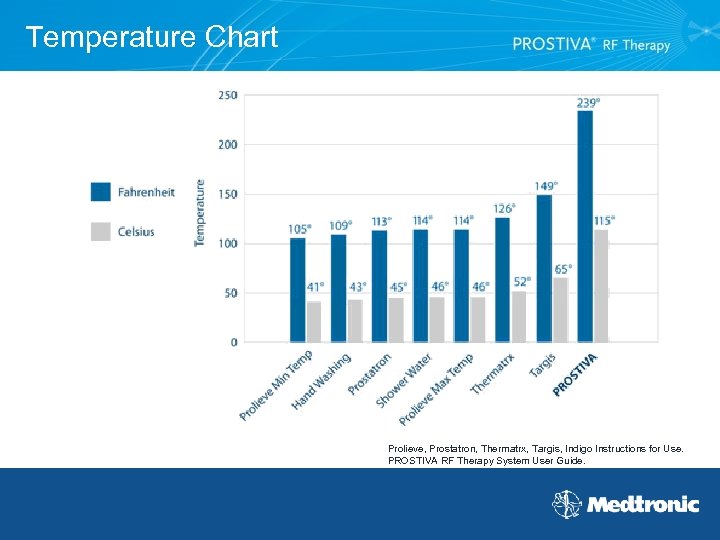 Temperature Chart Prolieve, Prostatron, Thermatrx, Targis, Indigo Instructions for Use. PROSTIVA RF Therapy System User Guide.
Temperature Chart Prolieve, Prostatron, Thermatrx, Targis, Indigo Instructions for Use. PROSTIVA RF Therapy System User Guide.
 What Side Effects are Associated with PROSTIVA® RF Therapy? • Possible side effects include: – – – – Obstruction Catheterization (for urinary retention) Bleeding/blood in urine Pain/discomfort Urgency to urinate Increased frequency of urination Urinary tract infection Patients may also experience a minor burning sensation when urinating for one to two weeks following the treatment • Compared to traditional surgical treatments, fewer side effects and adverse events PROSTIVA® RF Therapy System User Guide.
What Side Effects are Associated with PROSTIVA® RF Therapy? • Possible side effects include: – – – – Obstruction Catheterization (for urinary retention) Bleeding/blood in urine Pain/discomfort Urgency to urinate Increased frequency of urination Urinary tract infection Patients may also experience a minor burning sensation when urinating for one to two weeks following the treatment • Compared to traditional surgical treatments, fewer side effects and adverse events PROSTIVA® RF Therapy System User Guide.
 PROSTIVA® RF Therapy Overview
PROSTIVA® RF Therapy Overview
 Proven RF Technology • Nearly 100, 000 patients treated worldwide • Five-year efficacy data – After five years: • IPSS • Qmax • QOL - 55% +29% +68% • 115º C core lesion temperature • 89 published articles on RF therapy for BPH Hill, et al, J Urol, 2004.
Proven RF Technology • Nearly 100, 000 patients treated worldwide • Five-year efficacy data – After five years: • IPSS • Qmax • QOL - 55% +29% +68% • 115º C core lesion temperature • 89 published articles on RF therapy for BPH Hill, et al, J Urol, 2004.
 Precise Therapy Delivery • 360 degrees of precision to treat exactly the area you want • Six different needle length options to treat varying prostate sizes and shapes • 15 computer-monitored safety checks
Precise Therapy Delivery • 360 degrees of precision to treat exactly the area you want • Six different needle length options to treat varying prostate sizes and shapes • 15 computer-monitored safety checks
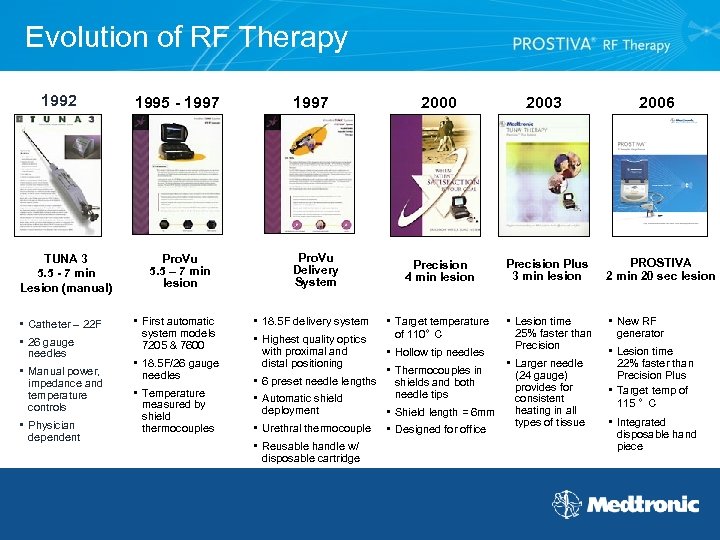 Evolution of RF Therapy 1992 TUNA 3 5. 5 - 7 min Lesion (manual) • Catheter – 22 F • 26 gauge needles • Manual power, impedance and temperature controls • Physician dependent 1995 - 1997 Pro. Vu 5. 5 – 7 min lesion • First automatic system models 7205 & 7600 • 18. 5 F/26 gauge needles • Temperature measured by shield thermocouples 1997 Pro. Vu Delivery System • 18. 5 F delivery system • Highest quality optics with proximal and distal positioning • 6 preset needle lengths • Automatic shield deployment • Urethral thermocouple • Reusable handle w/ disposable cartridge 2000 2003 Precision 4 min lesion Precision Plus 3 min lesion PROSTIVA 2 min 20 sec lesion • Lesion time • New RF • Target temperature of 110° C • Hollow tip needles • Thermocouples in shields and both needle tips • Shield length = 6 mm • Designed for office 25% faster than Precision • Larger needle (24 gauge) provides for consistent heating in all types of tissue 2006 generator • Lesion time 22% faster than Precision Plus • Target temp of 115 ° C • Integrated disposable hand piece
Evolution of RF Therapy 1992 TUNA 3 5. 5 - 7 min Lesion (manual) • Catheter – 22 F • 26 gauge needles • Manual power, impedance and temperature controls • Physician dependent 1995 - 1997 Pro. Vu 5. 5 – 7 min lesion • First automatic system models 7205 & 7600 • 18. 5 F/26 gauge needles • Temperature measured by shield thermocouples 1997 Pro. Vu Delivery System • 18. 5 F delivery system • Highest quality optics with proximal and distal positioning • 6 preset needle lengths • Automatic shield deployment • Urethral thermocouple • Reusable handle w/ disposable cartridge 2000 2003 Precision 4 min lesion Precision Plus 3 min lesion PROSTIVA 2 min 20 sec lesion • Lesion time • New RF • Target temperature of 110° C • Hollow tip needles • Thermocouples in shields and both needle tips • Shield length = 6 mm • Designed for office 25% faster than Precision • Larger needle (24 gauge) provides for consistent heating in all types of tissue 2006 generator • Lesion time 22% faster than Precision Plus • Target temp of 115 ° C • Integrated disposable hand piece
 PROSTIVA® RF Therapy • Designed by Medtronic • Target lesion temperature of 115°C • 2 min 20 second per lesion • Easy set-up • User interface with touch screen controls • Platform of the future
PROSTIVA® RF Therapy • Designed by Medtronic • Target lesion temperature of 115°C • 2 min 20 second per lesion • Easy set-up • User interface with touch screen controls • Platform of the future
 PROSTIVA® RF Therapy System Components
PROSTIVA® RF Therapy System Components
 Generator Features Computer Monitored Safety Checks: • Monitors urethral and prostatic temperatures six times per second • Controls RF power 5000 times per second • Measures impedance and power 50 million times per second • Computerized graphics allow physician to view treatment in real time
Generator Features Computer Monitored Safety Checks: • Monitors urethral and prostatic temperatures six times per second • Controls RF power 5000 times per second • Measures impedance and power 50 million times per second • Computerized graphics allow physician to view treatment in real time
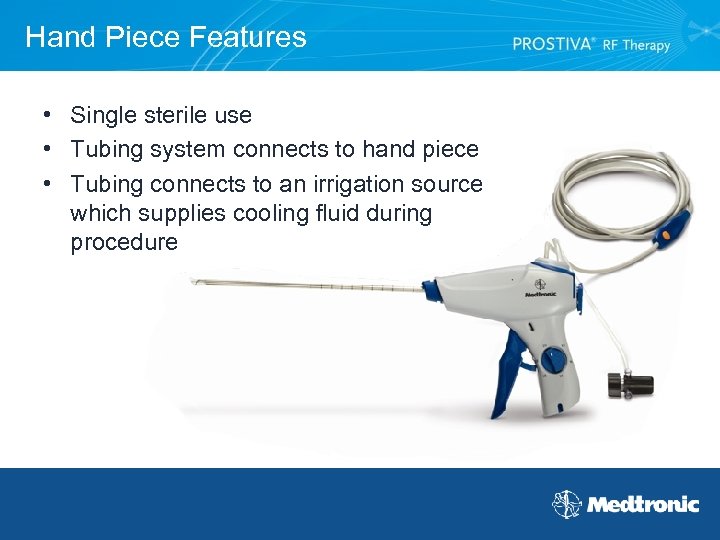 Hand Piece Features • Single sterile use • Tubing system connects to hand piece • Tubing connects to an irrigation source which supplies cooling fluid during procedure
Hand Piece Features • Single sterile use • Tubing system connects to hand piece • Tubing connects to an irrigation source which supplies cooling fluid during procedure
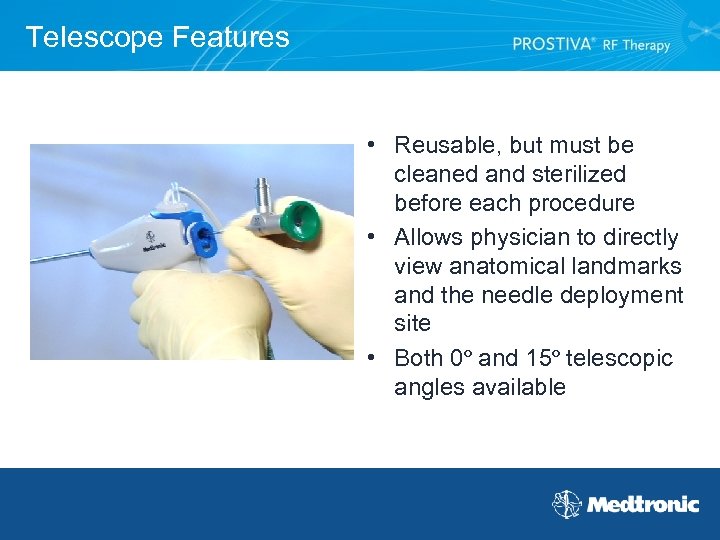 Telescope Features • Reusable, but must be cleaned and sterilized before each procedure • Allows physician to directly view anatomical landmarks and the needle deployment site • Both 0º and 15º telescopic angles available
Telescope Features • Reusable, but must be cleaned and sterilized before each procedure • Allows physician to directly view anatomical landmarks and the needle deployment site • Both 0º and 15º telescopic angles available
 Patient Selection and Assessment
Patient Selection and Assessment
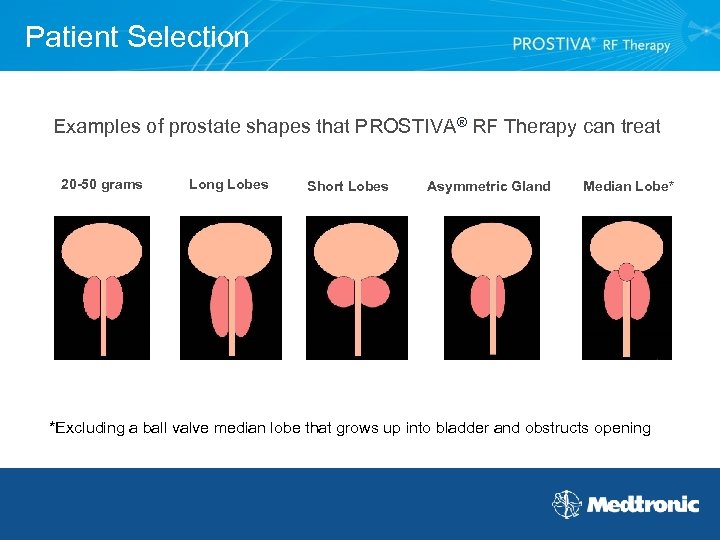 Patient Selection Examples of prostate shapes that PROSTIVA® RF Therapy can treat 20 -50 grams Long Lobes Short Lobes Asymmetric Gland Median Lobe* *Excluding a ball valve median lobe that grows up into bladder and obstructs opening
Patient Selection Examples of prostate shapes that PROSTIVA® RF Therapy can treat 20 -50 grams Long Lobes Short Lobes Asymmetric Gland Median Lobe* *Excluding a ball valve median lobe that grows up into bladder and obstructs opening
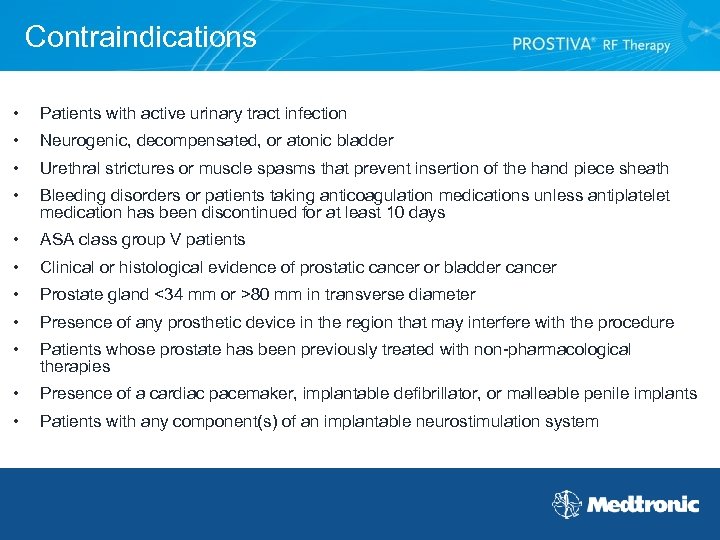 Contraindications • Patients with active urinary tract infection • Neurogenic, decompensated, or atonic bladder • Urethral strictures or muscle spasms that prevent insertion of the hand piece sheath • Bleeding disorders or patients taking anticoagulation medications unless antiplatelet medication has been discontinued for at least 10 days • ASA class group V patients • Clinical or histological evidence of prostatic cancer or bladder cancer • Prostate gland <34 mm or >80 mm in transverse diameter • Presence of any prosthetic device in the region that may interfere with the procedure • Patients whose prostate has been previously treated with non-pharmacological therapies • Presence of a cardiac pacemaker, implantable defibrillator, or malleable penile implants • Patients with any component(s) of an implantable neurostimulation system
Contraindications • Patients with active urinary tract infection • Neurogenic, decompensated, or atonic bladder • Urethral strictures or muscle spasms that prevent insertion of the hand piece sheath • Bleeding disorders or patients taking anticoagulation medications unless antiplatelet medication has been discontinued for at least 10 days • ASA class group V patients • Clinical or histological evidence of prostatic cancer or bladder cancer • Prostate gland <34 mm or >80 mm in transverse diameter • Presence of any prosthetic device in the region that may interfere with the procedure • Patients whose prostate has been previously treated with non-pharmacological therapies • Presence of a cardiac pacemaker, implantable defibrillator, or malleable penile implants • Patients with any component(s) of an implantable neurostimulation system
 PROSTIVA® RF Therapy Procedure Basic Steps
PROSTIVA® RF Therapy Procedure Basic Steps
 PROSTIVA® RF Therapy Procedure • Prepare patient • Administer comfort control • Measure prostate • Determine number of treatment planes • Treat median lobe if necessary • Create lesions
PROSTIVA® RF Therapy Procedure • Prepare patient • Administer comfort control • Measure prostate • Determine number of treatment planes • Treat median lobe if necessary • Create lesions
 Comfort Control Protocol • Describe your comfort control protocol • See Medtronic PROSTIVA® RF Therapy procedural video for several comfort control options, which can be used during the PROSTIVA RF procedure. Medical practice is solely the responsibility of the individual physician and not Medtronic.
Comfort Control Protocol • Describe your comfort control protocol • See Medtronic PROSTIVA® RF Therapy procedural video for several comfort control options, which can be used during the PROSTIVA RF procedure. Medical practice is solely the responsibility of the individual physician and not Medtronic.
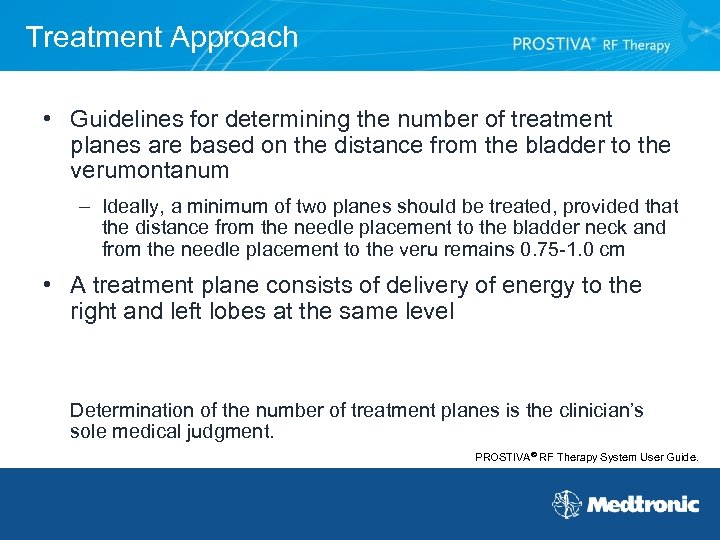 Treatment Approach • Guidelines for determining the number of treatment planes are based on the distance from the bladder to the verumontanum – Ideally, a minimum of two planes should be treated, provided that the distance from the needle placement to the bladder neck and from the needle placement to the veru remains 0. 75 -1. 0 cm • A treatment plane consists of delivery of energy to the right and left lobes at the same level Determination of the number of treatment planes is the clinician’s sole medical judgment. PROSTIVA® RF Therapy System User Guide.
Treatment Approach • Guidelines for determining the number of treatment planes are based on the distance from the bladder to the verumontanum – Ideally, a minimum of two planes should be treated, provided that the distance from the needle placement to the bladder neck and from the needle placement to the veru remains 0. 75 -1. 0 cm • A treatment plane consists of delivery of energy to the right and left lobes at the same level Determination of the number of treatment planes is the clinician’s sole medical judgment. PROSTIVA® RF Therapy System User Guide.
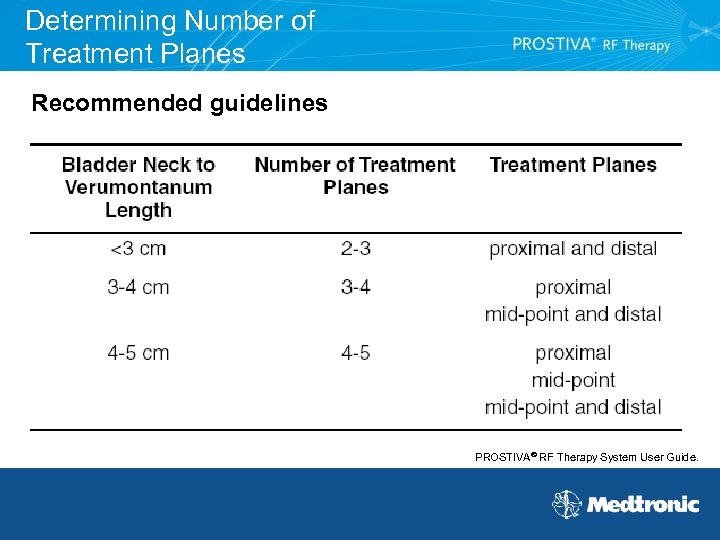 Determining Number of Treatment Planes Recommended guidelines PROSTIVA® RF Therapy System User Guide.
Determining Number of Treatment Planes Recommended guidelines PROSTIVA® RF Therapy System User Guide.
 Median Lobe Treatment • Visualize size and structure • Needles should be deployed 1 cm away from the proximal margin of the bladder neck • Select needle length of 12 or 14 is recommended Determination of median lobe treatment locations and appropriate needle length is the clinician’s sole medical judgment. PROSTIVA® RF Therapy System User Guide.
Median Lobe Treatment • Visualize size and structure • Needles should be deployed 1 cm away from the proximal margin of the bladder neck • Select needle length of 12 or 14 is recommended Determination of median lobe treatment locations and appropriate needle length is the clinician’s sole medical judgment. PROSTIVA® RF Therapy System User Guide.
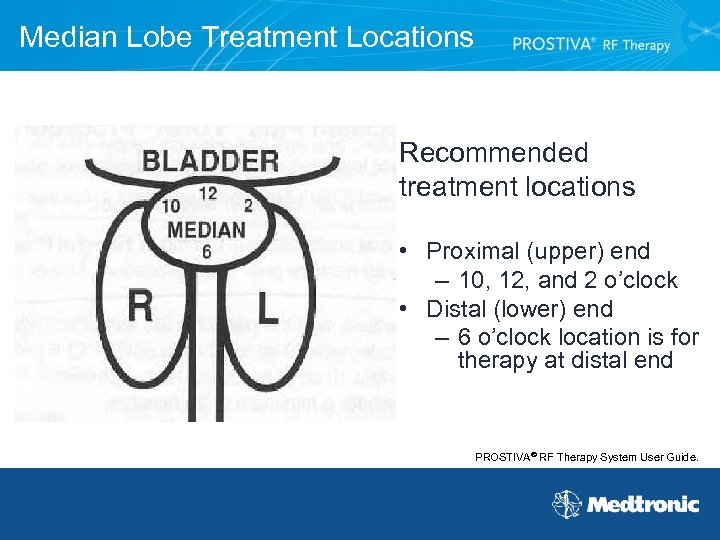 Median Lobe Treatment Locations Recommended treatment locations • Proximal (upper) end – 10, 12, and 2 o’clock • Distal (lower) end – 6 o’clock location is for therapy at distal end PROSTIVA® RF Therapy System User Guide.
Median Lobe Treatment Locations Recommended treatment locations • Proximal (upper) end – 10, 12, and 2 o’clock • Distal (lower) end – 6 o’clock location is for therapy at distal end PROSTIVA® RF Therapy System User Guide.
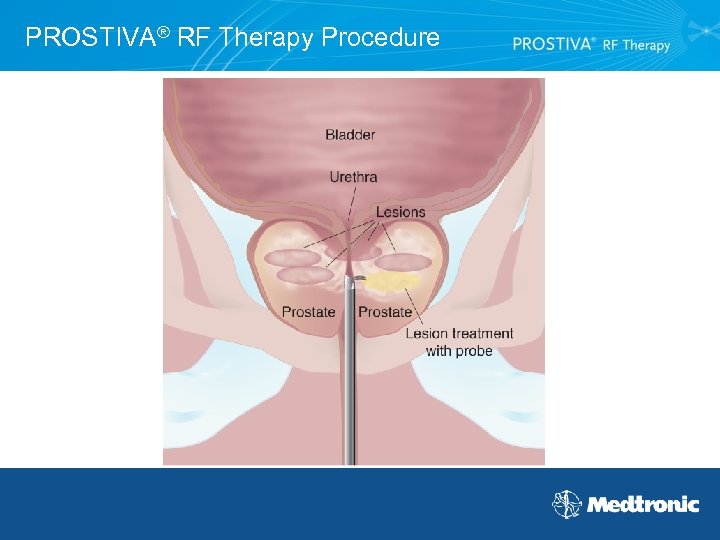 PROSTIVA® RF Therapy Procedure
PROSTIVA® RF Therapy Procedure
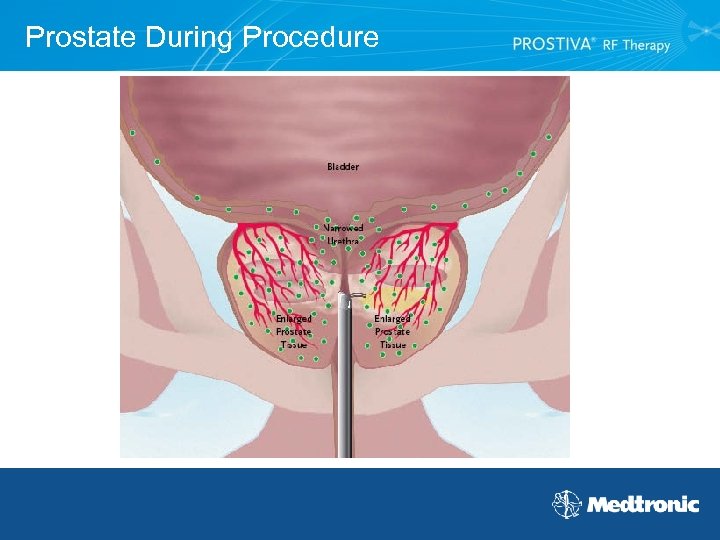 Prostate During Procedure
Prostate During Procedure
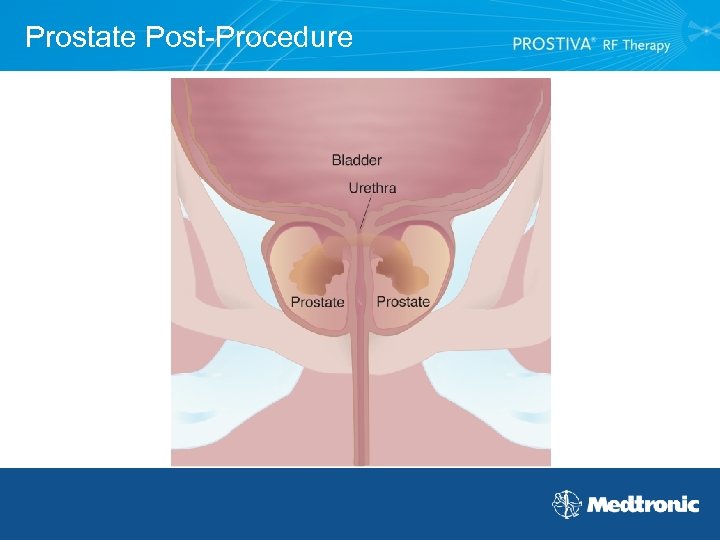 Prostate Post-Procedure
Prostate Post-Procedure
 MRI Image Post-Procedure Click on picture to show MRI image
MRI Image Post-Procedure Click on picture to show MRI image
 Reimbursement
Reimbursement
 Reimbursement Status • PROSTIVA® RF Therapy coverage: – Medicare in all 50 states – Many private pay and managed care insurance companies • Most patients will be responsible for a deductible and/or co-payment • Medicare reimburses physicians for performing the PROSTIVA RF Therapy procedure in their offices (there is a site of service differential)
Reimbursement Status • PROSTIVA® RF Therapy coverage: – Medicare in all 50 states – Many private pay and managed care insurance companies • Most patients will be responsible for a deductible and/or co-payment • Medicare reimburses physicians for performing the PROSTIVA RF Therapy procedure in their offices (there is a site of service differential)
 Clinical
Clinical
 Outcomes • Would you perform the PROSTIVA® RF Therapy procedure on your father? • Why do you think PROSTIVA RF Therapy works?
Outcomes • Would you perform the PROSTIVA® RF Therapy procedure on your father? • Why do you think PROSTIVA RF Therapy works?
 PROSTIVA® RF Therapy Long-term Durability Can you speak to long-term durability? • Hill B, Belville W, Bruskewitz R, Issa M, Perez-Marrero R, Roehrborn C, Terris M, Naslund M, “Transurethral Needle Ablation versus Transurethral Resection of the Prostate for the Treatment of Symptomatic Benign Prostatic Hyperplasia: 5 -Year Results of a Prospective, Randomized, Multicenter Clinical Trial, ” J Urol, 2004; 171: 2336 -2340 • Zlotta, AR, Giannakopoulos X, Maehlum O, Ostrem T, Schulman CC, “Long. Term Evaluation of Transurethral Needle Ablation of the Prostate (TUNA) for Treatment of Symptomatic Benign Prostatic Hyperplasia: Clinical Outcome Up To Five Years From Three Centers, ” Eur Urol, 2003; 44: 89 -93 • Boyle P, Robertson C, Vaughan E D, Fitzpatrick J, “A Meta-Analysis of Trials of Transurethral Needle Ablation for Treating Symptomatic Benign Prostatic Hyperplasia”, British Journal of Urology Intl, 2004; 94: 83 -88. • AUA Guidelines 2004, “Management of Benign Prostatic Hyperplasia: Diagnosis and Treatment Recommendations” Chapter 1, page 27.
PROSTIVA® RF Therapy Long-term Durability Can you speak to long-term durability? • Hill B, Belville W, Bruskewitz R, Issa M, Perez-Marrero R, Roehrborn C, Terris M, Naslund M, “Transurethral Needle Ablation versus Transurethral Resection of the Prostate for the Treatment of Symptomatic Benign Prostatic Hyperplasia: 5 -Year Results of a Prospective, Randomized, Multicenter Clinical Trial, ” J Urol, 2004; 171: 2336 -2340 • Zlotta, AR, Giannakopoulos X, Maehlum O, Ostrem T, Schulman CC, “Long. Term Evaluation of Transurethral Needle Ablation of the Prostate (TUNA) for Treatment of Symptomatic Benign Prostatic Hyperplasia: Clinical Outcome Up To Five Years From Three Centers, ” Eur Urol, 2003; 44: 89 -93 • Boyle P, Robertson C, Vaughan E D, Fitzpatrick J, “A Meta-Analysis of Trials of Transurethral Needle Ablation for Treating Symptomatic Benign Prostatic Hyperplasia”, British Journal of Urology Intl, 2004; 94: 83 -88. • AUA Guidelines 2004, “Management of Benign Prostatic Hyperplasia: Diagnosis and Treatment Recommendations” Chapter 1, page 27.
 References • • • Issa M, Marshall F. Contemporary Diagnosis and Management of Diseases of the Prostate. 3 rd ed. Newtown, Pa: Handbooks in Healthcare Co; 2005. American Urological Association Education and Research, Inc. AUA Guideline 2003/Updated 2006. O’Leary MP. LUTS, ED, QOL: alphabet soup or real concerns to aging men? Urology, 2000; 56(suppl 5 A): 7 -11. Boschef, et al. , “In vitro assessment of the efficacy of thermal therapy in human benign prostate hyperplasia, ” ASME, 2001 Nov; 2001. PROSTIVA RF Therapy Model 8930 System User Guide, 4 -3. Perchino M, et al. , “Does transurethral thermotherapy induce a long-term alpha blockade? An immunohistochemical study, ” Eur Urol, 1993, 23: 299 -301. Larson, Thayne. Institute of Medical Research and Lance Mynderse, M. D. , Mayo Clinic. “MRI study of 12 patients with average of 64, treatment focus on bladder neck and lateral lobe, ” 2006 Medtronic RF Therapy Study. http: //www. drugstore. com. Accessed March 7, 2006. PROSTIVA® RF Therapy System User Guide. Safety information from System User Guide is available at www. prostiva. com.
References • • • Issa M, Marshall F. Contemporary Diagnosis and Management of Diseases of the Prostate. 3 rd ed. Newtown, Pa: Handbooks in Healthcare Co; 2005. American Urological Association Education and Research, Inc. AUA Guideline 2003/Updated 2006. O’Leary MP. LUTS, ED, QOL: alphabet soup or real concerns to aging men? Urology, 2000; 56(suppl 5 A): 7 -11. Boschef, et al. , “In vitro assessment of the efficacy of thermal therapy in human benign prostate hyperplasia, ” ASME, 2001 Nov; 2001. PROSTIVA RF Therapy Model 8930 System User Guide, 4 -3. Perchino M, et al. , “Does transurethral thermotherapy induce a long-term alpha blockade? An immunohistochemical study, ” Eur Urol, 1993, 23: 299 -301. Larson, Thayne. Institute of Medical Research and Lance Mynderse, M. D. , Mayo Clinic. “MRI study of 12 patients with average of 64, treatment focus on bladder neck and lateral lobe, ” 2006 Medtronic RF Therapy Study. http: //www. drugstore. com. Accessed March 7, 2006. PROSTIVA® RF Therapy System User Guide. Safety information from System User Guide is available at www. prostiva. com.
 References • Hill B, Belville W, Bruskewitz R, Issa M, Perez-Marrero R, Roehrborn C, Terris M, Naslund M, “Transurethral Needle Ablation versus Transurethral Resection of the Prostate for the Treatment of Symptomatic Benign Prostatic Hyperplasia: 5 -Year Results of a Prospective, Randomized, Multicenter Clinical Trial, ” J Urol, 2004; 171: 2336 -2340. • Nickel JC, “Long-term implications of medical therapy on benign prostatic hyperplasia end points, ” Urology, 1998; 51(suppl 4 A): 50 -57. • Borth CS, Beiko DT, Nickel JC, “Impact of medical therapy on transurethral resection of the prostate: a decade of change, ” Urology, 001; 57: 1082 -1086. • Mebust WK, Holtgrewe HL, Cockett ATK, Peters PC, for the Writing Committee. “Transurethral prostatectomy: immediate and postoperative complications. A cooperative study of 13 participating institutions evaluating 3, 885 patients, ” J Urol, 1989; 141: 243 -247. • Wagner JR, Russo P, “Urologic complications of major pelvic surgery, ” Semin Surg Oncol, 2000; 18: 216 -228. For more information about PROSTIVA® RF Therapy, call (800) 643 -9099, x 6000; or visit www. prostiva. com CAUTION: Federal law (USA) restricts this device to sale by or on the order of a physician.
References • Hill B, Belville W, Bruskewitz R, Issa M, Perez-Marrero R, Roehrborn C, Terris M, Naslund M, “Transurethral Needle Ablation versus Transurethral Resection of the Prostate for the Treatment of Symptomatic Benign Prostatic Hyperplasia: 5 -Year Results of a Prospective, Randomized, Multicenter Clinical Trial, ” J Urol, 2004; 171: 2336 -2340. • Nickel JC, “Long-term implications of medical therapy on benign prostatic hyperplasia end points, ” Urology, 1998; 51(suppl 4 A): 50 -57. • Borth CS, Beiko DT, Nickel JC, “Impact of medical therapy on transurethral resection of the prostate: a decade of change, ” Urology, 001; 57: 1082 -1086. • Mebust WK, Holtgrewe HL, Cockett ATK, Peters PC, for the Writing Committee. “Transurethral prostatectomy: immediate and postoperative complications. A cooperative study of 13 participating institutions evaluating 3, 885 patients, ” J Urol, 1989; 141: 243 -247. • Wagner JR, Russo P, “Urologic complications of major pelvic surgery, ” Semin Surg Oncol, 2000; 18: 216 -228. For more information about PROSTIVA® RF Therapy, call (800) 643 -9099, x 6000; or visit www. prostiva. com CAUTION: Federal law (USA) restricts this device to sale by or on the order of a physician.


