50ad1c2575e8706f52722e18e8706ab8.ppt
- Количество слайдов: 12
Anatomic and Functional Evaluation of Bifurcation Lesions Undergoing Percutaneous Coronary Intervention Bon-Kwon Koo, MD, Ph. D, 1, 2 Katsuhisa Waseda, MD, Ph. D, 2 Hyun-Jae Kang, MD, Ph. D, 1 Hyo-Soo Kim, MD, Ph. D, 1 Chang-Wook Nam, MD, Ph. D, 3 Seung-Ho Hur, MD, Ph. D, 3 Jung-Sun Kim, MD, Ph. D, 4 Donghoon Choi, MD, Ph. D, 4 Yangsoo Jang, MD, Ph. D, 4 Joo-Yong Hahn, MD, Ph. D, 5 Hyeon-Cheol Gwon, MD, Ph. D, 5 Myeong-Ho Yoon, MD, Ph. D, 6 Seung-Jea Tahk, MD, Ph. D, 6 Woo-Young Chung, MD, Ph. D, 7 Young-Seok Cho, MD, Ph. D, 8 Dong-Ju Choi, MD, Ph. D, 8 Takao Hasegawa, MD, 9 Toru Kataoka, MD, 9 Sung Jin Oh, MD, 10 Yasuhiro Honda, MD, 2 Peter J Fitzgerald, MD, Ph. D, 2 William F. Fearon, MD, 2 1 Seoul National University Hospital, Seoul, Korea, 2 Stanford University Medical Center, Stanford, USA, University Dongsan Medical Center, Daegu, Korea, 4 Yonsei Cardiovascular Center, Seoul, Korea, 5 Samsung Medical Center, Seoul, Korea, 6 Ajou university school of medicine, Gyeonggi-do, Korea, 7 Seoul National University, Borame Hospital, Seoul, Korea, 8 Seoul National University Bundang Hospital, Gyeonggi-do, Korea, 9 Osaka City University Graduate School of Medicine, Osaka, Japan, 10 NHIC Ilsan Hospital, Gyeonggi-do, Korea 3 Keimyung
Background The mechanism of side branch (SB) luminal narrowing after main branch (MB) stent implantation in coronary bifurcation lesions is not completely understood.
Methods Patients with de novo, proximal or mid LAD - diagonal coronary bifurcation lesions Prospective multicenter trial (8 centers, US, Japan and Korea) SB lesion : minimum diameter of the SB >2 mm, vessel length >40 mm & SB lesion length <10 mm by visual estimation All patients underwent MB IVUS before and after MB stent implantation FFR of the jailed SB lesions MB lesion type A - when the site of MLA was located in the MB proximal to the takeoff of the SB
Intravascular ultrasound (IVUS) • A standard fashion using an automated motorized pullback system (0. 5 mm/s) • Intracoronary nitroglycerin(100~200 ug) before each IVUS run • Blind core-lab analysis at Stanford University Medical center
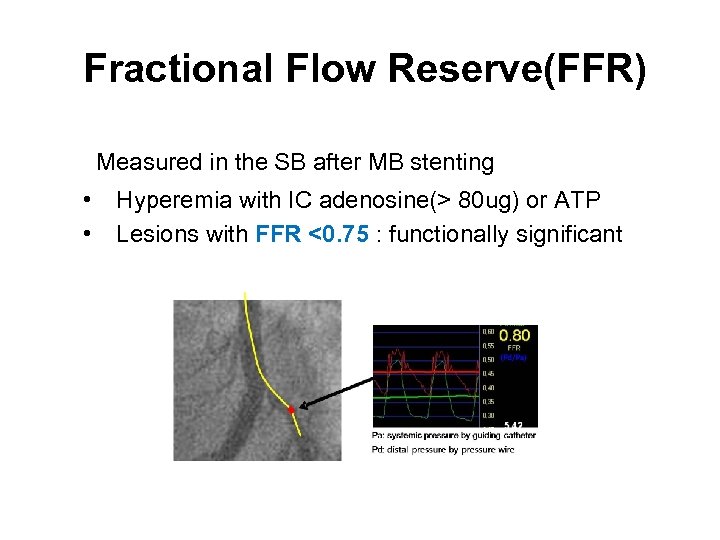
Fractional Flow Reserve(FFR) Measured in the SB after MB stenting • • Hyperemia with IC adenosine(> 80 ug) or ATP Lesions with FFR <0. 75 : functionally significant
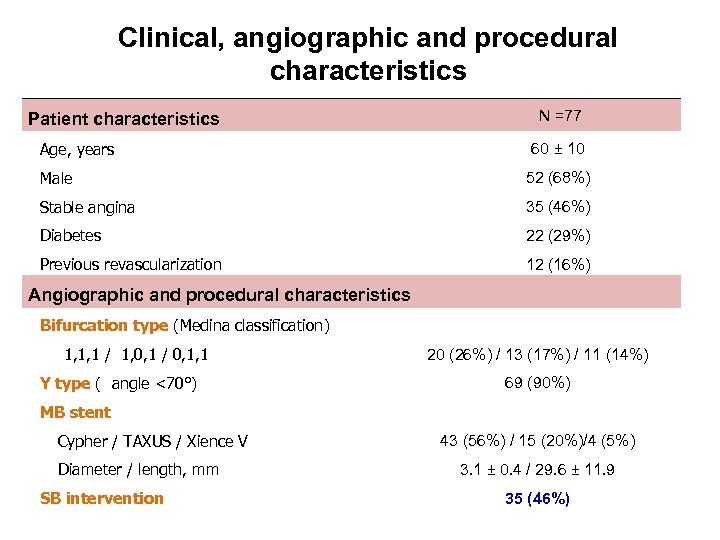
Clinical, angiographic and procedural characteristics Patient characteristics Age, years N =77 60 ± 10 Male 52 (68%) Stable angina 35 (46%) Diabetes 22 (29%) Previous revascularization 12 (16%) Angiographic and procedural characteristics Bifurcation type (Medina classification) 1, 1, 1 / 1, 0, 1 / 0, 1, 1 Y type ( angle <70°) 20 (26%) / 13 (17%) / 11 (14%) 69 (90%) MB stent Cypher / TAXUS / Xience V Diameter / length, mm SB intervention 43 (56%) / 15 (20%)/4 (5%) 3. 1 ± 0. 4 / 29. 6 ± 11. 9 35 (46%)
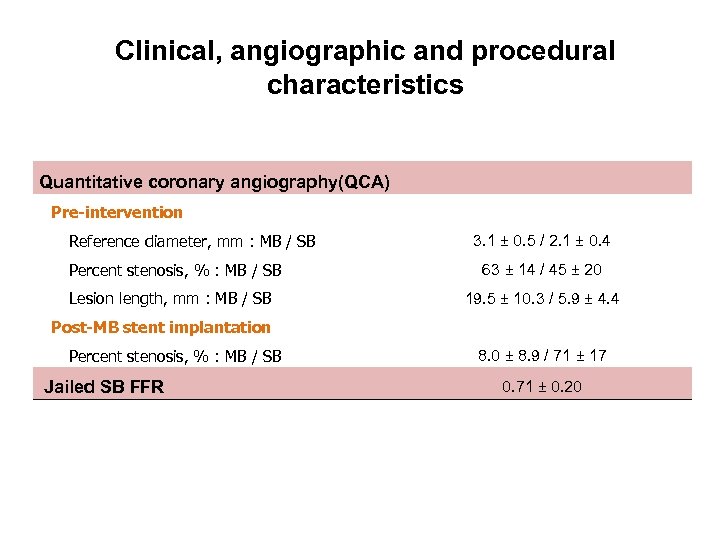
Clinical, angiographic and procedural characteristics Quantitative coronary angiography(QCA) Pre-intervention Reference diameter, mm : MB / SB 3. 1 ± 0. 5 / 2. 1 ± 0. 4 Percent stenosis, % : MB / SB 63 ± 14 / 45 ± 20 Lesion length, mm : MB / SB 19. 5 ± 10. 3 / 5. 9 ± 4. 4 Post-MB stent implantation Percent stenosis, % : MB / SB Jailed SB FFR 8. 0 ± 8. 9 / 71 ± 17 0. 71 ± 0. 20
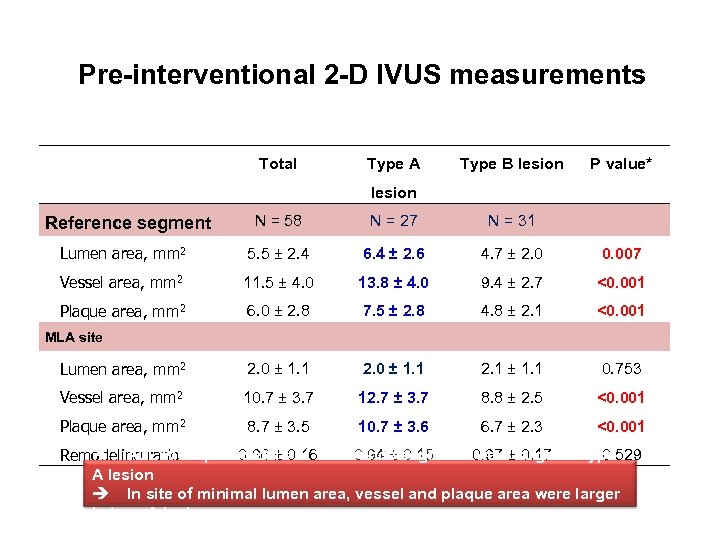
Pre-interventional 2 -D IVUS measurements Total Type A Type B lesion P value* lesion N = 58 N = 27 N = 31 Lumen area, mm 2 5. 5 ± 2. 4 6. 4 ± 2. 6 4. 7 ± 2. 0 0. 007 Vessel area, mm 2 11. 5 ± 4. 0 13. 8 ± 4. 0 9. 4 ± 2. 7 <0. 001 Plaque area, mm 2 6. 0 ± 2. 8 7. 5 ± 2. 8 4. 8 ± 2. 1 <0. 001 Lumen area, mm 2 2. 0 ± 1. 1 2. 1 ± 1. 1 0. 753 Vessel area, mm 2 10. 7 ± 3. 7 12. 7 ± 3. 7 8. 8 ± 2. 5 <0. 001 Plaque area, mm 2 8. 7 ± 3. 5 10. 7 ± 3. 6 6. 7 ± 2. 3 <0. 001 Reference segment MLA site ALL IVUS parameters 0. 16 Reference segment 0. 97 ±larger in type were 0. 17 0. 96 ± of 0. 94 ± 0. 15 0. 529 Remodeling ratio A lesion In site of minimal lumen area, vessel and plaque area were larger in type A lesion
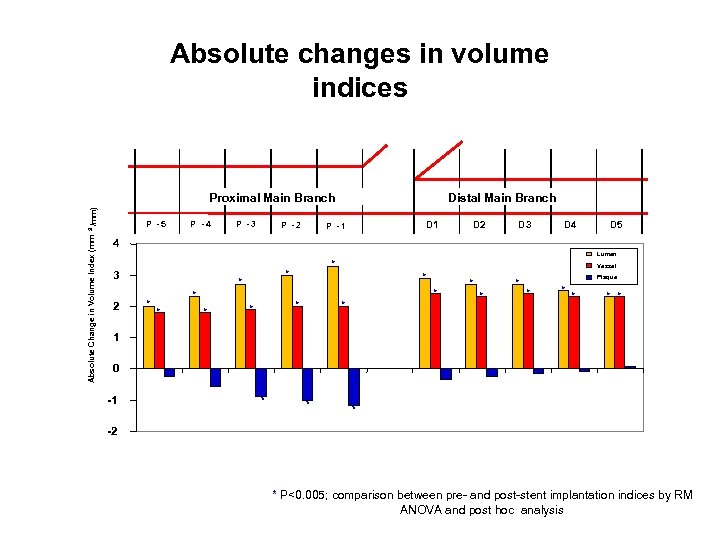
Absolute changes in volume indices /mm) Proximal Main Branch Absolute Change in Volume Index (mm 3 P -5 P -4 P -3 P -2 Distal Main Branch D 1 P -1 D 2 D 3 D 4 D 5 4 Lumen 3 2 * * Vessel * * * Plaque * * * 1 0 -1 * * * -2 * P<0. 005; comparison between pre- and post-stent implantation indices by RM ANOVA and post hoc analysis
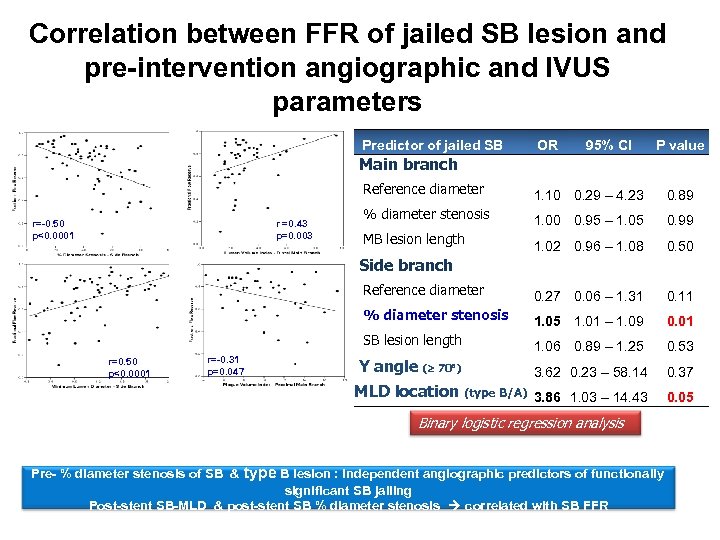
Correlation between FFR of jailed SB lesion and pre-intervention angiographic and IVUS parameters Predictor of jailed SB OR 95% CI P value Main branch Reference diameter % diameter stenosis 1. 00 0. 95 – 1. 05 0. 99 MB lesion length 1. 02 0. 96 – 1. 08 0. 50 0. 27 0. 06 – 1. 31 0. 11 % diameter stenosis 1. 05 1. 01 – 1. 09 0. 01 SB lesion length 1. 06 0. 89 – 1. 25 0. 53 Y angle ( 70 ) 3. 62 0. 23 – 58. 14 0. 37 MLD location (type B/A) 3. 86 1. 03 – 14. 43 r =0. 43 p=0. 003 0. 89 Reference diameter r=-0. 50 p<0. 0001 1. 10 0. 29 – 4. 23 0. 05 Side branch r=0. 50 p<0. 0001 r=-0. 31 p=0. 047 Binary logistic regression analysis Pre- % diameter stenosis of SB & type B lesion : independent angiographic predictors of functionally significant SB jailing Post-stent SB-MLD & post-stent SB % diameter stenosis correlated with SB FFR
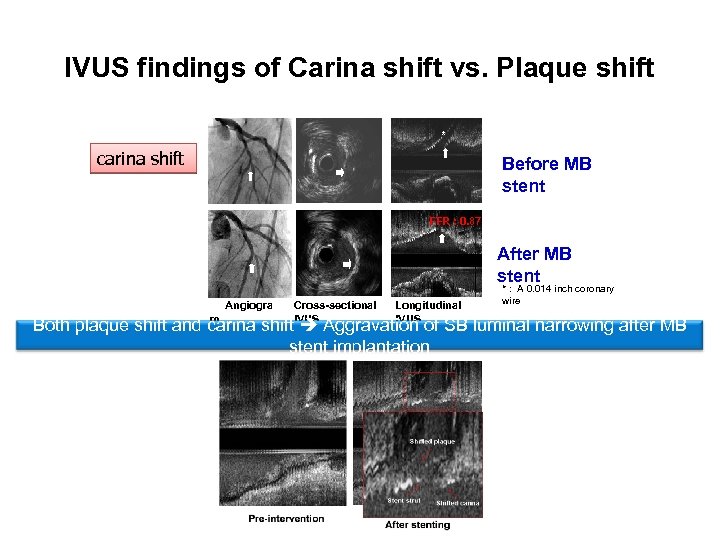
IVUS findings of Carina shift vs. Plaque shift * carina shift Before MB stent FFR : 0. 87 After MB stent Angiogra m Cross-sectional IVUS Longitudinal IVUS * : A 0. 014 inch coronary wire Both plaque shift and carina shift Aggravation of SB luminal narrowing after MB stent implantation
Conclusion • Aggravation of SB luminal narrowing after MB stent implantation results from both plaque shift and carina shift. • Anatomic evaluation does not reliably predict the functional significance of each jailed SB lesion due to the complex mechanism of luminal narrowing and its individual variability
50ad1c2575e8706f52722e18e8706ab8.ppt