dc57b809e9019dfee9b85d0cf7b4099f.ppt
- Количество слайдов: 35
 An Overview of Head Injury Management Eldad J. Hadar, M. D. Department of Neurosurgery
An Overview of Head Injury Management Eldad J. Hadar, M. D. Department of Neurosurgery
 Checklist • Definitions – Glasgow Coma Scale – Intracranial Pressure • Mechanisms of brain injury • Evaluation of head injury • Management of head injury – Operative – Nonoperative
Checklist • Definitions – Glasgow Coma Scale – Intracranial Pressure • Mechanisms of brain injury • Evaluation of head injury • Management of head injury – Operative – Nonoperative
 Head Injury Guidelines • • 1995 – 1 st edition 2000 – 2 nd edition 2007 – 3 rd edition Level I – Accepted principles reflecting high degree of clinical certainty • Level II – Strategies reflecting moderate degree of clinical certainty • Level III – Degree of clinical certainty not established
Head Injury Guidelines • • 1995 – 1 st edition 2000 – 2 nd edition 2007 – 3 rd edition Level I – Accepted principles reflecting high degree of clinical certainty • Level II – Strategies reflecting moderate degree of clinical certainty • Level III – Degree of clinical certainty not established
 Checklist Definitions – Glasgow Coma Scale – Intracranial Pressure • Mechanisms of brain injury • Evaluation of head injury • Management of head injury – Operative – Nonoperative
Checklist Definitions – Glasgow Coma Scale – Intracranial Pressure • Mechanisms of brain injury • Evaluation of head injury • Management of head injury – Operative – Nonoperative
 Glasgow Coma Scale (GCS) • Introduced by Teasdale and Jennett in 1974 • Consists of 3 clinical signs that have – Prognostic significance – Good reproducibility between observers • Scale range 3 -15 • GCS < 8 has generally become accepted as representing coma / severe head injury
Glasgow Coma Scale (GCS) • Introduced by Teasdale and Jennett in 1974 • Consists of 3 clinical signs that have – Prognostic significance – Good reproducibility between observers • Scale range 3 -15 • GCS < 8 has generally become accepted as representing coma / severe head injury
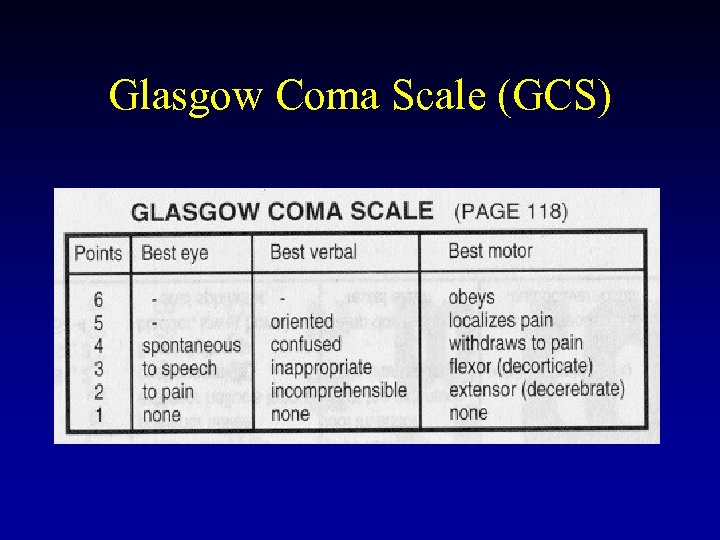 Glasgow Coma Scale (GCS)
Glasgow Coma Scale (GCS)
 Intracranial Pressure (ICP) CPP = MAP – ICP • Normal CPP > 50 mm Hg • Autoregulatory mechanisms maintain CBF at CPP’s down to 40 mm Hg
Intracranial Pressure (ICP) CPP = MAP – ICP • Normal CPP > 50 mm Hg • Autoregulatory mechanisms maintain CBF at CPP’s down to 40 mm Hg
 Intracranial Pressure (ICP) • In head injury, ICP > 20 -25 mm Hg may be more detrimental than low CPP (increasing CPP may not afford protection from intracranial hypertension). • Aggressive attempts to maintain CPP > 70 should be avoided due to ARDS (Level II) • CPP<50 should be avoided (Level III)
Intracranial Pressure (ICP) • In head injury, ICP > 20 -25 mm Hg may be more detrimental than low CPP (increasing CPP may not afford protection from intracranial hypertension). • Aggressive attempts to maintain CPP > 70 should be avoided due to ARDS (Level II) • CPP<50 should be avoided (Level III)
 Checklist • Definitions – Glasgow Coma Scale – Intracranial Pressure • Mechanisms of brain injury • Evaluation of head injury • Management of head injury – Operative – Nonoperative
Checklist • Definitions – Glasgow Coma Scale – Intracranial Pressure • Mechanisms of brain injury • Evaluation of head injury • Management of head injury – Operative – Nonoperative
 Mechanisms of Traumatic Brain Injury • Impact injury • Cerebral or brainstem contusions • Cerebral lacerations • Diffuse axonal injury (DAI) • Secondary injury • Intracranial hematoma • Edema • Ischemia
Mechanisms of Traumatic Brain Injury • Impact injury • Cerebral or brainstem contusions • Cerebral lacerations • Diffuse axonal injury (DAI) • Secondary injury • Intracranial hematoma • Edema • Ischemia
 Checklist • Statistics • Definitions – Glasgow Coma Scale – Intracranial Pressure • Mechanisms of brain injury • Evaluation of head injury • Management of head injury – Operative – Nonoperative
Checklist • Statistics • Definitions – Glasgow Coma Scale – Intracranial Pressure • Mechanisms of brain injury • Evaluation of head injury • Management of head injury – Operative – Nonoperative
 Initial Assessment Start with ABC’s History – – LOC +/Intoxicants Seizure Posttraumatic amnesia • Physical Exam – – – GCS Level of consciousness Cranial nerves Fundoscopic exam Motor exam
Initial Assessment Start with ABC’s History – – LOC +/Intoxicants Seizure Posttraumatic amnesia • Physical Exam – – – GCS Level of consciousness Cranial nerves Fundoscopic exam Motor exam
 Radiographic Evaluation • CT • Imaging study of choice for initial work-up • MRI • More helpful later in hospital course • Skull x-rays • Arteriography
Radiographic Evaluation • CT • Imaging study of choice for initial work-up • MRI • More helpful later in hospital course • Skull x-rays • Arteriography
 Indications for CT • Presence of any criteria placing patient at moderate or high risk for intracranial injury • Assessment prior to general anesthesia for other procedures
Indications for CT • Presence of any criteria placing patient at moderate or high risk for intracranial injury • Assessment prior to general anesthesia for other procedures
 Checklist • Definitions – Glasgow Coma Scale – Intracranial Pressure • Mechanisms of brain injury • Evaluation of head injury • Management of head injury – Operative – Nonoperative
Checklist • Definitions – Glasgow Coma Scale – Intracranial Pressure • Mechanisms of brain injury • Evaluation of head injury • Management of head injury – Operative – Nonoperative
 Head Injury Management • Nonoperative • Seen in absence of significant intracranial mass lesion. • Typically consists of assessment and/or treatment of intracranial pressure (ICP). • Operative • Typically required when a significant intracranial mass lesion is present. • Decompressive craniectomy or brain resection less common.
Head Injury Management • Nonoperative • Seen in absence of significant intracranial mass lesion. • Typically consists of assessment and/or treatment of intracranial pressure (ICP). • Operative • Typically required when a significant intracranial mass lesion is present. • Decompressive craniectomy or brain resection less common.
 Head Injury Management • Nonoperative • Seen in absence of significant intracranial mass lesion. • Typically consists of assessment and/or treatment of intracranial pressure (ICP). • Operative • Typically required when a significant intracranial mass lesion is present. • Decompressive craniectomy or brain resection less common.
Head Injury Management • Nonoperative • Seen in absence of significant intracranial mass lesion. • Typically consists of assessment and/or treatment of intracranial pressure (ICP). • Operative • Typically required when a significant intracranial mass lesion is present. • Decompressive craniectomy or brain resection less common.
 Nonoperative Management • • Frequent neuro checks ICP monitoring
Nonoperative Management • • Frequent neuro checks ICP monitoring
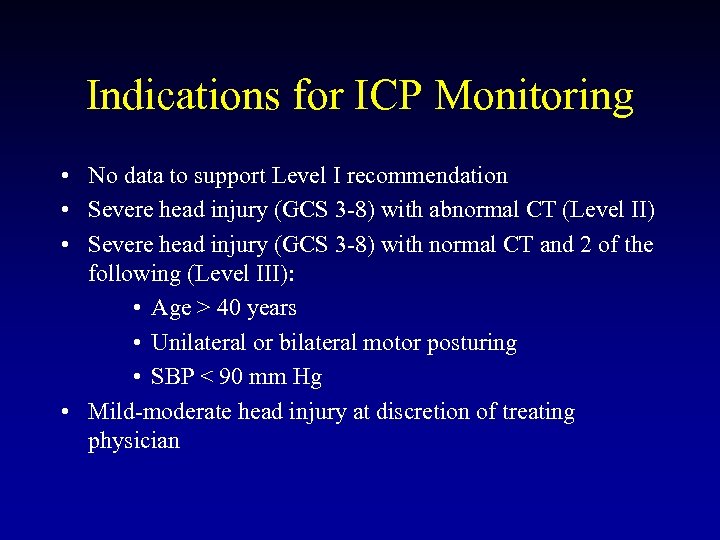 Indications for ICP Monitoring • No data to support Level I recommendation • Severe head injury (GCS 3 -8) with abnormal CT (Level II) • Severe head injury (GCS 3 -8) with normal CT and 2 of the following (Level III): • Age > 40 years • Unilateral or bilateral motor posturing • SBP < 90 mm Hg • Mild-moderate head injury at discretion of treating physician
Indications for ICP Monitoring • No data to support Level I recommendation • Severe head injury (GCS 3 -8) with abnormal CT (Level II) • Severe head injury (GCS 3 -8) with normal CT and 2 of the following (Level III): • Age > 40 years • Unilateral or bilateral motor posturing • SBP < 90 mm Hg • Mild-moderate head injury at discretion of treating physician
 Indications for ICP Monitoring • Loss of neurological examination • Sedation • General anesthesia
Indications for ICP Monitoring • Loss of neurological examination • Sedation • General anesthesia
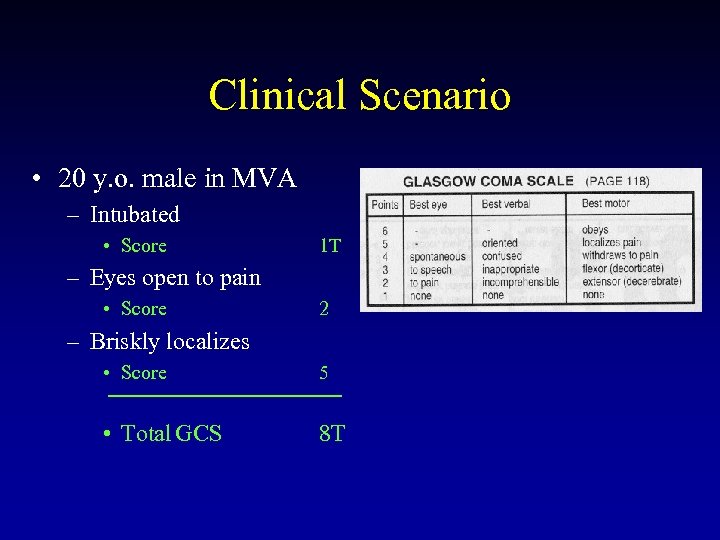 Clinical Scenario • 20 y. o. male in MVA – Intubated • Score 1 T – Eyes open to pain • Score 2 – Briskly localizes • Score 5 • Total GCS 8 T
Clinical Scenario • 20 y. o. male in MVA – Intubated • Score 1 T – Eyes open to pain • Score 2 – Briskly localizes • Score 5 • Total GCS 8 T
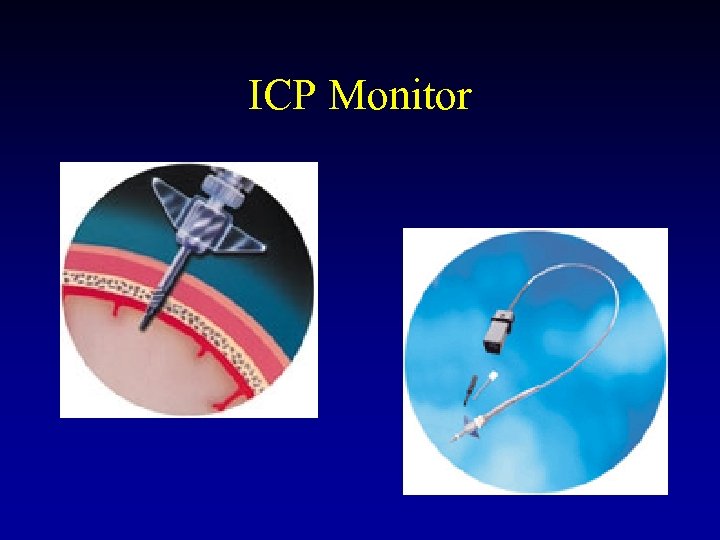 ICP Monitor
ICP Monitor
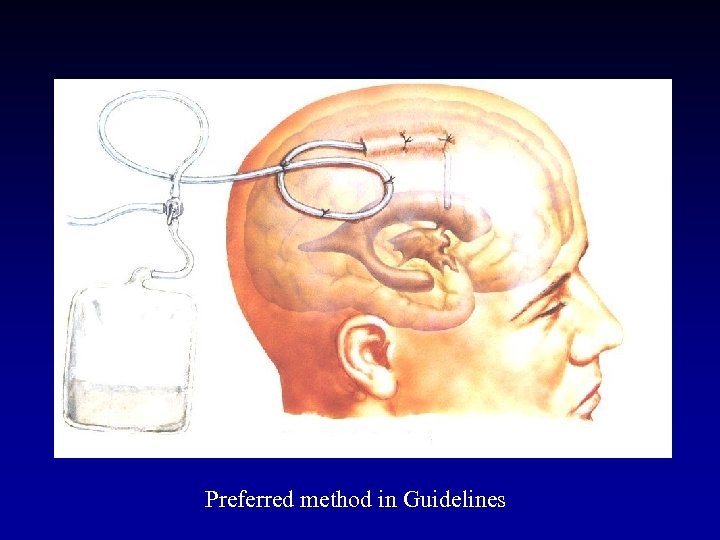 Preferred method in Guidelines
Preferred method in Guidelines
 Therapy for Intracranial Hypertension • First tier • • Positioning Ventricular drainage Osmotic diuresis Hyperventilation (Level III – temporizing measure) • Second tier • • Sedation Neuromuscular blockade Hypothermia Barbiturate coma • Glucocorticoids not recommended (Level I)
Therapy for Intracranial Hypertension • First tier • • Positioning Ventricular drainage Osmotic diuresis Hyperventilation (Level III – temporizing measure) • Second tier • • Sedation Neuromuscular blockade Hypothermia Barbiturate coma • Glucocorticoids not recommended (Level I)
 Head Injury Management • Nonoperative • Seen in absence of significant intracranial mass lesion. • Typically consists of assessment and/or treatment of intracranial pressure (ICP). • Operative • Typically required when a significant intracranial mass lesion is present. • Decompressive craniectomy or brain resection less common.
Head Injury Management • Nonoperative • Seen in absence of significant intracranial mass lesion. • Typically consists of assessment and/or treatment of intracranial pressure (ICP). • Operative • Typically required when a significant intracranial mass lesion is present. • Decompressive craniectomy or brain resection less common.
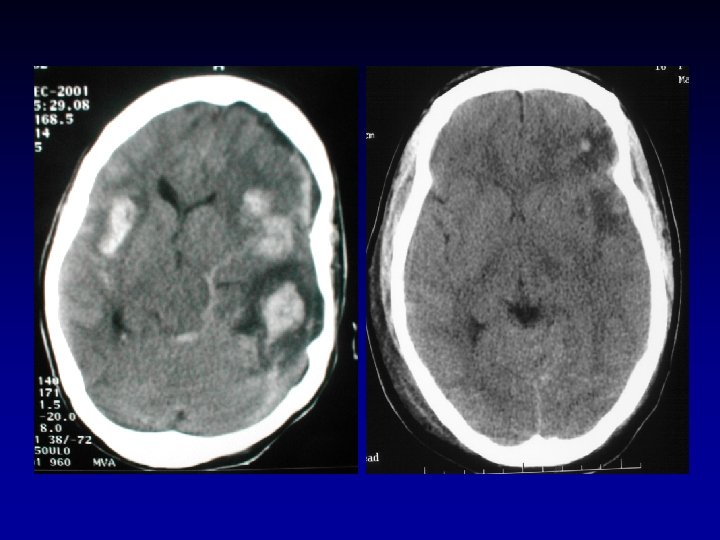
 Operative Management • Types of mass lesions • Epidural hematoma • Subdural hematoma • Cerebral contusion • Decompressive craniectomy/brain resection
Operative Management • Types of mass lesions • Epidural hematoma • Subdural hematoma • Cerebral contusion • Decompressive craniectomy/brain resection
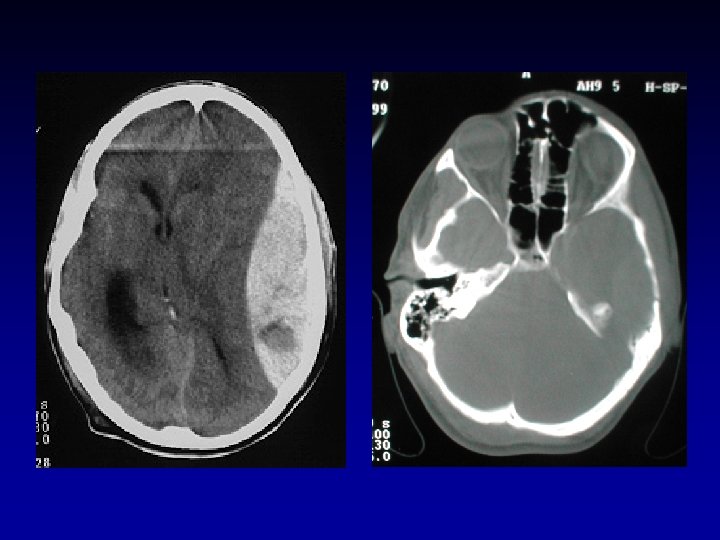
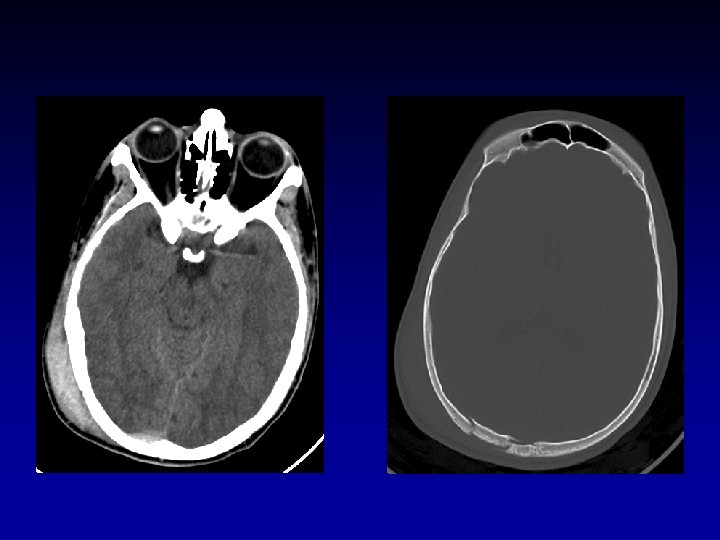
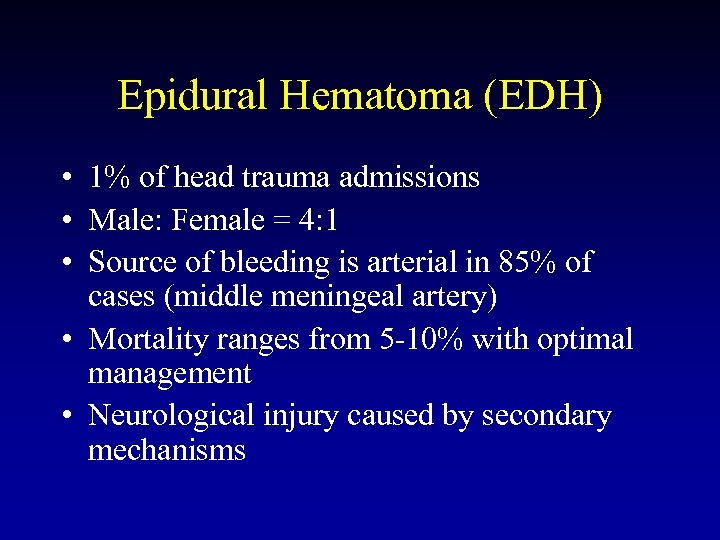 Epidural Hematoma (EDH) • 1% of head trauma admissions • Male: Female = 4: 1 • Source of bleeding is arterial in 85% of cases (middle meningeal artery) • Mortality ranges from 5 -10% with optimal management • Neurological injury caused by secondary mechanisms
Epidural Hematoma (EDH) • 1% of head trauma admissions • Male: Female = 4: 1 • Source of bleeding is arterial in 85% of cases (middle meningeal artery) • Mortality ranges from 5 -10% with optimal management • Neurological injury caused by secondary mechanisms
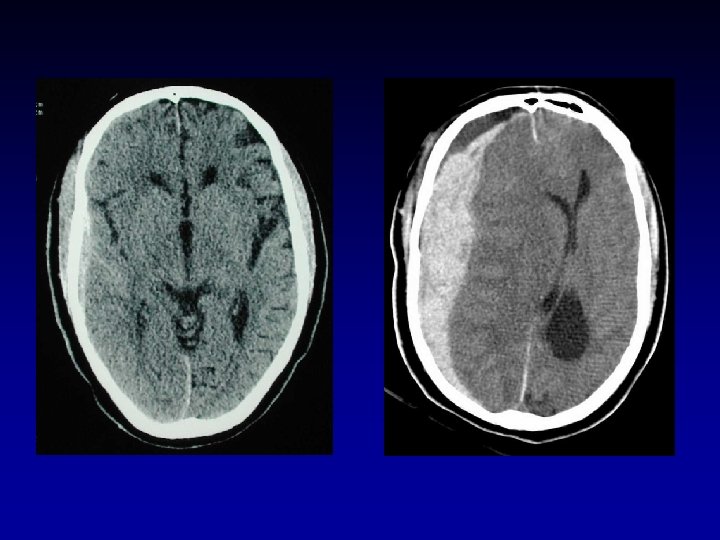
 Subdural Hematoma (SDH) • About twice as common as EDH • Mortality 50 -90% • Impact injury much higher than with EDH • Often associated brain injury • Two common sources of bleeding • Tearing of bridging veins • Cortical laceration
Subdural Hematoma (SDH) • About twice as common as EDH • Mortality 50 -90% • Impact injury much higher than with EDH • Often associated brain injury • Two common sources of bleeding • Tearing of bridging veins • Cortical laceration
 Cerebral Contusion • Often little mass effect • Not often operative
Cerebral Contusion • Often little mass effect • Not often operative
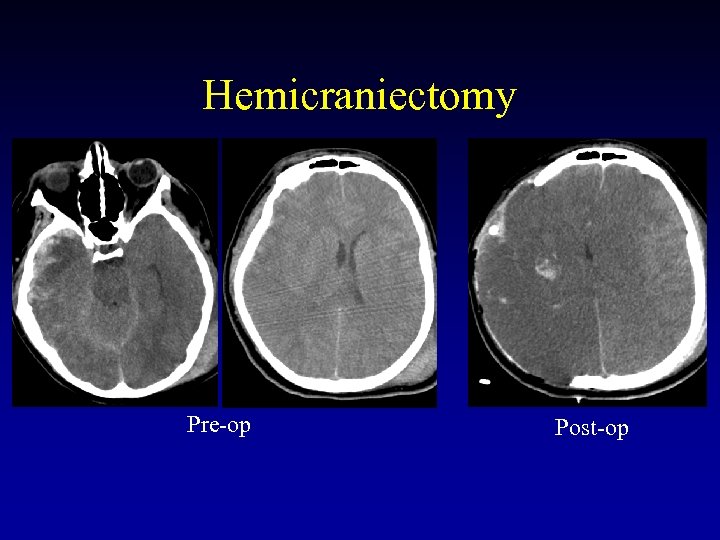 Hemicraniectomy Pre-op Post-op
Hemicraniectomy Pre-op Post-op
 Key Points • 2 mechanisms of brain injury • Impact injury • Secondary injury • GCS < 8 has generally become accepted as representing coma / severe head injury • CT is generally the imaging study of choice in the acute assessment of head injury • Operative and nonoperative strategies are generally aimed at reducing mass effect and, therefore, reducing ICP • Nothing beats a neuro exam.
Key Points • 2 mechanisms of brain injury • Impact injury • Secondary injury • GCS < 8 has generally become accepted as representing coma / severe head injury • CT is generally the imaging study of choice in the acute assessment of head injury • Operative and nonoperative strategies are generally aimed at reducing mass effect and, therefore, reducing ICP • Nothing beats a neuro exam.


