3d623dc6a66ef36683b021d48ee85a27.ppt
- Количество слайдов: 24
 An adherence intervention to support HIV Pre. Exposure Prophylaxis (Pr. EP) adherence in serodiscordant couples in Uganda Christina Psaros, Ph. D. (presenting author) Massachusetts General Hospital / Harvard Medical School, Boston, MA 6 th International Conference on HIV Treatment and Prevention Adherence May 23, 2011
An adherence intervention to support HIV Pre. Exposure Prophylaxis (Pr. EP) adherence in serodiscordant couples in Uganda Christina Psaros, Ph. D. (presenting author) Massachusetts General Hospital / Harvard Medical School, Boston, MA 6 th International Conference on HIV Treatment and Prevention Adherence May 23, 2011
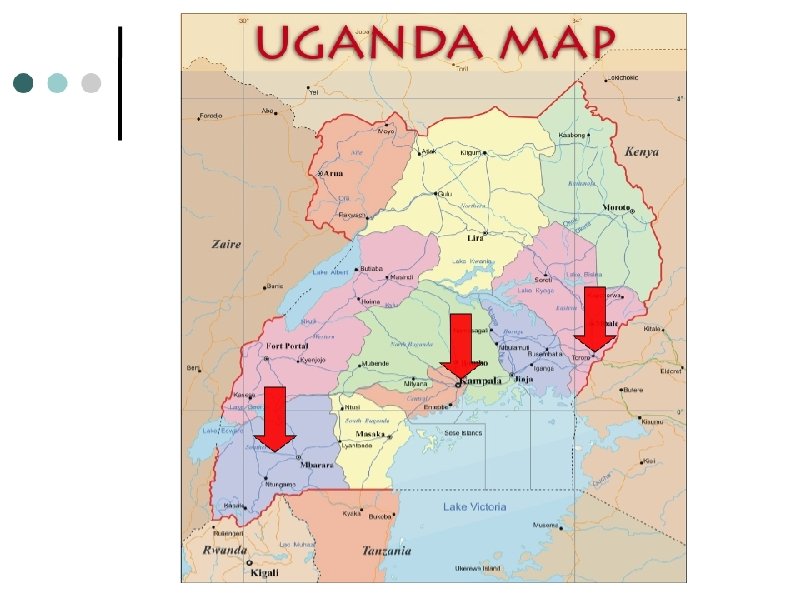
 Acknowledgements • Co-authors: Dr. David Bangsberg , Dr. Jessica Haberer , Dr. Andrew Mujugira , Dr. Alex Kintu , Dr. Kenneth Mugwanya , Dr. Michael Enyakoit , Dr. Elioda Tumwesigye , Dr. Elly Katabira , Dr. Edith Nakku-Joloba , Dr. Aloysius Kakia , Dr. Jonathan Wangisi , Dr. Jared Baeten , Dr. Connie Celum , Dr. Steven Safren • Participants and research teams in Kabwohe, Tororo, and Kampala • Collaborators at the University of Washington, DF/Net, and Massachusetts General Hospital/Harvard Medical School • Funding agency: The Bill and Melinda Gates Foundation
Acknowledgements • Co-authors: Dr. David Bangsberg , Dr. Jessica Haberer , Dr. Andrew Mujugira , Dr. Alex Kintu , Dr. Kenneth Mugwanya , Dr. Michael Enyakoit , Dr. Elioda Tumwesigye , Dr. Elly Katabira , Dr. Edith Nakku-Joloba , Dr. Aloysius Kakia , Dr. Jonathan Wangisi , Dr. Jared Baeten , Dr. Connie Celum , Dr. Steven Safren • Participants and research teams in Kabwohe, Tororo, and Kampala • Collaborators at the University of Washington, DF/Net, and Massachusetts General Hospital/Harvard Medical School • Funding agency: The Bill and Melinda Gates Foundation
 Disclosures • No conflicts of interest to declare.
Disclosures • No conflicts of interest to declare.
 Outline • Relevant background information about Pr. EP, adherence, and the Partners Pr. EP study • Process of developing a Pr. EP adherence intervention • Core components of Pr. EP adherence intervention • “Lessons learned” and implications for the future
Outline • Relevant background information about Pr. EP, adherence, and the Partners Pr. EP study • Process of developing a Pr. EP adherence intervention • Core components of Pr. EP adherence intervention • “Lessons learned” and implications for the future
 Background • Pr. EP is a promising biomedical HIV prevention method; however, effective Pr. EP use will require sustained adherence. • Findings from recent biomedical HIV prevention trials highlight the critical nature of adherence (e. g. , Grant el a. , 2010; Karim et al. , 2010). • The Partners Pr. EP Study o Ongoing phase III, double-blind, threearm, randomized, placebo-controlled trial of daily oral Pr. EP among 4700 serodiscordant African couples.
Background • Pr. EP is a promising biomedical HIV prevention method; however, effective Pr. EP use will require sustained adherence. • Findings from recent biomedical HIV prevention trials highlight the critical nature of adherence (e. g. , Grant el a. , 2010; Karim et al. , 2010). • The Partners Pr. EP Study o Ongoing phase III, double-blind, threearm, randomized, placebo-controlled trial of daily oral Pr. EP among 4700 serodiscordant African couples.
 Ancillary Adherence Study: Aims • To determine the level, pattern, and predictors of Pr. EP adherence using objective adherence measures (e. g. , MEMS, unannounced home pill counts, random drug levels). • To determine the rates and circumstances of Pr. EP sharing. • To deliver an intervention based on principles of cognitive behavioral therapy (CBT) and Motivational Interviewing (MI) targeted to HIVnegative participants with low (<80%) unannounced pill count adherence
Ancillary Adherence Study: Aims • To determine the level, pattern, and predictors of Pr. EP adherence using objective adherence measures (e. g. , MEMS, unannounced home pill counts, random drug levels). • To determine the rates and circumstances of Pr. EP sharing. • To deliver an intervention based on principles of cognitive behavioral therapy (CBT) and Motivational Interviewing (MI) targeted to HIVnegative participants with low (<80%) unannounced pill count adherence
 Intervention Fundamentals • There are no empirically supported Pr. EP adherence interventions • Intervention in progress based on the work of Safren et al on adherence to ART (Safren et al. , 1997; 2001; 2007) • Follows a CBT and M. I. model • Modular / checklist format: o Standardized provision of information while still tailoring counseling messages to individual needs o Delivery by a variety of study staff members with various levels of training o Provides a reference for future counseling
Intervention Fundamentals • There are no empirically supported Pr. EP adherence interventions • Intervention in progress based on the work of Safren et al on adherence to ART (Safren et al. , 1997; 2001; 2007) • Follows a CBT and M. I. model • Modular / checklist format: o Standardized provision of information while still tailoring counseling messages to individual needs o Delivery by a variety of study staff members with various levels of training o Provides a reference for future counseling
 Intervention Development • Goals: Standardize existing adherence counseling Refine and enhance existing adherence counseling messages to better meet specific needs of participants o Develop the best adherence counseling protocol based on behavioral science, site experience, and relevant cultural concerns; tested for effectiveness in future trials o o
Intervention Development • Goals: Standardize existing adherence counseling Refine and enhance existing adherence counseling messages to better meet specific needs of participants o Develop the best adherence counseling protocol based on behavioral science, site experience, and relevant cultural concerns; tested for effectiveness in future trials o o
 Intervention Development • Goals: Standardize existing adherence counseling Refine and enhance existing adherence counseling messages to better meet specific needs of participants o Develop the best adherence counseling protocol based on behavioral science, site experience, and relevant cultural concerns; tested for effectiveness in future trials o o
Intervention Development • Goals: Standardize existing adherence counseling Refine and enhance existing adherence counseling messages to better meet specific needs of participants o Develop the best adherence counseling protocol based on behavioral science, site experience, and relevant cultural concerns; tested for effectiveness in future trials o o
 Intervention Development • Iterative process of intervention development o Focus groups with study participants o Ongoing feedback from sites and counselors o Counselors trained over a two day-period; participate in monthly supervision calls and yearly site visits
Intervention Development • Iterative process of intervention development o Focus groups with study participants o Ongoing feedback from sites and counselors o Counselors trained over a two day-period; participate in monthly supervision calls and yearly site visits
 Intervention Delivery • After the intervention is triggered, counseling occurs in two phases: o With individual on Pr. EP § Monthly contact with interventionist § Number of sessions tailored and variable o With their HIV infected partner (optional) § Participant on Pr. EP dictates information to be shared with their partner
Intervention Delivery • After the intervention is triggered, counseling occurs in two phases: o With individual on Pr. EP § Monthly contact with interventionist § Number of sessions tailored and variable o With their HIV infected partner (optional) § Participant on Pr. EP dictates information to be shared with their partner
 Intervention Content • Module 1: Psychoeducation o o o o Basic participant information Orientation to counseling sessions Assessment sexual behavior Importance of adherence Resistance Problems with drug sharing Myths about Pr. EP Sero-conversion
Intervention Content • Module 1: Psychoeducation o o o o Basic participant information Orientation to counseling sessions Assessment sexual behavior Importance of adherence Resistance Problems with drug sharing Myths about Pr. EP Sero-conversion
 Intervention Content • Module 2: Brief Motivational Interviewing o Pros and cons of Pr. EP adherence (and study participation) § Pros: being part of the “solution”, accessing additional services, financial incentive, regular monitoring of HIV status, helping future generations § Cons: stigma related to being associated with an HIV infected person, anxiety around frequent HIV testing, burden of study visits (time off work, transportation), medication side effects (perceived and actual) o Each “con” is reviewed as a barrier to adherence during problem solving portion
Intervention Content • Module 2: Brief Motivational Interviewing o Pros and cons of Pr. EP adherence (and study participation) § Pros: being part of the “solution”, accessing additional services, financial incentive, regular monitoring of HIV status, helping future generations § Cons: stigma related to being associated with an HIV infected person, anxiety around frequent HIV testing, burden of study visits (time off work, transportation), medication side effects (perceived and actual) o Each “con” is reviewed as a barrier to adherence during problem solving portion
 Intervention Content • Module 3: Assessment of family, community, social support and privacy concerns o How these factors may support or impede adherence • Module 4: Assessment of daily routine and development of concrete medication taking schedule and reminder strategies o Involvement of an “adherence buddy” if appropriate
Intervention Content • Module 3: Assessment of family, community, social support and privacy concerns o How these factors may support or impede adherence • Module 4: Assessment of daily routine and development of concrete medication taking schedule and reminder strategies o Involvement of an “adherence buddy” if appropriate
 Intervention Content • Module 5: Identification of barriers to adherence o Sample barriers include travel (mostly unanticipated), stigma, sexual behavior changes, and partner discord • Module 6: Brief problem-solving o Identification of a plan and a back-up plan based on participant preferences and comfort, and feasibility of a solution
Intervention Content • Module 5: Identification of barriers to adherence o Sample barriers include travel (mostly unanticipated), stigma, sexual behavior changes, and partner discord • Module 6: Brief problem-solving o Identification of a plan and a back-up plan based on participant preferences and comfort, and feasibility of a solution
 Intervention Content • Module 7: Couples session Optional Focus is on issues related to Pr. EP adherence o Opportunity to explain study goals and the adherence intervention; to uncover any concerns the partner may have about Pr. EP o Provides information, correct myths, and problem-solve any relational barriers that may come up during this discussion o If partner is to serve as an “adherence buddy”, this plan is also discussed o o
Intervention Content • Module 7: Couples session Optional Focus is on issues related to Pr. EP adherence o Opportunity to explain study goals and the adherence intervention; to uncover any concerns the partner may have about Pr. EP o Provides information, correct myths, and problem-solve any relational barriers that may come up during this discussion o If partner is to serve as an “adherence buddy”, this plan is also discussed o o
 Intervention Content • Module 8: Follow-up sessions o Goals: § Review of last session and evaluation of adherence plan success (continued acceptability and effectiveness) making modifications as needed § Identification and problem-solving of new barriers to adherence
Intervention Content • Module 8: Follow-up sessions o Goals: § Review of last session and evaluation of adherence plan success (continued acceptability and effectiveness) making modifications as needed § Identification and problem-solving of new barriers to adherence
 Lessons Learned • As of May 2, 2011: 1, 029 couples have been enrolled in the adherence study o o ~ 48% female Mean age = 36. 5 [SD=8. 7] o 86 interventions have been delivered (90. 5%) • Adherence of < 80% has been detected in 95 individuals (9. 2%) • Initial follow-up adherence has improved to >80% in 86% of participants who have completed at least one intervention and have available data from a follow-up home
Lessons Learned • As of May 2, 2011: 1, 029 couples have been enrolled in the adherence study o o ~ 48% female Mean age = 36. 5 [SD=8. 7] o 86 interventions have been delivered (90. 5%) • Adherence of < 80% has been detected in 95 individuals (9. 2%) • Initial follow-up adherence has improved to >80% in 86% of participants who have completed at least one intervention and have available data from a follow-up home
 Lessons Learned • Counselor-reported barriers to adherence: o Sexual behavior changes o Partner discord o Unexpected travel • Participants report high levels of motivation to adhere to Pr. EP o Driven by wanting to improve HIV prevention for future generations • Counselors report high levels of intervention acceptability.
Lessons Learned • Counselor-reported barriers to adherence: o Sexual behavior changes o Partner discord o Unexpected travel • Participants report high levels of motivation to adhere to Pr. EP o Driven by wanting to improve HIV prevention for future generations • Counselors report high levels of intervention acceptability.
 Conclusions and Future Directions • Adapting evidenced-based treatment adherence interventions to Pr. EP adherence, with culturally-relevant topics is feasible and acceptable to counselors and participants. o Interventions developed in the clinical trial setting may differ than those delivered in the “real world”.
Conclusions and Future Directions • Adapting evidenced-based treatment adherence interventions to Pr. EP adherence, with culturally-relevant topics is feasible and acceptable to counselors and participants. o Interventions developed in the clinical trial setting may differ than those delivered in the “real world”.
 Conclusions and Future Directions • Further follow-up will address efficacy and sustainability of increasing adherence after this intervention in those with <80% adherence to daily Pr. EP. • Such work will increase confidence in interpretation of results from biomedical HIV prevention trials and will facilitate adherence and proper use of these strategies should they become widely available.
Conclusions and Future Directions • Further follow-up will address efficacy and sustainability of increasing adherence after this intervention in those with <80% adherence to daily Pr. EP. • Such work will increase confidence in interpretation of results from biomedical HIV prevention trials and will facilitate adherence and proper use of these strategies should they become widely available.