31e6f1221ae05157ef13bb8dcfc2a5c3.ppt
- Количество слайдов: 41
Allergic rhinitis in children Dr Gulamabbas Khakoo Consultant in Paediatrics, Hillingdon Hospital NHS Trust Consultant in Paediatric Allergy St Mary’s Hospital, Paddington
Scope of presentation • • Epidemiology - why allergic rhinitis is important Making a correct diagnosis Treatment Link with asthma – ? One airway, one disease
Key references • BSACI guidelines for the management of allergic and non-allergic rhinitis. Clin Exp Allergy 2007; 38: 19 -42 • Allergic rhinitis and its impact on asthma (ARIA guidelines). J Allergy Clin Immunol 2001; 108: S 147 -334
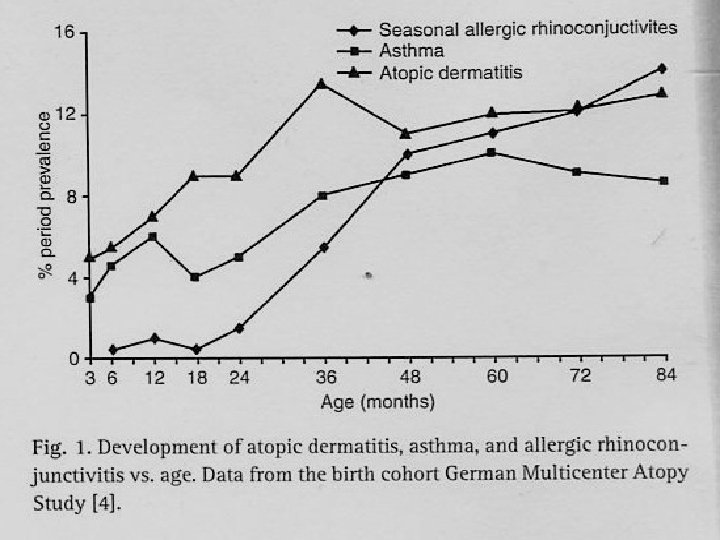
The allergic march • Distinction between sensitisation and allergy • Food allergies in early childhood tend to resolve, although food sensitisation predicts aeroallergen sensitisation • Allergic rhinitis and aeroallergen sensitisation starting earlier in childhood and recent data that it is more persistent BAMSE birth cohort Clin Exp Allergy 2008; 38: 1507 -13
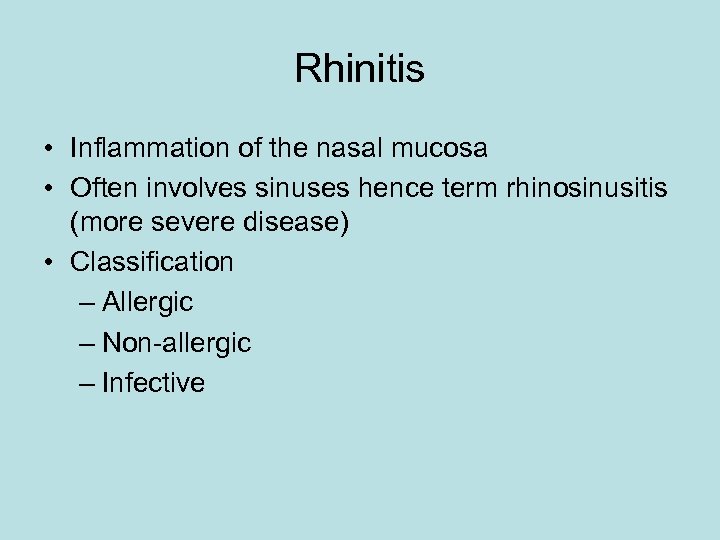
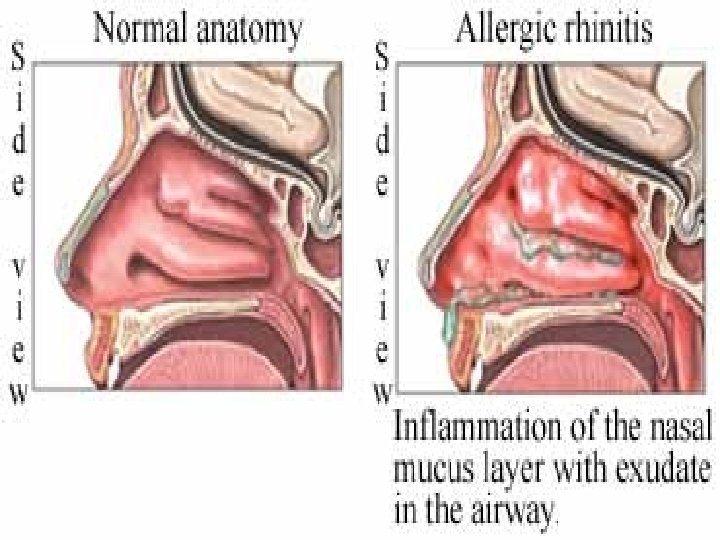
Rhinitis • Inflammation of the nasal mucosa • Often involves sinuses hence term rhinosinusitis (more severe disease) • Classification – Allergic – Non-allergic – Infective
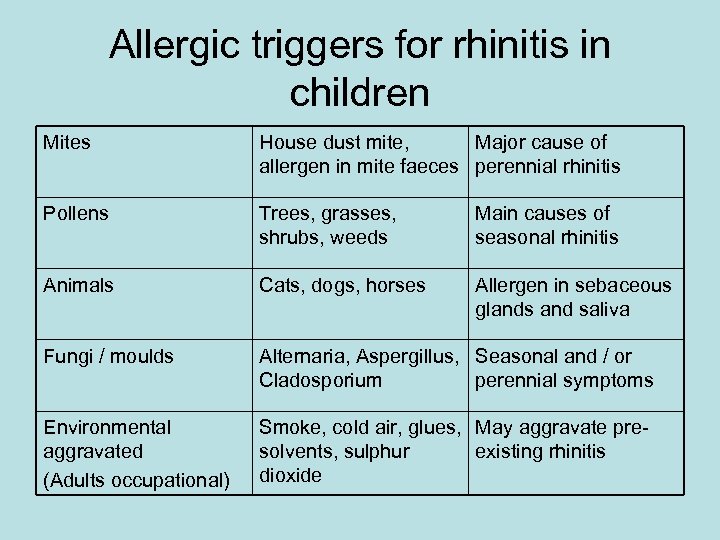
Allergic triggers for rhinitis in children Mites House dust mite, Major cause of allergen in mite faeces perennial rhinitis Pollens Trees, grasses, shrubs, weeds Main causes of seasonal rhinitis Animals Cats, dogs, horses Allergen in sebaceous glands and saliva Fungi / moulds Alternaria, Aspergillus, Seasonal and / or Cladosporium perennial symptoms Environmental aggravated (Adults occupational) Smoke, cold air, glues, May aggravate presolvents, sulphur existing rhinitis dioxide
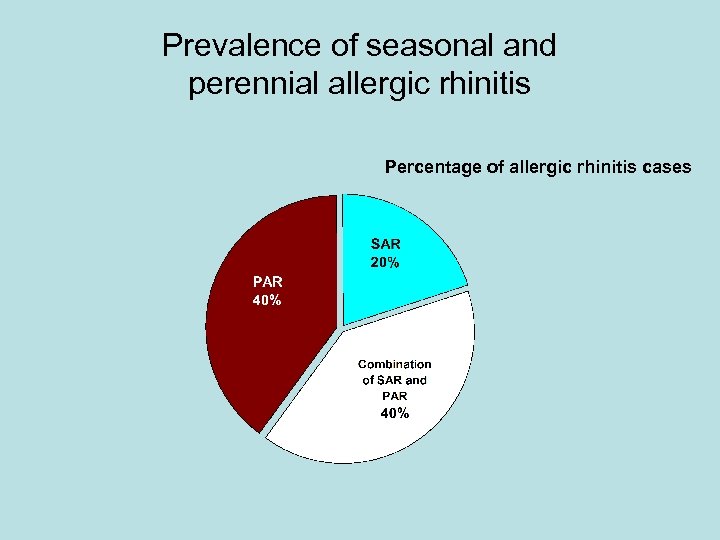
Prevalence of seasonal and perennial allergic rhinitis Percentage of allergic rhinitis cases
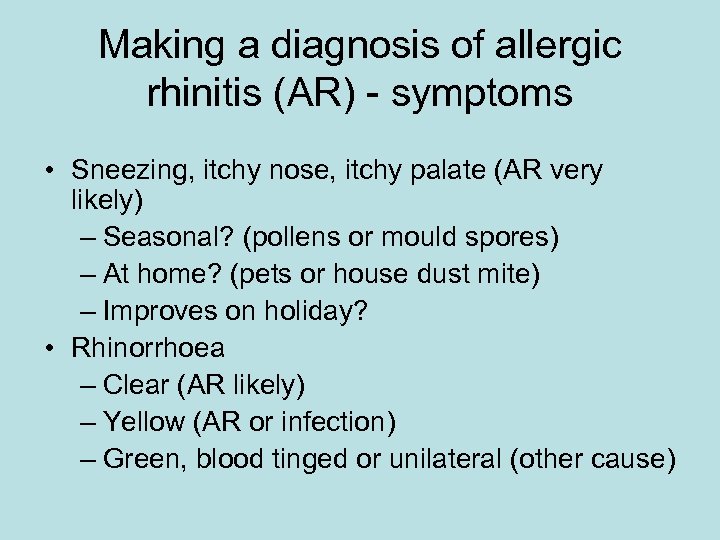
Making a diagnosis of allergic rhinitis (AR) - symptoms • Sneezing, itchy nose, itchy palate (AR very likely) – Seasonal? (pollens or mould spores) – At home? (pets or house dust mite) – Improves on holiday? • Rhinorrhoea – Clear (AR likely) – Yellow (AR or infection) – Green, blood tinged or unilateral (other cause)
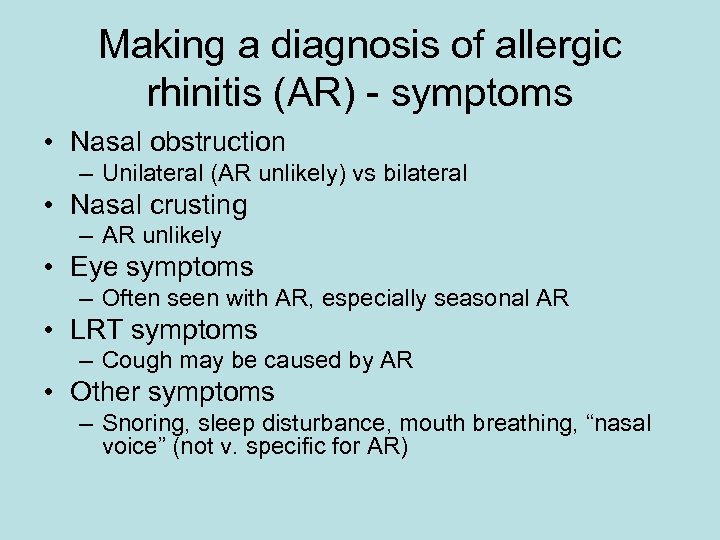
Making a diagnosis of allergic rhinitis (AR) - symptoms • Nasal obstruction – Unilateral (AR unlikely) vs bilateral • Nasal crusting – AR unlikely • Eye symptoms – Often seen with AR, especially seasonal AR • LRT symptoms – Cough may be caused by AR • Other symptoms – Snoring, sleep disturbance, mouth breathing, “nasal voice” (not v. specific for AR)
Other clues in history taking • Personal history of other allergic conditions • Family history of allergic conditions • Specific allergen and irritant exposure
Examination
Visual examination • Depressed / widened nasal bridge (AR unlikely) • Assess nasal airflow
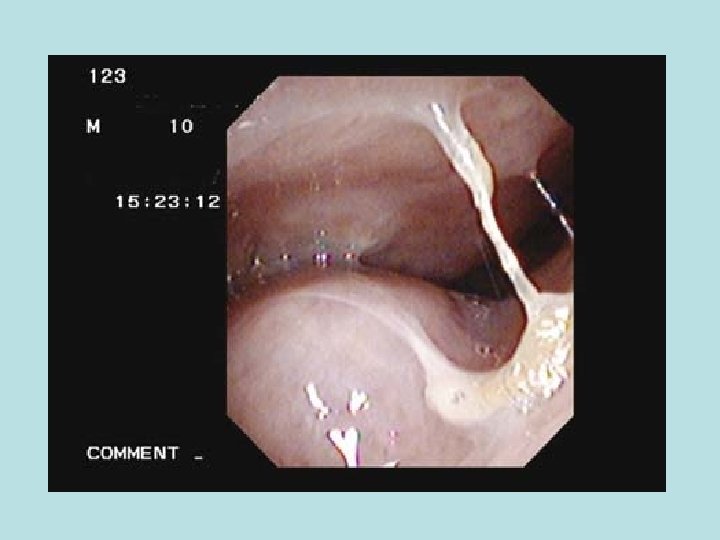
Anterior rhinoscopy • ? Purulent secretions (AR unlikely) • ? Nasal polyps (yellow/grey and lack sensitivity) • ? Nodules and crusting (AR unlikely)
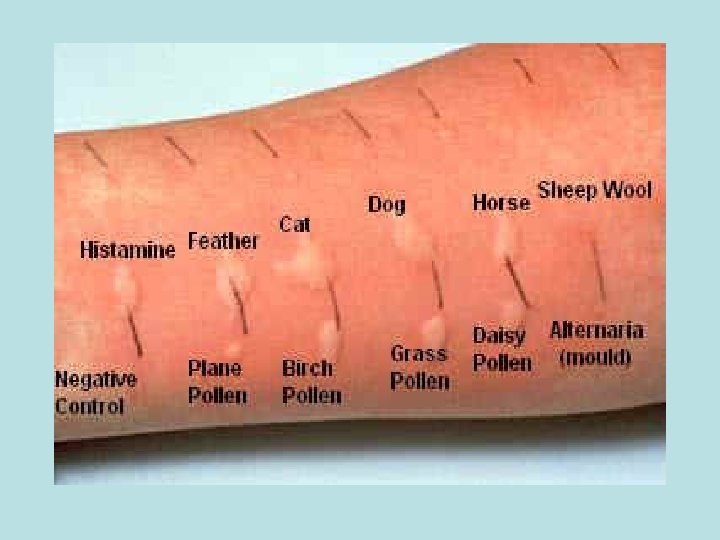
Investigations • • Peak nasal inspiratory flow Acoustic rhinometry Rhinomanometry Nasal endoscopy Total Ig. E generally unhelpful Specific Ig. E (RAST) helpful Skin prick testing – Very safe – Some contraindications
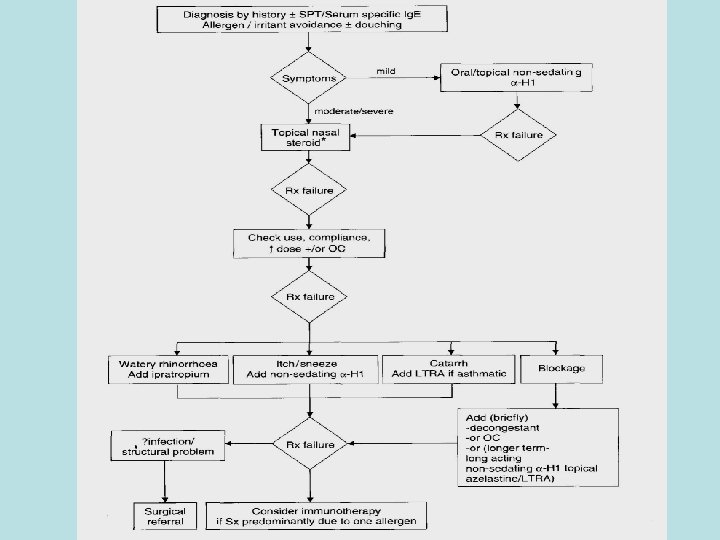
Treatment of AR
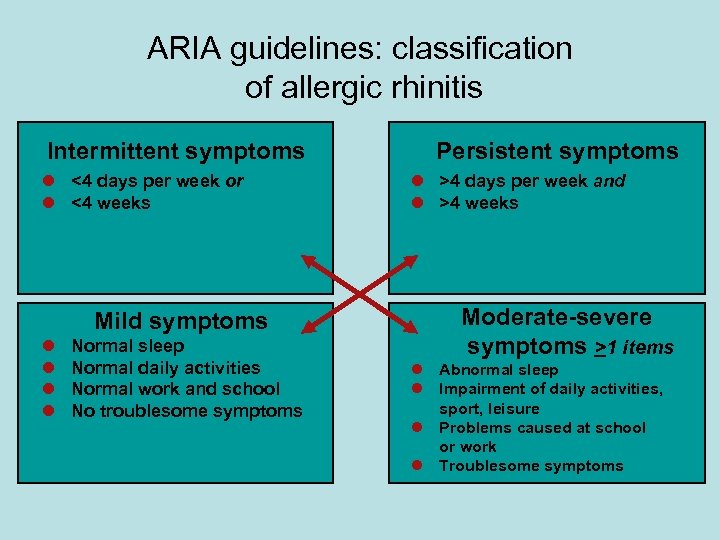
ARIA guidelines: classification of allergic rhinitis Intermittent symptoms l <4 days per week or l <4 weeks Mild symptoms l l Normal sleep Normal daily activities Normal work and school No troublesome symptoms Persistent symptoms l >4 days per week and l >4 weeks Moderate-severe symptoms >1 items l Abnormal sleep l Impairment of daily activities, sport, leisure l Problems caused at school or work l Troublesome symptoms
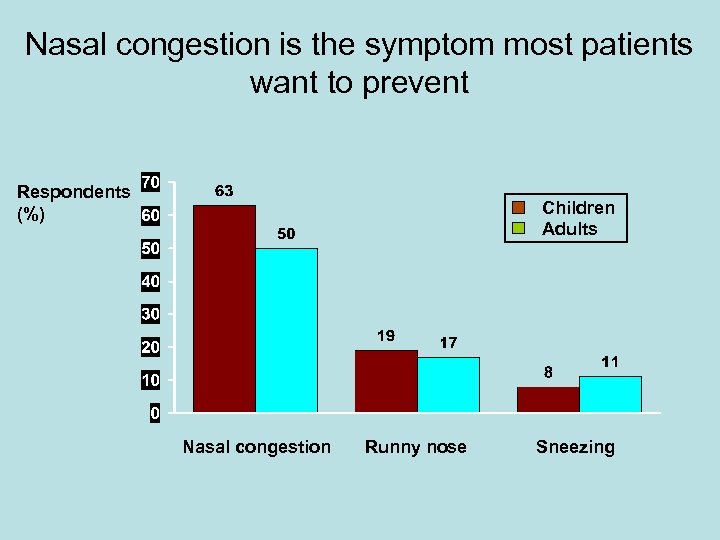
Nasal congestion is the symptom most patients want to prevent Respondents (%) Children Adults Nasal congestion Runny nose Sneezing
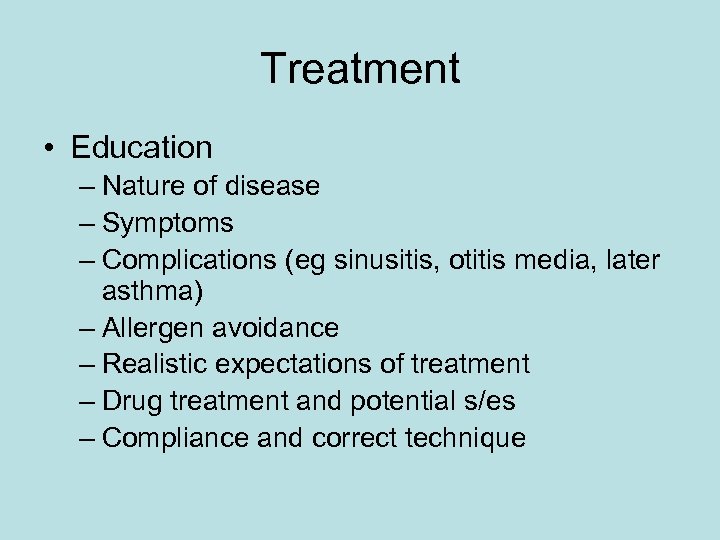
Treatment • Education – Nature of disease – Symptoms – Complications (eg sinusitis, otitis media, later asthma) – Allergen avoidance – Realistic expectations of treatment – Drug treatment and potential s/es – Compliance and correct technique
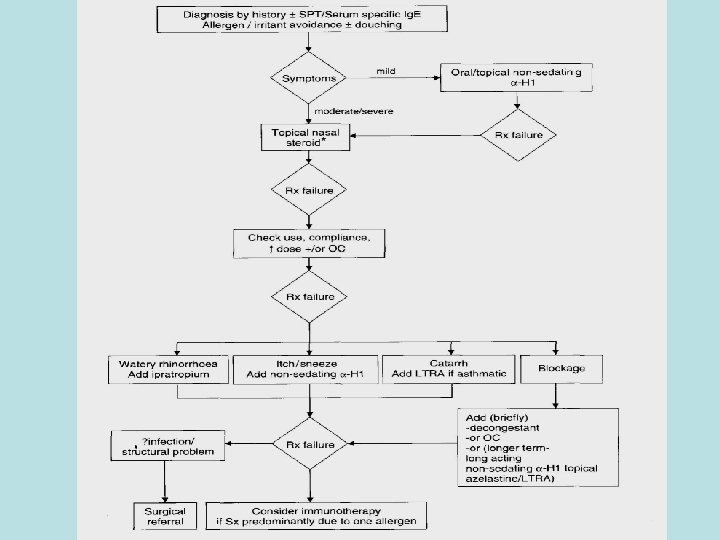
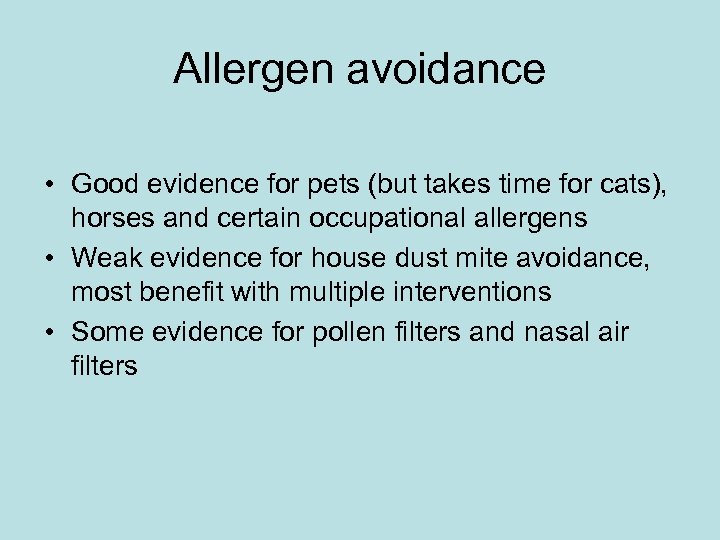
Allergen avoidance • Good evidence for pets (but takes time for cats), horses and certain occupational allergens • Weak evidence for house dust mite avoidance, most benefit with multiple interventions • Some evidence for pollen filters and nasal air filters
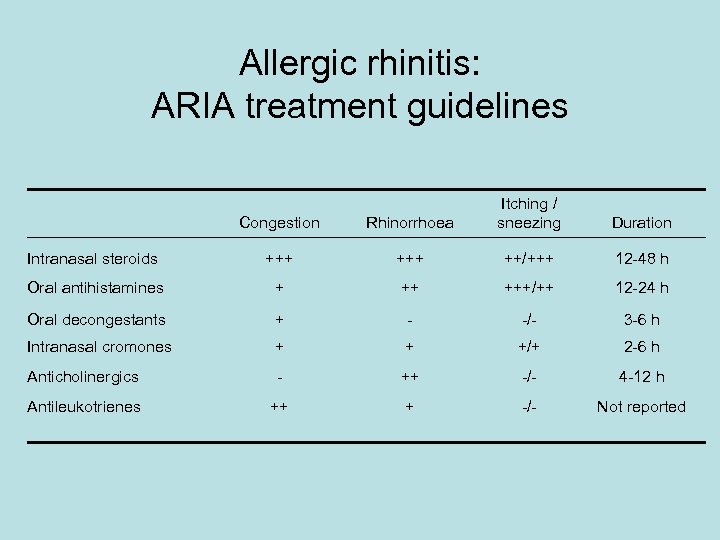
Allergic rhinitis: ARIA treatment guidelines Congestion Rhinorrhoea Itching / sneezing Intranasal steroids +++ ++/+++ 12 -48 h Oral antihistamines + ++ +++/++ 12 -24 h Oral decongestants + - -/- 3 -6 h Intranasal cromones + + +/+ 2 -6 h Anticholinergics - ++ -/- 4 -12 h Antileukotrienes ++ + -/- Not reported Duration
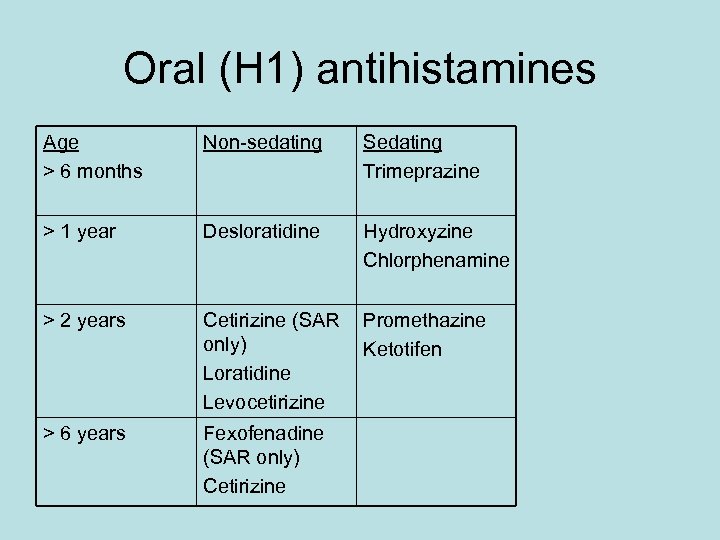
Oral (H 1) antihistamines Age > 6 months Non-sedating Sedating Trimeprazine > 1 year Desloratidine Hydroxyzine Chlorphenamine > 2 years Cetirizine (SAR only) Loratidine Levocetirizine Promethazine Ketotifen > 6 years Fexofenadine (SAR only) Cetirizine
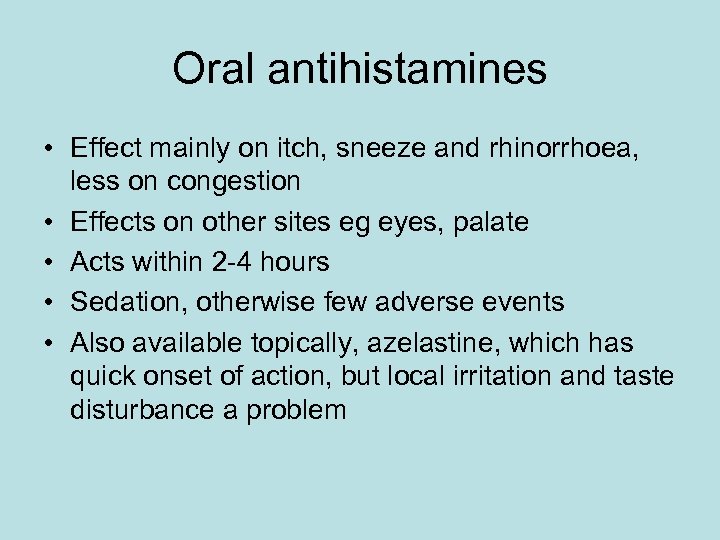
Oral antihistamines • Effect mainly on itch, sneeze and rhinorrhoea, less on congestion • Effects on other sites eg eyes, palate • Acts within 2 -4 hours • Sedation, otherwise few adverse events • Also available topically, azelastine, which has quick onset of action, but local irritation and taste disturbance a problem
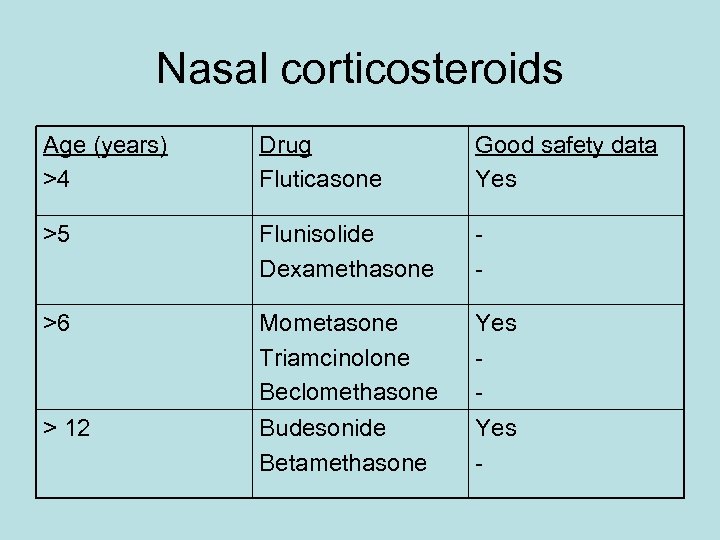
Nasal corticosteroids Age (years) >4 Drug Fluticasone Good safety data Yes >5 Flunisolide Dexamethasone - >6 Mometasone Triamcinolone Beclomethasone Budesonide Betamethasone Yes - > 12
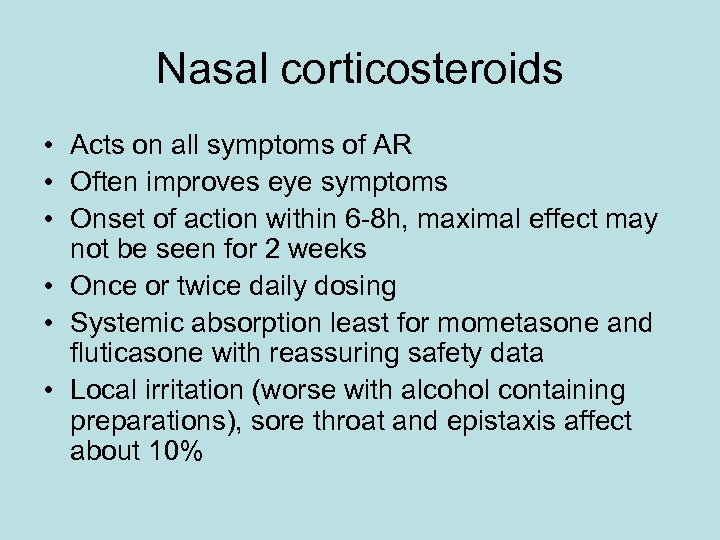
Nasal corticosteroids • Acts on all symptoms of AR • Often improves eye symptoms • Onset of action within 6 -8 h, maximal effect may not be seen for 2 weeks • Once or twice daily dosing • Systemic absorption least for mometasone and fluticasone with reassuring safety data • Local irritation (worse with alcohol containing preparations), sore throat and epistaxis affect about 10%
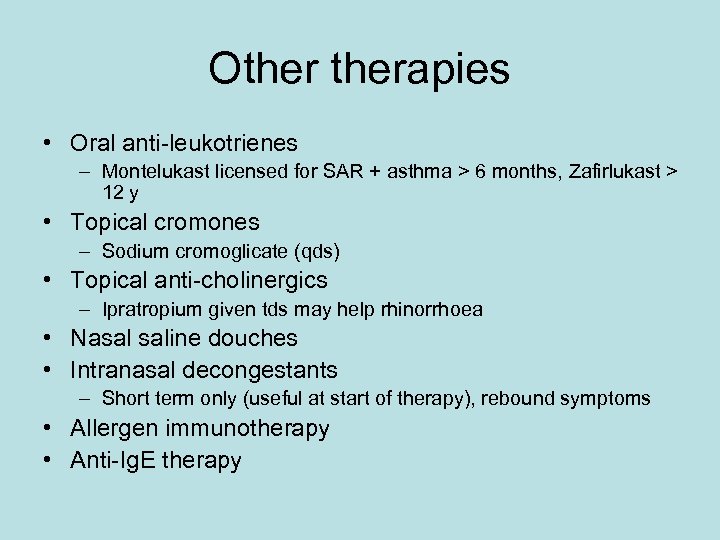
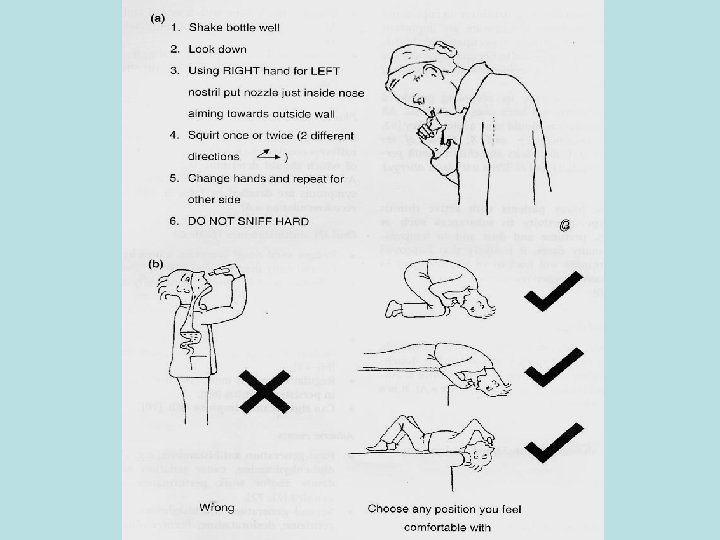
Otherapies • Oral anti-leukotrienes – Montelukast licensed for SAR + asthma > 6 months, Zafirlukast > 12 y • Topical cromones – Sodium cromoglicate (qds) • Topical anti-cholinergics – Ipratropium given tds may help rhinorrhoea • Nasal saline douches • Intranasal decongestants – Short term only (useful at start of therapy), rebound symptoms • Allergen immunotherapy • Anti-Ig. E therapy
One airway, one disease?
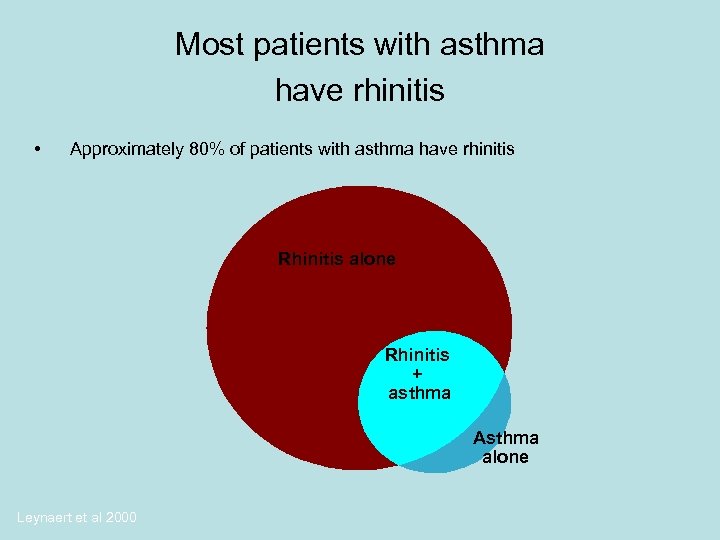
Most patients with asthma have rhinitis • Approximately 80% of patients with asthma have rhinitis Rhinitis alone Rhinitis + asthma Asthma alone Leynaert et al 2000
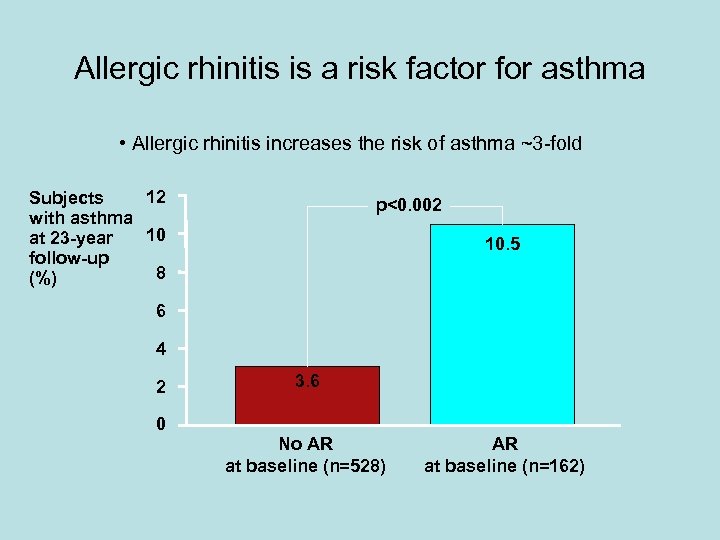
Allergic rhinitis is a risk factor for asthma • Allergic rhinitis increases the risk of asthma ~3 -fold 12 Subjects with asthma 10 at 23 -year follow-up 8 (%) p<0. 002 10. 5 6 4 2 0 3. 6 No AR at baseline (n=528) AR at baseline (n=162)
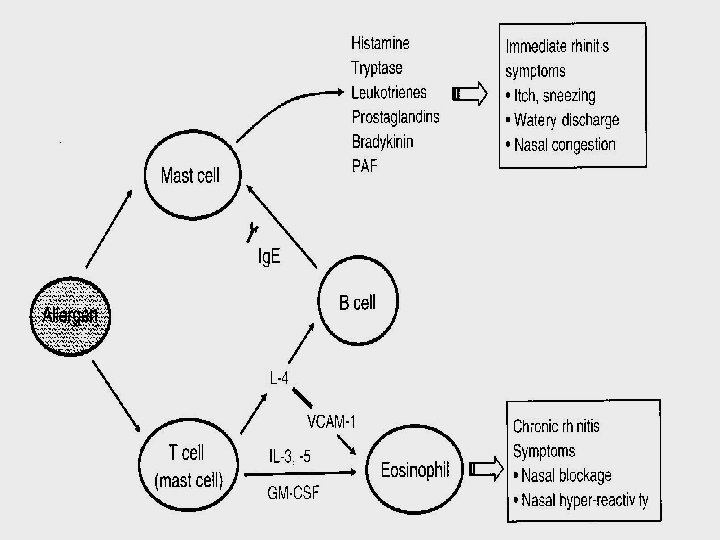
Link between allergic rhinitis and asthma • Some patients with allergic rhinitis report increased asthma symptoms during the pollen season • Rhinitis and asthma involve a common respiratory mucosa • Inflammation is involved in the pathogenesis of both allergic rhinitis and asthma • Allergic reactions in the nasal mucosa can potentially worsen asthmatic inflammatory processes in the lower airways • Allergen specific immunotherapy for rhinitis reduces development of asthma in children
How can rhinitis worsen asthma? • Nasal blockage leads to mouth breathing and exposure to cold, dry air, and an increase in allergens in the lower respiratory tract • Nasal challenge induces release of bone marrow eosinophils into the systemic circulation, which in turn can result in an inflammatory response within the entire respiratory tract • Rhinitis causes bronchial hyperreactivity • Neurogenic reflexes? • Nitric oxide changes?
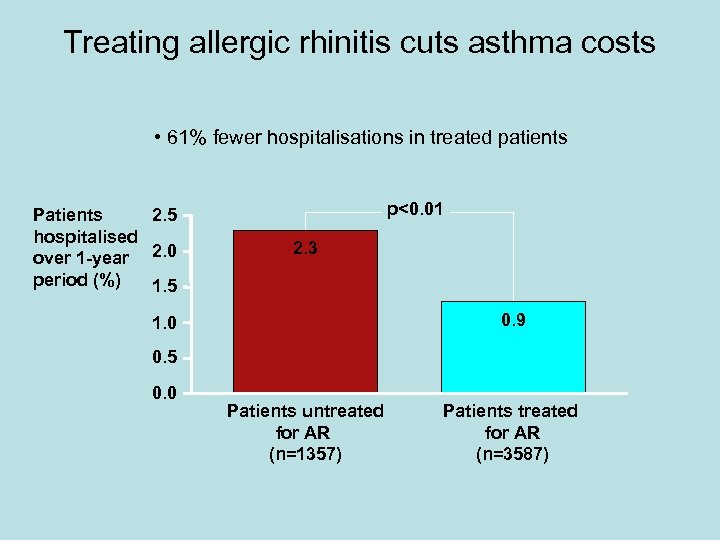
Treating allergic rhinitis cuts asthma costs • 61% fewer hospitalisations in treated patients Patients 2. 5 hospitalised over 1 -year 2. 0 period (%) 1. 5 p<0. 01 2. 3 0. 9 1. 0 0. 5 0. 0 Patients untreated for AR (n=1357) Patients treated for AR (n=3587)
Summary • Allergic rhinitis is common and often persistent, but often overlooked • Diagnosis is relatively straightforward if the right questions are asked • AR may be seasonal and / or perennial • Mainstays of treatment are allergen avoidance, oral antihistamines and intranasal corticosteroids • Strong link with asthma
31e6f1221ae05157ef13bb8dcfc2a5c3.ppt