133cd55207d28edec9efab3a7665f6b4.ppt
- Количество слайдов: 70
Allergic rhinitis
Before we start…. • It is important to know that although similar types of drugs are used to treat the symptoms of allergic rhinitis and the common cold, each condition is caused by distinctly different mechanism, thus different approaches to therapy are used.
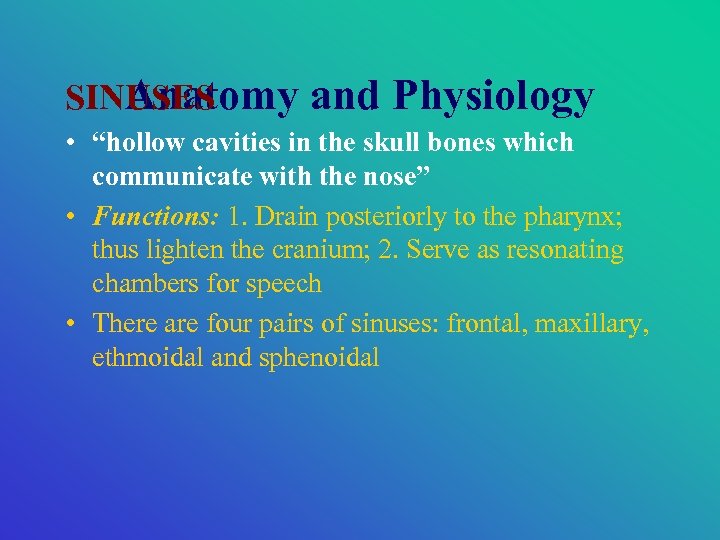
SINUSES Anatomy and Physiology • “hollow cavities in the skull bones which communicate with the nose” • Functions: 1. Drain posteriorly to the pharynx; thus lighten the cranium; 2. Serve as resonating chambers for speech • There are four pairs of sinuses: frontal, maxillary, ethmoidal and sphenoidal
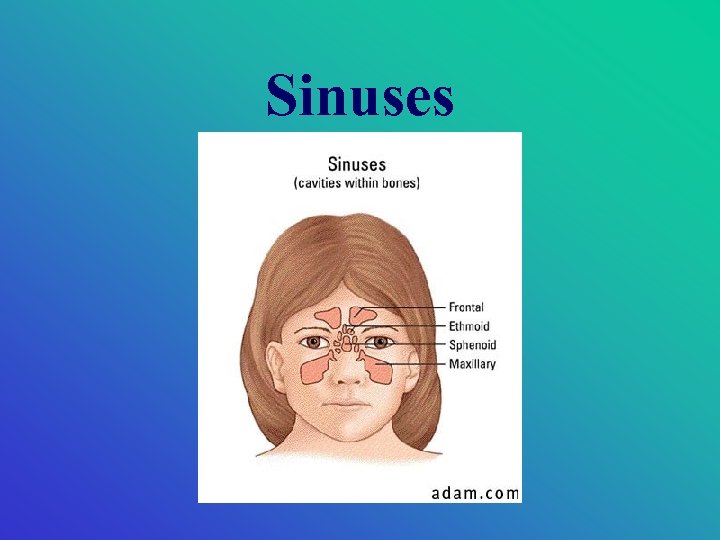
Sinuses
Allergic Rhinitis • The most common atopic disease • Hallmark of ~: temporal relationship between exposure to allergens & development of nasal symptoms • It takes at least 2 years of exposure to aeroallergens (airborne environmental allergens) to develop AR (thus, very rare in children <1 year) • Prevalence of AR: lowest in children < 5 yrs highest 2 nd---- 4 th decades • Genetic predisposition (60%)

Allergic Rhinitis • AR is classified as seasonal or perennial • Seasonal: repetitive & predictable symptoms (severe) • Perennial: symptoms persist throughout year without any obvious seasonal pattern • WHO: replaced terms with intermittent or persistent
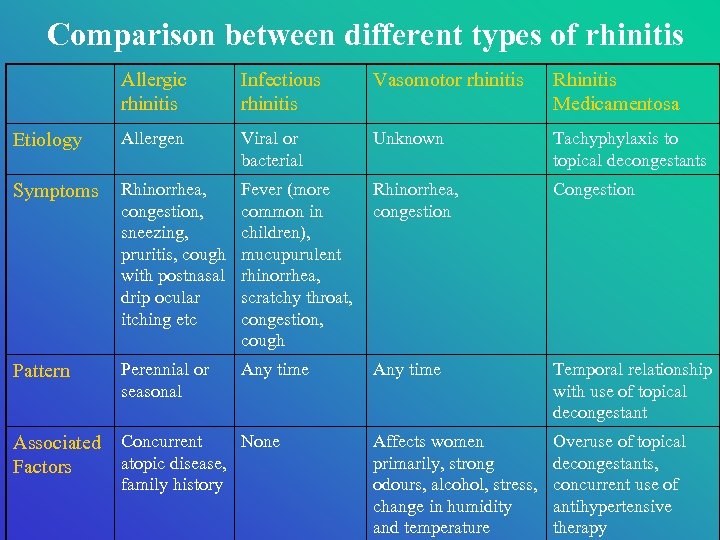
Comparison between different types of rhinitis Allergic rhinitis Infectious rhinitis Vasomotor rhinitis Rhinitis Medicamentosa Etiology Allergen Viral or bacterial Unknown Tachyphylaxis to topical decongestants Symptoms Rhinorrhea, congestion, sneezing, pruritis, cough with postnasal drip ocular itching etc Fever (more common in children), mucupurulent rhinorrhea, scratchy throat, congestion, cough Rhinorrhea, congestion Congestion Pattern Perennial or seasonal Any time Temporal relationship with use of topical decongestant Associated Factors Concurrent None atopic disease, family history Affects women primarily, strong odours, alcohol, stress, change in humidity and temperature Overuse of topical decongestants, concurrent use of antihypertensive therapy
Perennial Allergic Rhinitis 1 • Caused by continuous exposure to many different types of allergens • Dust Mite the most common cause of perennial allergic rhinitis • Commonly: household dust mites, molds, cockroaches, house pets • Less commonly: cottonseed & flaxseed (found in fertilizers, hair setting preparations and foods); some vegetable gums (found in hair setting prep & foods)
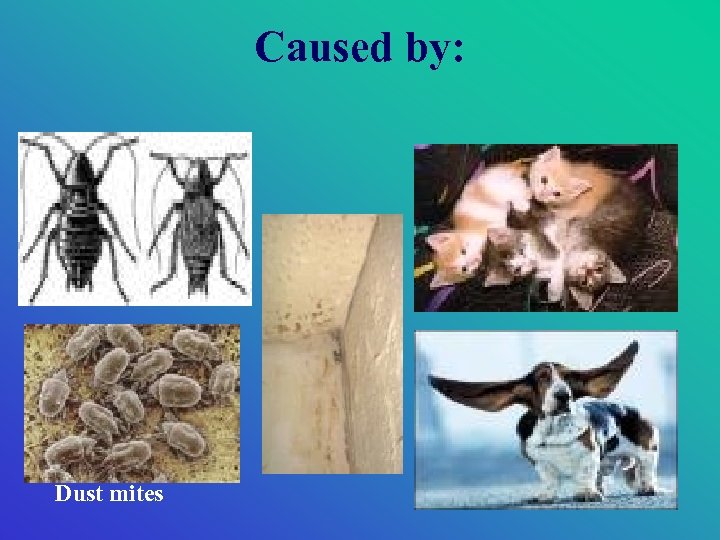
Caused by: Dust mites
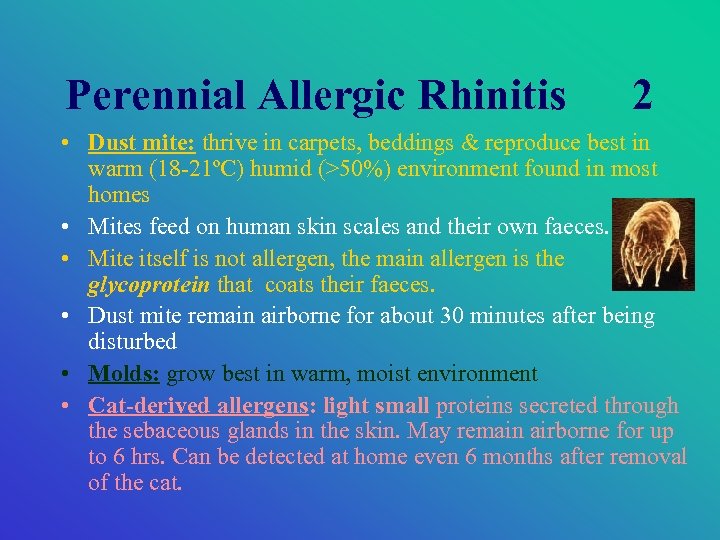
Perennial Allergic Rhinitis 2 • Dust mite: thrive in carpets, beddings & reproduce best in warm (18 -21ºC) humid (>50%) environment found in most homes • Mites feed on human skin scales and their own faeces. • Mite itself is not allergen, the main allergen is the glycoprotein that coats their faeces. • Dust mite remain airborne for about 30 minutes after being disturbed • Molds: grow best in warm, moist environment • Cat-derived allergens: light small proteins secreted through the sebaceous glands in the skin. May remain airborne for up to 6 hrs. Can be detected at home even 6 months after removal of the cat.

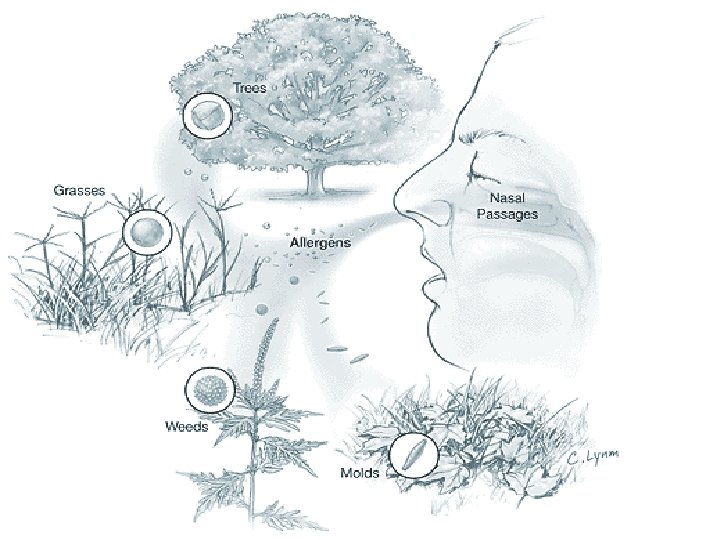
Seasonal Allergic Rhinitis • Caused by wind-borne plant pollens (e. g. tree, grass. etc) • “hay fever” & “rose fever” are terms related to seasons associated grass pollinosis and NOT associated with FEVER!
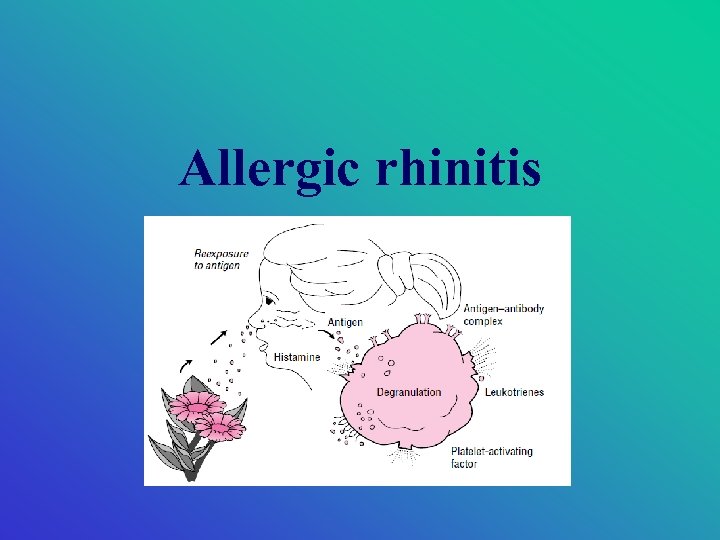
Pathophysiology • • • Complex pathogenesis involving numerous cells & mediators Histamine of the most important but not the sole Histamine: itching, pain, paroxysmal sneezing, vasodilation, and plasma exudation Sensory neural stimulation: nasal itch, sneeze, rhinorrhea Kinins, PG & Leukotrienes: nasal blockage, plasma protein exudation & glandular secretion
Pathophysiology Phases: 1. Sensitization: initial allergen exposure stimulates IG-E production by beta lymphocytes 2. Early phase response: subsequent allergen exposure results in rapid release of preformed mast cells mediators + production of additional mediators itching, sneezing and discomfort within minutes 3. Cellular-recruitment: inflammatory granulocytes & mast cells infiltrates the mu 7 cosa 4. Late phase response: a chronic inflammatory response, begins several hours after allergen exposure mucus hypersecretion secondary to infiltration of nasal mucosa with eosinophils, basophils, neutrophils and macrophages
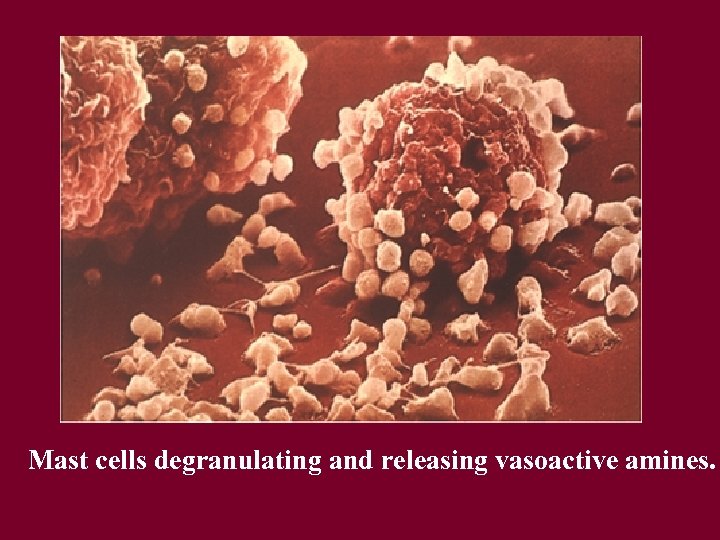
Mast cells degranulating and releasing vasoactive amines.
Complications 1. 2. 3. • • Sinusitis Recurrent otitis media & hearing loss Patients who develop: fever, purulent nasal discharge, refer to Dr. for evaluation frequent HA, and treatment earache

Symptoms of Allergic Rhinitis • Ocular: itching, lacrimation, mild soreness, puffiness & conjuctival erythema • Nasal: congestion, watery rhinorrhea, itching, sneezing, postnasal drip and nasal pruritus • Head & Neck: loss of taste and smell, mild sore throat due to postnasal drip, earache, sinus HA, itching of the palate and throat • Systemic: malaise & fatigue:
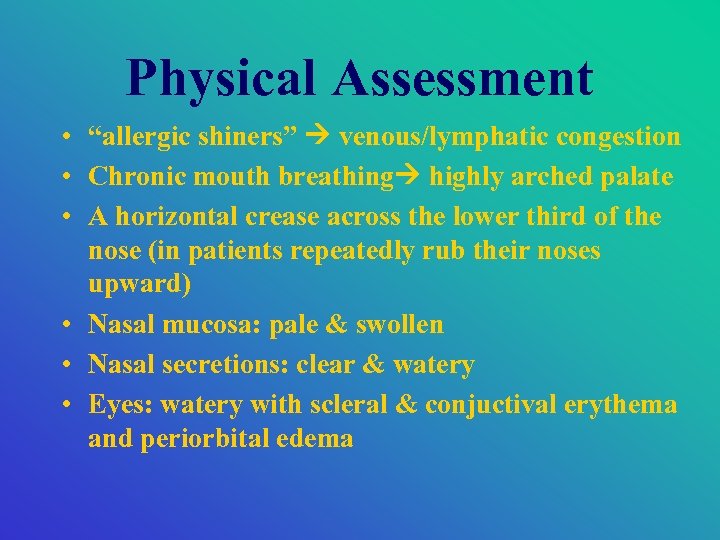
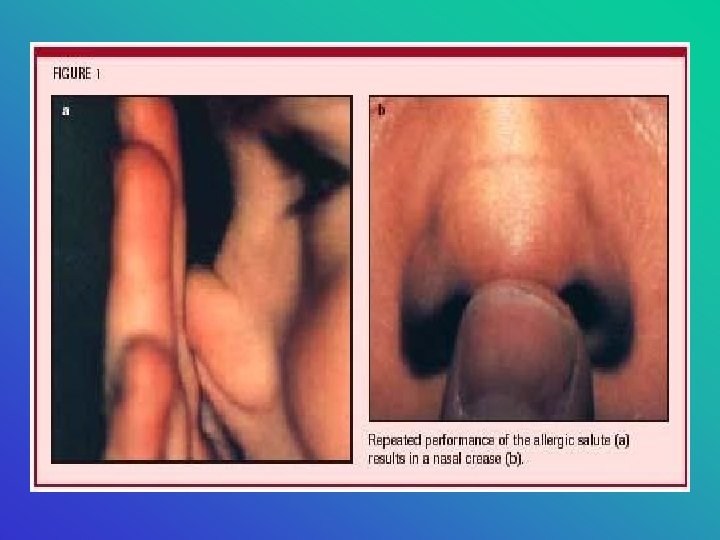
Physical Assessment • “allergic shiners” venous/lymphatic congestion • Chronic mouth breathing highly arched palate • A horizontal crease across the lower third of the nose (in patients repeatedly rub their noses upward) • Nasal mucosa: pale & swollen • Nasal secretions: clear & watery • Eyes: watery with scleral & conjuctival erythema and periorbital edema

Allergic shiners Arched palate because of mouth breathing Periorbital edema
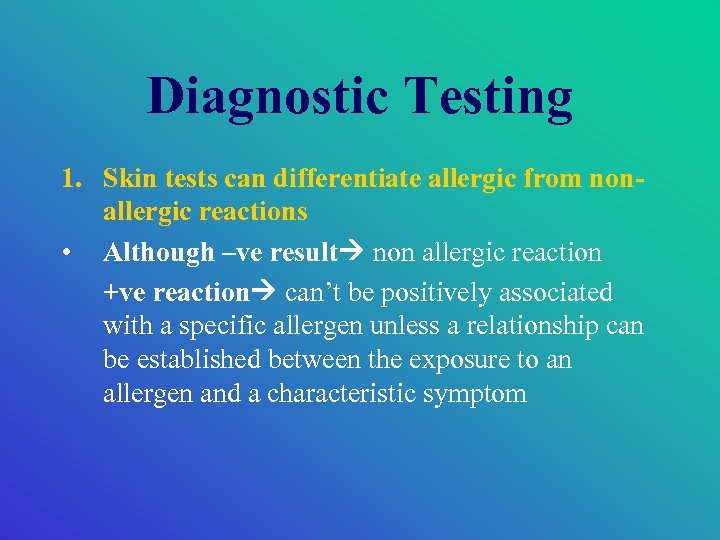
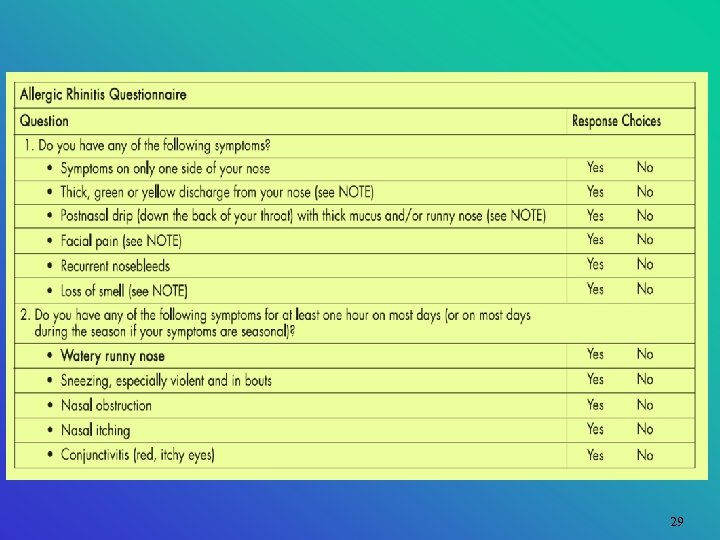
Diagnostic Testing 1. Skin tests can differentiate allergic from nonallergic reactions • Although –ve result non allergic reaction +ve reaction can’t be positively associated with a specific allergen unless a relationship can be established between the exposure to an allergen and a characteristic symptom
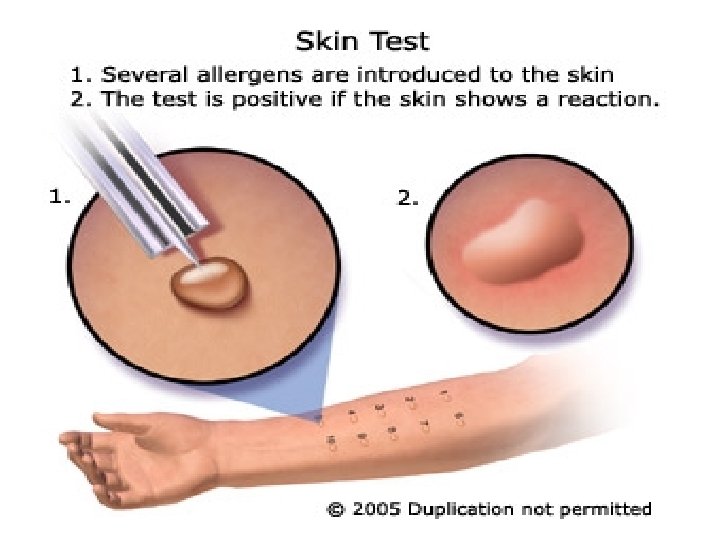
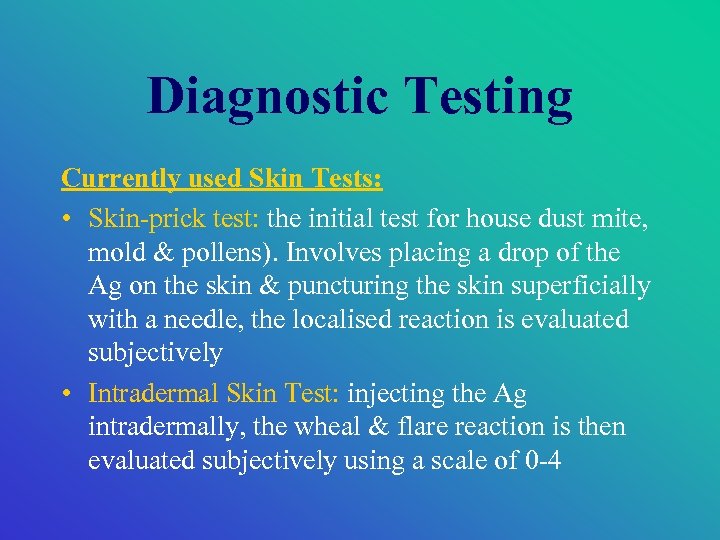
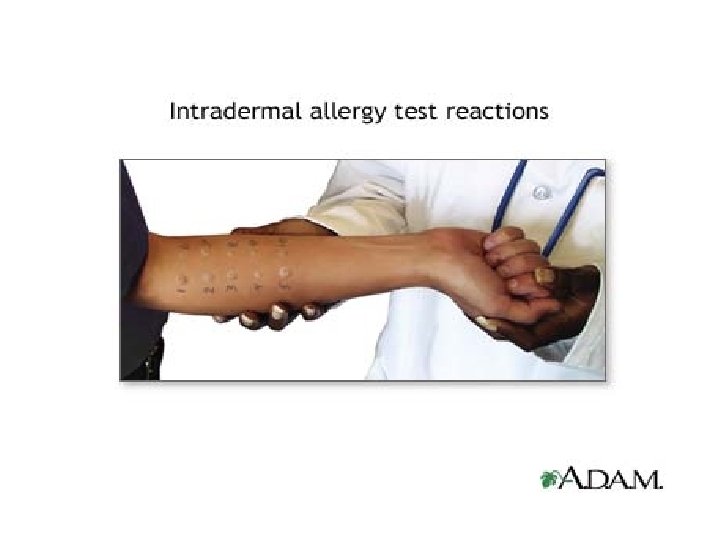
Diagnostic Testing Currently used Skin Tests: • Skin-prick test: the initial test for house dust mite, mold & pollens). Involves placing a drop of the Ag on the skin & puncturing the skin superficially with a needle, the localised reaction is evaluated subjectively • Intradermal Skin Test: injecting the Ag intradermally, the wheal & flare reaction is then evaluated subjectively using a scale of 0 -4

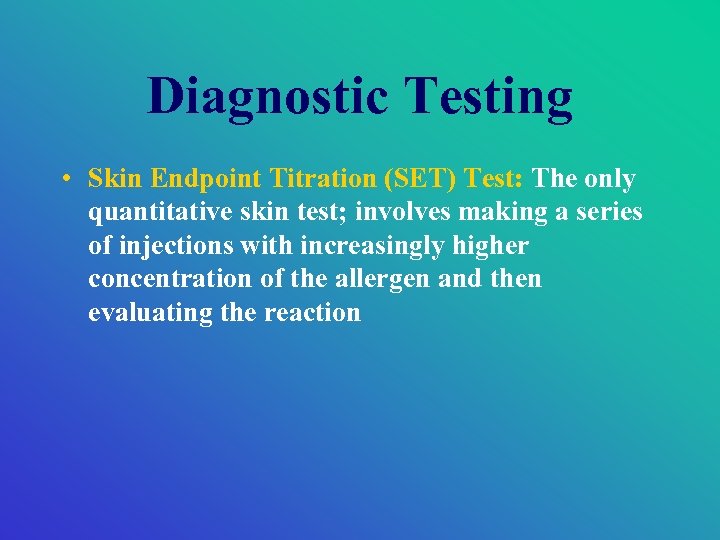
Diagnostic Testing • Skin Endpoint Titration (SET) Test: The only quantitative skin test; involves making a series of injections with increasingly higher concentration of the allergen and then evaluating the reaction
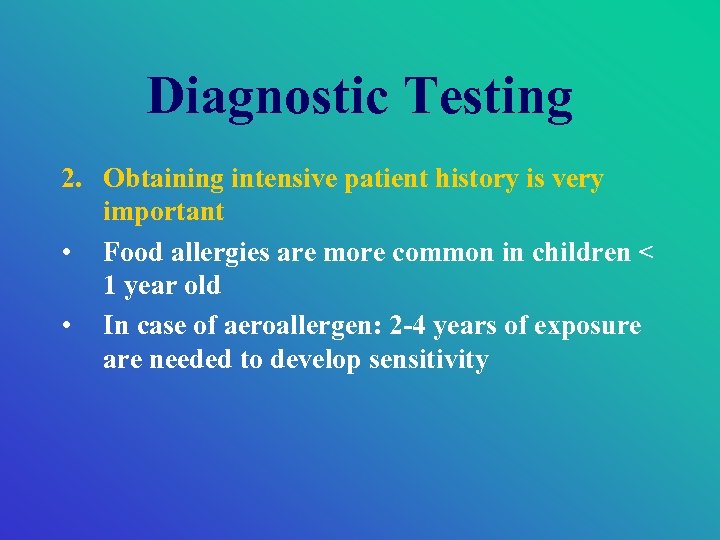
Diagnostic Testing 2. Obtaining intensive patient history is very important • Food allergies are more common in children < 1 year old • In case of aeroallergen: 2 -4 years of exposure are needed to develop sensitivity
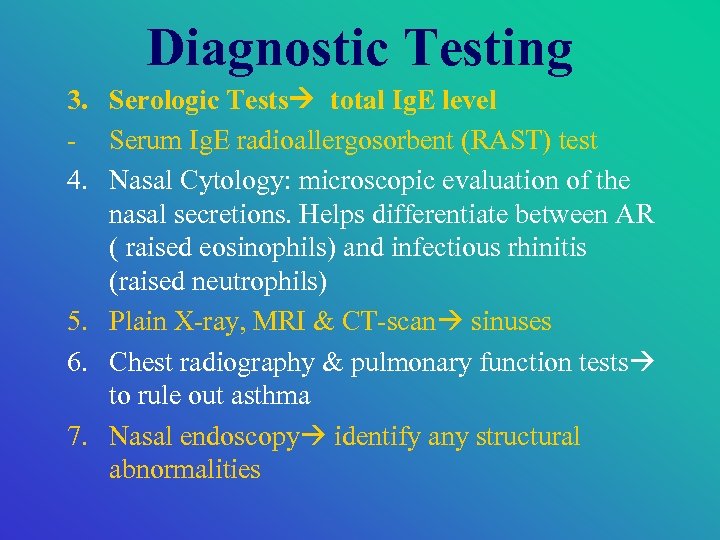
Diagnostic Testing 3. Serologic Tests total Ig. E level - Serum Ig. E radioallergosorbent (RAST) test 4. Nasal Cytology: microscopic evaluation of the nasal secretions. Helps differentiate between AR ( raised eosinophils) and infectious rhinitis (raised neutrophils) 5. Plain X-ray, MRI & CT-scan sinuses 6. Chest radiography & pulmonary function tests to rule out asthma 7. Nasal endoscopy identify any structural abnormalities
29
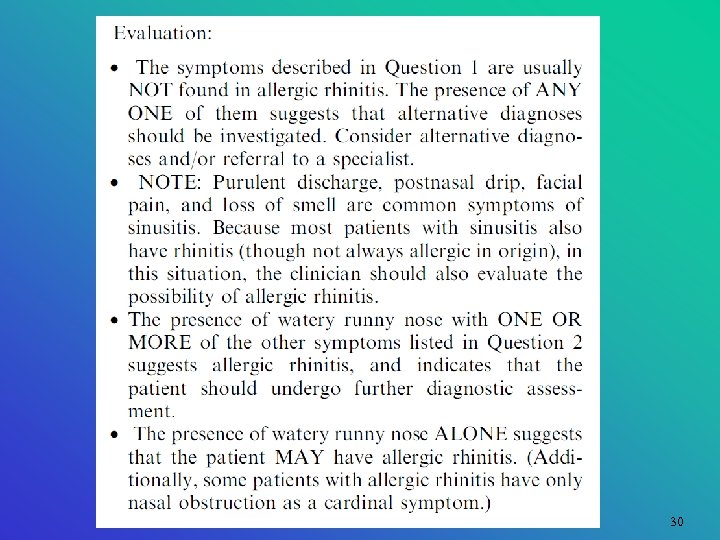
30

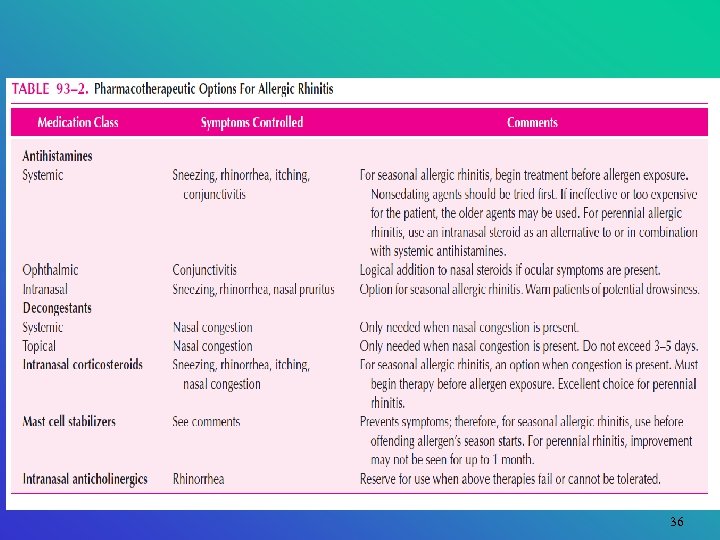
Disease Management 1. First step: avoidance of the offending allergens 2. Pharmacotherapy is used if the avoidance measures are not feasible or do not adequately relieve the symptoms • Treatment of allergic rhinitis should be targeted at the patient’s specific symptoms • Drugs: antihistamines, decongestants, mast cell -stabilizers, mucolytics & corticosteroids
Disease Management 3. Immunotherapy is indicated for patients: (a) whose symptoms can’t be adequately controlled with medication or (b) symptoms occur most days of the year
Preventative Measures • patients allergic to outdoor allergens should keep house and car windows closed and use airconditioners • Avoid grass if allergic etc • Reduce indoor mold by: - venting moist bathroom and kitchens, - using dehumidifiers How to reduce house dust mite exposure?

House dust mite by 1. Reduce indoor humidity to < 50% 2. Pillows, mattresses should be encased with a plastic cover that is cleaned weekly by a damp cloth 3. Items that collect dust should be removed from bedrooms (e. g. open bookshelves) 4. All beddings, including mattresses should be cleaned weekly with hot water 5. Vacuum cleaners should be equipped with special filters (HEPA) to avoid aerosolising the house dust mite faeces when vacuuming Animal allergen exposure: remove totally or at least from bedrooms. Wash cat fortnightly!
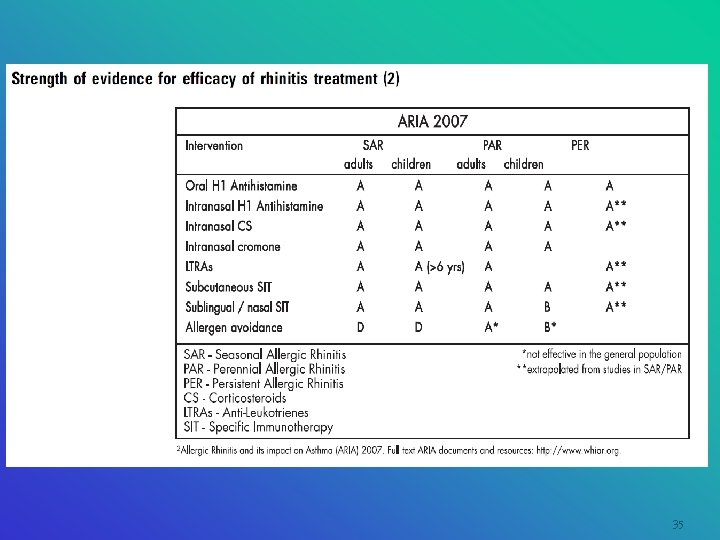
35
36
37
38
39
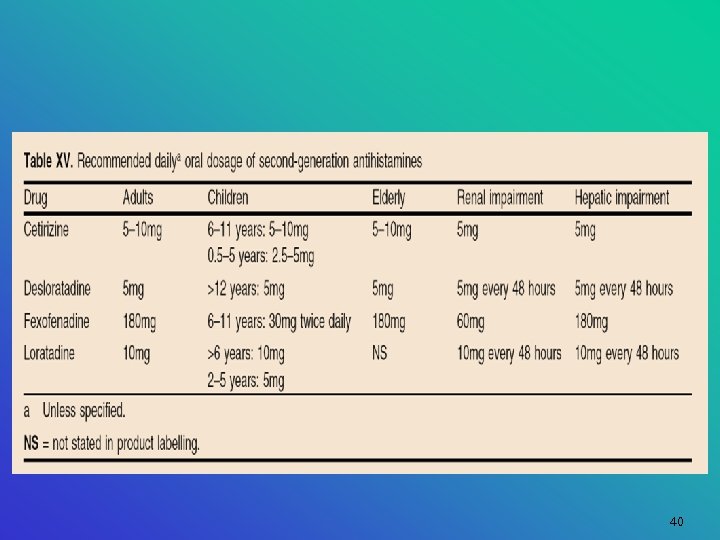
40
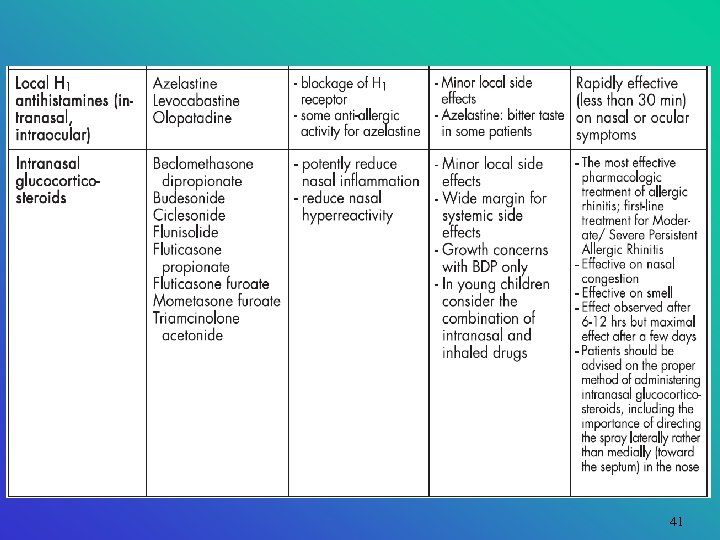
41
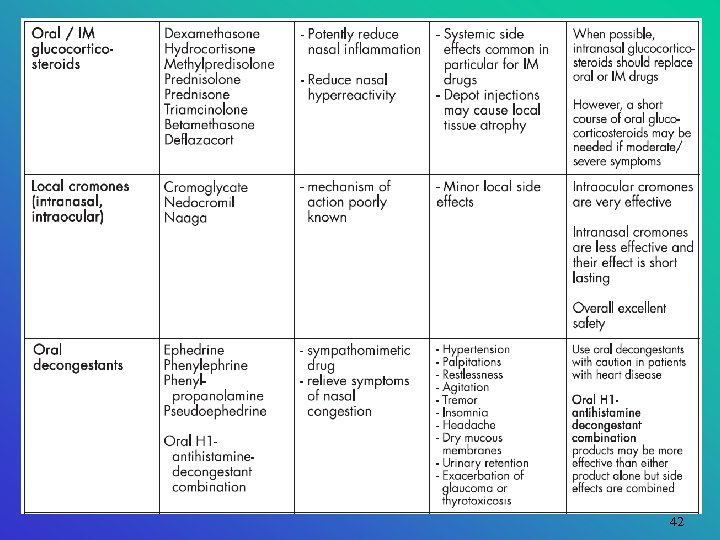
42
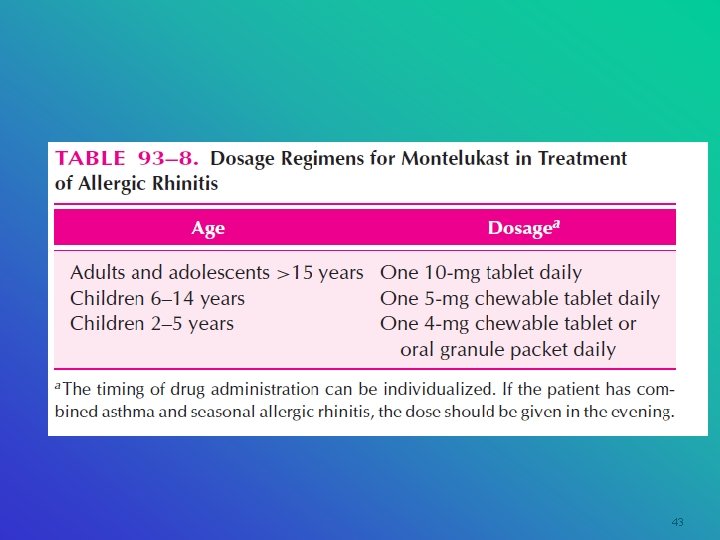
43
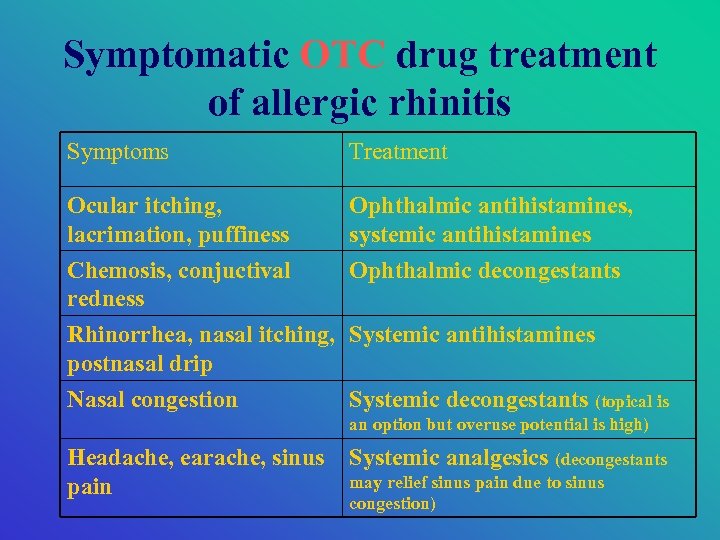
Symptomatic OTC drug treatment of allergic rhinitis Symptoms Treatment Ocular itching, lacrimation, puffiness Ophthalmic antihistamines, systemic antihistamines Chemosis, conjuctival redness Ophthalmic decongestants Rhinorrhea, nasal itching, Systemic antihistamines postnasal drip Nasal congestion Systemic decongestants (topical is an option but overuse potential is high) Headache, earache, sinus pain Systemic analgesics (decongestants may relief sinus pain due to sinus congestion)

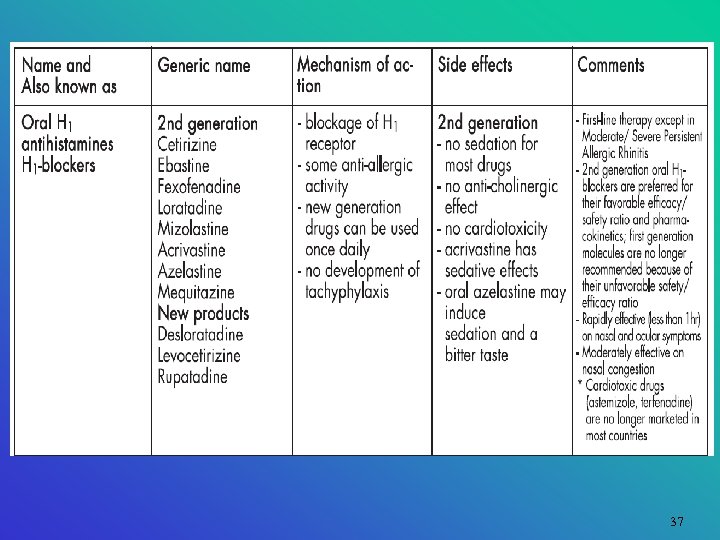
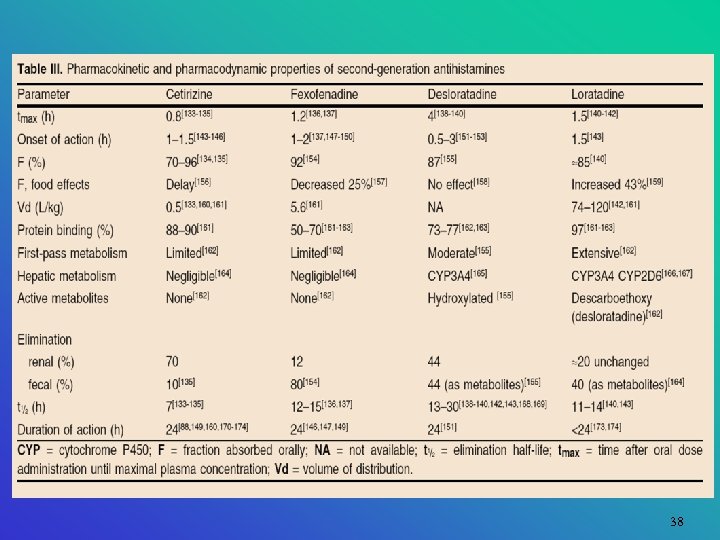
Antihistamines • First line for prophylaxis and treatment of allergic rhinitis • Usefulness is limited as they compete only with one mediator (histamine) • Antihistamines: - very effective in relieving symptoms of sneezing & itching - somewhat effective for reducing rhinorrhea - have no effect on nasal congestion
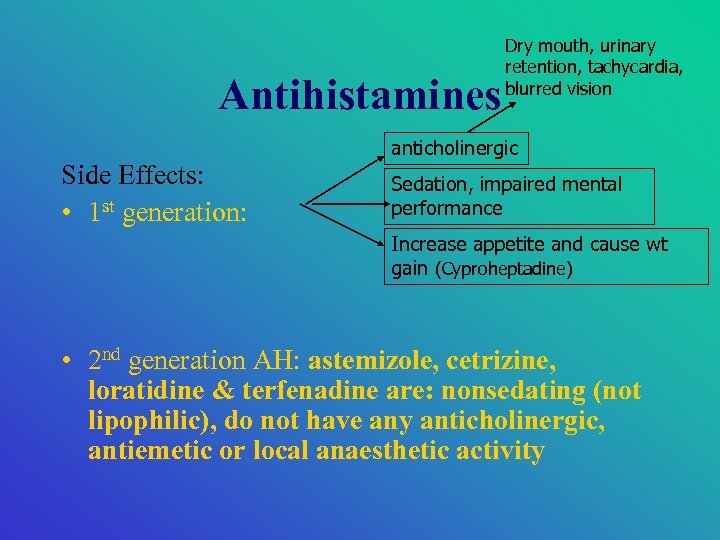
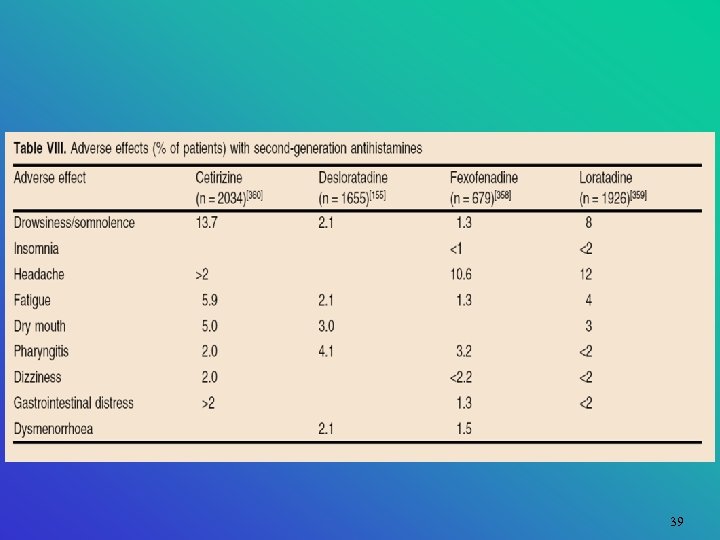
Antihistamines Side Effects: • 1 st generation: Dry mouth, urinary retention, tachycardia, blurred vision anticholinergic Sedation, impaired mental performance Increase appetite and cause wt gain (Cyproheptadine) • 2 nd generation AH: astemizole, cetrizine, loratidine & terfenadine are: nonsedating (not lipophilic), do not have any anticholinergic, antiemetic or local anaesthetic activity
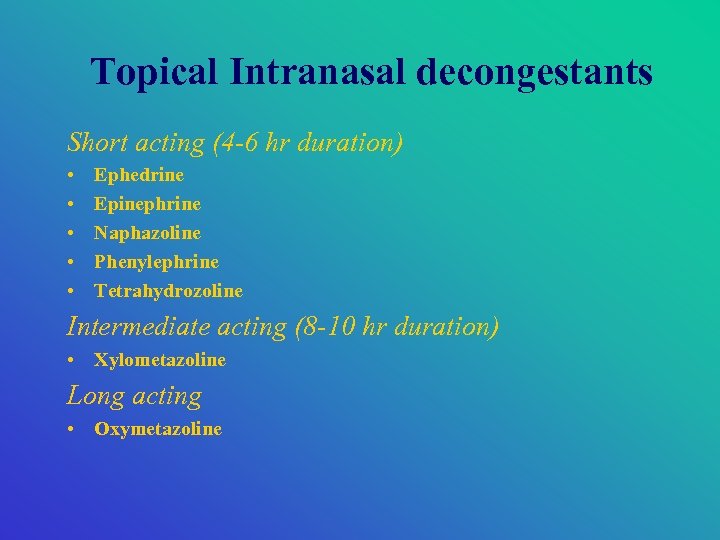
Topical Intranasal decongestants Short acting (4 -6 hr duration) • • • Ephedrine Epinephrine Naphazoline Phenylephrine Tetrahydrozoline Intermediate acting (8 -10 hr duration) • Xylometazoline Long acting • Oxymetazoline
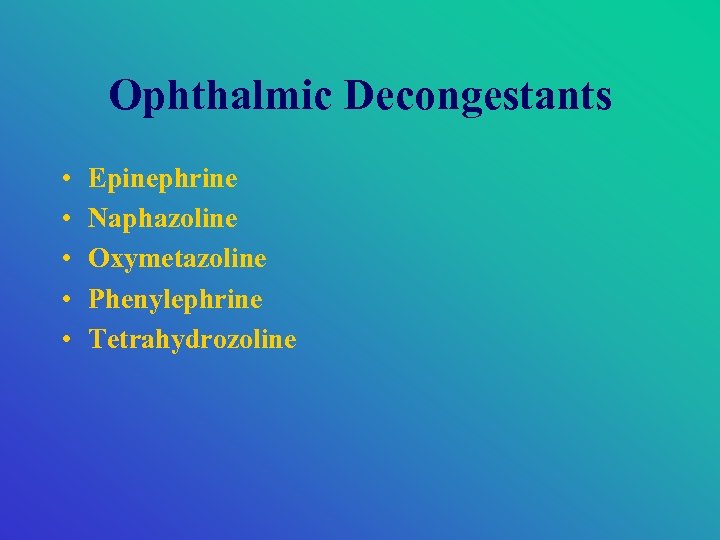
Ophthalmic Decongestants • • • Epinephrine Naphazoline Oxymetazoline Phenylephrine Tetrahydrozoline
Systemic Decongestants • • Ephedrine Pseudoephedrine Phenylephrine Phenylpropanolamine (withdrawn from market because of its relation with haemorrhagic stroke) Inhalers: • Desoxyephedrine • Propylhexedrine
Decongestants Side Effects of topical decongestants: • Topical decongestants are minimally absorbed, thus, systemic S. E: infrequent & minimal 1. May cause local irritation because of the propellant or vehicle 2. Rebound congestion “rhinitis medicamentosa” when topical decongestant is used > 3 -5 days - more common with short acting than long acting decongestants
Treatment of rebound congestion 1. Slow withdrawal of topical decongestant (one nostril at a time) 2. Replacement of topical decongestant with topical normal saline (soothe & moisten) 3. (if needed) topical corticosteroids & systemic decongestants The mucous membrane would return to normal 1 -2 weeks following discontinuation of the topical decongestant
Decongestants Product Selection Guidelines: • Depends on the expected duration of treatment and presence of concomitant disease • Patients of seasonal allergic rhinitis, requires decongestants throughout the period of exposure to allergens • Nasal sprays: the simplest drug delivery methods & preferred for older children and adults
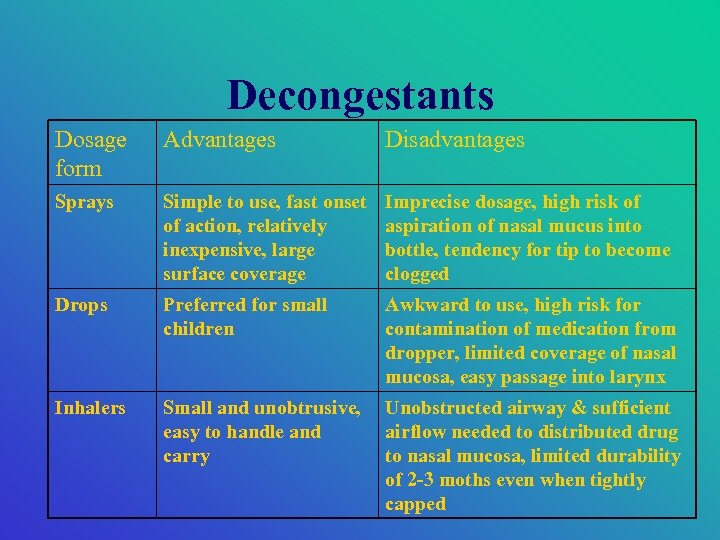
Decongestants Dosage form Advantages Disadvantages Sprays Simple to use, fast onset of action, relatively inexpensive, large surface coverage Imprecise dosage, high risk of aspiration of nasal mucus into bottle, tendency for tip to become clogged Drops Preferred for small children Awkward to use, high risk for contamination of medication from dropper, limited coverage of nasal mucosa, easy passage into larynx Inhalers Small and unobtrusive, easy to handle and carry Unobstructed airway & sufficient airflow needed to distributed drug to nasal mucosa, limited durability of 2 -3 moths even when tightly capped
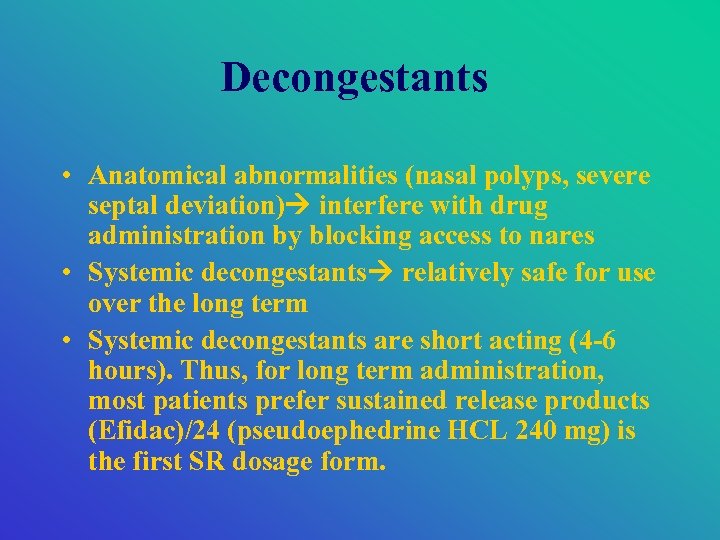
Decongestants • Anatomical abnormalities (nasal polyps, severe septal deviation) interfere with drug administration by blocking access to nares • Systemic decongestants relatively safe for use over the long term • Systemic decongestants are short acting (4 -6 hours). Thus, for long term administration, most patients prefer sustained release products (Efidac)/24 (pseudoephedrine HCL 240 mg) is the first SR dosage form.
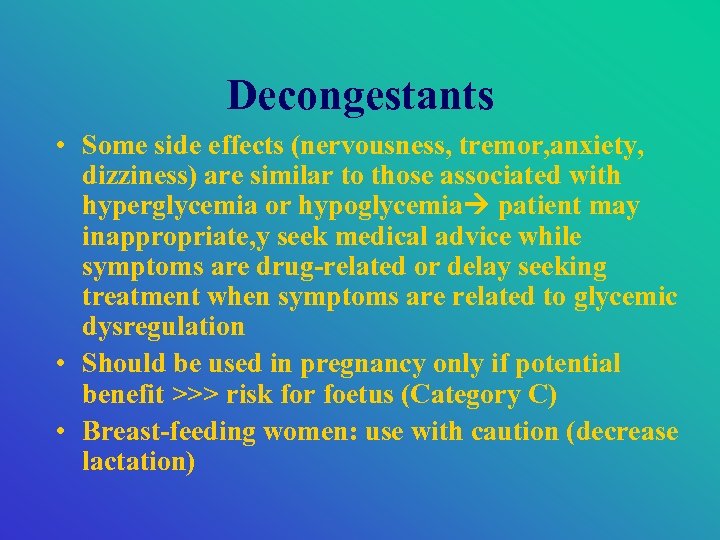
Decongestants • Some side effects (nervousness, tremor, anxiety, dizziness) are similar to those associated with hyperglycemia or hypoglycemia patient may inappropriate, y seek medical advice while symptoms are drug-related or delay seeking treatment when symptoms are related to glycemic dysregulation • Should be used in pregnancy only if potential benefit >>> risk for foetus (Category C) • Breast-feeding women: use with caution (decrease lactation)
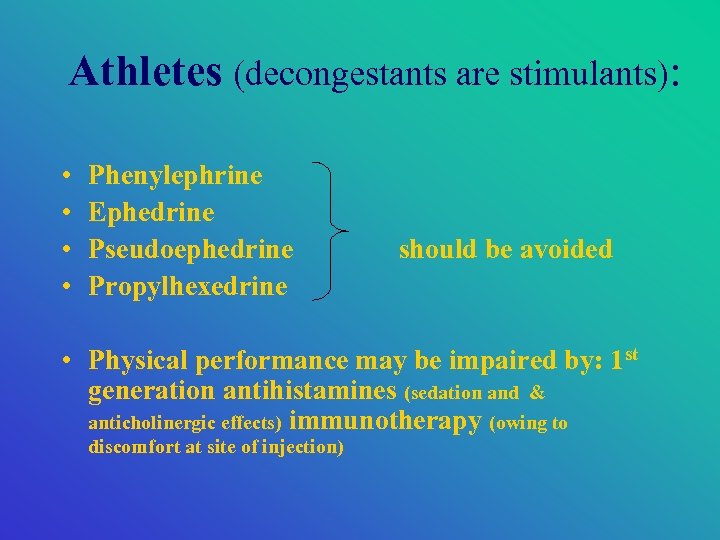
Athletes (decongestants are stimulants): • • Phenylephrine Ephedrine Pseudoephedrine Propylhexedrine should be avoided • Physical performance may be impaired by: 1 st generation antihistamines (sedation and & anticholinergic effects) immunotherapy (owing to discomfort at site of injection)
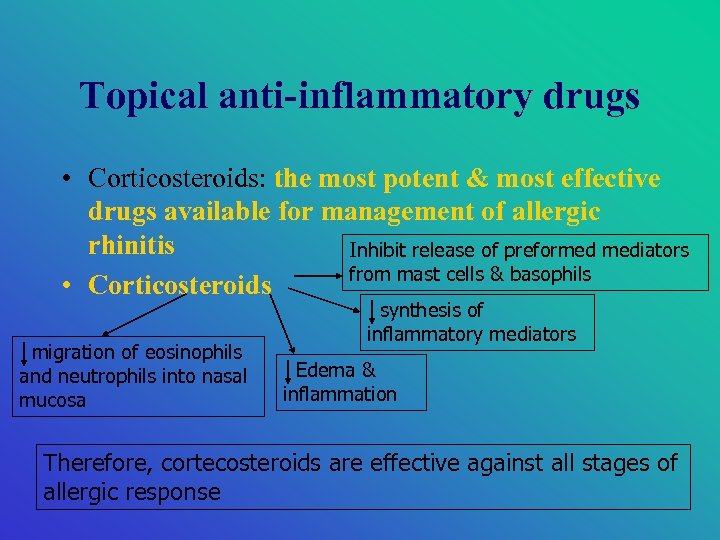
Topical anti-inflammatory drugs • Corticosteroids: the most potent & most effective drugs available for management of allergic rhinitis Inhibit release of preformed mediators from mast cells & basophils • Corticosteroids migration of eosinophils and neutrophils into nasal mucosa synthesis of inflammatory mediators Edema & inflammation Therefore, cortecosteroids are effective against all stages of allergic response
Topical anti-inflammatory agents • Intranasal administration corticosteoids is the route of choice as it minimizes the risk of systemic side effects • The side effects of intranasal ~: 1. Local irritation 2. Epistaxis • However, short term use of systemic cortecosteroids may be required for severe symptoms
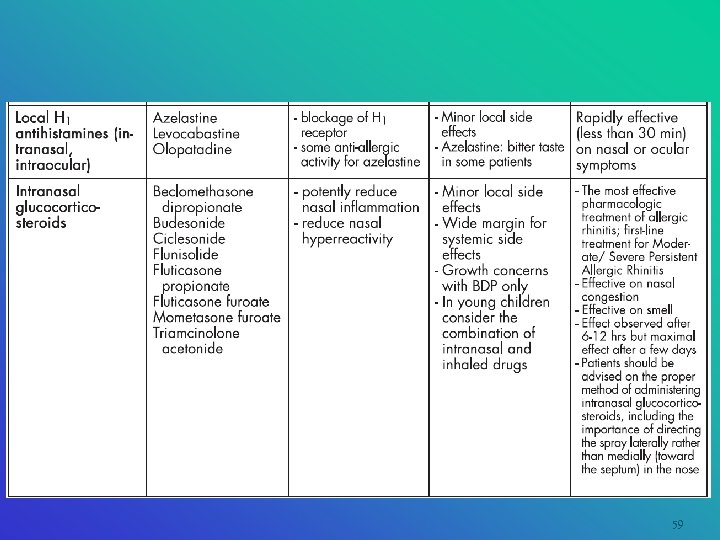
59
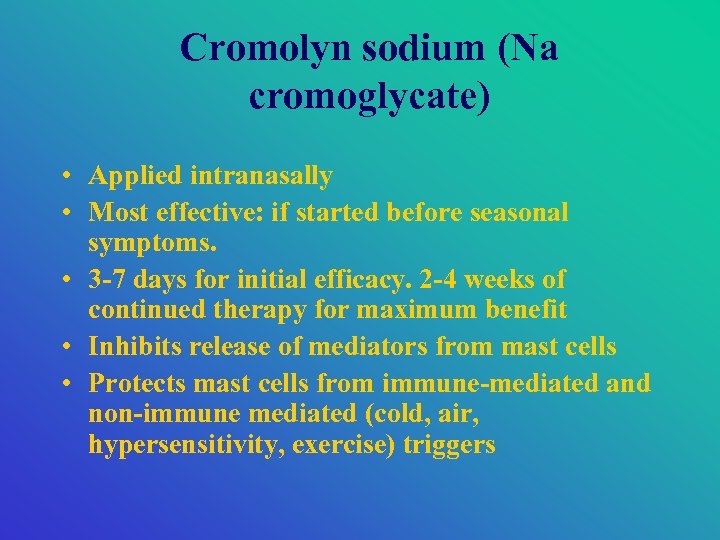
Cromolyn sodium (Na cromoglycate) • Applied intranasally • Most effective: if started before seasonal symptoms. • 3 -7 days for initial efficacy. 2 -4 weeks of continued therapy for maximum benefit • Inhibits release of mediators from mast cells • Protects mast cells from immune-mediated and non-immune mediated (cold, air, hypersensitivity, exercise) triggers
Cromolyn sodium (Na cromoglycate) • Has to be applied 1 spray per nostril: 4 -6 times daily to be effective (t 1/2= 1 -2 hours) • Not as effective as corticosteroids for patients with more severe symptoms, used as adjunctive therapy • Not associated with systemic side effects (< 7% absorption) • The most common S. E: sneezing then nasal stinging and burning
Cromolyn sodium (Na cromoglycate) • No drug interactions • Relative C/I: children < 5 year old, Hx of hypersensitity. • Wide margin of safety: safe during pregnancy, elderly and in children > 6 year old
Mucolytics • Drugs that thin the mucus, making it easier to expel secretions • Mucus= mucin, epithelial cells, leukocytes & various inorganic salts suspended in water • Hydration (by fluid intake or steam inhalation) will aid in the formation of a less viscid, more liquid mucus that is easy to expel • E. g. Ambroxol, Bromhexin
Expectorants • Facilitates mucociliary transport • E. g. Guaifensin, ammonia and ipecacuanha mixture, BP • but their efficacy in allergic rhinitis has not been proved
Immunotherapy • “ desensitization” “hyposensitization” • Most effective for pollen-related allergens • Indication: - in patients whose symptoms are not controlled by drugs - who have severe conditions or perennial symptoms - who are allergic to allergens that are difficult to avoid
Immunotherapy • • - Exact mechanism is not known yet BUT… Thought to work by: production of Ig-E antibodies Production of Ig-G blocking antibodies Generating antigen-specific suppressor Tlymphocytes - mononuclear cell-derived histamine releasing factor
Immunotherapy Administration Technique: • Consists of a series of injections with extracts of allergens identified as the cause of the symptoms • Treatment is initiated with very dilute solutions. • Injections then repeated weekly using gradually increasing concentrations • The top “maintenance” dose is generally reached within 4 -8 months
Immunotherapy • Injections of this dose are repeated every 3 -4 weeks for 3 -5 years • Patients may improve as early as 3 months after initiation of immunotherpay • About 80% of patients have significant relief while receiving immunotherapy • Approximately 60% will remain symptom-free after the discontinuation of the immunotherapy
Immunotherapy • Relative C/I: autoimmune disease, unstable CAD, unstable angina and concurrent therapy with B-blockers • Although it must not be initiated during pregnancy, maintenance therapy can be continued
Patient Counselling • Self-reading: Handbook of Nonprescription Drugs • Enjoy!
133cd55207d28edec9efab3a7665f6b4.ppt