e9cd256a889602a5e5eb072a5f9b1269.ppt
- Количество слайдов: 15
ALL YOU EVER WANTED TO KNOW ABOUT BILLING & REIMBURSEMENT BUT WERE AFRAID TO ASK Presented by: Evelyn Alwine, RHIA CHDA Director Revenue Cycle Management Bloomington Hospital 3/17/2018 1
Introduction n n We will be reviewing billing and reimbursement for services You will learn how services and supplies are charged, coding systems, and reimbursement methodologies 3/17/2018 2
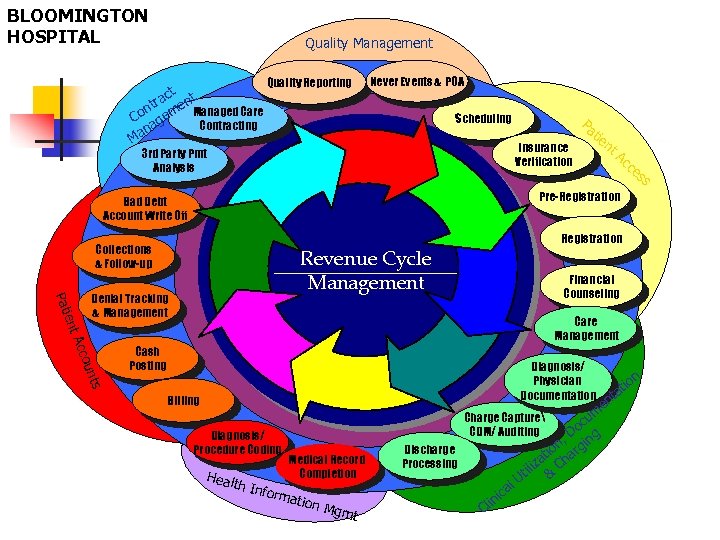
BLOOMINGTON HOSPITAL Quality Management ct t tra en. Managed Care n Co gem a Contracting an M Quality Reporting Never Events & POA Scheduling Pa Insurance Verification 3 rd Party Pmt Analysis tie nt Ac ce ss Pre-Registration Bad Debt Account Write Off Collections & Follow-up Registration ient Pat Revenue Cycle Management Denial Tracking & Management Financial Counseling Acc Care Management Diagnosis/ Physician Documentation ts oun Cash Posting Billing Diagnosis/ Procedure Coding m cu o , D ing n g tio har iza C til & U Charge Capture CDM/ Auditing Medical Record Completion Heal th In form ation Mgm t Discharge Processing C l ica lin en t n tio a
Overview It is vital that all participants in the healthcare industry work together to insure that services, supplies, and drugs are adequately reimbursed to enable health care providers to continue in their mission. 3/17/2018 4
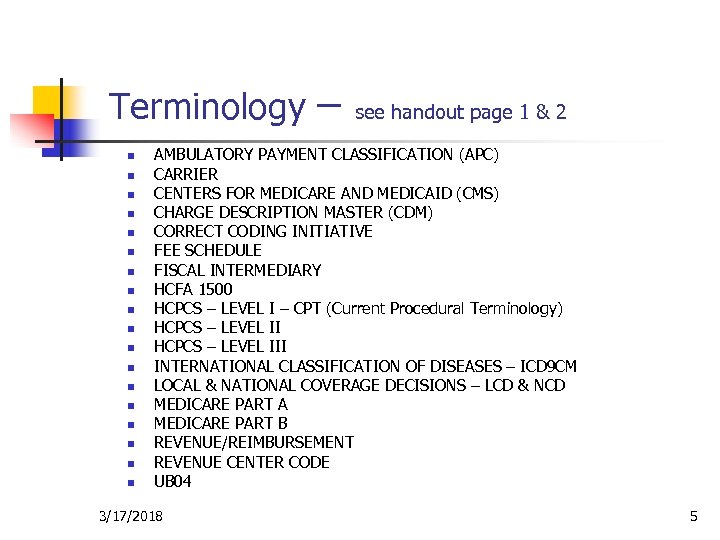
Terminology n n n n n – see handout page 1 & 2 AMBULATORY PAYMENT CLASSIFICATION (APC) CARRIER CENTERS FOR MEDICARE AND MEDICAID (CMS) CHARGE DESCRIPTION MASTER (CDM) CORRECT CODING INITIATIVE FEE SCHEDULE FISCAL INTERMEDIARY HCFA 1500 HCPCS – LEVEL I – CPT (Current Procedural Terminology) HCPCS – LEVEL III INTERNATIONAL CLASSIFICATION OF DISEASES – ICD 9 CM LOCAL & NATIONAL COVERAGE DECISIONS – LCD & NCD MEDICARE PART A MEDICARE PART B REVENUE/REIMBURSEMENT REVENUE CENTER CODE UB 04 3/17/2018 5
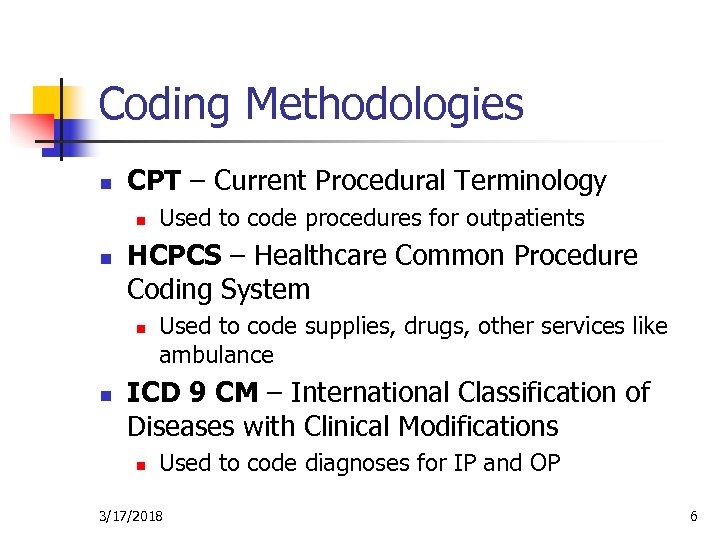
Coding Methodologies n CPT – Current Procedural Terminology n n HCPCS – Healthcare Common Procedure Coding System n n Used to code procedures for outpatients Used to code supplies, drugs, other services like ambulance ICD 9 CM – International Classification of Diseases with Clinical Modifications n Used to code diagnoses for IP and OP 3/17/2018 6
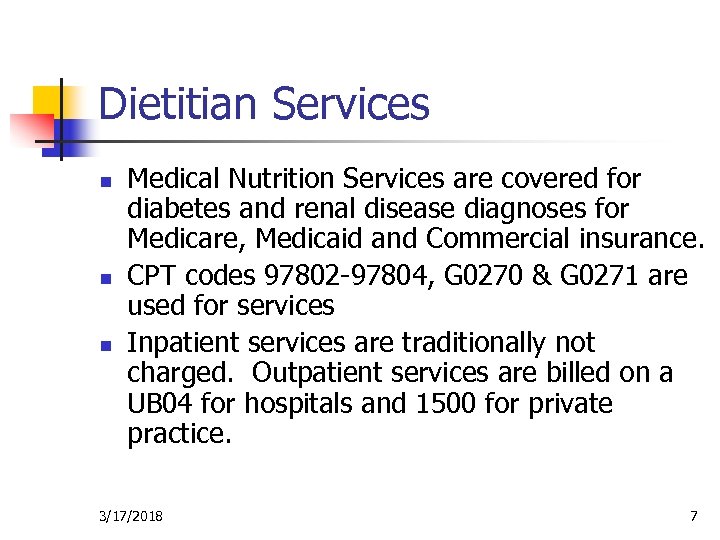
Dietitian Services n n n Medical Nutrition Services are covered for diabetes and renal disease diagnoses for Medicare, Medicaid and Commercial insurance. CPT codes 97802 -97804, G 0270 & G 0271 are used for services Inpatient services are traditionally not charged. Outpatient services are billed on a UB 04 for hospitals and 1500 for private practice. 3/17/2018 7
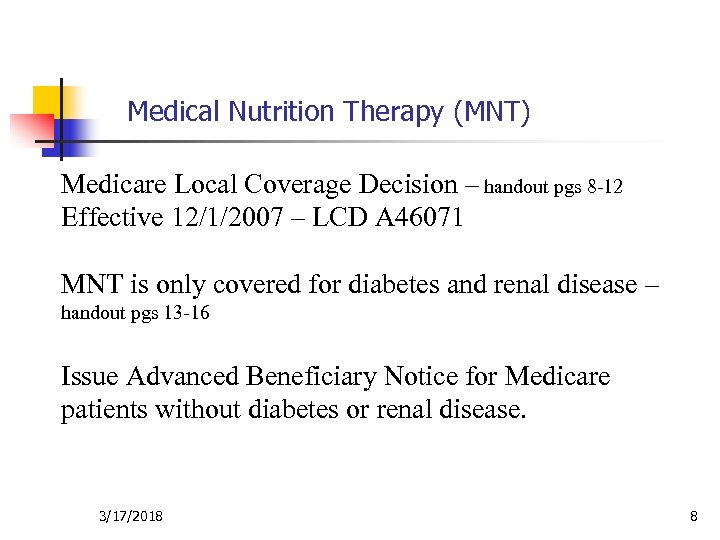
Medical Nutrition Therapy (MNT) Medicare Local Coverage Decision – handout pgs 8 -12 Effective 12/1/2007 – LCD A 46071 MNT is only covered for diabetes and renal disease – handout pgs 13 -16 Issue Advanced Beneficiary Notice for Medicare patients without diabetes or renal disease. 3/17/2018 8
CLAIMS SUBMISSION n n Forms – UB 04 and HCFA 1500 n Used by all payors Information required: n Charges (Services, Supplies & Drugs) n Coding n CPT, HCPCS and/or ICD-9 -CM Procedure codes –handout pgs 3, 4, & 5 n ICD-9 -CM Diagnoses 3/17/2018 9
REIMBURSEMENT - Medicare National Government Services - Indiana – Inpatient -MS DRG (Medical Severity - Diagnosis Related Group) Based on ICD-9 -CM codes – Outpatient l Fee Schedule – based on HCPCS l APC (Ambulatory Payment Classification) – based on HCPCS 3/17/2018 10
Medicare Inpatient Reimbursement Medicare Severity Diagnosis Related Groups (MS-DRGs) See Handout –page 6 & 7 What are DRGs? n n The Diagnosis Related Groups methodology is a classification system adopted by the Centers for Medicare and Medicaid (CMS) on October 1, 1983, as a method to reimburse hospitals providing health care to Medicare patients. Patients in a particular DRG use approximately the same amount of services. Effective October 1, 2007, Medicare Severity-DRGs were implemented (MS-DRGs). There are 745 MS-DRGs. Since 1983 other payors have adopted DRGs as a method of reimbursing hospitals. How are MS-DRGs assigned? n n n The principal diagnosis (the diagnosis that is primarily responsible for the patient being admitted), as well as other information, including secondary diagnosis, procedures, age and sex are used to assign a patient to a MS-DRG. For MS-DRGs, Medicare (CMS) assigned one of three severity levels to each diagnosis code. MCC – major complications or comorbidities CC – complications or comorbidities Non-CC – non complications or comorbidities The presence of secondary diagnoses and its severity level will determine if the case is classified to a higher MS-DRG. How is the hospital reimbursed? n n Each DRG is assigned a different payment amount. A hospital is only reimbursed one DRG per admission regardless of the number of diagnosis treated. In some cases, the patient’s charges are greater than the DRG payment and the hospital must absorb the loss. The patient cannot be billed for the difference. If, on the other hand, the DRG payment is greater than the patient’s charges, the hospital is allowed to keep the difference. There admissions that exceed certain charge parameters. These are referred to as “outliers” and result in additional reimbursement to the hospital. However, the bills of these patients usually exceed additional reimbursement. Outlier payments protect the Hospital from catastrophic health care cases. NOTE: The patient cannot be billed for remaining balance. A “notice of non-coverage” letter must be sent to a patient when the “medical necessity” of admission or continued stay is not met. Only then can a patient be billed for hospital days and/or services covered by their health plan. What is the effect of DRG reimbursement? n n Receiving a fixed amount for each admission forces hospitals to evaluate the delivery of health care. Only by providing necessary services in the most cost-effective manner without sacrificing quality can a facility hope to survive. When the “medical necessity” of acute hospital care is no longer met, other healthcare resources must be utilized. Healthcare payors, by analyzing historical data, will be better able to predict the DRG utilized by their beneficiaries and the resulting expense. 3/17/2018 11
REIMBURSEMENT - Medicaid n Inpatient n n APDRG – based on ICD-9 -CM codes Outpatient n n n 3/17/2018 Fee Schedule – based on HCPCS codes ASC – based on HCPCS codes Revenue Code 12
REIMBURSEMENT - Commercial n n n 3/17/2018 Inpatient – DRG or Percent of charge Outpatient – Percent of charge Physician/private practice – Fee Schedule 13
SUMMARY “Ok…I’ve listened politely …what do I need to remember!” l l Billing – UB 04 – Hospital, 1500 – Physician office Coding – 97802, 97803, 97804, G 0270, G 0271 Reimbursement – only covered for diabetes & renal disease Help your clients understand billing, coding & reimbursement 3/17/2018 14
Where to Get More Information n Medicare & Medicaid n n www. cms. hhs. gove www. ngsmedicare. com www. indianamedicaid. com Evelyn Alwine, RHIA CHDA Director Revenue Cycle Management (812) 353 -9384 ealwine@bloomingtonhospital. org 3/17/2018 15
e9cd256a889602a5e5eb072a5f9b1269.ppt