fd12562aae36437c26e430965cc07b70.ppt
- Количество слайдов: 41
All About Surgical Site Infections Lessons learned from the SSI surveillance pilot, SSI mini grant program, and the data presentation collaborative Andrea Alvarez, MPH HAI Program Coordinator Virginia Department of Health Jacqueline P. Butler, CIC Dir, Infection Prevention & Control Sentara Healthcare November 10, 2011
SSI Surveillance Pilot: Purpose Ø Public reporting expectations increasing § Multiple factors to consider when choosing a SSI for public reporting Ø Troubleshoot issues with surveillance definitions Ø Quantify time requirements for surveillance Ø Gather lessons to help prepare other facilities for reporting
Perceived Pilot Benefits Ø Increase awareness of SSIs § More focus on prevention practices, monitoring associated outcomes, physician awareness of surveillance definitions Ø High profile, high risk, high priority procedures Ø Providing standardized benchmark data Ø Prepare for future reporting requirements § Gain more experience in NHSN data entry § Increase upload or electronic capabilities § Quantify the time associated with procedure surveillance § Identify demands for reporting to facilitate processes to reduce burden Ø Feed data back to those who can make a difference
SSI Pilot: Methods – Selecting Hospitals and Procedures Ø Coronary artery bypass graft (CABG), hip replacement (HPRO), knee replacement (KPRO) surgeries § Consumer interest, experiences of other states, morbidity Ø Surgical Care Improvement Project (SCIP) antibiotic measures § Align process measures with outcome measures § Pilot feasibility of publicly reporting procedure-specific SCIP data Ø 18 hospitals § Randomly selected by bedsize category and number of procedures performed Ø Voluntary participation § Incentives: educational stipend (conferences, journal subscriptions, etc. )
Pre-Survey Ø 18/18 facilities responded Ø Well prepared: (100%) § 100% enrolled in NHSN and used NHSN definitions § 94% calculated SSI rates Ø Relatively well prepared: § 2/3 currently collected patient-level information § Prevention efforts already underway § SSI surveillance deemed high or medium priority Ø Not well prepared: § One facility was currently entering data into NHSN for the pilot procedure § No facilities currently uploaded denominator data § Limited communication between surgical and IP databases § 50% perceived surveillance to be somewhat or very difficult
Methods - Training Ø Partnership with APIC-VA for training and distribution of incentives Ø One-day training (June 9, 2010) § Case studies prepared by APIC-VA Ø Monthly conference calls § Surveillance Q&A § Data import discussions § Feedback of data

Some Surveillance Pointers Ø Definitions – Ensure the latest version of the definitions are being used § Deep incisional vs. organ space § Increases consistency and standardization Ø SSIs are attributed to the date of the operation § For SSIs identified on readmission, on the event form use the date of admission and discharge for the surgery visit Ø All surgical procedures must be entered into NHSN § Not only procedures with an event (like CLABSIs) Only need to report the required sensitivities Ø To report a pathogen that is not on the list of common pathogens, right-click in pathogen field Ø
NHSN Clarifications Ø Deep incisional vs. organ space § If an incision is opened, the infection is counted as deep incisional no matter where it travels ØA knee that has never been operated on before is always a primary regardless of whether it is a total or partial surgery Ø Transplant § Includes internal staples § Does not include a blood transfusion Ø SSI standardized infection ratios (SIRs) only include primary sites
Methods – Data Reporting Ø Monthly entry of procedures and infection events into NHSN § Procedures from July – Dec 2010 with 6 months of post-discharge surveillance Ø Quarterly submission of SCIP data § Jan-June 2010 (baseline), July-Dec 2010 (pilot) Ø Time and effort § Time spent on surveillance § Number of staff involved with surveillance
Electronic Upload Methods: ASCII File Ø Comma delimited ASCII file (. txt or. csv) created by the facility § Can be generated from different external sources, such as infection prevention databases or hospital information systems § Requires assistance of operating room and/or IT staff § Specifications for values, format, and data requirements must be followed Ø Specifications and instructions available on NHSN website: § http: //www. cdc. gov/nhsn/PDFs/Importing. Procedure Data_current. pdf
Electronic Upload Methods: CDA Ø Clinical Document Architecture (CDA) § Health Level 7 (HL 7) standards used to provide a consistent format framework for electronic documents § Not all vendors have the capacity to create documents in this HL 7 framework Ø Specifications and instructions available on NHSN website § http: //www. cdc. gov/nhsn/ CDA_e. Surveillance. html Ø Examples of vendors* by APIC *List compiled with CDA compatibility: § Atlas Development Corporation § BD Diagnostics (formerly known as AICE or ICPA) § Care. Fusion / Med. Mined™ from Cardinal Health § Cerner Corporation § Epi. Quest § ICNet International Limited § RL Solutions § Safety. Surveillor® by Premier § Sentri 7 by Pharmacy. One § Thera. Doc Hospira, Inc. § Vecna Technologies § Vigi. Lanz Corporation
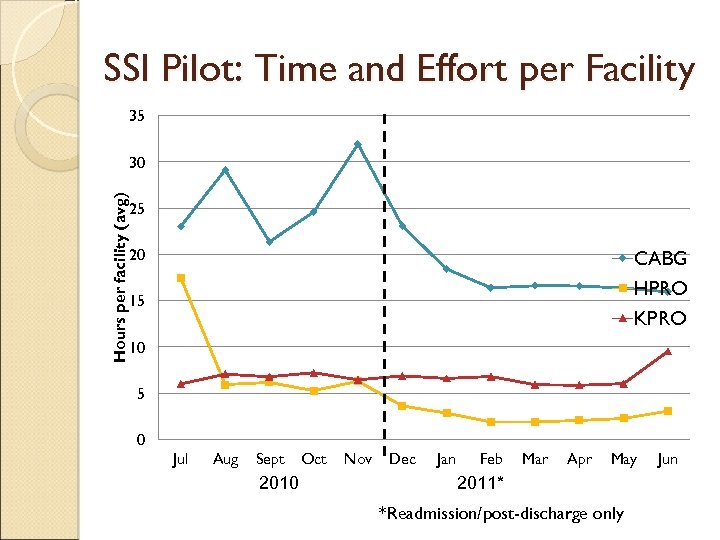
SSI Pilot: Time and Effort per Facility 35 Hours per facility (avg) 30 25 20 CABG HPRO KPRO 15 10 5 0 Jul Aug Sept 2010 Oct Nov Dec Jan Feb Mar Apr May 2011* *Readmission/post-discharge only Jun
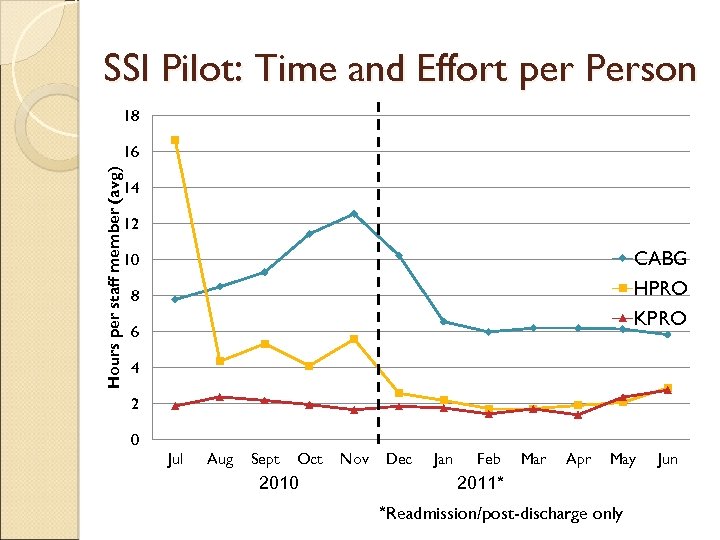
SSI Pilot: Time and Effort per Person 18 Hours per staff member (avg) 16 14 12 CABG HPRO KPRO 10 8 6 4 2 0 Jul Aug Sept Oct 2010 Nov Dec Jan Feb Mar Apr May 2011* *Readmission/post-discharge only Jun
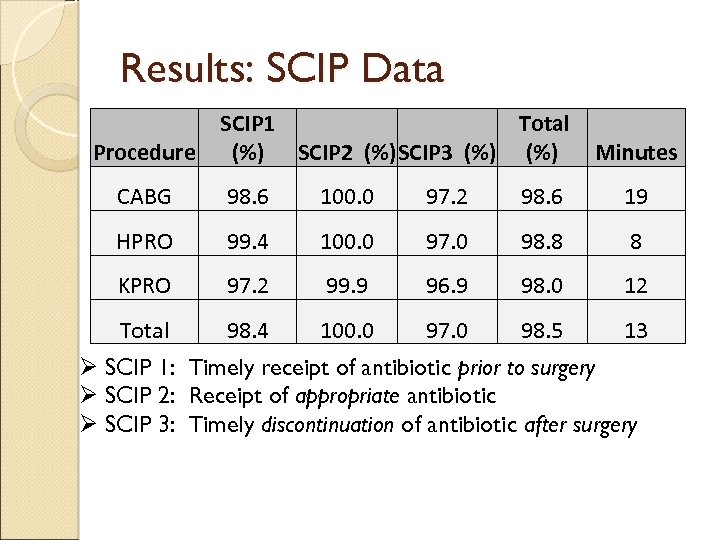
Results: SCIP Data Procedure SCIP 1 Total (%) SCIP 2 (%)SCIP 3 (%) Minutes CABG 98. 6 100. 0 97. 2 98. 6 19 HPRO 99. 4 100. 0 97. 0 98. 8 8 KPRO 97. 2 99. 9 96. 9 98. 0 12 Total 98. 4 100. 0 97. 0 98. 5 13 Ø SCIP 1: Timely receipt of antibiotic prior to surgery Ø SCIP 2: Receipt of appropriate antibiotic Ø SCIP 3: Timely discontinuation of antibiotic after surgery
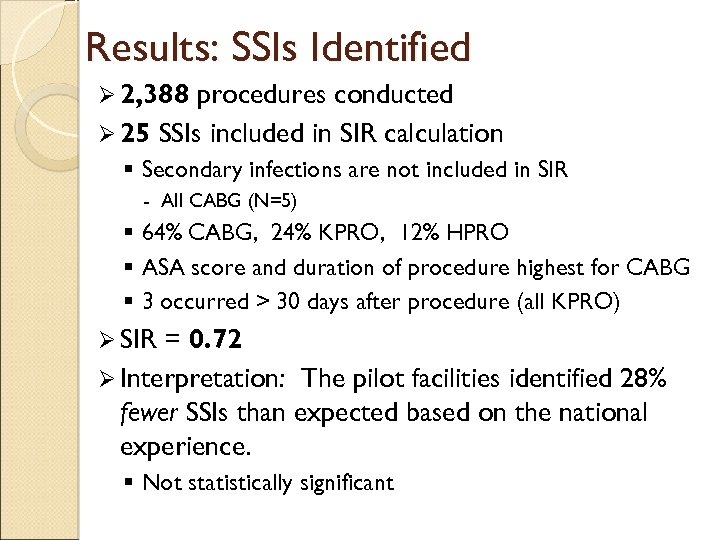
Results: SSIs Identified Ø 2, 388 procedures conducted Ø 25 SSIs included in SIR calculation § Secondary infections are not included in SIR - All CABG (N=5) § 64% CABG, 24% KPRO, 12% HPRO § ASA score and duration of procedure highest for CABG § 3 occurred > 30 days after procedure (all KPRO) Ø SIR = 0. 72 Ø Interpretation: The pilot facilities identified 28% fewer SSIs than expected based on the national experience. § Not statistically significant
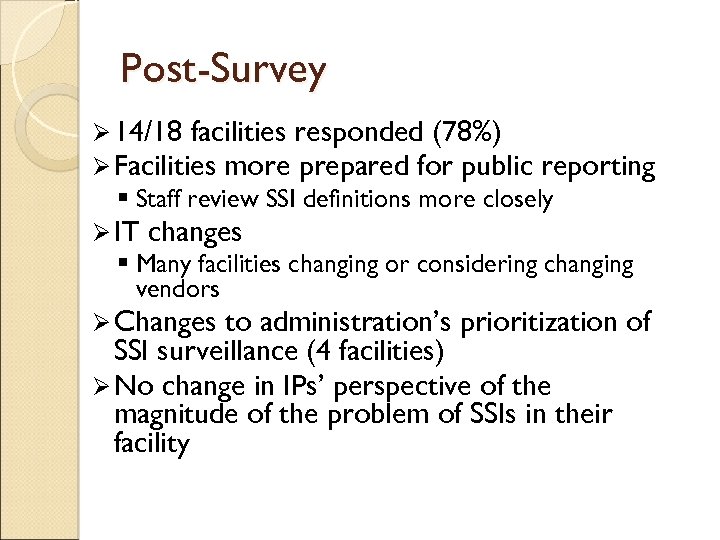
Post-Survey Ø 14/18 facilities responded (78%) Ø Facilities more prepared for public reporting § Staff review SSI definitions more closely Ø IT changes § Many facilities changing or considering changing vendors Ø Changes to administration’s prioritization of SSI surveillance (4 facilities) Ø No change in IPs’ perspective of the magnitude of the problem of SSIs in their facility
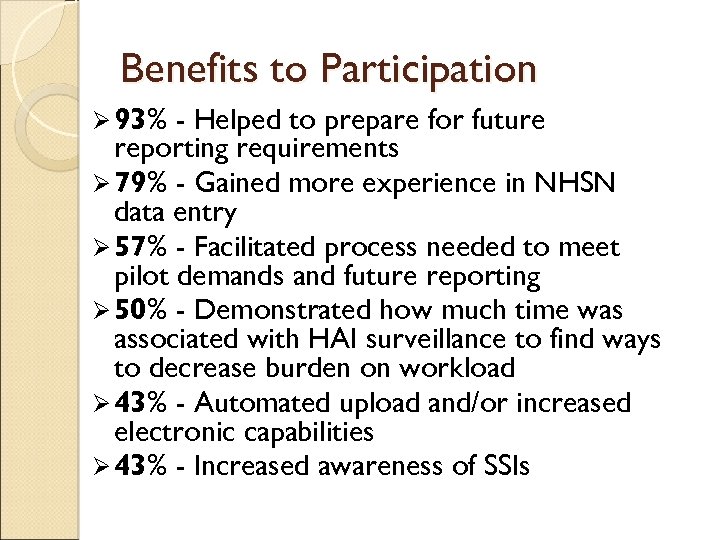
Benefits to Participation Ø 93% - Helped to prepare for future reporting requirements Ø 79% - Gained more experience in NHSN data entry Ø 57% - Facilitated process needed to meet pilot demands and future reporting Ø 50% - Demonstrated how much time was associated with HAI surveillance to find ways to decrease burden on workload Ø 43% - Automated upload and/or increased electronic capabilities Ø 43% - Increased awareness of SSIs
Barriers Encountered Ø 50% Learning curve § Data entry § Importing data Ø 43% Time/resource limitations § Data entry § Staffing Ø 29% No barriers Ø 14% Post-discharge surveillance Ø 14% Consistency between facilities
Electronic Upload to NHSN Ø Pre-survey: Ø 6 0 facilities End of pilot: 9 facilities (50%!) facilities submitted feedback on upload process § 4 used Clinical Document Architecture (CDA) technology - 3 BD/AICE, 1 unspecified vendor - Decreases in monthly surveillance effort after implementing CDA 8 hours to 2 hours 8 hours to 1 hour - Time required to set up import averaged several months § 2 used. CSV file - Decreased monthly surveillance effort in one hospital from 5 hours to 1 hour - Took 2 months for one hospital to set up its file transmission § 2 hospitals used DICON to help with their electronic import § 4 of these hospitals used Meditech for their patient medical records
Lessons Learned / Challenges Ø Electronic medical record system (EMR) is necessary for the electronic upload any movement towards increased use of EMR would be of help to the facility Ø Helpful to talk to other facilities using the same systems and see if they have been able to set up a file transfer § Sometimes easier for facility IT staff to talk to each other rather than IP trying to explain to IT what is needed Ø Importance for quality of monitoring all exported data
Lessons Learned / Challenges Ø Operating room system capability and compatibility Ø Writing the data dictionaries – challenge! § Concern about changing dictionaries/remapping elements if NHSN amends definitions or changes required fields Ø Team approach required (quality, IT, other departments) § Establish importance of support of the infection prevention program on a local level first § IT support is critical for implementation and to address data quality Ø Vendor role representatives can play a beneficial
PERSPECTIVES FROM THE PARTICIPANTS
Experiences of a Large System Sentara Healthcare (SH): Ø >23, 000 staff, >100 care giving sites, including 10 acute care hospitals with a total of 2, 349 beds Sentara Norfolk General Hospital / Sentara Heart Hospital Ø Patients receive comprehensive cardiac services - from diagnostics to open heart surgery and transplants. Ø State-of-the-art hospital features all-private rooms, including 112 inpatient beds and 45 pre/post procedural rooms for patients undergoing interventional cardiac procedures. Ø Houses 5 cardiac operating rooms designed to accommodate 2, 000 cardiac surgeries a year.
Timeline of Sentara’s Pilot Period Ø Calm down Ø Education – June 9, 2010 Ø Define current surveillance process for CABG Ø Develop a Team (IT, Contracted Vendor, Cardiac Auditors, Leadership, IP&C) to research ability to electronically export denominator surgical data to NHSN Ø Contracted Cardiac Vendor building a background program to develop a report off the STS Cardiac Surgery Database (CSD) for exporting Ø Began reporting requirements for pilot project (numerator data, denominator data export, SCIP measure data, time & effort measures) – September 1, 2010 for July 2010 data Ø Completion – ongoing…Why stop a good process?
Sentara’s Experiences Pit Falls: ØTook time to map SH surgical denominator components (STS CSD) to NHSN template for export ØTime allotment for cardiac abstractors to review surgical patients ØContracted vendor - Armus Experience: ØPositive ØDemonstrated SH’s ability to address issues of mandatory reporting
Building in a Collaborative Ø Requirement of ARRA funding Ø Create a project to be flexible and responsive to acute care IPs’ workload § Collecting data presentation templates § Sharing best practices for data feedback Ø Monthly conference calls Ø Survey given to IPs and unit-specific staff to capture the various perceptions of data utility
Data Presentation Survey Collect baseline of knowledge regarding data presentation practices targeted to direct care staff Ø Sent to IPs, direct care staff in a selected unit/area Ø § 18 facilities (100%): 17 IPs and 84 staff General statements about use of data to lower HAI rates or impact infection prevention compliance Ø Types of staff and their perceived awareness of HAI data and compliance with infection prevention practices Ø Outcome and process measures staff want to see and are currently provided Ø Types of data and whether they are easy to understand, useful, and currently presented Ø
Data Presentation Survey Results: IP and Staff Perceptions Ø Awareness of HAI data promotes dialogue among staff and impacts infection prevention compliance Ø IPs more likely to think that SSI rates were improving (65% vs. 48%) Ø Most respondents thought unit-specific HAI data were valid and reliable, easy to understand, timely, and shared at least quarterly
Survey Results (cont’d) Ø Color coding, comparisons (to average, benchmark) most useful to staff Ø Color coding, comparisons, HAI rates, number of HAIs, and number of days since last infection were most easy to understand Ø SIR – used in some hospitals (20%), useful (38%), easy to understand (26%) Ø HAI data most often presented: HH, CLABSI Ø Staff want environmental cleaning compliance data; however, it is least likely
Survey Results (cont’d) Ø Differences in awareness of what data are presented (IPs vs. staff receiving data) Ø Perceived differences in awareness of data and infection prevention compliance by type of staff § Most aware and compliant: nursing leadership, unit nurses § Least aware and compliant: physicians Ø IPs share data most often with units and Infection Control Committee § >75% of respondents present HH, BSIs, SSIs, UTIs, VAPs § >75% of respondents present comparison HAI data
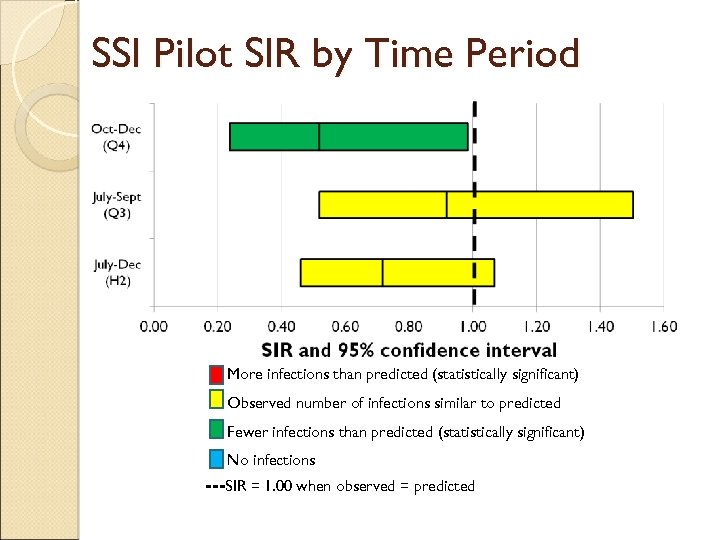
SSI Pilot SIR by Time Period More infections than predicted (statistically significant) Observed number of infections similar to predicted Fewer infections than predicted (statistically significant) No infections ---SIR = 1. 00 when observed = predicted
SSI Mini-Grant Program Ø Any activities that support implementation of the NHSN Procedure-Associated Module, including but not limited to: § Equipment and services, such as administrative and informatics costs - Example: upgrading or modifying internal systems § Training and education - Example: training for staff responsible for collecting and/or entering surgical site infection surveillance data § Consultative and technical assistance - Example: programmer support to help create an electronic file to upload surgical procedure data directly into NHSN § Administrative support
Awardees Ø Applications reviewed by VDH and Virginia Hospital & Healthcare Association (VHHA) Ø 22 hospitals Ø Total of ~$290, 000 Ø Monies dispersed by July 2011
PERSPECTIVES FROM THE PARTICIPANTS
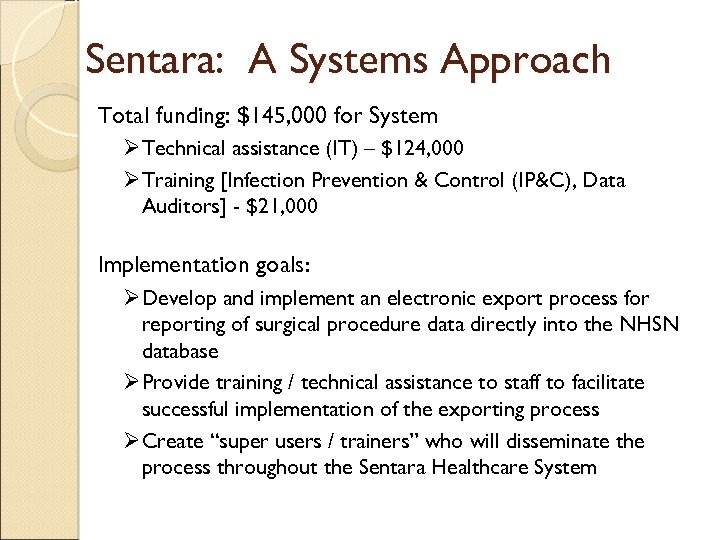
Sentara: A Systems Approach Total funding: $145, 000 for System Ø Technical assistance (IT) – $124, 000 Ø Training [Infection Prevention & Control (IP&C), Data Auditors] - $21, 000 Implementation goals: Ø Develop and implement an electronic export process for reporting of surgical procedure data directly into the NHSN database Ø Provide training / technical assistance to staff to facilitate successful implementation of the exporting process Ø Create “super users / trainers” who will disseminate the process throughout the Sentara Healthcare System
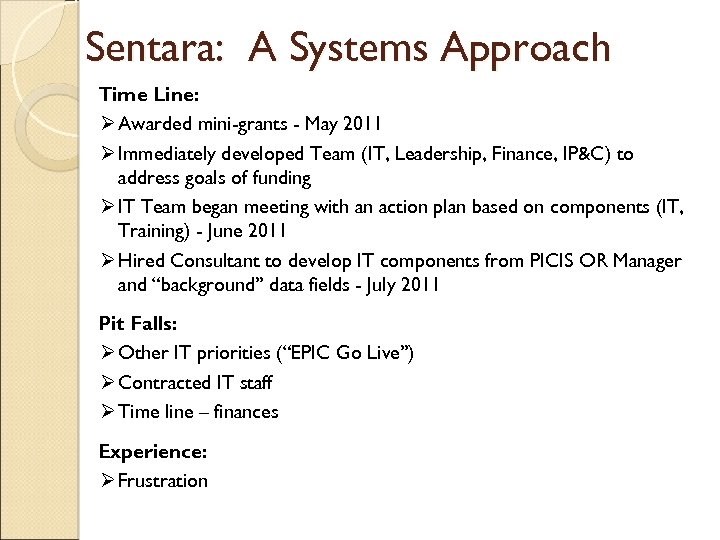
Sentara: A Systems Approach Time Line: Ø Awarded mini-grants - May 2011 Ø Immediately developed Team (IT, Leadership, Finance, IP&C) to address goals of funding Ø IT Team began meeting with an action plan based on components (IT, Training) - June 2011 Ø Hired Consultant to develop IT components from PICIS OR Manager and “background” data fields - July 2011 Pit Falls: Ø Other IT priorities (“EPIC Go Live”) Ø Contracted IT staff Ø Time line – finances Experience: Ø Frustration
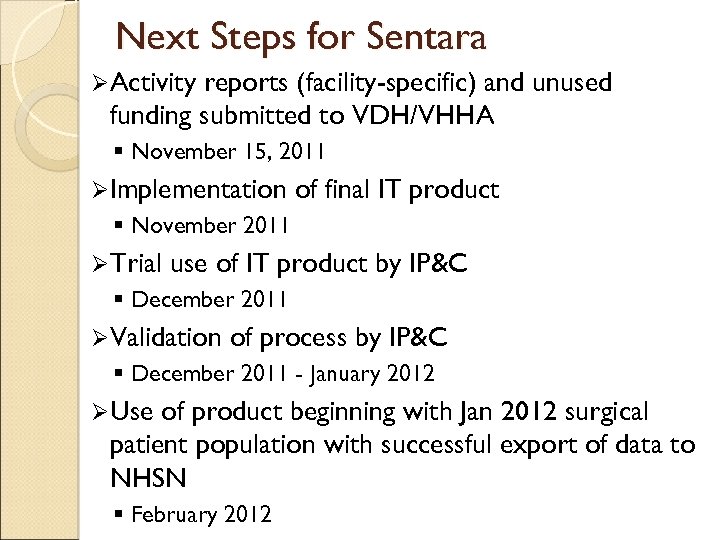
Next Steps for Sentara ØActivity reports (facility-specific) and unused funding submitted to VDH/VHHA § November 15, 2011 ØImplementation of final IT product § November 2011 ØTrial use of IT product by IP&C § December 2011 ØValidation of process by IP&C § December 2011 - January 2012 ØUse of product beginning with Jan 2012 surgical patient population with successful export of data to NHSN § February 2012
Lessons Learned: Other Facilities Ø Electronic medical records are great but present documentation challenges Ø Surgeons do not use ICD-9 codes Ø “Mapping” of required denominator components time consuming Ø IT needs “special handling”
Resources/Take Home Messages Ø Challenge codes of converting CPT codes to ICD-9 § Crosswalk soon available! Ø NHSN forms for Procedure-Associated Module § http: //www. cdc. gov/nhsn/psc_pa. html Ø Map entire facility in NHSN – infections can happen anywhere Ø Resources to Help Build Business Case for Electronic Upload (VDH document) Ø Future training opportunities – APIC-VA and NHSN
Acknowledgments Ø VDH: Dana Burshell, Carol Jamerson, Diane Woolard Ø VHHA: Barbara Brown Ø APIC-VA Ø SSI pilot participants Ø SSI mini-grant recipients
The Purpose of Our Work: “The names of the patients whose lives we save can never be known. Our contribution will be what did not happen to them” Donald M. Berwick, MD, MPP Former President and CEO of IHI Current Administrator of CMS Andrea. Alvarez@vdh. virginia. gov: JPButler@sentara. com: 804 -864 -8097 757 -388 -3949
fd12562aae36437c26e430965cc07b70.ppt