fbd8fcaaaad07ecfba25f8fbc0d36381.ppt
- Количество слайдов: 61
 Aligning with Physicians to Improve Care and Create Value AMGA IQL, September 2011 Mark Shields, MD, MBA Senior Medical Director
Aligning with Physicians to Improve Care and Create Value AMGA IQL, September 2011 Mark Shields, MD, MBA Senior Medical Director
 Disclosure § Nothing in Today’s Presentation Should Be Construed as Advising or Encouraging Any Person to Deal, Refuse to Deal or Threaten to Refuse to Deal with Any Payer, or Otherwise Interfere with Commerce § Opinions Expressed by Speakers are Their Own § APP Assumes No Responsibility for the Reliance by Conference Participants on Materials Presented at Today’s Session 2
Disclosure § Nothing in Today’s Presentation Should Be Construed as Advising or Encouraging Any Person to Deal, Refuse to Deal or Threaten to Refuse to Deal with Any Payer, or Otherwise Interfere with Commerce § Opinions Expressed by Speakers are Their Own § APP Assumes No Responsibility for the Reliance by Conference Participants on Materials Presented at Today’s Session 2
 Learning Objectives Participants will be able to: § Understand Challenges to ACO Development § Understand How Clinical Integration Drives Outcomes § Describe Key Components of Clinical Integration that Lead to Success 3
Learning Objectives Participants will be able to: § Understand Challenges to ACO Development § Understand How Clinical Integration Drives Outcomes § Describe Key Components of Clinical Integration that Lead to Success 3
 Presentation Topics § APP Overview and Role of CI § Integrating Physicians § CI to ACO 4
Presentation Topics § APP Overview and Role of CI § Integrating Physicians § CI to ACO 4
 Advocate Health Care § $4. 5 Billion Annual Revenue § AA Rated § 12 Acute Care Hospitals – – 2 Children’s Hospitals 5 Level 1 Trauma Centers 4 Major Teaching Hospitals 4 Magnet Designations § Over 250 Sites of Care – Advocate Medical Group – – – 5 Dreyer Medical Clinic Occupational Health Imaging Centers Immediate Care Centers Surgery Centers Home Health / Hospice
Advocate Health Care § $4. 5 Billion Annual Revenue § AA Rated § 12 Acute Care Hospitals – – 2 Children’s Hospitals 5 Level 1 Trauma Centers 4 Major Teaching Hospitals 4 Magnet Designations § Over 250 Sites of Care – Advocate Medical Group – – – 5 Dreyer Medical Clinic Occupational Health Imaging Centers Immediate Care Centers Surgery Centers Home Health / Hospice
 Advocate Physician Partners § § Advocate Physician Partners delivers services throughout Chicagoland. 6 Physician Membership – 1, 100 Primary Care Physicians – 2, 700 Specialist Physicians – Total Membership Includes 900 Advocate. Employed Physicians 10 Acute Care Hospitals and 2 Children’s Hospitals Central Verification Office Certified by NCQA 230, 000 Capitated Lives/700, 000 PPO Lives
Advocate Physician Partners § § Advocate Physician Partners delivers services throughout Chicagoland. 6 Physician Membership – 1, 100 Primary Care Physicians – 2, 700 Specialist Physicians – Total Membership Includes 900 Advocate. Employed Physicians 10 Acute Care Hospitals and 2 Children’s Hospitals Central Verification Office Certified by NCQA 230, 000 Capitated Lives/700, 000 PPO Lives
 Clinical Integration: Definition A structured collaboration among APP physicians and Advocate Hospitals on an active and ongoing program designed to improve the quality and efficiency of health care. Joint contracting with fee-for-service managed care organizations is a necessary component of this program in order to accelerate these improvements in health care delivery. 7
Clinical Integration: Definition A structured collaboration among APP physicians and Advocate Hospitals on an active and ongoing program designed to improve the quality and efficiency of health care. Joint contracting with fee-for-service managed care organizations is a necessary component of this program in order to accelerate these improvements in health care delivery. 7
 Challenges of Health Reform § Large Multi-specialty Groups Are the Exception § 9 of 10 Americans Get Their Medical Care in a Solo or Small Practice* § Infrastructure Is Required to Drive Quality Outcomes Demonstrated by Multi-specialty Groups § Culture Is Not Created Over Night * NEJM 360; 7 Feb. 12, 2009 8
Challenges of Health Reform § Large Multi-specialty Groups Are the Exception § 9 of 10 Americans Get Their Medical Care in a Solo or Small Practice* § Infrastructure Is Required to Drive Quality Outcomes Demonstrated by Multi-specialty Groups § Culture Is Not Created Over Night * NEJM 360; 7 Feb. 12, 2009 8
 Clinical Integration is the Foundation of an ACO § Provides Infrastructure for Integration of Small Practices § Overcomes Problems Seen Within the Fee-for -Service Model – Incentives to Providers Drive Improvement § Creates Business Case for Hospital and Doctors to Work for Common Goals § Allows One Approach for Commercial and Governmental Payers 9
Clinical Integration is the Foundation of an ACO § Provides Infrastructure for Integration of Small Practices § Overcomes Problems Seen Within the Fee-for -Service Model – Incentives to Providers Drive Improvement § Creates Business Case for Hospital and Doctors to Work for Common Goals § Allows One Approach for Commercial and Governmental Payers 9
 Presentation Topics § APP Overview and Role of CI § Integrating Physicians § CI to ACO 10
Presentation Topics § APP Overview and Role of CI § Integrating Physicians § CI to ACO 10
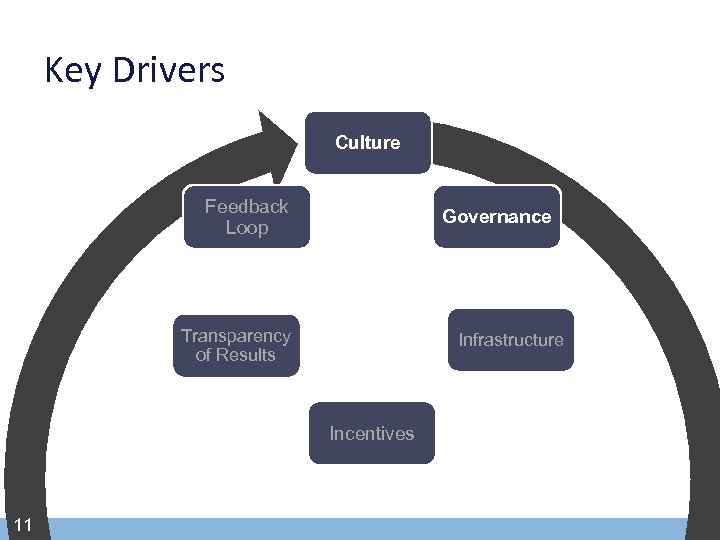 Key Drivers Culture Feedback Loop Governance Transparency of Results Infrastructure Incentives 11
Key Drivers Culture Feedback Loop Governance Transparency of Results Infrastructure Incentives 11
 Creating a Culture of Engaged Physicians § § § Physician Engagement in Governance Physician Leadership Development Shared Identity and Values → “Membership” Infrastructure Investment to Enable Success Appeals to Pride and Sense of Excellence – Recognition for Quality and Efficiency – Consistent Use of Evidence-based Medicine – Power of the Outcomes of the Group 12
Creating a Culture of Engaged Physicians § § § Physician Engagement in Governance Physician Leadership Development Shared Identity and Values → “Membership” Infrastructure Investment to Enable Success Appeals to Pride and Sense of Excellence – Recognition for Quality and Efficiency – Consistent Use of Evidence-based Medicine – Power of the Outcomes of the Group 12
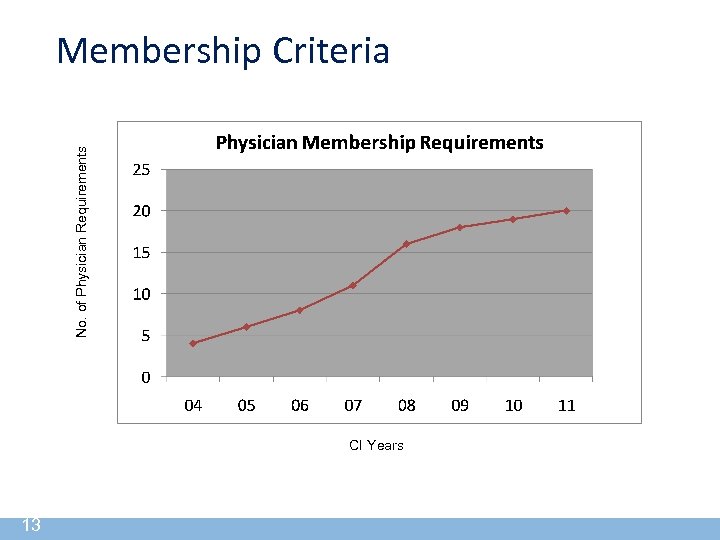 No. of Physician Requirements Membership Criteria CI Years 13
No. of Physician Requirements Membership Criteria CI Years 13
 APP Vision Statement The Vision of Advocate Physician Partners is to be the Leading Care Management and Managed Care Contracting Organization 14
APP Vision Statement The Vision of Advocate Physician Partners is to be the Leading Care Management and Managed Care Contracting Organization 14
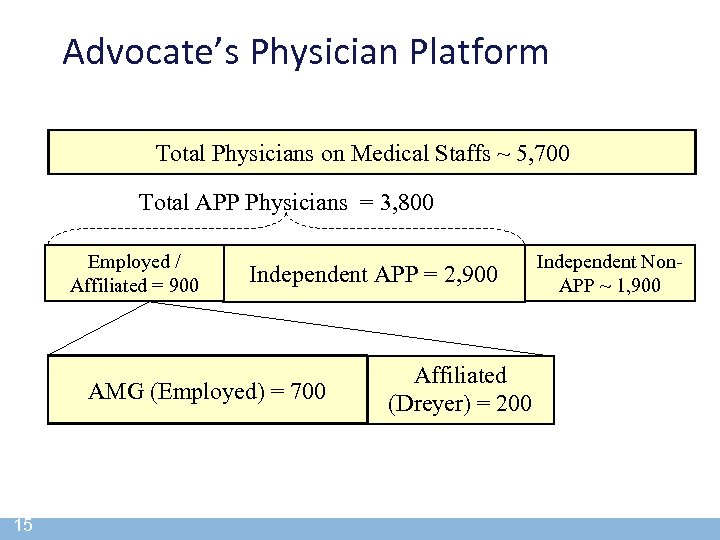 Advocate’s Physician Platform Total Physicians on Medical Staffs ~ 5, 700 Total APP Physicians = 3, 800 Employed / Affiliated = 900 Independent APP = 2, 900 AMG (Employed) = 700 15 Affiliated (Dreyer) = 200 Independent Non. APP ~ 1, 900
Advocate’s Physician Platform Total Physicians on Medical Staffs ~ 5, 700 Total APP Physicians = 3, 800 Employed / Affiliated = 900 Independent APP = 2, 900 AMG (Employed) = 700 15 Affiliated (Dreyer) = 200 Independent Non. APP ~ 1, 900
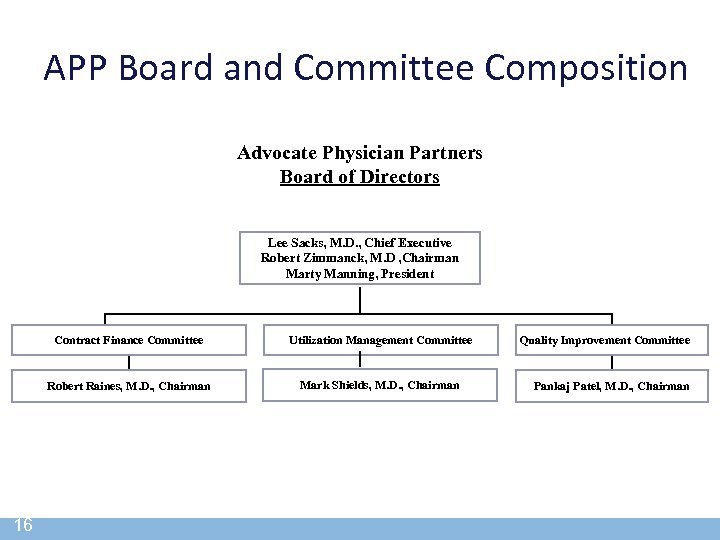 APP Board and Committee Composition Advocate Physician Partners Board of Directors Lee Sacks, M. D. , Chief Executive Robert Zimmanck, M. D , Chairman Marty Manning, President Contract Finance Committee Robert Raines, M. D. , Chairman 16 Utilization Management Committee Mark Shields, M. D. , Chairman Quality Improvement Committee Pankaj Patel, M. D. , Chairman
APP Board and Committee Composition Advocate Physician Partners Board of Directors Lee Sacks, M. D. , Chief Executive Robert Zimmanck, M. D , Chairman Marty Manning, President Contract Finance Committee Robert Raines, M. D. , Chairman 16 Utilization Management Committee Mark Shields, M. D. , Chairman Quality Improvement Committee Pankaj Patel, M. D. , Chairman
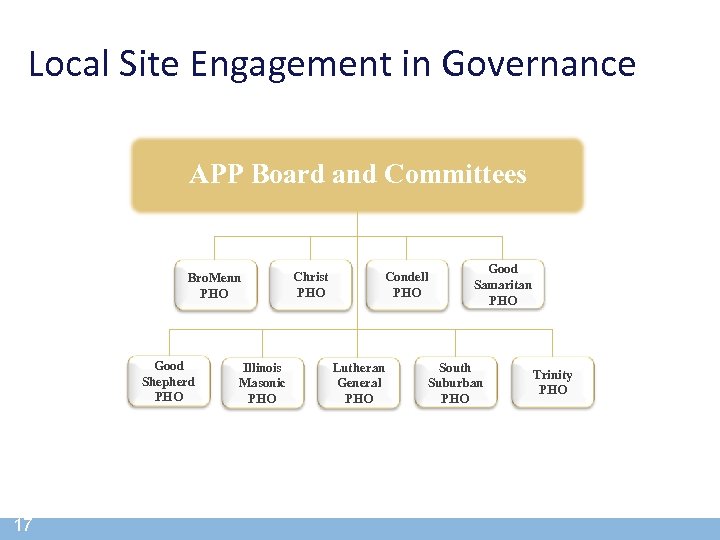 Local Site Engagement in Governance APP Board and Committees Bro. Menn PHO Good Shepherd PHO 17 Illinois Masonic PHO Christ PHO Condell PHO Lutheran General PHO Good Samaritan PHO South Suburban PHO Trinity PHO
Local Site Engagement in Governance APP Board and Committees Bro. Menn PHO Good Shepherd PHO 17 Illinois Masonic PHO Christ PHO Condell PHO Lutheran General PHO Good Samaritan PHO South Suburban PHO Trinity PHO
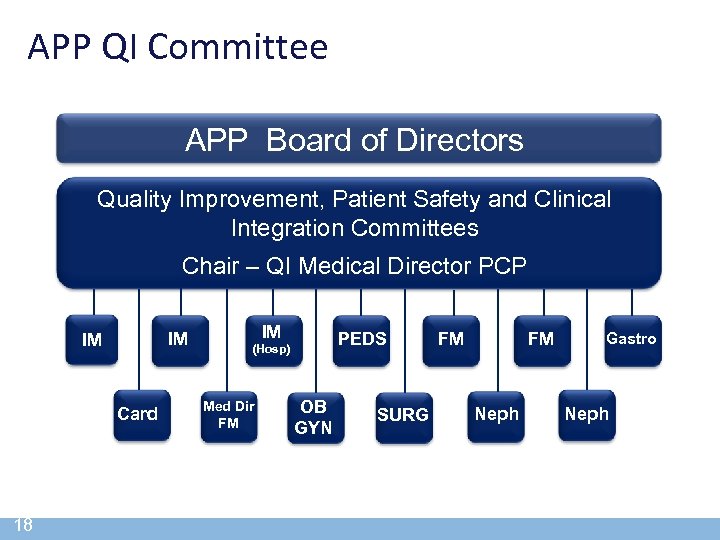 APP QI Committee APP Board of Directors Quality Improvement, Patient Safety and Clinical Integration Committees Chair – QI Medical Director PCP IM IM Card 18 IM PEDS (Hosp) Med Dir FM OB GYN SURG FM FM Neph Gastro Neph
APP QI Committee APP Board of Directors Quality Improvement, Patient Safety and Clinical Integration Committees Chair – QI Medical Director PCP IM IM Card 18 IM PEDS (Hosp) Med Dir FM OB GYN SURG FM FM Neph Gastro Neph
 Physician Leadership Development § Identification and Promotions Via Committees § Formal Governance Training § Mentoring Program for New Leaders § Currently Over 100 Physicians Involved in Governance § Physicians Compensated for Time 19
Physician Leadership Development § Identification and Promotions Via Committees § Formal Governance Training § Mentoring Program for New Leaders § Currently Over 100 Physicians Involved in Governance § Physicians Compensated for Time 19
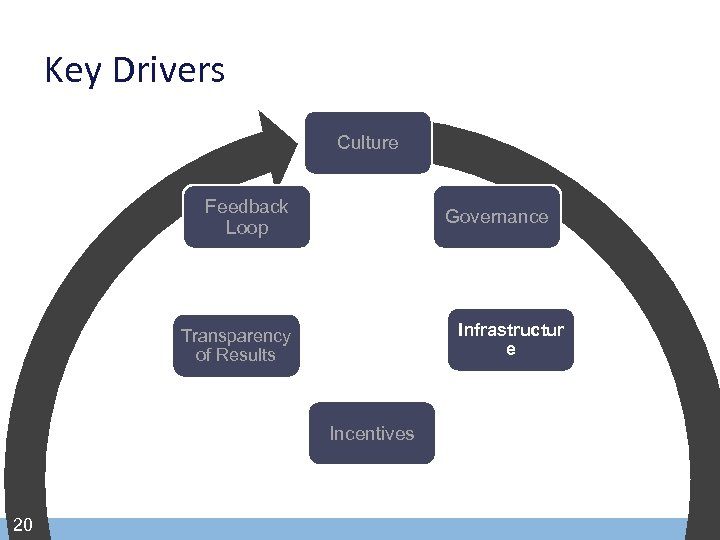 Key Drivers Culture Feedback Loop Governance Infrastructur e Transparency of Results Incentives 20
Key Drivers Culture Feedback Loop Governance Infrastructur e Transparency of Results Incentives 20
 2011 Performance Metrics § Physician Commitment to a Common Broad Set of Clinical Initiatives – 57 Initiatives – Broad Area of Focus – 147 Individual Performance Measures • Primary Care and Specialty – 5 Performance Domains • Clinical Outcomes • Efficiency • Medical and Technological Infrastructure • Patient Safety • Patient Satisfaction Physicians Determine All New Performance Measures 21
2011 Performance Metrics § Physician Commitment to a Common Broad Set of Clinical Initiatives – 57 Initiatives – Broad Area of Focus – 147 Individual Performance Measures • Primary Care and Specialty – 5 Performance Domains • Clinical Outcomes • Efficiency • Medical and Technological Infrastructure • Patient Safety • Patient Satisfaction Physicians Determine All New Performance Measures 21
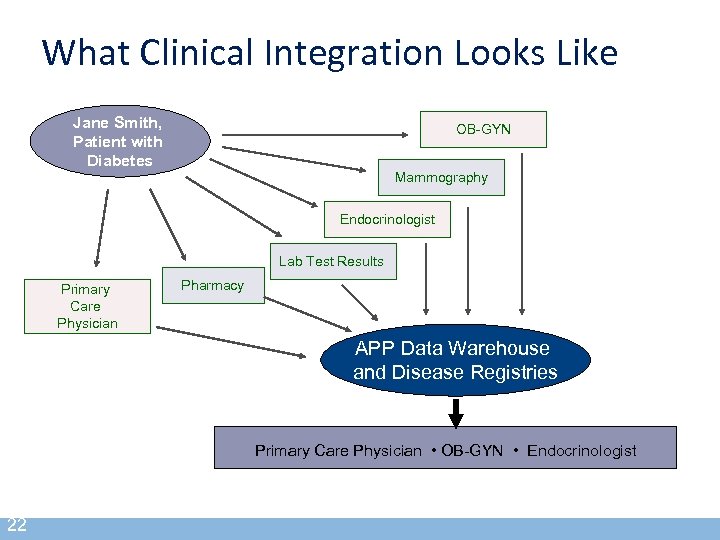 What Clinical Integration Looks Like Jane Smith, Patient with Diabetes OB-GYN Mammography Endocrinologist Lab Test Results Primary Care Physician Pharmacy APP Data Warehouse and Disease Registries Primary Care Physician • OB-GYN • Endocrinologist 22
What Clinical Integration Looks Like Jane Smith, Patient with Diabetes OB-GYN Mammography Endocrinologist Lab Test Results Primary Care Physician Pharmacy APP Data Warehouse and Disease Registries Primary Care Physician • OB-GYN • Endocrinologist 22
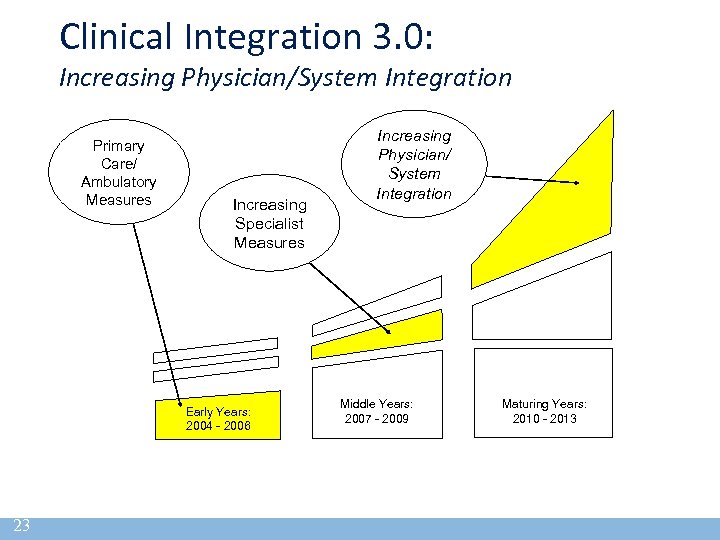 Clinical Integration 3. 0: Increasing Physician/System Integration Primary Care/ Ambulatory Measures Increasing Specialist Measures Early Years: 2004 - 2006 23 Increasing Physician/ System Integration Middle Years: 2007 - 2009 Maturing Years: 2010 - 2013
Clinical Integration 3. 0: Increasing Physician/System Integration Primary Care/ Ambulatory Measures Increasing Specialist Measures Early Years: 2004 - 2006 23 Increasing Physician/ System Integration Middle Years: 2007 - 2009 Maturing Years: 2010 - 2013
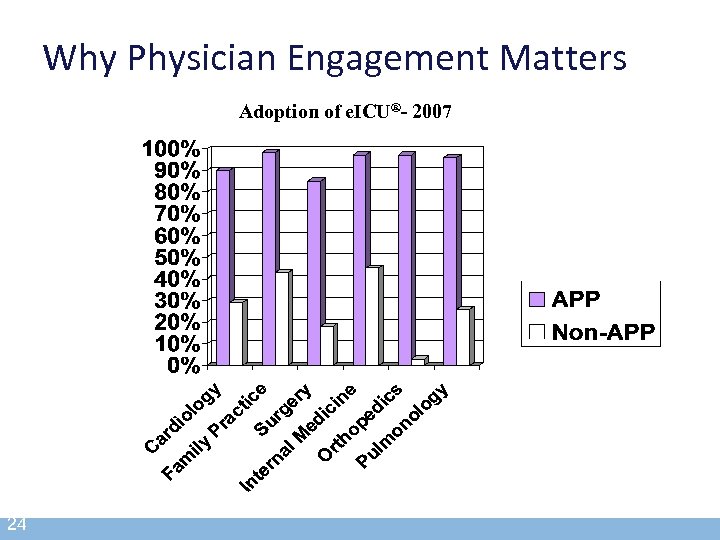 Why Physician Engagement Matters Adoption of e. ICU®- 2007 24
Why Physician Engagement Matters Adoption of e. ICU®- 2007 24
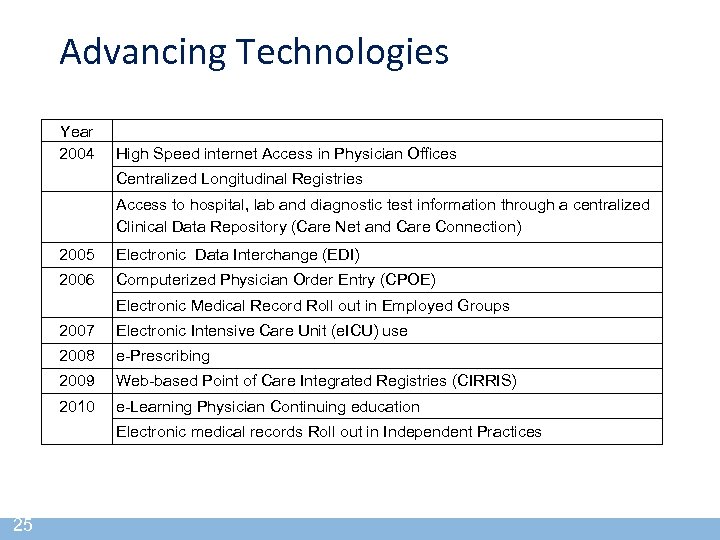 Advancing Technologies Year 2004 High Speed internet Access in Physician Offices Centralized Longitudinal Registries Access to hospital, lab and diagnostic test information through a centralized Clinical Data Repository (Care Net and Care Connection) 2005 Electronic Data Interchange (EDI) 2006 Computerized Physician Order Entry (CPOE) Electronic Medical Record Roll out in Employed Groups 2007 Electronic Intensive Care Unit (e. ICU) use 2008 e-Prescribing 2009 Web-based Point of Care Integrated Registries (CIRRIS) 2010 e-Learning Physician Continuing education Electronic medical records Roll out in Independent Practices 25
Advancing Technologies Year 2004 High Speed internet Access in Physician Offices Centralized Longitudinal Registries Access to hospital, lab and diagnostic test information through a centralized Clinical Data Repository (Care Net and Care Connection) 2005 Electronic Data Interchange (EDI) 2006 Computerized Physician Order Entry (CPOE) Electronic Medical Record Roll out in Employed Groups 2007 Electronic Intensive Care Unit (e. ICU) use 2008 e-Prescribing 2009 Web-based Point of Care Integrated Registries (CIRRIS) 2010 e-Learning Physician Continuing education Electronic medical records Roll out in Independent Practices 25
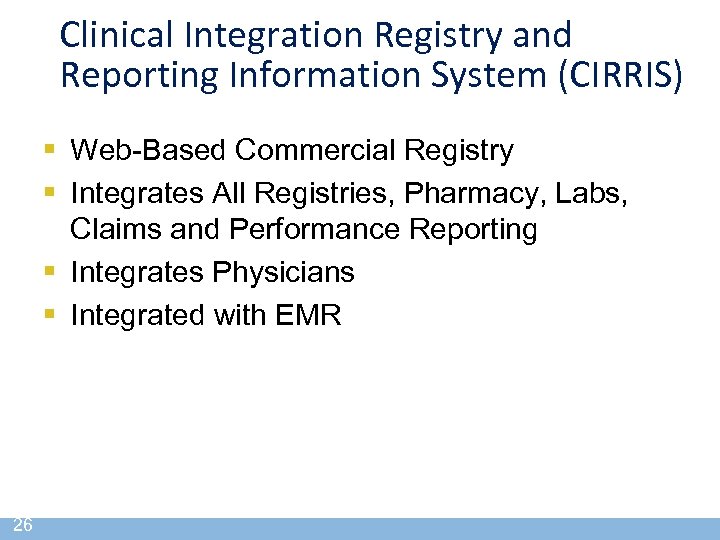 Clinical Integration Registry and Reporting Information System (CIRRIS) § Web-Based Commercial Registry § Integrates All Registries, Pharmacy, Labs, Claims and Performance Reporting § Integrates Physicians § Integrated with EMR 26
Clinical Integration Registry and Reporting Information System (CIRRIS) § Web-Based Commercial Registry § Integrates All Registries, Pharmacy, Labs, Claims and Performance Reporting § Integrates Physicians § Integrated with EMR 26
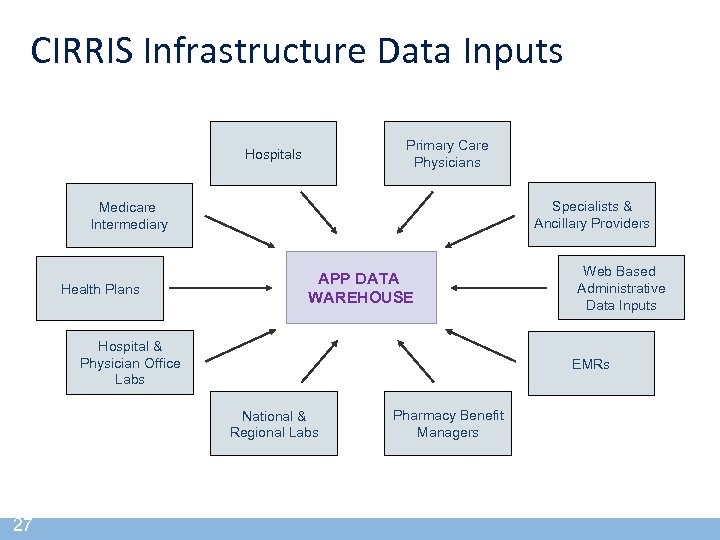 CIRRIS Infrastructure Data Inputs Primary Care Physicians Hospitals Specialists & Ancillary Providers Medicare Intermediary Health Plans APP DATA WAREHOUSE Hospital & Physician Office Labs EMRs National & Regional Labs 27 Web Based Administrative Data Inputs Pharmacy Benefit Managers
CIRRIS Infrastructure Data Inputs Primary Care Physicians Hospitals Specialists & Ancillary Providers Medicare Intermediary Health Plans APP DATA WAREHOUSE Hospital & Physician Office Labs EMRs National & Regional Labs 27 Web Based Administrative Data Inputs Pharmacy Benefit Managers
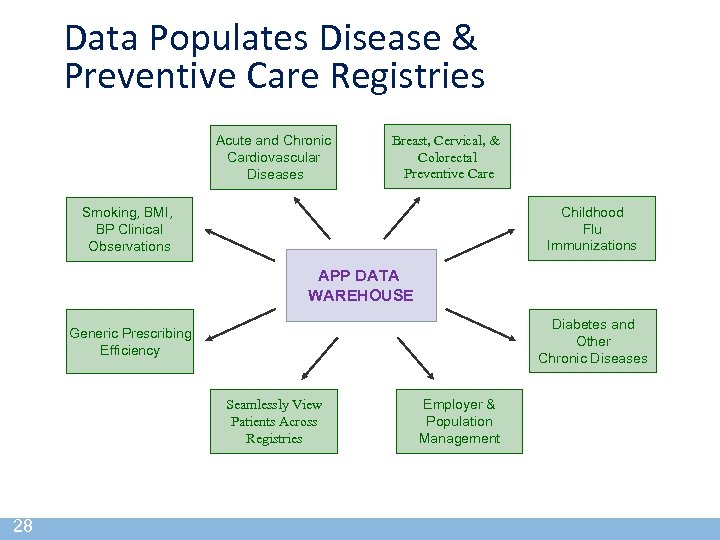 Data Populates Disease & Preventive Care Registries Acute and Chronic Cardiovascular Diseases Breast, Cervical, & Colorectal Preventive Care Childhood Flu Immunizations Smoking, BMI, BP Clinical Observations APP DATA WAREHOUSE Diabetes and Other Chronic Diseases Generic Prescribing Efficiency Seamlessly View Patients Across Registries 28 Employer & Population Management
Data Populates Disease & Preventive Care Registries Acute and Chronic Cardiovascular Diseases Breast, Cervical, & Colorectal Preventive Care Childhood Flu Immunizations Smoking, BMI, BP Clinical Observations APP DATA WAREHOUSE Diabetes and Other Chronic Diseases Generic Prescribing Efficiency Seamlessly View Patients Across Registries 28 Employer & Population Management
 Clinical Integration Program Progress Reports: Background § Progress Reports are Compiled and Made Available Quarterly – 4 th Quarter Progress Report is Reflective of Full Reporting Year Performance • Basis for Determining Physician’s Incentive Fund Payment § Physicians Retrieve a Customized Progress Report and Documentation Supporting Measurement on Key Initiatives (Efficiency Areas) 29
Clinical Integration Program Progress Reports: Background § Progress Reports are Compiled and Made Available Quarterly – 4 th Quarter Progress Report is Reflective of Full Reporting Year Performance • Basis for Determining Physician’s Incentive Fund Payment § Physicians Retrieve a Customized Progress Report and Documentation Supporting Measurement on Key Initiatives (Efficiency Areas) 29
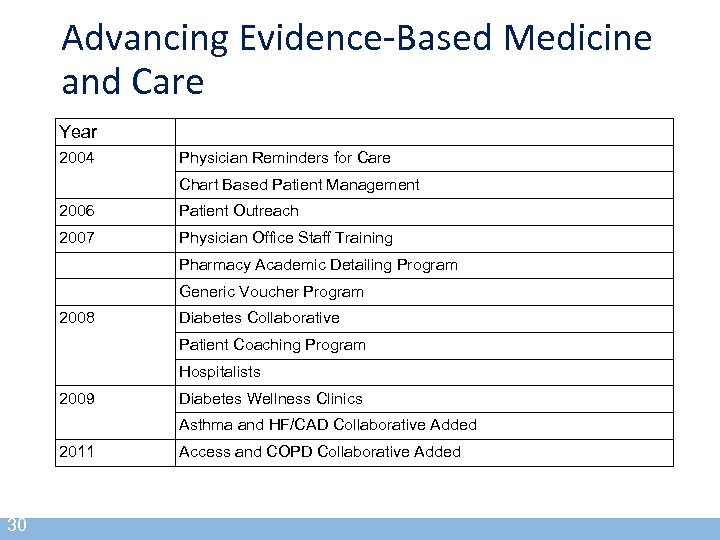 Advancing Evidence-Based Medicine and Care Year 2004 Physician Reminders for Care Chart Based Patient Management 2006 Patient Outreach 2007 Physician Office Staff Training Pharmacy Academic Detailing Program Generic Voucher Program 2008 Diabetes Collaborative Patient Coaching Program Hospitalists 2009 Diabetes Wellness Clinics Asthma and HF/CAD Collaborative Added 2011 30 Access and COPD Collaborative Added
Advancing Evidence-Based Medicine and Care Year 2004 Physician Reminders for Care Chart Based Patient Management 2006 Patient Outreach 2007 Physician Office Staff Training Pharmacy Academic Detailing Program Generic Voucher Program 2008 Diabetes Collaborative Patient Coaching Program Hospitalists 2009 Diabetes Wellness Clinics Asthma and HF/CAD Collaborative Added 2011 30 Access and COPD Collaborative Added
 Evidence-Based Clinical Decisions § E-Learning CME Programs – Congestive Heart Failure – Asthma – Diabetes – Smoking Cessation Counseling – Coaching for Behavioral Changes – Patient Satisfaction Strategies § Protocols § Pharmacist Academic Detailing 31
Evidence-Based Clinical Decisions § E-Learning CME Programs – Congestive Heart Failure – Asthma – Diabetes – Smoking Cessation Counseling – Coaching for Behavioral Changes – Patient Satisfaction Strategies § Protocols § Pharmacist Academic Detailing 31
 Health Plan Commitments Includes All Major Payers in the Market § Risk and Fee-for-Service Contracts § Base and Incentive Compensation § Same Measures Across All Payers – Common Procedures at Practice Level for All Contracted Plans 32
Health Plan Commitments Includes All Major Payers in the Market § Risk and Fee-for-Service Contracts § Base and Incentive Compensation § Same Measures Across All Payers – Common Procedures at Practice Level for All Contracted Plans 32
 Mechanisms to Increase Compliance § § § § 33 APP QI/Credentials Committee Membership Criteria Peer Pressure/Local Medical Director Mandatory Provider Education/CME Physician’s Office Staff Training Financial Incentives/Report Cards Targeted Programs
Mechanisms to Increase Compliance § § § § 33 APP QI/Credentials Committee Membership Criteria Peer Pressure/Local Medical Director Mandatory Provider Education/CME Physician’s Office Staff Training Financial Incentives/Report Cards Targeted Programs
 Key Drivers Culture Feedback Loop Governance Transparency of Results Infrastructure Incentives 34
Key Drivers Culture Feedback Loop Governance Transparency of Results Infrastructure Incentives 34
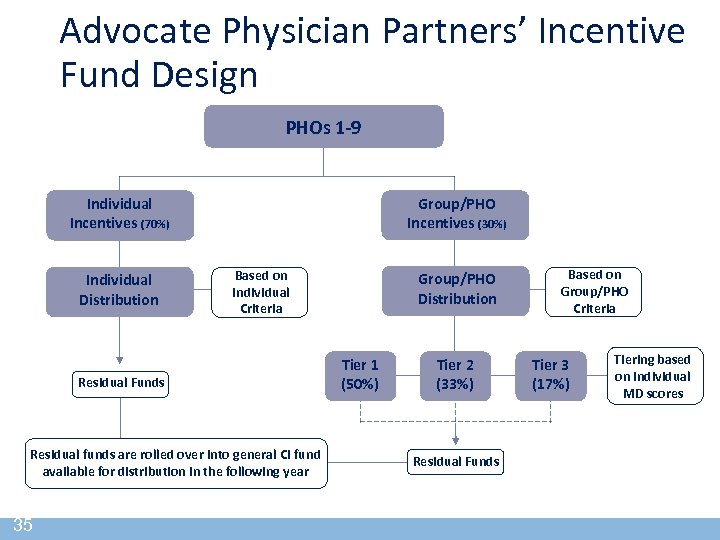 Advocate Physician Partners’ Incentive Fund Design PHOs 1 -9 Individual Incentives (70%) Individual Distribution Group/PHO Incentives (30%) Based on Individual Criteria Residual Funds Residual funds are rolled over into general CI fund available for distribution in the following year 35 Group/PHO Distribution Tier 1 (50%) Tier 2 (33%) Residual Funds Based on Group/PHO Criteria Tier 3 (17%) Tiering based on individual MD scores
Advocate Physician Partners’ Incentive Fund Design PHOs 1 -9 Individual Incentives (70%) Individual Distribution Group/PHO Incentives (30%) Based on Individual Criteria Residual Funds Residual funds are rolled over into general CI fund available for distribution in the following year 35 Group/PHO Distribution Tier 1 (50%) Tier 2 (33%) Residual Funds Based on Group/PHO Criteria Tier 3 (17%) Tiering based on individual MD scores
 Calculation and Distribution of CI Incentives to Physicians § CI Incentive Distribution for Each Physician Based on the Following: – Physician’s Allowable Physician Billings – Individual CI Score – CI Score of the Physician’s Primary PHO – Work Incentive Volume and Performance 36
Calculation and Distribution of CI Incentives to Physicians § CI Incentive Distribution for Each Physician Based on the Following: – Physician’s Allowable Physician Billings – Individual CI Score – CI Score of the Physician’s Primary PHO – Work Incentive Volume and Performance 36
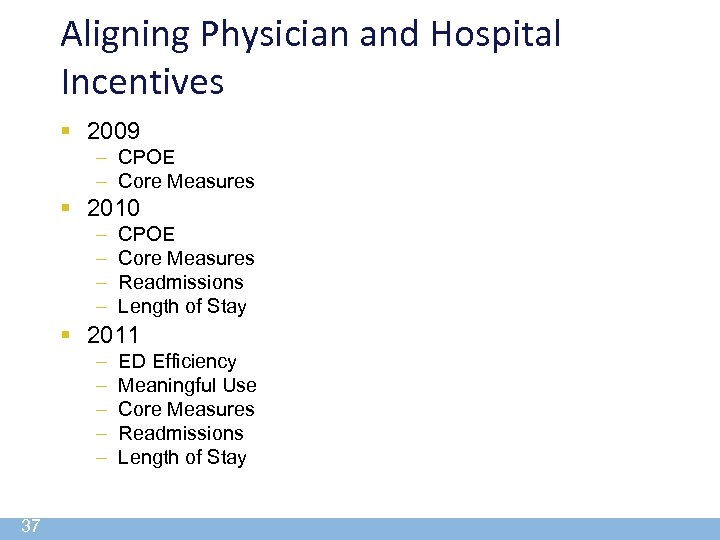 Aligning Physician and Hospital Incentives § 2009 – CPOE – Core Measures § 2010 – – CPOE Core Measures Readmissions Length of Stay § 2011 – – – 37 ED Efficiency Meaningful Use Core Measures Readmissions Length of Stay
Aligning Physician and Hospital Incentives § 2009 – CPOE – Core Measures § 2010 – – CPOE Core Measures Readmissions Length of Stay § 2011 – – – 37 ED Efficiency Meaningful Use Core Measures Readmissions Length of Stay
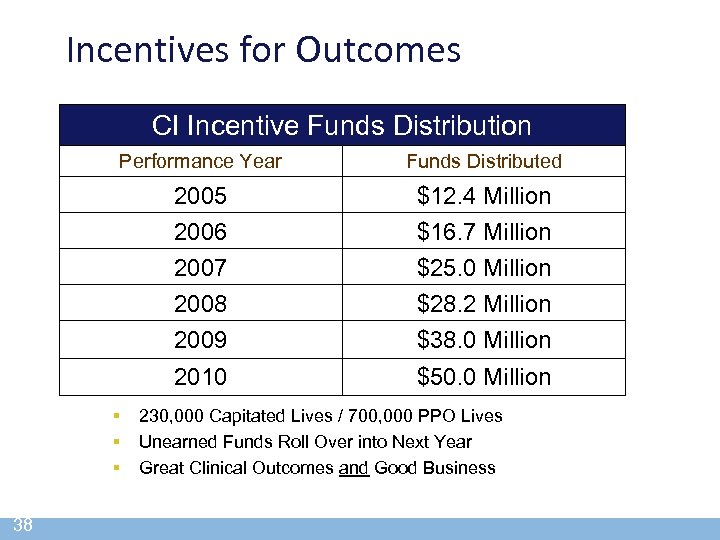 Incentives for Outcomes CI Incentive Funds Distribution Performance Year Funds Distributed 2005 2006 $12. 4 Million $16. 7 Million 2007 2008 2009 $25. 0 Million $28. 2 Million $38. 0 Million 2010 $50. 0 Million § § § 38 230, 000 Capitated Lives / 700, 000 PPO Lives Unearned Funds Roll Over into Next Year Great Clinical Outcomes and Good Business
Incentives for Outcomes CI Incentive Funds Distribution Performance Year Funds Distributed 2005 2006 $12. 4 Million $16. 7 Million 2007 2008 2009 $25. 0 Million $28. 2 Million $38. 0 Million 2010 $50. 0 Million § § § 38 230, 000 Capitated Lives / 700, 000 PPO Lives Unearned Funds Roll Over into Next Year Great Clinical Outcomes and Good Business
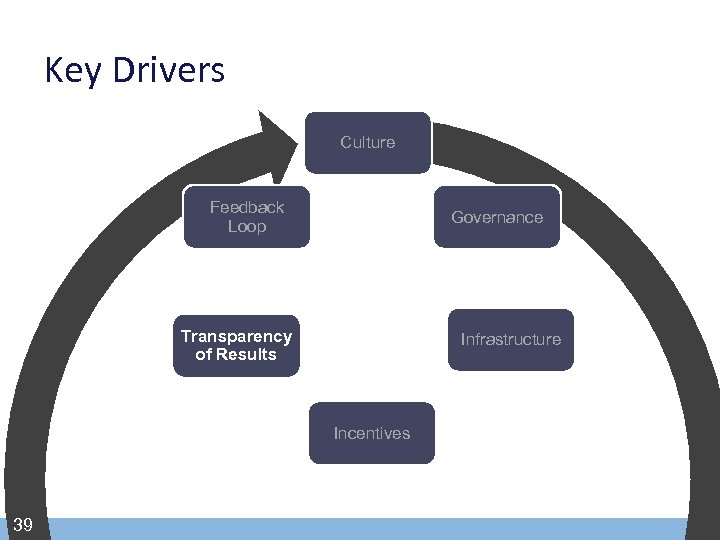 Key Drivers Culture Feedback Loop Governance Transparency of Results Infrastructure Incentives 39
Key Drivers Culture Feedback Loop Governance Transparency of Results Infrastructure Incentives 39
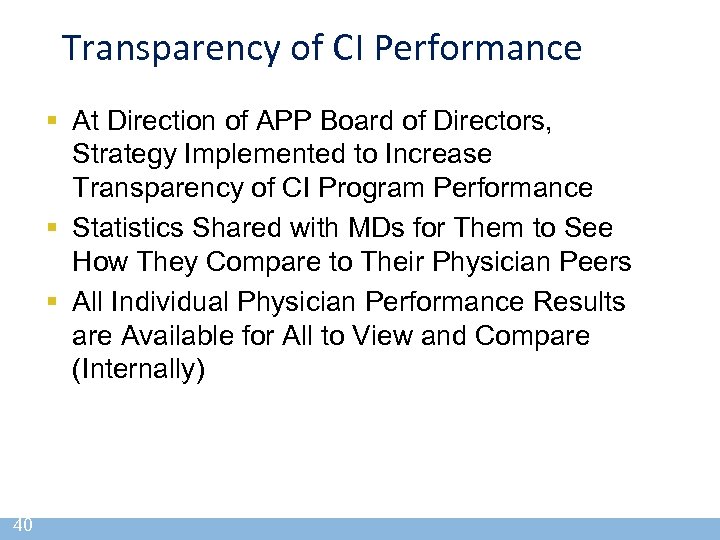 Transparency of CI Performance § At Direction of APP Board of Directors, Strategy Implemented to Increase Transparency of CI Program Performance § Statistics Shared with MDs for Them to See How They Compare to Their Physician Peers § All Individual Physician Performance Results are Available for All to View and Compare (Internally) 40
Transparency of CI Performance § At Direction of APP Board of Directors, Strategy Implemented to Increase Transparency of CI Program Performance § Statistics Shared with MDs for Them to See How They Compare to Their Physician Peers § All Individual Physician Performance Results are Available for All to View and Compare (Internally) 40
 Highlights of 2010 CI Program “Moving the Dial on Quality” § Generic Prescribing: 6 -9% > Local Plans § LDL Good Control in Patients with Diabetes: 43% > National Rate § Childhood Immunizations: 55% > National Rate § Depression Screening: 85% > National Rate § Diabetic Care: Exceeded National Rate on All 9 Measures § Asthma Action Plans: 75% > National Rate 41
Highlights of 2010 CI Program “Moving the Dial on Quality” § Generic Prescribing: 6 -9% > Local Plans § LDL Good Control in Patients with Diabetes: 43% > National Rate § Childhood Immunizations: 55% > National Rate § Depression Screening: 85% > National Rate § Diabetic Care: Exceeded National Rate on All 9 Measures § Asthma Action Plans: 75% > National Rate 41
 2011 Value Report www. advocatehealth. com/valuereport ehealth. com/app or call 1 -800 -3 -ADVOCATE (1 -800 -323 -8622 42
2011 Value Report www. advocatehealth. com/valuereport ehealth. com/app or call 1 -800 -3 -ADVOCATE (1 -800 -323 -8622 42
 Critical Success Factors § Physician Driven § Same Metrics Across All Payers § Minimize Additional Administrative Costs § Additional Funds Recognize Extra Work by Physicians and Staff § Infrastructure Necessary to Support Improvement § Physician/Hospital Alignment 43
Critical Success Factors § Physician Driven § Same Metrics Across All Payers § Minimize Additional Administrative Costs § Additional Funds Recognize Extra Work by Physicians and Staff § Infrastructure Necessary to Support Improvement § Physician/Hospital Alignment 43
 Value for Physicians § § § 44 Better Alignment with Hospital Marketplace Recognition Focus on Outcomes Incentives Compensate for Additional Work Interface with Multiple Payers
Value for Physicians § § § 44 Better Alignment with Hospital Marketplace Recognition Focus on Outcomes Incentives Compensate for Additional Work Interface with Multiple Payers
 Key Drivers Culture Feedback Loop Governance Transparency of Results Infrastructure Incentives 45
Key Drivers Culture Feedback Loop Governance Transparency of Results Infrastructure Incentives 45
 Presentation Topics § APP Overview and Role of CI § Integrating Physicians § CI to ACO 46
Presentation Topics § APP Overview and Role of CI § Integrating Physicians § CI to ACO 46
 From Clinical Integration to Accountable Care 47
From Clinical Integration to Accountable Care 47
 It’s a New Day § Insurers Acknowledge Inability to Manage Rising Costs § Medicare Finances are Not Sustainable § Payers Can No Longer Sustain Double-Digit Increases § Population is Aging § Uninsured Will Enter Care Delivery System 48
It’s a New Day § Insurers Acknowledge Inability to Manage Rising Costs § Medicare Finances are Not Sustainable § Payers Can No Longer Sustain Double-Digit Increases § Population is Aging § Uninsured Will Enter Care Delivery System 48
 Industry Has Difficulty Controlling… § § § 49 Utilization of High End Imaging Readmissions Outpatient Trend New Drugs & Technologies Ambulatory Sensitive Conditions
Industry Has Difficulty Controlling… § § § 49 Utilization of High End Imaging Readmissions Outpatient Trend New Drugs & Technologies Ambulatory Sensitive Conditions
 Change is Necessary § Significant Waste In System § Value of Partnering – To Eliminate Waste – To Have Price Competitive Product § Current Payment Model Does Not Support Shared Vision § Sense of Urgency 50
Change is Necessary § Significant Waste In System § Value of Partnering – To Eliminate Waste – To Have Price Competitive Product § Current Payment Model Does Not Support Shared Vision § Sense of Urgency 50
 Advocate. Care § ACO-Like Contract § Shared Savings Model § Improved Health Care Outcomes – Reductions in Waste, Duplications and Inefficiencies 51
Advocate. Care § ACO-Like Contract § Shared Savings Model § Improved Health Care Outcomes – Reductions in Waste, Duplications and Inefficiencies 51
 Introducing Advocate. Care - A Global Care Contracting Framework § Global Cost Management Overlay On Top of Existing FFS Structures § Responsibility for Managing Comparative Trend § Method for Sharing Savings § Involves Partnering With the Payer § One Model for Governmental & Commercial ACO-Like Contracts 52
Introducing Advocate. Care - A Global Care Contracting Framework § Global Cost Management Overlay On Top of Existing FFS Structures § Responsibility for Managing Comparative Trend § Method for Sharing Savings § Involves Partnering With the Payer § One Model for Governmental & Commercial ACO-Like Contracts 52
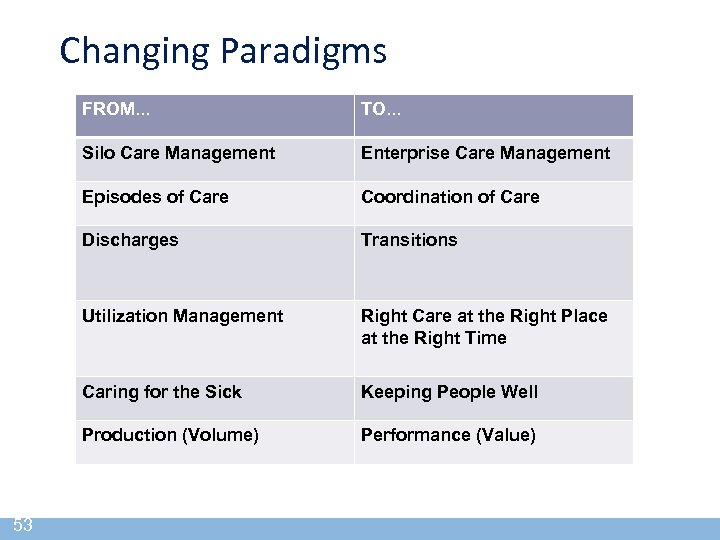 Changing Paradigms FROM. . . Silo Care Management Enterprise Care Management Episodes of Care Coordination of Care Discharges Transitions Utilization Management Right Care at the Right Place at the Right Time Caring for the Sick Keeping People Well Production (Volume) 53 TO. . . Performance (Value)
Changing Paradigms FROM. . . Silo Care Management Enterprise Care Management Episodes of Care Coordination of Care Discharges Transitions Utilization Management Right Care at the Right Place at the Right Time Caring for the Sick Keeping People Well Production (Volume) 53 TO. . . Performance (Value)
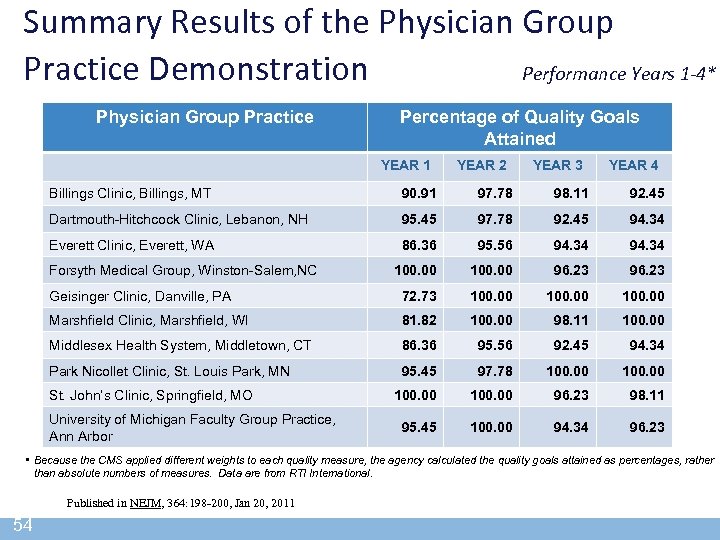 Summary Results of the Physician Group Practice Demonstration Performance Years 1 -4* Physician Group Practice Percentage of Quality Goals Attained YEAR 1 YEAR 2 YEAR 3 YEAR 4 Billings Clinic, Billings, MT 90. 91 97. 78 98. 11 92. 45 Dartmouth-Hitchcock Clinic, Lebanon, NH 95. 45 97. 78 92. 45 94. 34 Everett Clinic, Everett, WA 86. 36 95. 56 94. 34 100. 00 96. 23 Geisinger Clinic, Danville, PA 72. 73 100. 00 Marshfield Clinic, Marshfield, WI 81. 82 100. 00 98. 11 100. 00 Middlesex Health System, Middletown, CT 86. 36 95. 56 92. 45 94. 34 Park Nicollet Clinic, St. Louis Park, MN 95. 45 97. 78 100. 00 96. 23 98. 11 95. 45 100. 00 94. 34 96. 23 Forsyth Medical Group, Winston-Salem, NC St. John’s Clinic, Springfield, MO University of Michigan Faculty Group Practice, Ann Arbor • Because the CMS applied different weights to each quality measure, the agency calculated the quality goals attained as percentages, rather than absolute numbers of measures. Data are from RTI International. Published in NEJM, 364: 198 -200, Jan 20, 2011 54
Summary Results of the Physician Group Practice Demonstration Performance Years 1 -4* Physician Group Practice Percentage of Quality Goals Attained YEAR 1 YEAR 2 YEAR 3 YEAR 4 Billings Clinic, Billings, MT 90. 91 97. 78 98. 11 92. 45 Dartmouth-Hitchcock Clinic, Lebanon, NH 95. 45 97. 78 92. 45 94. 34 Everett Clinic, Everett, WA 86. 36 95. 56 94. 34 100. 00 96. 23 Geisinger Clinic, Danville, PA 72. 73 100. 00 Marshfield Clinic, Marshfield, WI 81. 82 100. 00 98. 11 100. 00 Middlesex Health System, Middletown, CT 86. 36 95. 56 92. 45 94. 34 Park Nicollet Clinic, St. Louis Park, MN 95. 45 97. 78 100. 00 96. 23 98. 11 95. 45 100. 00 94. 34 96. 23 Forsyth Medical Group, Winston-Salem, NC St. John’s Clinic, Springfield, MO University of Michigan Faculty Group Practice, Ann Arbor • Because the CMS applied different weights to each quality measure, the agency calculated the quality goals attained as percentages, rather than absolute numbers of measures. Data are from RTI International. Published in NEJM, 364: 198 -200, Jan 20, 2011 54
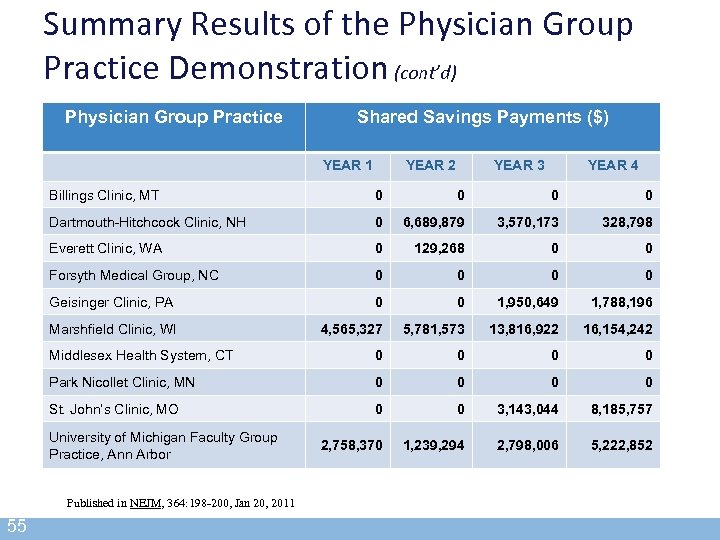 Summary Results of the Physician Group Practice Demonstration (cont’d) Physician Group Practice Shared Savings Payments ($) YEAR 1 YEAR 2 YEAR 3 YEAR 4 Billings Clinic, MT 0 0 Dartmouth-Hitchcock Clinic, NH 0 6, 689, 879 3, 570, 173 328, 798 Everett Clinic, WA 0 129, 268 0 0 Forsyth Medical Group, NC 0 0 Geisinger Clinic, PA 0 0 1, 950, 649 1, 788, 196 Marshfield Clinic, WI 4, 565, 327 5, 781, 573 13, 816, 922 16, 154, 242 Middlesex Health System, CT 0 0 Park Nicollet Clinic, MN 0 0 St. John’s Clinic, MO 0 0 3, 143, 044 8, 185, 757 2, 758, 370 1, 239, 294 2, 798, 006 5, 222, 852 University of Michigan Faculty Group Practice, Ann Arbor Published in NEJM, 364: 198 -200, Jan 20, 2011 55
Summary Results of the Physician Group Practice Demonstration (cont’d) Physician Group Practice Shared Savings Payments ($) YEAR 1 YEAR 2 YEAR 3 YEAR 4 Billings Clinic, MT 0 0 Dartmouth-Hitchcock Clinic, NH 0 6, 689, 879 3, 570, 173 328, 798 Everett Clinic, WA 0 129, 268 0 0 Forsyth Medical Group, NC 0 0 Geisinger Clinic, PA 0 0 1, 950, 649 1, 788, 196 Marshfield Clinic, WI 4, 565, 327 5, 781, 573 13, 816, 922 16, 154, 242 Middlesex Health System, CT 0 0 Park Nicollet Clinic, MN 0 0 St. John’s Clinic, MO 0 0 3, 143, 044 8, 185, 757 2, 758, 370 1, 239, 294 2, 798, 006 5, 222, 852 University of Michigan Faculty Group Practice, Ann Arbor Published in NEJM, 364: 198 -200, Jan 20, 2011 55
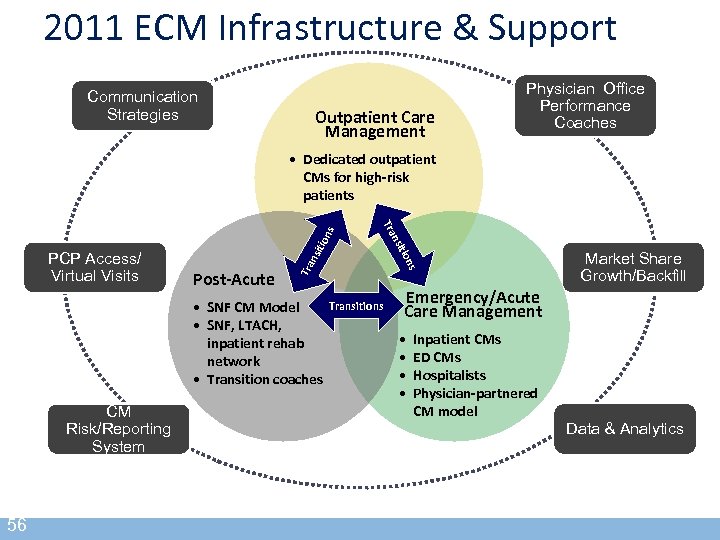 2011 ECM Infrastructure & Support Communication Strategies Outpatient Care Management Physician Office Performance Coaches CM Risk/Reporting System 56 tio Tra nsi ns • SNF CM Model • SNF, LTACH, inpatient rehab network • Transition coaches tio Post-Acute nsi PCP Access/ Virtual Visits Tra ns • Dedicated outpatient CMs for high-risk patients Transitions Market Share Growth/Backfill Emergency/Acute Care Management • • Inpatient CMs ED CMs Hospitalists Physician-partnered CM model Data & Analytics
2011 ECM Infrastructure & Support Communication Strategies Outpatient Care Management Physician Office Performance Coaches CM Risk/Reporting System 56 tio Tra nsi ns • SNF CM Model • SNF, LTACH, inpatient rehab network • Transition coaches tio Post-Acute nsi PCP Access/ Virtual Visits Tra ns • Dedicated outpatient CMs for high-risk patients Transitions Market Share Growth/Backfill Emergency/Acute Care Management • • Inpatient CMs ED CMs Hospitalists Physician-partnered CM model Data & Analytics
 Federal ACO Requirements § “Become Accountable for Quality, Cost, Overall Care” of FFS Beneficiaries § At Least 3 Yr Contract § Formal Legal Structure to Receive/Distribute Shared Savings § Enough Primary Care for Assigned Beneficiaries (At Least 5000) 57
Federal ACO Requirements § “Become Accountable for Quality, Cost, Overall Care” of FFS Beneficiaries § At Least 3 Yr Contract § Formal Legal Structure to Receive/Distribute Shared Savings § Enough Primary Care for Assigned Beneficiaries (At Least 5000) 57
 Federal ACO Requirements § Report Key Data to HHS: Assignment, Quality, Etc. § Leadership and Management Structure § Processes to Promote EBM, Patient Engagement, Quality, Cost, Care Coordination § Meet Patient-Centered Criteria 58
Federal ACO Requirements § Report Key Data to HHS: Assignment, Quality, Etc. § Leadership and Management Structure § Processes to Promote EBM, Patient Engagement, Quality, Cost, Care Coordination § Meet Patient-Centered Criteria 58
 Summary of Key Points § Culture Evolves Over Time and Takes Effort § Physician Engagement Requires Physician Involvement § Technology Plays Important Role § Evidence-based Management is Key § The Need for Change – Preparing for the Future 59
Summary of Key Points § Culture Evolves Over Time and Takes Effort § Physician Engagement Requires Physician Involvement § Technology Plays Important Role § Evidence-based Management is Key § The Need for Change – Preparing for the Future 59
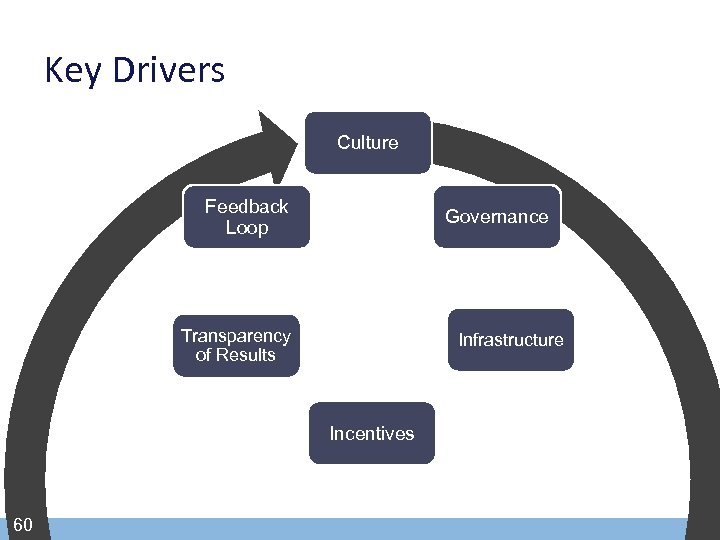 Key Drivers Culture Feedback Loop Governance Transparency of Results Infrastructure Incentives 60
Key Drivers Culture Feedback Loop Governance Transparency of Results Infrastructure Incentives 60
 Speaker § Mark Shields, MD, MBA, FACP Vice President, Advocate Health Care Senior Medical Director, Advocate Physician Partners mark. shields@advocatehealth. com 61
Speaker § Mark Shields, MD, MBA, FACP Vice President, Advocate Health Care Senior Medical Director, Advocate Physician Partners mark. shields@advocatehealth. com 61


