4bbd15609e1bdd726892685d8b96f978.ppt
- Количество слайдов: 68
 AIDS and related syndrome
AIDS and related syndrome
 Clinical manifestation and staging of HIV infection n n Acute HIV infection or primary HIV infection Asymptomatic stage or clinical latency Early symptomatic stage or AIDSrelated complex (ARC) Advanced HIV disease or AIDS
Clinical manifestation and staging of HIV infection n n Acute HIV infection or primary HIV infection Asymptomatic stage or clinical latency Early symptomatic stage or AIDSrelated complex (ARC) Advanced HIV disease or AIDS
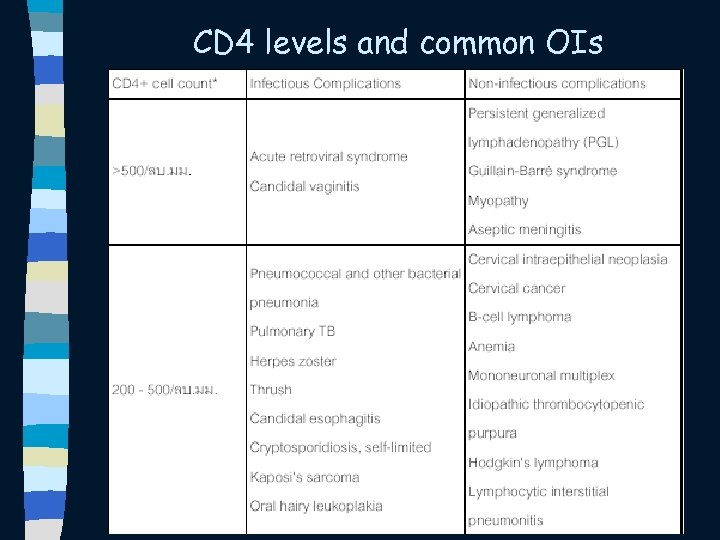 CD 4 levels and common OIs
CD 4 levels and common OIs
 CD 4 levels and common OIs
CD 4 levels and common OIs
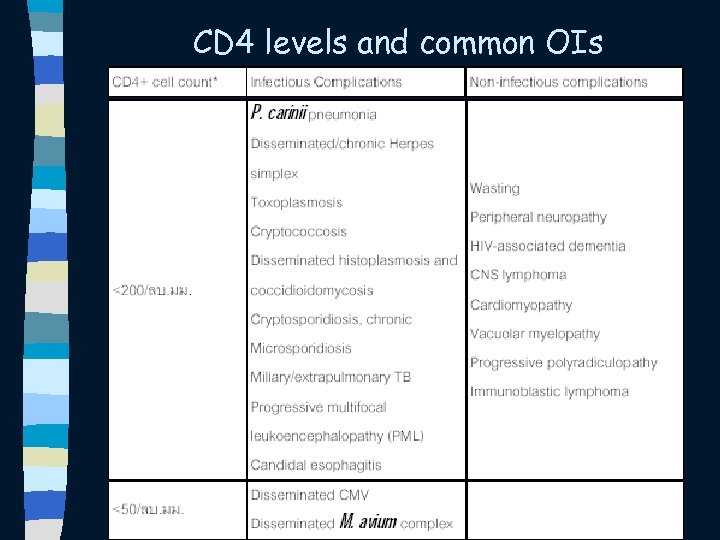
 Natural Course of HIV Infection and Common Complications 1000 VL CD 4+ cell Count 900 CD 4+ T cells 800 Relative level of Plasma HIV-RNA 700 TB 600 500 400 300 Acute HIV infection syndrome HZV Asymptomatic OHL 200 PPE OC PCP 100 0 TB CMV, MAC 0 1 2 3 4 5 Months 1 2 3 4 5 6 Years After HIV Infection 7 8 9 CM 10 11
Natural Course of HIV Infection and Common Complications 1000 VL CD 4+ cell Count 900 CD 4+ T cells 800 Relative level of Plasma HIV-RNA 700 TB 600 500 400 300 Acute HIV infection syndrome HZV Asymptomatic OHL 200 PPE OC PCP 100 0 TB CMV, MAC 0 1 2 3 4 5 Months 1 2 3 4 5 6 Years After HIV Infection 7 8 9 CM 10 11
 Advanced HIV disease or AIDS n n CD 4+ T cell < 200 cells/mm 3 Common AIDS-defining illness in HIV – infected Thai adults – Candidiasis – – – Cryptococcosis Penicillosis marneffei Histoplasmosis Cytomegalovirus Mycobacterium avium complex Toxoplasmosis
Advanced HIV disease or AIDS n n CD 4+ T cell < 200 cells/mm 3 Common AIDS-defining illness in HIV – infected Thai adults – Candidiasis – – – Cryptococcosis Penicillosis marneffei Histoplasmosis Cytomegalovirus Mycobacterium avium complex Toxoplasmosis
 Candidiasis n n Candida infection in AIDS is almost exclusively mucosal Oropharyngeal candidiasis occurs in 74% of HIV-infected patients 1/3 is recurrent and more severe as immunodeficiency advances Esophageal involvement is reported in 20 to 40% of all AIDS patients
Candidiasis n n Candida infection in AIDS is almost exclusively mucosal Oropharyngeal candidiasis occurs in 74% of HIV-infected patients 1/3 is recurrent and more severe as immunodeficiency advances Esophageal involvement is reported in 20 to 40% of all AIDS patients
 Clinical features of oral candidiasis n n Most patients are symptomatic and may complain of some oral discomfort 4 forms of oral lesions: pseudomembranous, erythematous (or atrophic), hypertrophic, and angular cheilitis
Clinical features of oral candidiasis n n Most patients are symptomatic and may complain of some oral discomfort 4 forms of oral lesions: pseudomembranous, erythematous (or atrophic), hypertrophic, and angular cheilitis
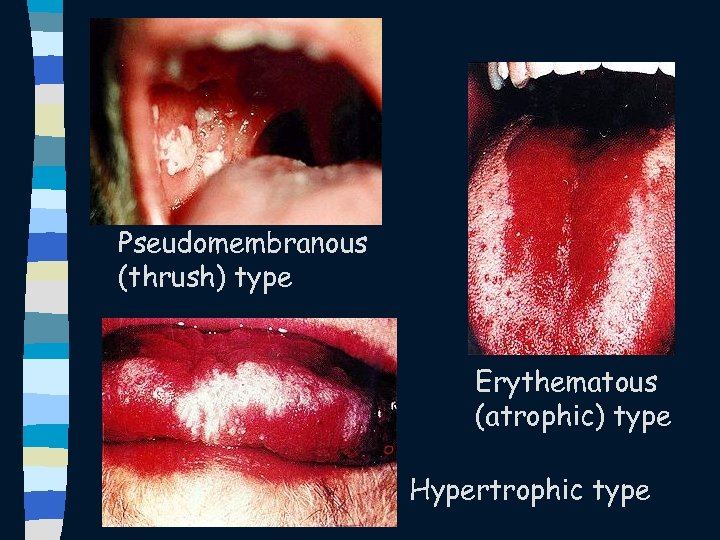 Pseudomembranous (thrush) type Erythematous (atrophic) type Hypertrophic type
Pseudomembranous (thrush) type Erythematous (atrophic) type Hypertrophic type
 Clinical features of vaginal candidiasis n n Most patients present with vaginal itching, burning or pain and vaginal discharge Examination of the vaginal cavity reveals thrush, identical to that seen in the oropharynx
Clinical features of vaginal candidiasis n n Most patients present with vaginal itching, burning or pain and vaginal discharge Examination of the vaginal cavity reveals thrush, identical to that seen in the oropharynx
 Clinical features of esophageal candidiasis n n n Typical symptom: dysphagia or odynophagia Esophageal lesions: pseudomembranes, erosions, and ulcers Combination of oral candidiasis and esophageal symptoms is both specific and sensitive in predicting esophageal involvement
Clinical features of esophageal candidiasis n n n Typical symptom: dysphagia or odynophagia Esophageal lesions: pseudomembranes, erosions, and ulcers Combination of oral candidiasis and esophageal symptoms is both specific and sensitive in predicting esophageal involvement
 Clinical features of esophageal candidiasis n n Patients who present in this manner can be treated empirically with antifungal therapy Endoscopy is reserved in those patients who fail to respond or to evaluate for the presence of other diagnoses: HSV or CMV esophagitis, idiopathic ulceration
Clinical features of esophageal candidiasis n n Patients who present in this manner can be treated empirically with antifungal therapy Endoscopy is reserved in those patients who fail to respond or to evaluate for the presence of other diagnoses: HSV or CMV esophagitis, idiopathic ulceration
 Diagnosis of candidiasis n n Fungal cultures are rarely required for diagnosis and can cause confusion, since many patients are colonized with Candida Scraping of a lesion will show characteristic spherical budding yeasts and pseudohyphae (KOH preparation or gram stain)
Diagnosis of candidiasis n n Fungal cultures are rarely required for diagnosis and can cause confusion, since many patients are colonized with Candida Scraping of a lesion will show characteristic spherical budding yeasts and pseudohyphae (KOH preparation or gram stain)
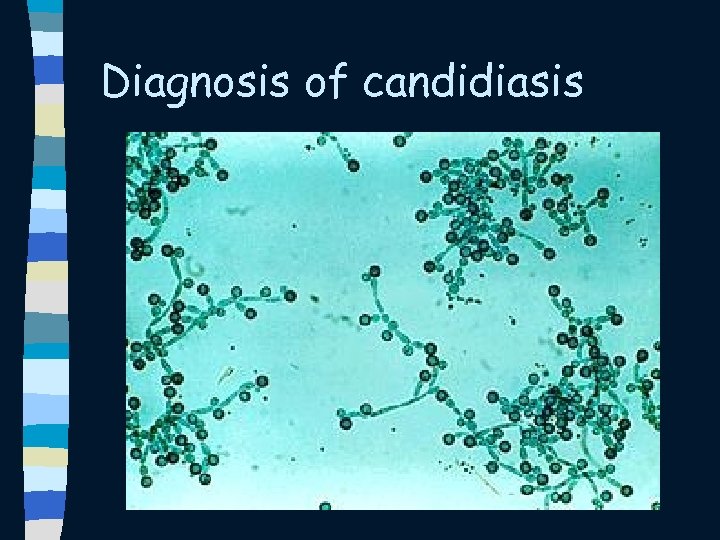 Diagnosis of candidiasis
Diagnosis of candidiasis
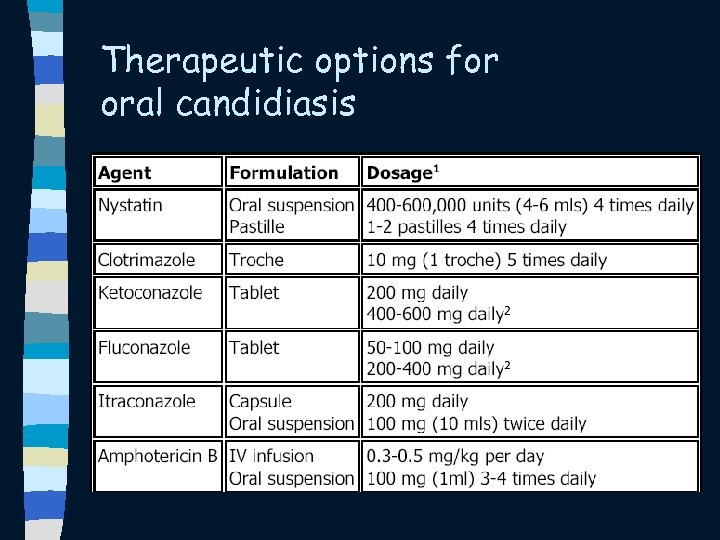 Therapeutic options for oral candidiasis
Therapeutic options for oral candidiasis
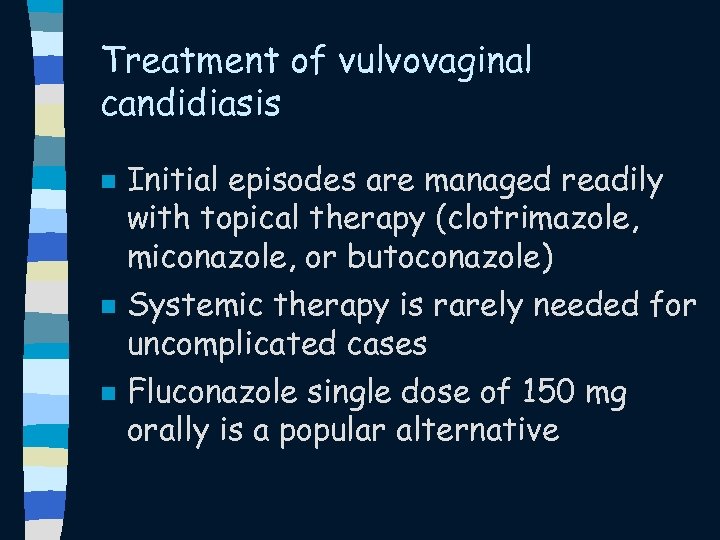 Treatment of vulvovaginal candidiasis n n n Initial episodes are managed readily with topical therapy (clotrimazole, miconazole, or butoconazole) Systemic therapy is rarely needed for uncomplicated cases Fluconazole single dose of 150 mg orally is a popular alternative
Treatment of vulvovaginal candidiasis n n n Initial episodes are managed readily with topical therapy (clotrimazole, miconazole, or butoconazole) Systemic therapy is rarely needed for uncomplicated cases Fluconazole single dose of 150 mg orally is a popular alternative
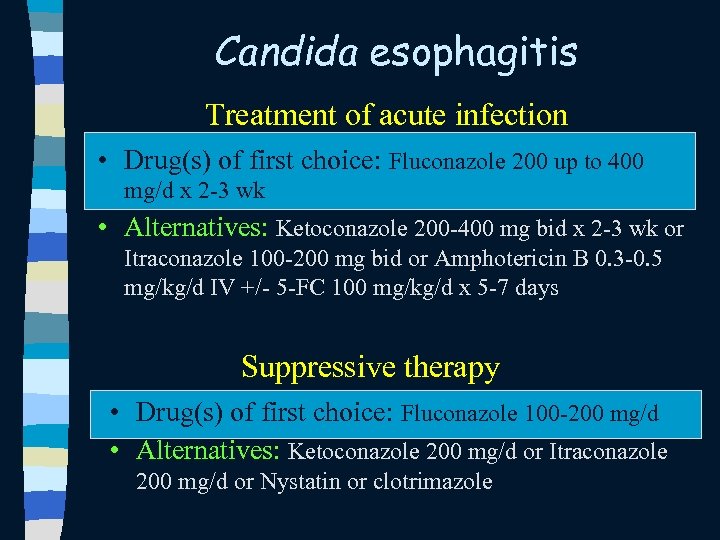 Candida esophagitis Treatment of acute infection • Drug(s) of first choice: Fluconazole 200 up to 400 mg/d x 2 -3 wk • Alternatives: Ketoconazole 200 -400 mg bid x 2 -3 wk or Itraconazole 100 -200 mg bid or Amphotericin B 0. 3 -0. 5 mg/kg/d IV +/- 5 -FC 100 mg/kg/d x 5 -7 days Suppressive therapy • Drug(s) of first choice: Fluconazole 100 -200 mg/d • Alternatives: Ketoconazole 200 mg/d or Itraconazole 200 mg/d or Nystatin or clotrimazole
Candida esophagitis Treatment of acute infection • Drug(s) of first choice: Fluconazole 200 up to 400 mg/d x 2 -3 wk • Alternatives: Ketoconazole 200 -400 mg bid x 2 -3 wk or Itraconazole 100 -200 mg bid or Amphotericin B 0. 3 -0. 5 mg/kg/d IV +/- 5 -FC 100 mg/kg/d x 5 -7 days Suppressive therapy • Drug(s) of first choice: Fluconazole 100 -200 mg/d • Alternatives: Ketoconazole 200 mg/d or Itraconazole 200 mg/d or Nystatin or clotrimazole
 Cryptococcosis : Cryptococcal meningitis n n n Virtually all HIV-associated infection is caused by C. neoformans var. neoformans (serotypes A and D) Most cases are seen in patients with CD 4 <50 cells/mm 3 acute primary infection or reactivation of previously dormant disease
Cryptococcosis : Cryptococcal meningitis n n n Virtually all HIV-associated infection is caused by C. neoformans var. neoformans (serotypes A and D) Most cases are seen in patients with CD 4 <50 cells/mm 3 acute primary infection or reactivation of previously dormant disease
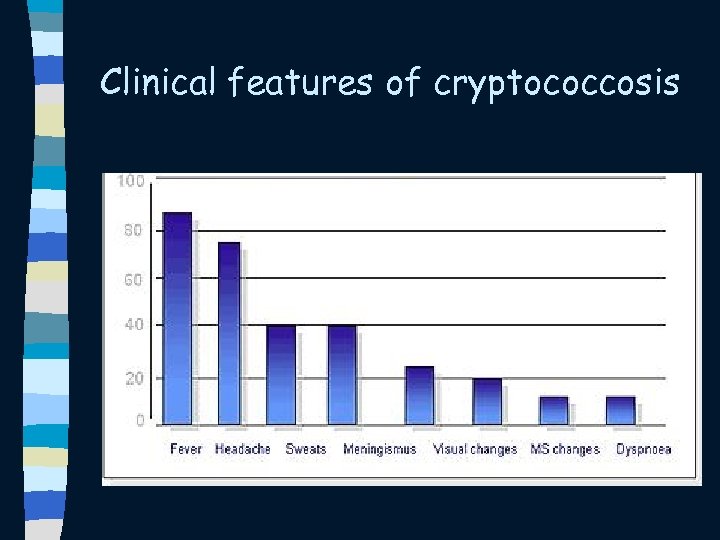 Clinical features of cryptococcosis
Clinical features of cryptococcosis
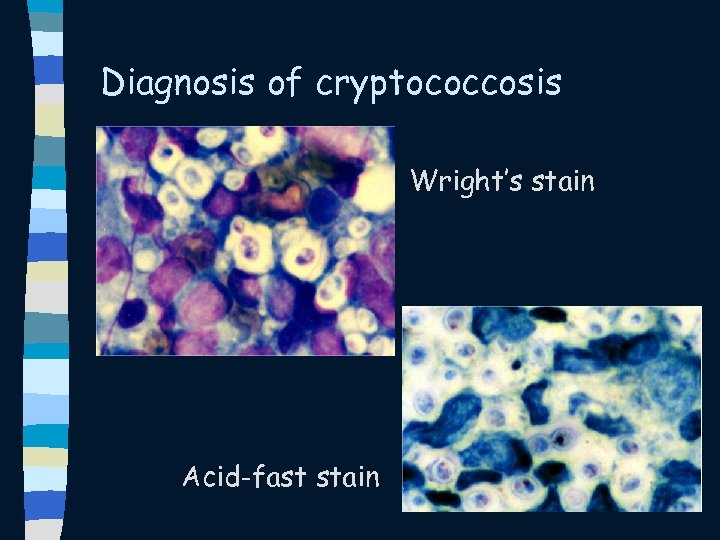 Diagnosis of cryptococcosis Wright’s stain Acid-fast stain
Diagnosis of cryptococcosis Wright’s stain Acid-fast stain
 Diagnosis of cryptococcosis n n n CSF: mildly elevated protein, normal or slightly low glucose, a few lymphocytes, and numerous organisms Cryptococcal antigen is almost invariably detectable in the CSF at high titer Opening pressure is elevated in up to 25%: important prognostic and therapeutic implications
Diagnosis of cryptococcosis n n n CSF: mildly elevated protein, normal or slightly low glucose, a few lymphocytes, and numerous organisms Cryptococcal antigen is almost invariably detectable in the CSF at high titer Opening pressure is elevated in up to 25%: important prognostic and therapeutic implications
 Diagnosis of cryptococcosis n n CSF culture positive India ink positive
Diagnosis of cryptococcosis n n CSF culture positive India ink positive
 Diagnosis of cryptococcosis n n Cryptococcal antigen in the serum is highly sensitive and specific for C. neoformans infection Positive serum cryptococcal antigen titer >1: 8 is regarded as presumptive evidence of cryptococcal infection and warrants antifungal therapy, even if infection is not subsequently documented
Diagnosis of cryptococcosis n n Cryptococcal antigen in the serum is highly sensitive and specific for C. neoformans infection Positive serum cryptococcal antigen titer >1: 8 is regarded as presumptive evidence of cryptococcal infection and warrants antifungal therapy, even if infection is not subsequently documented
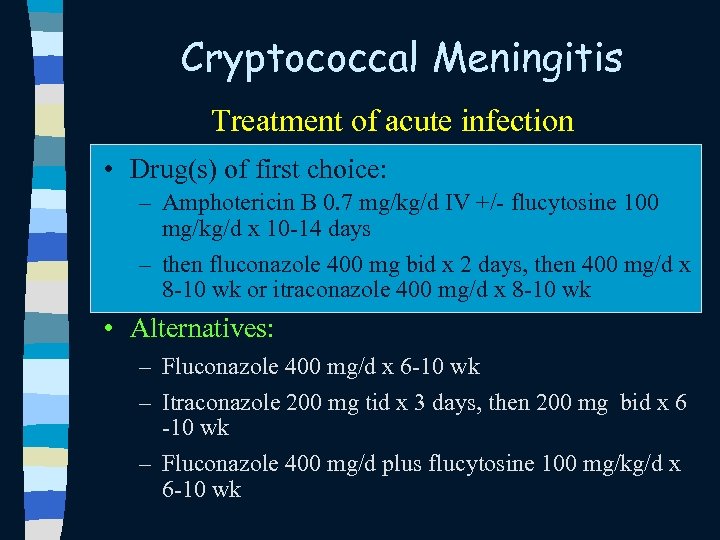 Cryptococcal Meningitis Treatment of acute infection • Drug(s) of first choice: – Amphotericin B 0. 7 mg/kg/d IV +/- flucytosine 100 mg/kg/d x 10 -14 days – then fluconazole 400 mg bid x 2 days, then 400 mg/d x 8 -10 wk or itraconazole 400 mg/d x 8 -10 wk • Alternatives: – Fluconazole 400 mg/d x 6 -10 wk – Itraconazole 200 mg tid x 3 days, then 200 mg bid x 6 -10 wk – Fluconazole 400 mg/d plus flucytosine 100 mg/kg/d x 6 -10 wk
Cryptococcal Meningitis Treatment of acute infection • Drug(s) of first choice: – Amphotericin B 0. 7 mg/kg/d IV +/- flucytosine 100 mg/kg/d x 10 -14 days – then fluconazole 400 mg bid x 2 days, then 400 mg/d x 8 -10 wk or itraconazole 400 mg/d x 8 -10 wk • Alternatives: – Fluconazole 400 mg/d x 6 -10 wk – Itraconazole 200 mg tid x 3 days, then 200 mg bid x 6 -10 wk – Fluconazole 400 mg/d plus flucytosine 100 mg/kg/d x 6 -10 wk
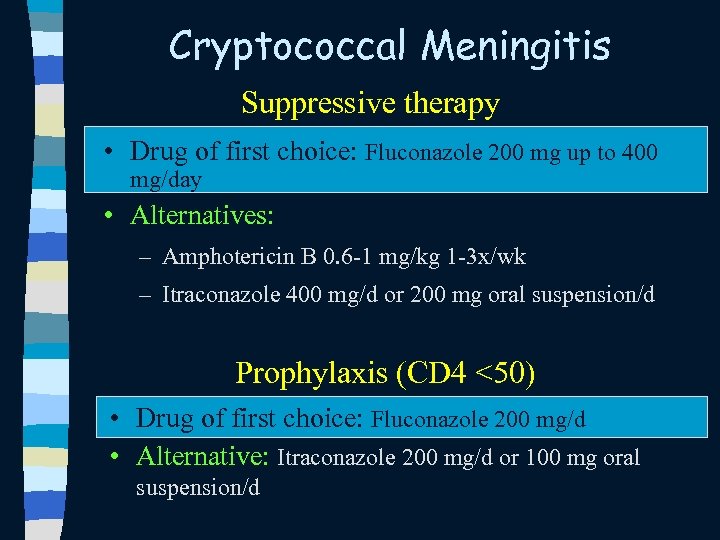 Cryptococcal Meningitis Suppressive therapy • Drug of first choice: Fluconazole 200 mg up to 400 mg/day • Alternatives: – Amphotericin B 0. 6 -1 mg/kg 1 -3 x/wk – Itraconazole 400 mg/d or 200 mg oral suspension/d Prophylaxis (CD 4 <50) • Drug of first choice: Fluconazole 200 mg/d • Alternative: Itraconazole 200 mg/d or 100 mg oral suspension/d
Cryptococcal Meningitis Suppressive therapy • Drug of first choice: Fluconazole 200 mg up to 400 mg/day • Alternatives: – Amphotericin B 0. 6 -1 mg/kg 1 -3 x/wk – Itraconazole 400 mg/d or 200 mg oral suspension/d Prophylaxis (CD 4 <50) • Drug of first choice: Fluconazole 200 mg/d • Alternative: Itraconazole 200 mg/d or 100 mg oral suspension/d
 การปองกน cryptococcosis ในประเทศไทย n ขอบงช – CD 4 <100/mm 3 – เคยเปน cryptococcosis มากอน ยาทใช Fluconazole 400 mg weekly n ผปวยทไดยาตาน ไวรส และม CD 4 > 100 -200/mm 3อยางนอย 6 เดอน สามารถหยดยาปองกนได n
การปองกน cryptococcosis ในประเทศไทย n ขอบงช – CD 4 <100/mm 3 – เคยเปน cryptococcosis มากอน ยาทใช Fluconazole 400 mg weekly n ผปวยทไดยาตาน ไวรส และม CD 4 > 100 -200/mm 3อยางนอย 6 เดอน สามารถหยดยาปองกนได n
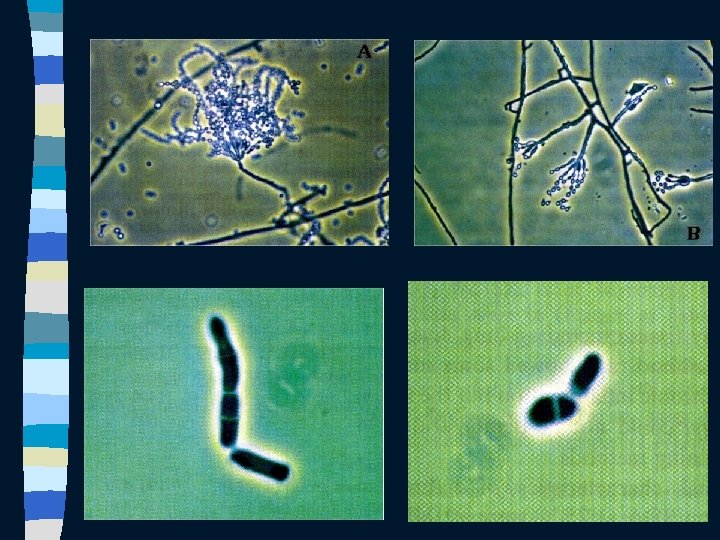
 Penicilliosis marneffei n n CD 4 +T cell < 100 cells/mm 3 Penicillium marneffei, a dimorphic fungus Endemic in Southeast Asia (especially Northern Thailand Southern China) Potential cause of infection in patients in endemic areas or with a history of travel to endemic areas
Penicilliosis marneffei n n CD 4 +T cell < 100 cells/mm 3 Penicillium marneffei, a dimorphic fungus Endemic in Southeast Asia (especially Northern Thailand Southern China) Potential cause of infection in patients in endemic areas or with a history of travel to endemic areas
 Clinical features of 74 hiv-infected patients with disseminated P. marneffei infection Source: Sirisanthana T, et al. Clin Infect Dis. 1998; 26: 1107 -10
Clinical features of 74 hiv-infected patients with disseminated P. marneffei infection Source: Sirisanthana T, et al. Clin Infect Dis. 1998; 26: 1107 -10
 Penicilliosis marneffei
Penicilliosis marneffei
 Penicilliosis marneffei
Penicilliosis marneffei
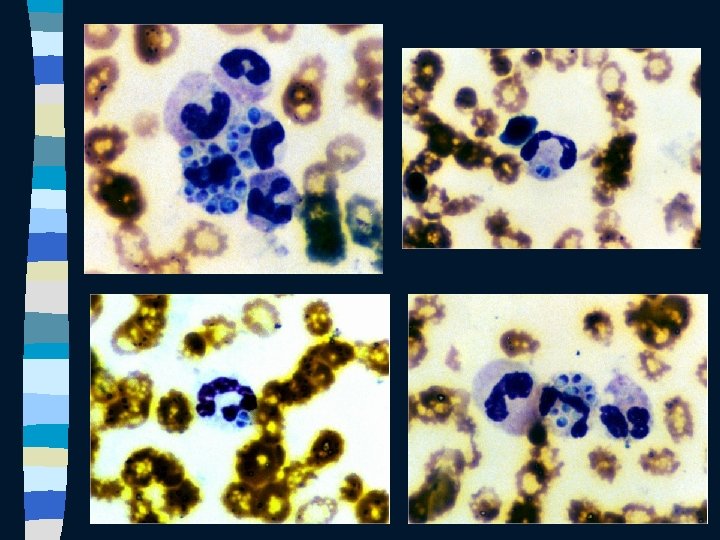
 Diagnosis of penicilliosis marneffei n n n Wright stain : smear from skin lesion, node biopsy, marrow biopsy : 2*3 -6 um yeast Culture from skin, bone marrow, LN Hemoculture
Diagnosis of penicilliosis marneffei n n n Wright stain : smear from skin lesion, node biopsy, marrow biopsy : 2*3 -6 um yeast Culture from skin, bone marrow, LN Hemoculture
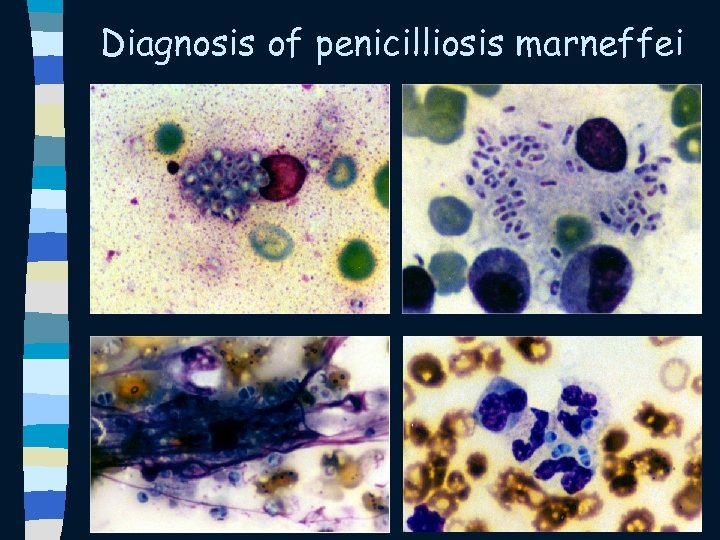 Diagnosis of penicilliosis marneffei
Diagnosis of penicilliosis marneffei
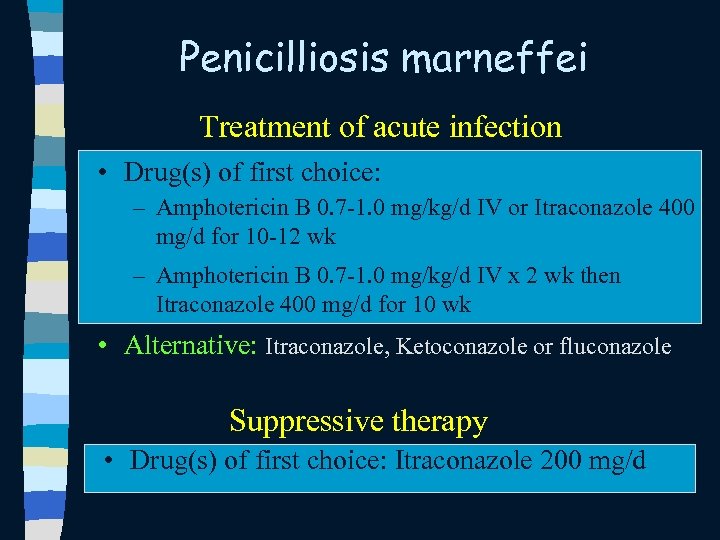 Penicilliosis marneffei Treatment of acute infection • Drug(s) of first choice: – Amphotericin B 0. 7 -1. 0 mg/kg/d IV or Itraconazole 400 mg/d for 10 -12 wk – Amphotericin B 0. 7 -1. 0 mg/kg/d IV x 2 wk then Itraconazole 400 mg/d for 10 wk • Alternative: Itraconazole, Ketoconazole or fluconazole Suppressive therapy • Drug(s) of first choice: Itraconazole 200 mg/d
Penicilliosis marneffei Treatment of acute infection • Drug(s) of first choice: – Amphotericin B 0. 7 -1. 0 mg/kg/d IV or Itraconazole 400 mg/d for 10 -12 wk – Amphotericin B 0. 7 -1. 0 mg/kg/d IV x 2 wk then Itraconazole 400 mg/d for 10 wk • Alternative: Itraconazole, Ketoconazole or fluconazole Suppressive therapy • Drug(s) of first choice: Itraconazole 200 mg/d
 Histoplasmosis n n n Histoplasma capsulatum, a dimorphic fungus Endemic in the Mississippi and Ohio river valleys of North America, certain areas of Central and South America, and the Caribbean Mycelial form is found in the soil; particularly soil associated with bird roosts, and caves
Histoplasmosis n n n Histoplasma capsulatum, a dimorphic fungus Endemic in the Mississippi and Ohio river valleys of North America, certain areas of Central and South America, and the Caribbean Mycelial form is found in the soil; particularly soil associated with bird roosts, and caves
 Clinical features of histoplasmosis n n most common: fever and weight loss, ~ 75% of patients Respiratory complaints, abdominal pain or gastrointestinal bleeding 5 -10% have an acute septic shock-like syndrome, very poor prognosis Skin lesions: uncommon, molluscum contagiosum-like
Clinical features of histoplasmosis n n most common: fever and weight loss, ~ 75% of patients Respiratory complaints, abdominal pain or gastrointestinal bleeding 5 -10% have an acute septic shock-like syndrome, very poor prognosis Skin lesions: uncommon, molluscum contagiosum-like
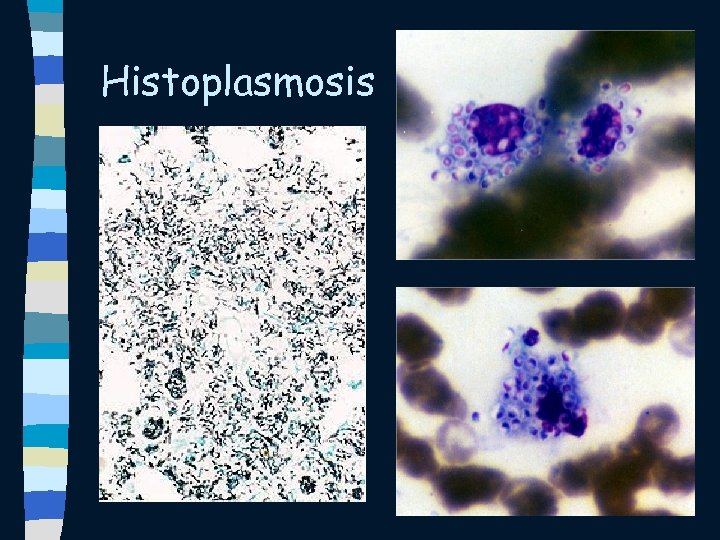 Histoplasmosis
Histoplasmosis
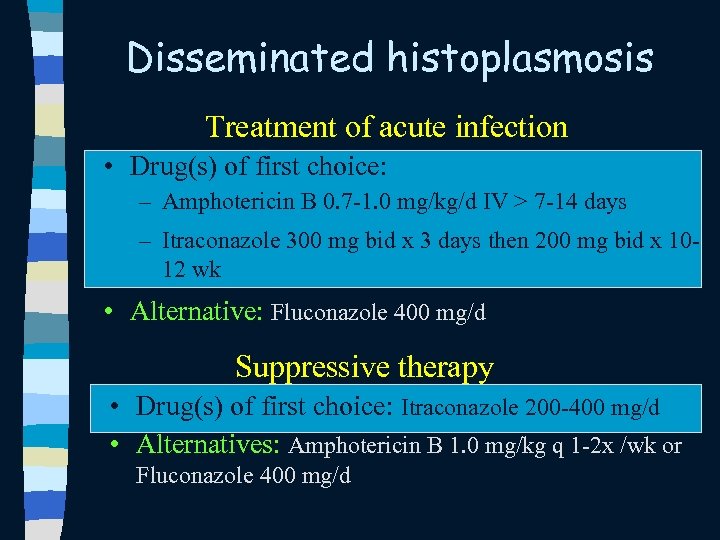 Disseminated histoplasmosis Treatment of acute infection • Drug(s) of first choice: – Amphotericin B 0. 7 -1. 0 mg/kg/d IV > 7 -14 days – Itraconazole 300 mg bid x 3 days then 200 mg bid x 1012 wk • Alternative: Fluconazole 400 mg/d Suppressive therapy • Drug(s) of first choice: Itraconazole 200 -400 mg/d • Alternatives: Amphotericin B 1. 0 mg/kg q 1 -2 x /wk or Fluconazole 400 mg/d
Disseminated histoplasmosis Treatment of acute infection • Drug(s) of first choice: – Amphotericin B 0. 7 -1. 0 mg/kg/d IV > 7 -14 days – Itraconazole 300 mg bid x 3 days then 200 mg bid x 1012 wk • Alternative: Fluconazole 400 mg/d Suppressive therapy • Drug(s) of first choice: Itraconazole 200 -400 mg/d • Alternatives: Amphotericin B 1. 0 mg/kg q 1 -2 x /wk or Fluconazole 400 mg/d
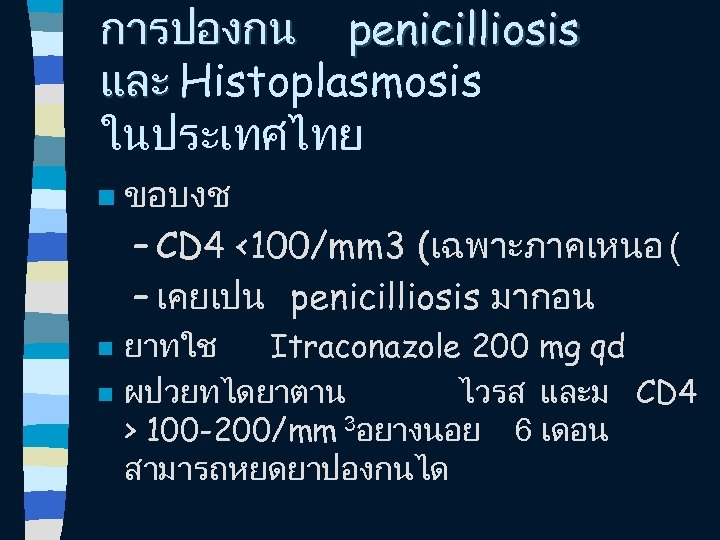 การปองกน penicilliosis และ Histoplasmosis ในประเทศไทย n n n ขอบงช – CD 4 <100/mm 3 (เฉพาะภาคเหนอ ( – เคยเปน penicilliosis มากอน ยาทใช Itraconazole 200 mg qd ผปวยทไดยาตาน ไวรส และม CD 4 > 100 -200/mm 3อยางนอย 6 เดอน สามารถหยดยาปองกนได
การปองกน penicilliosis และ Histoplasmosis ในประเทศไทย n n n ขอบงช – CD 4 <100/mm 3 (เฉพาะภาคเหนอ ( – เคยเปน penicilliosis มากอน ยาทใช Itraconazole 200 mg qd ผปวยทไดยาตาน ไวรส และม CD 4 > 100 -200/mm 3อยางนอย 6 เดอน สามารถหยดยาปองกนได
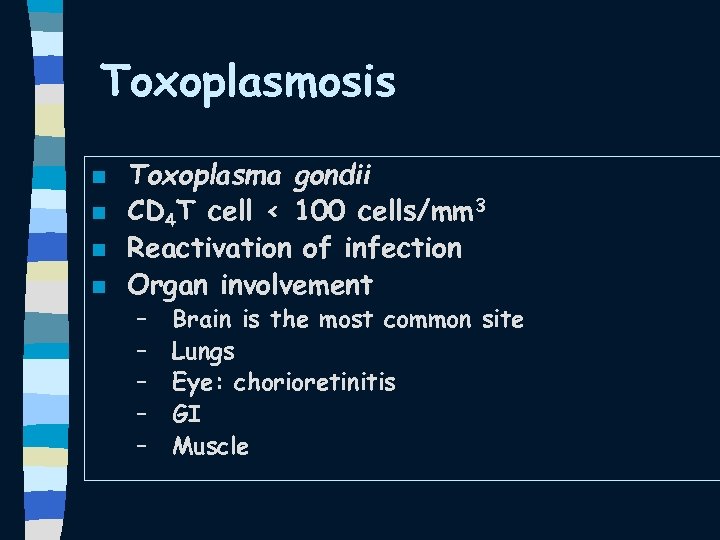 Toxoplasmosis n n Toxoplasma gondii CD 4 T cell < 100 cells/mm 3 Reactivation of infection Organ involvement – – – Brain is the most common site Lungs Eye: chorioretinitis GI Muscle
Toxoplasmosis n n Toxoplasma gondii CD 4 T cell < 100 cells/mm 3 Reactivation of infection Organ involvement – – – Brain is the most common site Lungs Eye: chorioretinitis GI Muscle
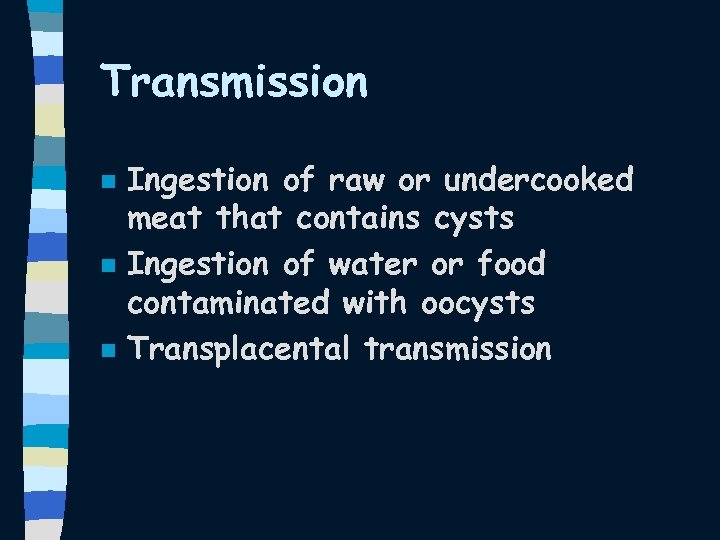 Transmission n Ingestion of raw or undercooked meat that contains cysts Ingestion of water or food contaminated with oocysts Transplacental transmission
Transmission n Ingestion of raw or undercooked meat that contains cysts Ingestion of water or food contaminated with oocysts Transplacental transmission
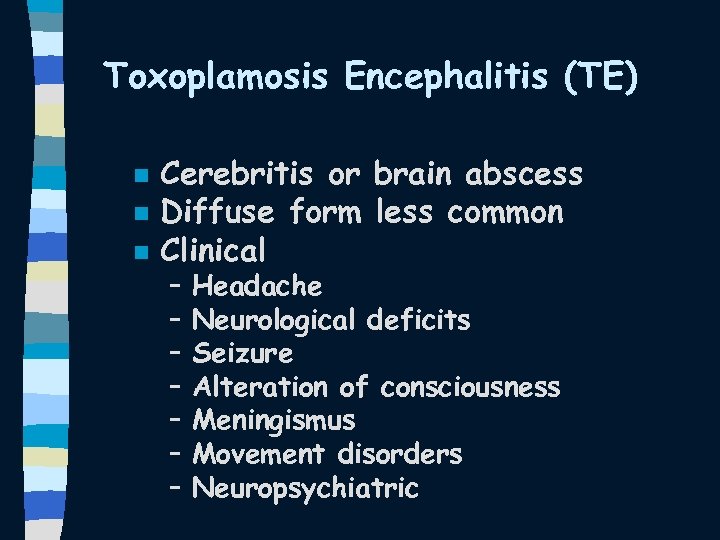 Toxoplamosis Encephalitis (TE) n n n Cerebritis or brain abscess Diffuse form less common Clinical – – – – Headache Neurological deficits Seizure Alteration of consciousness Meningismus Movement disorders Neuropsychiatric
Toxoplamosis Encephalitis (TE) n n n Cerebritis or brain abscess Diffuse form less common Clinical – – – – Headache Neurological deficits Seizure Alteration of consciousness Meningismus Movement disorders Neuropsychiatric
 Diagnosis of toxoplasmosis n n n Clinical CT brain scan or MRI Toxoplasma titer Response to treatment Brain biopsy
Diagnosis of toxoplasmosis n n n Clinical CT brain scan or MRI Toxoplasma titer Response to treatment Brain biopsy
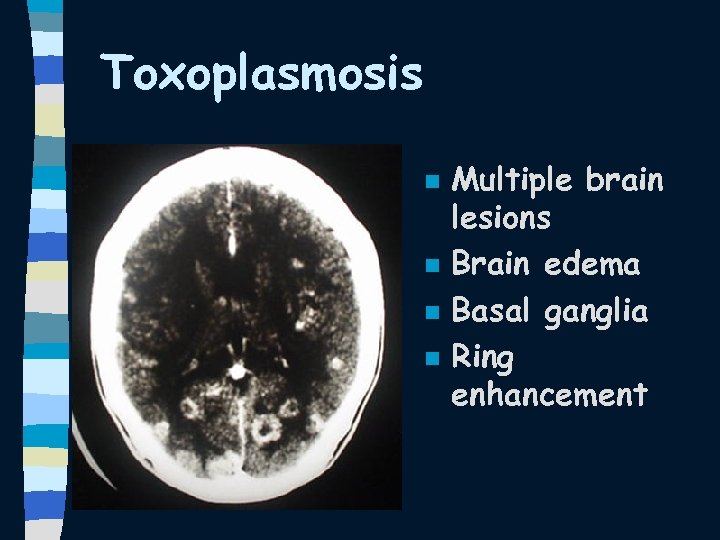 Toxoplasmosis n n Multiple brain lesions Brain edema Basal ganglia Ring enhancement
Toxoplasmosis n n Multiple brain lesions Brain edema Basal ganglia Ring enhancement
 CSF findings in TE n nonspecific mild mononuclear pleocytosis and mild to moderate elevations in CSF protein
CSF findings in TE n nonspecific mild mononuclear pleocytosis and mild to moderate elevations in CSF protein
 Toxoplasmosis Treatment n First choice Pyrimethamine 200 mg x 1 then 75 -100 mg /d + Sulfadiazine 1 -1. 5 g q 6 hr + Leukoverin 15 mg qd (if available) for -6 wks n Alternative Pyrimethamine + Leukoverin + Clindamycin 600 mg q 6 hr
Toxoplasmosis Treatment n First choice Pyrimethamine 200 mg x 1 then 75 -100 mg /d + Sulfadiazine 1 -1. 5 g q 6 hr + Leukoverin 15 mg qd (if available) for -6 wks n Alternative Pyrimethamine + Leukoverin + Clindamycin 600 mg q 6 hr
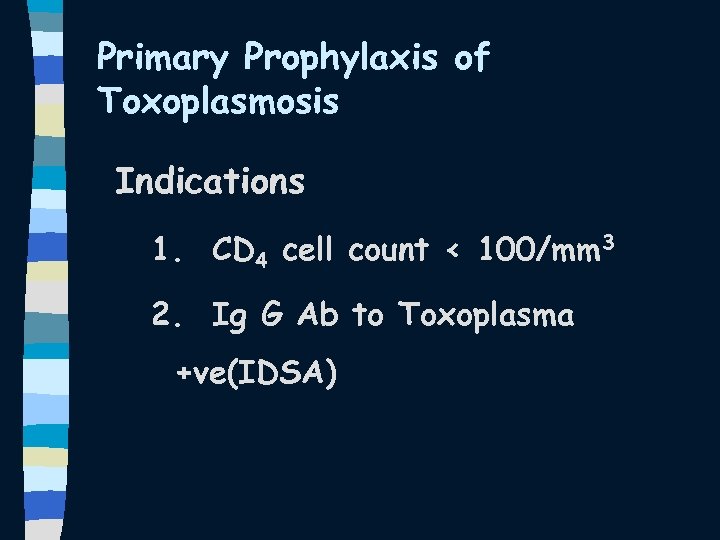 Primary Prophylaxis of Toxoplasmosis Indications 1. CD 4 cell count < 100/mm 3 2. Ig G Ab to Toxoplasma +ve(IDSA)
Primary Prophylaxis of Toxoplasmosis Indications 1. CD 4 cell count < 100/mm 3 2. Ig G Ab to Toxoplasma +ve(IDSA)
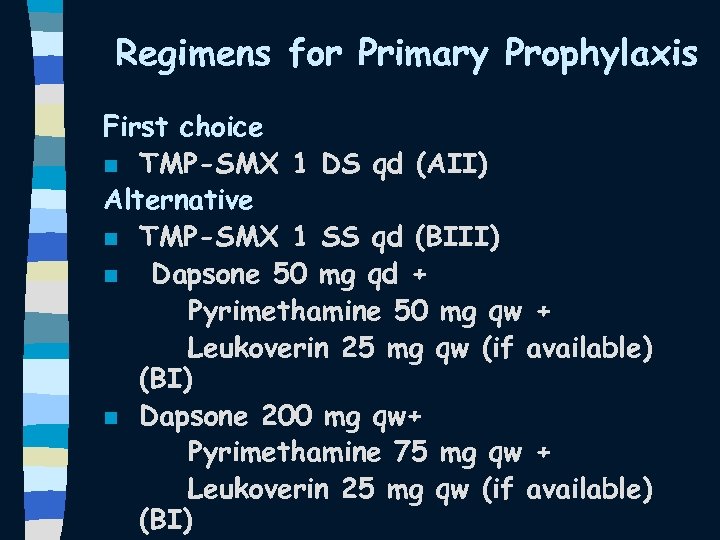 Regimens for Primary Prophylaxis First choice n TMP-SMX 1 DS qd (AII) Alternative n TMP-SMX 1 SS qd (BIII) n Dapsone 50 mg qd + Pyrimethamine 50 mg qw + Leukoverin 25 mg qw (if available) (BI) n Dapsone 200 mg qw+ Pyrimethamine 75 mg qw + Leukoverin 25 mg qw (if available) (BI)
Regimens for Primary Prophylaxis First choice n TMP-SMX 1 DS qd (AII) Alternative n TMP-SMX 1 SS qd (BIII) n Dapsone 50 mg qd + Pyrimethamine 50 mg qw + Leukoverin 25 mg qw (if available) (BI) n Dapsone 200 mg qw+ Pyrimethamine 75 mg qw + Leukoverin 25 mg qw (if available) (BI)
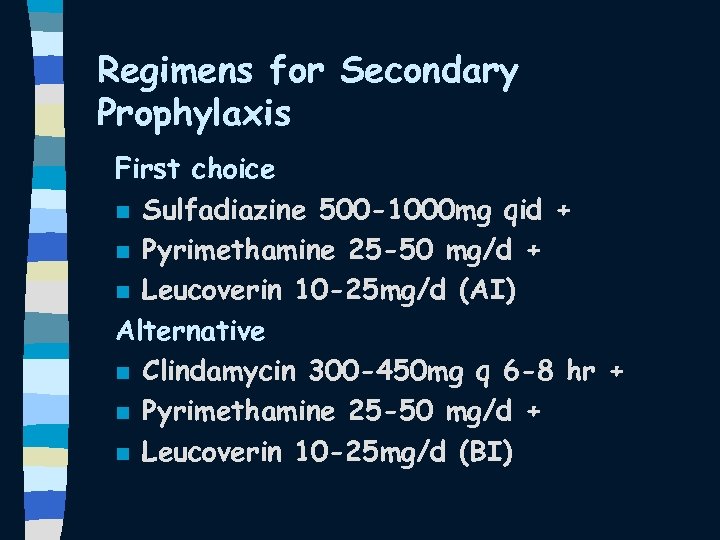 Regimens for Secondary Prophylaxis First choice n Sulfadiazine 500 -1000 mg qid + n Pyrimethamine 25 -50 mg/d + n Leucoverin 10 -25 mg/d (AI) Alternative n Clindamycin 300 -450 mg q 6 -8 hr + n Pyrimethamine 25 -50 mg/d + n Leucoverin 10 -25 mg/d (BI)
Regimens for Secondary Prophylaxis First choice n Sulfadiazine 500 -1000 mg qid + n Pyrimethamine 25 -50 mg/d + n Leucoverin 10 -25 mg/d (AI) Alternative n Clindamycin 300 -450 mg q 6 -8 hr + n Pyrimethamine 25 -50 mg/d + n Leucoverin 10 -25 mg/d (BI)
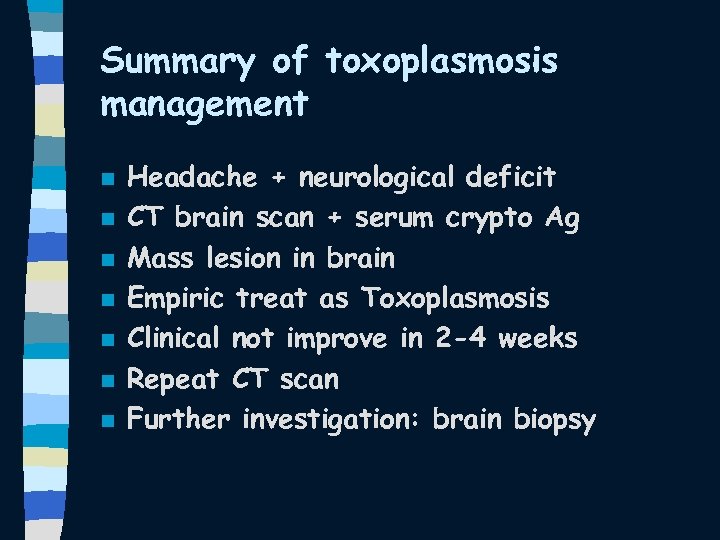 Summary of toxoplasmosis management n n n n Headache + neurological deficit CT brain scan + serum crypto Ag Mass lesion in brain Empiric treat as Toxoplasmosis Clinical not improve in 2 -4 weeks Repeat CT scan Further investigation: brain biopsy
Summary of toxoplasmosis management n n n n Headache + neurological deficit CT brain scan + serum crypto Ag Mass lesion in brain Empiric treat as Toxoplasmosis Clinical not improve in 2 -4 weeks Repeat CT scan Further investigation: brain biopsy
 Cytomegalovirus (CMV) • chorioretinitis • esophagitis • colitis • pneumonia • central nervous system disease
Cytomegalovirus (CMV) • chorioretinitis • esophagitis • colitis • pneumonia • central nervous system disease
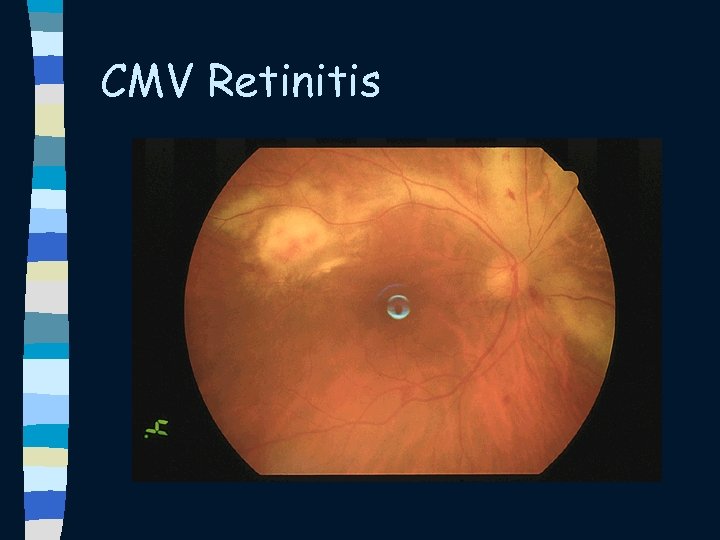
 Chorioretinitis n n n commonly occurs in patients with CD 4 < 50 cells/mm³ accounts for 80% to 90% of CMV disease in patients with AIDS common presenting symptoms include – decreased visual acuity – perception of floaters – visual field loss n Indirect ophthalmologic screening of patients with a CD 4 < 50 cells/mm³ can detect asymptomatic retinitis
Chorioretinitis n n n commonly occurs in patients with CD 4 < 50 cells/mm³ accounts for 80% to 90% of CMV disease in patients with AIDS common presenting symptoms include – decreased visual acuity – perception of floaters – visual field loss n Indirect ophthalmologic screening of patients with a CD 4 < 50 cells/mm³ can detect asymptomatic retinitis
 Chorioretinitis n n n Ophthalmologic exam. reveals large creamy to yellowish-white granular areas with perivascular exudates and hemorrhages these lesions may occur at either the periphery or center of the fundus. lesions generally progress within 2 to 3 weeks and can result in blindness retinitis often begins unilaterally, but progression to bilateral disease is common. systemic CMV disease involving other viscera may also be present
Chorioretinitis n n n Ophthalmologic exam. reveals large creamy to yellowish-white granular areas with perivascular exudates and hemorrhages these lesions may occur at either the periphery or center of the fundus. lesions generally progress within 2 to 3 weeks and can result in blindness retinitis often begins unilaterally, but progression to bilateral disease is common. systemic CMV disease involving other viscera may also be present
 Chorioretinitis n n n DDx: Toxo, Syphilis, HSV, VZV, and TB Patients with confirmed CMV chorioretinitis should begin treatment promptly A variety of agents have demonstrated efficacy in delaying time to progression of retinitis
Chorioretinitis n n n DDx: Toxo, Syphilis, HSV, VZV, and TB Patients with confirmed CMV chorioretinitis should begin treatment promptly A variety of agents have demonstrated efficacy in delaying time to progression of retinitis
 CMV Retinitis
CMV Retinitis
 CMV Retinitis • Systemic therapy • Local therapy Treatment n Ganciclovir n Foscarnet (phosphonoformic acid) n Cidofovir
CMV Retinitis • Systemic therapy • Local therapy Treatment n Ganciclovir n Foscarnet (phosphonoformic acid) n Cidofovir
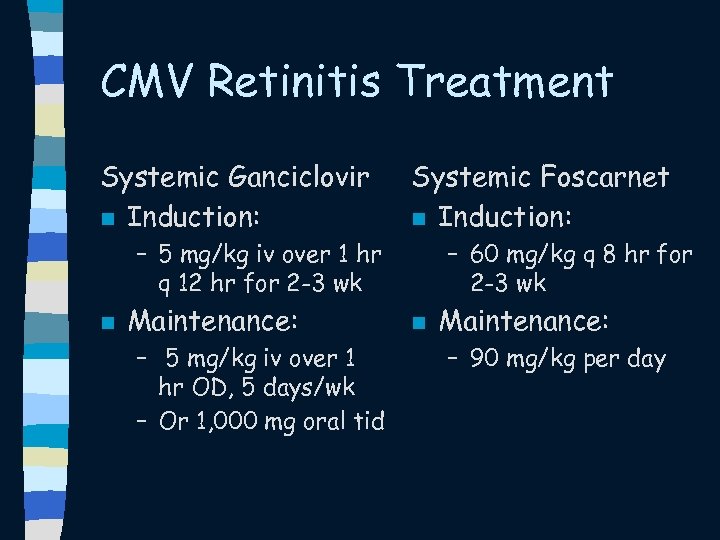 CMV Retinitis Treatment Systemic Ganciclovir n Induction: Systemic Foscarnet n Induction: – 5 mg/kg iv over 1 hr q 12 hr for 2 -3 wk n Maintenance: – 5 mg/kg iv over 1 hr OD, 5 days/wk – Or 1, 000 mg oral tid – 60 mg/kg q 8 hr for 2 -3 wk n Maintenance: – 90 mg/kg per day
CMV Retinitis Treatment Systemic Ganciclovir n Induction: Systemic Foscarnet n Induction: – 5 mg/kg iv over 1 hr q 12 hr for 2 -3 wk n Maintenance: – 5 mg/kg iv over 1 hr OD, 5 days/wk – Or 1, 000 mg oral tid – 60 mg/kg q 8 hr for 2 -3 wk n Maintenance: – 90 mg/kg per day
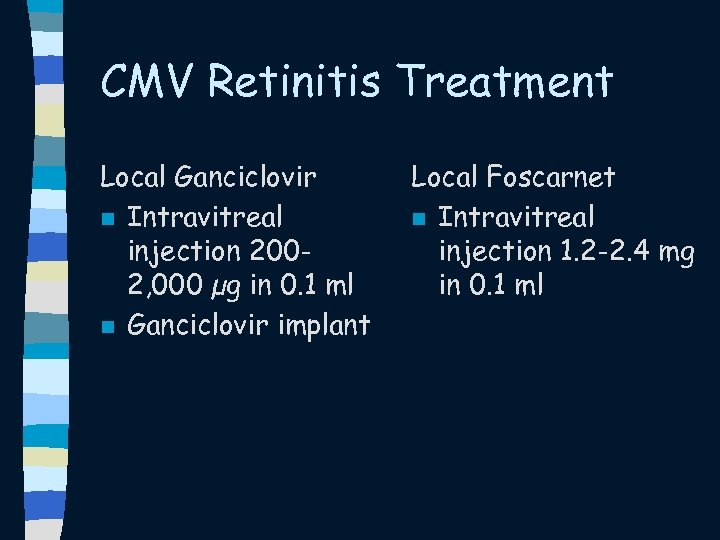 CMV Retinitis Treatment Local Ganciclovir n Intravitreal injection 2002, 000 µg in 0. 1 ml n Ganciclovir implant Local Foscarnet n Intravitreal injection 1. 2 -2. 4 mg in 0. 1 ml
CMV Retinitis Treatment Local Ganciclovir n Intravitreal injection 2002, 000 µg in 0. 1 ml n Ganciclovir implant Local Foscarnet n Intravitreal injection 1. 2 -2. 4 mg in 0. 1 ml
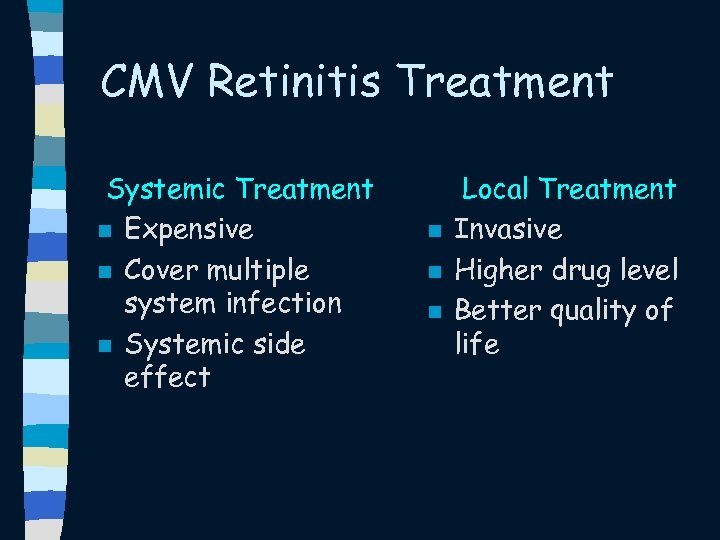 CMV Retinitis Treatment Systemic Treatment n Expensive n Cover multiple system infection n Systemic side effect n n n Local Treatment Invasive Higher drug level Better quality of life
CMV Retinitis Treatment Systemic Treatment n Expensive n Cover multiple system infection n Systemic side effect n n n Local Treatment Invasive Higher drug level Better quality of life
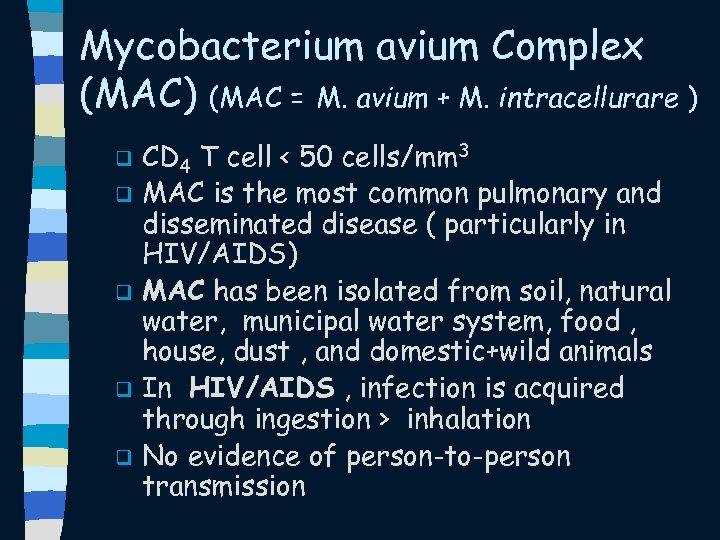 Mycobacterium avium Complex (MAC) (MAC = M. avium + M. intracellurare ) q q q CD 4 T cell < 50 cells/mm 3 MAC is the most common pulmonary and disseminated disease ( particularly in HIV/AIDS) MAC has been isolated from soil, natural water, municipal water system, food , house, dust , and domestic+wild animals In HIV/AIDS , infection is acquired through ingestion > inhalation No evidence of person-to-person transmission
Mycobacterium avium Complex (MAC) (MAC = M. avium + M. intracellurare ) q q q CD 4 T cell < 50 cells/mm 3 MAC is the most common pulmonary and disseminated disease ( particularly in HIV/AIDS) MAC has been isolated from soil, natural water, municipal water system, food , house, dust , and domestic+wild animals In HIV/AIDS , infection is acquired through ingestion > inhalation No evidence of person-to-person transmission
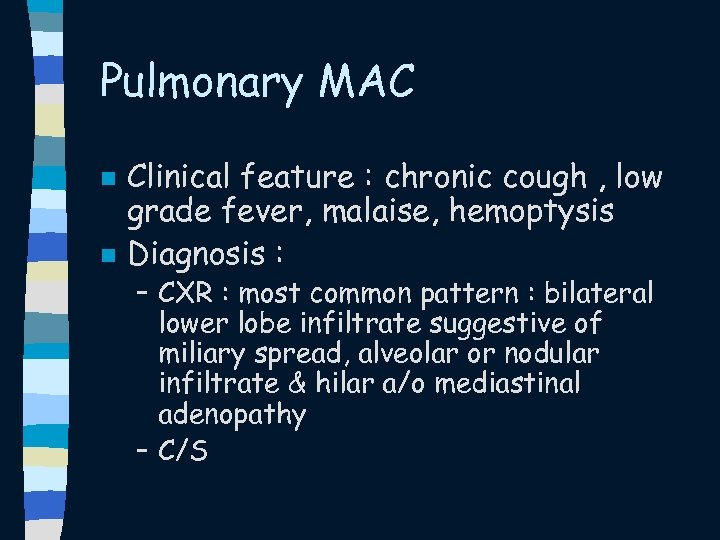 Pulmonary MAC n n Clinical feature : chronic cough , low grade fever, malaise, hemoptysis Diagnosis : – CXR : most common pattern : bilateral lower lobe infiltrate suggestive of miliary spread, alveolar or nodular infiltrate & hilar a/o mediastinal adenopathy – C/S
Pulmonary MAC n n Clinical feature : chronic cough , low grade fever, malaise, hemoptysis Diagnosis : – CXR : most common pattern : bilateral lower lobe infiltrate suggestive of miliary spread, alveolar or nodular infiltrate & hilar a/o mediastinal adenopathy – C/S
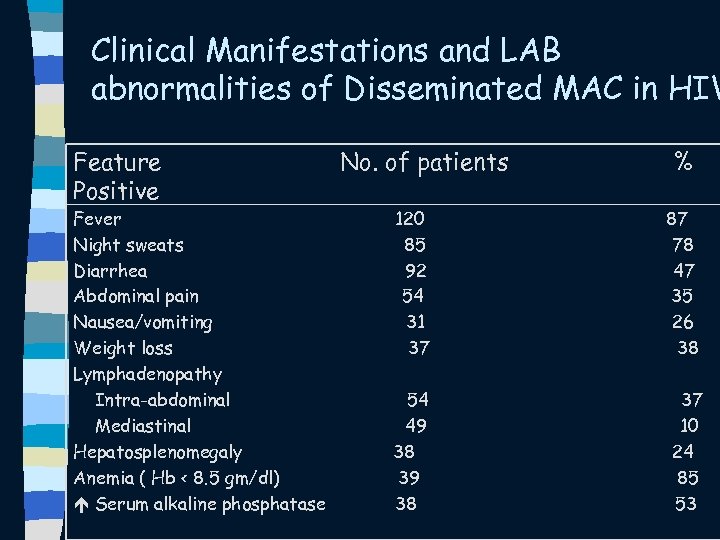 Clinical Manifestations and LAB abnormalities of Disseminated MAC in HIV Feature Positive Fever Night sweats Diarrhea Abdominal pain Nausea/vomiting Weight loss Lymphadenopathy Intra-abdominal Mediastinal Hepatosplenomegaly Anemia ( Hb < 8. 5 gm/dl) Serum alkaline phosphatase No. of patients % 120 85 92 54 31 37 87 78 47 35 26 38 54 49 38 37 10 24 85 53
Clinical Manifestations and LAB abnormalities of Disseminated MAC in HIV Feature Positive Fever Night sweats Diarrhea Abdominal pain Nausea/vomiting Weight loss Lymphadenopathy Intra-abdominal Mediastinal Hepatosplenomegaly Anemia ( Hb < 8. 5 gm/dl) Serum alkaline phosphatase No. of patients % 120 85 92 54 31 37 87 78 47 35 26 38 54 49 38 37 10 24 85 53
 Disseminated MAC n Dx – Positive culture of non-pulmonary, normally sterile site – H/C
Disseminated MAC n Dx – Positive culture of non-pulmonary, normally sterile site – H/C
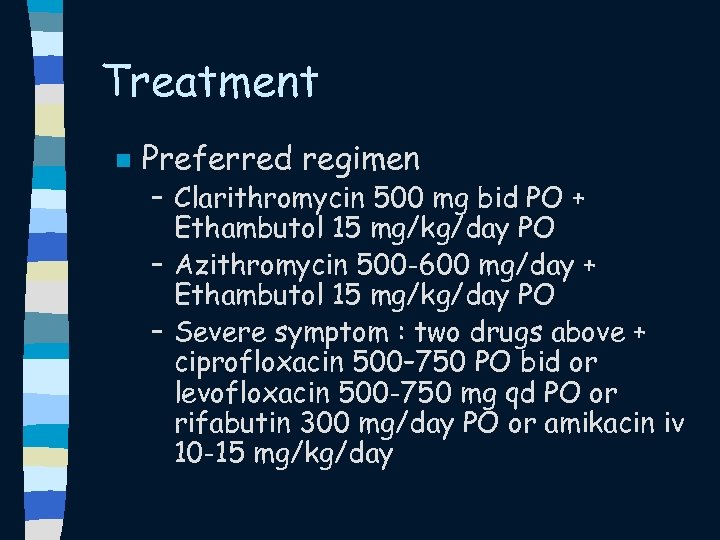 Treatment n Preferred regimen – Clarithromycin 500 mg bid PO + Ethambutol 15 mg/kg/day PO – Azithromycin 500 -600 mg/day + Ethambutol 15 mg/kg/day PO – Severe symptom : two drugs above + ciprofloxacin 500– 750 PO bid or levofloxacin 500 -750 mg qd PO or rifabutin 300 mg/day PO or amikacin iv 10 -15 mg/kg/day
Treatment n Preferred regimen – Clarithromycin 500 mg bid PO + Ethambutol 15 mg/kg/day PO – Azithromycin 500 -600 mg/day + Ethambutol 15 mg/kg/day PO – Severe symptom : two drugs above + ciprofloxacin 500– 750 PO bid or levofloxacin 500 -750 mg qd PO or rifabutin 300 mg/day PO or amikacin iv 10 -15 mg/kg/day
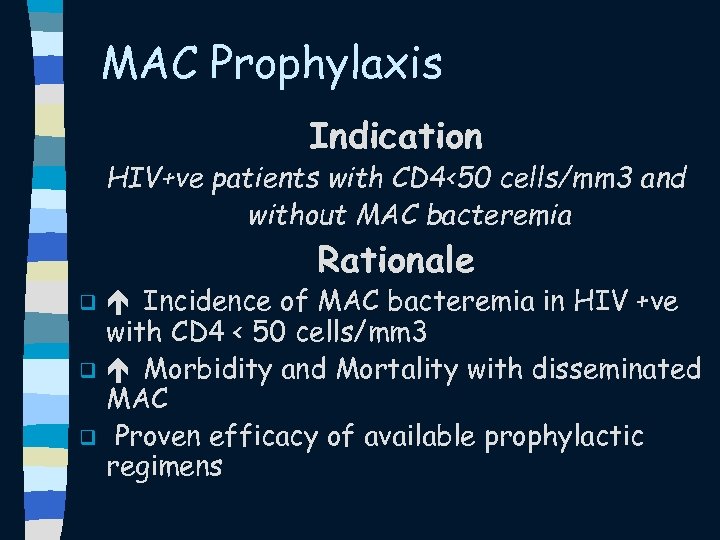 MAC Prophylaxis Indication HIV+ve patients with CD 4<50 cells/mm 3 and without MAC bacteremia Rationale q q q Incidence of MAC bacteremia in HIV +ve with CD 4 < 50 cells/mm 3 Morbidity and Mortality with disseminated MAC Proven efficacy of available prophylactic regimens
MAC Prophylaxis Indication HIV+ve patients with CD 4<50 cells/mm 3 and without MAC bacteremia Rationale q q q Incidence of MAC bacteremia in HIV +ve with CD 4 < 50 cells/mm 3 Morbidity and Mortality with disseminated MAC Proven efficacy of available prophylactic regimens
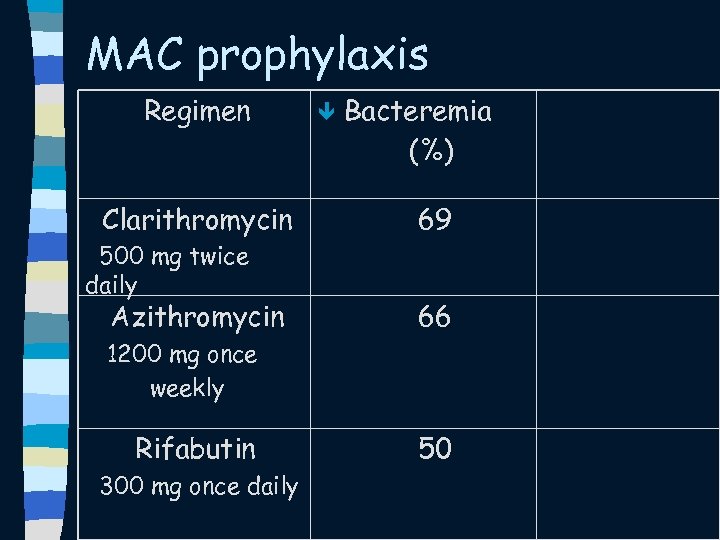 MAC prophylaxis Regimen Clarithromycin 500 mg twice daily Azithromycin ê Bacteremia (%) 69 66 1200 mg once weekly Rifabutin 300 mg once daily 50
MAC prophylaxis Regimen Clarithromycin 500 mg twice daily Azithromycin ê Bacteremia (%) 69 66 1200 mg once weekly Rifabutin 300 mg once daily 50
 Thank you
Thank you


