7a74afd2956ed146c01aeddfb51647a6.ppt
- Количество слайдов: 19
Aggressive meningioma Robert M. Koffie Neurosurgery sub-intern July 19, 2012 Department of Neurosurgery Massachusetts General Hospital Harvard Medical School
Case Presentation • HPI: 62 RHF 6 yrs ago p/w headaches, personality changes, & difficulty concentrating, and was found to have 7 -cm parasagittal extra-axial enhancing lesion c/w meningioma. • Multiple recurrence s/p surgery x 4, several cycles of radiotherapy.
Case Presentation • Oncological course: – 2006: GTR, benign meningioma – 2007: Recurrence, GTR, benign meningioma w/ atypical features • Post-op fractionated radiotherapy – 2009: Local recurrence, GTR, atypical meningioma – 2010: Multifocal recurrence, proton SRS x 3 – 2011: Recurrence, GTR, atypical meningioma w/ anaplastic features – 2012: Multifocal recurrence, ant. skull base invasion
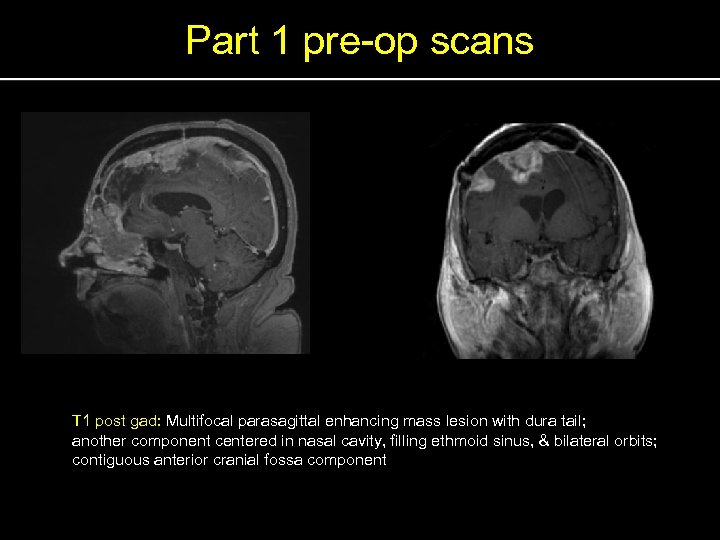
Part 1 pre-op scans T 1 post gad: Multifocal parasagittal enhancing mass lesion with dura tail; another component centered in nasal cavity, filling ethmoid sinus, & bilateral orbits; contiguous anterior cranial fossa component
Operative plan • Part 1 – Bifrontal craniotomy for resection of parasagittal tumor – 125 I brachytherapy seed placement • Part 2 – – Endonasal resection of tumor (ENT) Bifrontal craniotomy for skull base tumor Biorbital decompression (ENT/Oculoplastics) Titanium + free flap skull base reconstruction (Plastics)
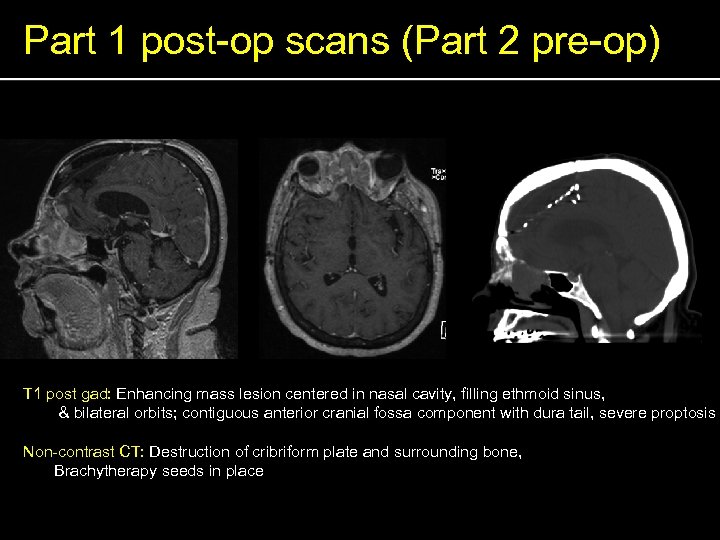
Part 1 post-op scans (Part 2 pre-op) T 1 post gad: Enhancing mass lesion centered in nasal cavity, filling ethmoid sinus, & bilateral orbits; contiguous anterior cranial fossa component with dura tail, severe proptosis Non-contrast CT: Destruction of cribriform plate and surrounding bone, Brachytherapy seeds in place
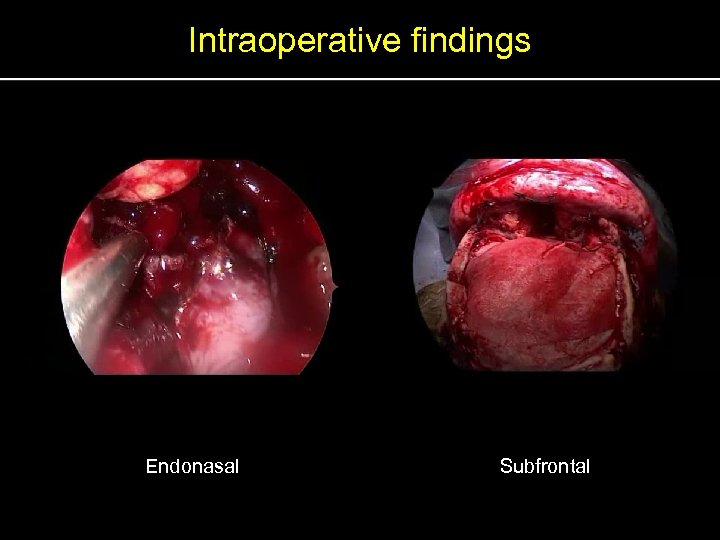
Intraoperative findings Endonasal Subfrontal
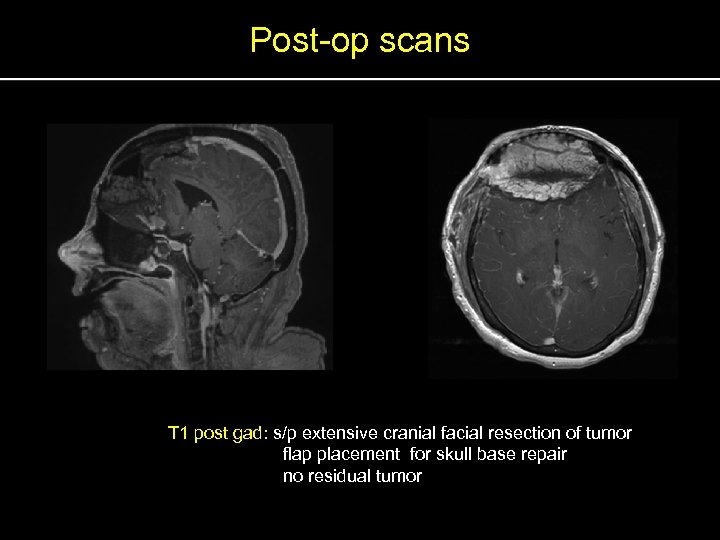
Post-op scans T 1 post gad: s/p extensive cranial facial resection of tumor flap placement for skull base repair no residual tumor
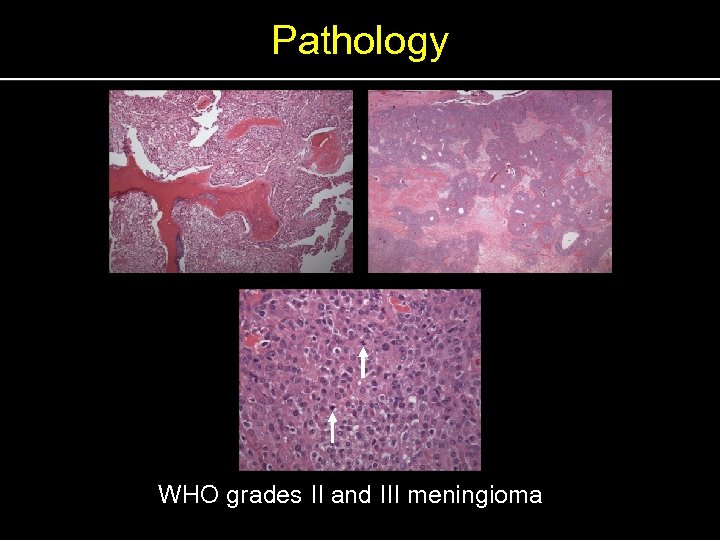
Pathology WHO grades II and III meningioma
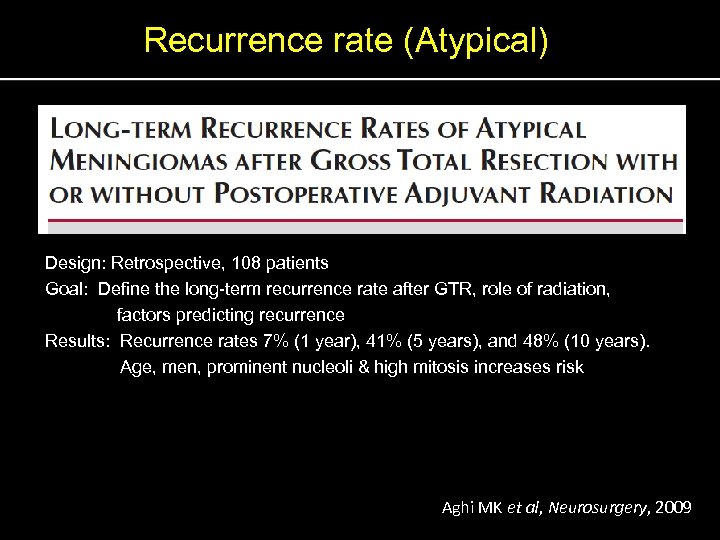
Recurrence rate (Atypical) Design: Retrospective, 108 patients Goal: Define the long-term recurrence rate after GTR, role of radiation, factors predicting recurrence Results: Recurrence rates 7% (1 year), 41% (5 years), and 48% (10 years). Age, men, prominent nucleoli & high mitosis increases risk Aghi MK et al, Neurosurgery, 2009
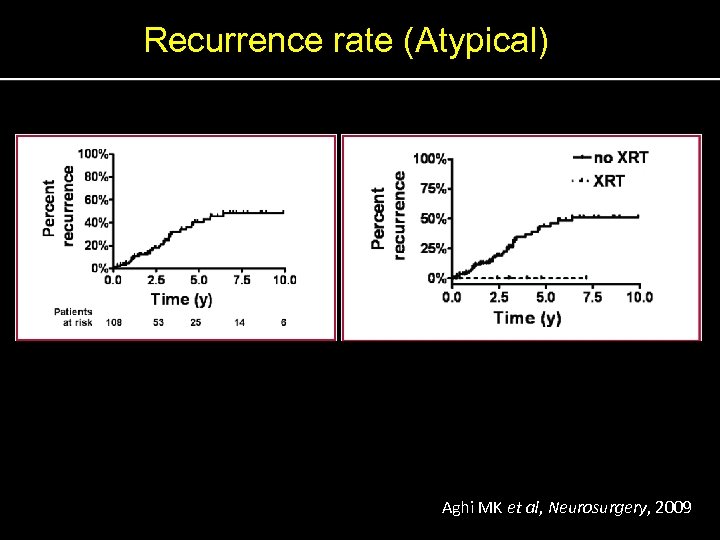
Recurrence rate (Atypical) Aghi MK et al, Neurosurgery, 2009
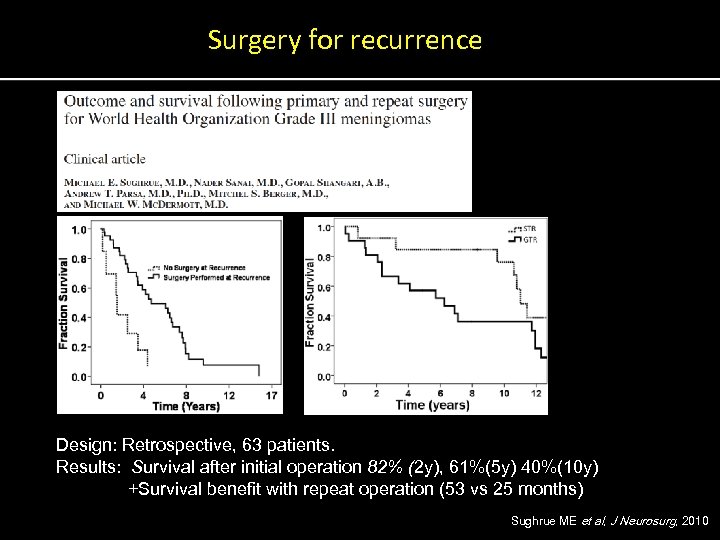
Surgery for recurrence Design: Retrospective, 63 patients. Results: Survival after initial operation 82% (2 y), 61%(5 y) 40%(10 y) +Survival benefit with repeat operation (53 vs 25 months) Sughrue ME et al, J Neurosurg, 2010
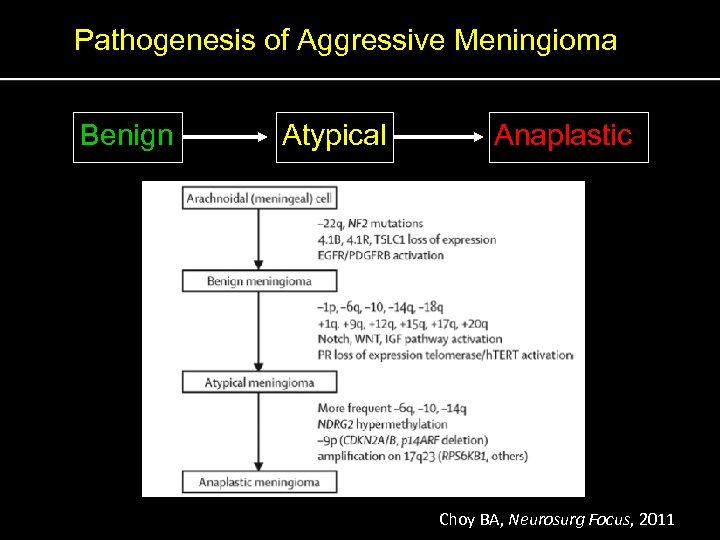
Pathogenesis of Aggressive Meningioma Benign Atypical Anaplastic Choy BA, Neurosurg Focus, 2011
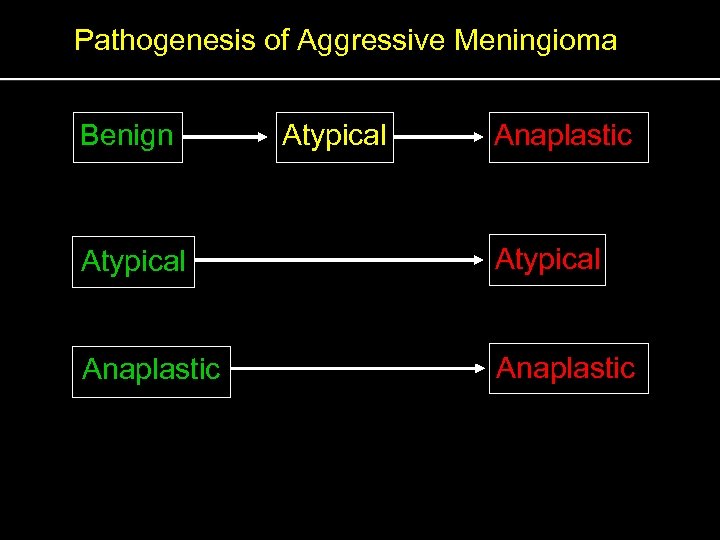
Pathogenesis of Aggressive Meningioma Benign Atypical Anaplastic Atypical Anaplastic
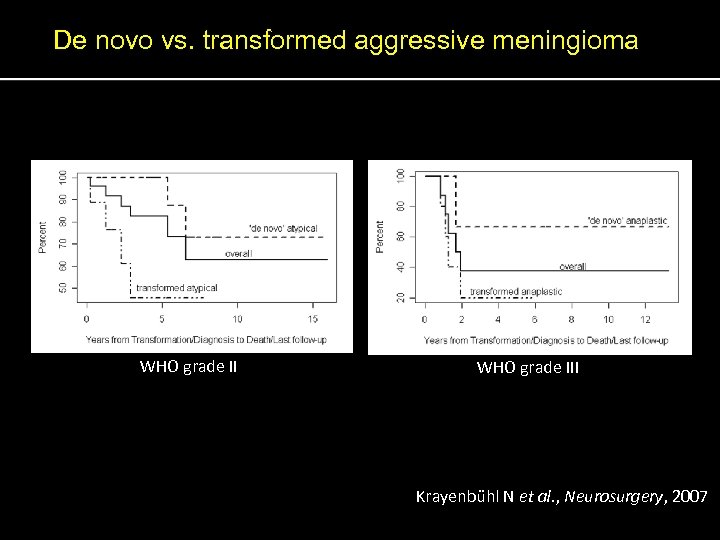
De novo vs. transformed aggressive meningioma WHO grade III Krayenbu hl N et al. , Neurosurgery, 2007
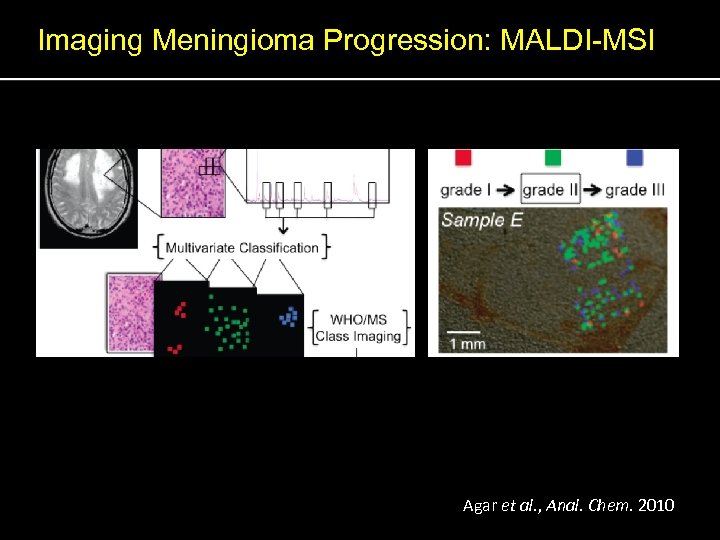
Imaging Meningioma Progression: MALDI-MSI Agar et al. , Anal. Chem. 2010
Hospital course • • • POD 8: Tension pneumocephalus s/p decompression POD 10: Thrombosed free flap, CSF Leak s/p repair POD 11: Lumbar drain POD 15: Trach/PEG POD 22: Doing well, transfer to rehab
Acknowledgements • MGH Faculty – William T. Curry, M. D. – David N. Louis, M. D. • MGH House staff – Gavin P. Dunn, M. D. , Ph. D. – Peter E. Fecci, M. D. , Ph. D. – Daniel A. Mordes, M. D. , Ph. D • Staff – Sylvia Weld – Neuro Nurses/NPs
Thank you
7a74afd2956ed146c01aeddfb51647a6.ppt