1d70d1361370d0488ed8cd7ac5976e33.ppt
- Количество слайдов: 56
agents Used in anemias HAEMATINICS
By the end of lecture students should be able to: n Know various types of anemias n Know aetiology of anemias n Know drugs used for treatment of anemias n Explain pharmacokinetics and pharmacodynamics of Iron n Know acute and chronic toxicities of iron n Know the management of overdose of iron
Haematopoiesis n 200 billion new blood cells are produced per day in normal person n Process occur in bone marrow in adults n Essential nutrients: iron, vitamin B 12, folic acid, pyridoxine, ascorbic acid and riboflavin n Hematopoietic growth factors
n Erythropoiesis is controlled by a feedback system in which a sensor in the kidney detects changes in oxygen delivery to modulate the erythropoietin secretion
Anemia Decrease in haemoglobin level below normal n Deficiency in oxygen-carrying erythrocytes n Symptoms Features of tissue hypoxia Pallor, fatigue, dizziness, exertional dyspnoea CVS adaptations to anemia (tachycardia, increased cardiac output, vasodilation) n
n ANEMIAS: Microcytic hypochromic anemia- iron deficiency most n Most common cause of chronic anemia is iron deficiency n Macrocytic anemias- Vit B 12 deficiency Folic acid deficiency n
n n n Drugs used for the correction of anemias Include: Iron Folic acid Vit B 12 Hematopoietic growth factors
IRON n Iron forms the nucleus of the ironporphyrin heme ring, which together with globin chains forms haemoglobin n Increased iron requirement Growing children Pregnancy Increased losses of iron (menstruating women)
n Iron containing heme is also an essential component of n n n n Myoglobin Cytochromes Catalase Peroxidase Metalloflavoprotein enzymes Xanthine oxidase Mitochondrial enzymes
Sources: Natural Meat, green vegetables, grain Synthetic Iron preparations In body catalysis of hemoglobin in senescent or damaged erythrocytes
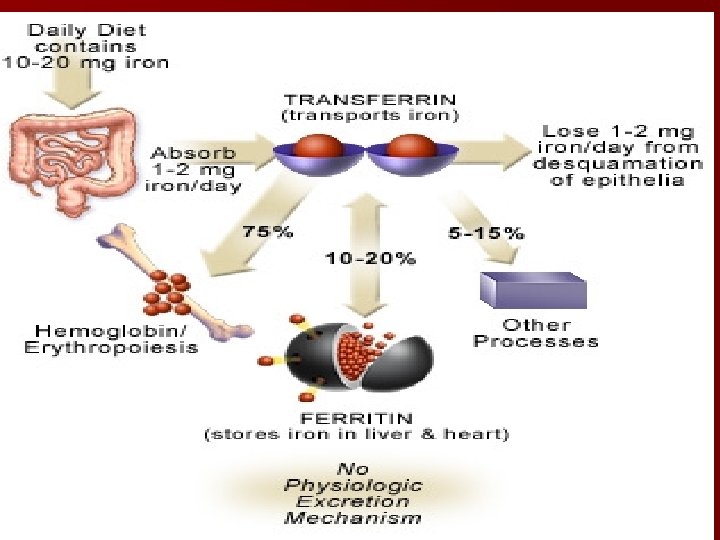
Pharmacokinetics Average diet contain 10 -15 mg of elemental iron daily Ø Total iron absorption can increase to 3 -4 mg/day in pregnant woman Ø Iron in meat is absorbed as such (hemoglobin and myoglobin) Ø Nonheme iron in foods is reduced by ferroreductase to ferrous form Ø A peptide hepcidin produced by liver cells-key central regulator of the system Ø
Absorption: Duodenum and Proximal jejunum as Fe+2 BY: Active transport by DMT 1 (divalent metal transporter) Iron complexed with heme Iron absorption increases when iron stores are depleted regulated by mucosal iron stores
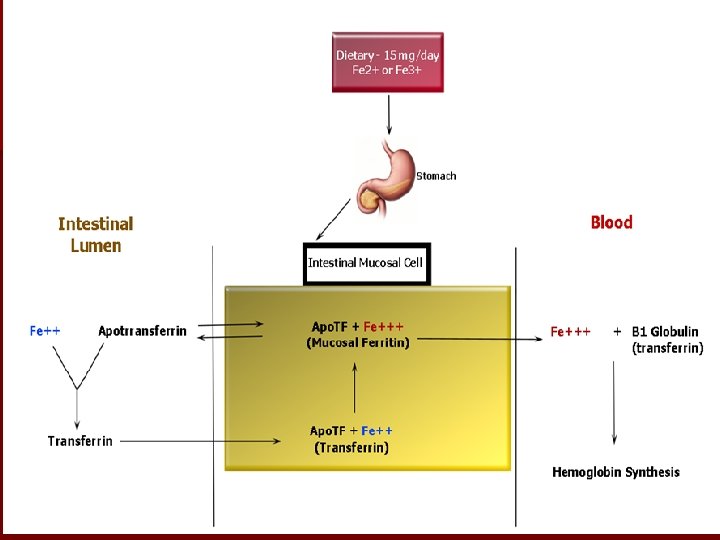

Absorption…. . n The absorbed iron is actively transported into the blood across the basolateral membrane by transporter ferroportin and oxidized to ferric iron by ferroxidase hephaestin
DISTRIBUTION n Bound to Transferrin (β –globulin) bind two molecules of ferric iron n The transferrin-iron complex enters maturing erytthoid cells n Transferrin receptors, transferrin iron complex is internalized in erythroid cells by endocytosis
Storage As ferritin in liver, spleen and bone and in parenchymal liver cells n Ferroportin is storage protein level is regulated by hepcidin n Low hepcidin lead to release of iron from storage sites n Ferritin level is checked in serum to estimate total body iron stores.
Elimination n Small amount lost in faeces by exfoliation of intestinal mucosal cells n Trace amounts in bile, urine and sweat n 1 mg of iron is lost from body per day
Therapeutic uses of Iron n Iron Deficient Anemia Treatment and prevention n n n Pregnancy Lactation Growing children Premature Babies Patents with chronic kidney disease Blood loss
n Inadequate iron absorption Gastrectomy Malabsorption Syndrome n GI Bleeding due to: § Ulcers § Aspirin § Excess consumption of coffee § Hookworm infestation
Oral preparations of iron Oral Iron n Ferrous Sulphate n Ferrous Gluconate n Ferrous Fumarate n Treatment with oral iron should be continued for 3 -6 months after correction of cause of iron loss.

Oral Iron Therapy n Dosage: n 200 - 400 mg/ day for 3 - 6 months n Adverse effects: n nausea, epigastric discomfort, abdominal cramps, constipation, diarrhea, black stools
n To overcome adverse effects n Lower daily dose of iron n Take iron with food n Change iron preparation.
PARENTRAL IRON THERAPY Indications: Ø Patients unable to tolerate oral iron Ø Patients with extensive blood loss Malabsorptive states Ø Patients with advanced chronic renal diseases. Ø
I/M and I/v use: n Iron dextran (ferric oxyhydroxide and dextran polymers) 50 mg /ml n n I/V n n only: Iron sucrose complex Sodium ferric gluconate complex
Dose calculation n Total iron deficit (TID) n Body wt (Kg) ˟ (Target Hb-Actual Hb g/dl) ˟ 2. 4 + depot iron (mg) n Total amount of venofer to be administered in ml = TID mg 200 mg/ml Ratio of total serum iron concentration and TIBC
Adverse Effects i) Local pain & tissue staining ii) Headache, giddiness, flushing iii) Fever, Arthralgia, Backache iv) Nausea, Vomiting v) Urticaria Rarely Anaphylaxis & death. Test dose of iron dextran is given.
Clinical Toxicity n Acute Iron Toxicity Seen in young children, who accidently ingest Iron tablets. 10 tablets in children Symptoms: vomiting, necrotizing gastroenteritis causing abdominal pain, bloody diarrhea followed by metabolic acidosis, dyspnea, coma & death
n Rx i) Gastric Aspiration Gastric lavage, with carbonate solution to form insoluble Iron. whole bowel irrigation ii) Deferoxamine - potent iron chelating compound given intravenously iii) Supportive Therapy
Chronic Iron Toxicity n Hemochromatosis (excess iron is deposited in the heart, liver, pancreas, and other organs) n Cause is inherited hemochromatosis and patient receiving many blood transfusions n Rx – Intermittent Phlebotomy (1 unit of blood is removed every week) – Iron. Chelation therapy (Deferoxamine, deferasirox is oral iron chelator)
Vit B 12 Ø Cofactor for several essential biochemical reactions in humans Ø Deficiency lead to megaloblastic anemia, GIT symptoms and neurologic abnormalities Cyanocobalamine n Hydroxocobalamine n
n Source: microbial synthesis from meat, eggs and dairy products (microorganisms grow in soil, sewage, water or in intestinal lumen of animals) n Chemistry: porphyrin like ring with a central cobalt atom attached to nucleotide
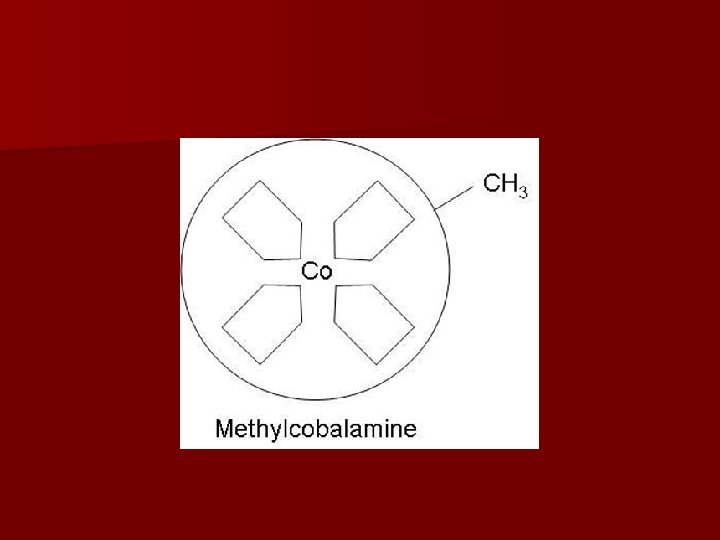
Structure……. n Various organic groups may be covalently bound to cobalt atom forming different cobalamines n Deoxyadenosylcobalamine n Methylcobalamine active form of vitamins in humans
Pharmacokinetics n Vitamin B 12 is absorbed only after it complexes with intrinsic factor (glycoprotein) n This complex of vit B 12 and intrinsic factor is absorbed in distal ileum n Transported to various cells by binding with transcobalamin I, II and III n Excess is transported to liver for storage.
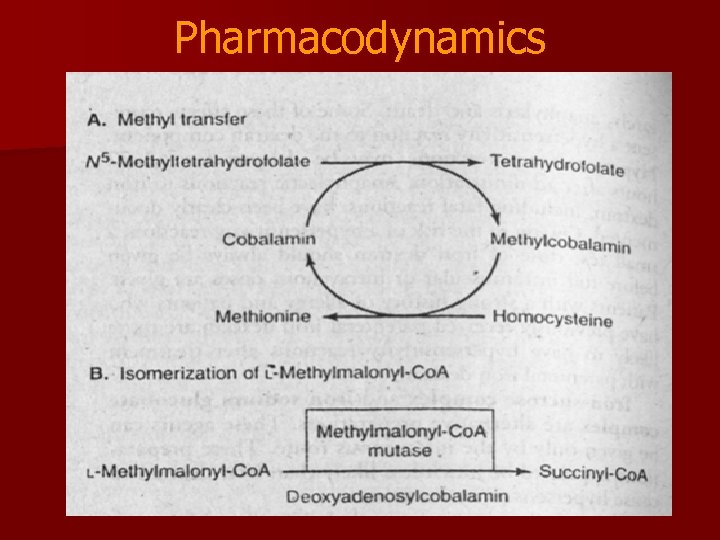
Pharmacodynamics
n Deficiency of vit B 12 also cause ‘folate trap’ n Methyltetrahydrofolate is not converted into other intracellular forms of folic acid
Clinical uses Ø Treat or prevent deficiency Ø Megaloblastic, macrocytic anemia mild or moderate leukopenia or thrombocytopenia. Ø Neurologic syndrome (paresthesias in peripheral nerves, weakness. Ø Progresses to spasticity, ataxia and CNS dysfunction.
Mechanism for Peripheral Neuropathy n Cobalamin is a cofactor for the enzyme Methylmalonyl-Co. A mutase which converts methylmalonyl-Co. A to succinyl-Co. A. n Succinyl-Co. A enters the Krebs cycles and goes into nerves to make myelin. n If no Vitamin B 12, methylmalonyl-Co. A goes on to form abnormal fatty acids and causes subacute degeneration of the nerves. Only B 12 can correct this problem.
Diagnosis n Serum levels of vitamins (Vit B 12 and Folic acid) n Schilling test (measures absorption and urinary excretion of radioactively labelled vitamin B 12)
Common causes of vit B 12 deficiency n Pernicious anemia Defective secretion of intrinsic factor Ø Partial and total gastrectomy Ø Malabsorption syndrome Ø Inflammatory bowel disease Ø Small bowel resection
Treatment n If the cause is malabsorption, n Parenteral injections of vit B 12 cyanocobalamine or hydroxocobalamine. n vitamin B 12 can be administered intranasally as a spray or gel.
Parenteral therapy Inj Cyanocobalamin or hydroxcobalamin n Initial therapy 100 – 1000 µg – I/M-D or on alternate days for 1 -2 weeks Maintenance therapy 100 – 1000 µg – I/M- once a month
Folic Acid Essential for normal DNA synthesis n Source Plant and animal (liver, kidney & green vegetables. n Chemistry Pteroylglutamic acid p-aminobenzoic acid and glutamic acid
Pharmacokinetics of Folic Acid n Site of absorption: Proximal jejunum Polyglutamates monoglutamate α- 1 glutamyl transferase (conjugase)
PHARMACODYNAMICS: Tetrahydrofolate cofactor participate in one-carbon transfer reactions d. TMP DNA synthesis Required for the synthesis of : Amino acids purines DNA
n d. TMP synthesis cycle d. TMP synthase, dihydrofolate reductase and serine transhydroxymethylase Ø Synthesis of methionine from homocystine Ø Donate one carbon for synthesis of essential purines
Folic Acid Deficiency Seen in i) iii) iv) v) vii) Inadequate dietary intake of folates Prolong cooking In alcholics & in pt with liver diseases Pregnancy Hemolytic Anemias Malabsorption Syndrome Drugs Methotrxate , trimethoprim pyrimethamine and
Treatment of Folic Acid Deficiency n parentral administ rarely needed. Oral therapy: Dose 1 mg/d – continued until cause is corrected or removed.
Hematopoietic Growth Factors n Glycoproteins n Erythropoietin n G-CSF n GM-CSF n Interlukin-II n Romiplostim hormones
Erythropoietin n Source: Recombinant DNA technology n I/V administration n Dose calculated in IU. n Epoetin alfa and epoetin beta n Half life is 4 -13 hrs n Darbepoetin alfa is heavily glycosylated (longer half life)
Pharmacodynamics n Erythropoietin receptors on red cell progenitors (JAK/STAT) n Increased production of RBCs in bone marrow if Ø No nutritional deficiency is present Ø No primary bone marrow disorder Ø No bone marrow suppression from drugs
Clinical uses Ø Anemia due to chronic renal disease After treatment increase in reticulocyte count is observed in 10 days Increase in Hb in 2 -6 weeks Ø Anemia due to zidovudine treatment in HIV patients Ø Reduce the need of transfusions in high risk patients

Toxicity n Hypertension n Thrombotic complications n Allergic reactions are rare n Erythropoieitin is banned by International Olympic Committee
Myeloid Growth factors Filgrastrim n Sargramostim n Pegfilgrastim n Leograstim used for cancer chemotherapy induced Neutropenia Congenital neutropenia Cyclic neutropenia Myelodysplasia Aplastic anemia n

Toxicity n Bone pain n Fever, malaise, arthralgia, myalgia
1d70d1361370d0488ed8cd7ac5976e33.ppt