42cc468a6f52f816272a3392ddc10b0d.ppt
- Количество слайдов: 74
Adverse Outcomes From Prenatal Alcohol Exposure By: Larry Burd, Ph. D. Director North Dakota Fetal Alcohol Syndrome Center
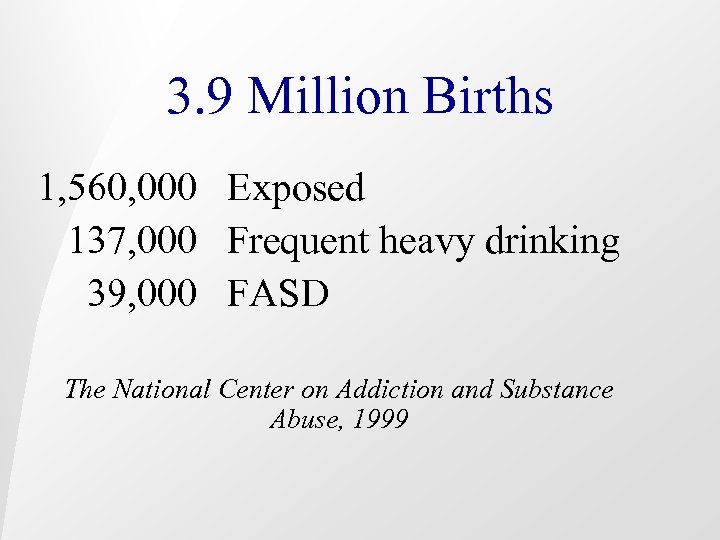
3. 9 Million Births 1, 560, 000 Exposed 137, 000 Frequent heavy drinking 39, 000 FASD The National Center on Addiction and Substance Abuse, 1999

§ Lost productivity due to FAS: Adults - $1, 000, 000/annually $2, 739, 000/day § Health care costs due to FAS: Children and adults - $2, 000, 000/annually $5, 479, 000/day The National Center on Addiction and Substance Abuse, 1999

North Dakota Alcohol Income (2000) Wholesale tax $ 5, 500, 000 Sales tax $14, 500, 000 Total $20, 000

FAS In Florida • Born Each Year FAS ARND Total 103 415 518 • Cost Per Day $957, 286 • Annual Cost $432 million • Annual Cost Special $82 million Education and Juvenile Justice • 5 year Costs $1. 7 billion
Family History Maternal Risk Factors
Family History • Familial • Multigenerational • Genetic Factors

Increased Probability of a Previous Child with Fetal Alcohol Syndrome Total number of live births prior to birth of FAS child 135 Number of Estimated Incidence of children with incidence of FAS in previous Risk FAS in prior FAS per 1, 000 births per 1, 000 increased by births live births 23 . 97 Source: E. L> Abel, Fetal Alcohol Syndrome in Families, Neurotoxicity and Teratology (1988), 10, pp. 1 -2. Copyright 1988 by Elsevier Science, Adapted with permission of the publisher. 170. 4 172 x

Increased Risk of Having a Second Child with Fetal Alcohol Syndrome Total number Number of of live births children with after birth of FAS in FAS child subsequent births 35 27 Estimated Incidence of incidence of FAS in Risk FAS per subsequent increased by 1, 000 live births per 1, 000 births live births. 97 Source: E. L> Abel, Fetal Alcohol Syndrome in Families, Neurotoxicity and Teratology (1988), 10, pp. 1 -2. Copyright 1988 by Elsevier Science, Adapted with permission of the publisher. 771 795 x

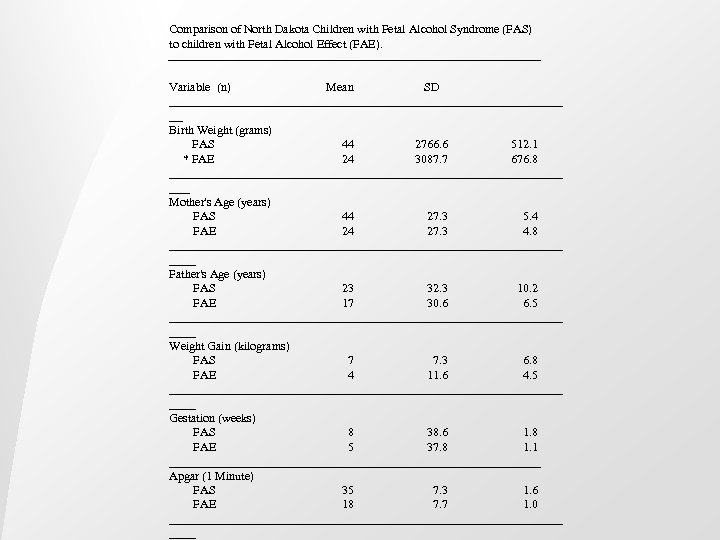
Comparison of North Dakota Children with Fetal Alcohol Syndrome (FAS) to children with Fetal Alcohol Effect (FAE). Variable (n) Mean SD ______________________________ __ Birth Weight (grams) FAS 44 2766. 6 512. 1 * FAE 24 3087. 7 676. 8 ______________________________ ___ Mother's Age (years) FAS 44 27. 3 5. 4 FAE 24 27. 3 4. 8 ______________________________ Father's Age (years) FAS 23 32. 3 10. 2 FAE 17 30. 6 6. 5 ______________________________ Weight Gain (kilograms) FAS 7 7. 3 6. 8 FAE 4 11. 6 4. 5 ______________________________ Gestation (weeks) FAS 8 38. 6 1. 8 FAE 5 37. 8 1. 1 _______________________________ Apgar (1 Minute) FAS 35 7. 3 1. 6 FAE 18 7. 7 1. 0 ______________________________

Maternal and Paternal Risk Factor for FAS from 132 Cases of FAS/FAE and 5 controls per case from North Dakota (adapted from Bagheri and Burd)21 ________________________________________ Variable Case/Control Mean (Difference) p-value Case/Control ________________________________________ Mother's Age (years) 132/660 27. 4/25. 4 (2. 0) <0. 001 Father's Age (years) 43/215 32. 0/27. 8 (4. 2) <0. 001 Weight gain in pregnancy (lbs. ) 33/165 22. 1/30. 4 (8. 3) <0. 001 Gestation (weeks) 101/505 38. 7/40. 0 (1. 3) <0. 001 Month prenatal care began 123/615 3. 4/2. 7 (0. 7) <0. 001 Number prenatal visits 123/615 5. 5/9. 7 (4. 2) <0. 001 Mother's education 125/625 10. 6/13. 0 (2. 4) <0. 001 Father's education 32/160 10. 8/13. 2 (2. 6) <0. 001 ________________________________________
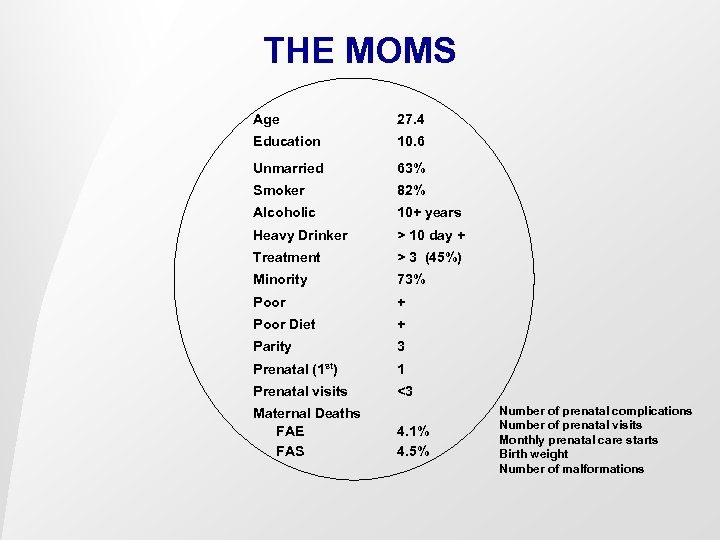
THE MOMS Age 27. 4 Education 10. 6 Unmarried 63% Smoker 82% Alcoholic 10+ years Heavy Drinker > 10 day + Treatment > 3 (45%) Minority 73% Poor + Poor Diet + Parity 3 Prenatal (1 st) 1 Prenatal visits <3 Maternal Deaths FAE FAS 4. 1% 4. 5% Number of prenatal complications Number of prenatal visits Monthly prenatal care starts Birth weight Number of malformations
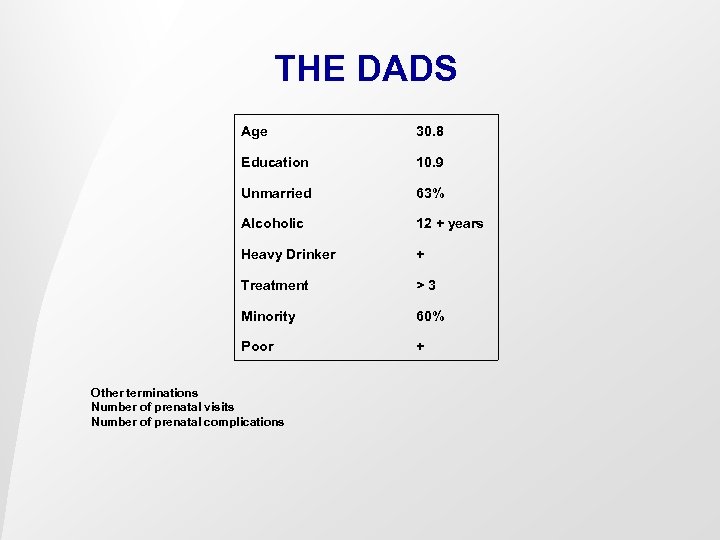
THE DADS Age 30. 8 Education 10. 9 Unmarried 63% Alcoholic 12 + years Heavy Drinker + Treatment >3 Minority 60% Poor + Other terminations Number of prenatal visits Number of prenatal complications

THE CHILDREN Age Diagnosis 7. 1 years Older Sibs 2 Younger 2 Birth Defects 20% Cerebral Palsy 6% Mental Retardation 30% ADHD 60% Out of Home 85% Head Injury 25% Dead Sibling FAS/FAE Controls 11% 2%
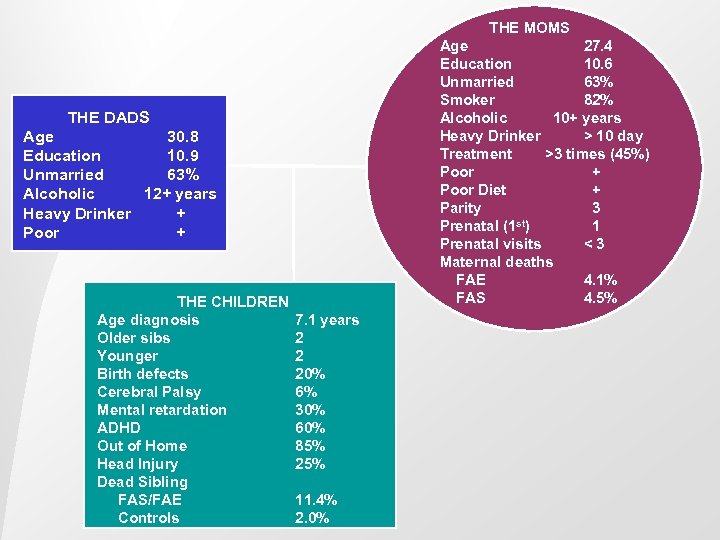
THE MOMS Age 27. 4 Education 10. 6 Unmarried 63% Smoker 82% Alcoholic 10+ years Heavy Drinker > 10 day Treatment >3 times (45%) Poor + Poor Diet + Parity 3 st) Prenatal (1 1 Prenatal visits <3 Maternal deaths FAE 4. 1% FAS 4. 5% THE DADS Age 30. 8 Education 10. 9 Unmarried 63% Alcoholic 12+ years Heavy Drinker + Poor + THE CHILDREN Age diagnosis Older sibs Younger Birth defects Cerebral Palsy Mental retardation ADHD Out of Home Head Injury Dead Sibling FAS/FAE Controls 7. 1 years 2 2 20% 6% 30% 60% 85% 25% 11. 4% 2. 0%
Mortality in a Ten-Year Follow -Up of FAS Children 18% cases 27% of the Mothers (Streissguth, 1985)
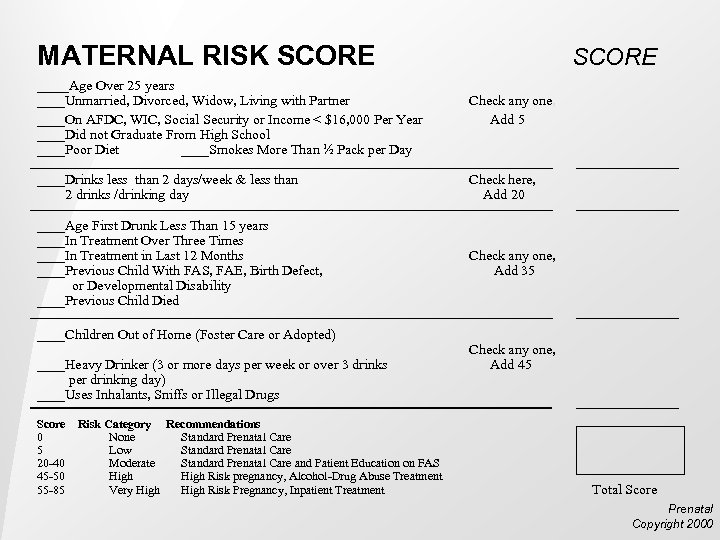
MATERNAL RISK SCORE ____Age Over 25 years SCORE ____Unmarried, Divorced, Widow, Living with Partner ____On AFDC, WIC, Social Security or Income < $16, 000 Per Year ____Did not Graduate From High School ____Poor Diet ____Smokes More Than ½ Pack per Day Check any one, Add 5 ____Drinks less than 2 days/week & less than 2 drinks /drinking day Check here, Add 20 ____Age First Drunk Less Than 15 years ____In Treatment Over Three Times ____In Treatment in Last 12 Months ____Previous Child With FAS, FAE, Birth Defect, or Developmental Disability ____Previous Child Died Check any one, Add 35 ____Children Out of Home (Foster Care or Adopted) ____Heavy Drinker (3 or more days per week or over 3 drinks per drinking day) ____Uses Inhalants, Sniffs or Illegal Drugs Score Risk Category Recommendations 0 None Standard Prenatal Care 5 Low Standard Prenatal Care 20 -40 Moderate Standard Prenatal Care and Patient Education on FAS 45 -50 High Risk pregnancy, Alcohol-Drug Abuse Treatment 55 -85 Very High Risk Pregnancy, Inpatient Treatment Check any one, Add 45 Total Score Prenatal Copyright 2000
Exposure
Adverse Outcomes Due to Prenatal Alcohol Exposure • Did mom drink? • Did she drink enough? • Abnormal signs or disorders Yes or No
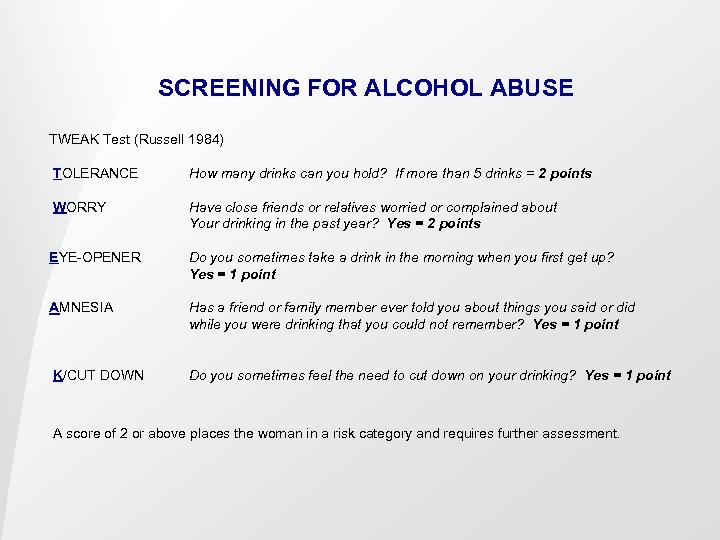
SCREENING FOR ALCOHOL ABUSE TWEAK Test (Russell 1984) TOLERANCE How many drinks can you hold? If more than 5 drinks = 2 points WORRY Have close friends or relatives worried or complained about Your drinking in the past year? Yes = 2 points EYE-OPENER Do you sometimes take a drink in the morning when you first get up? Yes = 1 point AMNESIA Has a friend or family member ever told you about things you said or did while you were drinking that you could not remember? Yes = 1 point K/CUT DOWN Do you sometimes feel the need to cut down on your drinking? Yes = 1 point A score of 2 or above places the woman in a risk category and requires further assessment.
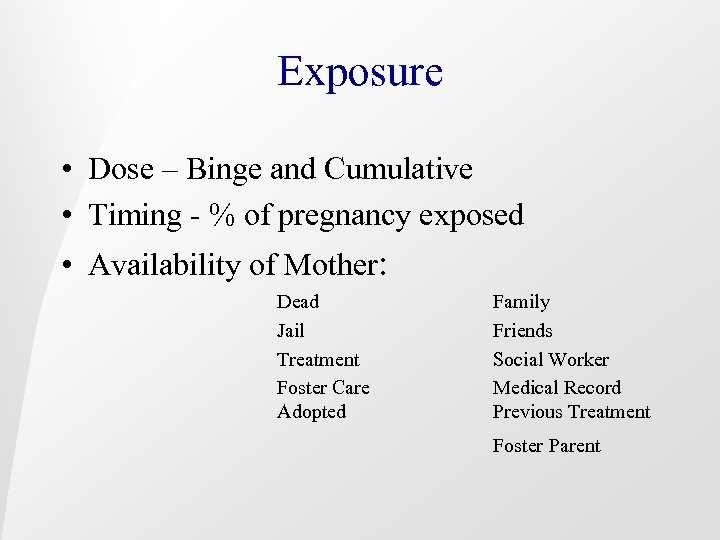
Exposure • Dose – Binge and Cumulative • Timing - % of pregnancy exposed • Availability of Mother: Dead Jail Treatment Foster Care Adopted Family Friends Social Worker Medical Record Previous Treatment Foster Parent

Fetal Alcohol Exposure: • Could increase severity of other disorders • Could cause other disorders to occur – lower susceptibility • Could cause FAS with other disorders • FAS could obscure other disorders • Could be irrelevant to phenotype

Tom Welty MD AAIHS 1998 Prevalence Rate FAS AAIHS: 8 per 1, 000 live births. 2 to 8 times above other population estimates.
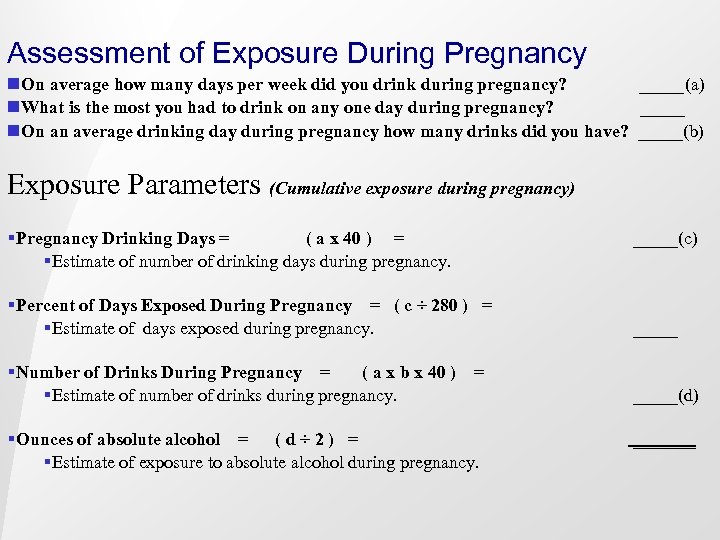
Assessment of Exposure During Pregnancy n. On average how many days per week did you drink during pregnancy? _____(a) n. What is the most you had to drink on any one day during pregnancy? _____ n. On an average drinking day during pregnancy how many drinks did you have? _____(b) Exposure Parameters (Cumulative exposure during pregnancy) §Pregnancy Drinking Days = ( a x 40 ) = §Estimate of number of drinking days during pregnancy. §Percent of Days Exposed During Pregnancy = ( c ÷ 280 ) = §Estimate of days exposed during pregnancy. §Number of Drinks During Pregnancy = ( a x b x 40 ) = §Estimate of number of drinks during pregnancy. §Ounces of absolute alcohol = ( d ÷ 2 ) = §Estimate of exposure to absolute alcohol during pregnancy. _____(c) _____ _____(d) _______

Mortality
Two Hundred and Fifty-Eight Cases of Suffocation of Infants By Charles Templeman, M. D. , B. Sc. (Pub. Health), Surgeon of Police; Surgeon to the Royal Infirmary, Dundee. (Read before the Medico-Chirurgical Society of Edinburgh, 1 st June 1892. )

If drinking over 2 years prior to pregnancy, mortality rate 62. 7% ¨ 46% deaths occur on Saturday night and Sunday morning
A Note on the Influence of Maternal Inebriety on the Offspring By W. C. Sullivan, M. D. , and Stewart Scholar in Mental Disease, R. U. I. , Deputy Medical Officer, H. M. Convict Prison, Parkhurst (July, 1899)
Mortality ¨Women n = 100 (plus 20 female relatives) 600 Children ¨ 335 (55. 8%) died ¨ 80 women had 3 or more dead infants
Second Cause of Death: Maternal Drunkenness

Mortality and Alcohol Use • Increased risk of SIDS • Sibling mortality FAS/FAE Controls 10% 2% • Increased risk of death Saturday and Sunday

Diagnosis

Diagnosis of People with Adverse Outcome from Prenatal Alcohol Exposure Specific Pattern of Malformations. Confirmed History of Maternal Alcohol Use-Abuse. Specific Pattern of Neurocognitive Deficits.

DIAGNOSTIC CRITERIA FAS AND ALCOHOL RELATED EFFECTS (3, 4, and 5 require the presumption that the finding is due to prenatal alcohol exposure) 1. FAS confirmed alcohol exposure A. confirmed maternal alcohol exposure B. characteristic facial anomalies C. growth retardation D. neurodevelopmental abnormalities 2. FAS without confirmed maternal alcohol exposure B, C, and D above 3. Partial FAS with confirmed maternal alcohol exposure A. confirmed maternal alcohol exposure B. some or partial characteristic facial features C. growth retardation D. neurodevelopmental abnormalities E. behavioral or cognitive abnormalities presumed due to prenatal alcohol exposure 4. Alcohol-Related Birth Defects (ARBD) Cardiac Ocular-Auditory Skeletal Renal 5. Other Alcohol-Related Neurodevelopmental Disorder (ARND) A. CNS neurodevelopmental abnormalities B. Complex pattern of behavior or cognitive abnormalities

Signs of Prenatal Alcohol Exposure • • • Vision Hearing ADHD Mental Disorders Cognitive Impairment Height Weight Head Circumfrence < 10 th Cleft Palate • 3 or more facial features: – Short palpebral fissions – Absent philtrum – Thin vermilion border upper lip – Epicanthal Folds • Neurological Abnormalities • Cardiac Deficits • Organ Abnormalities
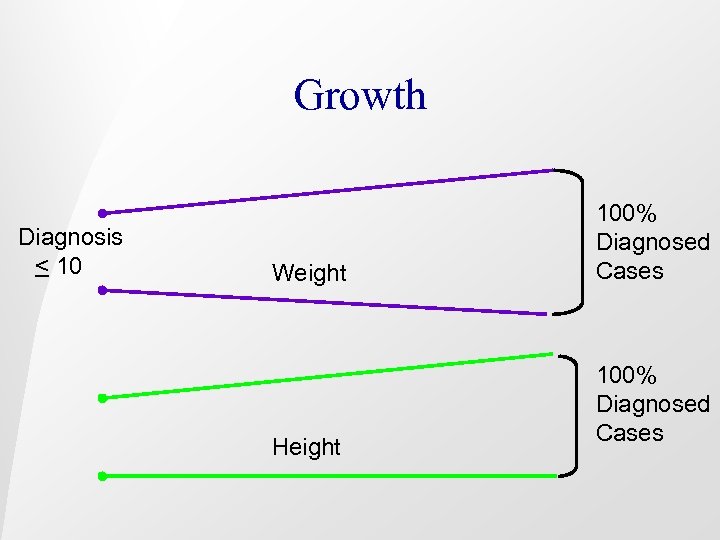
Growth Diagnosis < 10 Weight Height 100% Diagnosed Cases
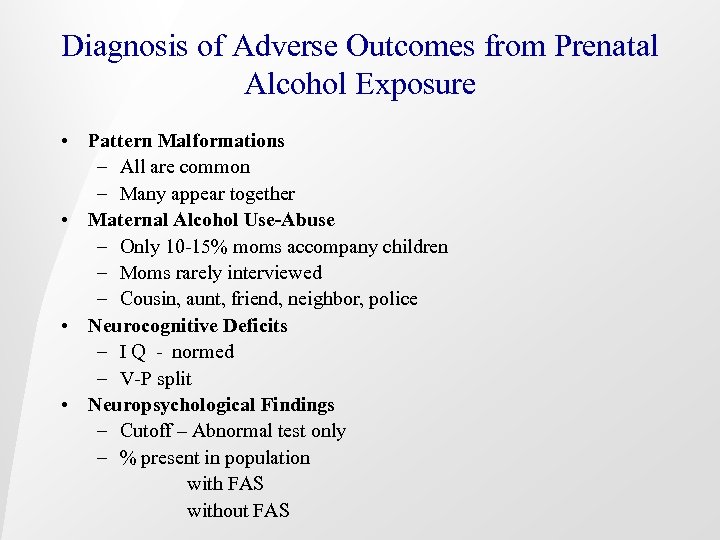
Diagnosis of Adverse Outcomes from Prenatal Alcohol Exposure • Pattern Malformations – All are common – Many appear together • Maternal Alcohol Use-Abuse – Only 10 -15% moms accompany children – Moms rarely interviewed – Cousin, aunt, friend, neighbor, police • Neurocognitive Deficits – I Q - normed – V-P split • Neuropsychological Findings – Cutoff – Abnormal test only – % present in population with FAS without FAS
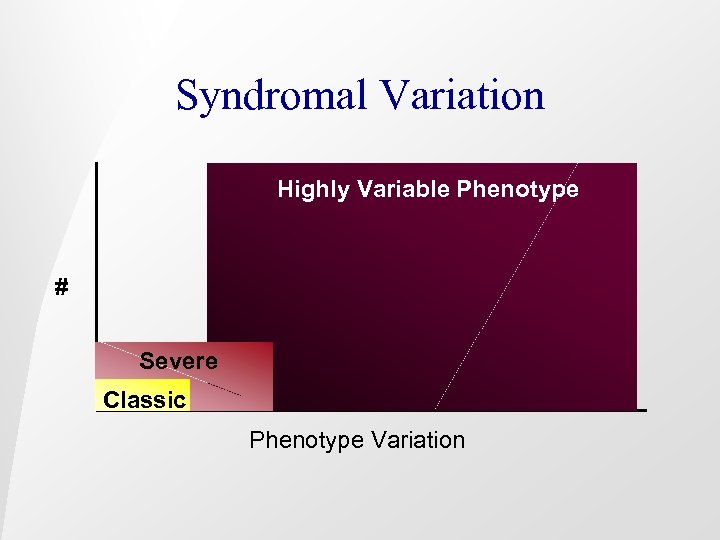
Syndromal Variation Highly Variable Phenotype # Severe Classic Phenotype Variation
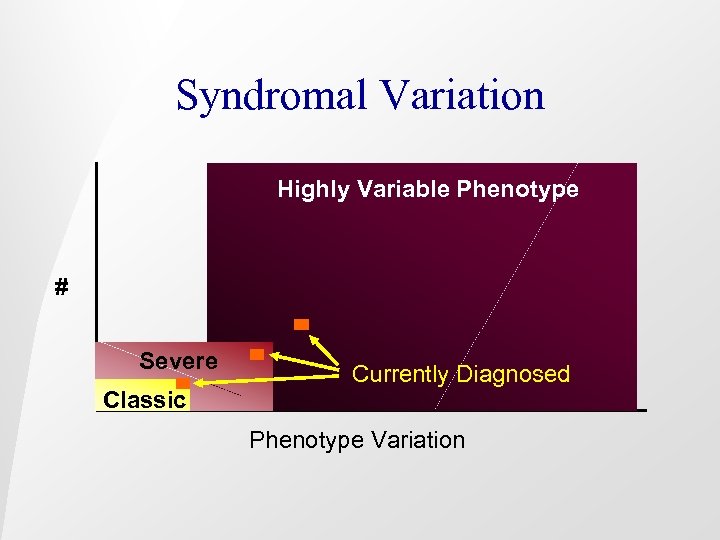
Syndromal Variation Highly Variable Phenotype # Severe Classic Currently Diagnosed Phenotype Variation
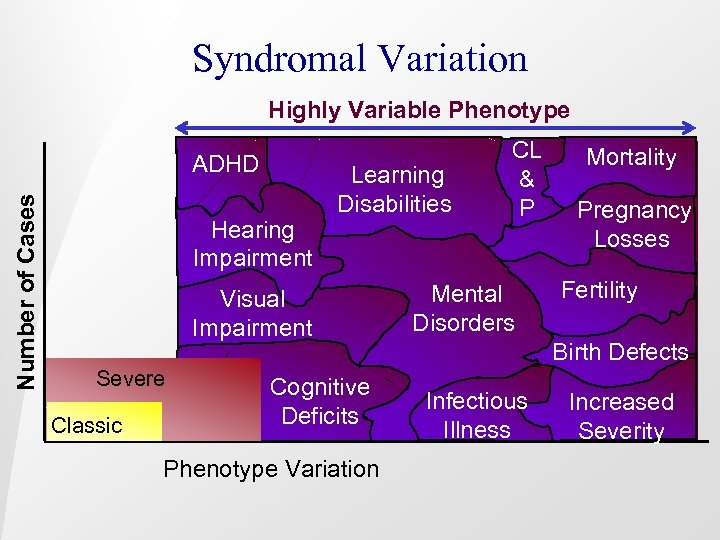
Syndromal Variation Number of Cases Highly Variable Phenotype ADHD Hearing Impairment Learning Disabilities Visual Impairment Severe Classic Cognitive Deficits Phenotype Variation CL & P Mental Disorders Mortality Pregnancy Losses Fertility Birth Defects Infectious Illness Increased Severity

No leaves Smooth bark “I found one! It’s the only tree here, but I expected to find a whole forest. . ” FAS Too big Too small House, not tree Trunk too Looks like thick Family Has fruit Has needles Poor soil

We have exact standards for trees. We do not want to label or stigmatize.

Inaccurate Diagnosis: Stigmatization of Mother Labeling of Child Diagnostic Imprecision • Parents • Schools • Doctors • Epidemiologist • Apathy

Consequences of Misdiagnosis Public Health § Inaccurate Prevalence Outcome § Causal Factors § Cost Estimates § Service Systems
Consequences of Misdiagnosis Mothers § Recurrence § Health § Death § Guilt § Search for what’s wrong

Consequences of Misdiagnosis Child § Misunderstood Behavior § Inappropriate Treatment § Secondary Disabilities § Jail § Substance Abuse § Multiple Foster Homes § Unnecessary testing
Consequences of Misdiagnosis Society § Cost § Low Priority for funding § Recurrence § Loss of Potential § Infant-child Mortality Rate § Increased Severity

Consequences of Misdiagnosis Public Health § Inaccurate Prevalence Outcome § Causal Factors § Cost Estimates § Service Systems Child § § § § Misunderstood Behavior Inappropriate Treatment Secondary Disabilities Jail Substance Abuse Multiple Foster Homes Unnecessary testing Mothers § Recurrence § Health § Death § Guilt § Search for what’s wrong Society § § § Cost Low Priority for funding Recurrence Loss of Potential Infant-child Mortality Rate Increased Severity
Current Imprecision (Top 10) 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Very few centers able to diagnose To complicated for most doctors Most moms missed Most children mislabeled Poor prevalence estimates Inadequate funding Low public health priority Generational recurrence High familial recurrence rate Inappropriate treatment – could but won’t

Protective Effect Williams Syndrome Dubowitz Syndrome Velocardiofacial Syndrome Downs Syndrome Cerebral Palsy Spina Bifida

Preferred Performance Characteristics 1. 2. 3. 4. 5. 6. 7. 8. Captures many – most cases Reflects understanding of comorbidity Does not exert a protective effect Easy to implement Leads to prevention of recurrence Protects mother Decreases secondary disability Leads to appropriate interventions


The Brain



Examination of the developing mouse brain following alcohol exposure shows cells that have been killed. Apoptotic cells Nile blue stained in two of the pictures and dark brown at bottom right. Kindly provided by Dr. K Sulik and Dr. W Dunty, Univ of North Carolina
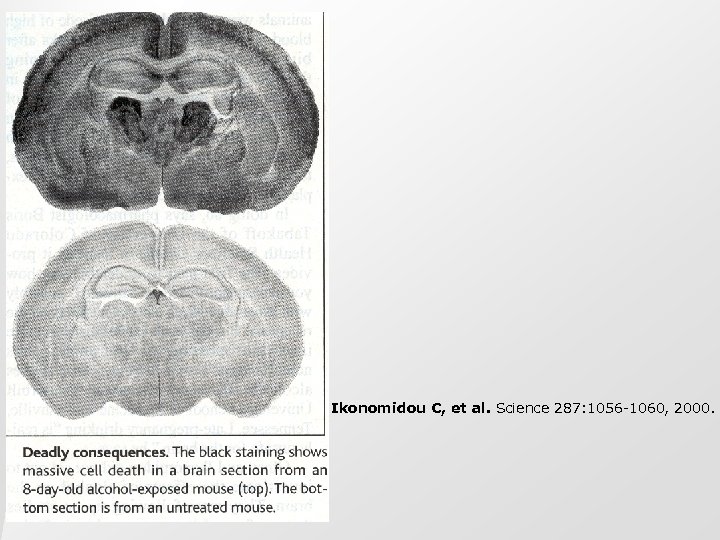
Ikonomidou C, et al. Science 287: 1056 -1060, 2000.

Impairments in: • Memory • Attention • Adaptive behavior • Use of social rules • Sleep • Behavior regulation


Treatment
Treatment of FAS Start early-Avoid Abuse Avoid multiple foster homes Treat in community Make a place in the community Avoid problem peers Use legal system Long term treatment-more than 10 years


A Developmental Management Model for Children and Adults With FAS and Related Disorders _______________________________________ Newborn Management: 1. Diagnostic assessment of both physical and neurologic anomalies 2. Early involvement of child protective services. 3. Referral to the Department of Human Services for initiation of infant stimulation. 4. Prevention of secondary disabilities, specific to age group; abuse, vision/hearing deficits. 5. Referral of mother to substance abuse treatment program. 6. Sensory evaluation (vision and hearing). Childhood Management: 1. Head Start Program with special learning environment, addressing specific learning disabilities. 2. Annual developmental assessment. 3. Referral for services to address neurologic deficits and psychosocial delays. 4. Prevention of secondary disabilities.

Monitoring social skill development Adolescent Management: 1. Prevention of secondary disabilities, specifically drug and alcohol use. Prevention of school failure, social problems and institutionalization. 2. Vocational training, preparation for future employment. 3. Continuation of developmental assessments. 4. Develop long term plan (10 years). 5. Social skill development and monitor peer group. Adult Management: 1. Employment services (vocational rehabilitation). 2. Social services and long-term support. 3. Monitor for substance abuse. 4. Enhance awareness in adult service systems: mental health, substance abuse, corrections. ____________________________________
Common Recommendations • • • Annual Evaluation Positive Behavior Management Program Respite Care IEP Monitor Peers Schedule Plan Ahead Evaluate All Siblings Find the Mom

State Capacity and Prevention
Estimating Capacity: Need for Diagnostic Services www. online-clinic. com FAS Cost and prevalence.
Funding Services Money Spent on People with FAS “We have no funding. You are not eligible. ” FAS Prevention

What Can We Do Now? • • Community Assessment FASD Task Force Inform Policy Makers Inform Policy Implementers
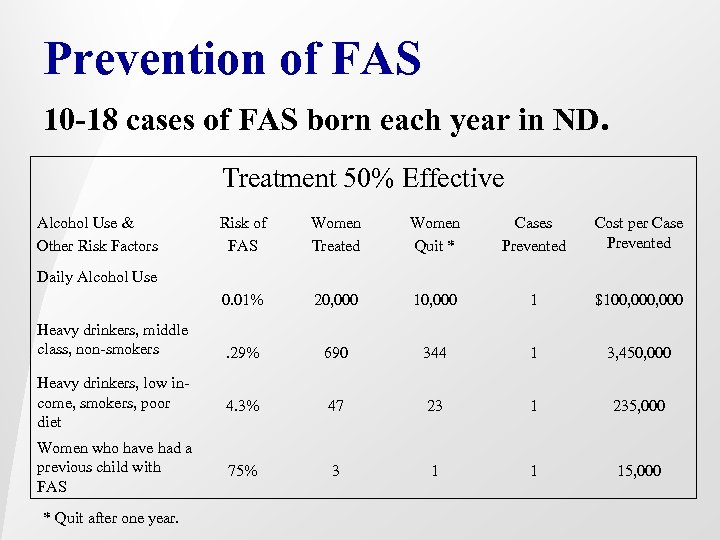
Prevention of FAS 10 -18 cases of FAS born each year in ND. Treatment 50% Effective Alcohol Use & Other Risk Factors Risk of FAS Women Treated Women Quit * Cases Prevented Cost per Case Prevented 0. 01% 20, 000 1 $100, 000 . 29% 690 344 1 3, 450, 000 Heavy drinkers, low income, smokers, poor diet 4. 3% 47 23 1 235, 000 Women who have had a previous child with FAS 75% 3 1 1 15, 000 Daily Alcohol Use Heavy drinkers, middle class, non-smokers * Quit after one year.

Our One Year Anniversary Number of new cases in one year: 518

42cc468a6f52f816272a3392ddc10b0d.ppt