507458d188893903e43f229974d60684.ppt
- Количество слайдов: 66
Advanced Therapies in Chronic Heart Failure By Susan George, DNP, APRNCNP, CCNS, CCRN, CHFN
Objectives Briefly review various pharmacologic agents used to manage heart failure (HF) Ø Define advanced HF Ø Identify warning signs of advanced HF Ø Discuss inotropes used in chronic HF Ø Review indication and contraindication for transplant. Ø Describe mechanical circulatory support in the management of chronic HF Ø
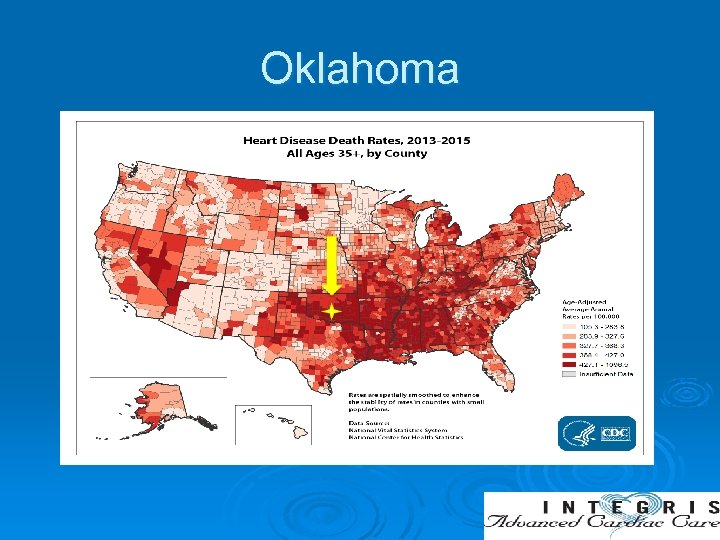
Oklahoma
Heart Failure More deaths from HF than all forms of cancer combined Ø 10% within 1 st year & 50% within 5 yrs Ø 300, 000 to 800, 000 advance HF patients in US Ø 60, 000 patients are younger than 65 yrs old Ø High morbidity, mortality, and poor quality of life Ø
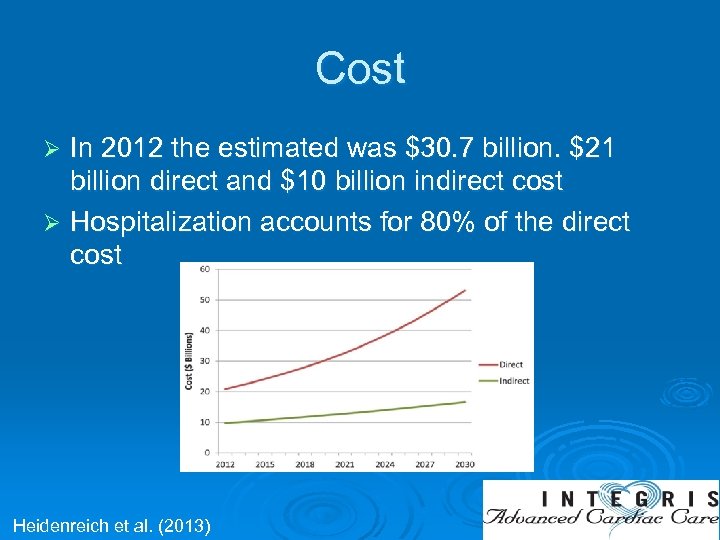
Cost In 2012 the estimated was $30. 7 billion. $21 billion direct and $10 billion indirect cost Ø Hospitalization accounts for 80% of the direct cost Ø Heidenreich et al. (2013)
Definition of Systolic HF Ø It is a complex clinical syndrome that can result from any structural or functional cardiac disorders that impairs ability of the left ventricle to ejects blood.
Classification of Heart Failure Ø Functional classification: NYHA class (I-IV) - Based on clinical signs Ø Staging of HF: ACC/AHA stages (A, B, C, D)
Management of HF HF tool box Ø Life style modification Ø Medications Ø Electrical Therapy Ø Advanced HF therapy (Transplant/ MCS)
Goals of HF Management Primary prevention Ø Control of day to day symptoms -Volume management -Congestive symptoms Ø Prevent disease progression -Decrease hospitalization -Decrease mortality -Preventricular remodeling, vascular remodeling, and activation of neurohormones (norepinephrine, angiotensin II, and aldosterone) Ø
Pharmacotherapy for Heart Failure Diuretics Ø Neurohormonal antagonists (ACEI, ARB, MRA, ARNI) Ø Digoxin Ø Ivabradine Ø Inotropics: (Phosphodiesterase Inhibitors. Milrinone and dobutamine) Ø Vasodilators (Hydralazine, Nitroglycerine & Nesiritide) Ø Yancy et al. 2013 ACC/AHA Guideline for Management of Heart Failure
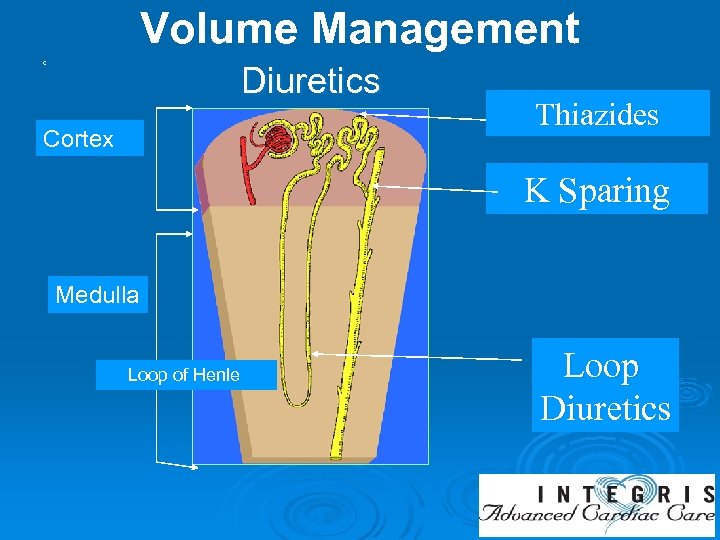
Volume Management c Diuretics Cortex Thiazides K Sparing Medulla Loop of Henle Loop Diuretics
Neurohormonal Antagonist Neurohormonal antagonists (ACEI, ARB, MRA, ARNI) Ø Change the natural history HF disease process by blocking activation of RAAS and SNS. Ø Arrest, prevent, and may even reverse the process of progressive ventricular remodeling. Ø Decrease morbidity and mortality associated with HF Ø
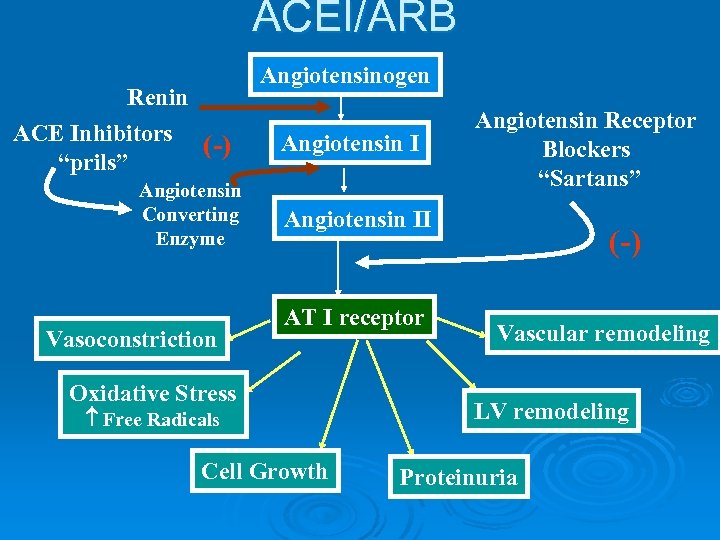
ACEI/ARB Renin ACE Inhibitors (-) “prils” Angiotensin Converting Enzyme Vasoconstriction Angiotensinogen Angiotensin I Angiotensin Receptor Blockers “Sartans” Angiotensin II AT I receptor Oxidative Stress Free Radicals Cell Growth (-) Vascular remodeling LV remodeling Proteinuria
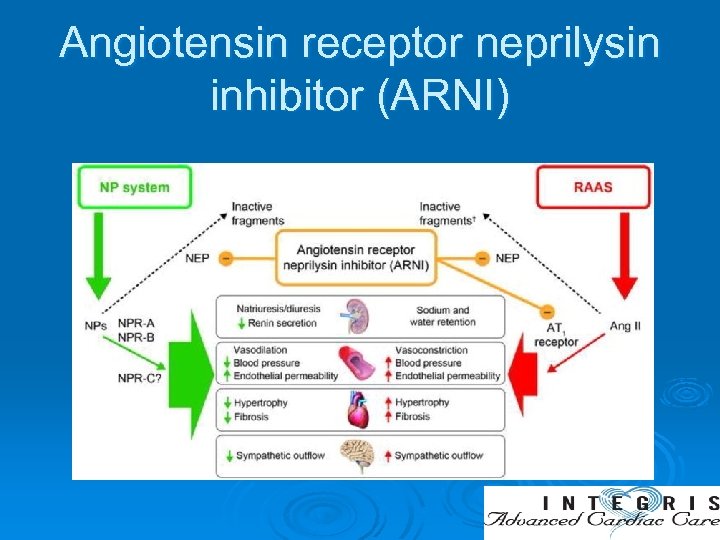
Angiotensin receptor neprilysin inhibitor (ARNI)
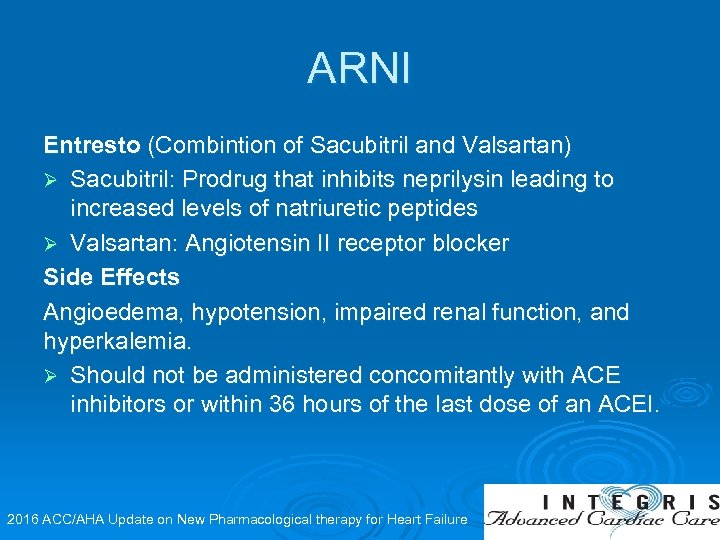
ARNI Entresto (Combintion of Sacubitril and Valsartan) Ø Sacubitril: Prodrug that inhibits neprilysin leading to increased levels of natriuretic peptides Ø Valsartan: Angiotensin II receptor blocker Side Effects Angioedema, hypotension, impaired renal function, and hyperkalemia. Ø Should not be administered concomitantly with ACE inhibitors or within 36 hours of the last dose of an ACEI. 2016 ACC/AHA Update on New Pharmacological therapy for Heart Failure
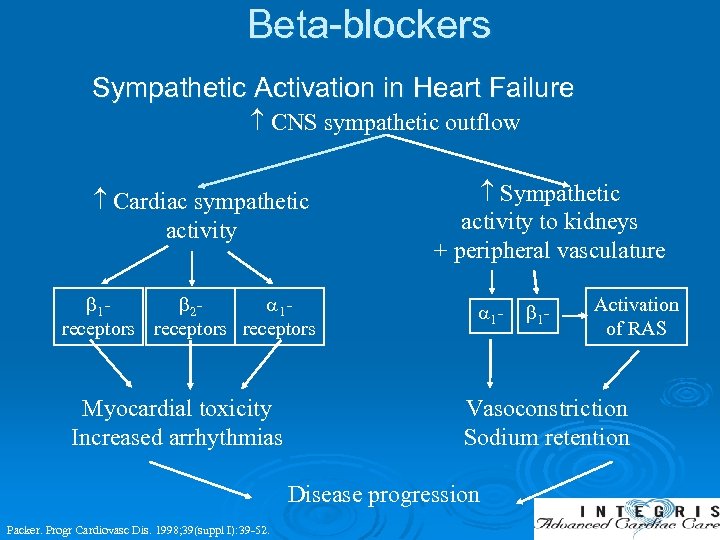
Beta-blockers Sympathetic Activation in Heart Failure CNS sympathetic outflow Cardiac sympathetic activity 1 2 1 receptors Myocardial toxicity Increased arrhythmias Sympathetic activity to kidneys + peripheral vasculature 1 - Activation of RAS Vasoconstriction Sodium retention Disease progression Packer. Progr Cardiovasc Dis. 1998; 39(suppl I): 39 -52. 1 -
Mineralocorticoid Receptor Antagonist (MRA) Effects of RAAS activation is also mediated through aldosterone. Ø Increase in aldosterone level persist in the circulation even in the presence of angiotensin II inhibition. Ø It is associated with increased myocardial fibrosis, inflammation, myocyte hypertrophy, and apoptosis. Ø MRAs inhibit aldosterone Ø
Ivabradine (Corlanor) Hyperpolarization-activated cyclic nucleotide-gated (HCN) channel blocker. Ø Reduces diastolic depolarization slope in the SA node, thereby decreasing heart rate via direct sinus node inhibition without direct effects on myocardial contractility and intracardiac conduction Ø Indicated to reduce the risk of HF hospitalization in patients with stable, symptomatic chronic HF with LVEF ≤ 35%, who are in sinus rhythm with resting heart rate ≥ 70 bpm and either are on maximally tolerated doses of betablockers or have a contraindication to beta-blocker use Ø 2016 ACC/AHA Update on New Pharmacological therapy for Heart Failure
Hydralazine and Isordil The combination of hydralazine and isosorbide dinitrate is recommended to reduce morbidity and mortality for African Americans patients with LVEF <40%, NYHA class III–IV symptoms receiving optimal therapy with ACE inhibitors and beta blockers. Ø Indicated for patients with LVEF <40% who can not tolerate ACEI/ARB secondary to renal insufficiency/impairment. Ø
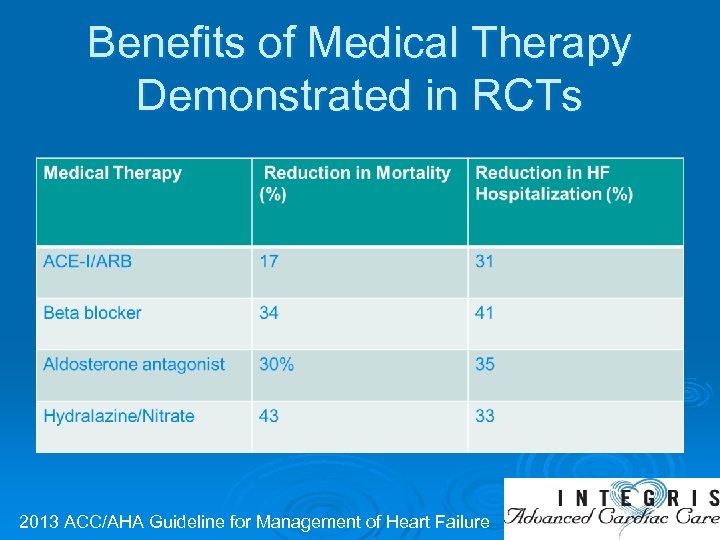
Benefits of Medical Therapy Demonstrated in RCTs 2013 ACC/AHA Guideline for Management of Heart Failure
Digoxin Ø No mortality benefit Ø Decrease hospitalization Ø Increase exercise tolerance Ø May help for rate control in patients with Afib
Drugs to Avoid in HF Ø Nonsteroidal anti-inflammatory drugs (NSAIDs) Ø Thiazolidinediones Ø Calcium channel blockers – nondihydropyridine Ø Dietary supplements Mann & Felker, 2016
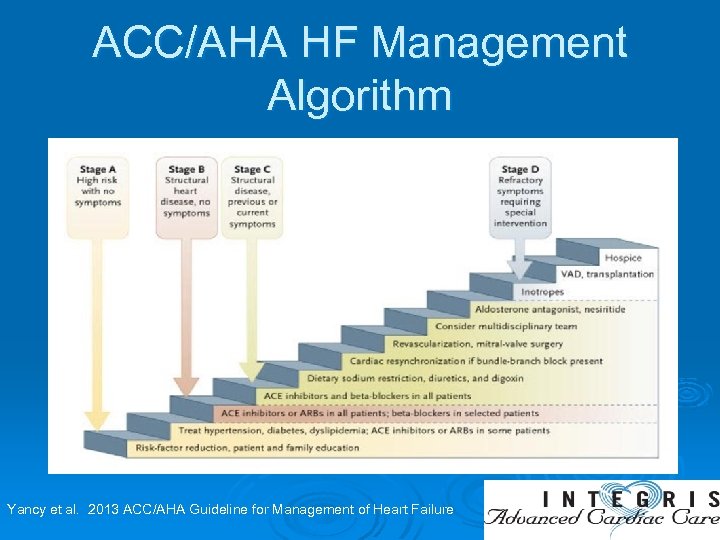
ACC/AHA HF Management Algorithm Yancy et al. 2013 ACC/AHA Guideline for Management of Heart Failure
Advanced/End Stage HF • Inability to tolerate HF medication or reduction of dose • Recurrent hospitalization • Severe exercise intolerance • Heart failure wasting syndrome • Cardiorenal syndrome • Right heart failure • Inotrope dependence
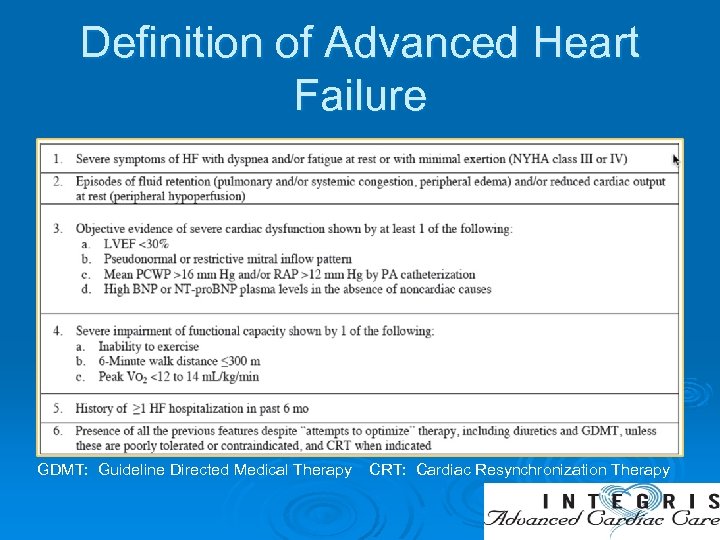
Definition of Advanced Heart Failure GDMT: Guideline Directed Medical Therapy CRT: Cardiac Resynchronization Therapy
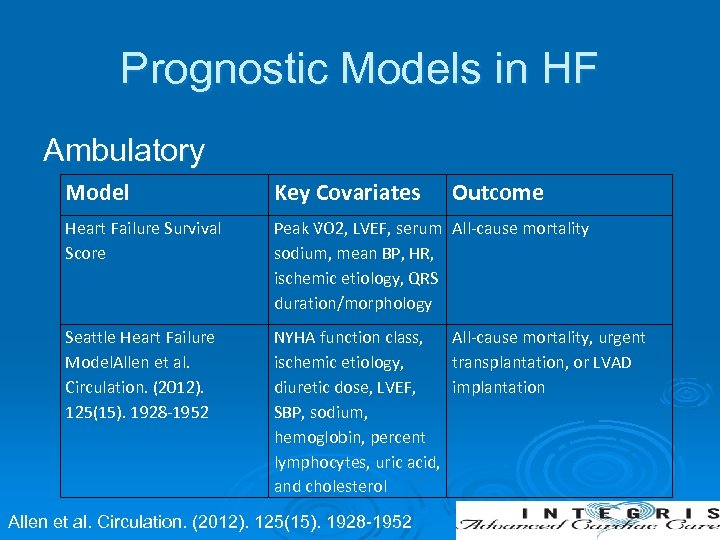
Prognostic Models in HF Ambulatory Model Key Covariates Heart Failure Survival Score Peak V O 2, LVEF, serum All-cause mortality sodium, mean BP, HR, ischemic etiology, QRS duration/morphology Seattle Heart Failure Model. Allen et al. Circulation. (2012). 125(15). 1928 -1952 NYHA function class, All-cause mortality, urgent ischemic etiology, transplantation, or LVAD diuretic dose, LVEF, implantation SBP, sodium, hemoglobin, percent lymphocytes, uric acid, and cholesterol Allen et al. Circulation. (2012). 125(15). 1928 -1952 Outcome
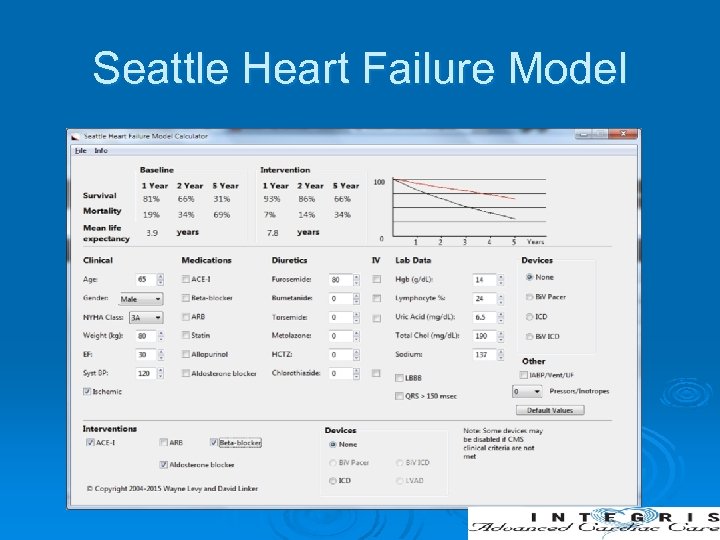
Seattle Heart Failure Model
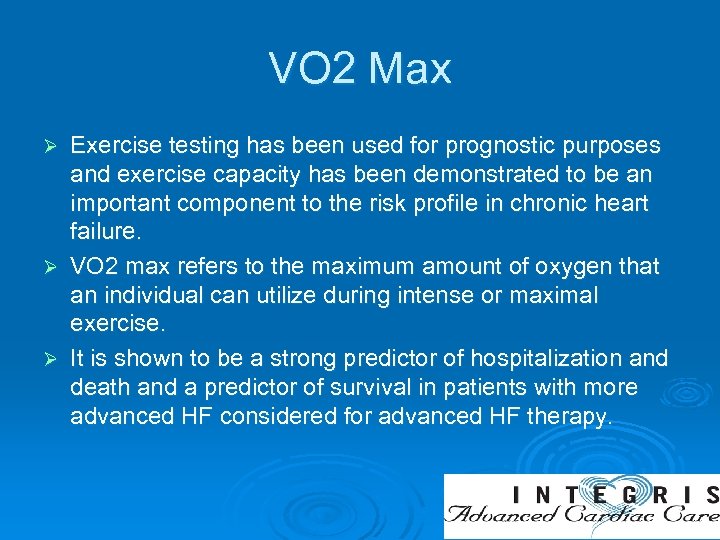
VO 2 Max Exercise testing has been used for prognostic purposes and exercise capacity has been demonstrated to be an important component to the risk profile in chronic heart failure. Ø VO 2 max refers to the maximum amount of oxygen that an individual can utilize during intense or maximal exercise. Ø It is shown to be a strong predictor of hospitalization and death and a predictor of survival in patients with more advanced HF considered for advanced HF therapy. Ø
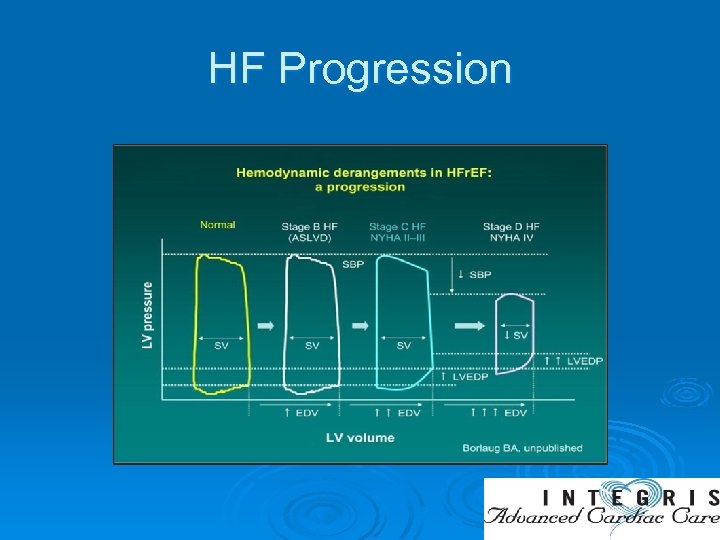
HF Progression
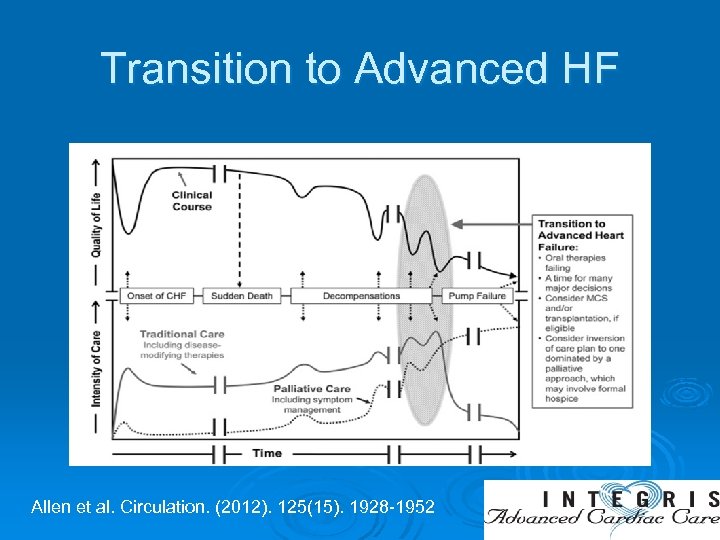
Transition to Advanced HF Allen et al. Circulation. (2012). 125(15). 1928 -1952
Advanced Heart Failure Ø Limited treatment option - Heart transplantation - Mechanical circulatory support (MCS) - Long-term inotropic therapy - Palliative care
Inotropes Indicated in the presence of acute or chronic hemodynamic compromise with end organ dysfunction. Ø Bridge to mechanical circulatory support (MCS) Ø Bridge to transplant Ø Palliative Ø
Inotropes in Advanced HF Milrinone and Dobutamine are currently the only two inotropes approved for use in the US. Ø Both increase cardiac output by increasing the intracellular level of cyclic adenosine monophosphate (c. AMP) Ø Dobutamine increases c. AMP indirectly through adrenergic agonism. Ø Milrinone, a phosphodiesterase inhibitor, directly blocks c. AMP breakdown Ø
Dobutamine Sympathomimetic amine, which acts on beta-1, beta-2, and alpha-1 adrenergic receptors. Ø Strong inotropic effect and relatively weak chronotropic effect Ø No significant change in BP due to its alpha-1 agonist activity causing vasoconstriction, that balances the beta-2 vasodilatory effect. Ø The use is problematic in patients who take beta blockers due to its adrenergic properties Ø
Milrinone inhibits phosphodiesterase 3 (PDE 3), which prevents the degradation of c. AMP and ultimately leads to an increase in protein kinase A (PKA). Ø It is an inodilator, both increasing cardiac contractility and reducing afterload with a consequent reduction in left ventricular filling pressures. Ø PKA increases contractility of the left ventricle and cardiac output through c. AMP dependent-PKA Ø
Milrinone Less myocardial oxygen consumption with milrinone when compared to dobutamine. Ø Can be used in patients on beta blockers, because its effects are not dependent on beta adrenoreceptors. Ø Milrinone not only acts as a systemic but also a pulmonary vasodilator. Ø It is the preferred agent in patients with pulmonary hypertension and HF. Ø
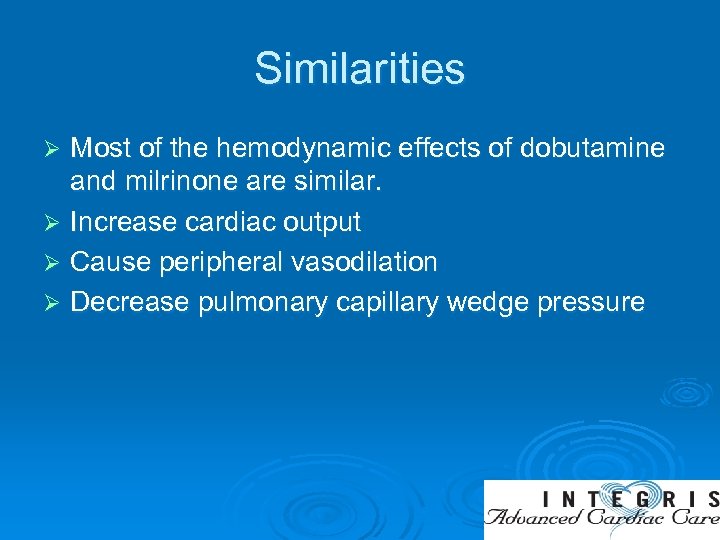
Similarities Most of the hemodynamic effects of dobutamine and milrinone are similar. Ø Increase cardiac output Ø Cause peripheral vasodilation Ø Decrease pulmonary capillary wedge pressure Ø
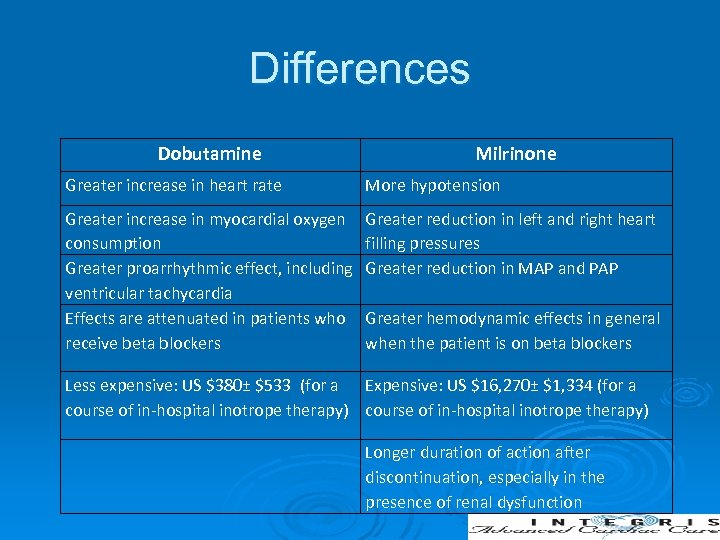
Differences Dobutamine Milrinone Greater increase in heart rate More hypotension Greater increase in myocardial oxygen consumption Greater proarrhythmic effect, including ventricular tachycardia Effects are attenuated in patients who receive beta blockers Greater reduction in left and right heart filling pressures Greater reduction in MAP and PAP Greater hemodynamic effects in general when the patient is on beta blockers Less expensive: US $380± $533 (for a Expensive: US $16, 270± $1, 334 (for a course of in-hospital inotrope therapy) Longer duration of action after discontinuation, especially in the presence of renal dysfunction
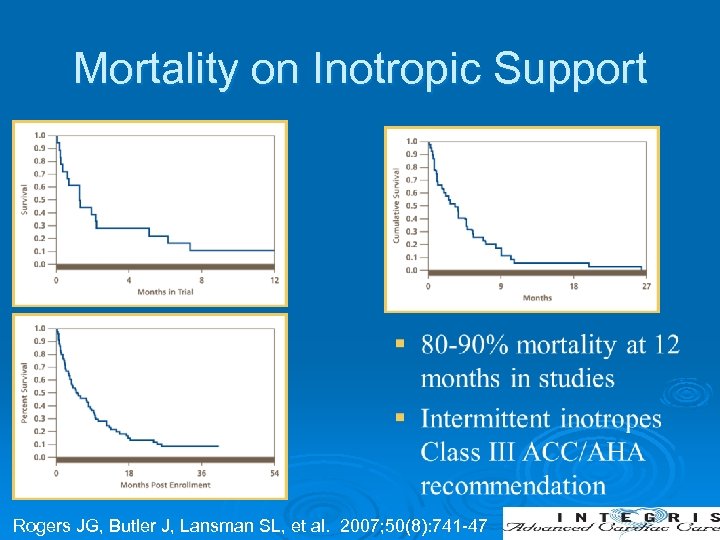
Mortality on Inotropic Support Rogers JG, Butler J, Lansman SL, et al. 2007; 50(8): 741 -47

Advanced HF therapies Ø Cardiac Transplantation Ø Mechanical Circulatory support
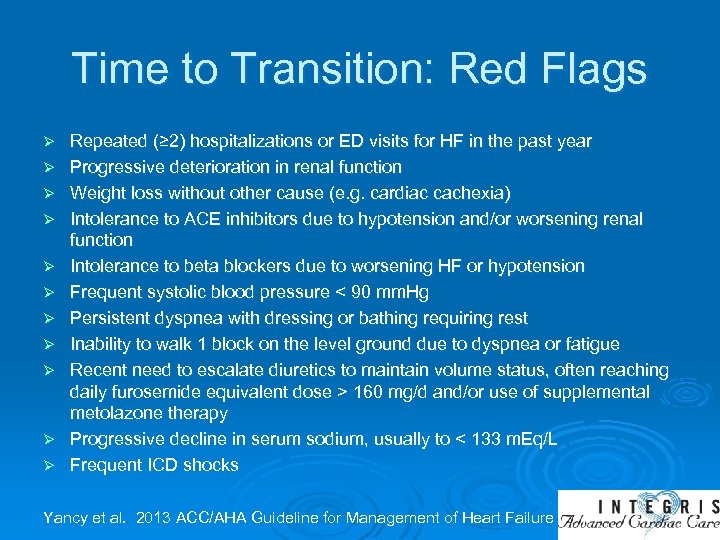
Time to Transition: Red Flags Ø Ø Ø Repeated (≥ 2) hospitalizations or ED visits for HF in the past year Progressive deterioration in renal function Weight loss without other cause (e. g. cardiac cachexia) Intolerance to ACE inhibitors due to hypotension and/or worsening renal function Intolerance to beta blockers due to worsening HF or hypotension Frequent systolic blood pressure < 90 mm. Hg Persistent dyspnea with dressing or bathing requiring rest Inability to walk 1 block on the level ground due to dyspnea or fatigue Recent need to escalate diuretics to maintain volume status, often reaching daily furosemide equivalent dose > 160 mg/d and/or use of supplemental metolazone therapy Progressive decline in serum sodium, usually to < 133 m. Eq/L Frequent ICD shocks Yancy et al. 2013 ACC/AHA Guideline for Management of Heart Failure
Cardiac Transplantation Ø Ideal treatment for advanced HF Ø Provides increased longevity and symptomatic relief Ø Approximately 3, 000 people are on waiting list at any given time Ø In 2015, there was only 2804 donors in US United Network for Organ Sharing [UNOS] (2017)
Listing criteria for Heart transplantation Ø Ø Ø Cardiopulmonary exercise testing: VO 2 max <14 ml/kg/min if patients intolerant to BB; <12 ml/kg/min in the presence f BB; or <50% of predicted VO 2 in young patients (50 yrs) and women. Acceptable pulmonary artery pressure Age <70 Diabetes well controlled Absence on neoplasm Psychosocial support
Contraindication Ø Ø Ø Noncompliance with medical regimen Active substance abuse Severe symptomatic cerebrovascular disease Severe organ dysfunction (lung, kidney, liver, coagulopathy) Active infection Active mental illness Inadequate social support Fixed, severe pulmonary hypertension Morbid obesity (BMI > 35 kg/m 2) Age > 70 years Recent or uncured malignancy
Transplant Listing Each US transplant center is part of the nationwide United Network of Organ Sharing (UNOS), which is divided into eleven regions, each with specific local organ procurement organizations (OPO) Ø Patients are listed by OPO, transplant center, and ABO blood type, and prioritized by medical urgency (UNOS Status). Ø Medical urgency status: 1 A, 1 B, 2, 7 Ø
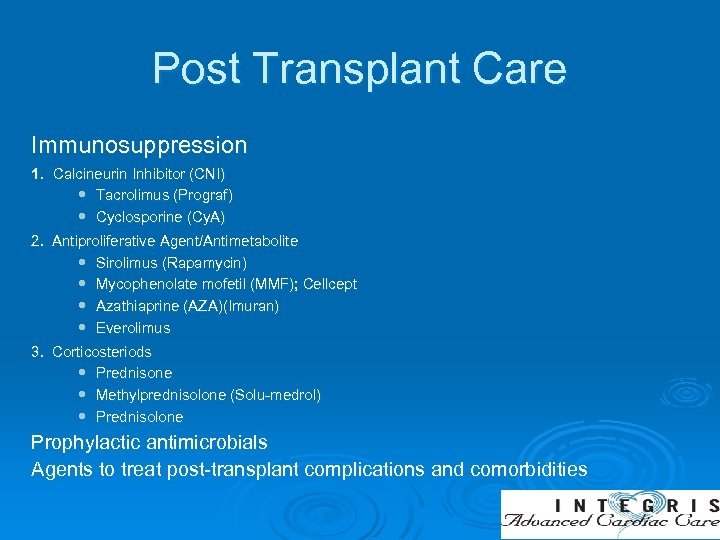
Post Transplant Care Immunosuppression 1. Calcineurin Inhibitor (CNI) Tacrolimus (Prograf) Cyclosporine (Cy. A) 2. Antiproliferative Agent/Antimetabolite Sirolimus (Rapamycin) Mycophenolate mofetil (MMF); Cellcept Azathiaprine (AZA)(Imuran) Everolimus 3. Corticosteriods Prednisone Methylprednisolone (Solu-medrol) Prednisolone Prophylactic antimicrobials Agents to treat post-transplant complications and comorbidities
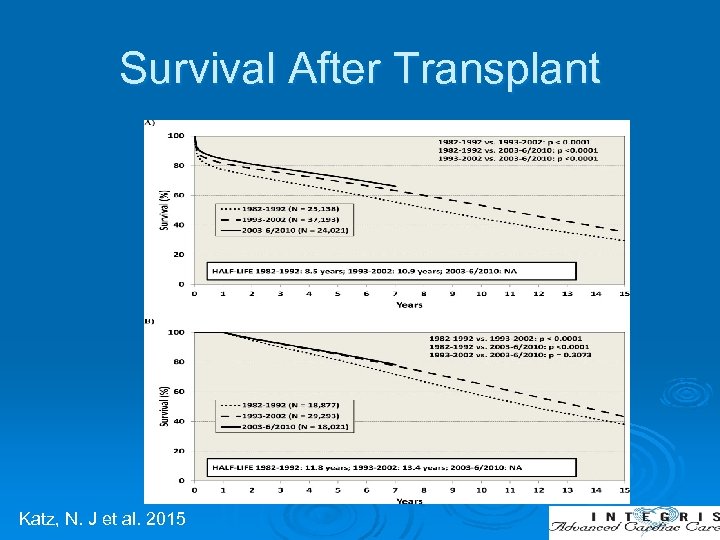
Survival After Transplant Katz, N. J et al. 2015
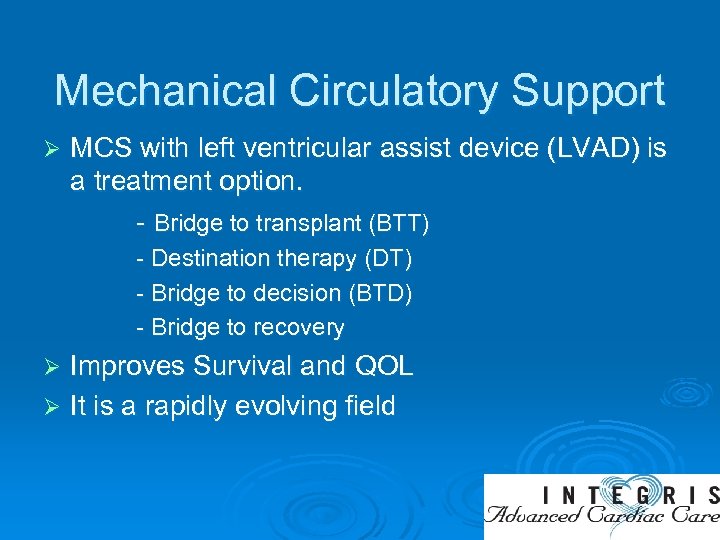
Mechanical Circulatory Support Ø MCS with left ventricular assist device (LVAD) is a treatment option. - Bridge to transplant (BTT) - Destination therapy (DT) - Bridge to decision (BTD) - Bridge to recovery Improves Survival and QOL Ø It is a rapidly evolving field Ø
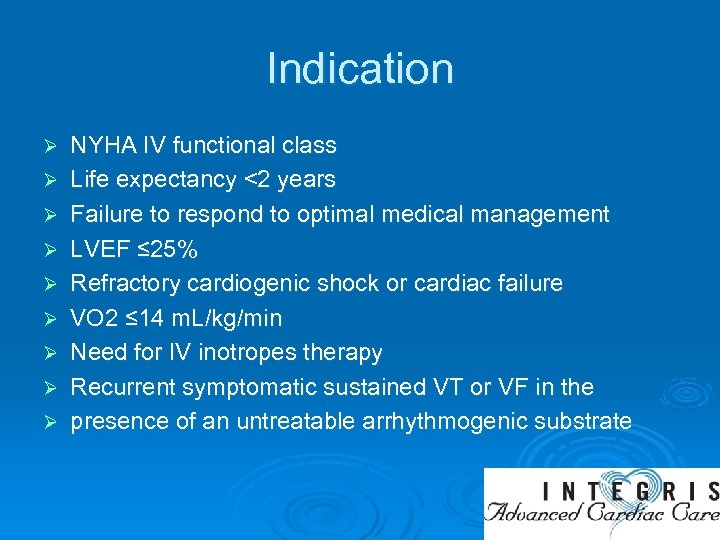
Indication Ø Ø Ø Ø Ø NYHA IV functional class Life expectancy <2 years Failure to respond to optimal medical management LVEF ≤ 25% Refractory cardiogenic shock or cardiac failure VO 2 ≤ 14 m. L/kg/min Need for IV inotropes therapy Recurrent symptomatic sustained VT or VF in the presence of an untreatable arrhythmogenic substrate
Exclusion Criteria Active systemic infection Ø Uncorrectable aortic insufficiency Ø Renal insufficiency that may require dialysis in the near future Ø History of cardiac transplant Ø Any condition, other than heart failure, which is expected to limit survival to less than 2 years Ø
INTERMACS Profiles of Advanced Heart Failure Ø Ø Ø Ø Profile 1: Critical cardiogenic shock Profile 2: Progressive decline- sliding on inotrope Profile 3: Stable but inotrope dependent Profile 4: Resting symptoms Profile 5: Exertion Intolerant Profile 6: Exertion Limited Profile 7: Advanced NYHA Class 3
Types of MCS Ø Left ventricular assist device (LVAD) Ø Biventricular support (Bi. VAD) Ø Total artificial heart (TAH)
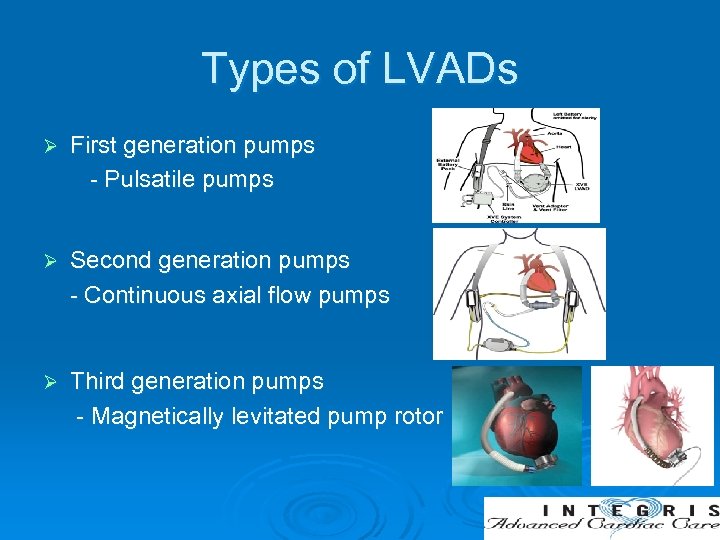
Types of LVADs Ø First generation pumps - Pulsatile pumps Ø Second generation pumps - Continuous axial flow pumps Ø Third generation pumps - Magnetically levitated pump rotor

Commonly Used Durable LVADs HVAD Centrifugal LVAD Magnetic Drive Hemodynamic Bearing Heart. Mate II Axial Flow LVAD Ruby Bearing Heart. Mate 3 Centrifugal LVAD Magnetic Levitation No Bearing
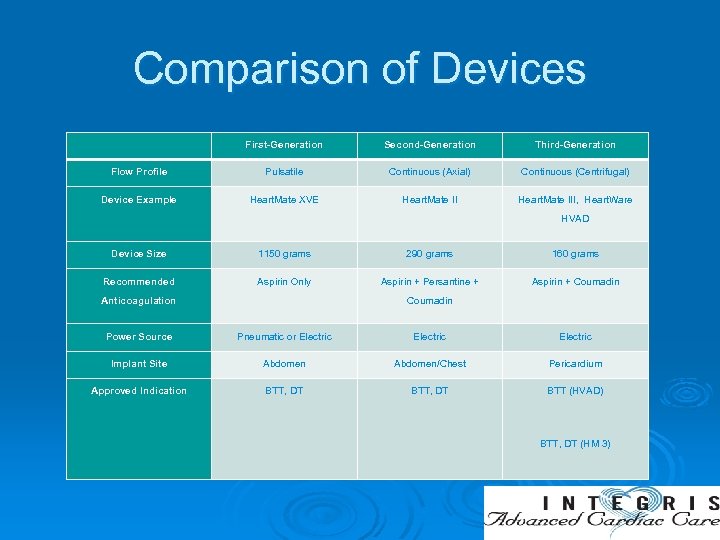
Comparison of Devices First-Generation Second-Generation Third-Generation Flow Profile Pulsatile Continuous (Axial) Continuous (Centrifugal) Device Example Heart. Mate XVE Heart. Mate III, Heart. Ware HVAD Device Size 1150 grams 290 grams 160 grams Recommended Aspirin Only Aspirin + Persantine + Aspirin + Coumadin Anticoagulation Coumadin Power Source Pneumatic or Electric Implant Site Abdomen/Chest Pericardium Approved Indication BTT, DT BTT (HVAD) BTT, DT (HM 3)
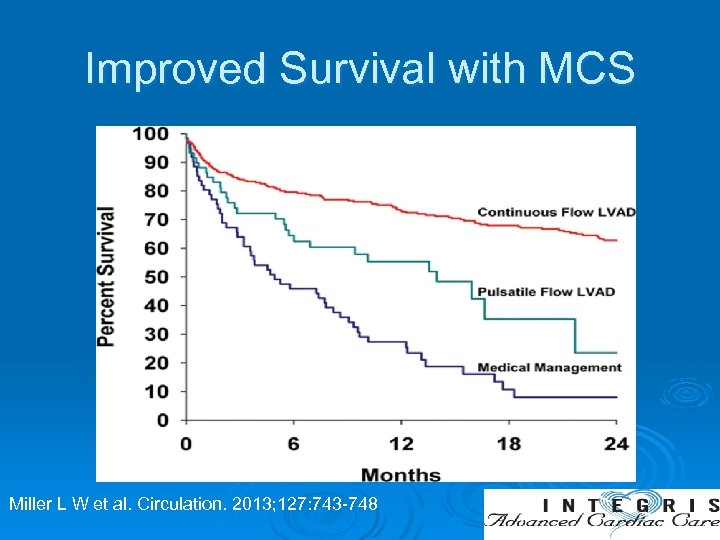
Improved Survival with MCS Miller L W et al. Circulation. 2013; 127: 743 -748
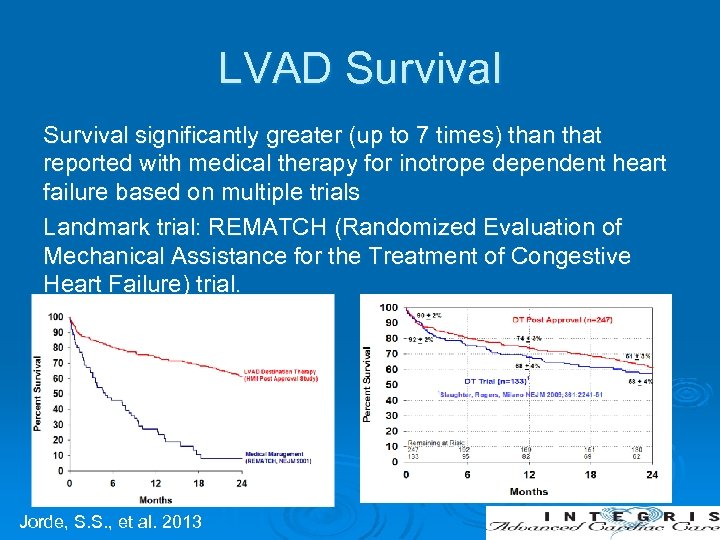
LVAD Survival significantly greater (up to 7 times) than that reported with medical therapy for inotrope dependent heart failure based on multiple trials Landmark trial: REMATCH (Randomized Evaluation of Mechanical Assistance for the Treatment of Congestive Heart Failure) trial. Jorde, S. S. , et al. 2013
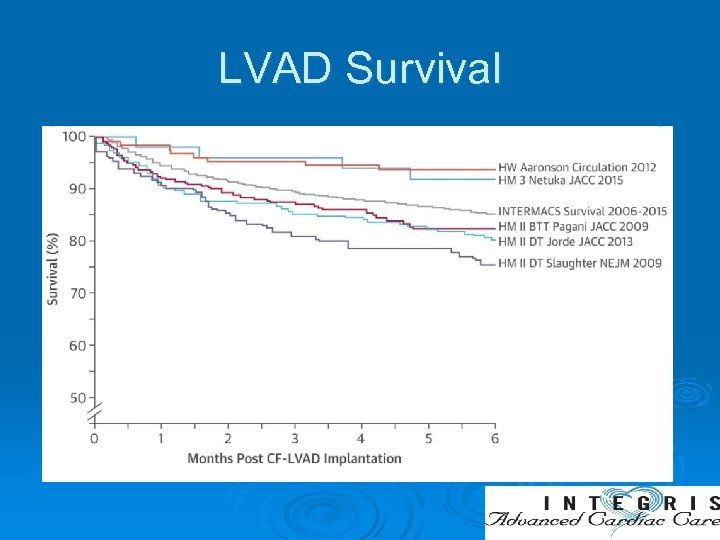
LVAD Survival
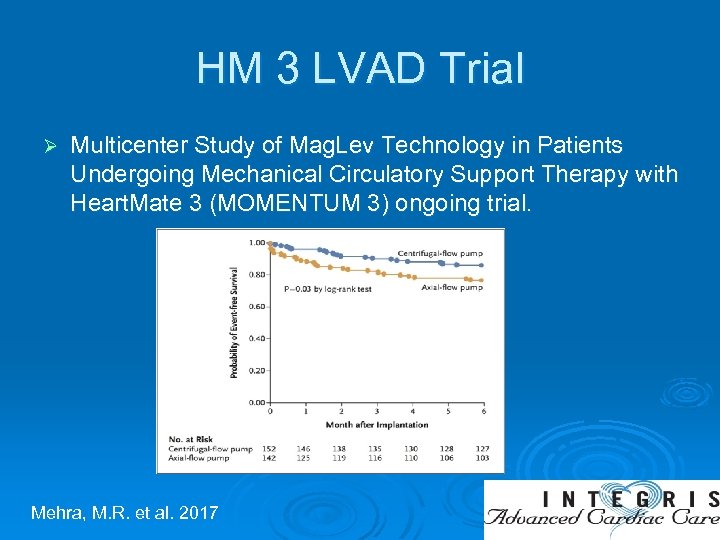
HM 3 LVAD Trial Ø Multicenter Study of Mag. Lev Technology in Patients Undergoing Mechanical Circulatory Support Therapy with Heart. Mate 3 (MOMENTUM 3) ongoing trial. Mehra, M. R. et al. 2017

Improved Outcomes Ø Improvements in patient selection Ø Improvements in technology Ø Improvements in patient management
Anti-Coagulation Guidelines Medications Aspirin – prevents platelet aggregation Ø Persantine – prevents platelet aggregation Ø Plavix/Effient- occasionally used for platelet aggregation Ø Coumadin- required, goal INR depends on patients underlying comorbidities Heart. Mate II: Aspirin + Persantine or Plavix/Effient + Coumadin Heart. Mate 3: Aspirin + Coumadin Ø
Complication with LVAD Ø Infections Ø Bleeding Ø Hemolysis Ø Thrombosis Ø Stroke Ø Aortic insufficiency

Key Success Ø Patient selection Ø Patient management Ø Multidisciplinary approach Ø Psychosocial support
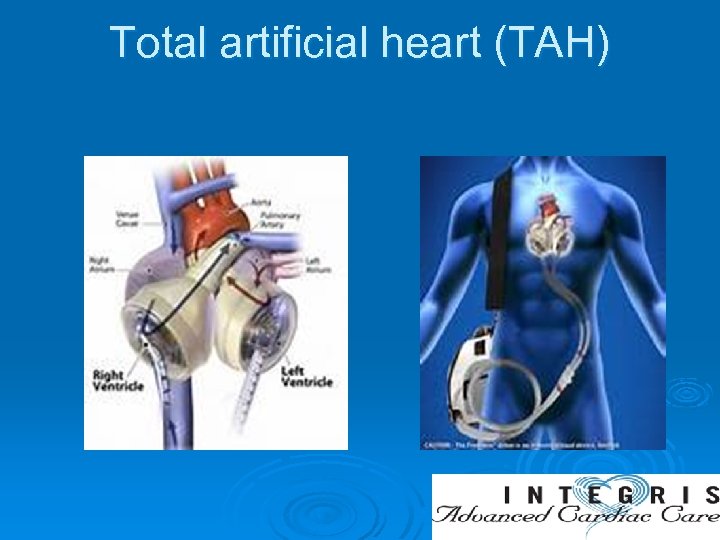
Total artificial heart (TAH)
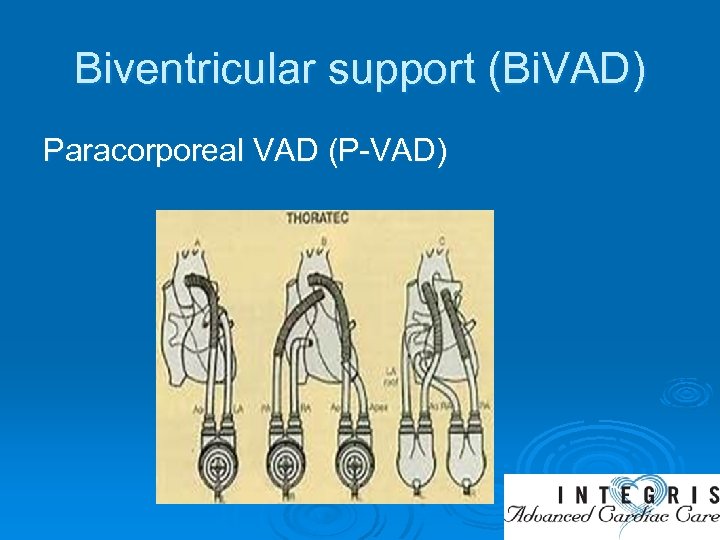
Biventricular support (Bi. VAD) Paracorporeal VAD (P-VAD)
Summary Advanced heart failure patients has limited treatment options. Ø Timely referral of end stage HF patients to advanced HF center is essential for success. Ø Heart transplantation is the ideal therapy for refractory end stage HF. However organ shortage limits therapy. Ø RCTs have demonstrated benefits LVADs in reducing mortality and improving QOL. Ø
507458d188893903e43f229974d60684.ppt