408e69689007c212b3a774597b7ac639.ppt
- Количество слайдов: 56
 Adult vaccination Dewald Steyn Department of Internal Medicine UFS
Adult vaccination Dewald Steyn Department of Internal Medicine UFS
 When to vaccinate? 1. Routine - children 2. High risk groups - adults 3. Travel – both children & adults
When to vaccinate? 1. Routine - children 2. High risk groups - adults 3. Travel – both children & adults
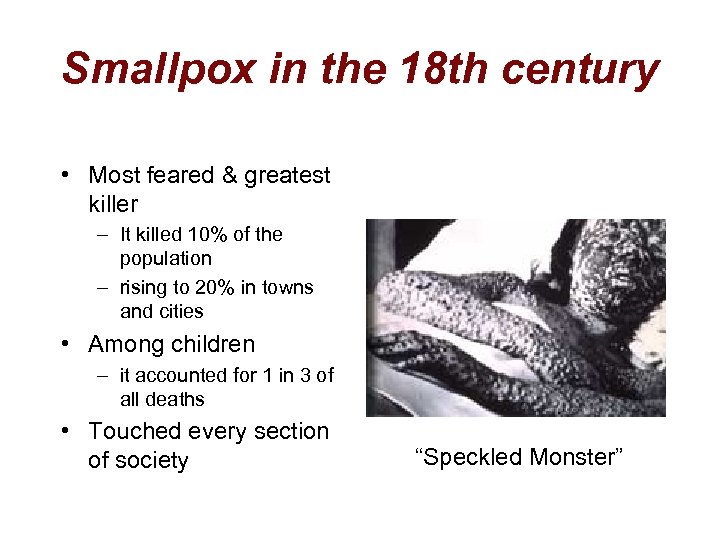 Smallpox in the 18 th century • Most feared & greatest killer – It killed 10% of the population – rising to 20% in towns and cities • Among children – it accounted for 1 in 3 of all deaths • Touched every section of society “Speckled Monster”
Smallpox in the 18 th century • Most feared & greatest killer – It killed 10% of the population – rising to 20% in towns and cities • Among children – it accounted for 1 in 3 of all deaths • Touched every section of society “Speckled Monster”
 Edward Jenner • vaccination with cowpox prevented the deadly smallpox 1749 -1823
Edward Jenner • vaccination with cowpox prevented the deadly smallpox 1749 -1823
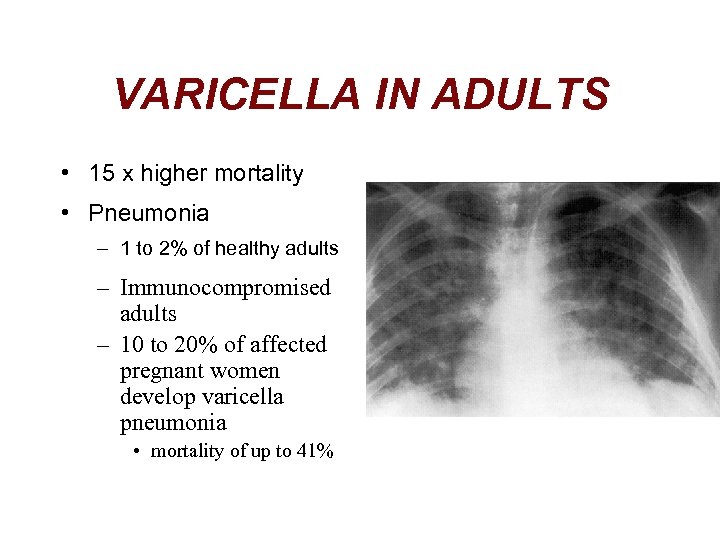 VARICELLA IN ADULTS • 15 x higher mortality • Pneumonia – 1 to 2% of healthy adults – Immunocompromised adults – 10 to 20% of affected pregnant women develop varicella pneumonia • mortality of up to 41%
VARICELLA IN ADULTS • 15 x higher mortality • Pneumonia – 1 to 2% of healthy adults – Immunocompromised adults – 10 to 20% of affected pregnant women develop varicella pneumonia • mortality of up to 41%
 Recommendations for varicella vaccine • All susceptible immuno-compromised individuals – who have retained a moderate degree of immune function • Women in the childbearing age group who never had chickenpox • All susceptible healthcare workers • Healthy adults who are exposed to children • Dose – live attenuated vaccine – > 1 year (single dose) – > 13 y (2 doses, 1 month apart)
Recommendations for varicella vaccine • All susceptible immuno-compromised individuals – who have retained a moderate degree of immune function • Women in the childbearing age group who never had chickenpox • All susceptible healthcare workers • Healthy adults who are exposed to children • Dose – live attenuated vaccine – > 1 year (single dose) – > 13 y (2 doses, 1 month apart)
 Varicella Post-exposure prophylaxis: 1. VZIG § 6 ml (3 ampoules) given imi – to all pregnant women or immuno-suppressed patients • who are exposed to varicella and who may lack antibodies to the virus (only 25% are truly susceptible) – as soon as possible after exposure • even up to 96 hours after exposure – the primary indication for VZIG in pregnant women is to prevent complications of varicella in the mother, rather than to protect the foetus
Varicella Post-exposure prophylaxis: 1. VZIG § 6 ml (3 ampoules) given imi – to all pregnant women or immuno-suppressed patients • who are exposed to varicella and who may lack antibodies to the virus (only 25% are truly susceptible) – as soon as possible after exposure • even up to 96 hours after exposure – the primary indication for VZIG in pregnant women is to prevent complications of varicella in the mother, rather than to protect the foetus
 Varicella Post-exposure prophylaxis: 2. Post-exposure administration of ACYCLOVIR – Effective in aborting VZV infections provided that the timing is correct – must be given relatively late in the incubation period - 7 to 9 days after exposure 3. VARICELLA VACCINE – healthy individual within about 48 to 72 hours after an exposure – you can prevent varicella • • Given within 36 hours: 90% chance of preventing varicella Given within 72 hours: 75% chance of preventing varicella
Varicella Post-exposure prophylaxis: 2. Post-exposure administration of ACYCLOVIR – Effective in aborting VZV infections provided that the timing is correct – must be given relatively late in the incubation period - 7 to 9 days after exposure 3. VARICELLA VACCINE – healthy individual within about 48 to 72 hours after an exposure – you can prevent varicella • • Given within 36 hours: 90% chance of preventing varicella Given within 72 hours: 75% chance of preventing varicella
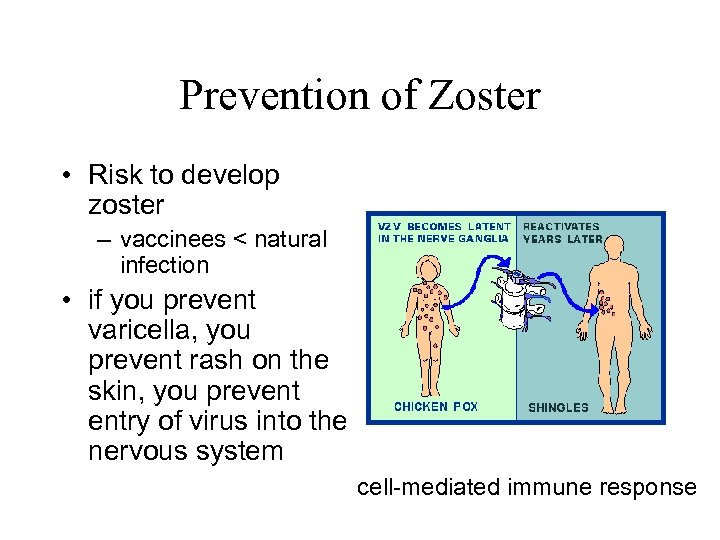 Prevention of Zoster • Risk to develop zoster – vaccinees < natural infection • if you prevent varicella, you prevent rash on the skin, you prevent entry of virus into the nervous system cell-mediated immune response
Prevention of Zoster • Risk to develop zoster – vaccinees < natural infection • if you prevent varicella, you prevent rash on the skin, you prevent entry of virus into the nervous system cell-mediated immune response
 Rabies + Tetanus • 100% FATAL but also • 100% PREVENTABLE – Human rabies immune globulin (HRIG) – Human diploid cell vaccine • Tetanus toxoid /TIG
Rabies + Tetanus • 100% FATAL but also • 100% PREVENTABLE – Human rabies immune globulin (HRIG) – Human diploid cell vaccine • Tetanus toxoid /TIG
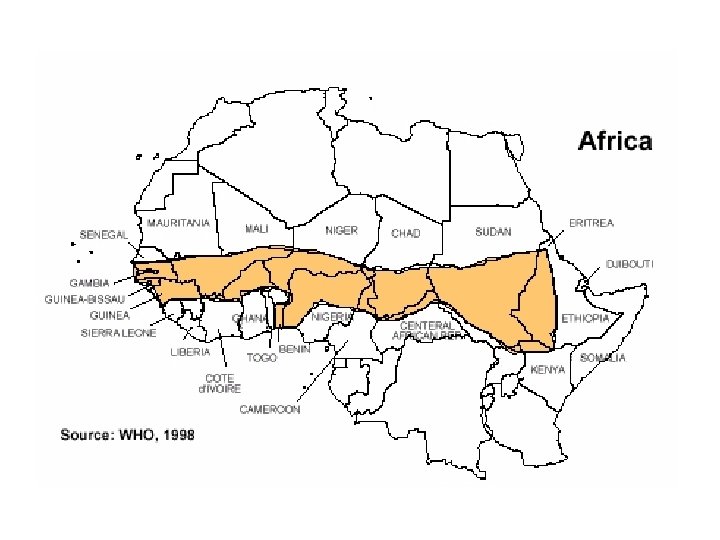
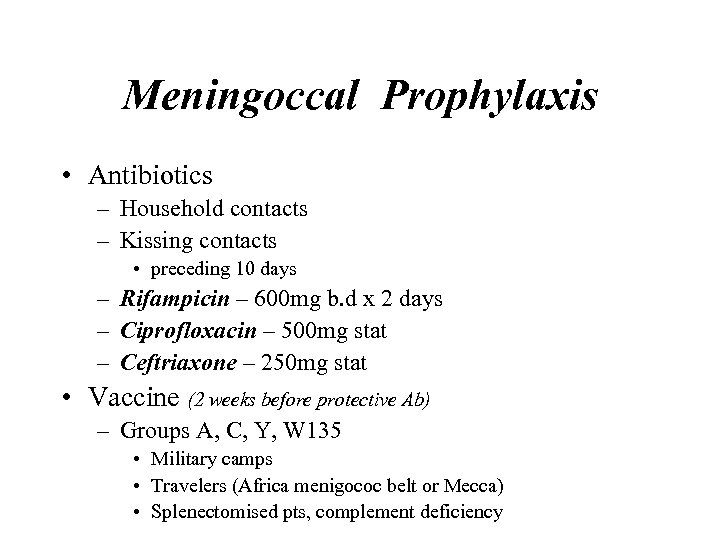 Meningoccal Prophylaxis • Antibiotics – Household contacts – Kissing contacts • preceding 10 days – Rifampicin – 600 mg b. d x 2 days – Ciprofloxacin – 500 mg stat – Ceftriaxone – 250 mg stat • Vaccine (2 weeks before protective Ab) – Groups A, C, Y, W 135 • Military camps • Travelers (Africa menigococ belt or Mecca) • Splenectomised pts, complement deficiency
Meningoccal Prophylaxis • Antibiotics – Household contacts – Kissing contacts • preceding 10 days – Rifampicin – 600 mg b. d x 2 days – Ciprofloxacin – 500 mg stat – Ceftriaxone – 250 mg stat • Vaccine (2 weeks before protective Ab) – Groups A, C, Y, W 135 • Military camps • Travelers (Africa menigococ belt or Mecca) • Splenectomised pts, complement deficiency
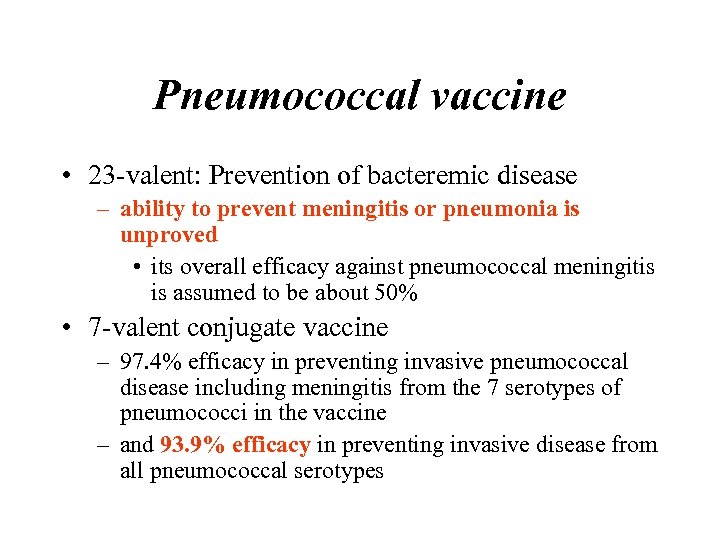 Pneumococcal vaccine • 23 -valent: Prevention of bacteremic disease – ability to prevent meningitis or pneumonia is unproved • its overall efficacy against pneumococcal meningitis is assumed to be about 50% • 7 -valent conjugate vaccine – 97. 4% efficacy in preventing invasive pneumococcal disease including meningitis from the 7 serotypes of pneumococci in the vaccine – and 93. 9% efficacy in preventing invasive disease from all pneumococcal serotypes
Pneumococcal vaccine • 23 -valent: Prevention of bacteremic disease – ability to prevent meningitis or pneumonia is unproved • its overall efficacy against pneumococcal meningitis is assumed to be about 50% • 7 -valent conjugate vaccine – 97. 4% efficacy in preventing invasive pneumococcal disease including meningitis from the 7 serotypes of pneumococci in the vaccine – and 93. 9% efficacy in preventing invasive disease from all pneumococcal serotypes
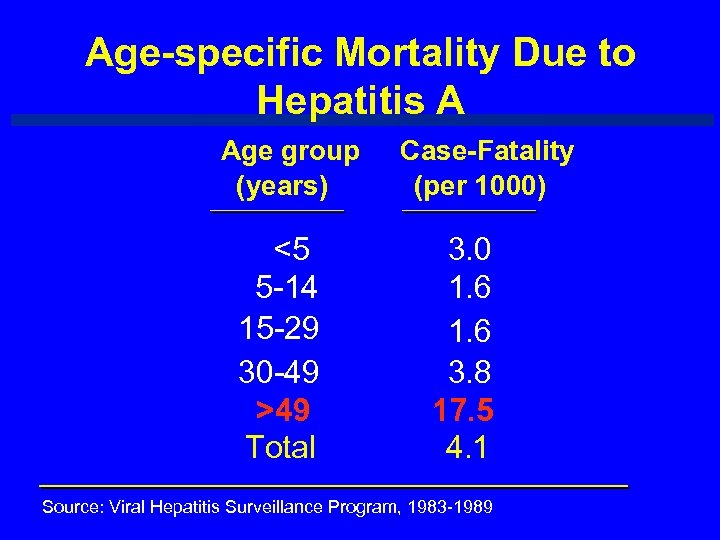 Age-specific Mortality Due to Hepatitis A Age group (years) <5 5 -14 15 -29 30 -49 >49 Total Case-Fatality (per 1000) 3. 0 1. 6 3. 8 17. 5 4. 1 Source: Viral Hepatitis Surveillance Program, 1983 -1989
Age-specific Mortality Due to Hepatitis A Age group (years) <5 5 -14 15 -29 30 -49 >49 Total Case-Fatality (per 1000) 3. 0 1. 6 3. 8 17. 5 4. 1 Source: Viral Hepatitis Surveillance Program, 1983 -1989
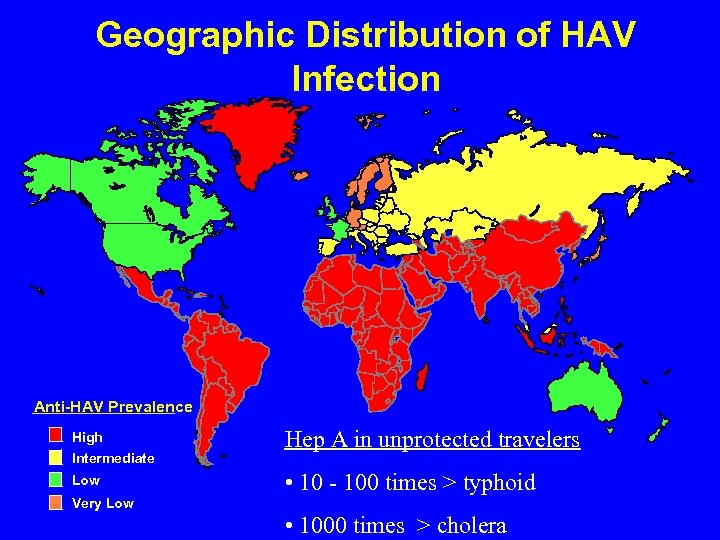 Geographic Distribution of HAV Infection Anti-HAV Prevalence High Intermediate Low Hep A in unprotected travelers • 10 - 100 times > typhoid Very Low • 1000 times > cholera
Geographic Distribution of HAV Infection Anti-HAV Prevalence High Intermediate Low Hep A in unprotected travelers • 10 - 100 times > typhoid Very Low • 1000 times > cholera
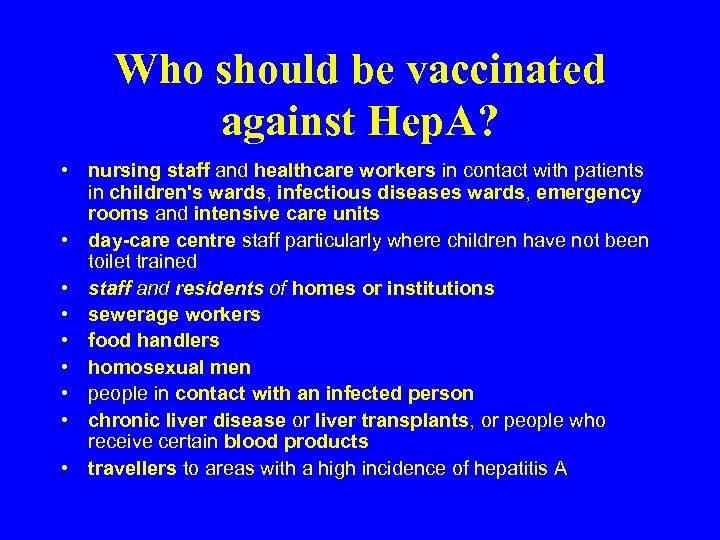 Who should be vaccinated against Hep. A? • nursing staff and healthcare workers in contact with patients in children's wards, infectious diseases wards, emergency rooms and intensive care units • day-care centre staff particularly where children have not been toilet trained • staff and residents of homes or institutions • sewerage workers • food handlers • homosexual men • people in contact with an infected person • chronic liver disease or liver transplants, or people who receive certain blood products • travellers to areas with a high incidence of hepatitis A
Who should be vaccinated against Hep. A? • nursing staff and healthcare workers in contact with patients in children's wards, infectious diseases wards, emergency rooms and intensive care units • day-care centre staff particularly where children have not been toilet trained • staff and residents of homes or institutions • sewerage workers • food handlers • homosexual men • people in contact with an infected person • chronic liver disease or liver transplants, or people who receive certain blood products • travellers to areas with a high incidence of hepatitis A
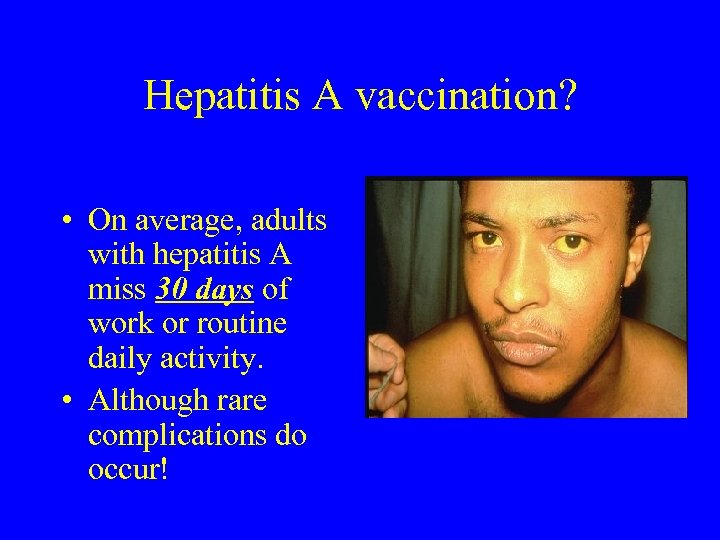 Hepatitis A vaccination? • On average, adults with hepatitis A miss 30 days of work or routine daily activity. • Although rare complications do occur!
Hepatitis A vaccination? • On average, adults with hepatitis A miss 30 days of work or routine daily activity. • Although rare complications do occur!
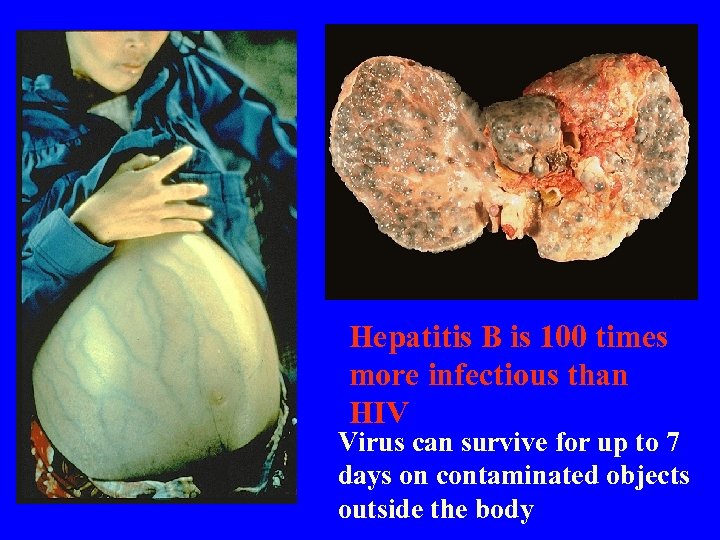 Hepatitis B is 100 times more infectious than HIV Virus can survive for up to 7 days on contaminated objects outside the body
Hepatitis B is 100 times more infectious than HIV Virus can survive for up to 7 days on contaminated objects outside the body
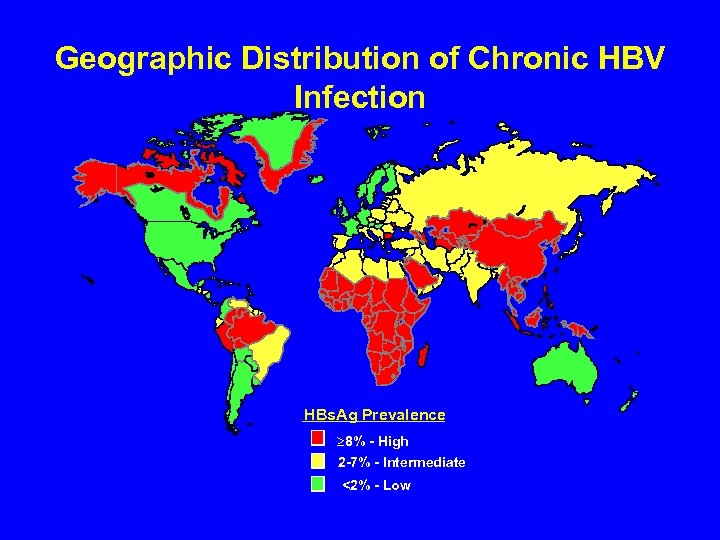 Geographic Distribution of Chronic HBV Infection HBs. Ag Prevalence ³ 8% - High 2 -7% - Intermediate <2% - Low
Geographic Distribution of Chronic HBV Infection HBs. Ag Prevalence ³ 8% - High 2 -7% - Intermediate <2% - Low
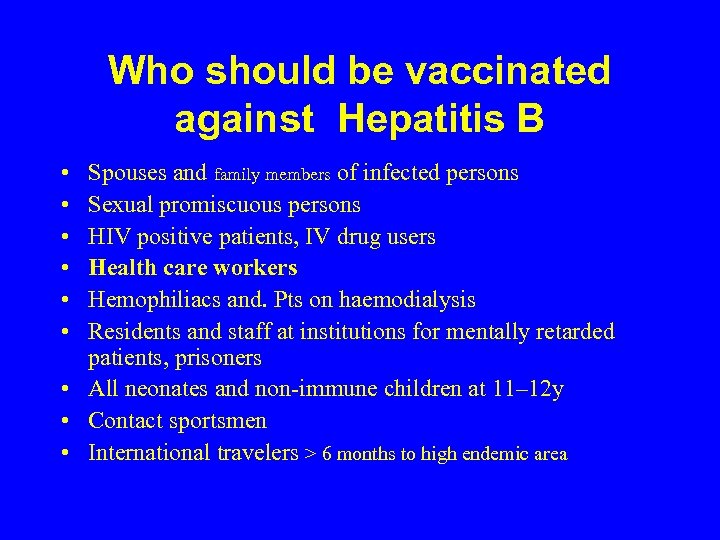 Who should be vaccinated against Hepatitis B • • • Spouses and family members of infected persons Sexual promiscuous persons HIV positive patients, IV drug users Health care workers Hemophiliacs and. Pts on haemodialysis Residents and staff at institutions for mentally retarded patients, prisoners • All neonates and non-immune children at 11– 12 y • Contact sportsmen • International travelers > 6 months to high endemic area
Who should be vaccinated against Hepatitis B • • • Spouses and family members of infected persons Sexual promiscuous persons HIV positive patients, IV drug users Health care workers Hemophiliacs and. Pts on haemodialysis Residents and staff at institutions for mentally retarded patients, prisoners • All neonates and non-immune children at 11– 12 y • Contact sportsmen • International travelers > 6 months to high endemic area
 Protective Antibody level? • Anti-HBs > 10 IU/L • Need for booster dose? – (7 to 10 years)
Protective Antibody level? • Anti-HBs > 10 IU/L • Need for booster dose? – (7 to 10 years)
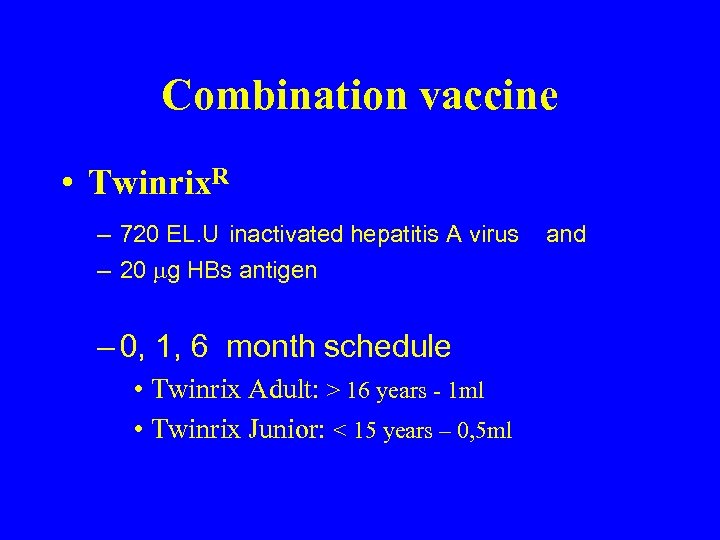 Combination vaccine • Twinrix. R – 720 EL. U inactivated hepatitis A virus – 20 g HBs antigen – 0, 1, 6 month schedule • Twinrix Adult: > 16 years - 1 ml • Twinrix Junior: < 15 years – 0, 5 ml and
Combination vaccine • Twinrix. R – 720 EL. U inactivated hepatitis A virus – 20 g HBs antigen – 0, 1, 6 month schedule • Twinrix Adult: > 16 years - 1 ml • Twinrix Junior: < 15 years – 0, 5 ml and
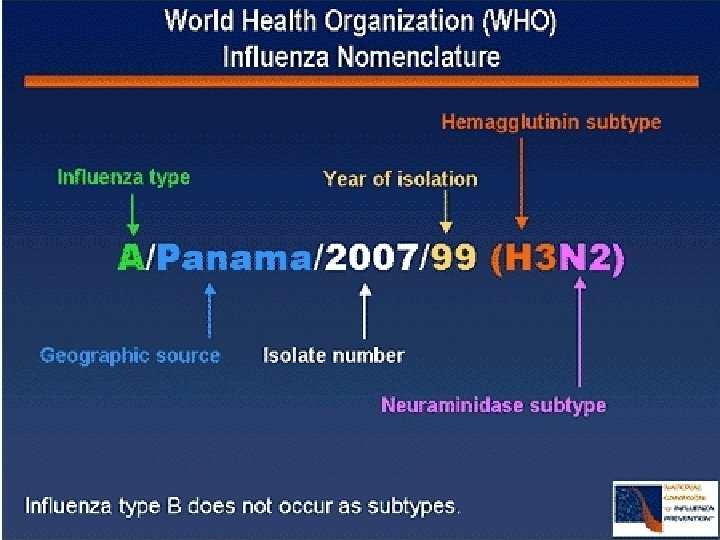
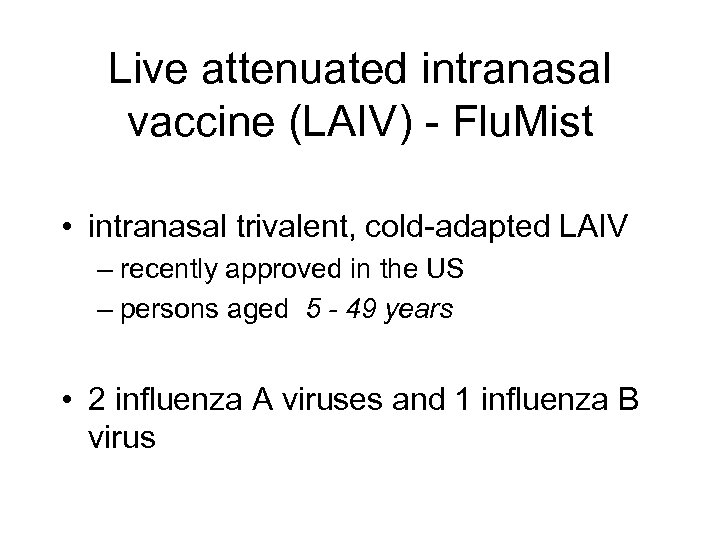 Live attenuated intranasal vaccine (LAIV) - Flu. Mist • intranasal trivalent, cold-adapted LAIV – recently approved in the US – persons aged 5 - 49 years • 2 influenza A viruses and 1 influenza B virus
Live attenuated intranasal vaccine (LAIV) - Flu. Mist • intranasal trivalent, cold-adapted LAIV – recently approved in the US – persons aged 5 - 49 years • 2 influenza A viruses and 1 influenza B virus
 Avian Flu • H 7 N 7 is unrelated to • avian influenza virus currently in Asia (H 5 N 1) • and the avian influenza reported in chickens with no human cases in the United States (H 5 N 2)
Avian Flu • H 7 N 7 is unrelated to • avian influenza virus currently in Asia (H 5 N 1) • and the avian influenza reported in chickens with no human cases in the United States (H 5 N 2)
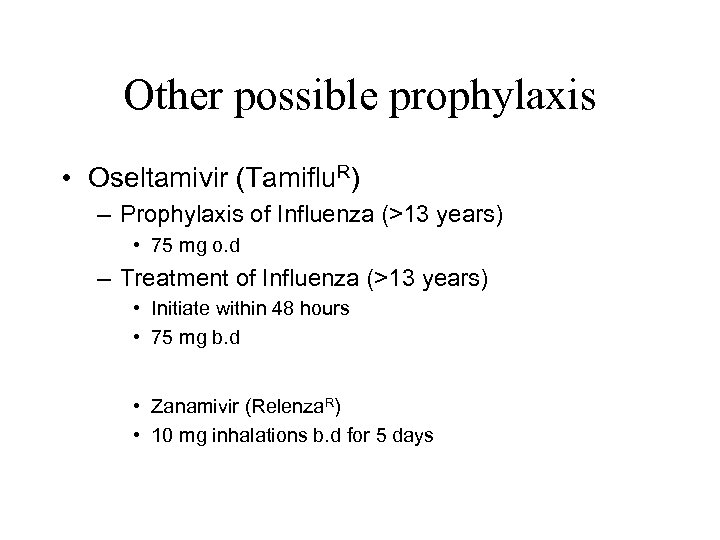 Other possible prophylaxis • Oseltamivir (Tamiflu. R) – Prophylaxis of Influenza (>13 years) • 75 mg o. d – Treatment of Influenza (>13 years) • Initiate within 48 hours • 75 mg b. d • Zanamivir (Relenza. R) • 10 mg inhalations b. d for 5 days
Other possible prophylaxis • Oseltamivir (Tamiflu. R) – Prophylaxis of Influenza (>13 years) • 75 mg o. d – Treatment of Influenza (>13 years) • Initiate within 48 hours • 75 mg b. d • Zanamivir (Relenza. R) • 10 mg inhalations b. d for 5 days
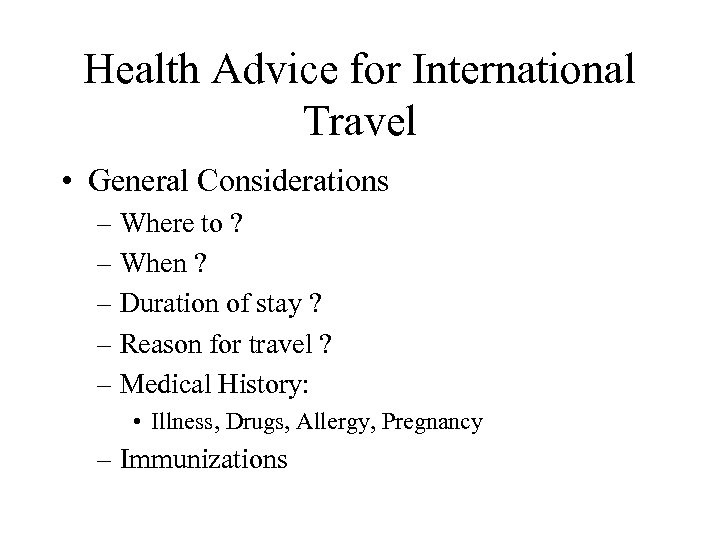 Health Advice for International Travel • General Considerations – Where to ? – When ? – Duration of stay ? – Reason for travel ? – Medical History: • Illness, Drugs, Allergy, Pregnancy – Immunizations
Health Advice for International Travel • General Considerations – Where to ? – When ? – Duration of stay ? – Reason for travel ? – Medical History: • Illness, Drugs, Allergy, Pregnancy – Immunizations
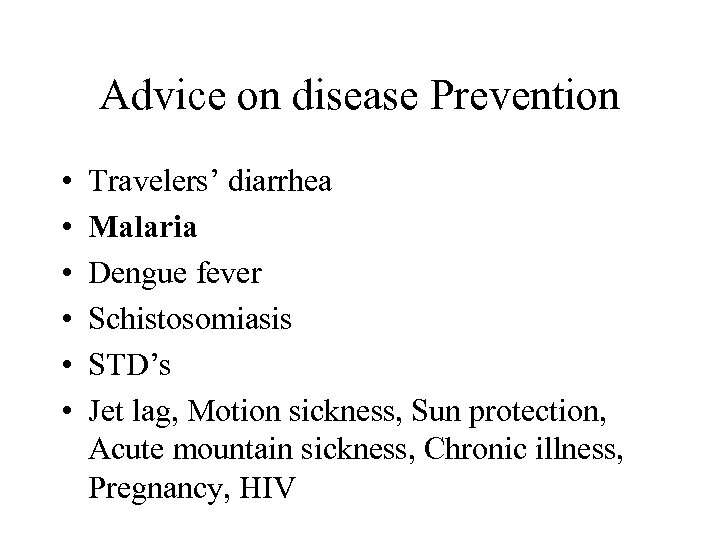 Advice on disease Prevention • • • Travelers’ diarrhea Malaria Dengue fever Schistosomiasis STD’s Jet lag, Motion sickness, Sun protection, Acute mountain sickness, Chronic illness, Pregnancy, HIV
Advice on disease Prevention • • • Travelers’ diarrhea Malaria Dengue fever Schistosomiasis STD’s Jet lag, Motion sickness, Sun protection, Acute mountain sickness, Chronic illness, Pregnancy, HIV
 - Myth 1: Not taking Malaria prophylaxis • highly irresponsible – parasites can multiply at phenomenal rates – malaria can quickly get out of hand • you will always be able to make the diagnosis – symptoms will present with the same intensity – time to progress to severe malaria may be longer • repeated blood smears • new antigen-assay tests
- Myth 1: Not taking Malaria prophylaxis • highly irresponsible – parasites can multiply at phenomenal rates – malaria can quickly get out of hand • you will always be able to make the diagnosis – symptoms will present with the same intensity – time to progress to severe malaria may be longer • repeated blood smears • new antigen-assay tests
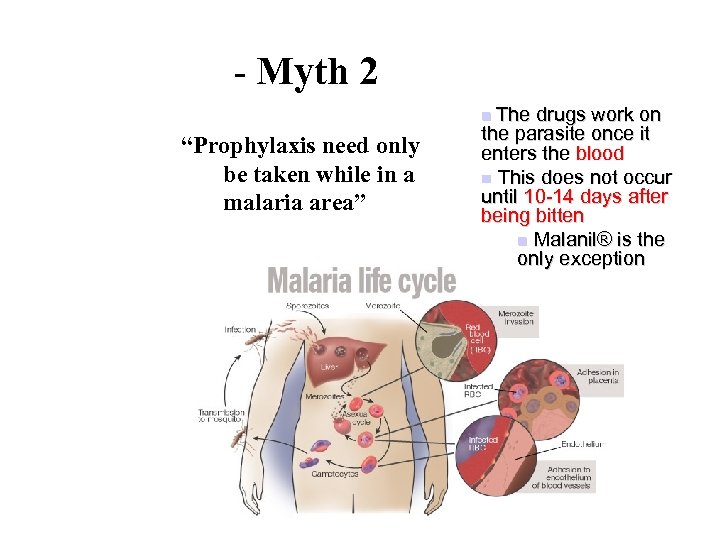 - Myth 2 The drugs work on the parasite once it enters the blood n This does not occur until 10 -14 days after being bitten n Malanil® is the only exception n “Prophylaxis need only be taken while in a malaria area”
- Myth 2 The drugs work on the parasite once it enters the blood n This does not occur until 10 -14 days after being bitten n Malanil® is the only exception n “Prophylaxis need only be taken while in a malaria area”
 - Myth 3 • 'the silent killer‘ • she does not buzz around your head at night “ I wasn't bitten, so can I stop taking my prophylaxis”
- Myth 3 • 'the silent killer‘ • she does not buzz around your head at night “ I wasn't bitten, so can I stop taking my prophylaxis”
 Insect repellents • DEET – The American Academy of Paediatrics recommends ≤ 10% for children < 12 y • Citronella oil – less active than DEET – shorter acting • must be reapplied every 4090 minutes • Bathing, showering, sweating – Re-apply more frequently after
Insect repellents • DEET – The American Academy of Paediatrics recommends ≤ 10% for children < 12 y • Citronella oil – less active than DEET – shorter acting • must be reapplied every 4090 minutes • Bathing, showering, sweating – Re-apply more frequently after
 Insecticide-treated nets (ITNs) • < 5 years – all-cause mortality: < 20% – < 0. 5 million deaths / year in Sub-Sahara Africa • Pregnant women – protected by ITNs every night during their first 4 pregnancies – 25% < underweight or premature babies - Kenya WHO
Insecticide-treated nets (ITNs) • < 5 years – all-cause mortality: < 20% – < 0. 5 million deaths / year in Sub-Sahara Africa • Pregnant women – protected by ITNs every night during their first 4 pregnancies – 25% < underweight or premature babies - Kenya WHO
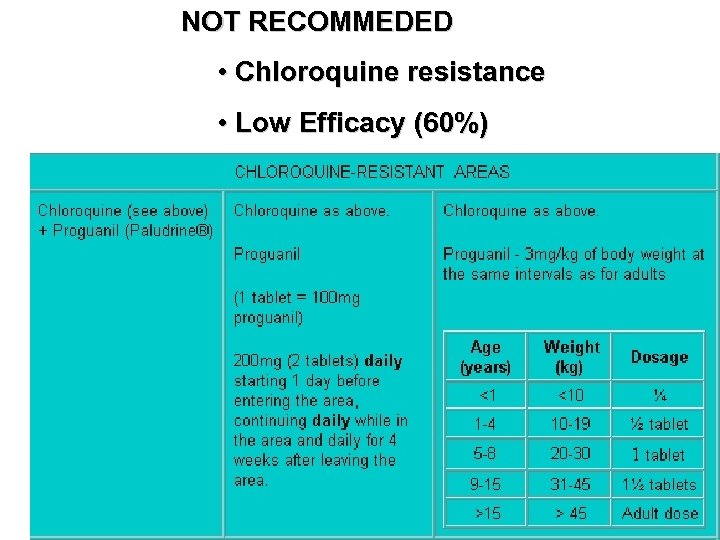 NOT RECOMMEDED • Chloroquine resistance • Low Efficacy (60%)
NOT RECOMMEDED • Chloroquine resistance • Low Efficacy (60%)
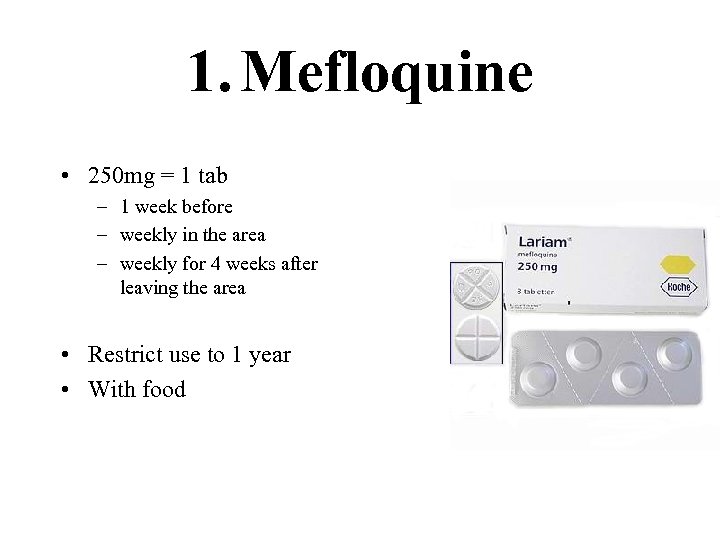 1. Mefloquine • 250 mg = 1 tab – 1 week before – weekly in the area – weekly for 4 weeks after leaving the area • Restrict use to 1 year • With food
1. Mefloquine • 250 mg = 1 tab – 1 week before – weekly in the area – weekly for 4 weeks after leaving the area • Restrict use to 1 year • With food
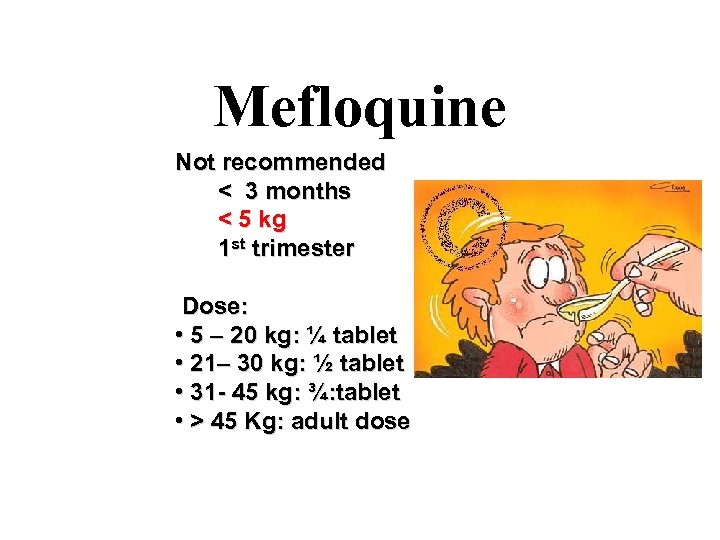 Mefloquine Not recommended < 3 months < 5 kg 1 st trimester Dose: • 5 – 20 kg: ¼ tablet • 21– 30 kg: ½ tablet • 31 - 45 kg: ¾: tablet • > 45 Kg: adult dose
Mefloquine Not recommended < 3 months < 5 kg 1 st trimester Dose: • 5 – 20 kg: ¼ tablet • 21– 30 kg: ½ tablet • 31 - 45 kg: ¾: tablet • > 45 Kg: adult dose
 Mefloquine • 1 in 10 000 Side Effects – serious (never again) • 1 in 100 – severe (will not tolerate) • 1 in 20 – minor (may not tolerate) • Well tolerated by children • mental illness or epilepsy • prolongation of the QTc interval
Mefloquine • 1 in 10 000 Side Effects – serious (never again) • 1 in 100 – severe (will not tolerate) • 1 in 20 – minor (may not tolerate) • Well tolerated by children • mental illness or epilepsy • prolongation of the QTc interval
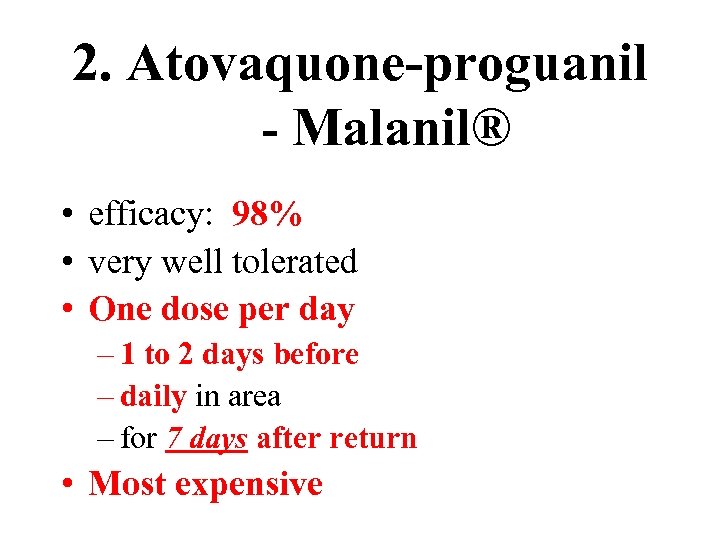 2. Atovaquone-proguanil - Malanil® • efficacy: 98% • very well tolerated • One dose per day – 1 to 2 days before – daily in area – for 7 days after return • Most expensive
2. Atovaquone-proguanil - Malanil® • efficacy: 98% • very well tolerated • One dose per day – 1 to 2 days before – daily in area – for 7 days after return • Most expensive
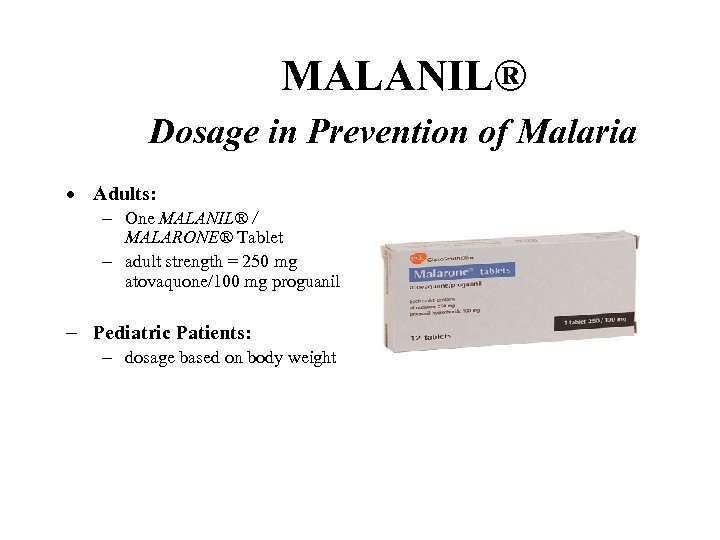 MALANIL® Dosage in Prevention of Malaria · Adults: - One MALANIL® / MALARONE® Tablet - adult strength = 250 mg atovaquone/100 mg proguanil - Pediatric Patients: - dosage based on body weight
MALANIL® Dosage in Prevention of Malaria · Adults: - One MALANIL® / MALARONE® Tablet - adult strength = 250 mg atovaquone/100 mg proguanil - Pediatric Patients: - dosage based on body weight
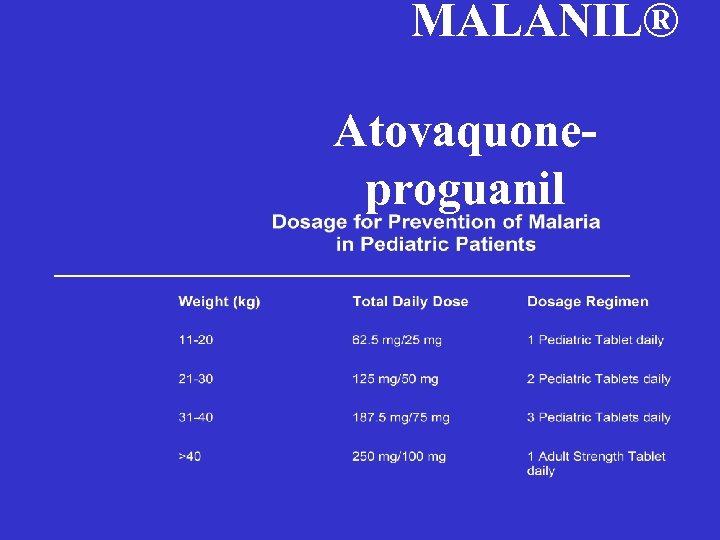 MALANIL® Atovaquoneproguanil
MALANIL® Atovaquoneproguanil
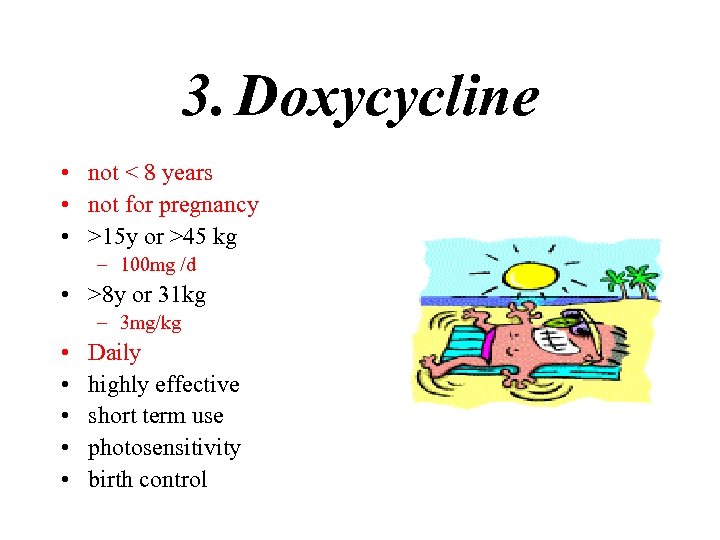 3. Doxycycline • not < 8 years • not for pregnancy • >15 y or >45 kg – 100 mg /d • >8 y or 31 kg – 3 mg/kg • • • Daily highly effective short term use photosensitivity birth control
3. Doxycycline • not < 8 years • not for pregnancy • >15 y or >45 kg – 100 mg /d • >8 y or 31 kg – 3 mg/kg • • • Daily highly effective short term use photosensitivity birth control
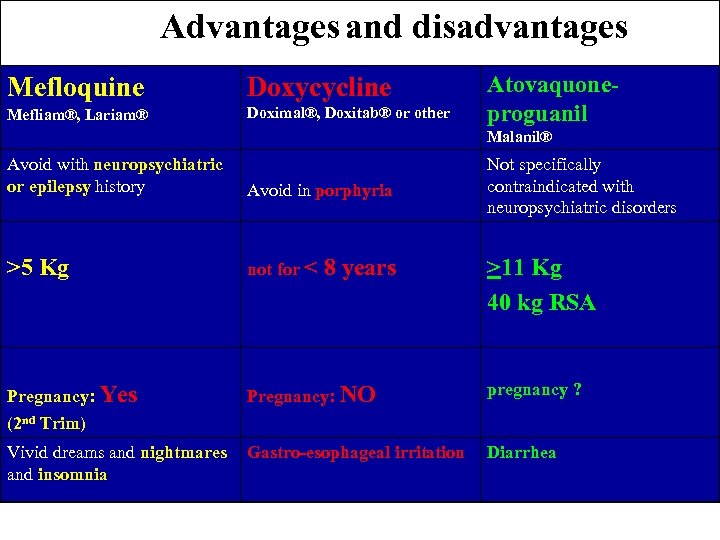 Advantages and disadvantages Mefloquine Doxycycline Mefliam®, Lariam® Doximal®, Doxitab® or other Atovaquoneproguanil Malanil® Avoid with neuropsychiatric or epilepsy history Avoid in porphyria >5 Kg not for < Pregnancy: Yes Pregnancy: NO 8 years Not specifically contraindicated with neuropsychiatric disorders >11 Kg 40 kg RSA pregnancy ? (2 nd Trim) Vivid dreams and nightmares Gastro-esophageal irritation and insomnia Diarrhea
Advantages and disadvantages Mefloquine Doxycycline Mefliam®, Lariam® Doximal®, Doxitab® or other Atovaquoneproguanil Malanil® Avoid with neuropsychiatric or epilepsy history Avoid in porphyria >5 Kg not for < Pregnancy: Yes Pregnancy: NO 8 years Not specifically contraindicated with neuropsychiatric disorders >11 Kg 40 kg RSA pregnancy ? (2 nd Trim) Vivid dreams and nightmares Gastro-esophageal irritation and insomnia Diarrhea
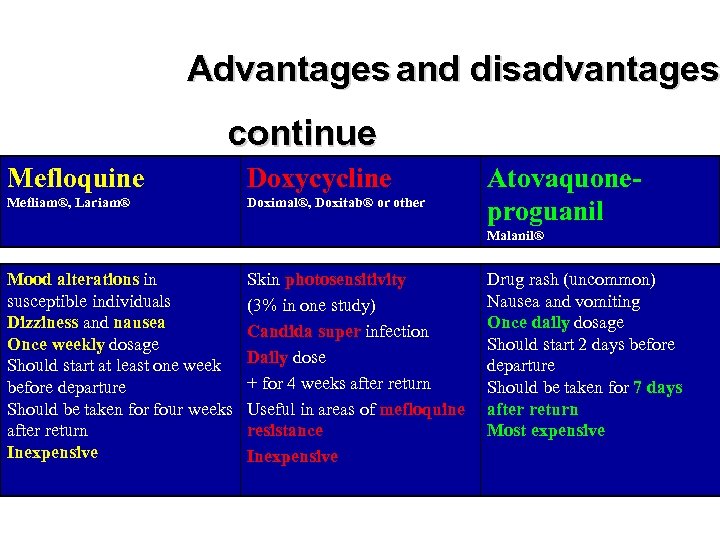 Advantages and disadvantages continue Mefloquine Doxycycline Mefliam®, Lariam® Doximal®, Doxitab® or other Atovaquoneproguanil Malanil® Mood alterations in susceptible individuals Dizziness and nausea Once weekly dosage Should start at least one week before departure Should be taken for four weeks after return Inexpensive Skin photosensitivity (3% in one study) Candida super infection Daily dose + for 4 weeks after return Useful in areas of mefloquine resistance Inexpensive Drug rash (uncommon) Nausea and vomiting Once daily dosage Should start 2 days before departure Should be taken for 7 days after return Most expensive
Advantages and disadvantages continue Mefloquine Doxycycline Mefliam®, Lariam® Doximal®, Doxitab® or other Atovaquoneproguanil Malanil® Mood alterations in susceptible individuals Dizziness and nausea Once weekly dosage Should start at least one week before departure Should be taken for four weeks after return Inexpensive Skin photosensitivity (3% in one study) Candida super infection Daily dose + for 4 weeks after return Useful in areas of mefloquine resistance Inexpensive Drug rash (uncommon) Nausea and vomiting Once daily dosage Should start 2 days before departure Should be taken for 7 days after return Most expensive
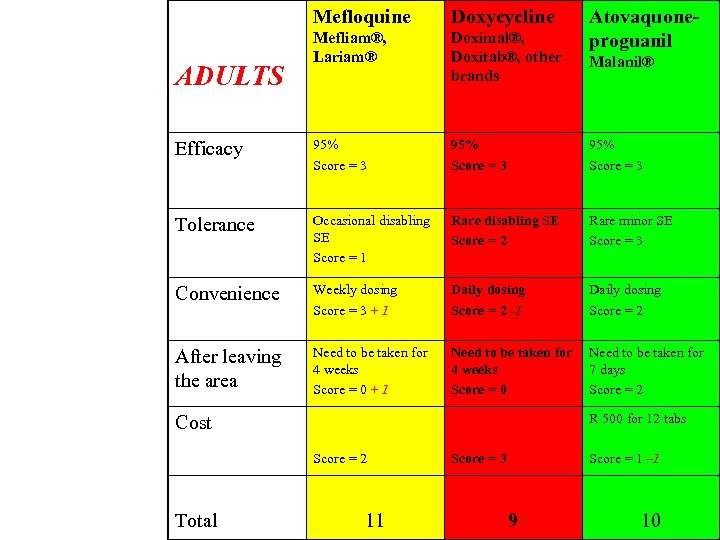 Mefloquine Doxycycline Mefliam®, Lariam® Doximal®, Doxitab®, other brands Efficacy 95% Score = 3 Tolerance Occasional disabling SE Score = 1 Rare disabling SE Score = 2 Rare minor SE Score = 3 Convenience Weekly dosing Score = 3 + 1 Daily dosing Score = 2 -1 Daily dosing Score = 2 After leaving the area Need to be taken for 4 weeks Score = 0 + 1 Need to be taken for 4 weeks Score = 0 Need to be taken for 7 days Score = 2 ADULTS Malanil® R 500 for 12 tabs Cost Score = 2 Total Atovaquoneproguanil 11 Score = 3 Score = 1 – 1 9 10
Mefloquine Doxycycline Mefliam®, Lariam® Doximal®, Doxitab®, other brands Efficacy 95% Score = 3 Tolerance Occasional disabling SE Score = 1 Rare disabling SE Score = 2 Rare minor SE Score = 3 Convenience Weekly dosing Score = 3 + 1 Daily dosing Score = 2 -1 Daily dosing Score = 2 After leaving the area Need to be taken for 4 weeks Score = 0 + 1 Need to be taken for 4 weeks Score = 0 Need to be taken for 7 days Score = 2 ADULTS Malanil® R 500 for 12 tabs Cost Score = 2 Total Atovaquoneproguanil 11 Score = 3 Score = 1 – 1 9 10
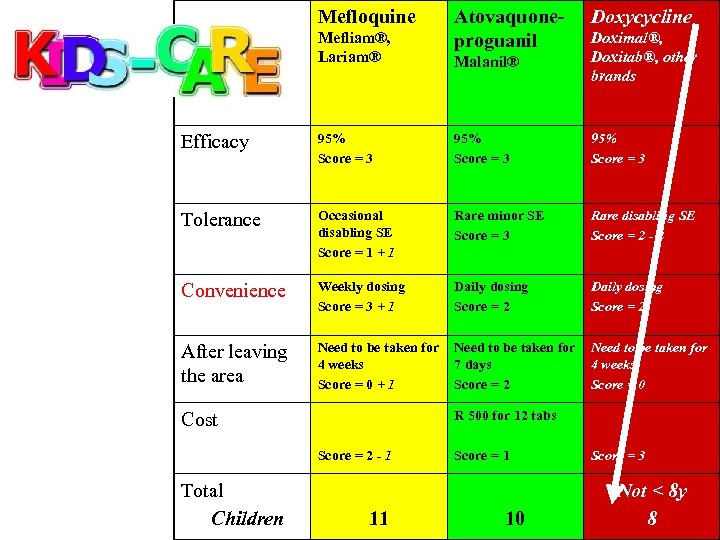 Mefloquine Mefliam®, Lariam® Atovaquoneproguanil Doxycycline Malanil® Doximal®, Doxitab®, other brands Efficacy 95% Score = 3 Tolerance Occasional disabling SE Score = 1 + 1 Rare minor SE Score = 3 Rare disabling SE Score = 2 - 2 Convenience Weekly dosing Score = 3 + 1 Daily dosing Score = 2 After leaving the area Need to be taken for 4 weeks Score = 0 + 1 Need to be taken for 7 days Score = 2 Need to be taken for 4 weeks Score = 0 R 500 for 12 tabs Cost Score = 2 - 1 Total Children 11 Score = 1 10 Score = 3 Not < 8 y 8
Mefloquine Mefliam®, Lariam® Atovaquoneproguanil Doxycycline Malanil® Doximal®, Doxitab®, other brands Efficacy 95% Score = 3 Tolerance Occasional disabling SE Score = 1 + 1 Rare minor SE Score = 3 Rare disabling SE Score = 2 - 2 Convenience Weekly dosing Score = 3 + 1 Daily dosing Score = 2 After leaving the area Need to be taken for 4 weeks Score = 0 + 1 Need to be taken for 7 days Score = 2 Need to be taken for 4 weeks Score = 0 R 500 for 12 tabs Cost Score = 2 - 1 Total Children 11 Score = 1 10 Score = 3 Not < 8 y 8
 • If the child vomits within 1 hour after oral dose, the dose must be repeated
• If the child vomits within 1 hour after oral dose, the dose must be repeated
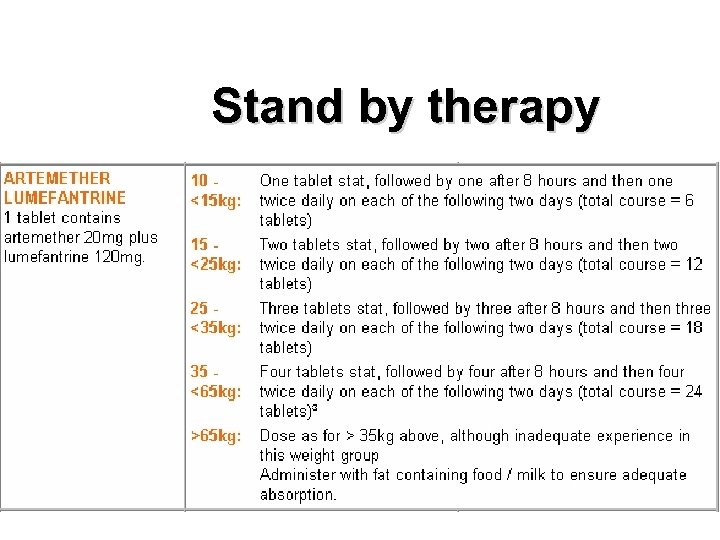 Stand by therapy
Stand by therapy
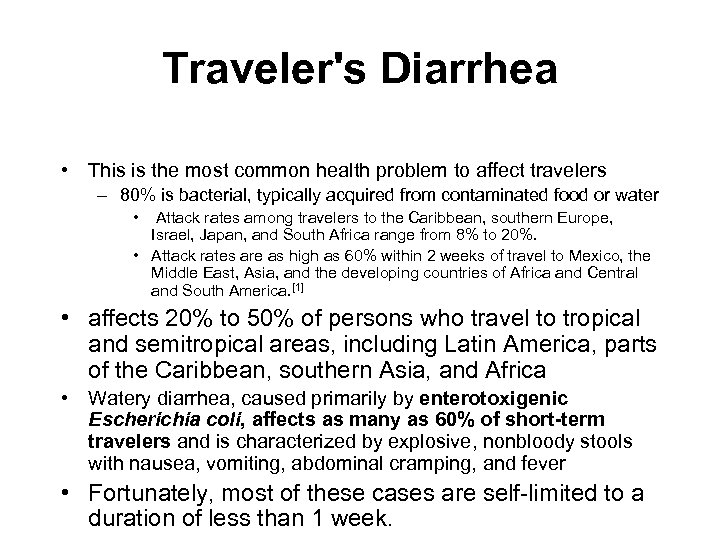 Traveler's Diarrhea • This is the most common health problem to affect travelers – 80% is bacterial, typically acquired from contaminated food or water • Attack rates among travelers to the Caribbean, southern Europe, Israel, Japan, and South Africa range from 8% to 20%. • Attack rates are as high as 60% within 2 weeks of travel to Mexico, the Middle East, Asia, and the developing countries of Africa and Central and South America. [1] • affects 20% to 50% of persons who travel to tropical and semitropical areas, including Latin America, parts of the Caribbean, southern Asia, and Africa • Watery diarrhea, caused primarily by enterotoxigenic Escherichia coli, affects as many as 60% of short-term travelers and is characterized by explosive, nonbloody stools with nausea, vomiting, abdominal cramping, and fever • Fortunately, most of these cases are self-limited to a duration of less than 1 week.
Traveler's Diarrhea • This is the most common health problem to affect travelers – 80% is bacterial, typically acquired from contaminated food or water • Attack rates among travelers to the Caribbean, southern Europe, Israel, Japan, and South Africa range from 8% to 20%. • Attack rates are as high as 60% within 2 weeks of travel to Mexico, the Middle East, Asia, and the developing countries of Africa and Central and South America. [1] • affects 20% to 50% of persons who travel to tropical and semitropical areas, including Latin America, parts of the Caribbean, southern Asia, and Africa • Watery diarrhea, caused primarily by enterotoxigenic Escherichia coli, affects as many as 60% of short-term travelers and is characterized by explosive, nonbloody stools with nausea, vomiting, abdominal cramping, and fever • Fortunately, most of these cases are self-limited to a duration of less than 1 week.

 Travel Medicine Resources • www. cdc. gov/travel • http: //travel. state. gov • http: //wwwn. cdc. gov/travel/content. Yellow. B ook. aspx
Travel Medicine Resources • www. cdc. gov/travel • http: //travel. state. gov • http: //wwwn. cdc. gov/travel/content. Yellow. B ook. aspx


