8cf117c8672b920192a5c244c8308287.ppt
- Количество слайдов: 32
 Addressing Disparities in HIV Disease, Care and Outcomes Kimberly Y. Smith MD, MPH Associate Professor of Medicine Section of Infection Diseases Rush University Medical Center Chicago, IL, USA Disclosures: Abbott, BMS, GSK, Gilead, Merck, Tibotec, Vii. V Advisory Boards
Addressing Disparities in HIV Disease, Care and Outcomes Kimberly Y. Smith MD, MPH Associate Professor of Medicine Section of Infection Diseases Rush University Medical Center Chicago, IL, USA Disclosures: Abbott, BMS, GSK, Gilead, Merck, Tibotec, Vii. V Advisory Boards
 Addressing Disparities in HIV Disease, Care and Outcomes I. II. III. HIV Disease-Incidence, Prevalence, Understanding Risk in the African-American Community Why Are Morbidity and Mortality Rates Higher in Blacks? Improving Our Efforts Toward Eliminating Disparities in HIV Disease, Care and Outcomes
Addressing Disparities in HIV Disease, Care and Outcomes I. II. III. HIV Disease-Incidence, Prevalence, Understanding Risk in the African-American Community Why Are Morbidity and Mortality Rates Higher in Blacks? Improving Our Efforts Toward Eliminating Disparities in HIV Disease, Care and Outcomes

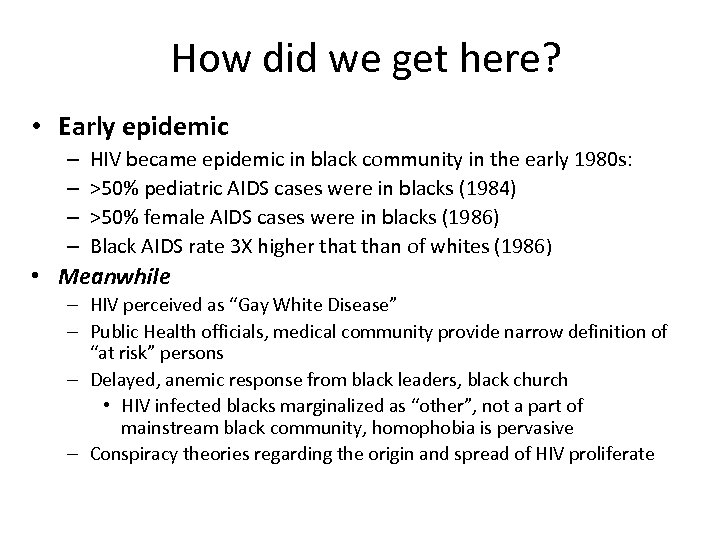 How did we get here? • Early epidemic – – HIV became epidemic in black community in the early 1980 s: >50% pediatric AIDS cases were in blacks (1984) >50% female AIDS cases were in blacks (1986) Black AIDS rate 3 X higher that than of whites (1986) • Meanwhile – HIV perceived as “Gay White Disease” – Public Health officials, medical community provide narrow definition of “at risk” persons – Delayed, anemic response from black leaders, black church • HIV infected blacks marginalized as “other”, not a part of mainstream black community, homophobia is pervasive – Conspiracy theories regarding the origin and spread of HIV proliferate
How did we get here? • Early epidemic – – HIV became epidemic in black community in the early 1980 s: >50% pediatric AIDS cases were in blacks (1984) >50% female AIDS cases were in blacks (1986) Black AIDS rate 3 X higher that than of whites (1986) • Meanwhile – HIV perceived as “Gay White Disease” – Public Health officials, medical community provide narrow definition of “at risk” persons – Delayed, anemic response from black leaders, black church • HIV infected blacks marginalized as “other”, not a part of mainstream black community, homophobia is pervasive – Conspiracy theories regarding the origin and spread of HIV proliferate
 1990’s 1992 1994 1995
1990’s 1992 1994 1995

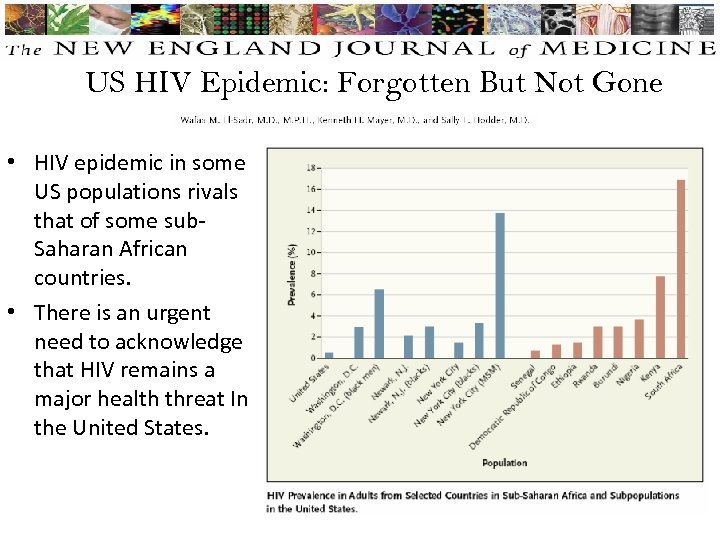 US HIV Epidemic: Forgotten But Not Gone • HIV epidemic in some US populations rivals that of some sub. Saharan African countries. • There is an urgent need to acknowledge that HIV remains a major health threat In the United States.
US HIV Epidemic: Forgotten But Not Gone • HIV epidemic in some US populations rivals that of some sub. Saharan African countries. • There is an urgent need to acknowledge that HIV remains a major health threat In the United States.
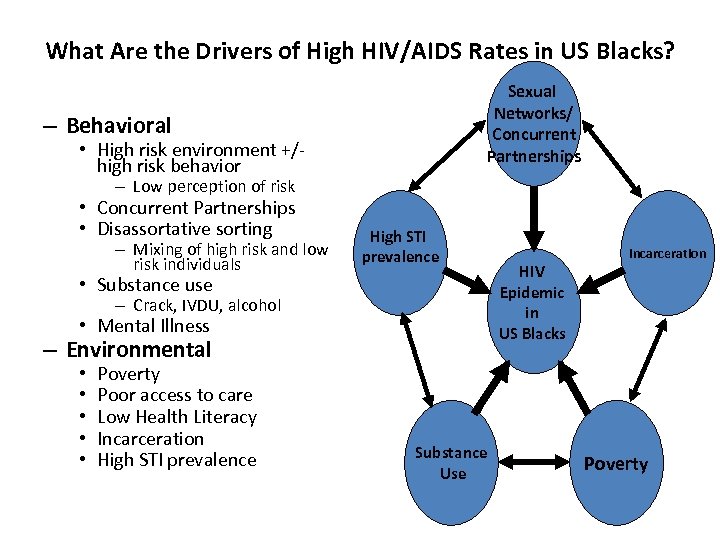 What Are the Drivers of High HIV/AIDS Rates in US Blacks? Sexual Networks/ Concurrent Partnerships – Behavioral • High risk environment +/high risk behavior – Low perception of risk • Concurrent Partnerships • Disassortative sorting – Mixing of high risk and low risk individuals High STI prevalence • Substance use – Crack, IVDU, alcohol • Mental Illness – Environmental • • • Poverty Poor access to care Low Health Literacy Incarceration High STI prevalence Substance Use HIV Epidemic in US Blacks Incarceration Poverty
What Are the Drivers of High HIV/AIDS Rates in US Blacks? Sexual Networks/ Concurrent Partnerships – Behavioral • High risk environment +/high risk behavior – Low perception of risk • Concurrent Partnerships • Disassortative sorting – Mixing of high risk and low risk individuals High STI prevalence • Substance use – Crack, IVDU, alcohol • Mental Illness – Environmental • • • Poverty Poor access to care Low Health Literacy Incarceration High STI prevalence Substance Use HIV Epidemic in US Blacks Incarceration Poverty
 High Risk Environment +/- High Risk Behavior • Black youth with low risk behavior 25 x more likely than whites to acquire STD – Low risk defined as having few partners, low alcohol, tobacco or other drug use • Heterosexually Acquired HIV: African Americans in North Carolina – In a case control (HIV+/HIV-) study of AA women, 27% of cases had no “high risk behavior” – Independent risk factors for HIV among lower risk cases: • Less than HS education (OR 5. 2; 95% CI: 2. 2, 11. 1) • Food insecurity (OR 3. 7; 95% CI: 1. 5, 8. 9) • Non–monogamous sex partner (OR 2. 9; 95% CI: 1. 3, 6. 4) • CDC-Funded National HIV Behavioral Surveillance (DC HIV Epidemic among heterosexuals) – 750 persons surveyed- 93% African-American, 60% annual income <10 K • 5. 2% HIV+ (6. 3% W, 3. 9% M) • > 50% h/o incarceration (M>W) • 46% women had one sexual partner in past yr – Condom use higher among Blacks and Hispanic than other groups Hallfors DD, et al. Am J Public Health. 2007; 97(1): 125 -132. ; Adimora AA, Schoenbach VJ, et al. JAIDS. 2006; 41: 616– 623. Magnus et al. JAIDS 2009 Reese, M et al. The Journal of Sexual Medicine. Volume 7, Issue Supplement s 5, pages 266– 276, October 2010
High Risk Environment +/- High Risk Behavior • Black youth with low risk behavior 25 x more likely than whites to acquire STD – Low risk defined as having few partners, low alcohol, tobacco or other drug use • Heterosexually Acquired HIV: African Americans in North Carolina – In a case control (HIV+/HIV-) study of AA women, 27% of cases had no “high risk behavior” – Independent risk factors for HIV among lower risk cases: • Less than HS education (OR 5. 2; 95% CI: 2. 2, 11. 1) • Food insecurity (OR 3. 7; 95% CI: 1. 5, 8. 9) • Non–monogamous sex partner (OR 2. 9; 95% CI: 1. 3, 6. 4) • CDC-Funded National HIV Behavioral Surveillance (DC HIV Epidemic among heterosexuals) – 750 persons surveyed- 93% African-American, 60% annual income <10 K • 5. 2% HIV+ (6. 3% W, 3. 9% M) • > 50% h/o incarceration (M>W) • 46% women had one sexual partner in past yr – Condom use higher among Blacks and Hispanic than other groups Hallfors DD, et al. Am J Public Health. 2007; 97(1): 125 -132. ; Adimora AA, Schoenbach VJ, et al. JAIDS. 2006; 41: 616– 623. Magnus et al. JAIDS 2009 Reese, M et al. The Journal of Sexual Medicine. Volume 7, Issue Supplement s 5, pages 266– 276, October 2010
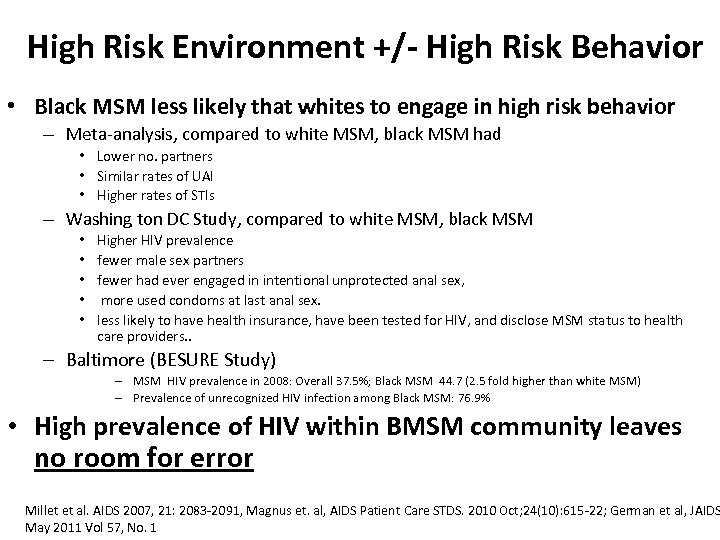 High Risk Environment +/- High Risk Behavior • Black MSM less likely that whites to engage in high risk behavior – Meta-analysis, compared to white MSM, black MSM had • Lower no. partners • Similar rates of UAI • Higher rates of STIs – Washing ton DC Study, compared to white MSM, black MSM • • • Higher HIV prevalence fewer male sex partners fewer had ever engaged in intentional unprotected anal sex, more used condoms at last anal sex. less likely to have health insurance, have been tested for HIV, and disclose MSM status to health care providers. . – Baltimore (BESURE Study) – MSM HIV prevalence in 2008: Overall 37. 5%; Black MSM 44. 7 (2. 5 fold higher than white MSM) – Prevalence of unrecognized HIV infection among Black MSM: 76. 9% • High prevalence of HIV within BMSM community leaves no room for error Millet et al. AIDS 2007, 21: 2083 -2091, Magnus et. al, AIDS Patient Care STDS. 2010 Oct; 24(10): 615 -22; German et al, JAIDS May 2011 Vol 57, No. 1
High Risk Environment +/- High Risk Behavior • Black MSM less likely that whites to engage in high risk behavior – Meta-analysis, compared to white MSM, black MSM had • Lower no. partners • Similar rates of UAI • Higher rates of STIs – Washing ton DC Study, compared to white MSM, black MSM • • • Higher HIV prevalence fewer male sex partners fewer had ever engaged in intentional unprotected anal sex, more used condoms at last anal sex. less likely to have health insurance, have been tested for HIV, and disclose MSM status to health care providers. . – Baltimore (BESURE Study) – MSM HIV prevalence in 2008: Overall 37. 5%; Black MSM 44. 7 (2. 5 fold higher than white MSM) – Prevalence of unrecognized HIV infection among Black MSM: 76. 9% • High prevalence of HIV within BMSM community leaves no room for error Millet et al. AIDS 2007, 21: 2083 -2091, Magnus et. al, AIDS Patient Care STDS. 2010 Oct; 24(10): 615 -22; German et al, JAIDS May 2011 Vol 57, No. 1
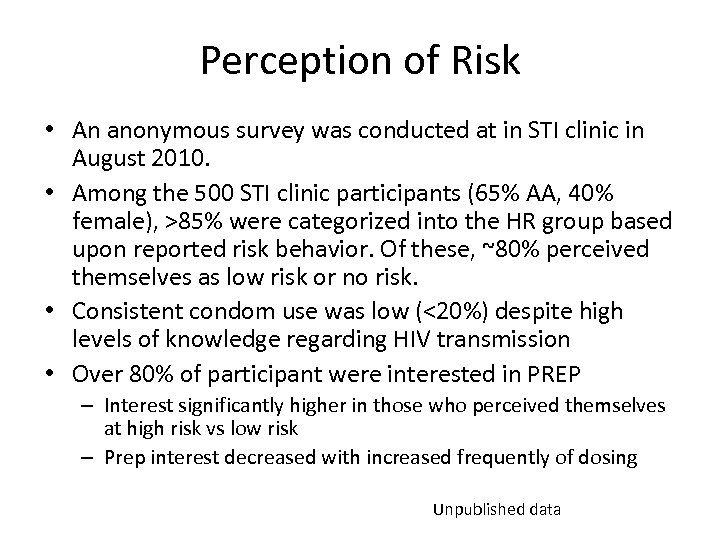 Perception of Risk • An anonymous survey was conducted at in STI clinic in August 2010. • Among the 500 STI clinic participants (65% AA, 40% female), >85% were categorized into the HR group based upon reported risk behavior. Of these, ~80% perceived themselves as low risk or no risk. • Consistent condom use was low (<20%) despite high levels of knowledge regarding HIV transmission • Over 80% of participant were interested in PREP – Interest significantly higher in those who perceived themselves at high risk vs low risk – Prep interest decreased with increased frequently of dosing Unpublished data
Perception of Risk • An anonymous survey was conducted at in STI clinic in August 2010. • Among the 500 STI clinic participants (65% AA, 40% female), >85% were categorized into the HR group based upon reported risk behavior. Of these, ~80% perceived themselves as low risk or no risk. • Consistent condom use was low (<20%) despite high levels of knowledge regarding HIV transmission • Over 80% of participant were interested in PREP – Interest significantly higher in those who perceived themselves at high risk vs low risk – Prep interest decreased with increased frequently of dosing Unpublished data
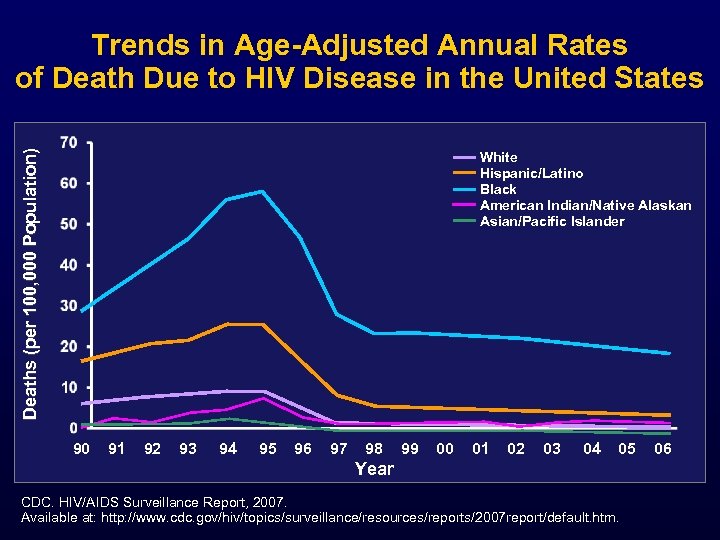 Deaths (per 100, 000 Population) Trends in Age-Adjusted Annual Rates of Death Due to HIV Disease in the United States White Hispanic/Latino Black American Indian/Native Alaskan Asian/Pacific Islander 90 91 92 93 94 95 96 97 98 99 00 01 02 03 04 05 Year CDC. HIV/AIDS Surveillance Report, 2007. Available at: http: //www. cdc. gov/hiv/topics/surveillance/resources/reports/2007 report/default. htm. 06
Deaths (per 100, 000 Population) Trends in Age-Adjusted Annual Rates of Death Due to HIV Disease in the United States White Hispanic/Latino Black American Indian/Native Alaskan Asian/Pacific Islander 90 91 92 93 94 95 96 97 98 99 00 01 02 03 04 05 Year CDC. HIV/AIDS Surveillance Report, 2007. Available at: http: //www. cdc. gov/hiv/topics/surveillance/resources/reports/2007 report/default. htm. 06
 Why Are Morbidity and Mortality Rates Higher in Blacks? Never in Care/Delayed Entry into care n Late Initiation of ART/Less time on ART n Missed visits/Lower retention in care n Lower Treatment Success n Higher Co-morbid conditions n Poverty/Competing Priorities n Substance Use n Mistrust of Medical Establishment n
Why Are Morbidity and Mortality Rates Higher in Blacks? Never in Care/Delayed Entry into care n Late Initiation of ART/Less time on ART n Missed visits/Lower retention in care n Lower Treatment Success n Higher Co-morbid conditions n Poverty/Competing Priorities n Substance Use n Mistrust of Medical Establishment n
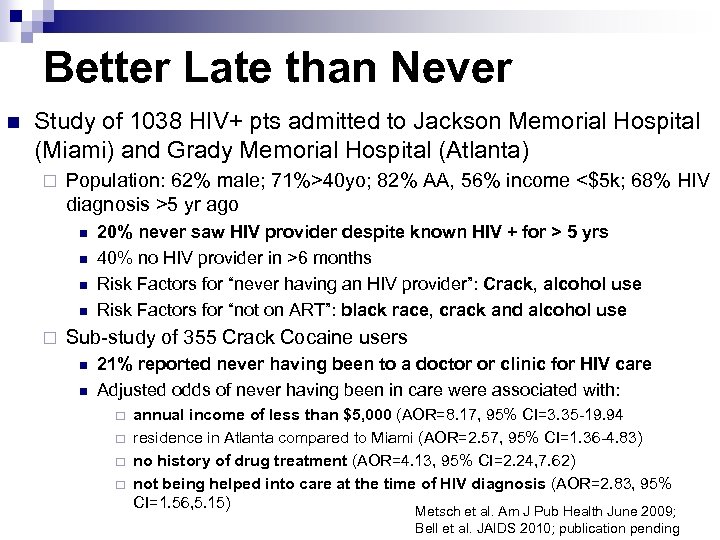 Better Late than Never n Study of 1038 HIV+ pts admitted to Jackson Memorial Hospital (Miami) and Grady Memorial Hospital (Atlanta) ¨ Population: 62% male; 71%>40 yo; 82% AA, 56% income <$5 k; 68% HIV diagnosis >5 yr ago n n ¨ 20% never saw HIV provider despite known HIV + for > 5 yrs 40% no HIV provider in >6 months Risk Factors for “never having an HIV provider”: Crack, alcohol use Risk Factors for “not on ART”: black race, crack and alcohol use Sub-study of 355 Crack Cocaine users n n 21% reported never having been to a doctor or clinic for HIV care Adjusted odds of never having been in care were associated with: ¨ ¨ annual income of less than $5, 000 (AOR=8. 17, 95% CI=3. 35 -19. 94 residence in Atlanta compared to Miami (AOR=2. 57, 95% CI=1. 36 -4. 83) no history of drug treatment (AOR=4. 13, 95% CI=2. 24, 7. 62) not being helped into care at the time of HIV diagnosis (AOR=2. 83, 95% CI=1. 56, 5. 15) Metsch et al. Am J Pub Health June 2009; Bell et al. JAIDS 2010; publication pending
Better Late than Never n Study of 1038 HIV+ pts admitted to Jackson Memorial Hospital (Miami) and Grady Memorial Hospital (Atlanta) ¨ Population: 62% male; 71%>40 yo; 82% AA, 56% income <$5 k; 68% HIV diagnosis >5 yr ago n n ¨ 20% never saw HIV provider despite known HIV + for > 5 yrs 40% no HIV provider in >6 months Risk Factors for “never having an HIV provider”: Crack, alcohol use Risk Factors for “not on ART”: black race, crack and alcohol use Sub-study of 355 Crack Cocaine users n n 21% reported never having been to a doctor or clinic for HIV care Adjusted odds of never having been in care were associated with: ¨ ¨ annual income of less than $5, 000 (AOR=8. 17, 95% CI=3. 35 -19. 94 residence in Atlanta compared to Miami (AOR=2. 57, 95% CI=1. 36 -4. 83) no history of drug treatment (AOR=4. 13, 95% CI=2. 24, 7. 62) not being helped into care at the time of HIV diagnosis (AOR=2. 83, 95% CI=1. 56, 5. 15) Metsch et al. Am J Pub Health June 2009; Bell et al. JAIDS 2010; publication pending
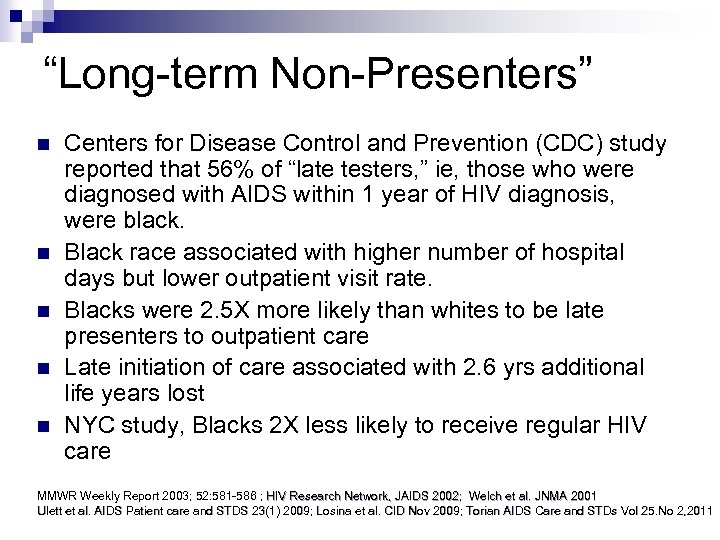 “Long-term Non-Presenters” n n n Centers for Disease Control and Prevention (CDC) study reported that 56% of “late testers, ” ie, those who were diagnosed with AIDS within 1 year of HIV diagnosis, were black. Black race associated with higher number of hospital days but lower outpatient visit rate. Blacks were 2. 5 X more likely than whites to be late presenters to outpatient care Late initiation of care associated with 2. 6 yrs additional life years lost NYC study, Blacks 2 X less likely to receive regular HIV care MMWR Weekly Report 2003; 52: 581 -586 ; HIV Research Network, JAIDS 2002; Welch et al. JNMA 2001 Ulett et al. AIDS Patient care and STDS 23(1) 2009; Losina et al. CID Nov 2009; Torian AIDS Care and STDs Vol 25. No 2, 2011
“Long-term Non-Presenters” n n n Centers for Disease Control and Prevention (CDC) study reported that 56% of “late testers, ” ie, those who were diagnosed with AIDS within 1 year of HIV diagnosis, were black. Black race associated with higher number of hospital days but lower outpatient visit rate. Blacks were 2. 5 X more likely than whites to be late presenters to outpatient care Late initiation of care associated with 2. 6 yrs additional life years lost NYC study, Blacks 2 X less likely to receive regular HIV care MMWR Weekly Report 2003; 52: 581 -586 ; HIV Research Network, JAIDS 2002; Welch et al. JNMA 2001 Ulett et al. AIDS Patient care and STDS 23(1) 2009; Losina et al. CID Nov 2009; Torian AIDS Care and STDs Vol 25. No 2, 2011
 n AA more likely than whites to have missed visits (OR 1. 85; CI 1. 61 -2. 14) n Missed visits associated with virologic failure (OR 1. 78; CI 1. 482. 13) n n AA had 1. 56 times more likely to experience virologic failure (P<0. 05), but no significant difference when controlled for missed visits Nested study reveals 2. 3 x higher mortality in persons with missed visits in 1 st yr of tx. Mugavero et al. JAIDS Jan 2009, Mugavero et al. CID Jan 2009
n AA more likely than whites to have missed visits (OR 1. 85; CI 1. 61 -2. 14) n Missed visits associated with virologic failure (OR 1. 78; CI 1. 482. 13) n n AA had 1. 56 times more likely to experience virologic failure (P<0. 05), but no significant difference when controlled for missed visits Nested study reveals 2. 3 x higher mortality in persons with missed visits in 1 st yr of tx. Mugavero et al. JAIDS Jan 2009, Mugavero et al. CID Jan 2009
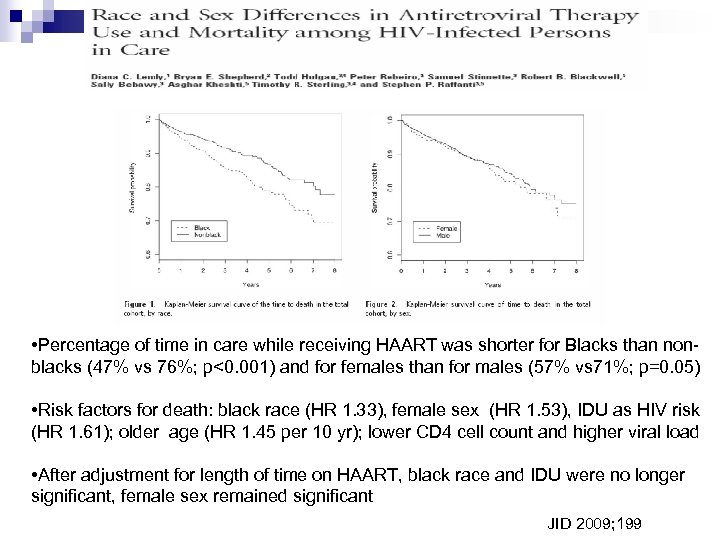 • Percentage of time in care while receiving HAART was shorter for Blacks than nonblacks (47% vs 76%; p<0. 001) and for females than for males (57% vs 71%; p=0. 05) • Risk factors for death: black race (HR 1. 33), female sex (HR 1. 53), IDU as HIV risk (HR 1. 61); older age (HR 1. 45 per 10 yr); lower CD 4 cell count and higher viral load • After adjustment for length of time on HAART, black race and IDU were no longer significant, female sex remained significant JID 2009; 199
• Percentage of time in care while receiving HAART was shorter for Blacks than nonblacks (47% vs 76%; p<0. 001) and for females than for males (57% vs 71%; p=0. 05) • Risk factors for death: black race (HR 1. 33), female sex (HR 1. 53), IDU as HIV risk (HR 1. 61); older age (HR 1. 45 per 10 yr); lower CD 4 cell count and higher viral load • After adjustment for length of time on HAART, black race and IDU were no longer significant, female sex remained significant JID 2009; 199
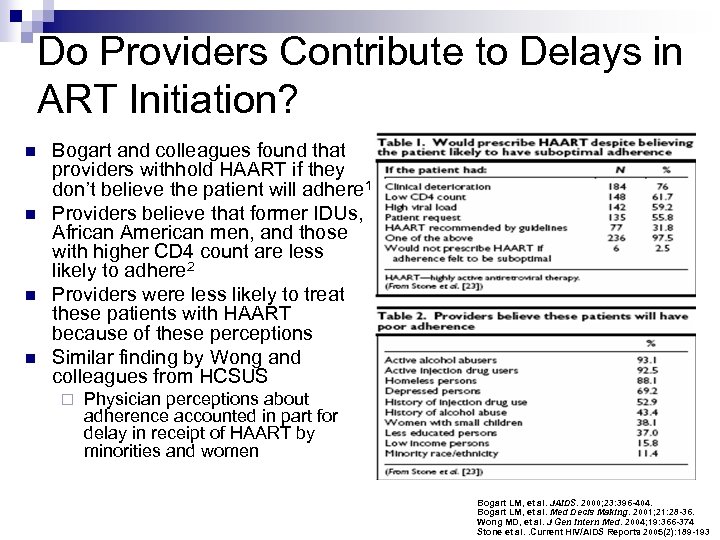 Do Providers Contribute to Delays in ART Initiation? n n Bogart and colleagues found that providers withhold HAART if they don’t believe the patient will adhere 1 Providers believe that former IDUs, African American men, and those with higher CD 4 count are less likely to adhere 2 Providers were less likely to treat these patients with HAART because of these perceptions Similar finding by Wong and colleagues from HCSUS ¨ Physician perceptions about adherence accounted in part for delay in receipt of HAART by minorities and women Bogart LM, et al. JAIDS. 2000; 23: 396 -404. Bogart LM, et al. Med Decis Making. 2001; 21: 28 -36. Wong MD, et al. J Gen Intern Med. 2004; 19: 366 -374 Stone et al. . Current HIV/AIDS Reports 2005(2): 189 -193
Do Providers Contribute to Delays in ART Initiation? n n Bogart and colleagues found that providers withhold HAART if they don’t believe the patient will adhere 1 Providers believe that former IDUs, African American men, and those with higher CD 4 count are less likely to adhere 2 Providers were less likely to treat these patients with HAART because of these perceptions Similar finding by Wong and colleagues from HCSUS ¨ Physician perceptions about adherence accounted in part for delay in receipt of HAART by minorities and women Bogart LM, et al. JAIDS. 2000; 23: 396 -404. Bogart LM, et al. Med Decis Making. 2001; 21: 28 -36. Wong MD, et al. J Gen Intern Med. 2004; 19: 366 -374 Stone et al. . Current HIV/AIDS Reports 2005(2): 189 -193
 LOWER TREATMENT SUCCESS
LOWER TREATMENT SUCCESS
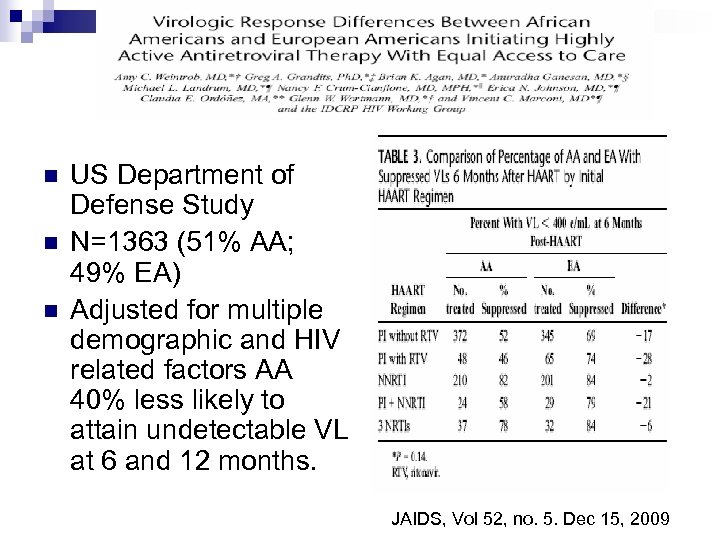 n n n US Department of Defense Study N=1363 (51% AA; 49% EA) Adjusted for multiple demographic and HIV related factors AA 40% less likely to attain undetectable VL at 6 and 12 months. JAIDS, Vol 52, no. 5. Dec 15, 2009
n n n US Department of Defense Study N=1363 (51% AA; 49% EA) Adjusted for multiple demographic and HIV related factors AA 40% less likely to attain undetectable VL at 6 and 12 months. JAIDS, Vol 52, no. 5. Dec 15, 2009
 Clinical Trials n HIV-1 RNA <50 c/m. L at Week 96 ACTG 5095 (ZDV/3 TC/EFZ +/ABC) ¨ n ACTG 5142 - EFV vs LPV ¨ n Blacks were 67% less likely to achieve virologic success compared to whites Blacks 36% more likely to experience virologic failure and whites regardless of treatment arm HEAT (ABC/3 TC vs TFD/FTC w/ LPV/r) Study population included 49% nonwhite; 38% African-American. ¨ African-American race, but not female sex, was a significant predictor of virologic failure in a multivariate logistic regression model. ¨ n ABC/3 TC + LPV/r TDF/FTC + LPV/r 343 345 119 124 143 147 73 62 8 12 . Gulick et al NEJM 2004. 350 pp 1850 -61. Riddler et al. NEJM 2008: 358: 2095— 2106; Smith KY, et al. 5 th IAS. Cape Town, 2009. Abstract Mo. PEB 033
Clinical Trials n HIV-1 RNA <50 c/m. L at Week 96 ACTG 5095 (ZDV/3 TC/EFZ +/ABC) ¨ n ACTG 5142 - EFV vs LPV ¨ n Blacks were 67% less likely to achieve virologic success compared to whites Blacks 36% more likely to experience virologic failure and whites regardless of treatment arm HEAT (ABC/3 TC vs TFD/FTC w/ LPV/r) Study population included 49% nonwhite; 38% African-American. ¨ African-American race, but not female sex, was a significant predictor of virologic failure in a multivariate logistic regression model. ¨ n ABC/3 TC + LPV/r TDF/FTC + LPV/r 343 345 119 124 143 147 73 62 8 12 . Gulick et al NEJM 2004. 350 pp 1850 -61. Riddler et al. NEJM 2008: 358: 2095— 2106; Smith KY, et al. 5 th IAS. Cape Town, 2009. Abstract Mo. PEB 033
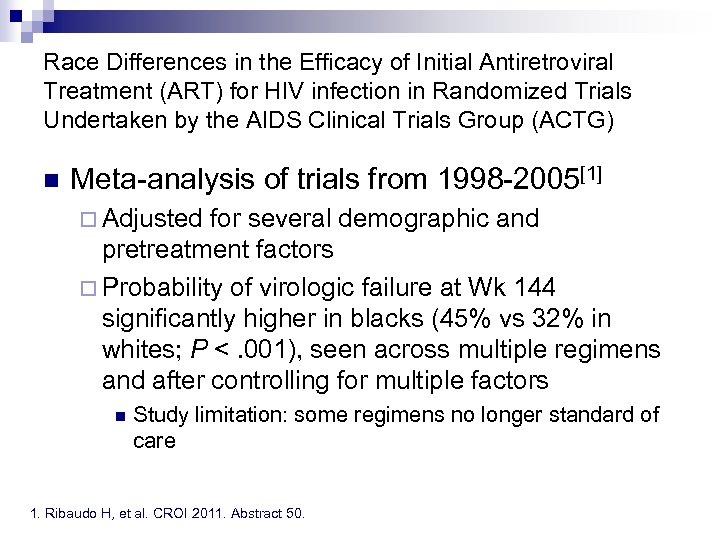 Race Differences in the Efficacy of Initial Antiretroviral Treatment (ART) for HIV infection in Randomized Trials Undertaken by the AIDS Clinical Trials Group (ACTG) n Meta-analysis of trials from 1998 -2005[1] ¨ Adjusted for several demographic and pretreatment factors ¨ Probability of virologic failure at Wk 144 significantly higher in blacks (45% vs 32% in whites; P <. 001), seen across multiple regimens and after controlling for multiple factors n Study limitation: some regimens no longer standard of care 1. Ribaudo H, et al. CROI 2011. Abstract 50.
Race Differences in the Efficacy of Initial Antiretroviral Treatment (ART) for HIV infection in Randomized Trials Undertaken by the AIDS Clinical Trials Group (ACTG) n Meta-analysis of trials from 1998 -2005[1] ¨ Adjusted for several demographic and pretreatment factors ¨ Probability of virologic failure at Wk 144 significantly higher in blacks (45% vs 32% in whites; P <. 001), seen across multiple regimens and after controlling for multiple factors n Study limitation: some regimens no longer standard of care 1. Ribaudo H, et al. CROI 2011. Abstract 50.
 Time to Virologic Failure by Race Kaplan-Meier failure distribution Numbers of subjects at risk 1151 798 1067 1344 571 840 302 445 45% P<0. 001* 32% Time since starting ART * Log-rank test stratified on ART regimen and parent study 58 107
Time to Virologic Failure by Race Kaplan-Meier failure distribution Numbers of subjects at risk 1151 798 1067 1344 571 840 302 445 45% P<0. 001* 32% Time since starting ART * Log-rank test stratified on ART regimen and parent study 58 107
 ACTG 5202: Sex and Race Differences in Efficacy and Safety of Initial ART n Black race associated with increased risk of VF across regimens ¨ 1. 0 n Poorer adherence, lower baseline CD 4+ counts in blacks Week 192: Probability of Remaining Free of Virologic Failure Non-Hispanic whites Non-Hispanic blacks In females, but not males, higher HR for VF with ATV/RTV vs EFV ¨ ABC/3 TC: 2. 90 (1. 32 -6. 36), P =. 004 ¨ TDF/FTC: 2. 20 (0. 97 -4. 98), P =. 03 Wk 192: Probability of Remaining Free of Virologic Failure in Females 1. 0 0. 8 0. 6 0. 4 0. 2 0. 0 EFV + ATV/r + TDF/FTC ABC/3 TC TDF/FTC ATV/r + ABC/3 TC Smith KY, et al. CROI 2011. Abstract 536. 0. 0 EFV + TDF/FTC EFV + ABC/3 TC ATV/r + TDF/FTC ATV/r + ABC/3 TC
ACTG 5202: Sex and Race Differences in Efficacy and Safety of Initial ART n Black race associated with increased risk of VF across regimens ¨ 1. 0 n Poorer adherence, lower baseline CD 4+ counts in blacks Week 192: Probability of Remaining Free of Virologic Failure Non-Hispanic whites Non-Hispanic blacks In females, but not males, higher HR for VF with ATV/RTV vs EFV ¨ ABC/3 TC: 2. 90 (1. 32 -6. 36), P =. 004 ¨ TDF/FTC: 2. 20 (0. 97 -4. 98), P =. 03 Wk 192: Probability of Remaining Free of Virologic Failure in Females 1. 0 0. 8 0. 6 0. 4 0. 2 0. 0 EFV + ATV/r + TDF/FTC ABC/3 TC TDF/FTC ATV/r + ABC/3 TC Smith KY, et al. CROI 2011. Abstract 536. 0. 0 EFV + TDF/FTC EFV + ABC/3 TC ATV/r + TDF/FTC ATV/r + ABC/3 TC
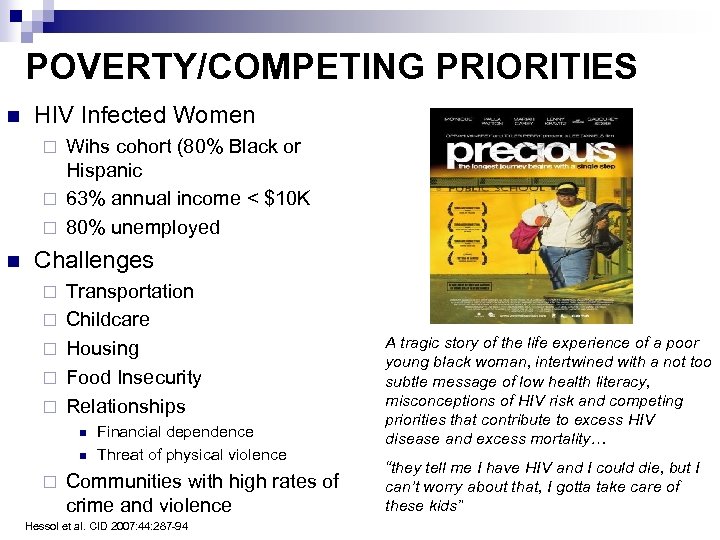 POVERTY/COMPETING PRIORITIES n HIV Infected Women Wihs cohort (80% Black or Hispanic ¨ 63% annual income < $10 K ¨ 80% unemployed ¨ n Challenges ¨ ¨ ¨ Transportation Childcare Housing Food Insecurity Relationships n n ¨ Financial dependence Threat of physical violence Communities with high rates of crime and violence Hessol et al. CID 2007: 44: 287 -94 A tragic story of the life experience of a poor young black woman, intertwined with a not too subtle message of low health literacy, misconceptions of HIV risk and competing priorities that contribute to excess HIV disease and excess mortality… “they tell me I have HIV and I could die, but I can’t worry about that, I gotta take care of these kids”
POVERTY/COMPETING PRIORITIES n HIV Infected Women Wihs cohort (80% Black or Hispanic ¨ 63% annual income < $10 K ¨ 80% unemployed ¨ n Challenges ¨ ¨ ¨ Transportation Childcare Housing Food Insecurity Relationships n n ¨ Financial dependence Threat of physical violence Communities with high rates of crime and violence Hessol et al. CID 2007: 44: 287 -94 A tragic story of the life experience of a poor young black woman, intertwined with a not too subtle message of low health literacy, misconceptions of HIV risk and competing priorities that contribute to excess HIV disease and excess mortality… “they tell me I have HIV and I could die, but I can’t worry about that, I gotta take care of these kids”
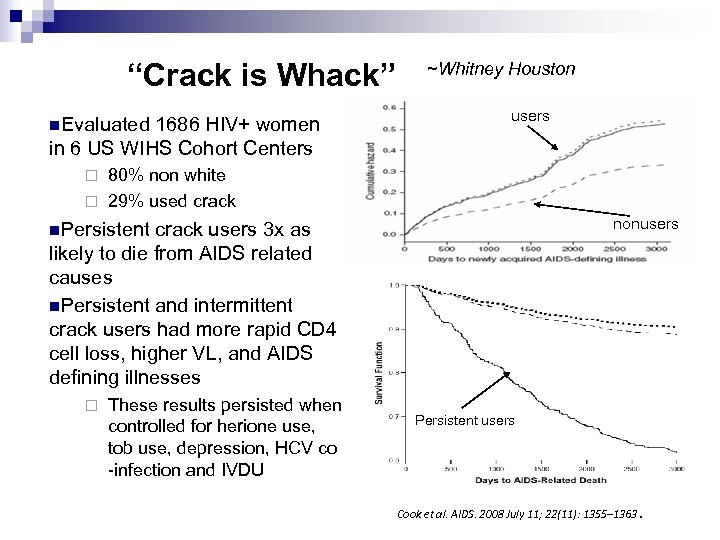 “Crack is Whack” n. Evaluated 1686 HIV+ women in 6 US WIHS Cohort Centers ~Whitney Houston users 80% non white ¨ 29% used crack ¨ nonusers n. Persistent crack users 3 x as likely to die from AIDS related causes n. Persistent and intermittent crack users had more rapid CD 4 cell loss, higher VL, and AIDS defining illnesses ¨ These results persisted when controlled for herione use, tob use, depression, HCV co -infection and IVDU Persistent users Cook et al. AIDS. 2008 July 11; 22(11): 1355– 1363.
“Crack is Whack” n. Evaluated 1686 HIV+ women in 6 US WIHS Cohort Centers ~Whitney Houston users 80% non white ¨ 29% used crack ¨ nonusers n. Persistent crack users 3 x as likely to die from AIDS related causes n. Persistent and intermittent crack users had more rapid CD 4 cell loss, higher VL, and AIDS defining illnesses ¨ These results persisted when controlled for herione use, tob use, depression, HCV co -infection and IVDU Persistent users Cook et al. AIDS. 2008 July 11; 22(11): 1355– 1363.
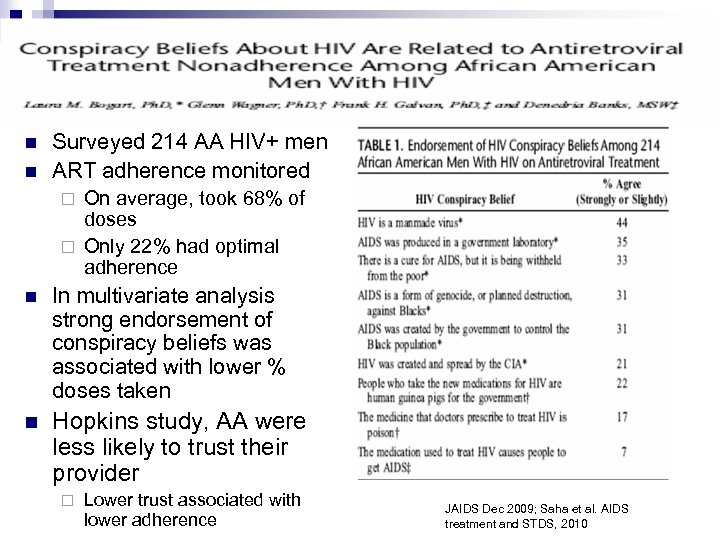 n n Surveyed 214 AA HIV+ men ART adherence monitored On average, took 68% of doses ¨ Only 22% had optimal adherence ¨ n In multivariate analysis strong endorsement of conspiracy beliefs was associated with lower % doses taken n Hopkins study, AA were less likely to trust their provider ¨ Lower trust associated with lower adherence JAIDS Dec 2009; Saha et al. AIDS treatment and STDS, 2010
n n Surveyed 214 AA HIV+ men ART adherence monitored On average, took 68% of doses ¨ Only 22% had optimal adherence ¨ n In multivariate analysis strong endorsement of conspiracy beliefs was associated with lower % doses taken n Hopkins study, AA were less likely to trust their provider ¨ Lower trust associated with lower adherence JAIDS Dec 2009; Saha et al. AIDS treatment and STDS, 2010
 Towards Elimination of Disparities in HIV Prevention Strategies ¨ Decrease focus on “high risk” behavior n Misses persons with low perception of risk ¨ Media campaigns-Black, Latino Radio, BET, MTV, Novellas n Greater than AIDS Campaign 1 ¨ Target youth (Sex Education Curriculum) ¨ Incarcerated individuals n n Aggressive prevention targeting incarcerated individuals during incarceration regardless of HIV status, prevention counseling at discharge MAKE VOLUNTARY TESTING AND CONDOMS UNIVERSALLY AVAILABLE ¨ Identify positives and engage in care n Engagement in HIV care associated with less unprotected sex 1 Greater than AIDS. org~
Towards Elimination of Disparities in HIV Prevention Strategies ¨ Decrease focus on “high risk” behavior n Misses persons with low perception of risk ¨ Media campaigns-Black, Latino Radio, BET, MTV, Novellas n Greater than AIDS Campaign 1 ¨ Target youth (Sex Education Curriculum) ¨ Incarcerated individuals n n Aggressive prevention targeting incarcerated individuals during incarceration regardless of HIV status, prevention counseling at discharge MAKE VOLUNTARY TESTING AND CONDOMS UNIVERSALLY AVAILABLE ¨ Identify positives and engage in care n Engagement in HIV care associated with less unprotected sex 1 Greater than AIDS. org~
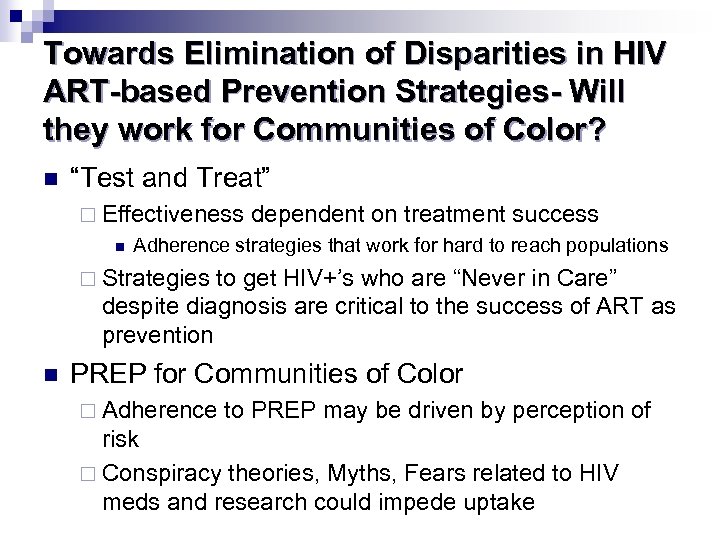 Towards Elimination of Disparities in HIV ART-based Prevention Strategies- Will they work for Communities of Color? n “Test and Treat” ¨ Effectiveness n dependent on treatment success Adherence strategies that work for hard to reach populations ¨ Strategies to get HIV+’s who are “Never in Care” despite diagnosis are critical to the success of ART as prevention n PREP for Communities of Color ¨ Adherence to PREP may be driven by perception of risk ¨ Conspiracy theories, Myths, Fears related to HIV meds and research could impede uptake
Towards Elimination of Disparities in HIV ART-based Prevention Strategies- Will they work for Communities of Color? n “Test and Treat” ¨ Effectiveness n dependent on treatment success Adherence strategies that work for hard to reach populations ¨ Strategies to get HIV+’s who are “Never in Care” despite diagnosis are critical to the success of ART as prevention n PREP for Communities of Color ¨ Adherence to PREP may be driven by perception of risk ¨ Conspiracy theories, Myths, Fears related to HIV meds and research could impede uptake
 Towards Elimination of Disparities in HIVIN Care and ON ART n “Hard to Reach” Populations ¨ Direct and rapid link from + test to HIV care regardless of insurance status n Link with testing centers, STD clinics, health departments ¨ n n Provide case management that links HIV+ to care Systematic follow-up “no shows” Earlier treatment initiation ¨ Provide opportunity for success ¨ Improve n n n success of ART in hard to reach populations Need clinical trials that focus on improving success in diverse populations Improve adherence with visits and treatment Improved Patient-Provider relationships
Towards Elimination of Disparities in HIVIN Care and ON ART n “Hard to Reach” Populations ¨ Direct and rapid link from + test to HIV care regardless of insurance status n Link with testing centers, STD clinics, health departments ¨ n n Provide case management that links HIV+ to care Systematic follow-up “no shows” Earlier treatment initiation ¨ Provide opportunity for success ¨ Improve n n n success of ART in hard to reach populations Need clinical trials that focus on improving success in diverse populations Improve adherence with visits and treatment Improved Patient-Provider relationships
 Provide Culturally Competent HIV Care n Build trust and optimize patient-provider encounter n Be aware of health-related cultural beliefs, including stigma, within the predominant minority groups in your practice Explore the patient’s social context ¨ Life control ¨ Change in environment ¨ Literacy and language ¨ Support systems ¨ n n Negotiate across patient-physician culture to develop a treatment plan that is mutually agreeable Diversity and Cultural Competency n Increase diversity of clinical staff ¨ ¨ Linguistic competency Incentives and training programs for clinicians of color Stone V, et al. HIV/AIDS in U. S. Communities of Color. Springer; New York, NY: 2009. Carrillo JE, et al. Ann Intern Med. 1999; 130: 829 -834. , Stone VE. Clin Infect Dis. 2004; 38: 400 -404.
Provide Culturally Competent HIV Care n Build trust and optimize patient-provider encounter n Be aware of health-related cultural beliefs, including stigma, within the predominant minority groups in your practice Explore the patient’s social context ¨ Life control ¨ Change in environment ¨ Literacy and language ¨ Support systems ¨ n n Negotiate across patient-physician culture to develop a treatment plan that is mutually agreeable Diversity and Cultural Competency n Increase diversity of clinical staff ¨ ¨ Linguistic competency Incentives and training programs for clinicians of color Stone V, et al. HIV/AIDS in U. S. Communities of Color. Springer; New York, NY: 2009. Carrillo JE, et al. Ann Intern Med. 1999; 130: 829 -834. , Stone VE. Clin Infect Dis. 2004; 38: 400 -404.
 Thank You
Thank You


