e9baafe615d598188b66574ded74f467.ppt
- Количество слайдов: 46
 Adapting self-management support strategies to the needs of individuals and groups Roy Batterham Senior Research Fellow Public Health Innovation, Deakin April 11 th 2012
Adapting self-management support strategies to the needs of individuals and groups Roy Batterham Senior Research Fellow Public Health Innovation, Deakin April 11 th 2012
 Outline • What is self management and self management support • Understanding individual needs and customising SMS to the needs of individuals – Summarising behaviour change research, 5 pillars and stages of change – Levels of self management – Functional/life needs approach – Health literacy • Understanding group needs and customising SMS to the needs of groups
Outline • What is self management and self management support • Understanding individual needs and customising SMS to the needs of individuals – Summarising behaviour change research, 5 pillars and stages of change – Levels of self management – Functional/life needs approach – Health literacy • Understanding group needs and customising SMS to the needs of groups
 What is self-management and self-management support?
What is self-management and self-management support?
 Recommended reference Health Behavior Change and Treatment Adherence, Evidence-based Guidelines for Improving Healthcare, 2009 Martin, Leslie, Professor of Psychology, La Sierra University, Riverside Haskard-Zolnierek, Kelly, Assistant Professor of Psychology, Texas State University, San Marcos Di. Matteo, M. Robin, Distinguished Professor of Psychology, University of California, Riverside • 1 Understanding Behavior Change: Theory Behind Informing, Motivating, and Planning for Health • 2 Persuading and Motivating Positive Health Behaviors • 3 Understanding and Remembering • 4 Improving Health Through the Development and Management of Habits • 5 Evaluation of Risks, Decision Making, and Outcomes • 6 Relationships and Communication Between Caregivers and Patients • 7 Effective Collaboration with Patients—On a Tight Schedule • 8 Partnering for Adherence in the Healthcare System
Recommended reference Health Behavior Change and Treatment Adherence, Evidence-based Guidelines for Improving Healthcare, 2009 Martin, Leslie, Professor of Psychology, La Sierra University, Riverside Haskard-Zolnierek, Kelly, Assistant Professor of Psychology, Texas State University, San Marcos Di. Matteo, M. Robin, Distinguished Professor of Psychology, University of California, Riverside • 1 Understanding Behavior Change: Theory Behind Informing, Motivating, and Planning for Health • 2 Persuading and Motivating Positive Health Behaviors • 3 Understanding and Remembering • 4 Improving Health Through the Development and Management of Habits • 5 Evaluation of Risks, Decision Making, and Outcomes • 6 Relationships and Communication Between Caregivers and Patients • 7 Effective Collaboration with Patients—On a Tight Schedule • 8 Partnering for Adherence in the Healthcare System
 Management of chronic disease Health care workers
Management of chronic disease Health care workers
 Management of chronic disease Self management +/- carer & family +/- community
Management of chronic disease Self management +/- carer & family +/- community
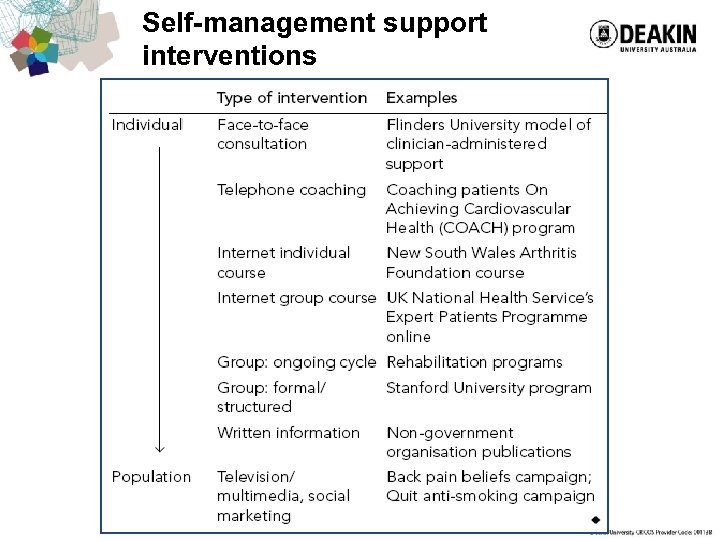 Self-management support interventions Jordan JE, Osborne RH. Chronic disease self-management education programs: challenges ahead Med J Aust 2007; 186(2): 84 -7.
Self-management support interventions Jordan JE, Osborne RH. Chronic disease self-management education programs: challenges ahead Med J Aust 2007; 186(2): 84 -7.
 Variability: Understanding individual needs and customising SMS to the needs of individuals
Variability: Understanding individual needs and customising SMS to the needs of individuals
 Three types of behaviour change theories 1. Predictive theories: Theories that try to predict which people in a group are likely to change and which are not 2. Stages of change theories: Theories that try and help people understand the process of change and how they can help it 3. Integrative theories: Theories that try and draw all of the above together
Three types of behaviour change theories 1. Predictive theories: Theories that try to predict which people in a group are likely to change and which are not 2. Stages of change theories: Theories that try and help people understand the process of change and how they can help it 3. Integrative theories: Theories that try and draw all of the above together
 Predictive theories have emphasised. . . • Cues and stimuli (health beliefs model) • Beliefs (and attitudes) (health beliefs model) • Personal perceptions of what is normal and other competing values (personal norms) (theory of reasoned action) • Perceived behavioural control (general: locus of control; specific: self-efficacy) (modified health beliefs model theory of planned behaviour) • Intentions (theory of reasoned action) • Environmental factors (social cognitive theory)
Predictive theories have emphasised. . . • Cues and stimuli (health beliefs model) • Beliefs (and attitudes) (health beliefs model) • Personal perceptions of what is normal and other competing values (personal norms) (theory of reasoned action) • Perceived behavioural control (general: locus of control; specific: self-efficacy) (modified health beliefs model theory of planned behaviour) • Intentions (theory of reasoned action) • Environmental factors (social cognitive theory)
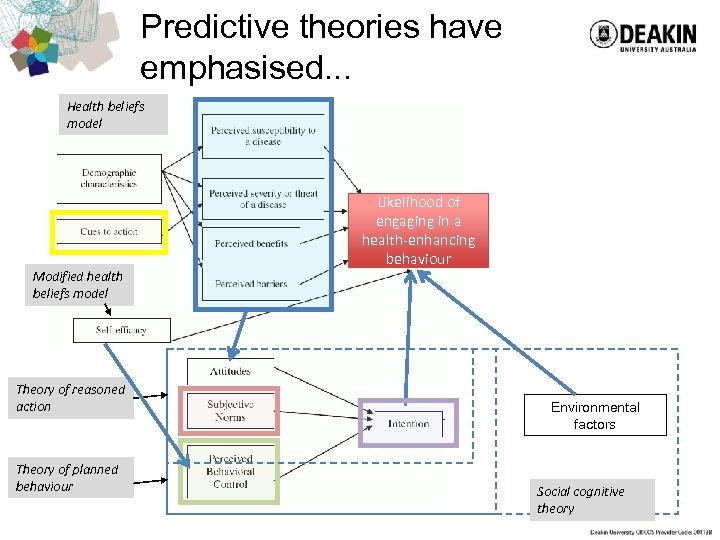 Predictive theories have emphasised. . . Health beliefs model Modified health beliefs model Theory of reasoned action Theory of planned behaviour Likelihood of engaging in a health-enhancing behaviour Environmental factors Social cognitive theory
Predictive theories have emphasised. . . Health beliefs model Modified health beliefs model Theory of reasoned action Theory of planned behaviour Likelihood of engaging in a health-enhancing behaviour Environmental factors Social cognitive theory
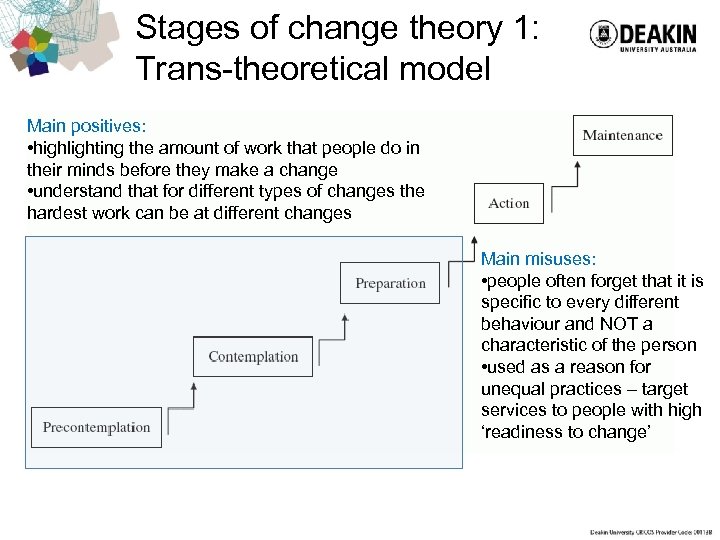 Stages of change theory 1: Trans-theoretical model Main positives: • highlighting the amount of work that people do in their minds before they make a change • understand that for different types of changes the hardest work can be at different changes Main misuses: • people often forget that it is specific to every different behaviour and NOT a characteristic of the person • used as a reason for unequal practices – target services to people with high ‘readiness to change’
Stages of change theory 1: Trans-theoretical model Main positives: • highlighting the amount of work that people do in their minds before they make a change • understand that for different types of changes the hardest work can be at different changes Main misuses: • people often forget that it is specific to every different behaviour and NOT a characteristic of the person • used as a reason for unequal practices – target services to people with high ‘readiness to change’
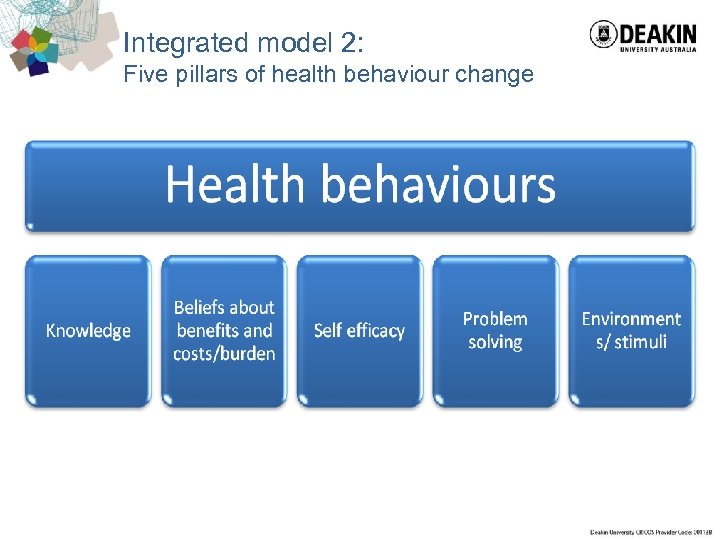 Integrated model 2: Five pillars of health behaviour change
Integrated model 2: Five pillars of health behaviour change
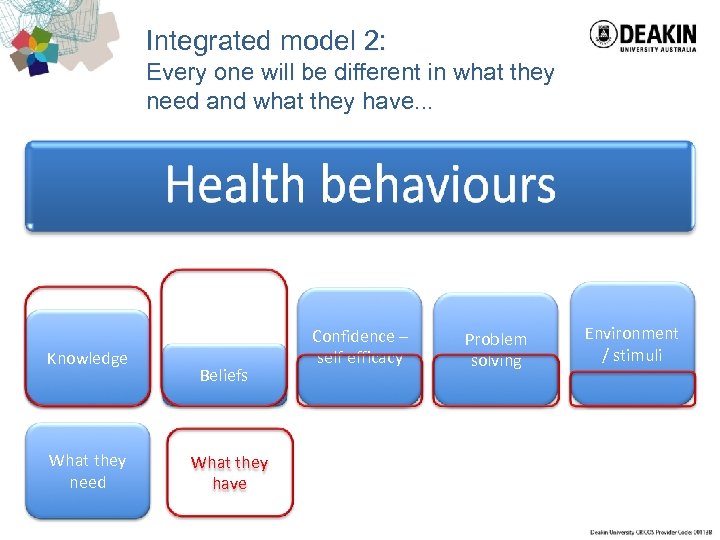 Integrated model 2: Every one will be different in what they need and what they have. . . Knowledge What they need Beliefs What they have Confidence – self efficacy Problem solving Environment / stimuli
Integrated model 2: Every one will be different in what they need and what they have. . . Knowledge What they need Beliefs What they have Confidence – self efficacy Problem solving Environment / stimuli
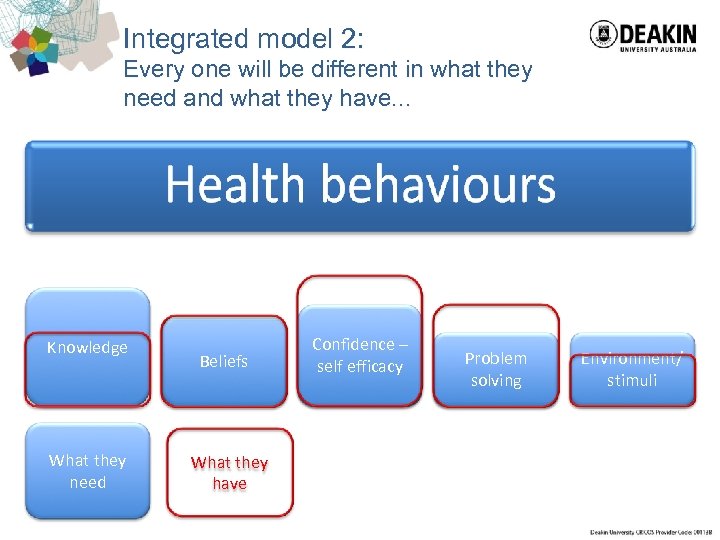 Integrated model 2: Every one will be different in what they need and what they have. . . Knowledge What they need Beliefs What they have Confidence – self efficacy Problem solving Environment/ stimuli
Integrated model 2: Every one will be different in what they need and what they have. . . Knowledge What they need Beliefs What they have Confidence – self efficacy Problem solving Environment/ stimuli
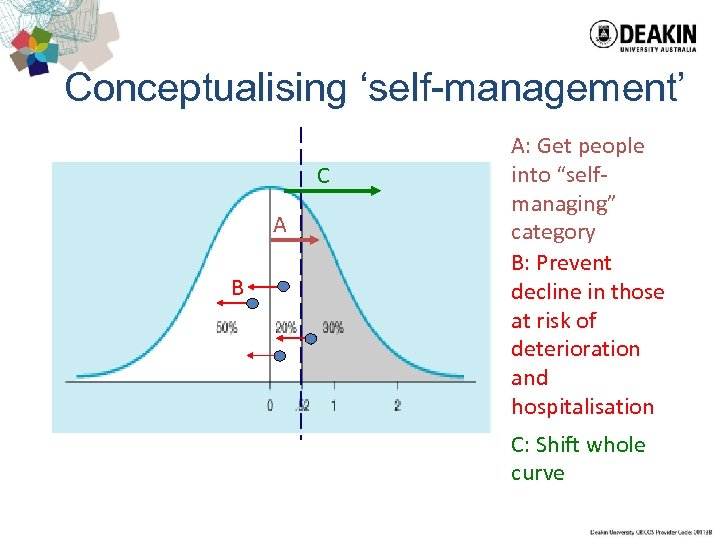 Conceptualising ‘self-management’ C A B A: Get people into “selfmanaging” category B: Prevent decline in those at risk of deterioration and hospitalisation C: Shift whole curve
Conceptualising ‘self-management’ C A B A: Get people into “selfmanaging” category B: Prevent decline in those at risk of deterioration and hospitalisation C: Shift whole curve
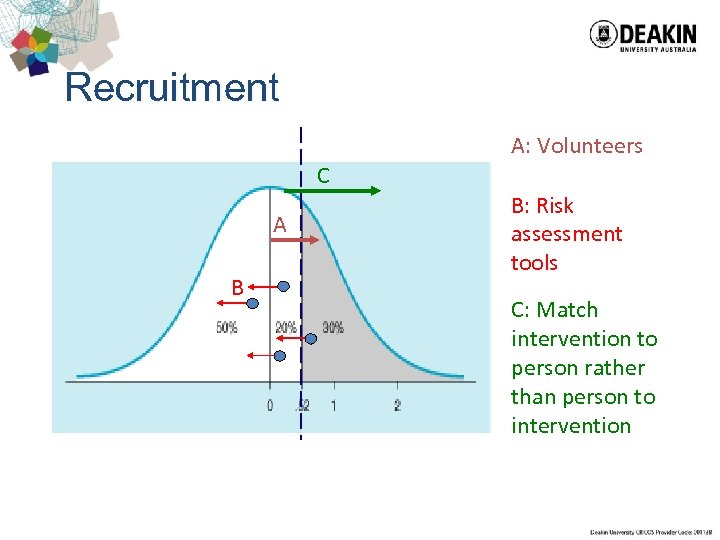 Recruitment A: Volunteers C A B B: Risk assessment tools C: Match intervention to person rather than person to intervention
Recruitment A: Volunteers C A B B: Risk assessment tools C: Match intervention to person rather than person to intervention
 Risk assessment tools • The best risk assessment tools in the world predict a maximum of about 20% variance in hospital utilisation over 12 months or more. Most do much worse. • If a biological screening tool had a false positive and false negative rates > 80% anyone who suggested using it would be laughed out of town • Only useful for 2 month readmission risk • Risk assessment tools should be used for care-planning NOT screening
Risk assessment tools • The best risk assessment tools in the world predict a maximum of about 20% variance in hospital utilisation over 12 months or more. Most do much worse. • If a biological screening tool had a false positive and false negative rates > 80% anyone who suggested using it would be laughed out of town • Only useful for 2 month readmission risk • Risk assessment tools should be used for care-planning NOT screening
 Variability: thinking about complexity
Variability: thinking about complexity
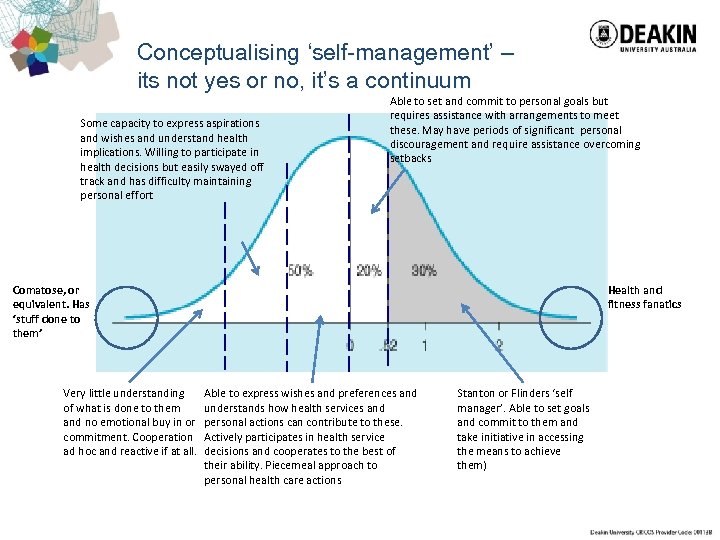 Conceptualising ‘self-management’ – its not yes or no, it’s a continuum Some capacity to express aspirations and wishes and understand health implications. Willing to participate in health decisions but easily swayed off track and has difficulty maintaining personal effort Able to set and commit to personal goals but requires assistance with arrangements to meet these. May have periods of significant personal discouragement and require assistance overcoming setbacks Comatose, or equivalent. Has ‘stuff done to them’ Very little understanding of what is done to them and no emotional buy in or commitment. Cooperation ad hoc and reactive if at all. Health and fitness fanatics Able to express wishes and preferences and understands how health services and personal actions can contribute to these. Actively participates in health service decisions and cooperates to the best of their ability. Piecemeal approach to personal health care actions Stanton or Flinders ‘self manager’. Able to set goals and commit to them and take initiative in accessing the means to achieve them)
Conceptualising ‘self-management’ – its not yes or no, it’s a continuum Some capacity to express aspirations and wishes and understand health implications. Willing to participate in health decisions but easily swayed off track and has difficulty maintaining personal effort Able to set and commit to personal goals but requires assistance with arrangements to meet these. May have periods of significant personal discouragement and require assistance overcoming setbacks Comatose, or equivalent. Has ‘stuff done to them’ Very little understanding of what is done to them and no emotional buy in or commitment. Cooperation ad hoc and reactive if at all. Health and fitness fanatics Able to express wishes and preferences and understands how health services and personal actions can contribute to these. Actively participates in health service decisions and cooperates to the best of their ability. Piecemeal approach to personal health care actions Stanton or Flinders ‘self manager’. Able to set goals and commit to them and take initiative in accessing the means to achieve them)
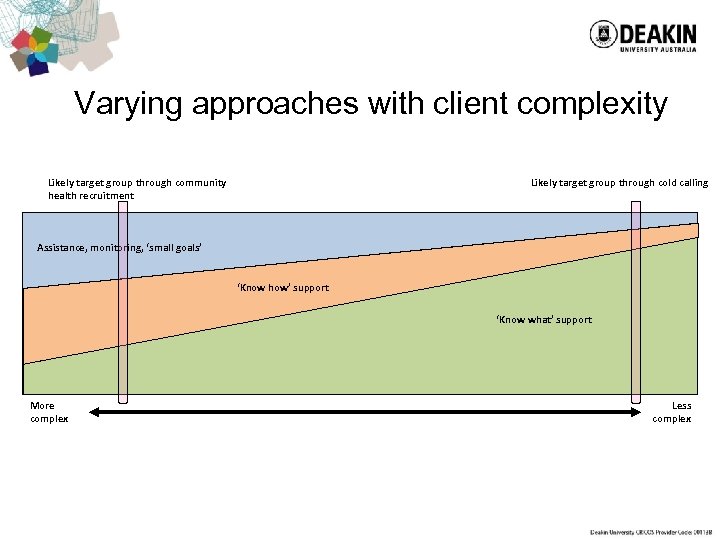 Varying approaches with client complexity Likely target group through community health recruitment Likely target group through cold calling Assistance, monitoring, ‘small goals’ ‘Know how’ support ‘Know what’ support More complex Less complex
Varying approaches with client complexity Likely target group through community health recruitment Likely target group through cold calling Assistance, monitoring, ‘small goals’ ‘Know how’ support ‘Know what’ support More complex Less complex
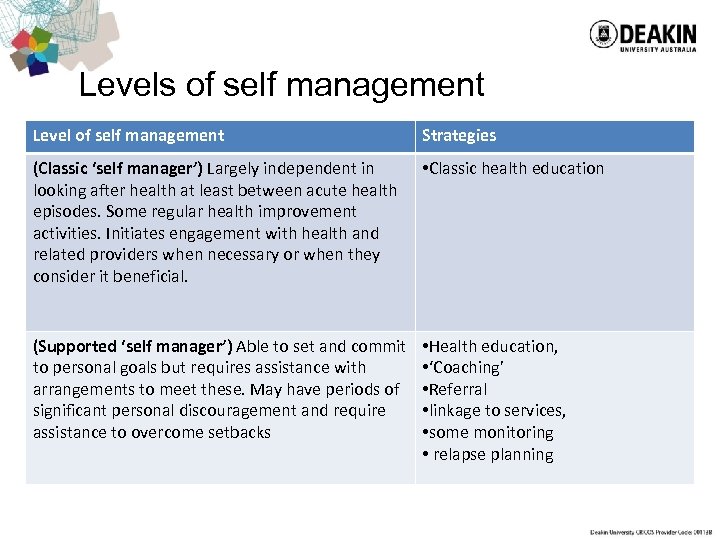 Levels of self management Level of self management Strategies (Classic ‘self manager’) Largely independent in looking after health at least between acute health episodes. Some regular health improvement activities. Initiates engagement with health and related providers when necessary or when they consider it beneficial. • Classic health education (Supported ‘self manager’) Able to set and commit to personal goals but requires assistance with arrangements to meet these. May have periods of significant personal discouragement and require assistance to overcome setbacks • Health education, • ‘Coaching’ • Referral • linkage to services, • some monitoring • relapse planning
Levels of self management Level of self management Strategies (Classic ‘self manager’) Largely independent in looking after health at least between acute health episodes. Some regular health improvement activities. Initiates engagement with health and related providers when necessary or when they consider it beneficial. • Classic health education (Supported ‘self manager’) Able to set and commit to personal goals but requires assistance with arrangements to meet these. May have periods of significant personal discouragement and require assistance to overcome setbacks • Health education, • ‘Coaching’ • Referral • linkage to services, • some monitoring • relapse planning
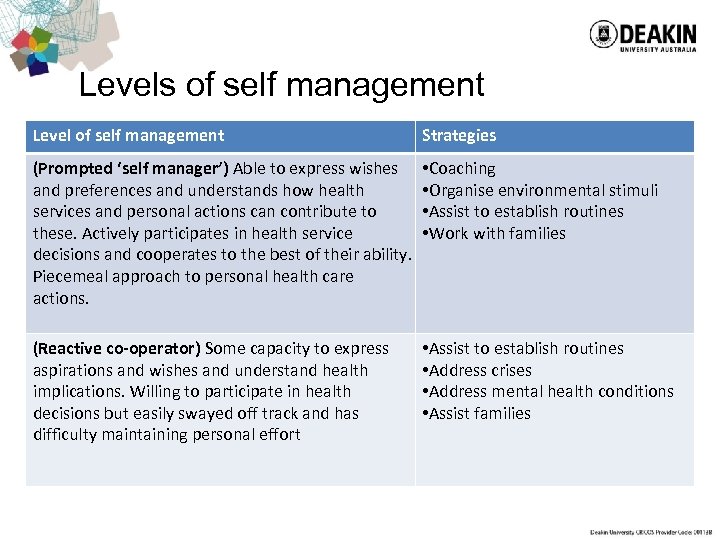 Levels of self management Level of self management Strategies (Prompted ‘self manager’) Able to express wishes and preferences and understands how health services and personal actions can contribute to these. Actively participates in health service decisions and cooperates to the best of their ability. Piecemeal approach to personal health care actions. • Coaching • Organise environmental stimuli • Assist to establish routines • Work with families (Reactive co-operator) Some capacity to express aspirations and wishes and understand health implications. Willing to participate in health decisions but easily swayed off track and has difficulty maintaining personal effort • Assist to establish routines • Address crises • Address mental health conditions • Assist families
Levels of self management Level of self management Strategies (Prompted ‘self manager’) Able to express wishes and preferences and understands how health services and personal actions can contribute to these. Actively participates in health service decisions and cooperates to the best of their ability. Piecemeal approach to personal health care actions. • Coaching • Organise environmental stimuli • Assist to establish routines • Work with families (Reactive co-operator) Some capacity to express aspirations and wishes and understand health implications. Willing to participate in health decisions but easily swayed off track and has difficulty maintaining personal effort • Assist to establish routines • Address crises • Address mental health conditions • Assist families
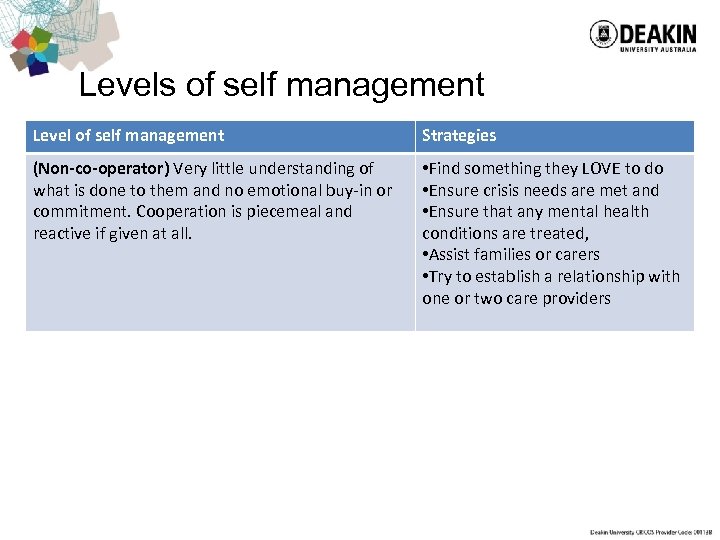 Levels of self management Level of self management Strategies (Non-co-operator) Very little understanding of what is done to them and no emotional buy-in or commitment. Cooperation is piecemeal and reactive if given at all. • Find something they LOVE to do • Ensure crisis needs are met and • Ensure that any mental health conditions are treated, • Assist families or carers • Try to establish a relationship with one or two care providers
Levels of self management Level of self management Strategies (Non-co-operator) Very little understanding of what is done to them and no emotional buy-in or commitment. Cooperation is piecemeal and reactive if given at all. • Find something they LOVE to do • Ensure crisis needs are met and • Ensure that any mental health conditions are treated, • Assist families or carers • Try to establish a relationship with one or two care providers
 People at highest risk require more intensive interventions and cost more. . . but not as much as multiple admissions to hospital
People at highest risk require more intensive interventions and cost more. . . but not as much as multiple admissions to hospital
 Variability: adding mental health issues
Variability: adding mental health issues
 The ‘complex’ client Often, clients who don't 'succeed' in traditional self-management programs are dismissed as having no/low self-management capacity. Some have described these clients as fitting into two broad categories those with cognitive impairment and those with multiple comorbidities or concerns. We hope to design 'Stepping up. . . ' in such a way that it also supports this later group. To do so we make a number of ASSUMPTIONS about this group: Most of them are in fact willing and able to make changes to improve their health and wellbeing (although the extent and type of change may conflict with health professionals priorities). The lack of 'success' of SMS programs in engaging this group in the past has largely been due to a lack of 'fit' between the program and the client's needs. Improving the 'fit' between client needs and the program requires a different approach
The ‘complex’ client Often, clients who don't 'succeed' in traditional self-management programs are dismissed as having no/low self-management capacity. Some have described these clients as fitting into two broad categories those with cognitive impairment and those with multiple comorbidities or concerns. We hope to design 'Stepping up. . . ' in such a way that it also supports this later group. To do so we make a number of ASSUMPTIONS about this group: Most of them are in fact willing and able to make changes to improve their health and wellbeing (although the extent and type of change may conflict with health professionals priorities). The lack of 'success' of SMS programs in engaging this group in the past has largely been due to a lack of 'fit' between the program and the client's needs. Improving the 'fit' between client needs and the program requires a different approach
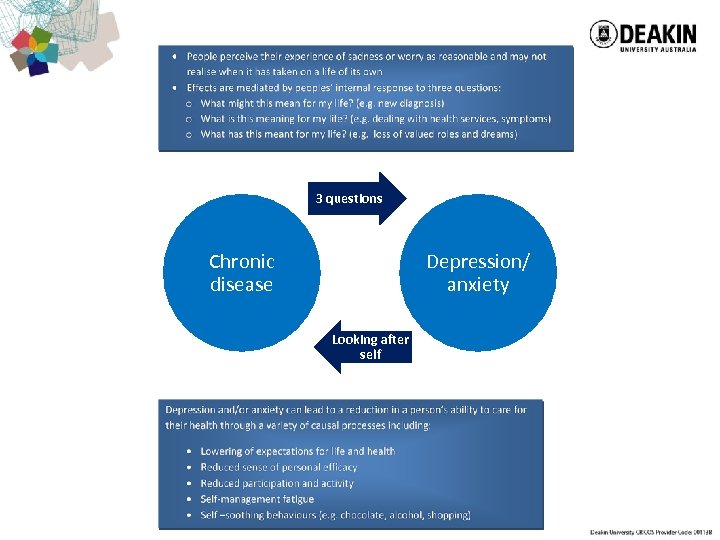 3 questions Chronic disease Depression/ anxiety Looking after self
3 questions Chronic disease Depression/ anxiety Looking after self
 Improving Treatment ‘Fit’ 3 features of the ‘Stepping up. . . ’ model hope to improve treatment fit: 1. Problem prioritisation - using a collaborative case formulation approach 2. Tailored content - rather than a one size fits all approach 3. Flexibility in treatment intensity - capacity to scale down treatment expectations and burden
Improving Treatment ‘Fit’ 3 features of the ‘Stepping up. . . ’ model hope to improve treatment fit: 1. Problem prioritisation - using a collaborative case formulation approach 2. Tailored content - rather than a one size fits all approach 3. Flexibility in treatment intensity - capacity to scale down treatment expectations and burden
 © 2011, Deakin University, Australia.
© 2011, Deakin University, Australia.
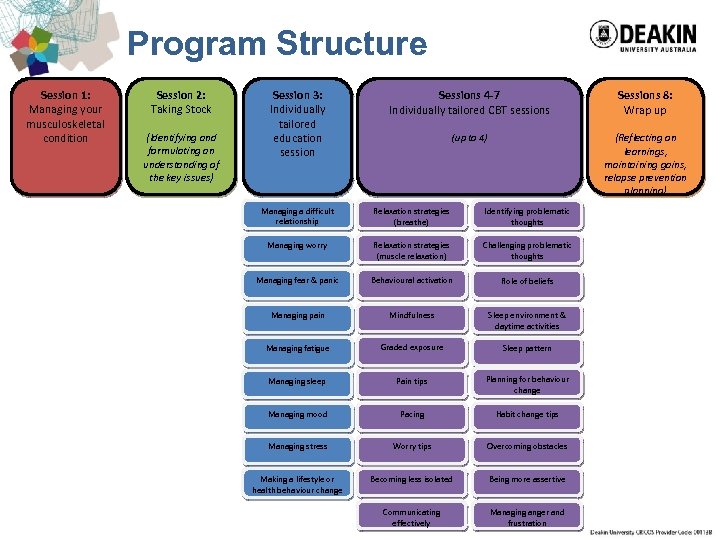 Program Structure Session 1: Managing your musculoskeletal condition Session 2: Taking Stock (Identifying and formulating an understanding of the key issues) Session 3: Individually tailored education session Sessions 4 -7 Individually tailored CBT sessions Sessions 8: Wrap up (up to 4) (Reflecting on learnings, maintaining gains, relapse prevention planning) Managing a difficult relationship Relaxation strategies (breathe) Identifying problematic thoughts Managing worry Relaxation strategies (muscle relaxation) Challenging problematic thoughts Managing fear & panic Behavioural activation Role of beliefs Managing pain Mindfulness Sleep environment & daytime activities Managing fatigue Graded exposure Sleep pattern Managing sleep Pain tips Planning for behaviour change Managing mood Pacing Habit change tips Managing stress Worry tips Overcoming obstacles Making a lifestyle or health behaviour change Becoming less isolated Being more assertive Communicating effectively Managing anger and frustration
Program Structure Session 1: Managing your musculoskeletal condition Session 2: Taking Stock (Identifying and formulating an understanding of the key issues) Session 3: Individually tailored education session Sessions 4 -7 Individually tailored CBT sessions Sessions 8: Wrap up (up to 4) (Reflecting on learnings, maintaining gains, relapse prevention planning) Managing a difficult relationship Relaxation strategies (breathe) Identifying problematic thoughts Managing worry Relaxation strategies (muscle relaxation) Challenging problematic thoughts Managing fear & panic Behavioural activation Role of beliefs Managing pain Mindfulness Sleep environment & daytime activities Managing fatigue Graded exposure Sleep pattern Managing sleep Pain tips Planning for behaviour change Managing mood Pacing Habit change tips Managing stress Worry tips Overcoming obstacles Making a lifestyle or health behaviour change Becoming less isolated Being more assertive Communicating effectively Managing anger and frustration
 Consumer Concerns Eight presenting concerns addressed: 1. 2. 3. 4. 5. 6. 7. 8. Pain Fatigue Mood Anxiety & worry Stress Sleep Relationship issues Lifestyle change © 2011, Deakin University, Australia.
Consumer Concerns Eight presenting concerns addressed: 1. 2. 3. 4. 5. 6. 7. 8. Pain Fatigue Mood Anxiety & worry Stress Sleep Relationship issues Lifestyle change © 2011, Deakin University, Australia.
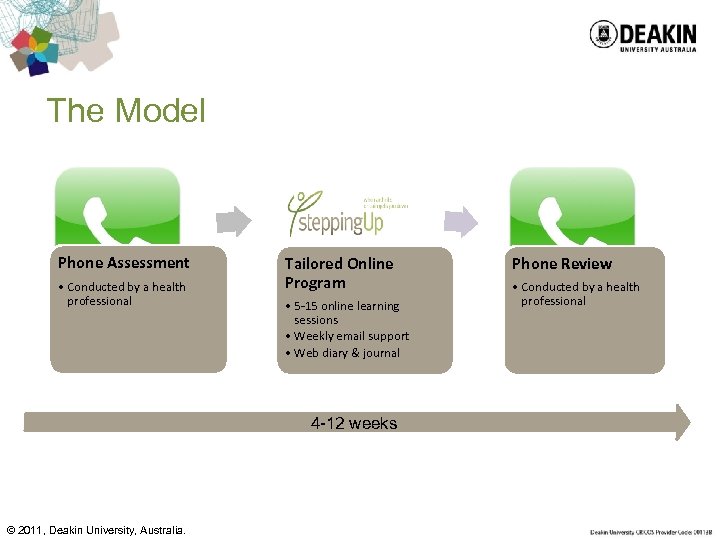 The Model Phone Assessment • Conducted by a health professional Tailored Online Program • 5 -15 online learning sessions • Weekly email support • Web diary & journal 4 -12 weeks © 2011, Deakin University, Australia. Phone Review • Conducted by a health professional
The Model Phone Assessment • Conducted by a health professional Tailored Online Program • 5 -15 online learning sessions • Weekly email support • Web diary & journal 4 -12 weeks © 2011, Deakin University, Australia. Phone Review • Conducted by a health professional
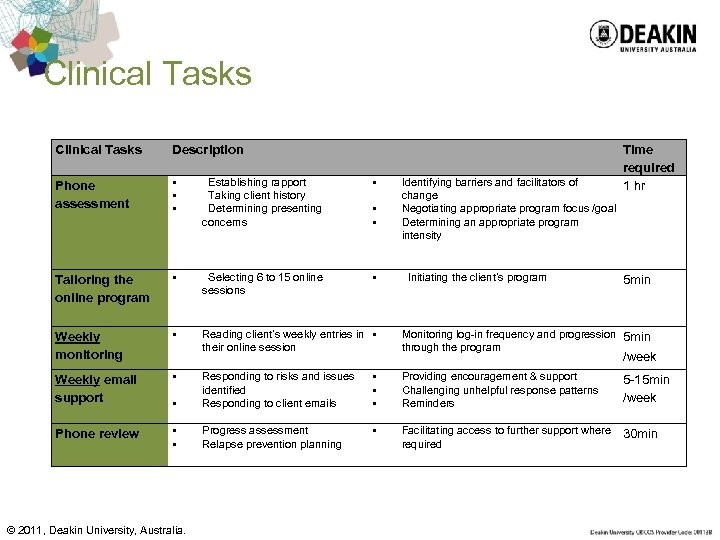 Clinical Tasks Description Phone assessment § § § Establishing rapport Taking client history Determining presenting concerns § Tailoring the online program § Selecting 6 to 15 online sessions § Weekly monitoring § Reading client’s weekly entries in § their online session Weekly email support § Phone review § § Identifying barriers and facilitators of change Negotiating appropriate program focus /goal Determining an appropriate program intensity Initiating the client’s program Time required 1 hr 5 min Monitoring log-in frequency and progression 5 min through the program /week § Responding to risks and issues identified Responding to client emails § § § Providing encouragement & support Challenging unhelpful response patterns Reminders 5 -15 min /week § § Progress assessment Relapse prevention planning § Facilitating access to further support where required 30 min © 2011, Deakin University, Australia.
Clinical Tasks Description Phone assessment § § § Establishing rapport Taking client history Determining presenting concerns § Tailoring the online program § Selecting 6 to 15 online sessions § Weekly monitoring § Reading client’s weekly entries in § their online session Weekly email support § Phone review § § Identifying barriers and facilitators of change Negotiating appropriate program focus /goal Determining an appropriate program intensity Initiating the client’s program Time required 1 hr 5 min Monitoring log-in frequency and progression 5 min through the program /week § Responding to risks and issues identified Responding to client emails § § § Providing encouragement & support Challenging unhelpful response patterns Reminders 5 -15 min /week § § Progress assessment Relapse prevention planning § Facilitating access to further support where required 30 min © 2011, Deakin University, Australia.
 Variability: Understanding group needs and customising SMS to the needs of groups
Variability: Understanding group needs and customising SMS to the needs of groups
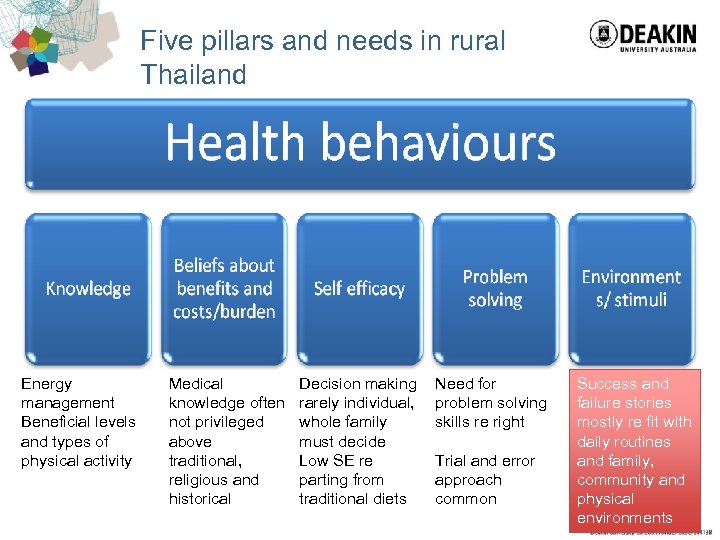 Five pillars and needs in rural Thailand Energy management Beneficial levels and types of physical activity Medical knowledge often not privileged above traditional, religious and historical Decision making rarely individual, whole family must decide Low SE re parting from traditional diets Need for problem solving skills re right Trial and error approach common Success and failure stories mostly re fit with daily routines and family, community and physical environments
Five pillars and needs in rural Thailand Energy management Beneficial levels and types of physical activity Medical knowledge often not privileged above traditional, religious and historical Decision making rarely individual, whole family must decide Low SE re parting from traditional diets Need for problem solving skills re right Trial and error approach common Success and failure stories mostly re fit with daily routines and family, community and physical environments
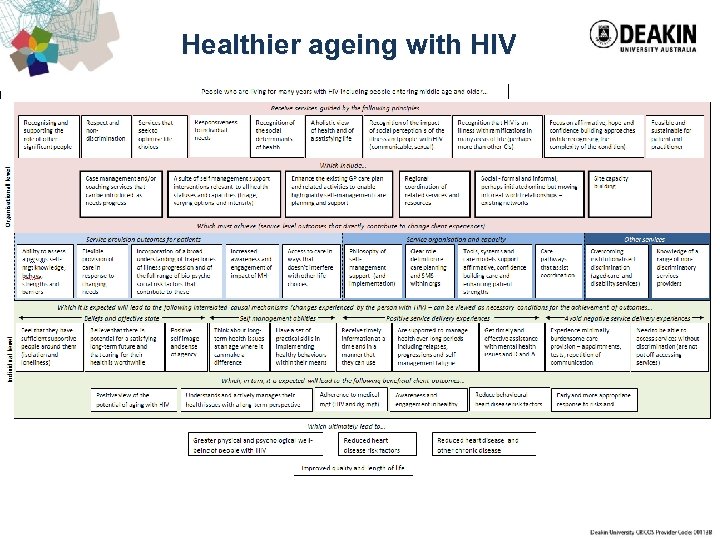 Healthier ageing with HIV
Healthier ageing with HIV
 Self management beyond the ‘self’ What does self management mean for: – People living in aboriginal communities? – A tired mother whose family rebels at eating her ‘diabetic’ food? – People living in a village in Thailand? – A person with a disability who is dependent on others for many care needs? – An adolescent whose priority is developing and maintaining an acceptable sense of self among her/his peers? – Anyone whose health related choices are made by, or largely determined by, people other than themselves?
Self management beyond the ‘self’ What does self management mean for: – People living in aboriginal communities? – A tired mother whose family rebels at eating her ‘diabetic’ food? – People living in a village in Thailand? – A person with a disability who is dependent on others for many care needs? – An adolescent whose priority is developing and maintaining an acceptable sense of self among her/his peers? – Anyone whose health related choices are made by, or largely determined by, people other than themselves?
 Health Literacy: several definitions • “Health literacy represents the cognitive and social skills which determine the motivation and ability of individuals to gain access to, understand use information in ways which promote and maintain good health” (World Health Organization) • “Health literacy is the ability to make sound health decisions in the context of everyday life – at home, in the community, at the workplace, the healthcare system, the market place and the political arena” (Kickbusch, 2001)
Health Literacy: several definitions • “Health literacy represents the cognitive and social skills which determine the motivation and ability of individuals to gain access to, understand use information in ways which promote and maintain good health” (World Health Organization) • “Health literacy is the ability to make sound health decisions in the context of everyday life – at home, in the community, at the workplace, the healthcare system, the market place and the political arena” (Kickbusch, 2001)
 Why is everyone talking about Health Literacy? • Previous tools failed • New national / international surveys – Australia, Taiwan, Europe • Public Health and Health Promotion still do not meet the needs of those with low literacy • Accepted as a priority in International Union for Health Promotion and Health Education
Why is everyone talking about Health Literacy? • Previous tools failed • New national / international surveys – Australia, Taiwan, Europe • Public Health and Health Promotion still do not meet the needs of those with low literacy • Accepted as a priority in International Union for Health Promotion and Health Education
 Why is everyone talking about Health Literacy? • Health education, prevention and disease management programs continue to fail to engage and improve outcomes for people who are most at risk –Why is this?
Why is everyone talking about Health Literacy? • Health education, prevention and disease management programs continue to fail to engage and improve outcomes for people who are most at risk –Why is this?
 The new person-centred health literacy Strongly Agree—Strongly disagree 1. Healthcare provider support I have at least one health provider who knows me well 2. Perceived information adequacy I have all the information I need to manage my health properly 3. Taking responsibility for health I set my own goals about health and fitness 4. Being health focused My health is important to me 5. Social support If I need help, I have plenty of people I can rely on Cannot do—Very easy 7. Agency in relationships with providers Discuss things with healthcare providers until you understand all you need to 8. Navigating the health system Work out what is the best care for you 9. Ability to access health information Get health information in words you understand 10. Reading, writing, understanding Follow the instructions from healthcare providers properly 6. Critical appraisal 11. Beliefs and values I know which places provide health information that I can trust Getting sick is part of getting old
The new person-centred health literacy Strongly Agree—Strongly disagree 1. Healthcare provider support I have at least one health provider who knows me well 2. Perceived information adequacy I have all the information I need to manage my health properly 3. Taking responsibility for health I set my own goals about health and fitness 4. Being health focused My health is important to me 5. Social support If I need help, I have plenty of people I can rely on Cannot do—Very easy 7. Agency in relationships with providers Discuss things with healthcare providers until you understand all you need to 8. Navigating the health system Work out what is the best care for you 9. Ability to access health information Get health information in words you understand 10. Reading, writing, understanding Follow the instructions from healthcare providers properly 6. Critical appraisal 11. Beliefs and values I know which places provide health information that I can trust Getting sick is part of getting old
 Requirements for a Thai Health Literacy evaluation system • Cultural issues – Alternatives to just focusing on the individual – Beliefs about sickness – Cultural diversity • Health system issues – ? Health volunteers as ‘health literacy workers’ – Health literacy needs of service providers – Priority on equity – historical and present • Health literacy for the illiterate
Requirements for a Thai Health Literacy evaluation system • Cultural issues – Alternatives to just focusing on the individual – Beliefs about sickness – Cultural diversity • Health system issues – ? Health volunteers as ‘health literacy workers’ – Health literacy needs of service providers – Priority on equity – historical and present • Health literacy for the illiterate
 Thank you roy. batterham@deakin. edu. au
Thank you roy. batterham@deakin. edu. au


